
Associations Between Symptoms of Borderline
Personality Disorder, Externalizing Disorders,
and Suicide-Related Behaviors
Lisa M. James
&
Jeanette Taylor
Published online: 4 January 2008
# Springer Science + Business Media, LLC 2007
Abstract Borderline personality disorder and externalizing
disorders are associated with suicide-related behaviors. The
present study examined whether symptoms of borderline
personality disorder mediate the relationship between
externalizing disorders and suicide-related behaviors. Diag-
nostic interviews were administered to 344 participants (n=
233 women). Results indicated that symptoms of antisocial
personality disorder, alcohol use disorders, and drug use
disorders each were significantly associated with suicide
threats and self-injurious behavior in women and symptoms
of antisocial personality disorder were associated with
suicide attempts in women. With the exception of the
association between symptoms of alcohol dependence and
self-injurious behaviors, borderline personality disorder
symptoms mediated or partially mediated all associations
between externalizing disorders and suicide-related behav-
iors in women. These results highlight the importance of
assessment and treatment of borderline personality disorder
symptoms in individuals with externalizing disorders,
particularly in the presence of suicide-related behaviors.
Keywords Borderline personality disorder . Externalizing
disorders . Suicide-related behavior . Mediation
Suicide is among the leading causes of death in the USA
(Kochanek et al.
) and suicide-related behavior was the
fifth most common reason for mental health-related visits to
the emergency room between 1992 and 2001 (Larken et al.
). Suicide-related behaviors (i.e., self-injurious behav-
ior, suicide threats, suicide attempts, and suicide comple-
tions; O
’Carroll et al.
) occur most often among those
with clinical disorders although the prevalence of suicide-
related behaviors in non-clinical samples is noteworthy
(Kessler et al.
). For example, Kessler et al. (
reported that 13.5% of a nationally representative sample of
adults reported lifetime suicidal ideation and 4.6% attemp-
ted suicide. Among young people, ages 15
–24, suicide is
the third-leading cause of death (Kochanek et al.
) and
a study of college students noted that 10% reported
seriously considering suicide in the 12 months prior to the
study and 2% attempted suicide at least once (Brenner et al.
). Prior suicide-related behavior is the single best
predictor of future suicide-related behavior (Joiner et al.
; Kessler et al.
); thus, further understanding the
correlates of suicide-related behavior is important for
assessment and prevention of suicide.
Borderline personality disorder is often associated with
self-injury and suicide attempts (i.e., parasuicidal behavior)
in adults. Approximately 60
–80% of individuals with
borderline personality disorder engage in parasuicidal
behavior (see Linehan and Heard
, for a review), and
10% die of suicide (Paris and Zweig-Frank
). Among
personality disorders, substantial research also documents a
relationship between suicide-related behavior and antisocial
personality disorder (Duberstein and Conwell
; Verona
et al.
). Approximately 30
–40% of suicides are
committed by individuals with Axis II disorders and
borderline personality disorder and antisocial personality
disorder account for a large majority of these (Duberstein
and Conwell
). A consistent relationship between
substance use disorders and suicide-related behaviors has
also been documented (Haw et al.
; Kessler et al.
;
also see Wilcox et al.
, for review) and it has been
reported that up to two thirds of individuals that complete
suicide had a diagnosable substance use disorder (Conwell
J Psychopathol Behav Assess (2008) 30:1
–9
DOI 10.1007/s10862-007-9074-9
L. M. James (
*)
:
J. Taylor
Department of Psychology, Florida State University,
209 Eppes Hall,
Tallahassee, FL 32306-1270, USA
e-mail: james@psy.fsu.edu

et al.
). Adding to a growing body of literature, two
recent epidemiological studies found that symptoms of
antisocial personality disorder and substance use disorders
were associated with suicide attempts and completions
(Verona et al.
; Hills et al.
Thus, in addition to borderline personality disorder, both
antisocial personality disorder and substance use disorders
(i.e., externalizing disorders) are also associated with
suicide-related behavior and recently it has been suggested
that borderline personality disorder might mediate that
relationship (Hills et al.
). This potential link has not
been examined although various lines of evidence support
this possibility. For instance, both antisocial personality
disorder and substance use disorders are highly comorbid
with borderline personality disorder. Approximately 25% of
borderline patients also meet criteria for antisocial person-
ality disorder (Zanarini et al.
), although Axis II
pathology is not limited to psychiatric patients. In fact, one
recent study found that the prevalence of personality
disorders in a community sample was 11% (Ekselius et al.
). Notably, prior research suggests that the risk for
suicide in borderline personality disorder patients is even
greater in the presence of antisocial traits (Black et al.
). Regarding comorbidity with substance use, a recent
review of the literature indicated that approximately 50% of
study participants with borderline personality disorder also
met criteria for an alcohol use disorder and roughly 40%
met criteria for a comorbid drug use disorder (Trull et al.
). Similarly, these authors noted high rates of comorbid
borderline personality disorder among those with substance
use disorders.
Further, these disorders share a common relationship
with impulsivity. Externalizing disorders are characterized
by impulse control problems and acting out behaviors that
may be harmful to oneself or others (Verona and Patrick
) and this conceptualization has garnered substantial
support (Cloninger
; Gorenstein and Newman
McGue et al.
; Moeller and Dougherty
; Sher and
Trull
). Although borderline personality disorder is not
typically considered an externalizing disorder, character-
istics of externalizing disorders such as impulsivity and
self-harm are among the hallmark features of borderline
personality disorder. Impulsivity is considered a core
feature of borderline personality disorder (Links et al.
) and two recent reviews (Bornolova et al.
; Trull
et al.
) suggest that impulsivity might be a common
process that underlies the comorbidity between borderline
personality disorder and substance use disorders. Impulsiv-
ity has also been linked to suicide-related behaviors and
substantial research suggests that impulsivity is associated
with self-injury (Crowell et al.
), suicide attempts
(Dougherty et al.
), and suicide completions (Maser et
al.
Finally, it seems that suicide-related behaviors and
externalizing disorders are underlain by common neurobi-
ological mechanisms. In a review of the literature, Verona
and Patrick (
) noted that a reliable association exists
between decreased serotonergic functioning, suicide-related
behaviors, and features of externalizing disorders such as
impulsivity, aggression, and violence. Serotonergic systems
have also been implicated in borderline personality disor-
der. Oquenda and Mann (
) reviewed various lines of
human and animal research including fenflumarine chal-
lenge, cerebrospinal fluid, and brain imaging studies that
converge on findings of reduced serotonergic functioning in
individuals with borderline personality disorder, particular-
ly in those with higher impulsive and aggressive behavior
or more suicide-related behavior.
