Nursing Management of the
Pregnancy at Risk:
Preexisting Conditions
20
chapter
Key
TERMS
acquired immunodeficiency
syndrome (AIDS)
adolescence
anemia
fetal alcohol spectrum
disorder
gestational diabetes mellitus
glycosylated hemoglobin
(HbA1C) level
human immunodeficiency
virus (HIV)
impaired fasting glucose
impaired glucose tolerance
neonatal abstinence
syndrome
perinatal drug abuse
pica
teratogen
Type 1 diabetes
Type 2 diabetes
Learning
OBJECTIVES
After studying the chapter content, the student should be able to:
1. Define the key terms.
2. Identify at least two preexisting conditions that can affect a pregnancy.
3. Analyze the physiologic and psychological impact of a preexisting condition on a
pregnancy.
4. Describe the nursing management for a pregnant woman with diabetes.
5. Explain the effects, treatment, and nursing management of heart disease and
respiratory conditions during pregnancy.
6. Outline appropriate assessment and interventions for the client experiencing
violence during her pregnancy.
7. Differentiate among the types of anemia in terms of prevention and management.
8. Identify the infections that can jeopardize a pregnancy.
9. Describe the nurse’s role in the prevention and management of adolescent pregnancy.
10. Discuss the importance of continued prenatal care for high-risk women.
11. Identify the effects, treatment, and nursing management of HIV/AIDS and
substance abuse during pregnancy.
12. Delineate the role of the nurse in assessing, managing care, and referring high-risk
clients to appropriate community services and resources.
Key
Learning
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 543
regnancy and childbirth are excit-
ing yet complex facets within the continuum of women’s
health. Ideally the pregnant woman is free of any pre-
existing conditions, but in reality many women enter
pregnancy with a multitude of medical or psychosocial
issues that can have a negative impact on the outcome.
Most pregnant women express the wish, “I hope my
baby is born healthy.” Nurses can be instrumental in help-
ing this to become a reality by educating women before
they become pregnant. In addition, medical conditions
such as diabetes, cardiac and respiratory disorders, ane-
mias, and specific infections can frequently be controlled
so that their impact on pregnancy is minimized through
close prenatal management. Pregnancy-prevention strate-
gies are helpful when counseling teenagers. Meeting the
developmental needs of pregnant adolescents is challeng-
ing for many healthcare providers. Finally, lifestyle choices
can place many women at risk during pregnancy and
nurses need to remain nonjudgmental in working with
these special populations. Lifestyle choices such as use of
alcohol, nicotine, and illicit substances during pregnancy
are addressed in a National Health goal.
Chapter 19 described pregnancy-related conditions
that place the woman at risk. This chapter addresses the
most common conditions that are present before preg-
nancy that can have a negative effect on the pregnancy
and outlines appropriate nursing assessments and inter-
ventions for each. The unique skills of nurses, in con-
junction with the other members of the healthcare team,
can increase the potential for a positive outcome in many
high-risk pregnancies.
Diabetes Mellitus
Diabetes mellitus is a chronic disease characterized by a
relative lack of insulin or absence of the hormone, which
is necessary for glucose metabolism. The prevalence of
diabetes in the United States is increasing at an alarming
rate, already reaching epidemic proportions. A contribut-
ing factor to these increasing rates is the incidence of obe-
sity. It is a common endocrine disorder affecting 1% to
14% of all pregnancies (American Diabetes Association
[ADA], 2004).
Diabetes in pregnancy is categorized into two groups:
preexisting diabetes, which includes women with type 1 or
type 2 disease, and gestational diabetes, which develops in
women during pregnancy (Kendrick, 2004). Pregestational
diabetes complicates 0.2% to 0.3% of all pregnancies and
affects up to 14,000 women annually. Gestational diabetes
occurs in approximately 7% of all pregnant women and
complicates more than 200,000 pregnancies annually in
the United States. This type accounts for 90% of diabetic
pregnancies (ADA, 2004).
Before the discovery of insulin in 1922, most female
diabetics were infertile or experienced spontaneous abor-
tion (Kendrick, 2004). Over the past several decades,
great strides have been made in improving the outcomes
of pregnant women with diabetes, but this chronic meta-
bolic disorder remains a high-risk condition during preg-
nancy. A favorable outcome requires commitment on the
woman’s part to comply with frequent prenatal visits,
dietary restrictions, self-monitoring of blood glucose lev-
els, frequent laboratory tests, intensive fetal surveillance,
and perhaps hospitalization.
Classification of Diabetes
Some form of diabetes mellitus complicates up to 14% of
all pregnancies. The classification system commonly used
is based on disease etiology (Expert Committee, 2003).
It includes four groups (Box 20-1). The vast majority of
women (88%) have gestational diabetes; the remainder
have pregestational diabetes (Samson & Ferguson, 2004).
Attempting to classify women as having pregesta-
tional or gestational diabetes is problematic because many
women are not aware they have a problem before their
pregnancy. Many women with type 2 diabetes have gone
wow
544
As the sun sets each day, nurses should make sure they have done
something for others, and be understanding even under the
most difficult of conditions.
P
HEALTHY PEOPLE
2010
National Health Goals Related to Substance Exposure
Objective
Significance
Increase abstinence from
alcohol, cigarettes, and
illicit drugs among
pregnant women
Increase in reported
abstinence in the
past month from
substances by pregnant
women
Alcohol from a baseline of
86% to 94%
Binge drinking from a
baseline of 99% to 100%
Cigarette smoking from a
baseline of 87% to 99%
Illicit drugs from a baseline
of 98% to 100%
USDHHS, 2000.
Will help to focus
attention on measures
for reducing substance
exposure and use,
thereby minimizing the
effects of these
substances on the
fetus and newborn
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 544

undiagnosed; only when they are screened at a prenatal
visit is the diabetes discovered. Although the classifications
seem clear-cut, many women have glucose intolerance
long before they become pregnant, but it has not been
diagnosed. Preconceptual counseling might help to iden-
tify women who have not been diagnosed so that measures
can be taken to achieve glucose control, thereby helping to
prevent congenital anomalies during the embryonic stage
of development.
