
Use of Clinical and Impairment-
Based Tests to Predict Falls by
Community-Dwelling Older Adults
Background and Purpose. Few tests have been found to be strongly
predictive of falls in community-dwelling older adults. The purpose of
this study was to determine whether data from 5 balance tests—
combined with data regarding fall history, number of medications,
dizziness, visual problems, use of an assistive device, physical activity
level, sex, and age— could predict falls in community-dwelling older
adults who were independent. Subjects. Ninety-nine community-
dwelling older adults aged 65 to 90 years (X
⫽74.02, SD⫽5.64) were
tested. Methods. Subjects were tracked for falls over a 1-year period
following testing. Impairment-based tests, which are tests that attempt
to specifically identify which sensory systems are impaired or how
motor control is impaired (eg, speed, accuracy of movement), were the
Modified Clinical Tests of Sensory Interaction for Balance (Modified
CTSIB) and the 100% Limits of Stability Test, both of which were done
on the Balance Master 6.1. Performance-based tests, which are func-
tional tests that identify functional limitations without necessarily
identifying their causes, were the Berg Balance Scale, the Timed “Up
& Go” Test, and the Dynamic Gait Index. Demographic and health
data included age, sex, number of medications, physical activity level,
presence of dizziness, vision problems, and history of falls over the
previous year. Logistic regression was used to determine which com-
binations of data from balance tests, demographics, and health factors
were predictive of falls. Results. Two models—(1) the “standing on a
firm surface with eyes closed” (FEC) condition of the Modified CTSIB
and (2) the FEC combined with age and sex—were predictive of falls,
but predicted only 1 and 2 subjects who were at risk for falling,
respectively, out of 20 people who were at risk for falling. Discussion
and Conclusion. Five balance tests combined with health and demo-
graphic factors did not predict falls in a sample of community-dwelling
older adults who were active and independent. [Boulgarides LK,
McGinty SM, Willett JA, Barnes CW. Use of clinical and impairment-
based tests to predict falls by community-dwelling older adults. Phys
Ther. 2003;83:328 –339.]
Key Words: Balance tests, Fall prediction, Older adults.
Lois K Boulgarides, Susan M McGinty, Jayne A Willett, Carole W Barnes
328
Physical Therapy . Volume 83 . Number 4 . April 2003
Research
Report
䢇
ўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўў
ўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўў
ўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўў

A
n estimated 25% to 35% of adults aged 65
years and older fall each year.
1– 4
The high
fall incidence in older adults is costly in terms
of both health care dollars and quality of life.
Most older adults hospitalized for falls are discharged to
long-term care facilities.
5
Fear of falling is an important
factor that affects the willingness of many older adults to
participate in physical activity and exercise.
6,7
Cessation
of physical activities, whether due to fear of falling or
due to declining mobility and balance, accelerates the
decline in muscle force production and function, fur-
ther increasing fall risk and further decreasing quality of
life.
6,7
Low fall-related self-efficacy has been associated
with decreased function, increased fall risk, and risk of
admission
to
assisted
living
or
long-term
care
institutions.
6,7
A number of interventions to improve balance and
decrease fall risk have been found to be effective.
8 –10
Interventions may be performed in the hospital, clinic,
retirement facility, or community. Some researchers
11–14
have found multifaceted intervention programs that
include exercise to increase muscle force, flexibility, and
balance to be effective approaches.
A number of fall-risk screening tests have been used to
identify people at risk for falling (“fallers”) among
residents of nursing homes; however, these tests are less
predictive of falls in older adults who have fewer health
problems, live independently, and are more active.
15,16
The
Berg
Balance
Scale
(BBS),
17,18
the
Tinetti
Performance-Oriented Mobility Assessment (POMA),
19
the Tinetti Balance Subscales,
19
and the Timed “Up &
Go” Test (TUGT)
20
were developed for, and validated
primarily on, residents of nursing homes.
The usefulness of a test in predicting falls may vary
depending on the health status and level of function of
the older adults being tested. In a study of community-
dwelling older adults who were in good health, O’Brien
LK Boulgarides, PT, MS, is Lecturer, Kinesiology and Health Science Department, California State University, Sacramento, 6000 J St, Sacramento,
CA 95819-6073 (USA) (boulgarides@csus.edu), and Faculty Director, CSUS LIFE Center for Senior Fitness and Wellness. Address all
correspondence to Ms Boulgarides.
SM McGinty, PT, EdD, is Chair, Department of Physical Therapy, California State University, Sacramento.
JA Willett, PhD, ATC, is Associate Professor, Kinesiology and Health Science Department, California State University, Sacramento.
CW Barnes, PhD, is Professor, Department of Sociology, California State University, Sacramento, and Director, CSUS Institute for Social Research.
All authors provided concept/research design. Ms Boulgarides, Dr McGinty, and Dr Willett provided writing, data collection, project management,
fund procurement, and subjects. Ms Boulgarides, Dr McGinty, and Dr Barnes provided data analysis. Dr McGinty and Dr Willett provided
facilities/equipment and consultation (including review of manuscript before submission). Ms Boulgarides and Dr McGinty provided institutional
liaisons. Dr McGinty provided clerical/secretarial support. The authors thank Edward Barakatt for assistance with statistical analysis and Heather
Carling-Smith and Patricia A Harris for their contributions to data collection. The authors also thank the baccalaureate and post-baccalaureate
students from the Department of Kinesiology and Health Science and the Department of Physical Therapy, California State University,
Sacramento, for their assistance with subject recruitment and data collection.
This study was approved by the California State University, Sacramento, Committee for Protection of Human Subjects.
This study was supported by a grant from the California State University, Sacramento, Research and Creative Activity Committee.
This article was submitted May 8, 2002, and was accepted November 22, 2002.
Physical Therapy . Volume 83 . Number 4 . April 2003
Boulgarides et al . 329
ўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўў
et al
16
found the BBS was less sensitive in predicting falls
than did Berg et al
17
who studied residents of a nursing
home.
Other
researchers
21
studying
community-
dwelling older adults found BBS scores to be predictive
of falls. The fallers, however, were only those who had a
history of recurrent falls, which, in our opinion, indi-
cates that the group was at greater fall risk. Thus, the
BBS may better identify older adults who have greater
impairments and who are at risk for falls than older
adults who are in good health and more active but who
also may be at risk for falls.
Many factors affect a person’s likelihood of falling. Age,
vision, muscle force, flexibility, sensation, balance, num-
ber and type of medications, cognitive impairment, and
concomitant medical problems have all been associated
with fall risk.
