
To Print: Click your browser's PRINT button.
NOTE:
To view the article with Web enhancements, go to:
http://www.medscape.com/viewarticle/416999
Chronic Prostatitis: A Myofascial Pain Syndrome?
Dirk-Henrik Zermann, MD, Manabu Ishigooka, MD, Ragi Doggweiler, MD, Richard A. Schmidt, MD,
University of Colorado Health Sciences Center, Denver.
Infect Urol 12(3):84-92, 1999. © 1999 Cliggott Publishing, Division of SCP Communications
Posted 05/01/1999
Abstract and Introduction
Abstract
Chronic abacterial prostatitis with associated pain remains a diagnostic and therapeutic challenge. Although the
focus is most commonly a bacterial etiology, given the often unsuccessful results of antimicrobial therapy to
relieve symptoms, it is reasonable to ask whether chronic pelvic pain syndrome may be a consequence of a
functional disease within the pelvis. An analysis of clinical and urodynamic findings in 103 men with a complaint
of chronic prostatitis-chronic pelvic pain was carried out with a neurourologic focus to evaluate the role of pelvic
floor dysfunction as a cause of symptoms. All patients included in this study had negative microbiologic tests
before entering the study group. A significant number of the men had neurologic dysfunction.
Introduction
Men with pain in the genitourinary tract, a common problem, are generally given a descriptive diagnosis such as
orchialgia, chronic abacterial prostatitis, or prostatodynia. The latter 2 terms have historically been used to
classify benign prostatic disorders.
[1]
These classifications have helped to provide guidelines for antibiotic
therapy in prostatic diseases. However, these same classifications have not adequately explained neurologic
pain mechanisms or defined potential therapies to relieve symptoms in men with pelvic pain syndromes. Thus,
the National Institutes of Health (NIH) recently redefined the categories of prostatitis (Table I).
[2]
Male voiding dysfunction is often associated with discomfort or pain in the suprapubic or perineal region, testes,
tip of the penis, and low back area. Neural dysregulation of the lower urinary tract could manifest as symptoms
of frequency and urgency.
Much of the research regarding prostatitis syndromes has centered around microbiology as an etiology.
Investigations have focused on cultures of prostatic secretions and polymerase chain reaction to identify various
organisms responsible for inflammation in the prostate.
[3-5]
Most patients continue to be treated with repeated
antibiotic regimens without significant relief.
[6-8]
In recent years, alpha-blockers, because they act on smooth muscle of the bladder neck and prostate, have
been found to be therapeutically useful in prostatitis syndromes.
[9]
Furthermore, investigations show a
correlation between symptoms of prostatitis and those of bladder dysfunction.
[10,11]
Additionally, although
infection is not a prerequisite for symptoms, it is possible that the presence of an infectious organism results in
an immune reaction causing inflammation and subsequent pain and other symptoms.
Chronic prostatitis-chronic pelvic pain syndrome (CPPS) remains a diagnostic and therapeutic enigma. Thus,
other approaches have been utilized to explain and treat this condition. A neurobehavioral perspective is
emerging as a plausible basis for diagnosing and treating some patients with CPPS. The current study was
conducted to evaluate voiding dysfunction and pelvic pain in 103 men through a retrospective review of
symptoms, physical examination, and urodynamic findings.
Página 1 de 8
Chronic Prostatitis: A Myofascial Pain Syndrome?
26/8/2005
http://www.medscape.com/viewarticle/416999_print

Patients and Methods
Patients who had been treated at the University of Colorado Health Sciences Center Clinic in Denver for voiding
dysfunction and pelvic pain were the subjects of this retrospective review. The clinic functions primarily as a
tertiary care center for patients referred with functional disorders of the lower urinary tract. The clinic utilizes a
standardized approach with all new patients, including evaluating past medical history with a focus on previous
infection or inflammation, surgery, and traumatic events; documenting current pain and dysfunctional voiding
behavior; and evaluating other conditions that are potentially related to somatic and autonomic dysregulation.