Effects of Diabetes on Pregnancy
Pregnancy produces profound metabolic alterations that
are necessary to support the growth and development of the
fetus. Maternal metabolism is directed toward supply-
ing adequate nutrition for the fetus. In pregnancy, placen-
tal hormones cause insulin resistance at a level that tends to
parallel the growth of the fetoplacental unit. As the placenta
grows, more placental hormones are secreted. Human pla-
cental lactogen (hPL) and growth hormone (somatotropin)
increase in direct correlation with the growth of placental
tissue, rising throughout the last 20 weeks of pregnancy and
causing insulin resistance. Subsequently, insulin secre-
tion increases to overcome the resistance of these two hor-
mones. In the nondiabetic pregnant woman, the pancreas
can respond to the demands for increased insulin produc-
tion to maintain normal glucose levels throughout the preg-
nancy (Ryan, 2003). However, the woman with glucose
intolerance or diabetes during pregnancy cannot cope with
changes in metabolism resulting from insufficient insulin to
meet the needs during gestation.
Over the course of pregnancy, insulin resistance
changes. It peaks in the last trimester to provide more nutri-
ents to the fetus. The insulin resistance typically results in
postprandial hyperglycemia, although some women also
have an elevated fasting blood glucose level (Turok et al.,
2003). With this increased demand on the pancreas in late
pregnancy, women with diabetes or glucose intolerance
cannot accommodate the increased insulin demand.
The pregnancy of a woman with diabetes carries risk
factors such as perinatal mortality and congenital anom-
alies. Tight metabolic control reduces this risk, but still
many problems remain for her and her fetus. Major effects
of hyperglycemia on a pregnancy include:
•
Hydramnios due to fetal diuresis caused by hyper-
glycemia
•
Gestational hypertension due to an unknown etiology
•
Ketoacidosis due to uncontrolled hyperglycemia
•
Preterm labor secondary to premature membrane
rupture
•
Cord prolapse secondary to hydramnios and abnormal
fetal presentation
•
Stillbirth in pregnancies complicated by ketoacidosis
and poor glucose control
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
545
Consider
THIS!
Scott and I had been busy all day setting up the new crib
and nursery, and we finally sat down to rest. I was due
any day, and we had been putting this off until we had a
long weekend to complete the task. I was excited to think
about all the frilly pinks that decorated her room. I was
sure that my new daughter would love it as much as I loved
her already. A few days later I barely noticed any fetal
movement, but I thought that she must be as tired as
I was by this point.
That night I went into labor and kept looking at the
worried faces of the nurses and the midwife in atten-
dance. I had been diagnosed with gestational diabetes a
few months ago and had tried to follow the instructions
regarding diet and exercise, but old habits are hard to
change when you are 38 years old. I was finally told after
a short time in the labor unit that they couldn’t pick up a
fetal heartbeat and an ultrasound was to be done—still no
heartbeat was detected. Scott and I were finally told that
our daughter was a stillborn. All I could think about was
that she would never get to see all the pink colors in the
nursery. . . . .
Consider
• Type 1 diabetes—absolute insulin deficiency (due to
an autoimmune process); usually appears before the
age of 30 years; approximately 10% of those diagnosed
have type 1 diabetes (Wallerstedt & Clokey, 2004)
• Type 2 diabetes—insulin resistance or deficiency
(related to obesity, sedentary lifestyle); diagnosed
primarily in adults older than 30 years of age, but is
now being seen in children; accounts for 90% of all
diagnosed cases.
• Impaired fasting glucose and impaired glucose
tolerance—characterized by hyperglycemia at a level
lower than what qualifies as a diagnosis of diabetes;
symptoms of diabetes are absent; newborns are at risk
for being large for gestational age (LGA) (Wallerstedt
& Clokey, 2004).
• Gestational diabetes mellitus—glucose intolerance
due to pregnancy
BOX 20-1
CLASSIFICATION OF DIABETES MELLITUS
Thoughts:
This woman is typical of a gestational
diabetic in that she was older and found it difficult
to change her old dietary habits. Perhaps her blood
glucose levels had been out of control throughout
the pregnancy, or maybe just recently. It is difficult
to pinpoint the how and whys of such a tragedy, but
it remains a reality even today. What went wrong?
How can you help this family to cope with this loss?
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 545
•
Hypoglycemia as glucose is diverted to the fetus (occur-
ring in first trimester)
•
Urinary tract infections resulting from excess glucose in
the urine (glucosuria), which promotes bacterial growth
•
Chronic monilial vaginitis due to glucosuria, which pro-
motes growth of yeast
•
Difficult labor, cesarean birth, postpartum hemorrhage
secondary to an overdistended uterus to accommodate
a macrosomic infant
In addition, fetal-neonatal risks include:
•
Congenital anomaly due to hyperglycemia in the first
trimester (cardiac problems, neural tube defects, skele-
tal deformities, and genitourinary problems)
•
Macrosomia resulting from hyperinsulinemia stimulated
by fetal hyperglycemia
•
Birth trauma due to increased size of fetus, which com-
plicates the birthing process (shoulder dystocia)
•
Preterm birth secondary to hydramnios and an aging
placenta, which places the fetus in jeopardy if the preg-
nancy continues
•
Perinatal death due to poor placental perfusion and
hypoxia
•
Fetal asphyxia secondary to fetal hyperglycemia and
hyperinsulinemia
•
Respiratory distress syndrome (RDS) resulting from poor
surfactant production secondary to hyperinsulinemia
inhibiting the production of phospholipids, which make
up surfactant
•
Polycythemia due to excessive red blood cell (RBC)
production in response to hypoxia
•
Intrauterine growth restriction (IUGR) secondary to
maternal vascular impairment and decreased placen-
tal perfusion, which restricts growth
•
Hyperbilirubinemia due to excessive RBC breakdown
from hypoxia and an immature liver unable to break
down bilirubin
•
Neonatal hypoglycemia resulting from ongoing hyper-
insulinemia after the placenta is removed
•
Subsequent childhood obesity and carbohydrate intol-
erance (Messner, 2004)
Pregestational Diabetes
Pregestational diabetes exists when an alteration in carbo-
hydrate metabolism is identified before conception. The
client’s diabetes may be long standing or of short dura-
tion. As with most chronic disorders, a stable disease
state before conception will produce the best pregnancy
outcome. Excellent control of blood glucose, as evidenced
by normal fasting blood glucose levels and a
glyco-
sylated hemoglobin (HbA1C) level
(an average mea-
surement of the glucose levels over the past 100 to
120 days), is a key factor to address in preconception
counseling. A glycosylated hemoglobin level of 7% to
10% indicates good control; a value of more than 15%
indicates that the diabetes is out of control and war-
rants notification of the healthcare provider (Samson &
Ferguson, 2004).