In sum, independent lines of research have found that
borderline personality disorder and externalizing disorders
are associated with suicide-related behaviors. These disor-
ders are highly comorbid and share links with personality
traits and neurobiological factors. As suggested by Hills et
al. (
), it is possible that borderline personality disorder
symptoms mediate the relationship between externalizing
disorders and suicide-related behaviors and the goal of the
current study was to assess this possibility in a non-clinical
sample given the prevalence of suicide-related behaviors in
non-clinical populations. Consistent with previous litera-
ture, it was expected that symptoms of externalizing
disorders would be associated with suicide-related behav-
iors but, as suggested by Hills et al. (
), it was
hypothesized that these relationships would become non-
significant after accounting for borderline personality
disorder symptoms. Although it is not possible to draw
conclusions regarding causality in this study due to the
cross-sectional design, several recent studies have similarly
examined mediation in cross-sectional studies to provide a
useful initial test of a model (e.g., Orcutt et al.
; Sachs-
Ericsson et al.
Method
Participants
The data for this study were obtained from a series of
studies aimed at examining risk factors associated with
personality disorders and substance use disorders. Partic-
ipants were 344 individuals (n=233 women) who had
participated in one of three studies conducted between 2001
and 2006 at a large southeastern university. Most of the
participants were college students, including 115 members
of twin pairs recruited for a paid twin study, 123 individuals
recruited for a paid study on physiological reactivity and
substance use, and 70 individuals recruited for a study of
2
J Psychopathol Behav Assess (2008) 30:1
–9

physiological and cognitive factors associated with person-
ality and substance use for which they received credit in an
introductory psychology course. The remainder of the
sample comprised 36 members of twin pairs recruited from
the community with newspaper advertisements for the paid
twin study. Participants were pooled across studies in order
to provide adequate power to test hypotheses given the low
base rate of suicide-related behaviors. Participants were age
18 to 58 years (mean = 20.41, SD = 4.79). The racial
composition was 0.6% American Indian/Alaska Native,
0.6% Asian, 15.0% Black/African American, 9.3% Hispanic/
Latino, 0.9% Native Hawaiian/Other Pacific Islander,
70.1% white, and 3.6% Other (included those that affiliated
with more than one ethnic category and those that felt their
ethnic category was not represented). The racial composition
was largely representative of the racial/ethnic distribution of
the community in which the studies were conducted. Twelve
percent of the sample were freshmen, 30% were sophomores,
26% were juniors, 19% were seniors, and 12% had completed
college. In each study from which participants for this study
were drawn, informed written consent was obtained prior to
beginning any procedures and the university IRB approved all
procedures.
Procedures and Measures
The studies from which the participants were drawn used
similar though not identical methods for assessing person-
ality disorders and substance use disorders. Differences in
assessment measures across the samples are noted below.
Personality Disorder Symptoms
All participants completed semistructured diagnostic inter-
views to assess the presence of Axis II symptoms.
Interviews were conducted by clinical graduate students
trained by one of the authors (J.T.), a Ph.D.-level clinical
psychologist. Seventy participants were administered the
Structured Clinical Interview for DSM-IV Axis II Person-
ality Disorders (SCID-II; First et al.
) and 274 were
administered the Structured Interview for DSM-IV Person-
ality (SIDP-IV; Pfohl et al.
). In all cases, the
interviews were audio taped. In the study that used the
SCID-II, the trained interviewer assigned symptoms. In
the two studies that used the SIDP-IV, two or more clinical
graduate students who reviewed all available information
and came to a consensus on the presence or absence of a
symptom assigned symptoms. In all cases, symptom level
data were then entered into a computer. For this particular
study only items assessing borderline personality disorder
and antisocial personality disorder were included. Symptom
counts of each disorder were created via a computer
algorithm that simply summed the positively endorsed
symptoms. The symptom assessing recurrent suicidal
threats, gestures, or behaviors was not included in the
symptom count for borderline personality disorder. Also,
although the diagnostic interviews include substance use as
part of the criteria for borderline personality disorder
impulsivity, substance use was not included in the
impulsivity criteria for the present study to avoid artificially
inflating comorbidity by means of shared symptomatology.
Similarly, although impulsivity is a feature of both
antisocial personality disorder and borderline personality
disorder, care was taken to avoid coding the same behavior
as impulsive for both disorders. In order to meet the
impulsivity criteria for both disorders participants had to
provide distinct examples of impulsivity that reflected
failure to plan ahead (e.g., walking off of a job) and
impulsivity that could be self-damaging (e.g., promiscuity,
binge-eating, etc.) as consistent with the DSM-IV criteria
for antisocial personality disorder and borderline personal-
ity disorder, respectively.
In the study using the SCID-II, reliability was assessed
by an independent interviewer who was blind to the
original interviewer
’s coding using the audiotapes of the
original interviews to assign symptoms on a random sample
of 10% of cases. In each of the two studies using the SIDP-
IV, the consensus case conference procedure described
above was repeated for a random sample of approximately
15% of cases by an independent team that was blind to the
original team
’s coding. Inter-rater reliability of symptom
counts was excellent across measures and procedures for
both borderline personality disorder (r=0.94
–0.96 for SID-
P; r=0.99 for SCID-II) and antisocial personality disorder
(r=0.84 for SID-P; r=1.0 for SCID-II). Approximately 2%
of the sample met threshold for formal diagnosis of BPD
(i.e., 5+ symptoms) and 6% of the sample met criteria for
ASPD (i.e., 3+ symptoms).
Substance Use Disorder Symptoms
All participants were administered diagnostic interviews to
assess the presence of symptoms of alcohol and drug abuse
and dependence. Drugs assessed included cannabis, stimu-
lants, cocaine, hallucinogens, opioids, sedatives, PCP, and
other (inhalants, steroids, etc.). Participants were adminis-
tered either the Structured Clinical Interview for DSM-IV
Axis I Disorders (SCID-I; First et al.
; n=193) or the
Mini International Neuropsychiatric Interview (MINI;
Sheehan et al.
; n=151). The SCID is often considered
the gold standard of clinical diagnoses (e.g., Shear et al.
) and concordance with the MINI is generally good
(Sheehan et al.
). In all cases, the interviews were
audio taped. For participants in one of the studies (n=70),
SCID symptoms were assigned by the trained interviewer.