The clinical examination includes a neurourologic investigation that evaluates the pelvic floor muscles via rectal
examination. Voluntary contraction and, by implication, control of the pelvic muscles are assessed. Urodynamic
studies are also performed. Sphincter function profiles (microtip catheter) are performed in a staged fashion to
record the reflex reactivity of the sphincter to light touch. Sensation experienced by the patient to catheter
withdrawal is noted. Hypersensitivity is scored as none, mild, or significant. Basal sphincter tone and behavior
are recorded continuously during bladder filling and voiding by keeping the pressure transducer within the
external urethral sphincter region. Overall pelvic floor activity is monitored via an intra-anal surface electrode
(Dantec, Denmark).
The urodynamic database includes a cystometrogram; uroflow measurement; and measurement of sphincter
sensitivity and closure pressures at rest and during active filling; urethral functional length with a full and empty
bladder; and the ability of the patient to voluntarily contract and relax the sphincter with a "hold" command.
All study patients had been screened with a urine analysis and culture to exclude a microbiologic basis for
symptoms, and cystoscopy or uroradiology to exclude significant morphologic changes within the lower urinary
tract.
Between August 1994 and August 1997, 103 patients with the main complaint of pelvic pain of at least 12
months' duration were evaluated (Table II). All patients had undergone extensive urologic and microbiologic
evaluation -- as well as several therapeutic attempts without relief of pain -- before being seen at the clinic. All
patients were considered to have NIH category IIIb noninflammatory chronic pel-vic pain syndrome. The majority
of patients had pain within the perineum and testicular regions.
Results
Findings from a total of 103 men (mean age, 47 years, range, 23-89) were included in the review. The most
common lower urinary tract symptoms reported by patients included a slow, weak urinary stream (n=65) and
hesitancy and frequency (n=16). Incontinence (n=4) and retention (n=5) were rare. A small percentage of
patients reported headache (n=11) and bowel (n=8) and erectile (n=6) dysfunction. One individual reported pain
in both feet, the onset and severity of which paralleled symptoms of dysfunctional voiding.
Four patients had a history of preexisting neurologic problems: myelomeningocele (n=1), spinal cord
malformation (n=2), and Persian Gulf syndrome (n=1). A history of previous surgery was reported in 37 patients
(35.9%) (Table III), 25 of whom had no pain before surgery. In these cases, pain began as a consequence of
elective or accident-related surgery. Twelve patients underwent surgery specifically to relieve pain (orchiectomy
for orchialgia, cystectomy for uncontrollable bladder pain) without success.
Evaluation of the pelvic floor via rectal examination revealed tenderness of the striated muscle in 91 men
(88.3%). This myofascial tenderness was always associated with the inability to relax the pelvic floor efficiently
either as a single or repetitive effort. Follow-up evaluations confirmed these findings. Although improvements
were noted in some patients, rarely did these patients learn to relax and control pelvic muscles.
Eighty-four patients (81.6%) underwent a urodynamic workup. The remaining 19 patients refused a urodynamic
evaluation. The principal findings in nearly all patients were: (1) hypersensitivity of the urethra or tenderness in
the external sphincter region, (2) a hypertonic sphincter, and (3) dyssynergic behavior with voiding. These
findings were scored individually to quantify the degree of muscular dysfunction and hyperalgesia.
The average maximum bladder capacity was 395 mL. Cystometry showed abnormal compliance in 5 patients.
Normal compliance was evident in 95% of all patients. Sphincter sensitivity, as evaluated by catheter insertion
and movement within the urethra during urethral evaluation, revealed that 10 patients had normal sensitivity, 40
had minimally increased sensitivity, and 34 had markedly increased sensitivity. This was scored using a linear
analog scale.
The average functional sphincter length with an empty bladder was 45.7 mm (range, 25-65 mm), and with a full
Página 2 de 8
Chronic Prostatitis: A Myofascial Pain Syndrome?