Infants born to diabetic mothers are at risk for con-
genital malformations. The most common ones associ-
ated with diabetes occur in the renal, cardiac, skeletal,
and central nervous systems. Since these defects occur by
the eighth week of gestation, the need for preconception
counseling is critical. The rate of congenital anomalies in
women with pregestational diabetes can be reduced if
excellent glycemic control is achieved at the time of con-
ception (Feig & Palda, 2003). This information needs to
be stressed with all diabetic women contemplating a
pregnancy (Nursing Care Plan 20-1).
Treatment
In addition to preconception counseling, the woman needs
to be evaluated for complications of diabetes. This evalu-
ation should be part of baseline screening and continuing
assessment during pregnancy. These women need com-
prehensive prenatal care. The primary goals of care are to
maintain glycemic control and minimize the risks of the
disease on the fetus. Key aspects of treatment include
dietary management, insulin regimens, and close maternal
and fetal surveillance.
Dietary Management
Dietary management may be sufficient to control the
woman’s glucose levels and ideally is handled by a nutri-
tionist. Nutritional recommendations include:
•
Adhere to the same nutrient requirements and recom-
mendations for weight gain as the nondiabetic woman.
•
Avoid weight loss and dieting during pregnancy.
•
Ensure food intake is adequate to prevent ketone for-
mation and promote weight gain.
•
Eat three meals a day plus three snacks to promote
glycemic control.
•
Include complex carbohydrates, fiber, and limited fat
and sugar in the diet.
•
Continue dietary consultation throughout pregnancy
(Dudek, 2006).
Insulin Regimens
At present, insulin remains the medication of choice
for glycemic control in pregnant and lactating women
with any type of diabetes (Turok et al., 2003). Insulin is
required when diet alone is ineffective in maintaining nor-
mal glucose control. Oral hypoglycemic agents are not
usually prescribed to control blood glucose levels because
of their potential teratogenic effect. However, they may be
an option in the future after additional research has been
completed. Glyburide is one alternative to insulin that
does not cross the placenta. Diabetes can be controlled
in many women with this agent, and it has a low risk
of producing maternal hypoglycemia (Barbour, 2003).
546
Unit 7
CHILDBEARING AT RISK
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 546
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
547
Outcome identification and
evaluation
Client will demonstrate increased knowledge of type
1 diabetes and effects on pregnancy
as evi-
denced by proper techniques for blood glucose
monitoring and insulin administration, ability to
modify insulin doses and dietary intake to achieve
control, and verbalization of need for glycemic
control prior to pregnancy, with blood glucose
levels remaining within normal range.
Interventions with
rationales
Assess client’s knowledge of diabetes and pregnancy.
Review the underlying problems associated with dia-
betes and how pregnancy affects glucose control
to provide client with a firm knowledge base for
decision making.
Review signs and symptoms of hypoglycemia and
hyperglycemia and prevention and manage-
ment measures
to ensure client can deal with
them should they occur.
Provide written materials describing diabetes and
care needed for control
to provide opportunity for
client’s review and promote retention of learning.
Observe client administering insulin and self-glucose
testing for technique and offer suggestions for
improvement if needed
to ensure adequate self-
care ability.
Discuss proper foot care
to prevent future infections.
Teach home treatment for symptomatic hypo-
glycemia
to minimize risk to client and fetus.
Outline acute and chronic diabetic complications
to
reinforce the importance of glucose control.
Discuss use of contraceptives until blood glucose lev-
els can be optimized before conception occurs
to
promote best possible health status before con-
ception.
Discuss the rationale for good glucose control and
the importance of achieving excellent glycemic
control before pregnancy
to promote a positive
pregnancy outcome.
Review self-care practices—blood glucose monitor-
ing and frequency of testing; insulin administra-
tion; adjustment of insulin dosages based on
blood glucose levels—
to foster independence in
self-care and feelings of control over the situation.
Donna, a 30-year-old type 1 diabetic, presents to the maternity clinic for preconception
care. She has been a diabetic for 8 years and takes insulin twice daily by injection. She does
blood glucose self-monitoring four times daily. She reports that her disease is fairly well
controlled but worries about how her diabetes will affect a pregnancy. She is concerned
about what changes she will have to make in her regimen and what the pregnancy outcome
will be. She reports that she recently had a foot infection and needed to go to the emer-
gency room because it led to an episode of ketoacidosis. She states that her last glycosy-
lated hemoglobin A1c test results were abnormal.
Nursing Care Plan
Nursing Diagnosis: Deficient knowledge related to type 1 diabetes, blood glucose control, and
effects of condition on pregnancy
(continued )
Nursing Care Plan
20-1
Overview of the Pregnant Woman with Type 1 Diabetes
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 547
Glyburide is not yet approved by the U.S. Food and Drug
Administration (FDA) for the treatment of gestational
diabetes. Studies of the use of these agents during preg-
nancy are in their infancy, but they may hold great
promise for reducing the long-term metabolic effects on
women and their offspring (Kendrick, 2004).
Insulin requirements may drop slightly in the first
trimester before increasing significantly during the latter
half of the pregnancy. Changes in diet and activity level add
to the changes in insulin dosages throughout pregnancy.
Insulin regimens vary, and controversy remains over
the best strategy for insulin delivery in pregnancy. Many
healthcare providers use a split-dose therapy with morn-
ing and evening doses. Others advocate the use of an
insulin pump to deliver a continuous subcutaneous insu-
lin infusion. Regardless of which protocol is used, fre-
quent blood glucose measurements are necessary, and
the insulin dosage is adjusted on the basis of daily glu-
cose levels.