2– 4,19
The purpose of our study was to
determine whether data from a combination of 5 bal-
ance assessment tests— combined with data regarding
fall history, number of medications, dizziness, visual
problems, use of an assistive device, physical activity
level, sex, and age— could predict fall risk in a group of
community-dwelling older adults who were indepen-
dent. The balance tests that we used were the BBS,
17,18
the Dynamic Gait Index (DGI),
11,21
the TUGT,
20
the
100% Limits of Stability Test (100% LOS),
22
and the
Modified Clinical Test of Sensory Interaction for Bal-
ance (Modified CTSIB).
23,24
Method
Subjects
One hundred six community-dwelling
older adults (age range
⫽65–90 years)
who were independent were recruited
from retirement communities, senior
centers, the 50-Plus Wellness Program,
and the general community in Sacra-
mento, Calif. Ninety-nine subjects (60
women and 39 men) completed the
study. One subject died, 1 subject
declined to continue the study, and 5
subjects could not be reached for con-
tinued follow-up.
In order to participate in the study,
subjects must have been able to stand
for at least 5 minutes without an assis-
tive device and to walk a minimum of
12 m (40 ft) at a time with or without an
assistive device. Inclusion criteria were
communicated
through
recruiting
materials,
confirmed
by
telephone
when appointments were scheduled,
and reconfirmed in the medical history
questionnaire at the time of testing.
People with cognitive deficits or medical or neurological
problems were excluded only if the condition prevented
them from meeting the inclusion criteria. No screening
for dementia was done, but all subjects were able to
follow directions, give appropriate responses to survey
questions, and participate in the interview process with-
out assistance. Subjects with conditions such as heart or
pulmonary problems, in which mild activity could cause
medical risk during the testing, were excluded from the
study. Before participating in the study, all subjects
signed an informed consent form that summarized the
purpose of the study, explained risks and discomforts,
indicated that all information gathered would remain
confidential, and assured subjects that they could with-
draw at any time.
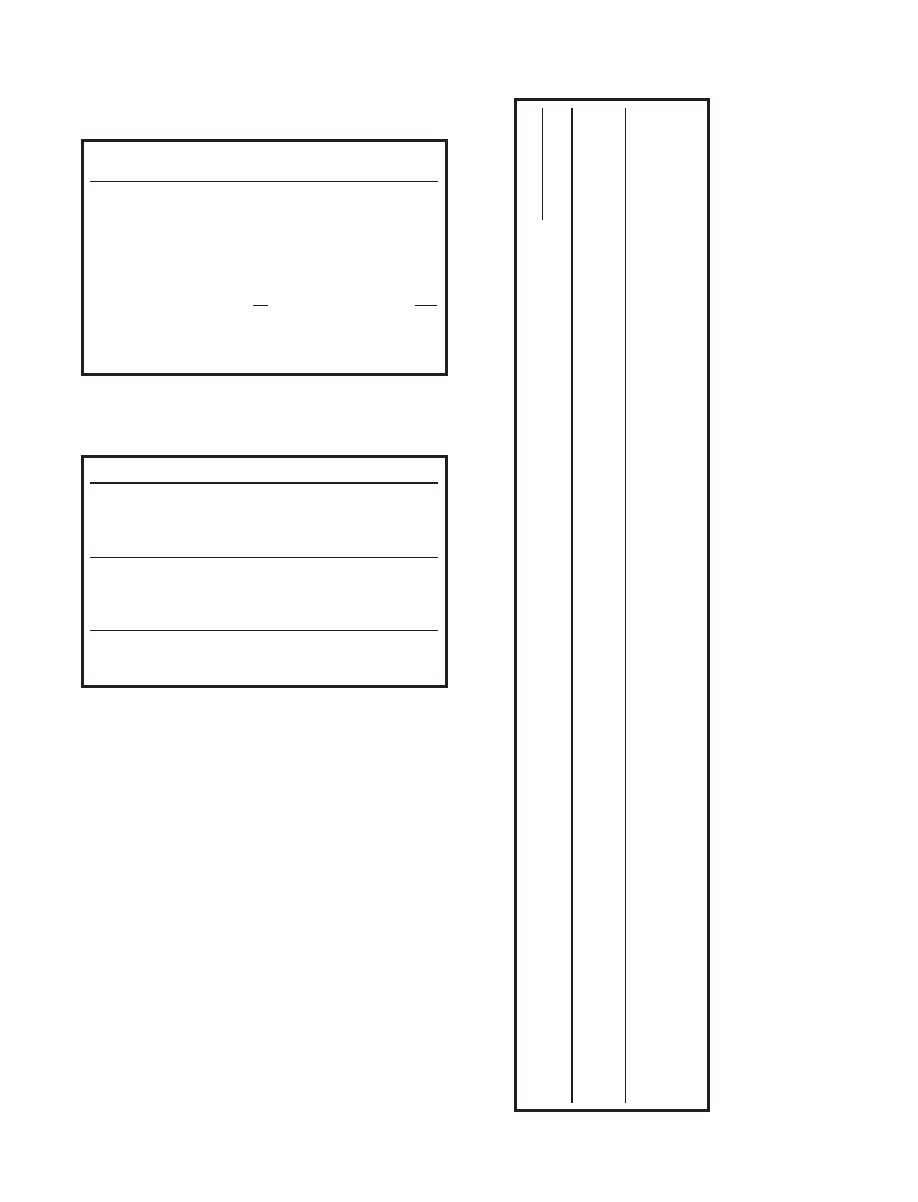
Table 1 summarizes the subjects’ demographic informa-
tion. Subjects had a mean age of 74.02 years (SD
⫽5.64,
range
⫽65–90). The number of medications the subjects
took ranged from 0 to 10 (X
⫽2.74, SD⫽2.26). Fifty-six
subjects (56.6%) reported problems with dizziness, 5
subjects (5.1%) reported vision problems when using
corrective lenses, 10 subjects (10.1%) reported using an
assistive device, and 87 subjects (87.9%) reported being
involved in regular physical exercise. Seventeen subjects
(17.2%) recalled falling 3 or more times, 33 subjects
(33.3%) recalled falling 1 or 2 times, and 49 subjects
(49.5%) recalled no falls in the year prior to the study.
Table 1.
Subject Characteristics (N
⫽99)
n
%
X
SD
Median
Range
Age (y)
74.02
5.64
74
65–90
No. of medications
2.74
2.26
2
0–10
Sex
Female
60
61
Male
39
39
Reported dizziness
No
43
43.4
Yes
56
56.6
Reported vision problems (corrected)
No
94
94.9
Yes
5
5.1
Use of assistive device
No
89
89.9
Yes
10
10.1
History of falls
0
49
49.5
1–2
33
33.3
3 or more
17
17.2
Regular physical activity
No regular exercise
12
12.1
Regular exercise
87
87.9
330 . Boulgarides et al
Physical Therapy . Volume 83 . Number 4 . April 2003

Procedure
Subjects were tested one time for the study. They were
then followed for 12 months to track falls. Testing was
performed in the Kinesiology/Physical Therapy Labora-
tory at California State University, Sacramento, by phys-
ical therapy and kinesiology faculty and by graduate and
undergraduate
students
in
physical
therapy
and
kinesiology.