The other two studies employed the consensus case
J Psychopathol Behav Assess (2008) 30:1
–9
3
3

conference procedure described above. In all cases, symp-
tom level data were entered into a computer. Separate
symptom counts were generated via computer algorithm for
alcohol abuse, alcohol dependence, drug abuse, and drug
dependence. The latter two variables reflected the number
of symptoms met for the most used drug as reported by the
participant. The reliability procedures described above for
the personality disorder assessments were also used for
substance use disorders. The reliability of symptom counts
was excellent for all classes of substance dependence (r=
1.0 for MINI; r=0.94
–1.0 for SCID-I;) and abuse (r=0.86–
1.0 for MINI; r=0.81
–1.0 for SCID-I) with the following
exceptions for drugs assessed with the SCID-I: sedative
abuse (r=0.69), cannabis abuse (r=0.75),
“other” abuse
(r=0.73) and
“other” dependence (r=0.73), which were
acceptable. A substantial number of participants met the
diagnostic threshold for formal diagnosis of substance use
disorders: alcohol abuse
—26%, alcohol dependence—13%,
drug abuse
—19%, and drug dependence—16%.
Suicide-Related Behavior
Suicide-related behavior was assessed by endorsement of
the borderline personality disorder symptom regarding
recurrent suicide threats, attempts, or self-injurious behav-
ior. For this particular study, sub-threshold cases as well as
those meeting full criteria for suicide-related behavior were
included. Analyses were completed on categorical endorse-
ment of the subcomponents of this item (i.e., threats,
attempts, self-injury), resulting in three dependent varia-
bles. The inter-rater reliability was excellent across meas-
ures and procedures (r=0.89 for SCID-II; r=0.97
–1.0 for
SID-P).
Analyses
According to procedures outlined in Baron and Kenny
(
), independent logistic regression analyses were con-
ducted to test the ability of symptoms of borderline
personality disorder (minus the suicide-related behavior
item), antisocial personality disorder, alcohol dependence,
alcohol abuse, drug dependence, and drug abuse to predict
suicide related behavior (i.e., threats, attempts, and self-
injurious behavior). Any significant associations were
followed up with additional logistic regression analyses to
determine if borderline personality disorder symptoms
mediated the relationship. Mediational analyses were fol-
lowed by Sobel tests, which are designed to formally test the
significance of a mediator (Preacher and Leonardelli
).
Because Sobel tests are conservative (MacKinnon et al.
), p values less than 0.05 were considered significant.
To provide an additional test of borderline personality
disorder symptoms as a mediator, the analyses were
repeated using borderline personality disorder symptoms as
the independent variable predicting suicide-related behav-
iors and mediating effects of each of the externalizing
disorders on that relationship were independently examined.
Results
Prior to data analysis, all variables were examined for
outlier values and normality of score distributions. Univar-
iate outlier values were adjusted after bringing the scores to
within three times the standard deviation of the mean of
each variable. Distributions for symptoms of antisocial
personality disorder and drug dependence were log trans-
formed to correct for kurtosis and all analyses were
completed on the transformed variables. For ease of
interpretation, results for transformed variables are pre-
sented in terms of raw scores. All remaining distributions
were normal.
Means and standard deviations for all variables are
presented in Table
. Missing data resulted in variable
sample sizes as indicated in Table
. Men endorsed
significantly more symptoms of antisocial personality
disorder and substance use disorders than women. There
was no gender difference for borderline personality disorder
symptoms or any of the suicide-related variables. The
relationships among the variables also differed for men and
women (Table
). Focused comparisons of effect size
contrasting the magnitude of the correlations between men
and women (Cohen
’s q) indicated generally small to
medium effects ranging from 0.01 to 0.38 (mean=0.15).
In women, all externalizing disorder symptoms were
associated with suicide threats and self-injurious behavior.
Only endorsement of symptoms of antisocial personality
disorder or borderline personality disorder was correlated
with suicide attempts in women. In men, borderline
personality disorder symptoms were significantly correlated
with recurrent self-injurious behavior. This was the only
significant correlation between externalizing disorder
symptoms and suicide-related behavior in men, suggesting
that the proposed mediation analyses were not warranted in
this sample of men. Thus, the following analyses were only
completed for women.
Logistic regressions indicated that symptoms of each of
the externalizing disorders significantly predicted suicide
threats in women and borderline personality disorder
symptoms mediated these relationships (Table
). Only
symptoms of antisocial personality disorder predicted
recurrent suicide attempts in women [Wald=8.28, Exp (B) =
66.42, p<0.004] and this relationship was also mediated by
borderline personality disorder symptoms (p>0.09). As with
suicide threats, symptoms of each of the externalizing
disorders significantly predicted self-injurious behavior in
4
J Psychopathol Behav Assess (2008) 30:1
–9
women (Table
). Borderline personality disorder symptoms
mediated the relationships between symptoms of drug
dependence and drug abuse with self-injurious behavior.
The relationships between alcohol abuse symptoms and
antisocial personality disorder symptoms to self-injury were
partially mediated by symptoms of borderline personality
disorder. Borderline personality disorder symptoms failed to
mediate the relationship between alcohol dependence symp-
toms and self-injury
1
. Sobel test statistics were computed for
each of the significant mediation analyses. In all cases,
borderline personality disorder symptoms significantly re-
duced the effect of symptoms of externalizing disorders on
suicide-related variables, formally demonstrating that bor-
derline personality disorder symptoms significantly mediated
these relationships (p<0.005 except for the associations
between symptoms of alcohol use disorders and suicide-
related variables which were significant at p<0.05).
Analyses were repeated using borderline personality
disorder symptoms as the independent variable predicting
suicide-related behaviors and mediating effects of each of
the externalizing disorders on that relationship were
independently examined. The relationship between border-
line personality disorder symptoms and suicide-related
behaviors remained significant at p<0.001 in all of the
analyses.
Discussion
Consistent with previous studies utilizing community
samples (Hills et al.
; Verona et al.
), externalizing
disorder symptoms were associated with suicide-related
behavior in the current study, providing further evidence
that suicide-related behaviors are not limited to clinical
samples; however, self-injury, suicide attempts, and suicide
threats were only associated with symptoms of externaliz-
ing disorders in women in the present study. The current
sample was comprised of considerably more women than
men and relatively few men endorsed suicide-related
behavior in the current study so there may not have been
adequate power to examine these relationships in men.
Similarly, generally low endorsement of suicide-related
behavior may have limited power to detect gender differ-
ences on suicide-related variables as previous studies have
found that women were significantly more likely to engage
in suicide behaviors than men (Verona et al.