Maternal and Fetal Surveillance
Frequent laboratory studies are done during pregnancy
to monitor the woman’s diabetic status. These studies
might include:
548
Unit 7
CHILDBEARING AT RISK
Outcome identification and
evaluation
Interventions with
rationales
Refer client for dietary counseling
to ensure optimal
diet for glycemic control.
Outline obstetric management and fetal surveillance
needed for pregnancy
to provide client with infor-
mation on what to expect.
Discuss strategies for maintaining optimal glycemic
control during pregnancy
to minimize risks to client
and fetus.
Overview of the Pregnant Woman with Type 1 Diabetes
(continued)
Nursing Diagnosis: Anxiety related to future pregnancy and its outcome secondary to
underlying diabetes
Client will express her feelings related to her diabetes
and pregnancy
as evidenced by statements of
feeling better about her pre-existing condition
and pregnancy outlook, and statements of under-
standing related to future childbearing by linking
good glucose control with positive outcomes for
both herself and offspring.
Review the need for a physical examination
to eval-
uate for any effects of diabetes on the client’s
health status.
Explain the rationale for assessing client’s blood pres-
sure, vision, and peripheral pulses at each visit
to
provide information related to possible effects of
diabetes on health status.
Identify any alterations in present diabetic
condition that need intervention
to aid in
minimizing risks that may potentiate client’s
anxiety level.
Review potential effects of diabetes on pregnancy
to promote client understanding of risks and ways
to control or minimize them.
Encourage active participation in decision making
and planning pregnancy
to promote feelings of
control over the situation and foster self-confi-
dence.
Provide positive reinforcement for healthy behaviors
and actions
to foster continued use and
enhancement of self-esteem.
Discuss feelings about future childbearing and man-
aging pregnancy
to help reduce anxiety related
to uncertainties.
Encourage client to ask questions or voice con-
cerns
to help decrease anxiety related to the
unknown.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 548
•
Fingerstick blood glucose levels at every prenatal visit
to evaluate the accuracy of the self-monitoring docu-
mentation brought in by the woman
•
Urine check for protein (may indicate the need for fur-
ther evaluation for preeclampsia) and for nitrates and
leukocyte esterase (may indicate a urinary tract infection)
•
Urine check for ketones (may indicate the need for eval-
uation of eating habits)
•
Kidney function evaluation every trimester for creati-
nine clearance and protein levels
•
Eye examination in the first trimester to evaluate the
retina for vascular changes
•
HbA1c every 4 to 6 weeks to monitor glucose trends
(Gilbert & Harmon, 2003)
Fetal surveillance is essential during the pregnancy to
evaluate the fetal well-being and assist in determining the
best time for birth. The evaluation may include:
•
Ultrasound to provide information about fetal growth,
activity, and amniotic fluid volume and to validate ges-
tational age
•
Alpha-fetoprotein levels to detect an open neural tube
or ventral wall defects of omphalocele or gastroschisis
•
Fetal echocardiogram to rule out cardiac anomalies
•
Daily fetal movements to monitor fetal well-being
•
Biophysical profile to monitor fetal well-being and utero-
placental profusion
•
Nonstress tests weekly after 28 weeks to determine fetal
well-being
•
Amniocentesis to determine the lecithin/sphingomyelin
(L/S) ratio and the presence of phosphatidyl glycerol
(PG) to evaluate whether the fetal lung is mature enough
for birth (Gilbert & Harmon, 2003)
Gestational Diabetes
One of the biggest challenges nurses and other healthcare
providers face is the growing number of women develop-
ing gestational diabetes as the obesity epidemic escalates.
The increasing development of gestational diabetes in the
mother and glucose intolerance in the offspring set the
stage for a perpetuating cycle that must be addressed with
effective primary prevention strategies and more effective
antepartum interventions (Barbour, 2003).
Gestational diabetes mellitus
is defined as glu-
cose intolerance with its onset during pregnancy (or first
detected during pregnancy). Major risk factors for devel-
oping gestation diabetes include maternal age older than
30 years, being obese or overweight, a family history of dia-
betes, a history of diabetes in a prior pregnancy, a history
of poor obstetric outcome (such as a large-for-gestational
age [LGA] infant or stillbirth), and African-American,
Hispanic, or Native American ethnicity (U.S. Preventive
Services Task Force, 2003).
Women with gestational diabetes mellitus are at
increased risk for preeclampsia and glucose control-related
complications such as hypoglycemia, hyperglycemia, and
ketoacidosis. Gestational diabetes of any severity increases
the risk of fetal macrosomia. It is also associated with an
increased frequency of maternal hypertensive disorders and
the need for an operative birth. This may be the result of
fetal growth disorders (ADA, 2004). Even though gesta-
tional diabetes is diagnosed during pregnancy, the woman
may have had glucose intolerance before the pregnancy.
Screening
The American College of Obstetricians and Gynecologists
(ACOG) currently recommends routine screening of all
pregnant women at 24 to 28 weeks, or earlier if risk fac-
tors are present, although this is controversial. Published
data indicate that universal screening is not cost-effective
(Samson & Ferguson, 2004). The ADA recommends
selective screening based on the woman’s risk factors.
High-risk women include those with a prior history of
gestational diabetes, a strong family history of type 2 dia-
betes, marked obesity, multiple pregnancy, glycosuria,
advanced maternal age, non-white ethnicity, history of
polycystic ovary syndrome, hydramnios, recurrent vaginal
or urinary infections, prior infant with macrosomia, or
prior poor obstetric outcome. Women at high risk should
be screened earlier than 24 weeks. If the initial screening
is negative, rescreening should take place between 24 and
28 weeks. A woman with abnormal early results may have
had diabetes before the pregnancy, and her fetus is a great
risk for congenital anomalies. An elevated glycosylated
hemoglobin supports the likelihood of gestational diabetes
(Gabbe & Graves, 2003).