Before administering the tests, students and faculty
completed 6 hours of training and practice in the
correct use of the NeuroCom Balance Master 6.1,*
administration and recording of all tests, and interview
techniques. All were tested for the reliability of their data
collection skills. We were concerned about the reliability
of the data collected by all testers because the BBS and
DGI require raters to make a judgment about movement
quality. Interrater reliability for these tests was estab-
lished by having all testers view videotapes of 3 subjects
and judge movement quality using the BBS and the DGI.
An 80% or better agreement between testers was
achieved before proceeding with subject testing. Reli-
ability was not assessed with the use of any statistics, such
as those that correct for chance agreement or are based
on probabilistic models.
Subjects were interviewed about their medical history,
history of falls, and physical activity. Medical history
included questions about vision (with and without cor-
rective lenses, in poor light), dizziness experienced in
the year before the study, number of medications,
cardiac and pulmonary problems, use of an assistive
device, and cancer. Fall history was determined by
self-report of the number of falls that the subject recalled
from the previous year, including the time of day,
location, conditions, and injuries. A fall was defined as
any disturbance of balance during routine activities that
resulted in a person’s trunk, knee, or hand unintention-
ally coming to rest on the ground, wall, table, chair, or
some other surface. Physical activity was determined by
self-report of the activity type and how often and how
regularly the activity was performed in the year before
the study. Subjects were classified as “active” if they
exercised regularly at least one time per week.
After the interview, 2 subjects were tested at a time.
Subjects’ heights were measured to the nearest half inch.
One subject was given performance-based tests (the BBS,
TUGT, and DGI) followed by impairment-based tests
(100% LOS and Modified CTSIB) on the NeuroCom
Balance Master 6.1. The other subject was given
impairment-based tests, followed by performance-based
tests. Performance-based tests are functional tests that we
believe identify functional limitations without necessarily
identifying their causes. Impairment-based tests, which
were done using the Balance Master 6.1, are tests that
attempt to specifically identify which sensory systems are
impaired or how motor control is impaired (eg, speed,
direction of movement, accuracy of movement). Two
test administrators were present for each subject’s test-
ing. One tester administered the test, and the other
tester assisted primarily by standing by the subject to
prevent falls during testing. All subjects wore gait safety
belts throughout the balance testing.
Each subject was given a booklet at the end of the
balance test session. The booklet contained a calendar
for recording falls, the definition of a fall, and instruc-
tions for use of the calendar. Subjects were asked to
record daily whether a fall occurred. Details of any falls,
including time, location, and circumstances, were
recorded on a form provided on the back of each
month’s page.
Telephone Survey
Follow-up contact was made by telephone or e-mail every
2 to 4 weeks during the 12 months following the balance
assessment to track the subjects’ fall history. Subjects
referred to their fall calendars to report losses of bal-
ance. If a fall had occurred, the subjects were asked
whether they were injured and whether they sought
medical attention. Subjects were asked if they were using
the fall calendar on a daily basis and were encouraged to
continue daily recording of fall status.
Balance Tests
The balance assessment consisted of 3 performance-
based balance tests (BBS, TUGT, and DGI) and 2
impairment-based tests (Modified CTSIB and 100%
LOS). Both impairment-based tests were conducted
using the NeuroCom Balance Master 6.1.
Berg Balance Scale. Reliability of data obtained with
the BBS has been established in a previous study of 35
residents of nursing homes and 35 patients with stroke
(intraclass correlation coefficient [ICC]
⫽.97–.98).
18
Cri-
terion validity was established in a study of 31 subjects
with a mean age of 83 years. The BBS scores were
correlated to the Tinetti Balance Subscale and the
TUGT (r
⫽.76–.91).
17
The BBS is designed to challenge
subjects to keep their balance with an increasingly
narrow base of support; the initial level is sitting, and the
final level is one-leg standing. Weight shifting, turning,
and reaching also are measured. Points for each item are
totaled. The highest possible score is 56 points. In a
clinical setting, the cutoff score to separate fallers from
people who are not at risk for falling (“nonfallers”) is
usually 45 points.
15
We used the BBS score for statistical
analysis, rather than as a cutoff value for distinguishing
fallers from nonfallers.
* NeuroCom International, 9570 SE Lawnfield Rd, Clackamas, OR 97015.
Physical Therapy . Volume 83 . Number 4 . April 2003
Boulgarides et al . 331
ўўўўўўўўўўўўўўўўўўўўўўўўўўўў

Dynamic Gait Index. The DGI uses 8 test items to
measure a person’s ability to accommodate to changes in
environment, speed, and head position during gait.
Tasks are rated on a 3-point scale from 0 (unable) to 3
(normal execution). The highest possible score is 24.
The rating is based on the person maintaining normal
gait pace (a person’s natural walking pace) and staying
within a 38.1-cm-wide (15-in) pathway without stumbling
or staggering during walking. This test is designed to
demand many of the adjustments to gait that should
occur when walking in the community or home, includ-
ing walking with horizontal and vertical head turns,
walking while speeding up and slowing down, walking
over and around objects, and ascending and descending
stairs. No studies measuring intrarater and interrater
reliability of data obtained with the DGI as a single test
have been found. We chose the DGI for our study
because we believed it to be the most challenging gait
mobility test available for older adults. For statistical
analysis, we used the DGI score rather than a cutoff value
to distinguish fallers from nonfallers.
Timed “Up & Go” Test. The TUGT is measured with a
stopwatch. The subject is instructed to move from a
seated position in a chair to a standing position, walk 3 m
(10 ft) at a normal and safe pace, turn around, walk back
to the chair, and sit down. The subject is given a practice
trial followed by 2 timed trials. The 2 timed trials are
averaged for each subject’s score. Excellent intertester
and intratester reliability of data obtained with the
TUGT were established (ICC
⫽.99 for both) in a study of
60 older adults who were frail and 10 older adults who
were in good health.
20
Trueblood et al
24
felt that a cutoff
time of 10 to 12 seconds separated fallers from nonfall-
ers in a group of community-dwelling older adults. A
20-second cutoff time had previously been used when
testing elderly people who were frail for independence
in functional mobility.
20
In another study in which
investigators chose a 14-second cutoff time, the TUGT
was found to have 87% sensitivity of correctly predicting
fallers and 87% specificity for correctly predicting non-
fallers.
25
In our study, we did not use a cutoff time, but
we used total time in the logistic regression equation.
Modified Clinical Test for Sensory Interaction on Balance.
The Modified CTSIB was conducted on the NeuroCom
Balance Master 6.1.