26/8/2005
http://www.medscape.com/viewarticle/416999_print
bladder, it was 44.6 mm (range, 24-65 mm). The urethral profile was normal in 12 men (11.7%); 44 (52.4%)
showed a dysfunctional/dyssynergic pattern, 10 (11.9%) had an obstructive behavior, and 18 (21.4%) had a
combined functional and obstructive pattern. The average urethral sphincter pressure was 81.9 cm H
2
O (range,
44-117 cm H
2
O) with the bladder less than 50% filled and 93.6 cm H
2
O (range, 44-157 cm H
2
O) with the bladder
more than 50% filled.
Uroflow measurements revealed, in general, a decrease of maximum and average uroflow. Peak uroflow was
14.4 mL/sec (range, 4-21 mL/sec; normal = >25 mL/sec). Average uroflow was 8.0 mL/sec (range, 2-15 mL/sec;
normal = >11-13 mL/sec).
Discussion
Conventional approaches to diagnosis and treatment of chronic abacterial prostatitis/CPPS have not adequately
relieved the suffering of many men with this condition. Clearly there is a need to investigate other factors that
may be involved in or contribute to the generation and maintenance of chronic pain in the male pelvis.
[12]
The pelvic organs are uniquely linked to and organized by the nervous system, involving sympathetic,
parasympathetic, and somatic innervation.
[13]
It has been suggested that chronic nociceptive bombardment of
central regulatory (micturition) circuits via somatic (pelvic floor) afferents could trigger a cascade of neural
events, culminating in neurogenically mediated inflammation.
[14]
Function of the pelvic floor (striated muscle)
directly affects that of the pelvic viscera. It is not surprising, therefore, that chronic pelvic floor dysfunction is
often combined with smooth muscle dysfunction of the lower urinary tract, and both may be maintained by
upregulated sacral reflexes.
A more complete understanding of the pathophysiologic relationship between chronic pain and striated muscle
behavior could lead to prevention and/or more effective therapy for CPPS. Indeed, a review of these data
showed that 92.2% of men who presented to the tertiary care center for pelvic pain had dysfunction of pelvic
floor muscles. This finding was true regardless of evidence of inflammation (prostatitis, cystitis). It should be
noted, however, that this patient population was a selected patient pool and therefore may not reflect the typical
patient with CPPS.
Many of these patients responded to modulation-based therapy, such as biofeedback, alpha-blockers, or sacral
nerve stimulation
[15]
after failing therapy with antibiotics and analgesics. This observation would suggest a role
for the nervous system in generating and maintaining symptoms of prostatitis and pain.
The central nervous system (CNS) is composed of a balanced (gated) circuitry that appears to be predisposed
toward neuronal instability (Fig. 1).
[16]
Disturbances of the CNS network may cause central dysfunction and
dysfunction of peripheral targets -- eg, the lower urinary tract. For example, the relationship between
dysfunctional muscle behavior and myalgia has been clearly demonstrated for temporomandibular disorders.
[17]
These relationships in turn can create changes in central neural circuitry, with resultant permanent change in the
way in which nociceptive sensory information is processed (Fig. 2).
[18]
In the current study, 4 patients had a
neurologic disease and pelvic pain. Even if the pelvic floor dysfunction was secondary to neuropathology, the
same cascade of changed central processing could be initiated as in a "primary" muscle dysfunction.
Página 3 de 8
Chronic Prostatitis: A Myofascial Pain Syndrome?