There is little consensus regarding the value of screen-
ing for gestational diabetes and the appropriate screening
method. Typically, screening is based on a 50-g 1-hour
glucose challenge test, usually performed between week 24
and 28 of gestation (U.S. Preventive Services Task Force,
2003). A 50-g oral glucose load is given, without regard to
the timing or content of the last meal. Blood glucose is
measured 1 hour later; a level above 140 mg/dL is abnor-
mal. If the result is abnormal, a 3-hour glucose tolerance
test is done. A diagnosis of gestational diabetes can be
made only after an abnormal result on the glucose tol-
erance test. Normal values are:
•
Fasting blood glucose level: less than 105 mg/dL
•
At 1 hour: less than 190 mg/dL
•
At 2 hours: less than 165 mg/dL
•
At 3 hours: less than 145 mg/dL
Two or more abnormal values confirm a diagnosis of
gestational diabetes (ADA, 2004).
Treatment
Women with gestational diabetes may be asymptomatic
throughout the pregnancy or they may exhibit subtle signs.
Early identification is important to facilitate prompt inter-
vention. Controlling maternal hyperglycemia with diet
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
549
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 549

alone or diet and insulin can reduce the risk of inappropri-
ate accelerated fetal growth. Once the diagnosis of gesta-
tional diabetes is made, the management is similar to
treatment for pregestational diabetes.
Nursing Management
The ultimate goal of nursing management when caring
for the woman with pregestational or gestational diabetes
is to minimize risks and complications. Education and
patient cooperation are key in achieving this goal. The
ideal outcome of every pregnancy is a healthy newborn
and mother, and nurses can be pivotal in realizing this
positive outcome.
Nursing management of the woman with pregesta-
tional diabetes or gestational diabetes is the same. Careful,
frequent antepartum care visits are necessary. The nurse
must take time to counsel and educate the women about
the changes needed in diet, possible need for insulin or
increased insulin dosages, and lifestyle changes. Since the
diabetic client is at high risk, the prenatal visits will be more
frequent (every 2 weeks up to 28 weeks and then twice a
week until birth).
Assessment
Nursing assessment should begin at the first prenatal visit.
For the woman with pregestational diabetes, obtain a
thorough history of the woman’s preexisting diabetic con-
dition. Ask about her duration of disease, management of
glucose levels (insulin injections, insulin pump, or oral
hypoglycemic agents), dietary adjustments, presence of
vascular complications and current vascular status, cur-
rent insulin regimen, and technique used for glucose test-
ing. The nurse should have a working knowledge of the
nutritional requirements of diabetics and should be able
to assess the adequacy and pattern of the woman’s dietary
intake. Assess the woman’s blood glucose self-monitoring
in terms of frequency and her ability to adjust the insulin
dose based on the changing patterns. Ask about the fre-
quency of episodes of hypoglycemia or hyperglycemia to
ascertain the woman’s ability to recognize and treat them.
During antepartum visits, assess the client’s knowl-
edge about her disease, including the signs and symptoms
of hypoglycemia, hyperglycemia, and diabetic ketoacido-
sis, insulin administration techniques, and impact of preg-
nancy on her chronic condition. Although the client may
have had diabetes for some time, do not assume that she
has a firm knowledge base about her disease process or
management of it (Fig. 20-1).
Risk assessment for gestational diabetes also is under-
taken at the first prenatal visit. Women with clinical
characteristics consistent with a high risk for gestational
diabetes should undergo glucose testing as soon as fea-
sible. These risk factors include:
•
Previous infant with congenital anomaly (skeletal, renal,
central nervous system [CNS], cardiac)
•
History of gestational diabetes or hydramnios in a pre-
vious pregnancy
•
Family history of diabetes
•
Age 35 or older
•
Previous infant weighing more than 9 pounds (4,000 g)
•
Previous unexplained fetal demise or neonatal death
•
Maternal obesity (Body Mass Index [BMI] > 30)
•
Hypertension
•
Hispanic, Native American, or African-American
ethnicity
•
Recurrent Monilia infections that don’t respond to
treatment
•
Signs and symptoms of glucose intolerance (polyuria,
polyphagia, polydipsia, fatigue)
•
Presence of glycosuria or proteinuria (Mattson & Smith,
2004)
Assessment of the woman’s psychosocial adaptation to
her condition is critical to gain her cooperation for a change
in regimen or the addition of a new regimen throughout
pregnancy. Identify her support systems and note any
financial constraints, as she will need more intense moni-
toring and frequent fetal surveillance. Laboratory studies
may include a glycosylated hemoglobin to determine the
mean blood glucose levels for the previous few months,
urine testing for glucose and protein, and cardiovascular
assessment.
Nursing Interventions
Nursing interventions include counseling and education
about the need for strict glucose monitoring, diet and exer-
cise, and signs and symptoms of complications. Encourage
the client and her family to make any lifestyle changes
needed to maximize the pregnancy outcome. Providing
dietary education and lifestyle advice that extends beyond
pregnancy may have the potential to lessen the risk of ges-
tational diabetes in subsequent pregnancies as well as
type 2 diabetes in the mother (Dornhorst & Frost, 2002).