26
The Modified CTSIB examines
postural sway during the 4 conditions assessed for the
CTSIB: “standing on a firm surface with eyes open”
(FEO), “standing on a firm surface with eyes closed”
(FEC), “standing on a foam surface with eyes open”
(FOEO), and “standing on a foam surface with eyes
closed” (FOEC). Composite sway is the mean sway speed
averaged over the 4 conditions. Each condition is tested
3 times. Although visual examination of amplitude and
speed of sway is used as a measure in the CTSIB, testing
with the Modified CTSIB on the Balance Master uses
dual force platforms to measure amplitude, direction,
and speed of movement of a person’ center of pressure.
Subjects stood straight and still on a force platform
during three 20-second trials in each of the 4 conditions.
For each condition, each subject’s feet were placed in
the standard position recommended by the manufac-
turer of the Balance Master.
26
Foot position was moni-
tored throughout the test. If foot placement changed,
the feet were again placed in the correct position. The
Modified CTSIB gives 2 sets of data collected by the
computer from the 4 conditions. Data include mean
center of pressure sway speed (which is measured in
degrees per second) and average center of pressure
position (which measures deviation of the center of
pressure in degrees over 20 seconds). We used center-
of-pressure speed for the 4 conditions and composite
sway for statistical analysis. In a study of 12 subjects from
24 to 68 years of age (X
⫽42.2), test-retest reliability for
the Modified CTSIB using only FEO and FEC conditions
was found to be high (ICC [3,4]
⫽.91 for FEO, ICC
[3,4]
⫽.97 for FEC).
27
It should be noted, however, that
the sample studied was much younger than the sample
used in the present study.
100% Limits of Stability Test. A theoretical 100% LOS is
established for each person by the Balance Master 6.1
software based on the person’s height. This theoretical
100% LOS is the maximum angle a person of a given
height should be able to sway the body over the feet
without losing balance and having to take a step. It is
measured by a person’s ability to shift his or her center
of pressure from a center point to 8 targets viewed on a
computer screen that are placed around the center of
pressure: front, sides, back, and 4 diagonal points. The
targets represent the maximum distance the person
should be able to sway the center of pressure in any
direction without losing balance and having to change
foot position.
The 100% LOS provides 5 sets of information as a
person shifts his or her center of pressure from the
center toward individual visual targets on the computer
screen. Reaction time, measured in milliseconds, is the
time from the computer’s command to move and the
initiation of movement. Movement speed, measured in
degrees per second, is the average speed of movement of
the center of pressure. End-point excursion is the greatest
distance reached by the center of pressure in the first
sustained attempt to reach the target and is expressed as
a percentage of a straight line from center to target.
Readjustments in position after the initial movement are
not calculated in end-point excursion. Maximum excur-
sion is the greatest distance reached by the center of
pressure toward the target during the target’s entire trial
332 . Boulgarides et al
Physical Therapy . Volume 83 . Number 4 . April 2003

period. Maximum excursion is expressed as a percent-
age of a straight line from center to target. Directional
control is a ratio of the distance of a straight line from
center to target to the total distance that the subject
moved. Deviation from a straight path will increase the
total distance moved. Directional control is given as a
percentage, with a higher percentage showing better
directional control. A directional control score of 100%
would mean that the subject did not deviate from a
straight path.
26
Data from all four 100% LOS measures were used in the
statistical analysis. In a study of 38 community-dwelling
older adults without histories of falling, test-retest reli-
ability estimates of the 100% LOS, using the 8 targets
over 3 test days, were found to be moderately high to
high for movement speed, maximum excursion, and
end-point excursion.
22
No differences in measurements
across the 3 test days were found for movement speed
(F
⫽2.07; df⫽2,23; P⬎.10), maximum excursion
(F
⫽1.02; df⫽2,29; P⬎.25), and end-point excursion
(F
⫽4.50; df⫽2,17; P⬎.025). A study of 12 subjects
between 24 and 68 years of age (X
⫽42) demonstrated
what we would consider moderate test-retest reliability of
movement time to targets (the measure of speed on
older versions of Balance Master programs) and path
length to targets (the measure of end-point excursion on
older versions of Balance Master programs) (ICC
⫽.83
and .78, respectively).
27
Data Analysis
Logistic regression was performed using the SPSS 10.0
for Windows program.
†
Forward stepwise logistic regres-
sion was used, with multiple (more than 1) falls or no
multiple falls (0 or 1) as the dichotomous dependent
variable in order to analyze which tests, combinations of
tests, or other variables predicted falls. Because of the
sample size and number of variables, the entry probabil-
ity for analysis was set at the .10 instead of .05 level of
significance in an effort to avoid a type II error. Number
of medications, fall history, dizziness, visual problems,
previous falls, physical activity level, and balance test
scores were included as independent variables in the
logistic regression. Kendall tau correlations were calcu-
lated to determine which dependent and independent
variables were related (Tab. 2). Variables that were
correlated were not placed in the same logistic regres-
sion model to prevent interaction that could confound
the analysis. Variables that seemed logical based on
previous research, correlation values, and clinical rea-
soning were used for different models. If variables were
correlated—and, therefore, not placed into regression
models together— different combinations of variables
were used until all possible combinations of noncorre-
lated variables were entered into the regression models.
After models were suggested by the forward stepwise
regression, logistic regression calculations were run, and
each variable was entered one at a time to determine the
contribution of each variable to the predictive value of
the model. Logistic regression also was used to deter-
mine whether various balance tests or combinations of
tests could predict injurious falls.
Results
Reported Falls
Because of a lack of personnel, 30 subjects were not
called for a 3-month period. When contact was resumed,
subjects were asked to refer to their calendars to report
fall status.
In the 12 months following testing, 22 of the 42 fallers
(52%) fell only once, 11 (26%) fell twice, and 9 fell 3 or
more times (Tab. 3). Fifty-seven subjects (57.6%)
reported no falls as compared with 42 subjects (42.4%)
who reported 1 or more falls (mean for the entire
group
⫽0.91 falls per person, SD⫽1.67) (Tabs. 3 and 4).
Of those who fell in the year following testing, the mean
number of falls per person was 2.14 (SD
⫽2, median⫽1)
(Tab. 3). Multiple falls (2 or more falls) were reported by
20 (20.2%) of the entire subject group (Tab. 4). Only 4
subjects (4.0%) sustained falls with injuries serious
enough to seek medical care (Tab. 4). Because of the
small number of subjects who fell more than twice
(9.1%), we used a multiple falls category (2 or more
falls). For logistic regression analysis, multiple falls was
defined as 2 or more falls, and nonmultiple falls was
defined as 0 or 1 fall.