). The
findings regarding gender differences in externalizing
disorder symptoms were in the expected direction and
consistent with previous literature. In the present study
there were no gender differences in the mean number of
borderline personality disorder symptoms. Similarly, Johnson
et al. (
) reported no gender differences regarding the
mean numbers of BPD criteria in patients diagnosed with
BPD although they reported that almost three times as many
women met diagnostic criteria for BPD than men. In line
with the present study and with Johnson et al., Skodol and
Bender (
) reviewed several studies that found little to no
gender difference in borderline personality disorder symp-
tomatology and concluded that reported gender differences
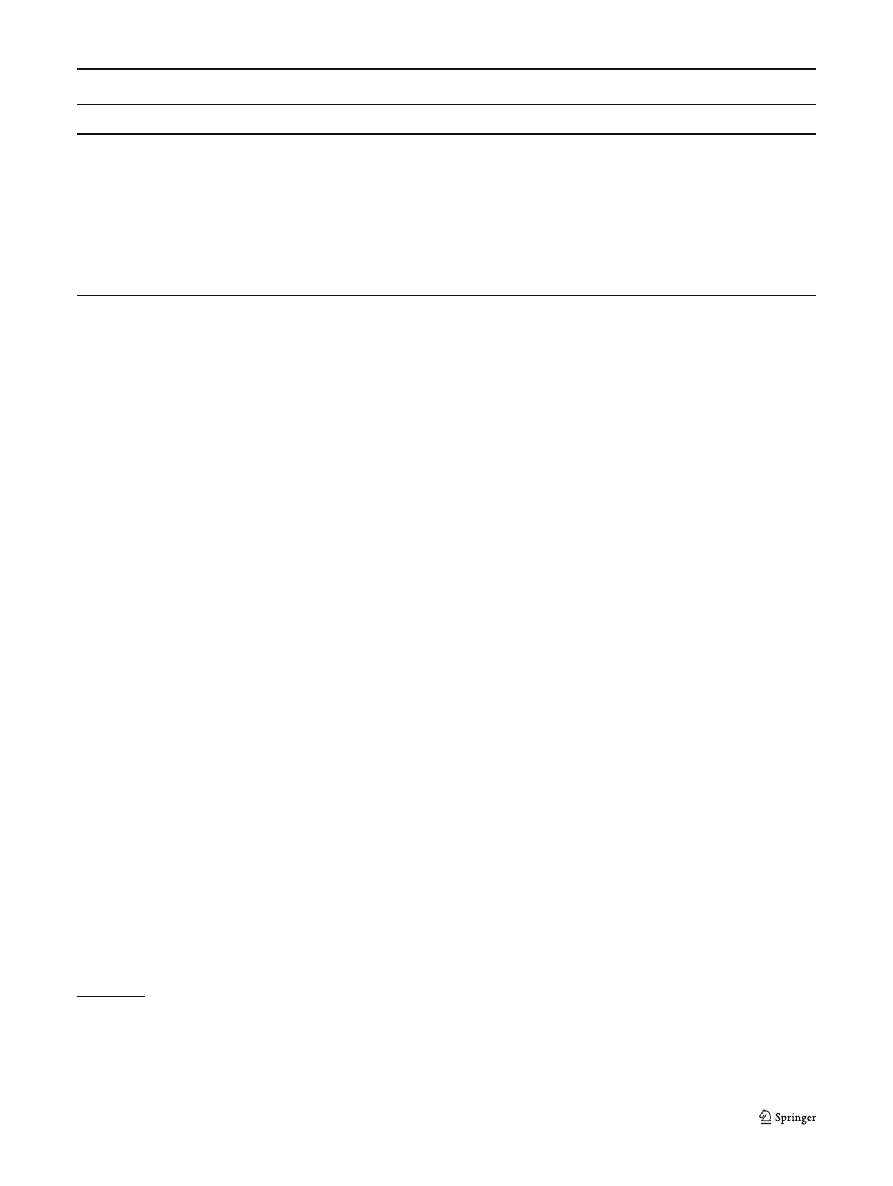
Table 1 Means, standard deviations, and percent endorsement of variables
Men
N
b
(%)
c
Women
N
b
(%)
c
t
ASPD
0.77 (1.12)
109 (40.5)
0.31 (.81)
233 (16.7)
2.88**
Alc-D
1.25 (1.63)
103 (44.5)
0.69 (1.17)
223 (33.5)
3.28**
Alc-A
0.61 (0.92)
104 (34.5)
0.33 (0.67)
219 (21.8)
2.88**
BPD
0.60 (0.86)
110 (39.5)
0.57 (1.04)
227 (30.9)
ns
Drug-D
1.04 (1.7)
109 (31.8)
0.67 (1.43)
227 (21.8)
2.13*
Drug-A
0.43 (0.82)
107 (26.4)
0.22 (0.57)
225 (14.6)
2.60**
Threat
5
a
111 (4.6)
16
a
233 (6.9)
ns
d
Attempt
2
a
111 (1.9)
11
a
233 (4.7)
ns
d
SIB
6
a
111 (5.6)
22
a
233 (9.4)
ns
d
ASPD Antisocial personality disorder symptoms, Alc-D alcohol dependence symptoms, Alc-A alcohol abuse symptoms, BPD borderline
personality disorder symptoms, Drug-D drug dependence symptoms, Drug-A drug abuse symptoms, threat suicide threats, attempt suicide
attempts, SIB self-injurious behavior
*p<0.05
**p<0.01
a
Number of participants endorsing
b
Number of participants with data on variable
c
Percent of sample endorsing at least one symptom
d
Mann
–Whitney U test
1
Since some of the participants (n=142) used in this study were
members of a twin pair, one twin was randomly excluded from
complete twin pairs and the data were reanalyzed. The results
remained unchanged except symptoms of drug dependence no longer
predicted suicide threats (p>0.117).
J Psychopathol Behav Assess (2008) 30:1
–9
5
5
might be a result of biases in sampling or in the application
and assessment of diagnostic criteria.
In general, there was relatively low endorsement of
suicide-related behaviors in this sample, particularly in
men, and considerably fewer participants endorsed suicide
threats and attempts as compared to self-injurious behavior.
Regarding suicide attempts, it is interesting that only
antisocial personality disorder symptoms and borderline
personality disorder symptoms were predictive of suicide
attempts in women. Alcohol and drug use have been
associated with suicide attempts in previous studies so it
is unclear why this relationship did not bear out in the
present study. One possibility is that alcohol and drug use
may be relatively normative in a sample containing a
substantial portion of undergraduate students. In contrast,
those endorsing symptoms of borderline or antisocial
personality disorder may be more pathological and more
prone to extreme behaviors such as suicide attempts. In
addition, drug use in this study was predominantly
characterized by cannabis abuse and dependence. Although
there is limited research examining the association of
suicide related behaviors and cannabis use (Wilcox et al.