550
Unit 7
CHILDBEARING AT RISK
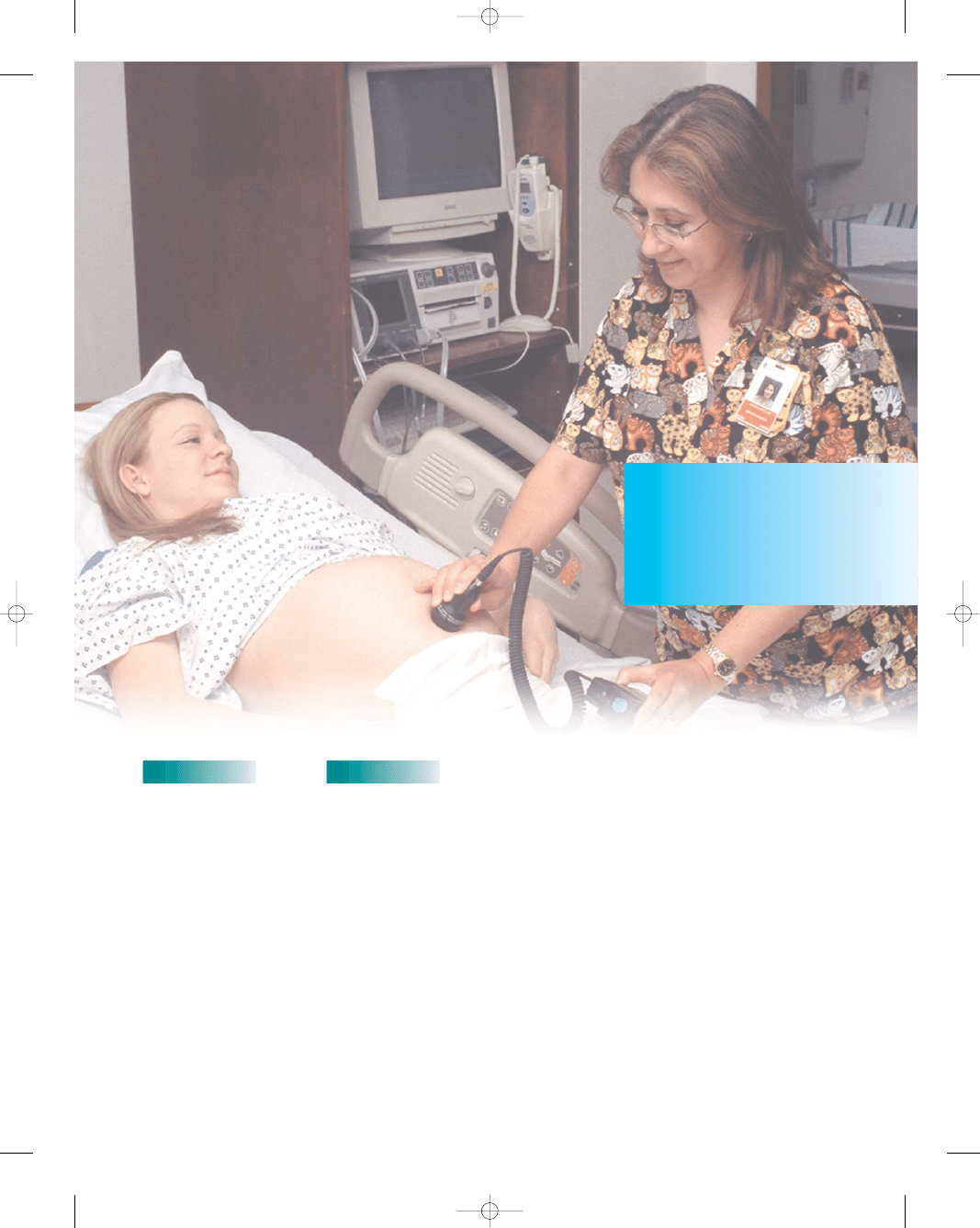
●
Figure 20-1
The nurse is demonstrating the technique for
self-blood glucose monitoring with a pregnant client.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 550
At each visit reinforce the importance of performing blood
glucose screening and documenting the results. With
proper instruction, the client and her family will be able to
cope with all the changes in her body during pregnancy
(Teaching Guidelines 20-1).
During the antepartum period, nursing interventions
typically include:
•
Monitoring weight, urine glucose, protein, and ketone
levels
•
Obtaining blood pressure measurements at each visit
•
Teaching the mother how to assess fetal activity to eval-
uate fetal well-being
•
Assisting with serial ultrasounds to monitor fetal growth
and with assessments of fetal well-being through non-
stress tests and biophysical profiles
•
Anticipating complications and planning appropriate
interventions or referrals
•
Discussing dietary measures related to blood glucose
control (Fig. 20-2); initiating referrals for nutritional
counseling to individualize the dietary plan
•
Encouraging the client to participate in an exercise pro-
gram that includes at least three sessions lasting longer
than 15 minutes per week (exercise may lessen the need
for insulin or dosage adjustments)
•
Assessing for signs and symptoms of preeclampsia and
hydramnios
•
Assisting with and teaching about insulin therapy,
including any changes needed if glucose levels are not
controlled
•
Urging the woman to perform blood glucose screening
(usually four times a day, before meals and at bedtime)
•
Reviewing discussions about the timing of birth and the
rationale
•
Counseling the client about the possibility of cesarean
birth for an LGA infant or informing the woman who
will be giving birth vaginally of the possible need for
augmentation with oxytocin (Pitocin)
•
Establishing fetal lung maturity prior to birth
•
Encouraging breastfeeding to normalize blood glucose
levels
•
Teaching the woman that her insulin needs after birth
will drastically decrease
•
Discussing future childbearing plans and contraception
after birth
•
Informing the client that she will need a repeat glucose
challenge test at a postpartum visit (ADA, 2004)
Nursing Interventions During the
Intrapartum Period
In the woman with well-controlled diabetes, birth is typ-
ically not induced before term unless there are complica-
tions, such as preeclampsia or fetal compromise. An
early delivery date might be set for the woman with
poorly controlled diabetes who is having complications.
During labor, intravenous saline is given and blood
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
551
T E A C H I N G G U I D E L I N E S 2 0 - 1
Teaching for the Pregnant Woman With Diabetes
•
Be sure to keep your appointments for frequent
prenatal visits and tests for fetal well-being.
•
Perform blood glucose self-monitoring as directed,
usually before each meal and at bedtime. Keep a record
of your results and call your healthcare provider with
any levels outside the established range. Bring your
results to each prenatal visit.
•
Perform daily “fetal kick counts.” Document them
and report any decrease in activity.
•
Drink 8 to 10 8-ounce glasses of water each
day to prevent bladder infections and maintain
hydration.
•
Wear proper, well-fitted footwear when walking to
prevent injury.
•
Engage in a regular exercise program such as walking
to aid in glucose control, but avoid exercising in
temperature extremes.
•
Consider breastfeeding your infant to lower your
blood glucose levels.
•
If you are taking insulin:
••
Administer the correct dose of insulin at the correct
time every day.
••
Eat breakfast within 30 minutes after injecting
regular insulin to prevent a reaction.
••
Plan meals at a fixed time and snacks to prevent
extremes in glucose levels.
•
Avoid simple sugars (cake, candy, cookies), which
raise blood glucose levels.