Table 2 shows the Kendall tau correlations between the
test variables. Highly correlated test scores were not
placed together into logistic models. In fall prediction
calculation, both forward stepwise and the enter method
logistic regression gave similar models. Logistic regres-
sion revealed that the FEC portion of the Modified
CTSIB, the speed of center of pressure sway while a
subject stands on a firm surface with eyes closed, was
predictive of multiple falls (Tab. 5). A model containing
FEC and the covariates of age and sex also resulted in a
predictive model, although adding age and sex to FEC
did not improve the predictive ability of the model
(Tab. 5). Closer scrutiny of FEC scores revealed one
score of 1.3°/s that fell more than 2 standard deviations
(SD
⫽0.186) from the mean score of 0.381°/s. After this
extreme score was removed from the data, we found no
model of significance. The FEC score, however, was
consistent with the other Modified CTSIB scores for this
subject; therefore, the score was included in the data for
analysis. Logistic regression analysis revealed no other
†
SPSS Inc, 233 S Wacker Dr, Chicago, IL 60606-6307.
Physical Therapy . Volume 83 . Number 4 . April 2003
Boulgarides et al . 333
ўўўўўўўўўўўўўўўўўўўўўўўўўўўў
Table
2.
Kendall
Tau
Correlation
Matrix
of
Balance
Variables
With
Multiple
Falls
a
M
Falls
MVL
EPE
MXE
DCL
RT
FEO
FEC
FOEO
FOEC
Comp
Dizzy
Glauc
Meds
Fall
H
P
Act
BBS
FRT
TUGT
DGI
M
Falls
1.000
⫺
.017
⫺
.132
⫺
.083
⫺
.064
.000
.038
.145
.060
⫺
.089
.112
⫺
.067
.072
.054
⫺
.009
⫺
.121
⫺
.013
.013
.143
⫺
.024
MVL
1.000
.326
b
.219
b
⫺
.069
⫺
.296
b
.151
.066
⫺
.025
⫺
.094
.032
.055
.094
⫺
.121
.128
.124
.129
.130
⫺
.177
c
.195
b
EPE
1.000
.732
b
.463
b
⫺
.217
b
⫺
.058
⫺
.101
⫺
.255
b
⫺
.214
c
⫺
.112
.118
.074
⫺
.102
.176
c
.103
.308
b
.180
c
⫺
.293
b
.311
b
MXE
1.000
.523
b
⫺
.234
b
⫺
.049
⫺
.093
⫺
.207
b
⫺
.196
c
⫺
.076
.094
.082
⫺
.073
.127
.044
.313
b
.182
c
⫺
.263
b
.278
b
DCL
1.000
⫺
.003
⫺
.224
b
⫺
.178
c
⫺
.312
b
⫺
.219
b
⫺
.122
.015
.088
⫺
.024
.048
.065
.347
b
.138
⫺
.279
b
.225
b
RT
1.000
⫺
.103
⫺
.083
.036
.122
.045
⫺
.006
⫺
.084
.012
⫺
.123
⫺
.002
⫺
.082
.019
.099
⫺
.091
FEO
1.000
.612
b
.323
b
.132
.451
b
⫺
.110
⫺
.158
.075
⫺
.044
⫺
.145
⫺
.256
b
⫺
.101
.138
⫺
.193
c
FEC
1.000
.218
b
.231
b
.392
b
⫺
.191
c
⫺
.135
.102
⫺
.078
⫺
.122
⫺
.234
b
⫺
.125
.138
⫺
.211
b
FOEO
1.000
.311
b
.381
b
⫺
.053
⫺
.146
.093
⫺
.156
⫺
.194
b
⫺
.376
b
⫺
.277
b
.328
b
⫺
.317
b
FOEC
1.000
.217
c
⫺
.050
⫺
.206
c
.132
⫺
.159
⫺
.107
⫺
.202
c
⫺
.051
.252
b
⫺
.373
b
Comp
1.000
⫺
.226
c
⫺
.126
.162
c
⫺
.127
⫺
.201
c
⫺
.093
⫺
.070
.173
c
⫺
.227
b
Dizzy
1.000
.164
⫺
.169
.216
c
.237
c
.065
⫺
.075
⫺
.196
c
.149
Glauc
1.000
⫺
.109
.042
.387
b
.181
c
.106
⫺
.170
.175
c
Meds
1.000
⫺
.260
b
⫺
.087
⫺
.171
c
⫺
.138
.213
b
⫺
.163
c
Fall
H
1.000
.098
.210
c
.086
⫺
.207
c
.264
b
P
Act
1.000
.167
.068
⫺
.201
c
.182
c
BBS
1.000
.399
b
⫺
.431
b
.457
b
FRT
1.000
⫺
.313
b
.222
b
TUGT
1.000
⫺
.435
b
DGI
1.000
a
M
Falls
⫽
multiple
falls
(2
or
more
falls),
MVL
⫽
movement
speed,
EPE
⫽
end-point
excursion,
MXE
⫽
maximum
excursion,
DCL
⫽
directional
control,
RT
⫽
reaction
time,
FEO
⫽
“standing
on
a
firm
surface
with
eyes
open,
”
FEC
⫽
“standing
on
a
firm
surface
with
eyes
closed,
”
FOEO
⫽
“standing
on
a
foam
surface
with
eyes
open,
”
FOEC
⫽
“standing
on
a
foam
surface
with
eyes
closed,
”
Comp
⫽
composite
sway,
Dizzy
⫽
reports
of
dizziness,
Glauc
⫽
glaucoma,
Meds
⫽
number
of
medications,
Fall
H
⫽
history
of
falls,
P
Act
⫽
physical
activity,
BBS
⫽
Berg
Balance
Scale,
FRT
⫽
Functional
Reach
Test,
TUGT
⫽
Timed
“U
p&G
o
”
Test,
DGI
⫽
Dynamic
Gait
Index.
b
Significant
at
P
⫽
.01.
c
Significant
at
P
⫽
.05.
334 . Boulgarides et al
Physical Therapy . Volume 83 . Number 4 . April 2003
variables or combinations of variables that predicted
multiple fall or nonmultiple fall status.
Use of assistive device. Logistic regression analysis did
not indicate that the use of an assistive device was
predictive of falls. The small number of people using
assistive devices in our sample (10 subjects) may have
affected the results.
Injurious falls. Only 4 subjects reported injurious falls in
the study (Tab. 4). Dizziness problems were found to be
predictive of injurious falls in the logistic regression. A
96% correct prediction rate was found, although none
of the 4 fallers were correctly identified.
Discussion
The rate of multiple falls reported by our subjects was
consistent with previous reports.
21,24,28
Trueblood et al
24
reported a 16.5% fall rate compared with the 20.2% rate
that we found, but Trueblood et al followed their
subjects for only 6 months. Our results suggest the
possibility that older adults are falling even more often
Table 3.