26/8/2005
http://www.medscape.com/viewarticle/416999_print
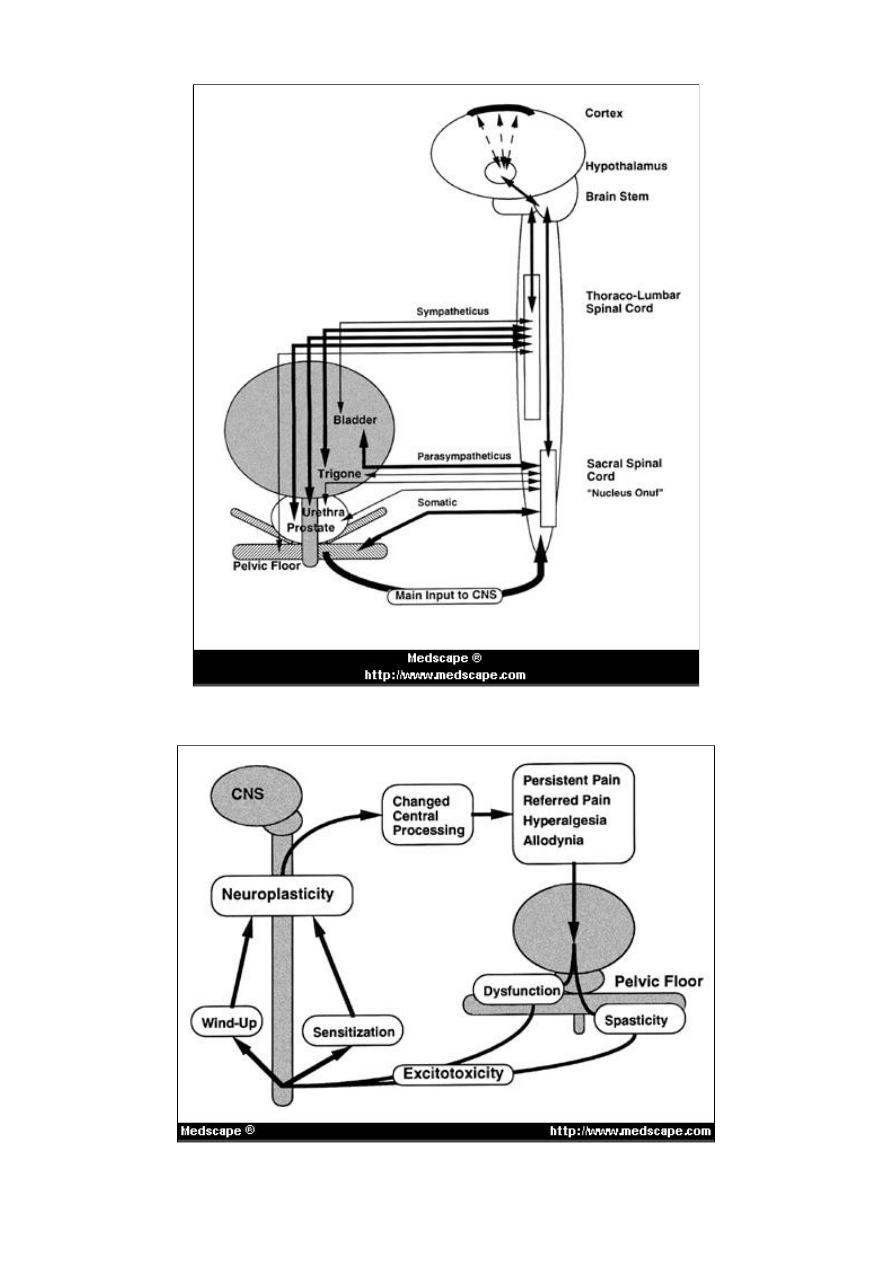
Figure 1. Circuitry of central nervous system and lower urinary tract.
Página 4 de 8
Chronic Prostatitis: A Myofascial Pain Syndrome?
26/8/2005
http://www.medscape.com/viewarticle/416999_print

Figure 2. Cycle of generating and supporting pelvic pain.
Surgical wounding, by its nature, involves an inflammatory reaction as a necessary step toward healing.
However, this process is also associated with inappropriate afferent input to the spinal cord. It is known that a
large nociceptive barrage of afferent activity delivered to the CNS as a by-product of surgical wounding can be
destabilizing to neuronal circuits.
[18]
This risk increases if the neural regulatory pathways are already in a
compromised metabolic state. The mechanisms that determine excitability within CNS circuits, hence the
mechanisms that affect the modulation or processing of information (afferent CNS input) on the cellular and
molecular level within the CNS, are only partly understood at this time. However, it is an accepted principle that
surgery can "wind up" central processing and initiate a chronic pain state.
[19]
Surgical wounding, as part of
therapy, could aggravate symptoms in the long term via these wind-up mechanisms.