•
Know the signs and symptoms of hypoglycemia and
treatment needed:
••
Sweating, tremors, cold, clammy skin, headache
••
Feeling hungry, blurred vision, disorientation,
irritability
••
Treatment: Drink 8 ounces of milk and eat two
crackers or glucose tablets
•
Carry “glucose boosters” (such as Life Savers) to
prevent hypoglycemia.
•
Know the signs and symptoms of hyperglycemia and
treatment needed:
••
Dry mouth, frequent urination, excessive thirst,
rapid breathing
••
Feeling tired, flushed, hot skin, headache,
drowsiness
••
Treatment: Notify health care provider, since
hospitalization may be needed
•
Wear a diabetic identification bracelet at all
times.
•
Wash your hands frequently to prevent infections.
•
Report any signs and symptoms of illness,
infection, and dehydration to your health care
provider, because these can affect blood glucose
control.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 551
glucose levels are monitored every 1 to 2 hours. Glucose
levels should be kept below 110 mg/dL throughout labor.
If necessary, an infusion of regular insulin may be given
to sustain this level (Messner, 2004).
When caring for the laboring woman with diabetes,
adjust the IV rate and the rate of supplemental regular
insulin based on the blood glucose levels as ordered. Keep
a syringe with 50% dextrose solution available at the bed-
side to treat profound hypoglycemia. Monitor fetal heart
rate patterns throughout labor to detect reassuring or non-
reassuring patterns. Assess maternal vital signs every hour,
in addition to assessing the woman’s urinary output with
an indwelling catheter. If a cesarean birth is scheduled,
monitor the woman’s blood glucose levels hourly and
administer short-acting insulin or glucose based on the
blood glucose levels as ordered. After birth, monitor blood
glucose levels every 2 to 4 hours and continue IV fluid
administration as ordered.
Nursing Interventions During the
Postpartum Period
Nursing care should focus on monitoring blood glucose
levels during this period. Maternal control of glucose is
essential in the first few weeks postpartum, and breast-
feeding should be encouraged to assist in maintaining
good control. For the pregestational diabetic, no insulin
may be needed due to the sudden drop in human pla-
cental lactogen (hPL) after the delivery of the placenta.
For the woman with gestational diabetes, the focus is
on lifestyle education. Women with gestational diabetes
have a greater than 50% increased risk of developing
type 2 diabetes (ADA, 2004). Screening should be done
at the postpartum follow-up appointment in 6 weeks.
Women with normal results at that visit should be screened
every 3 years thereafter (ADA, 2004). The woman should
maintain an optimal weight to reduce her risk of develop-
ing diabetes. A referral to a dietitian can be helpful in out-
lining a balanced nutritious diet for the woman to achieve
this goal.
Cardiovascular Disorders
Every minute, an American woman dies of cardiovascu-
lar disease (Wenger, 2004). Cardiovascular disease is the
leading cause of death for men and women in the United
States. It kills nearly 500,000 women each year (Katz,
2004). Despite the prominent reduction in cardiovascu-
lar mortality among men, it has not declined for women.
Cardiovascular disease has killed more women then men
since 1984 (American Heart Association, 2003). In addi-
tion to being the number-one killer of women, on diag-
nosis, women have both a poorer overall prognosis and a
higher risk of death than men diagnosed with heart dis-
ease (Peddicord, 2005).
Approximately 1% of pregnant women have cardiac
disease, which can be dangerous to maternal well-being
(Cunningham et al., 2001). Rheumatic heart disease used
to represent the majority of cardiac conditions during
pregnancy, but congenital heart disease now constitutes
nearly half of all cases of heart disease encountered dur-
ing pregnancy. Management of heart disease during preg-
nancy has improved, and most women can continue the
pregnancy successfully (Kuczkowski, 2004). Few women
with heart disease die during pregnancy, but they are at
risk for other complications such as heart failure, arrhyth-
mias, and stroke. Their offspring are also at risk of com-
plications such as premature birth, low birthweight for
gestational age, respiratory distress syndrome, intra-
ventricular hemorrhage, and death (Siu & Colman, 2004).
Effects of Heart Disease on Pregnancy
To understand the consequences of heart disease during
pregnancy, it is important to review the hemodynamic
changes that occur in all pregnant women. First, blood
volume increases by approximately 50%, starting in early
pregnancy and rising rapidly by the third trimester.
Proportionately, plasma volume increases much more
than erythrocyte mass, which can lead to physiologic ane-
mia. These changes usually raise the maternal heart rate
by 10 beats per minute (Prasad & Ventura, 2001).