Number of Reported Falls per Subject
No. of Falls
per Subject
No. of
Subjects
%
0
57
58
1
22
22
2
11
11
3
3
3
4
2
2
5
2
2
9
1
1
10
1
1
99
100
Average falls/subject (N
⫽99)⫽0.91, SD⫽1.67, Median⫽0
Average falls/subject who fell (n
⫽42)⫽2.14, SD⫽2.0,
Median
⫽1
Table 4.
Summary of Fall Frequency (N
⫽99)
Falls Occurrence
n
%
No falls
57
57.6
1 or more falls
42
42.4
Total
99
100
Multiple Falls
Zero or one fall
79
79.8
Two or more falls
20
20.2
Total
99
100
Fall Severity
No or noninjurious falls
95
96
Injurious falls
4
4
Total
99
100
Table
5.
Logistic
Regression:
Prediction
of
Multiple
Falls
a
Models
Comprising
Independent
and
Control
Variables
Level
of
Significance
%
Correct
Prediction
Correctly
Predicted
Nonmultiple
Fallers
Correctly
Predicted
Multiple
Fallers
Coefficient
of
Terms
(B)
SE
of
B
Odds
Ratio
(Exp
B)
95%
CI
for
B
Lower
Upper
Model
.042
80.8
79/79
1/20
FEC
2.556
1.285
12.884
1.039
159.830
Model
.045
80.8
78/79
2/20
FEC
1.786
1.332
5.967
0.438
81.146
Age
0.072
0.048
1.075
0.978
1.181
Sex
0.822
0.540
2.275
0.790
6.557
a
In
testing
population
subgroups,
FEC
was
predictive
of:
(1)
multiple
falls
in
men
(P
⫽
.033,
n
⫽
39)
but
not
women
(P
⫽
.840,
n
⫽
60),
(2)
multiple
falls
in
those
subjects
who
were
74
years
of
age
or
younger
(P
⫽
.005,
n
⫽
55)
but
not
in
those
subjects
who
were
older
than
74
years
of
age
(P
⫽
.856,
n
⫽
44),
and
(3)
multiple
falls
in
those
subjects
taking
2
o
r
more
medications
(P
⫽
.029,
n
⫽
66)
but
not
in
those
subjects
taking
fewer
than
2
medications
(P
⫽
.169,
n
⫽
33).
Because
of
the
small
sample
sizes,
caution
is
warranted
in
the
interpretation
of
subgroup
results.
Physical Therapy . Volume 83 . Number 4 . April 2003
Boulgarides et al . 335
ўўўўўўўўўўўўўўўўўўўўўўўўўўўў

than is generally reported. In the literature, one third to
one half of community-dwelling older adults fall 1 or
more times in a year.
1–3
Forty-two percent of the subjects
in our study reported at least 1 fall, which is a fairly high
proportion of the sample population. Whether our
sample was unique in terms of fall status or whether the
large number of reported falls was due to the frequency
with which we tracked falls is not known. Use of a fall
report calendar and the frequent follow-up may have
resulted in a more accurate report of falls than in studies
with more infrequent follow-up.
In another prospective study of falls in which subjects
were contacted weekly for 12 months, researchers found
a similar fall rate: 40% of the subjects reported at least 1
fall.
29
Older adults may fall and forget that they have
fallen. Weekly follow-up of 304 older adults over a 12
month period by Cummings and colleagues
30
showed
that 13% to 32% of those with confirmed falls did not
recall falling 3, 6, or 12 months after the fall, and only a
weak correlation was found between falls and recalled
falls. We believe that the possibility of recall errors
underscores the importance of prospective study design
to predict fall risk.
Fall Prediction Tests
We expected that falls would be predicted by some
combination of demographic and health covariates and
the 5 commonly used tests that were selected. In our
opinion, the poor ability to predict falls from data
obtained with these tests suggests that new screening
tests are needed for community-dwelling older adults
who are active. Although logistic regression tests showed
a weak ability to predict multiple falls using FEC, the
FEC, after removal of an extreme score, did not predict
falls. The score, 1.3°/s of sway, fell greater than 2
standard deviations from the mean FEC score. All other
FEC scores ranged from 0.1°/s to 0.9°/s, with 85% of
scores falling between 0.2°/s and 0.5°/s (X
⫽0.371,
SD
⫽0.1618). The ability of the model to predict falls was
weak even with the extreme score included (Tab. 5).
Although logistic regression attributes were statistically
significant, clinical relevance is doubtful because only 1
of 20 falls was correctly predicted.
Trueblood et al
24
found FEO to be predictive of falls.
The mean FEO score was 0.47°/s for fallers and 0.36°/s
for nonfallers. The standard deviation was 0.304°/s for
fallers and 0.118°/s for nonfallers (N
⫽179). With a
standard deviation of 0.118°/s to 0.304°/s, a difference
of 0.11°/s between fallers and nonfallers seems quite
small. In our opinion, differences as small as 0.10°/s (the
difference between means for FEC for multiple and
nonmultiple fallers in our study) and 0.11°/s (the dif-
ference between means for FEO for fallers and nonfall-
ers in the study by Trueblood et al) are not clinically
meaningful.
We selected the BBS for this study because it is designed
to narrow the subject’s base of support to a single-leg
stance. Some researchers
17,21
found better fall prediction
using the BBS than we did, but subjects in those studies
were known to be frail, were residents of a nursing
home, or had an unknown physical activity status. In
other studies of community-dwelling older adults,
15,16
the BBS was not found to be a good predictor of falls.
O’Brien et al
16
tested 49 subjects, 13 of whom reported
1 or more falls in the year before testing. Their subjects
were recruited from family medicine clinics, geriatric
day hospitals, senior centers, and home care programs.
Because some of the locations where they recruited
subjects tend to be used by older adults who need
assistance, these subjects may have been more frail than
the subjects involved in our study. The mean BBS score
for fallers who fell 1 or more times in the study by
O’Brien et al was 45 (range
⫽21–54) as compared with a
mean BBS score of 53.18 (range
⫽46–56) in our study.
The mean BBS score of nonfallers in the study by
O’Brien et al was 55 (range
⫽46–56) as compared with a
mean score of 53.15 (range
⫽34–56) in our study. The
range for nonfallers was much narrower (10 points) in
the study by O’Brien et al than in our study (22 points).
We found virtually no difference in BBS scores between
the groups, whereas O’Brien et al found a 10-point
difference. Even with a less fit population and a greater
difference in scores between fallers and nonfallers than
our study, O’Brien et al found poor sensitivity (54%) for
correctly predicting fallers using the BBS.
Examination of the individual scores of the multiple
fallers in our study showed that many of them did quite
well on the BBS and other performance-based tests. For
instance, one subject scored 55/56 on the BBS but fell 9
times. Two subjects scored 54/56 and 56/56 on the BBS,
and each subject fell 4 times. Some subjects may have
been very active and engaged in more risky activities.
