C
ha
pt
er
29
5
Susan P. Weinstein, MD
Screening MaMMography
1. What is a screening mammogram?
A screening mammogram is a radiographic examination of the breasts performed for early detection of breast cancer
in asymptomatic women.
2. When should an average woman start getting mammograms?
The American College of Radiology recommends that a woman get a first mammogram at age 40 and annual
mammograms thereafter.
3. Are there instances when screening should start earlier than 40?
Patients with a history of Hodgkin disease treated with radiation or women with a strong family history of breast cancer
may be candidates for earlier screening. In women treated for Hodgkin disease, surveillance may begin 10 years after
chest wall/mediastinal radiation exposure. Patients who received radiation therapy during puberty are at greatest
risk for breast cancer. Patients who received radiation therapy after age 30 have a minimally increased risk over the
general population. For patients with a history of a first-degree relative with breast cancer, screening should begin
10 years before the age at which the relative was diagnosed. If the relative was diagnosed after age 50, there would
be no impact on the screening recommendation. If the relative was diagnosed before age 50, the woman should begin
screening before the age of 40.
4. How many views are obtained for a routine mammogram?
Four views are obtained for a routine mammogram. Craniocaudal (CC) and medio-lateral oblique (MLO) views of each
breast are obtained. In some patients, more than four images may be needed to visualize all of the breast parenchyma
adequately.
5. Which view visualizes the most breast tissue?
MLO view visualizes the most breast tissue.
6. Which portion of the breast is better visualized on CC view than on MLO view?
The medial breast is better visualized on CC view.
7. How should a film screen mammogram be hung?
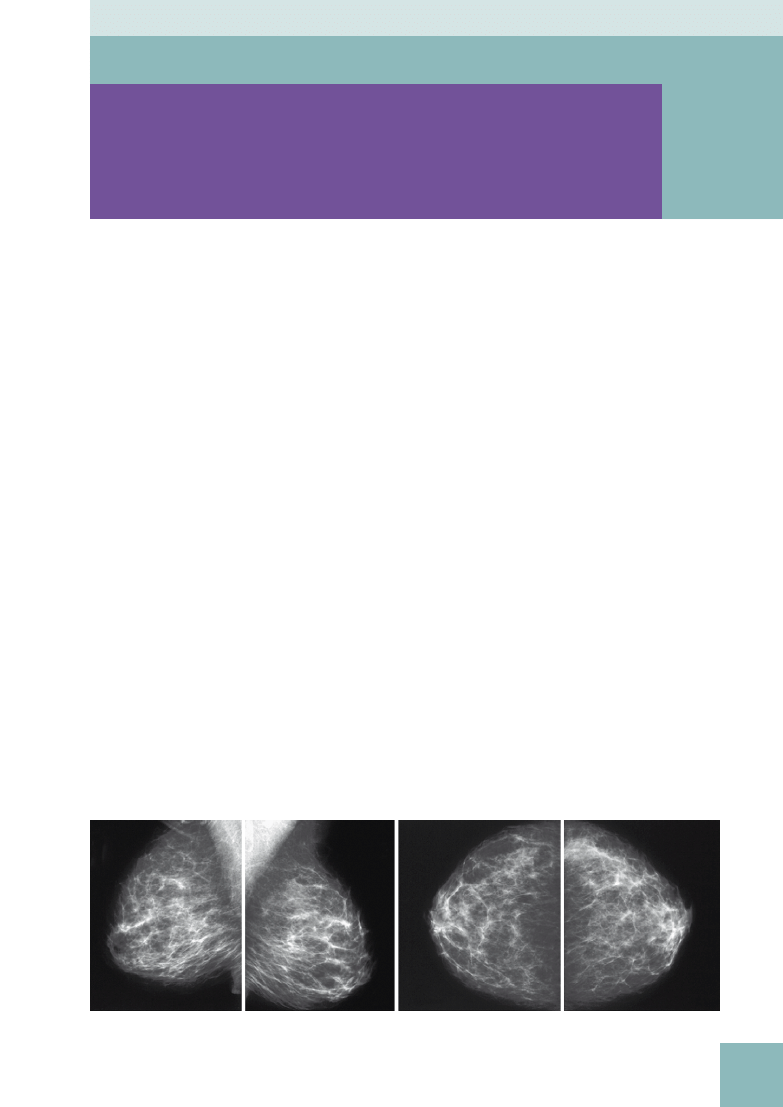
CC views are hung next to one another, and MLO views are hung adjacent to each other (
). The films are hung with
the labels in the upper corner. On CC views, the labels are placed adjacent to the lateral breast. On MLO views, the labels
are placed adjacent to the superior breast. The comparison films are hung in the same manner above the current study.