Nearly 60% of the study patients had no significant medical history and no apparent anatomic or medical cause
that accounted for their chronic pelvic pain. This finding, however, does not exclude the possibility that these
patients had a long-standing pelvic floor dysfunction. This could predispose them over time to chronic pain and
urinary tract dysfunction because of compromised local immunity related to altered peptide pools (eg, substance
P presence or release).
[20,21]
The pelvic organs share their innervation with the pelvic floor. Neurons at the level of the spinal cord and the
brain stem have broad functions to control and modulate the activity of various pelvic organs. The flooding of
nociceptive afferent information (associated with dysfunctional activity within the pelvic floor) into the brain stem
nuclei could create a breakdown of normal gating within these centers. A cascade of dysfunctional and
autonomic symptoms could follow.
Neuroanatomic studies
[22]
using the retrograde transneuronal tracer pseudorabies virus have shown a significant
overlap of areas within the spinal cord and the brain stem, which are involved in the innervation of perineal
muscles of the pelvic floor (ischiocavernosus muscle, bulbospongiosus muscle),
[23]
external urethral sphincter,
[24]
urethra,
[25]
and bladder.
[26]
Most of the spinal cord labeled neurons belong to areas representing the
sympathetic autonomic system. The labeled areas in the brain could be considered to be directly connected with
those in the spinal cord. However, it should be emphasized that the premotor autonomic area in the
hypothalamus and ventrolateral medulla contains topographically segregated populations of neurons that
innervate individual sympathetic preganglionic functional units and control specific patterns of their activity.
[27]
The periventricular nucleus of the hypothalamus serves as a "master control" for the autonomic nervous system
by providing highly specialized innervation to all autonomic relay centers.
[28]
Pain, once it is established, could
be maintained via these central sympathetic pathways.
This thinking is supported by concepts that have emerged from pain research. Changes in central processing,
expansion of receptor fields within the CNS, and even cell death have been experimentally induced via noxious
inputs to the spinal cord.
[29]
A compromise of brain stem regulation of micturition (and other pelvic organs) may
be possible based on current understanding of neurophysiologic control for structures within the pelvis.
[30]
The
mechanisms that allow for the overfacilitated and permissive communication within the cord and brain stem are
not clear, but would be similar to flawed inhibitory gating observed in neuropathic states. This hypothesis is
supported by improvement rates of approximately 80% using therapeutic modalities that modulate the pelvic
floor function (eg, biofeedback, medication, sacral anterior root stimulation). Spasticity of pelvic muscles could
cause urine reflux into prostatic ducts, causing inflammatory reactions.
[12]
Thus, a neurophysiologic perspective
may contribute to our understanding of the pathophysiology of clinical symptoms and supports a modulation-
based therapeutic approach.
Conclusions
Given the association of muscle dysfunction and nociception, chronic pelvic pain in some men could be
considered a myofascial pain condition that is caused and maintained by central neurogenic mechanisms. The
observations reported, as a whole, support the perspective that the bladder and urethral striated muscle, when
functionally compromised, are capable of triggering changes within the CNS. These concepts regarding the
origin of pelvic pain should be considered when there is dysregulation of pelvic floor activity and traditional
clinical approaches fail to explain symptoms. This neurologic perspective requires a more subtle diagnostic
evaluation, but can shift emphasis of care toward modulation-based treatments that "wind down" CNS
excitability. Based on the possible neuroregulation of CPPS, biofeedback and other modalities of
neuromodulation may improve symptoms.
Tables
Table I. National Institutes of Health Categories of Prostatitis
Página 5 de 8
Chronic Prostatitis: A Myofascial Pain Syndrome?