The 3 subjects just mentioned were very active people in
their early to middle 70s. One woman did weight train-
ing and used a stationary bicycle and a ski machine
regularly. One subject swam competitively and partici-
pated in the Senior Olympics. The BBS was not sensitive
enough to uncover factors that contributed to falls in
these older adults who were active. Conversely, 3 subjects
who scored lowest on the BBS—1 who scored 34/56 and
2 who scored 39/56 — had no falls. At least one of these
subjects participated only in activities of daily living. She
did not exercise and was less likely to go into high-risk
situations. Again, we are faced with the multifactorial
nature of falls. Although physical activity is important in
maintaining balance function, people who are active are
more likely to engage in activities that put them at
336 . Boulgarides et al
Physical Therapy . Volume 83 . Number 4 . April 2003

greater risk for falls. Speechley and Tinetti
4
found that
older adults who were vigorous had a lower incidence of
falls (17%) compared with older adults who were frail
(52%), but they were more likely to fall on stairs and
away from home, situations encountered less frequently
by older adults who are frail.
Scores on the TUGT were not predictive of falls. A 10- to
12-second cutoff time to differentiate fallers from non-
fallers has been recommended
24
as has a 13.5-second
cutoff time.
25
The times of nonfallers in our study
clustered around 8 to 10 seconds, and the times of
multiple fallers clustered around 9 to 13 seconds. Many
of the multiple fallers had times that were below com-
monly used cutoff times. Although a cutoff time would
be difficult to find in this population, investigators
should try to determine whether a lower (10-second)
cutoff time should be established for fall risk in
community-dwelling older adults who are active.
In a prospective study similar in design to our study, 100
older adults were tested using the BBS, the Functional
Reach Test, a step-up test, lateral reach, FEO and FEC
measures, and an LOS test in an effort to predict falls
over a 1-year period.
28
The best impairment-based test,
step time during a step-up task, gave only 66% predictive
ability. The best combination of factors gave a 77%
correct prediction.
Factors Affecting Fall Prediction and Fall Risk
Falls are known to be multifactorial,
4,19
and a complex
interaction among different factors determines whether
a person is at risk for falls.
19,31
A model that included the
covariates age and sex with FEC did not improve predic-
tive ability of the model (Tab. 5). Although the sample
size was too small for analysis of subgroups based on age,
sex, and number of medications, exploratory analysis of
subgroups showed that FEC was more predictive of falls
in men, younger subjects, and those taking 2 or more
medications (see footnote in Tab. 5). This preliminary
information suggests that an interaction between FEC
and the covariates of age, sex, or number of medications
may be important in predicting falls. Based on the data
we gathered, we used nQuery Advisor 3.0 software
‡
to
estimate that a sample size of 182 subjects would be
necessary to evaluate a model with 80% power, assuming
an odds ratio of 2.0 for FEC, while controlling for age
(alpha
⫽.05, 2-sided test). In the future, if this or a
similar study were done with a larger sample size,
subjects could be grouped by sex, age, and number of
medications to determine whether multiple-fall predic-
tion results vary in the different groups. The fall screen-
ing tests that effectively predict falls may differ from
group to group.
Many factors affecting fall prediction remain to be
identified. If these factors can be identified, health care
professionals might be able to discern what tests should
be used in different situations. Some tests, for example,
may be appropriate for an active rather than an inactive
population or a relatively younger rather than older
population.
In a study of the effect of physical activity on balance and
falls,
32
the researchers found that older adults who were
active performed better than older adults who were
inactive on some balance tests, including the sharpened
Romberg test (active subjects: X
⫽59.4–60.0 seconds,
standard error [SE]
⫽0.0–0.5 seconds; inactive subjects:
X
⫽41.5–41.8 seconds, SE⫽6.1–7.2 seconds) and one-leg
stance time (active subjects: X
⫽40.0–55.1 seconds,
SE
⫽3.4–4.5 seconds; inactive subjects⫽27.5–33.0 sec-
onds, SE
⫽6.1–7.1 seconds). In a study related to ours
that used the same sample, physical exercise correlated
with improved scores on many balance tests (Boulgar-
ides et al, unpublished data, December 2001). The lack
of significance in fall prediction of these balance tests
may have been influenced by more high-risk activities
that were engaged in by some of the higher scoring
subjects. Although the subjects who were active scored
well on balance tests, they also engaged in more activities
that might result in falls. Some descriptions of falls after
testing included falling off a bicycle, falling while run-
ning backward in a tennis game, and falling while
getting off a bus while touring Europe. Only 4 subjects
had injurious falls. Falls without injuries may not be of as
great a concern as falls with injuries. Whether the
long-term effects of noninjurious falls will be harmful is
not known. Falls of any type we believe should not be
underestimated, particularly because the effect may be
to decrease confidence and thus a person’s willingness
to continue an active lifestyle.
6,7
In general, multiple fallers and nonmultiple fallers both
scored very well on many of the balance tests. The small
sample size, the large number of subjects who were
physically active, and the high level of subject perfor-
mance may have affected the results of the statistical
tests. Multiple falls did occur in this population, but
these falls could not be predicted by the tests. Because
many subjects scored very high on the BBS, the DGI, and
TUGT, a ceiling effect may have occurred, indicating
that these performance-based tests are not suitable for
older adults who are high functioning, even when they
are at risk for falls. Different, possibly more challenging,
performance-based tests might reveal balance deficits
that could cause falls in people who are high function-
ing. The development of new tests for this population is
indicated.
‡
Statistical Solutions Ltd, South Bank, Crosse’s Green, Cork, Ireland.
Physical Therapy . Volume 83 . Number 4 . April 2003
Boulgarides et al . 337
ўўўўўўўўўўўўўўўўўўўўўўўўўўўў

Limitations of the Study
With only 99 subjects, the power of the logistic regres-
sion calculations was determined to be 38% for the FEC
model using nQuery Advisor 3.0 software. Statistical
power of logistic regression tests would have been
greater with a larger sample size. Similar studies should
be done with larger sample sizes. Because the population
studied was quite homogeneous, a larger sample size is
necessary to give the power necessary to show signifi-
cance. A larger sample size would allow tests of the
interaction of factors such as age, number of medica-
tions, and sex with independent variables in a popula-
tion of older adults who are active.
The physical activity level of the subjects in our study
probably does not represent the current population of
older adults in this country, and this may be part of the
reason that results of our study differ from some other
studies. Eighty-four percent of the subjects in our study
reported performing some type of physical exercise,
which included exercising at least one time per week.
The percentage of adults over 65 in the general popu-
lation who participate in regular exercise is reported to
be between 30% and 50%, decreasing to between 15%
and 20% of people over the age of 85 years.