A
B
C
D
Figure 5-1.
Screening mammogram hung for viewing.
A-D, From the viewer’s left, the images are the left MLO view (A), the right MLO view
(
B), the left CC view (C), and the right CC view (D). The comparison films are typically hung above the current study.
30
Screening MaMMography
8. How old should the comparison films be?
If the patient has multiple sets of prior films, we like to compare with the studies that are 2 years old.
Early changes from breast cancer can be subtle, and the changes are easier to detect over the 2-year interval.
9. What if there are comparison films elsewhere? Do we need to get them?
If the mammogram results are considered to be negative, no. Studies have shown that it is not cost-effective and does
not improve patient care to obtain comparison films for studies with normal results. If there is an abnormal finding,
an attempt should be made to get the prior studies from the outside institution. If the prior films cannot be obtained,
the patient should be recalled for additional evaluation.
10. What is the incidence of screening-detected breast cancer?
In a population that has never been screened, the incidence is about 6 to 10/1000. In a population that is routinely
screened, the incidence decreases to about 2 to 4/1000.
11. What is the reported sensitivity of screening mammography?
False-negative interpretation (mammograms that are interpreted as negative, but a cancer is present) is usually 15%
to 20%. The sensitivity decreases as the glandularity of the breast tissue increases. The sensitivity of mammography in
women with dense breast tissue is about 50%. In fatty breast tissue, the sensitivity of mammography is quite high, in
the high 90s.
12. What is the difference between a screening mammogram and a diagnostic
mammogram?
A screening mammogram is performed on asymptomatic patients as part of routine annual surveillance. A diagnostic
mammogram is performed when the patient has a history of breast cancer or presents with a breast-related complaint
or symptom.
13. Are there other types of breast cancer screening modalities? Which modalities are
used in everyday clinical practice?
Digital mammography is similar to film screen mammography, but the images are acquired in a digital form. After
acquisition, image processing is possible with the digitized images. The images can be printed and viewed as hard
copies similar to film screen mammography or reviewed on a computer monitor. The soft copy images can be
manipulated to enhance the image interpretation. The contrast can be changed, and the images can be magnified.
Although film screen mammography has better spatial resolution than digital mammography, digital mammography has
better contrast resolution than film screen images.
Screening breast ultrasound (US) consists of US examination of both breasts in asymptomatic women. The largest
prospective study to date was sponsored by American College of Radiology Imaging Network (ACRIN) 6666. The goal
of the prospective, multicenter trial was to compare the diagnostic yield of screening breast mammography plus US
versus mammography alone in high-risk women. Although the added screening US examinations found additional breast
cancers, there was a high false-positive rate. That is, many biopsies were recommended for benign findings, resulting
in a low positive predictive value.
Screening magnetic resonance imaging (MRI) is not likely to be used in everyday clinical practice because of the
lack of availability, high cost, and variable specificity leading to many false-positive interpretations. MRI screening
has shown to be promising in very high-risk patients, however. The American Cancer Society guidelines recommend
MRI screening in women with a greater than 20% to 25% lifetime risk for breast cancer. The screening groups
include women who are carriers of the BRCA mutations or untested women with a first-degree relative who is a
known carrier; women with a history of mantle radiation before age 30; and women with Li-Fraumeni, Cowden,
and Bannayan-Riley-Ruvalcaba syndromes. MRI screening cancer yield in high-risk patients has consistently been
2% to 3%.
Key Points: Screening Mammography
1. Annual screening mammography should begin at age 40.
2. Mammography is still the best screening test to detect subclinical breast cancer.
3. The sensitivity of mammography is in the range of 85%.
4. Most breast cancers occur in women with no family history of the disease.

Screening MaMMography
31
breaSt iMaging
14. Is digital mammography better than film screen mammography in detecting breast
cancer?