26/8/2005
http://www.medscape.com/viewarticle/416999_print
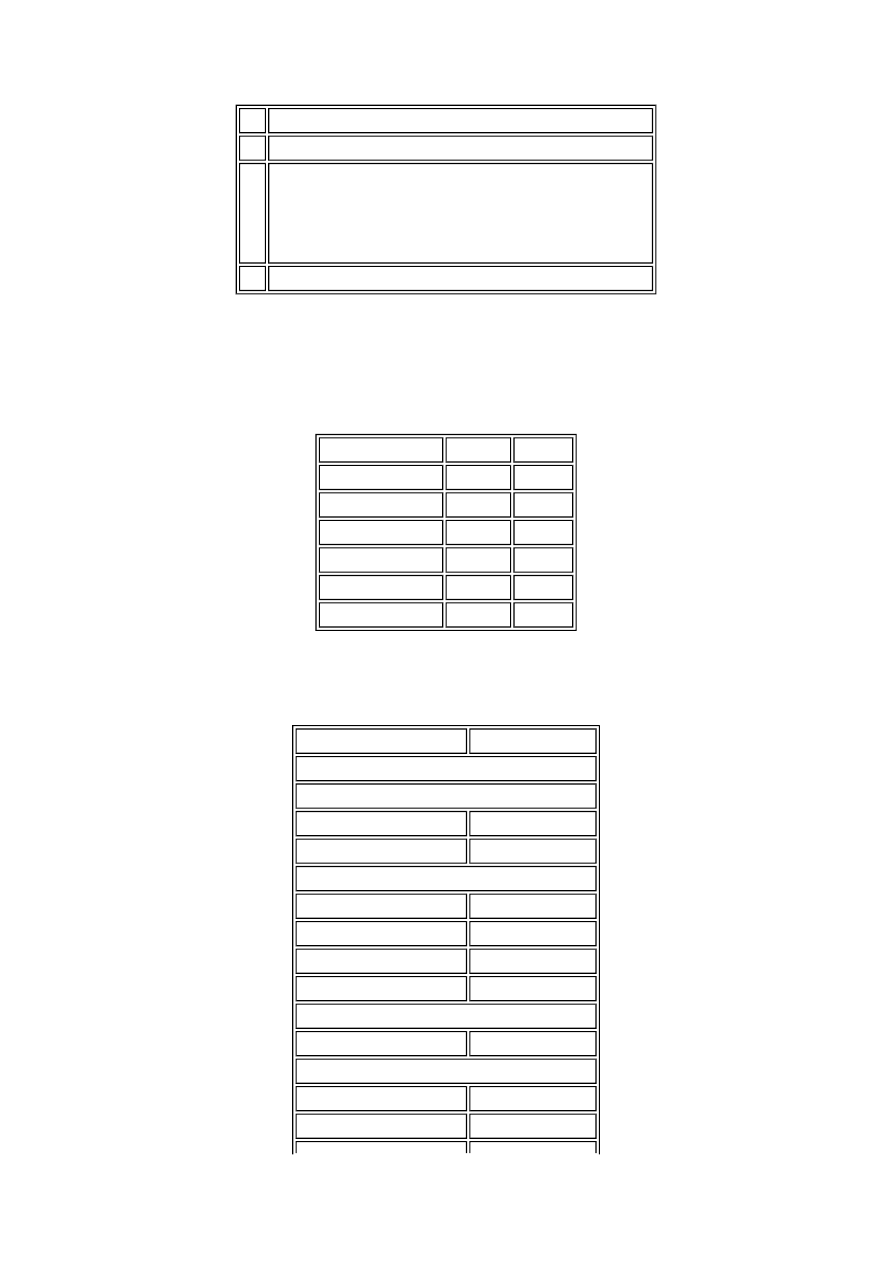
Table II. Location of Pelvic Pain in 103 Men
Table III. Surgical History in Men With Pelvic Pain
I.
Acute bacterial prostatitis
II.
Chronic bacterial prostatitis
III. Chronic abacterial prostatitis-chronic pelvic pain syndrome
a.
Inflammatory chronic pelvic pain syndrome
b.
Noninflammatory chronic pelvic pain syndrome
IV. Asymptomatic inflammatory prostatitis
Adapted from the National Institutes of Health, 1995.