8
Because of
the recruitment of many subjects from a 50 Plus Wellness
program, activity and fitness levels might be expected to
be higher than in the general population. Many subjects
were very active— dancing, walking, swimming, playing
golf or tennis, and competing in sports.
Conclusions
Five currently used balance tests combined with health
and demographic factors did not predict falls in a
sample of community-dwelling older adults who were
active and independent. Two conclusions can be drawn
from the current study. The results reinforce the notion
that fall risk depends on an interaction of many factors
and is particularly difficult to predict in older adults who
live active independent lives. The factors contributing to
falls may interact differently at different ages and activity
levels. A larger sample size than the one used in this
study may reveal the interaction among factors contrib-
uting to fall risk. It is also evident that current tests are
not as successful in predicting fall risk in active older
adults as they have been found to be in more frail
populations. This study indicates the need for develop-
ment and testing of new assessment tools for an increas-
ingly active aging population.
References
1
Sattin RW. Falls among older persons: a public health perspective.
Annu Rev Public Health. 1992;13:489 –508.
2
Tinetti ME, Doucette J, Claus E, Marottoli R. Risk factors for serious
injury during falls by older persons in the community. J Am Geriatr
Soc. 1995;43:1214 –1221.
3
Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for
falls, incontinence, and functional dependence: unifying the approach
to geriatric syndromes. JAMA. 1995;273:1348 –1353.
4
Speechley M, Tinetti M. Falls and injuries in frail and vigorous
community elderly persons. J Am Geriatr Soc. 1991;39:46 –52.
5
Ellis AA, Trent RB. Do the risks and consequences of hospitalized fall
injuries among older adults in California vary by type of fall? J Gerontol
A Biol Sci Med Sci. 2001;56:M686 –M692.
6
Legters K. Fear of falling. Phys Ther. 2002;82:264 –272.
7
Cumming RG, Salkeld G, Thomas M, Szony G. Prospective study of
the impact of fear of falling on activities of daily living, SF-36 scores,
and nursing home admission. J Gerontol A Biol Sci Med Sci. 2000;55:
M299 –M305.
8
Shephard RJ. Aging, Physical Activity and Health. Champaign, Ill:
Human Kinetics; 1997.
9
Steinberg M, Cartwright C, Peel N, Williams G. A sustainable
programme to prevent falls and near falls in community dwelling older
people: results of a randomised trial. J Epidemiol Community
Health. 2000;54:227–232.
10
Yan J. Tai Chi practice improves senior citizens’ balance and arm
movement control. Journal of Aging and Physical Activity. 1998;6:
271–284.
11
Shumway-Cook A, Gruber W, Baldwin M, Liao S. The effect of
multidimensional exercises on balance, mobility, and fall risk in
community-dwelling older adults. Phys Ther. 1997;77:46 –57.
12
Verfaillie D, Nichols J, Turkel E, Hovell M. Effects of resistance,
balance, and gait training on reduction of risk factors leading to falls
in elders. Journal of Aging and Physical Activity. 1997;5:215–228.
13
Province MA, Hadley EC, Hornbrook MC, et al. The effects of
exercise on falls in elderly patients: a preplanned meta-analysis of the
FICSIT trials. JAMA. 1995;273:1341–1347.
14
Rooks D, Ransil B, Hayes W. Self-paced exercise and neuromotor
performance in community-dwelling older adults. Journal of Aging and
Physical Activity. 1997;5:135–149.
15
Bogle Thorbahn LD, Newton RA. Use of the Berg Balance Test to
predict falls in elderly persons. Phys Ther. 1996;76:576 –582.
16
O’Brien K, Pickles B, Culham E. Clinical measures of balance in
community-dwelling elderly female fallers and non-fallers. Physiotherapy
Canada. Summer 1998:212–221.
17
Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring
balance in the elderly: validation of an instrument. Can J Public
Health. 1992;83(suppl 2):S7–S11.
18
Berg K, Wood-Dauphinee S, Williams JI. The Balance Scale: reli-
ability assessment with elderly residents and patients with an acute
stroke. Scand J Rehabil Med. 1995;27:27–36.
19
Tinetti ME, Williams TF, Mayewski R. Fall risk index for elderly
patients based on number of chronic disabilities. Am J Med. 1986;80:
429 – 434.
20
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic
functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:
142–148.
21
Shumway-Cook A, Baldwin M, Polissar NL, Gruber W. Predicting
the probability for falls in community-dwelling older adults. Phys Ther.
1997;77:812– 819.
22
Clark S, Rose DJ, Fujimoto K. Generalizability of the limits of
stability test in the evaluation of dynamic balance among older adults.
Arch Phys Med Rehabil. 1997;78:1078 –1084.
338 . Boulgarides et al
Physical Therapy . Volume 83 . Number 4 . April 2003

23
El-Kashlan HK, Shepard NT, Asher AM, et al. Evaluation of clinical
measures of equilibrium. Larynngoscope. 1998;108:311–319.
24
Trueblood PR, Hodson-Chennault N, McCubbin A, Youngclarke D.
Performance and impairment-based assessments among community
dwelling elderly: sensitivity and specificity. Issues on Aging. 2001;24(1):
2– 6.
25
Shumway-Cook A, Brauer S, Woollacott M. Predicting the probabil-
ity for falls in community-dwelling older adults using the Timed Up &
Go Test. Phys Ther. 2000;80:896 –903.
26 Manual for the Balance Master 6.1: The Objective Quantification of Daily
Life Tasks. Clackamas, Ore: Neurocom International Inc; 1996.
27
Hageman PA, Leibowitz JM, Blanke D. Age and gender effects on
postural control measures. Arch Phys Med Rehabil. 1995;76:961–965.
28
Brauer SG, Burns YR, Galley P. A prospective study of laboratory
and clinical measures of postural stability to predict community-
dwelling fallers. J Gerontol A Biol Med Sci. 2000;55:M469 –M476.
29
Hausdorff JM, Rios DA, Edelberg, HK. Gait variability and fall risk in
community-living older adults: a 1-year prospective study. Arch Phys Med
Rehabil. 2001;82:1050 –1056.
30
Cummings SR, Nevitt MC, Kidd S. Forgetting falls: the limited
accuracy of recall of falls in the elderly. J Am Geriatr Soc. 1988;36:
613– 616.
31
Herndon J, Helmick C, Sattin R, et al. Chronic medical conditions
and risk of fall injury events at home in older adults. J Am Geriatr Soc.
1997;45:739 –743.
32
Bulbulian R, Hargan ML. The effect of activity history and current
activity on static and dynamic postural balance in older adults. Physiol
Behav. 2000;70:319 –325.
Physical Therapy . Volume 83 . Number 4 . April 2003
Boulgarides et al . 339
ўўўўўўўўўўўўўўўўўўўўўўўўўўўў
Wyszukiwarka
Podobne podstrony:
więcej podobnych podstron