The largest prospective multicenter trial comparing digital mammography with film screen mammography is the Digital
Mammographic Imaging Screening Trial (DMIST) sponsored by ACRIN. The study recruited more than 49,000 women.
Overall, in the general population, the accuracy of digital mammography was similar to film screen mammography.
The accuracy of digital mammography was higher than film screen mammography, however, in certain subpopulations,
including women younger than age 50 years, women with heterogeneously or extremely dense breasts, and
premenopausal or perimenopausal women.
15. Is there an age at which breast cancer screening should stop?
In the United States, there are no guidelines for when screening should stop. In other countries, the recommended age
at which screening should stop ranges from 59 to 74 years.
16. What is batch reading of screening mammograms?
Batch reading is the most efficient way to read screening mammograms. The women are imaged. The films are hung on
a multiviewer or loaded onto a workstation, and all the studies are batch read by the radiologist, typically the following
day. This approach increases efficiency. The results are mailed to the patients.
17. What are some risk factors for developing breast cancer?
Perhaps the greatest risk factor is being a female. Men get breast cancer, but male breast cancer accounts
for less than 1% of all breast cancers diagnosed annually. Other risk factors include being genetic mutation
carrier (BRCA1 and BRCA2) status, history of mantle radiation, first-degree relative with breast cancer, personal
history of breast cancer, history of atypia such as atypical ductal hyperplasia and lobular carcinoma in situ
on biopsy, early menarche, late menopause, nulliparous status, late first-term pregnancy (>30 years old), and
advancing age.
18. True or false: Most breast cancers occur in women with a family history of breast
cancer.
False. About 20% of breast cancers occur in patients with a positive family history. About 75% to 80% of breast cancers
are sporadic.
19. True or false: With increased use of breast cancer screening, the incidence of breast
cancer has been declining
False. The incidence of breast cancer has been steadily increasing since the 1980s. This increase has been partly
attributed to early detection owing to increased breast cancer screening with mammography during this time
period. The incidence leveled off in the 1990s and began to decline starting about 1999 according to the National
Cancer Institute Surveillance Epidemiology and End Results (SEER) data. The reason for this decreased incidence
is unclear. According to the SEER data, it was estimated that 182,460 women would be diagnosed with breast
cancer in 2008 and 40,480 women would die of cancer from breast cancer (National Cancer Institute Surveillance
Epidemiology and End Results [SEER], Table I-1. Available at:
http://seer.cancer.gov/csr/1975_2005/results_
20. It has been said that one in eight women has a risk of developing breast
cancer. Does a 40-year-old woman have the same risk as an 80-year-old
woman?
No. The one-in-eight risk of developing breast cancer refers to an overall lifetime risk if the woman lives to age 85.
Given identical circumstances, a 40-year-old woman does not have the same risk as an 80-year-old woman. The
National Cancer Institute gives an overall risk based on the age of the patient (
). The incidence peaks
between ages 45 and 74, then decreases.
21. What are BRCA1 and BRCA2? What is the risk of getting breast cancer by age 70 in a
patient who is a BRCA1 gene carrier?
BRCA1 and BRCA2 are genetic mutations. Both genes have autosomal dominant expression and may be inherited
from the maternal or the paternal side. Women who carry a BRCA1 or BRCA2 gene have increased risk of developing
cancers, with breast and ovarian cancers being the two most common types. In regards to breast cancer, the women
who have the genetic mutation tend to develop breast cancer at an earlier age than the general population and
are more likely to develop bilateral breast cancer. Men with BRCA1 and BRCA2 mutations are at increased risk of
developing prostate cancer. Men who carry the BRCA1 mutation are also at increased risk for breast cancer. Genetic
testing for BRCA1 and BRCA2 is available. In a woman who is a BRCA1 carrier, the risk of developing breast cancer
can be 85%.
32
Screening MaMMography
22. How much radiation does a woman
receive from a routine screening
mammogram?
The amount of radiation is 0.2 rad (2 mGy) for two
views of one breast. Although there is radiation
exposure, the amount is considered small and is
believed to be outweighed by the benefits of early
detection from screening.
23. How is a patient who has undergone
screening informed of her test
results?
Usually, a letter is sent in the mail. There are two
potential results. The patient may be informed
that her mammogram was normal. Alternatively,
the patient may be informed of the need for
additional evaluation, which may be in the form of
additional imaging or obtaining the patient’s prior
mammograms for comparison.