), the available literature suggests that suicide risk in
cannabis users is indirectly conferred from environmental
factors (i.e., sociodemographic disadvantage) and/or comor-
bidity with other disorders rather than directly associated
with cannabis use (Beautrais et al.
). In contrast,
substantial research (see Wilcox et al.
for review)
supports robust associations between other drugs (e.g.,
opiates) and suicide attempts. Thus, replication of this study
in a sample of heterogeneous substance users may help
clarify whether the results of the current study extend to
other types of drugs.
In contrast to suicide attempts, all variables of interest
were associated with self-injurious behavior and suicide
threats in women. This study adds to the growing body of
literature documenting associations between externalizing
disorders and self-injury but is among the first studies to
examine the relationship between externalizing disorders
and suicide threats. In the present study, symptoms of
substance use disorders and antisocial personality disorder
were each associated with recurrent suicide threats in
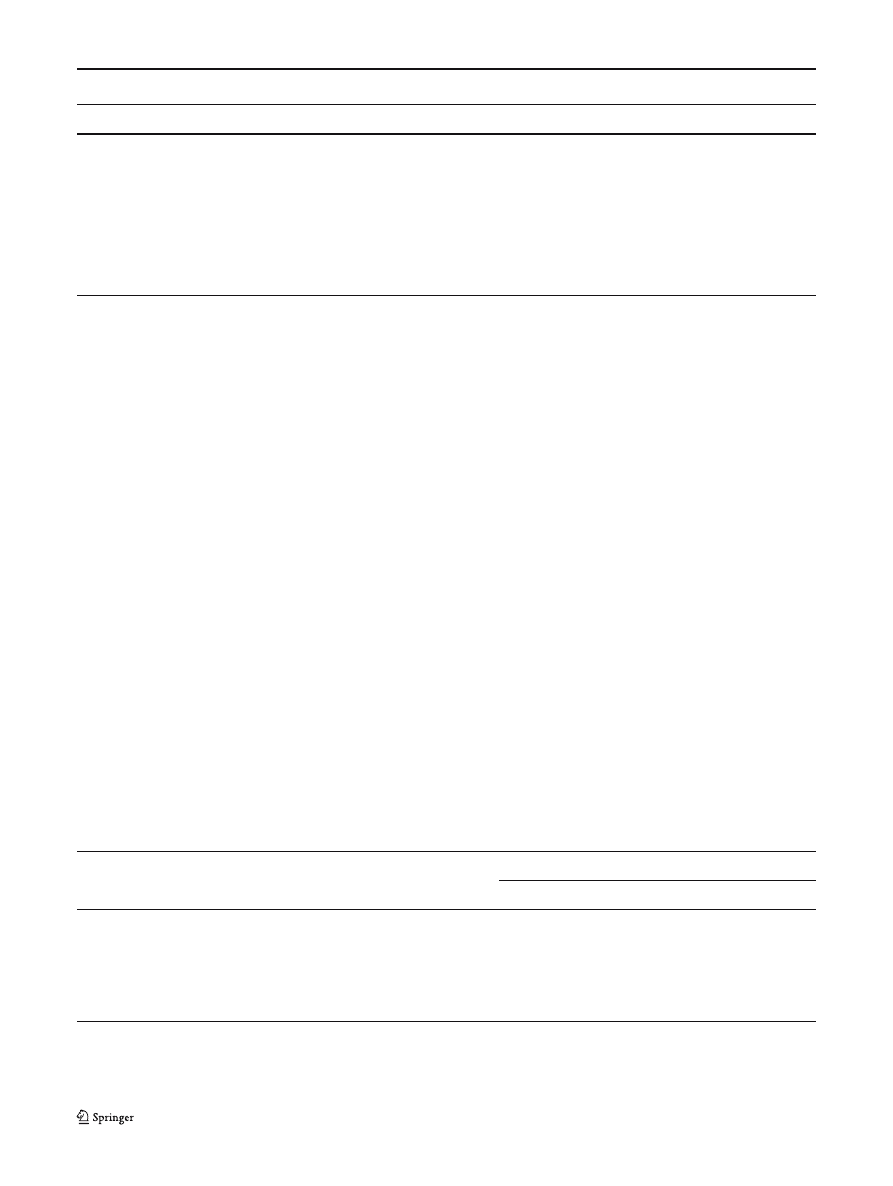
Table 3 Logistic regression and mediation analyses for suicide threats in women
Controlling for BPD
B
SE B
Wald value
EXP(B)
p value
B
SE B
Wald value
EXP(B)
p value
ASPD
4.22
1.31
10.35
67.79
0.001
2.36
1.45
2.68
10.62
0.102
Alc-D
0.44
0.18
6.34
1.55
0.012
0.39
0.22
3.11
1.48
0.078
Alc-A
0.76
0.31
6.06
2.15
0.014
0.58
0.38
2.37
1.79
0.124
Drug-D
2.36
0.94
6.29
10.54
0.012
0.47
1.17
0.16
1.59
0.690
Drug-A
0.85
0.31
7.82
2.35
0.005
0.26
0.36
0.52
1.29
0.47
BPD
1.11
0.21
28.63
3.03
0.000
Significant results are in bold.
ASPD Antisocial personality disorder symptoms, Alc-D alcohol dependence symptoms, Alc-A alcohol abuse symptoms, BPD borderline
personality disorder symptoms, Drug-D drug dependence symptoms, Drug-A drug abuse symptoms
Table 2 Correlation for all variables in men and women
Variable
ASPD
Alc-D
Alc-A
BPD
Drug-D
Drug-A
Threat
Attempt
SIB
ASPD
–
0.17**
0.33***
0.41***
0.21**
0.32***
0.27***
0.21**
0.26***
Alc-D
0.23*
–
0.70***
0.15*
0.36***
0.29***
0.18**
0.05
0.30***
Alc-A
0.39***
0.80***
–
0.22**
0.44***
0.29***
0.18**
0.05
0.22**
BPD
0.34***
0.49***
0.48***
–
0.32***
0.34***
0.46***
0.29***
0.38***
Drug-D
0.42***
0.44***
0.47***
0.39***
–
0.68***
0.17**
0.12
0.22**
Drug-A
0.41***
0.19
0.29**
0.27**
0.63***
–
0.21**
0.13
0.15*
Threat
0.01
−0.01
0.05
0.12
0.02
0.02
–
0.50***
0.51***
Attempt
0.03
0.06
0.14
0.14
0.08
−0.05
0.62***
–
0.35***
SIB
0.09
0.09
0.15
0.28**
0.08
0.05
0.72***
0.57***
–
Correlations for men are below the diagonal. Correlations for women are above the diagonal. ASPD Antisocial personality disorder symptoms,
Alc-D alcohol dependence symptoms, Alc-A alcohol abuse symptoms, BPD borderline personality disorder symptoms, Drug-D drug dependence
symptoms, Drug-A drug abuse symptoms, threat suicide threats, attempt suicide attempts, SIB self-injurious behavior
*p<0.05
**p<0.01
***p<0.001
6
J Psychopathol Behav Assess (2008) 30:1
–9

women and this is consistent with findings from the only
other study that examined this relationship. Lambert and
Bonner (
) noted that patients who threatened suicide to
increase the chance of hospital admission were more likely
to have substance dependence and exhibit antisocial
behavior. Both self-injury (Cooper et al.