[2]
Main pain region Patients
(%)
Prostate/Perineal
47
(45.6%)
Scrotal/Testicular
40
(38.8%)
Penis
6
(5.8%)
Pelvis/Bladder
6
(5.8%)
Lower abdomen
2
(1.9%)
Lower back
2
(1.9%)
Surgery
Patients (N=103)
Normal Scheduled/Elective
CNS/Spine surgery
Brain surgery
1
Lumbar surgery
7
Urologic surgery
Vasectomy
4
Varicocele
1
TURP
4
Cystectomy+pouch
3
Accident related (ski/motor vehicle accidents)
Back injury
5
Pain related
TURP
5
Radical prostatectomy
1
Página 6 de 8
Chronic Prostatitis: A Myofascial Pain Syndrome?
26/8/2005
http://www.medscape.com/viewarticle/416999_print

References
1.
Drach GW, Meares EM, Fair WR, Stamey TA. Classification of benign diseases associated with prostatic
pain: prostatitis or prostatodynia? J Urol. 1978;120:266.
2.
National Institutes of Health (NIH). Chronic Prostatitis Workshop. Bethesda, Md: December 7-8, 1995.
3.
Pfau A: Prostatitis: a continuing enigma. Urol Clin North Am. 1986;13:695-715.
4.
Krieger JN, Egan KJ. Comprehensive evaluation and treatment of 75 men referred to chronic prostatitis
clinic. Urology. 1991;38: 11-19.
5.
Shortliffe LMD, Sellers RG, Schachter J. The characterization of nonbacterial prostatitis: search for an
etiology. J Urol. 1992;148:1461-1466.
6.
Thin RN, Simmons PD. Review of results of four regimens for treatment of chronic non-bacterial
prostatitis. Br J Urol. 1983;55:519-521.
7.
Greenberg RN, Reilly PM, Luppen KL, et al. Chronic prostatitis: comments on infectious etiologies and
antimicrobial treatment. Prostate. 1985;6:445-448.
8.
DeLaRosette JJ, Humbregste MR, Meuleman EJH, et al. Diagnosis and treatment of 409 patients with
prostatitis syndrome. Urology. 1993;41:301-307.
9.
Barbalias GA, Nikiforidis G, Liatsikos EN. Alpha-blockers for the treatment of chronic prostatitis in
combination with antibiotics. J Urol. 1998;159:883-887.
10.
Kaplan SA, Ikeguchi EF, Santarosa RP, et al. Etiology of voiding dysfunction in men less than 50 years of
age. Urology. 1996;47:836-839.
11.
Kaplan SA, Santarosa RP, D'Alisera PM, et al. Pseudodyssynergia (contraction of the external sphincter
during voiding) misdiagnosed as chronic nonbacterial prostatitis and the role of biofeedback as a
therapeutic option. J Urol. 1997;157:2234-2237.
12.
Hellstrom WJG, Schmidt RA, Lue TF, et al. Neuromuscular dysfunction in nonbacterial prostatitis.
Urology. 1987;30:183-188.
13.
Jÿnemann KP, Lue TF, Schmidt RA, et al. Clinical significance and pudendal nerve anatomy. J Urol.
1988;139:74-78.
14.
Mense S. Nociception from skeletal muscle in relation to clinical muscle pain. Pain. 1993;54: 241-289.
15.
Food and Drug Administration. Gastroenterology and Urology Devices Panel. Rockville, Md: August 6,
1997.
16.
Price DD, Mao J, Mayer DJ. Central consequences of persistent pain states. In: Jensen TS, Turner JA,
Wiesenfeld-Hallin Z, eds. Proceedings of the 8th World Congress on Pain: Progress in Pain Research
and Management. Seattle, Wash: IASP Press; 1997:155-184.
17.
Svenson P. Pain mechanism in myogenous temporomandibular disorders. Pain Forum. 1997;6:158-165.
18.
Dubner R, Ruda MA. Activity-dependent neuronal plasticity following tissue injury and inflammation.
Trends Neurosci. 1992;15: 96-103.
19.
Coderre TJ, Katz J, Vaccarino AL, et al. Contribution of central neuroplasticity to pathological pain: review
of clinical and experimental evidence. Pain. 1993;52:259-285.