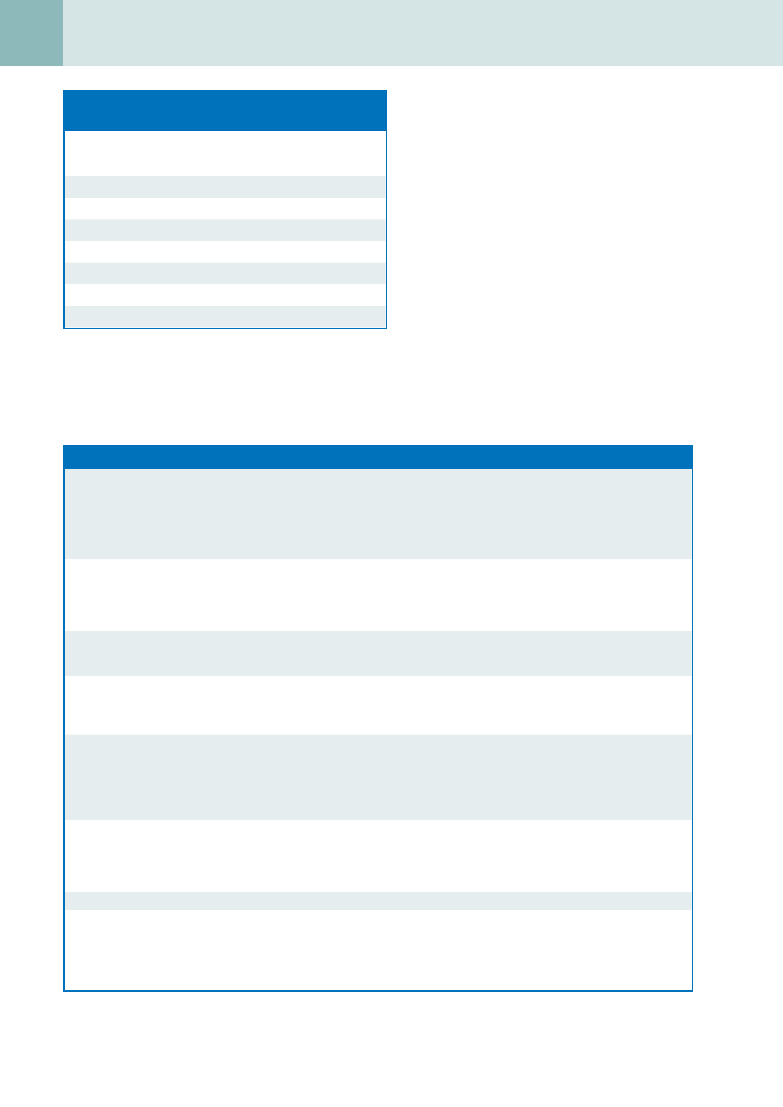
Table 5-2. Definitions
Annual percent change (APC)
Average annual percent change over several years. APC is used to
measure trends or the change in rates over time. For information
on how this is calculated, go to “Trend Algorithms” in the
SEER*Stat Help system. The calculation involves fitting a straight
line to the natural logarithm of the data when it is displayed by
calendar year
Joinpoint analyses
Statistical model for characterizing cancer trends that uses statistical
criteria to determine how many times and when the trends in
incidence or mortality rates have changed. The results of joinpoint
are given as calendar-year ranges and APC in the rates over each
period
Survival rate
Survival rate examines how long after diagnosis people live. Cancer
survival is measured in many different ways depending on the
intended purpose
Relative survival rate
Measure of net survival that is calculated by comparing observed
(overall) survival with expected survival from a comparable set of
individuals who do not have cancer to measure the excess mortality
that is associated with a cancer diagnosis
Stage distribution
Stage provides a measure of disease progression, detailing the degree
to which the cancer has advanced. Two methods commonly used
to determine stage are AJCC and SEER historic. The AJCC method
(see Collaborative Staging Method) is more commonly used in clinical
settings, whereas SEER has standardized and simplified staging to
ensure consistent definitions over time
Lifetime risk
Probability of developing cancer in the course of one’s life span. Lifetime
risk may also be discussed in terms of the probability of developing
or dying from cancer. Based on cancer rates from 2003-2005, it was
estimated that men had about a 44% chance of developing cancer in
their lifetimes, whereas women had about a 37% chance
Probability of developing cancer
Chance that an individual will develop cancer in his or her lifetime
Prevalence
Number of people who have received a diagnosis of cancer during a
defined time period, and who are alive on the last day of that period.