) and suicide
threats (Shafii et al.
) are good indicators of future
suicide-related behaviors and additional research regarding
the associations between these behaviors and externalizing
disorders may provide useful clues for treatment and
prevention of suicidal behavior in populations characterized
by externalizing pathology.
As expected, symptoms of borderline personality disor-
der mediated most of the relationships between symptoms
of externalizing disorders and suicide-related behavior in
women. Notably, the relationships between symptoms of
alcohol-related disorders and self-injurious behavior and
symptoms of antisocial personality disorder and self-
injurious behaviors in women were not fully accounted
for by borderline personality disorder symptoms. One
possible explanation for this is that different processes
drive self-injurious behavior in women with alcohol-related
symptoms and antisocial personality disorder symptoms as
compared to women with drug-related symptoms. For
instance, the former may be driven by negative emotional-
ity whereas the latter may be linked more to impulsivity.
Prominent theories of suicide such as the hopelessness
theory of Beck et al. (
) and Baumeister
’s (
escape theory emphasize the role of negative affect and lack
of impulse control, respectively, in suicidal behavior. Other
theorists have proposed subtypes of suicidality (e.g., Apter
et al.
; Durkheim 1897/
). Apter et al. (
suggest that there are two types of suicidal behaviors: one
associated with depression and characterized by a wish to
die and another associated with aggression and impulsivity
and characterized by a desire to escape momentarily (Apter
et al.
). Inappropriate anger that can include aggression
and impulsivity are features of borderline personality
disorder and may be the mechanisms through which
borderline personality disorder symptoms mediated or
partially mediated most of the relationships between
externalizing disorders and suicide-related behaviors. That
is, for some individuals, suicide threats, attempts, or self-
injurious behavior may be attempts, albeit ineffective, to
communicate or manage anger or frustration. In contrast,
symptoms of borderline personality disorder did not
mediate the relationship between symptoms of alcohol
dependence and self-injurious behavior, suggesting that
relationship may be more strongly driven by depression.
The current study provides some initial insight into the
relationship between externalizing disorders and suicide-
related behaviors, particularly in women, and suggests
several additional avenues for future research. The use of
clinical interviews in a relatively large sample is a notable
strength of the current study. In addition, alcohol and drug
use were not included as part of the impulsivity criteria for
borderline personality disorder, reducing the possibility that
associations between symptoms of substance use disorders
and borderline personality disorder are limited to symptom
overlap. Similarly, an effort was made to reduce symptom
overlap between borderline personality disorder and antiso-
cial personality disorder by carefully assessing impulsivity.
The use of the borderline personality disorder symptom
regarding recurrent suicide threats, attempts, and self-injury
as an outcome measure was a limitation of the current
study. Future studies utilizing standard comprehensive
measures of suicide-related behaviors would be a useful
contribution to this area. Another limitation of the current
study was that men were under-represented and, due to
their low endorsement of suicide-related behaviors, there
may not have been adequate power to examine relation-
ships between externalizing disorders and suicide-related
behaviors in men. Previous studies reporting significant
associations between externalizing disorders and suicide-
related behaviors in men utilized large epidemiological
samples. For instance, Verona et al. (
) reported on
2,265 men. Of those, only 44 men (1.9%) had attempted
suicide in their lifetime. Thus, the rate of suicide-related
Table 4 Logistic regression and mediation analyses for self-injurious behavior in women
Controlling for BPD
B
SE B
Wald value
EXP(B)
p value
B
SE B
Wald value
EXP(B)
p value
ASPD
4.35
1.24
12.41
77.88
0.000
2.78
1.32
4.42
16.18
0.036
Alc-D
0.61
0.16
15.48
1.84
0.000
0.58
0.17
12.02
1.79
0.001
Alc-A
0.83
0.27
9.30
2.29
0.002
0.67
0.30
5.07
1.96
0.024
Drug-D
2.84
0.84
11.55
17.12
0.001
1.69
0.95
3.20
5.44
0.074
Drug-A
0.64
0.29
4.67
1.89
0.031
0.14
0.33
0.18
1.15
0.67
BPD
0.84
0.17
23.42
2.31
0.000
Significant results are in bold.
ASPD Antisocial personality disorder symptoms, Alc-D alcohol dependence symptoms, Alc-A alcohol abuse symptoms, BPD borderline
personality disorder symptoms, Drug-D drug dependence symptoms, Drug-A drug abuse symptoms
J Psychopathol Behav Assess (2008) 30:1
–9
7
7

behavior in the current study is comparable although a
larger sample may have been necessary to detect significant
relationships. Although externalizing disorders are associ-
ated with suicide-related behavior even after accounting for
depression and other internalizing disorders (Verona et al.
), it is possible that affective disorders may contribute
to or partially explain suicide-related behaviors. It was not
possible to examine the potential impact of affective
disorders on suicide-related behaviors in this sample and
future research examining associations between externaliz-
ing disorders, borderline personality disorder, and suicide-
related behaviors would be enhanced by the ability to parse
out the influence of affective disorders on these associa-
tions. Another limitation is that the sample was derived by
combining separately recruited participants from different,
albeit very similar, studies. The diagnostic interviews used
for the studies are generally comparable in terms of
psychometric properties and are widely used; however, it
is possible that the different formats used across studies
result in different response styles, which potentially
represents a limitation of the current study. Moreover, some
of the participants were members of a twin pair, which
might limit generalizability. Finally, the data from the
present study were cross-sectional, which prohibits con-
clusions regarding causality. Future studies utilizing longi-
tudinal designs are necessary to establish temporal
sequence and help rule out alternative explanations. Despite
these limitations, the current study provides a useful step
toward understanding suicide-related behaviors as they
relate to externalizing disorders, especially in women.