20.
Birder LA, de Groat WC. Increased c-fos expression in spinal neurons after irritation of the lower urinary
tract in the rat. J Neurosci. 1992;12:4878-4889.
21.
Doyle CA, Palmer JA, Munglani R, et al. Molecular consequences of noxious stimulation. In: Borsook D,
ed. Molecular Neurobiology of Pain: Progress in Pain Research and Management. Seattle, Wash: IASP
Press; 1997:145-169.
22.
Kuypers HG, Ugolini G. Viruses as transneuronal tracers. Trends Neurosci. 1990; 13:71-75.
23.
Marson L, McKenna KE. CNS cell groups involved in the control of the ischiocavernosus and
bulbospongiosus muscles: a transneuronal tracing study using pseudorabies virus. J Comp Neurol.
1996;374:161-179.
24.
Nadelhaft I, Vera PL. Neurons in the rat brain and the spinal cord labeled after pseudorabies virus
injected into the external urethral sphincter. J Comp Neurol. 1996;375:502-517.
25.
Vizzard MA, Erickson VL, Card JP, et al. Transneuronal labeling of neurons in the adult rat brainstem and
spinal cord after injection of pseudorabies virus into the urethra. J Comp Neurol. 1995;355:629-640.
26.
Nadelhaft I, Vera PL, Card JP, et al: Central nervous system neurons labelled following the injection of
pseudorabies virus into the rat urinary bladder. Neurosci Lett. 1992;143:271-274.
27.
Benarroch EE. The central autonomic network: functional organization, dysfunction and perspective.
Mayo Clin Proc. 1993;68:988-995.
28.
Swanson LW. The hypothalamus. In: Björklund A, Höfkelt T, Swanson LW, eds. Handbook of Chemical
Neuroanatomy. Integrated Systems of the CNS. Amsterdam: Elsevier; 1987:1-125.
29.
McMahon SB, Wall PD. Receptive fields of lamina I projection cells move to incorporate a nearby region
Abdominal surgery
2
Testicular surgery
4
TURP = transurethral resection of prostate
Página 7 de 8
Chronic Prostatitis: A Myofascial Pain Syndrome?
26/8/2005
http://www.medscape.com/viewarticle/416999_print
of injury. Pain. 1984;19:235-247.
30.
de Groat WC, Steers WD. Autonomic regulation of the urinary bladder and sex organs. In: Loewy AD,
Spyer KM, eds. Central Regulation of Autonomic Functions. New York, NY: Oxford University Press;
1990;310-333.
Dr. Zermann is in the Department of Urology, University Hospital at Friedrich-Schiller University in Jena,
Germany. Dr. Ishigooka is in the Department of Urology, Yamagata University, Yamagata, Japan. Dr.
Doggweiler is in the Department of Urology, University of Tennessee, Memphis. Dr. Schmidt is Professor of
Urology at the University of Colorado, Denver.
Página 8 de 8
Chronic Prostatitis: A Myofascial Pain Syndrome?
26/8/2005
http://www.medscape.com/viewarticle/416999_print
Wyszukiwarka
Podobne podstrony:
Chronic Pain Syndromes After Ischemic Stroke PRoFESS Trial
Chronic Pain Syndromes After Ischemic Stroke PRoFESS Trial
Serum cytokine levels in patients with chronic low back pain due to herniated disc
Treating Non Specific Chronic Low Back Pain Through the Pilates Method
Evidence for Therapeutic Interventions for Hemiplegic Shoulder Pain During the Chronic Stage of Stro
Chronic Pain for Dummies
Lumbar lordosis and pelvic inclinations in adults with chronic lumbar pain
Ebsco Farezadi Chronic pain and psychological well being
combination teraphy chronic pain
Chronic Fatigue Syndrome
Chronic Fatigue Syndrome R Moss Morris, K Petrie (Routledge, 2001) WW
Chronic Hepatitis
Restless legs syndrom
úagodny przerost prostaty
Prostata
więcej podobnych podstron