Most prevalence data in SEER are for limited duration because
information on cases diagnosed before 1973 is not generally
available
AJCC, American Joint Committee on Cancer; SEER, Surveillance, Epidemiology, and End Results.
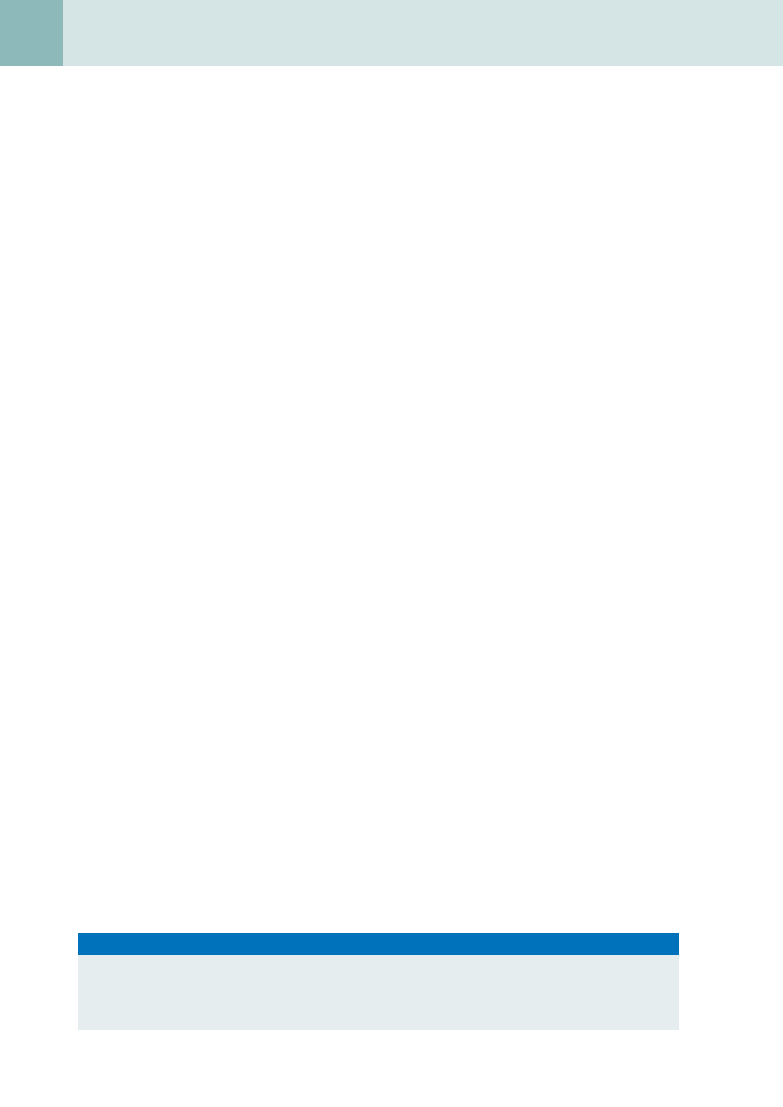
Table 5-1. Age-Related Incidence of Breast
Cancer
AGE
INCIDENCE (%)
<20
0
20-34
1.9
35-44
10.6
45-54
22.4
55-64
23.3
65-74
19.8
75-84
16.5
>85
5.5
Data from National Cancer Institute Surveillance, Epidemiology, and
End Results Program 2008 website. Most of the data can be found in
Ries LAG, Melbert D, Krapcho M, et al (eds): SEER Cancer Statistics
Review, 1975-2005. Bethesda, MD, National Cancer Institute, 2007.
Available at:
http://seer.cancer.gov/csr/1975_2005/
.

Screening MaMMography
33
breaSt iMaging
24. What happens if additional imaging evaluation is needed based on findings on the
screening mammogram?
The patient is sent a letter advising her that additional evaluation is needed. In addition, at our institution, a coordinator
calls the patient to schedule the necessary appointment.