The results of this study suggest important consider-
ations regarding treatment of externalizing disorders. In
both men and women, borderline personality disorder was
highly associated with externalizing disorders. Thus,
assessment and treatment of borderline personality disorder
symptoms in individuals with externalizing disorders is
important, particularly in the presence of suicide-related
behaviors. Furthermore, thorough assessment of borderline
personality disorder may be especially important in settings
that focus on treating substance use disorders where Axis II
assessment may not be a priority. Finally, for individuals
with borderline personality disorder symptoms, treatment
outcomes for externalizing disorders may be enhanced by
incorporation of techniques designed specifically for bor-
derline personality disorder such as Linehan
’s (
dialectical behavior therapy.
References
Apter, A., Gothelf, D., Orbach, I., Weizman, R., Ratzoni, G., Har-
Even, D., et al. (1995). Correlation of suicidal and violent
behavior in different diagnostic categories of hospitalized
adolescent inpatients. Journal of the American Academy of Child
and Adolescent Psychiatry, 34(7), 912
–918.
Baron, R. M., & Kenny, D. A. (1986). The moderator
–mediator
variable distinction in social psychological research: Conceptual,
strategic, and statistical considerations. Journal of Personality
and Social Psychology, 51, 1173
–1182.
Baumeister, R. F. (1990). Suicide as escape from self. Psychological
Reivew, 97, 90
–113.
Beautrais, A. L., Joyce, P. R., & Mulder, R. T. (1999). Cannabis abuse
and serious suicide attempts. Addiction, 94(8), 1155
–1164.
Beck, A. T., Steer, R., Kovacs, M., & Garrison, B. (1985).
Hopelessness and eventual suicide: A 10-year prospective study
of patients hospitalized with suicidal ideation. American Journal
of Psychiatry, 142, 559
–563.
Black, D. W., Blum, M., Pfohl, B., & Hale, N. (2004). Suicidal
behavior in borderline personality disorder: prevalence, risk
factors, prediction, and prevention. Journal of Personality
Disorders, 18(3), 226
–239.
Bornovalova, M. A., Lejuez, C. W., Daughters, S. B., Rosenthal, M. Z., &
Lynch, T. R. (2005). Impulsivity as a common process across
borderline personality and substance use disorders. Clinical
Psychology Review, 25, 790
–812.
Brenner, N. D., Barrios, L. C., & Hassan, S. S. (1999). Suicidal
ideation among college students in the United States. Journal of
Consulting and Clinical Psychology, 67(6), 1004
–1008.
Cloninger, C. R. (1987). Neurogenetic adaptive mechanisms in
alcoholism. Science, 236, 410
–416.
Conwell, Y., Duberstein, P. R., Cox, C., Hermann, J. H., Forbes, N. T.,
& Caine, E. D. (1996). Relationships of age and axis I diagnoses
in victims of completed suicide: a psychological autopsy study.
American Journal of Psychiatry, 153(8), 1001
–1008.
Cooper, J., Kapur, N., Webb, R., Lawlor, M., Guthrie, E., Mackway-
Jone, K., et al. (2005). Suicide after deliberate self-harm:
A 4-year cohort study. American Journal of Psychiatry, 162(2),
297
–303.
Crowell, S. E., Beauchaine, T. P., McCauley, E., Smith, C. J.,
Stevens, A. L., & Sylvers, P. (2005). Psychological, autonomic,
and serotonergic correlates of parasuicide among adolescent
girls. Development and Psychopathology, 17(4), 1105
–1127.
Dougherty, D. B., Mathias, C. W., Marsh, T. M., Papageorgiou, T. D.,
Swann, A. C., & Moeller, F. G. (2004). Laboratory measured
behavioral impulsivity relates to suicide attempt history. Suicide
and Life-Threatening Behavior, 34(4), 374
–385.
Duberstein, P. R., & Conwell, Y. (1997). Personality disorders and
completed suicide: A methodological and conceptual review.
Clinical Psychology: Science and Practice, 4(4), 359
–376.
Durkheim, E. (1951). Suicide: A study in sociology (J. A. Spaulding &
G. Simpson, Trans.). Illinois: Free Press (Original work pub-
lished in 1897).
Ekselius, L., Tillfors, M., Furmark, T., & Fredrikson, M. (2001).
Personality disorders in the general population: DSM-IV and
ICD-10 defined prevalence as related to sociodemographic
profile. Personality and Individual Differences, 30, 311
–320.
First, M. B., Gibbon, M., Spitzer, R. L., Williams, J., & Benjamin, L. S.
(1997). Structured clinical interview for DSM- IV axis II
personality disorders (SCID-II). Washington, DC: American
Psychiatric Press Inc.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. E. W. (1995).
Structured clinical interview for DSM-IV Axis I, disorders-non-
patient Edition (SCID-I/NP, Version 2.0). New York: Biometrics
Research Department, State Psychiatric Institute.
Gorenstein, E. E., & Newman, J. P. (1980). Disinhibitory psychopa-
thology: A new perspective and a model for research. Psycho-
logical Review, 87, 301
–315.
Haw, C., Hawton, K., Casey, D., Bale, E., & Shepherd, A. (2005).
Alcohol dependence, excessive drinking and deliberate self-
8
J Psychopathol Behav Assess (2008) 30:1
–9

harm: Trends and patterns in Oxford, 1989
–2002. Social
Psychiatry and Psychiatric Epidemiology, 40(12), 964
–971.
Hills, A. L., Cox, B. J., McWilliams, L. A., & Sareen, J. (2005).
Suicide attempts and externalizing psychopathology in a nation-
ally representative sample. Comprehensive Psychiatry, 46(5),
334
–339.
Johnson, D. M., Shea, M. T., Yen, S., Battle, C. L., Zlotnick, C.,
Sanislow, C. A., et al. (2003). Gender differences in borderline
personality disorder: Findings from the Collaborative Longitudi-
nal Personality Disorders Study. Comprehensive Psychiatry, 44
(4), 284
–292.
Joiner, T. E., Conwell, Y., Fitzpatrick, K. K., Witte, T. K., Schmidt, N. B.,
Berlim, M. T., et al. (2005). Four studies on how past and current
suicidality relate even when
“everything but the kitchen sink” is
covaried. Journal of Abnormal Psychology, 114(2), 291
–303.
Kessler, R. C., Borges, G., & Walters, E. (1999). Prevalence of and
risk factors for lifetime suicide attempts in the National
Comorbidity Survey. Archives of General Psychiatry, 56(7),
617
–626.
Kochanek, K. D., Murphy, S. L., Anderson, R. N., & Scott, C. (2004).
Deaths: final data for 2002. National Vital Statistics Reports, 53
(5), 1
–115.
Lambert, M. T., & Bonner, J. (1996). Characteristics and six-month
outcome of patients who use suicide threats to seek hospital
admission. Psychiatric Services, 47(8), 871
–873.