25. What is the call-back rate? What should the call-back rate be for a radiologist?
The call-back rate is the percentage of the screening cases that the radiologist recommends for additional imaging
evaluations. The rate should be 10% or less.
26. Is the breast a modified skin gland, fatty tissue, muscle, or lymphatic structure?
The breast tissue is derived from ectodermal origin and is a modified skin gland.
27. How does accessory breast tissue form? Where is it most commonly located?
Breast tissue development begins at about 6 weeks of gestation and originates from ectodermal elements. The “milk
line” extends from the groin region to the axillary region. Most of the potential breast tissue atrophies except in the
fourth intercostal region, where “normal” mammary tissue eventually develops. The lack of appropriate regression
results in accessory breasts anywhere along the “milk line.”
B
iBliography
[1] W.A. Berg, J.D. Blume, J.B. Cormack, et al., ACRIN 6666 Investigators: Combined screening with ultrasound and mammography vs
mammography alone in women at elevated risk of breast cancer, JAMA 299 (2008) 2151–2163.
[2] D.B. Kopans, Breast Imaging, third ed., Lippincott Williams & Wilkins, Philadelphia, 2007.
[3] C.D. Lehman, C. Isaacs, M.D. Schnall, et al., Cancer yield of mammography, MR, and US in high-risk women: prospective multi-institution
breast cancer screening study, Radiology 244 (2007) 381–388.
[4] E.D. Pisano, C. Gatsonis, E. Hendrick, et al., Diagnostic performance of digital versus film mammography for breast-cancer screening,
N. Engl. J. Med. 353 (2005) 1773–1783.
[5] D. Saslow, C. Boetes, W. Burke, et al., American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography,
CA Cancer J. Clin. 57 (2007) 75–89.
[6] S. Shapiro, E.A. Coleman, M. Broeders, et al., Breast cancer screening programs in 22 countries: current policies, administration and
guidelines, Int. J. Epidemiol. 27 (1998) 735–742.
Document Outline
- Screening Mammography
- What is a screening mammogram?
- When should an average woman start getting mammograms?
- Are there instances when screening should start earlier than 40?
- How many views are obtained for a routine mammogram?
- Which view visualizes the most breast tissue?
- Which portion of the breast is better visualized on CC view than on MLO view?
- How should a film screen mammogram be hung?
- How old should the comparison films be?
- What if there are comparison films elsewhere? Do we need to get them?
- What is the incidence of screening-detected breast cancer?
- What is the reported sensitivity of screening mammography?
- What is the difference between a screening mammogram and a diagnostic mammogram?
- Are there other types of breast cancer screening modalities? Which modalities are used in everyday clinical practice?
- Is digital mammography better than film screen mammography in detecting breast cancer?
- Is there an age at which breast cancer screening should stop?
- What is batch reading of screening mammograms?
- What are some risk factors for developing breast cancer?
- True or false: Most breast cancers occur in women with a family history of breast cancer.
- True or false: With increased use of breast cancer screening, the incidence of breast cancer has been declining
- It has been said that one in eight women has a risk of developing breast cancer. Does a 40-year-old woman have the s
- What are BRCA1 and BRCA2? What is the risk of getting breast cancer by age 70 in a patient who is a BRCA1 gene ...
- How much radiation does a woman receive from a routine screening mammogram?
- How is a patient who has undergone screening informed of her test results?
- What happens if additional imaging evaluation is needed based on findings on the screening mammogram?
- What is the call-back rate? What should the call-back rate be for a radiologist?
- Is the breast a modified skin gland, fatty tissue, muscle, or lymphatic structure?
- How does accessory breast tissue form? Where is it most commonly located?
- Bibliography
Wyszukiwarka
Podobne podstrony:
C20090551288 B9780323067942000420 main
C20090551288 B9780323067942000407 main
C20090551288 B9780323067942000225 main
C20090551288 B9780323067942000432 main
C20090551288 B9780323067942000547 main
C20090551288 B9780323067942000298 main
C20090551288 B9780323067942000316 main
C20090551288 B9780323067942000286 main
C20090551288 B9780323067942000560 main
C20090551288 B9780323067942000341 main
C20090551288 B9780323067942000390 main
C20090551288 B9780323067942000766 main
C20090551288 B9780323067942000754 main
C20090551288 B9780323067942000122 main
C20090551288 B9780323067942000626 main
więcej podobnych podstron