Larken, G. L., Classen, C. A., Emond, J. A., Pelletier, A. J., &
Camargo, C. A. (2005). Trends in U.S. emergency department
visits for mental health conditions, 1992 to 2001. Psychiatric
Services, 56, 671
–677.
Linehan, M. M. (1993). Cognitive behavioral treatment of borderline
personality disorder. New York: Guilford Press.
Linehan, M. M., & Heard, H. (1999). Borderline personality disorder:
costs, course, and treatment outcomes. In N. Miller, & K.
Magruder (Eds.) The cost-effectiveness of psychotherapy: A
guide for practitioners, researchers, and policy-makers (pp.
291
–305). New York: Oxford Press.
Links, P. S., Heslegrave, R., & van Reekum, R. (1999). Impulsivity:
Core aspect of borderline personality disorder. Journal of
Personality Disorders, 13(1), 1
–9.
MacKinnon, D. P., Warsi, G., & Dwyer, J. H. (1995). A simulation
study of mediated effect measures. Multivariate Behavioral
Research, 30, 41
–62.
Maser, J. D., Akiskal, H. S., Schettler, P., Scheftner, W., Mueller, T.,
Endicott, J., et al. (2002). Can temperament identify affectively
ill patients who engage in lethal or near-lethal suicidal behavior?
A 14-year prospective study. Suicide and Life-Threatening
Behavior, 32(1), 10
–32.
McGue, M., Slutske, W., & Iacono, W. G. (1999). Personality and
substance use disorders: II. Alcoholism versus drug use
disorders. Journal of Consulting and Clinical Psychology, 67
(3), 394
–404.
Moeller, F. G., & Dougherty, D. M. (2002). Impulsivity and substance
abuse: What is the connection? Addictive Disorders and Their
Treatment, 1(1), 3
–10.
O
’Carroll, P. W., Berman, A. L., Maris, R. W., Moscicki, E. K.,
Tanney, B. L., & Silverman, M. M. (1996). Beyond the tower of
Babel: A nomenclature for suicidology. Suicide and Life-
Threatening Behavior, 36(3), 237
–252.
Oquenda, M. A., & Mann, J. J. (2000). The biology and impulsivity
and suicidality. The Psychiatric Clinics of North America, 23(1),
11
–25.
Orcutt, H. K., Pickett, S. M., & Pope, E. P. (2005). Experiential avoidance
and forgiveness as mediators in the relation between traumatic
interpersonal events and posttraumatic stress disorder symptoms.
Journal of Social & Clinical Psychology, 24(7), 1003
–1029.
Paris, J., & Zweig-Frank, H. (2001). A 27-year follow-up of patients
with borderline personality disorder. Comprehensive Psychiatry,
42, 782
–787.
Pfohl, B., Blum, N., & Zimmerman, M. (1994). Structured interview
for DSM-IV personality: SIDP-IV. Iowa City, IA: American
Psychiatric Publishing.
Preacher, K. J., & Leonardelli, G. J. (2001). Calculation for the Sobel
test: An interactive calculation tool for mediation tests [Computer
software]. Available from
http://www.unc.edu~preacher/sobel/
(March).
Sachs-Ericsson, N., Verona, E., Joiner, T., & Preacher, K. J. (2006).
Parental verbal abuse and the mediating role of self-criticism in adult
internalizing disorders. Journal of Affective Disorders, 93, 71
–78.
Shafii, M., Carrigan, S., Whittinghill, J. R., & Derrick, A. (1985).
Psychological autopsy of completed suicide in children and
adolescents. American Journal of Psychiatry, 142(9), 1061
–1064.
Shear, M. K., Greeno, C., Kang, J., Ludewig, D., Frank, E., Swartz, H. A.,
et al. (2000). Diagnosis of nonpsychotic patients in community
clinics. American Journal of Psychiatry, 157, 581
–587.
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J.,
Weiller, E., et al. (1998). The Mini-International Neuropsychiat-
ric Interview (M.I.N.I.): The development and validation of a
structured diagnostic psychiatric interview for DSM-IV and ICD-
10. Journal of Clinical Psychiatry, 59, 22
–33.
Sher, K. J., & Trull, T. J. (1994). Personality and disinhibitory
psychopathology: Alcoholism and antisocial personality disorder.
Journal of Abnormal Psychology, 103, 92
–102.
Skodol, A. E., & Bender, D. S. (2003). Why are women diagnosed
borderline more than men? Psychiatric Quarterly, 74(4), 349
–360.
Trull, T. J., Sher, K. J., Minks-Brown, C., Durbin, J., & Burr, R.
(2000). Borderline personality disorder and substance use
disorders: A review and integration. Clinical Psychology Review,
20(2), 235
–253.
Verona, E., & Patrick, C. J. (2000). Suicide risk in externalizing
syndromes: temperamental and neurobiological underpinnings. In
T. E. Joiner, & M. D. Rudd (Eds.) Suicide science: Expanding
the boundaries (pp. 137
–173). New York, NY: Kluwer.
Verona, E., Patrick, C. J., & Joiner, T. E. (2001). Psychopathy,
antisocial personality, and suicide risk. Journal of Abnormal
Psychology, 110(3), 462
–470.
Verona, E., Sachs-Ericsson, N., & Joiner, T. E. (2004). Suicide attempts
associated with externalizing psychopathology in an epidemio-
logical sample. American Journal of Psychiatry, 161, 444
–451.
Wilcox, H. C., Conner, K. R., & Caine, E. D. (2004). Association of
alcohol and drug use disorders and completed suicide: An
empirical review of cohort studies. Drug and Alcohol Depen-
dence. Special Issue: Drug Abuse and Suicidal Behavior, 76
(Suppl7), 11
–19.
Zanarini, M. C., Frankenburg, F. R., Dubo, E. D., Sickel, A. E., Trikha,
A., Levin, A., et al. (1998). Axis II comorbidity of borderline
personality disorder. Comprehensive Psychiatry, 39(5), 296
–302.
J Psychopathol Behav Assess (2008) 30:1
–9
9
9
Wyszukiwarka
Podobne podstrony:
Biological Underpinnings of Borderline Personality Disorder
No Man's land Gender bias and social constructivism in the diagnosis of borderline personality disor
Biological Underpinnings of Borderline Personality Disorder
Family Experience of Borderline Personality Disorder
No Man s land Gender bias and social constructivism in the diagnosis of borderline personality disor
Borderline Personality Disorder and Adolescence
APA practice guideline for the treatment of patients with Borderline Personality Disorder
Hypothesized Mechanisms of Change in Cognitive Therapy for Borderline Personality Disorder
więcej podobnych podstron