Similarly, cardiac output increases steadily during
pregnancy by 30% to 50% over prepregnancy levels. The
increase is due to both the expansion in blood volume and
552
Unit 7
CHILDBEARING AT RISK
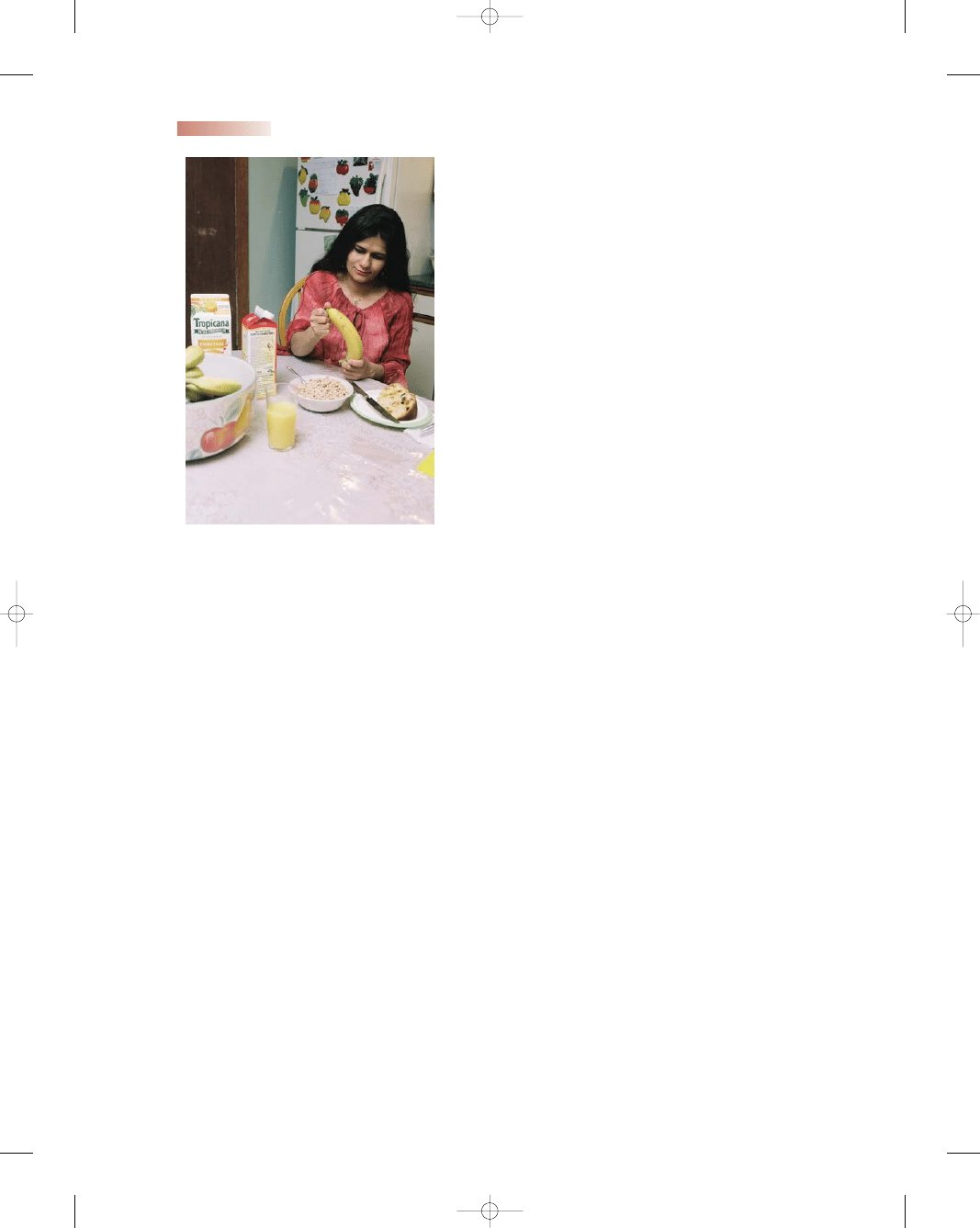
●
Figure 20-2
The pregnant client eating a
nutritious meal to ensure adequate glucose
control.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 552

the augmentation of stroke volume and heart rate. Other
hemodynamic changes associated with pregnancy include
a decrease in both the systemic vascular resistance and
pulmonary vascular resistance, thereby lowering the sys-
tolic and diastolic blood pressure. In addition, the hyper-
coagulability associated with pregnancy might increase
the risk of arterial thrombosis and embolization. These
normal physiologic changes may increase the risks of
pregnancy for women with underlying cardiovascular dis-
ease (Samson & Ferguson, 2004) (Table 20-1).
Classification of Heart Disease
How a woman is able to function during her pregnancy
is often more important than the diagnosis of cardiovas-
cular disease. The following is a functional classification
system developed by the Criteria Committee of the New
York Heart Association (1994) based on past and present
disability and physical signs:
•
Class I: asymptomatic with no limitation of physical
activity
•
Class II: symptomatic (dyspnea, chest pain) with
increased activity
•
Class III: symptomatic (fatigue, palpitations) with
normal activity
•
Class IV: symptomatic at rest or with any physical
activity
The classification may change as the pregnancy pro-
gresses due to the expanding stress on the cardiovascular
system. Typically, a woman with class I or II cardiac dis-
ease can go through a pregnancy without major compli-
cations. A woman with class III disease usually has to
maintain bed rest during pregnancy. A woman with class
IV disease should avoid pregnancy (McCann, 2004).
Many pregnant women progress through all the func-
tional classes as they cope with the numerous physiologic
changes taking place. Women with cardiac disease may
benefit from preconception counseling so that they know
the risks before deciding to become pregnant.
Maternal mortality varies directly with the functional
class at pregnancy onset. ACOG has adopted a three-tiered
classification according to risks for death during pregnancy.
Group I (minimal risk) has a mortality rate of 1%
and comprises women with:
•
Patent ductus arteriosus
•
Tetralogy of Fallot, corrected
•
Atrial septal defect
•
Ventricular septal defect
•
Mitral stenosis, class I and II
Group II (moderate risk) has a mortality rate of 5%
to 15% and comprises women with:
•
Tetralogy of Fallot, uncorrected
•
Mitral stenosis with atrial fibrillation
•
Aortic stenosis, class III and IV
•
Aortic coarctation without valvular involvement
•
Artificial valve replacement
Group III (major risk) has a 25% to 50% mortality
rate and comprises women with:
•
Pulmonary hypertension
•
Complicated aortic coarctation
•
Previous myocardial infarction (Gilbert & Harmon,
2003)
Clinical Manifestations
The clinical picture varies with the type of cardiac disorder.
Symptoms such as fatigue, dyspnea, palpitations, light-
headedness, and swollen feet may mimic many common
complaints of pregnancy, making clinical assessment of the
underlying cardiac disease challenging.
Congenital Heart Conditions
Pregnancy in women with congenital heart disease is
a relatively new field, since until recently women with
congenital heart defects didn’t live long enough to bear
children. Today, due to new surgical techniques to cor-
rect these defects, many of these women can bear chil-
dren. Table 20-2 highlights some of these congenital
conditions.
In some congenital heart conditions, women should be
advised to avoid pregnancy: uncorrected tetralogy of Fallot
or transposition of the great arteries, and Eisenmenger’s
syndrome, a defect with both cyanosis and pulmonary
hypertension (Martin & Foley, 2002). In most other
congenital heart conditions, pregnancy can be attempted,
although close monitoring is needed.
Pregnancy is considered safe for many women once
congenital defects are corrected. However, a cardiologist
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
553
Table 20-1
Measurement
Prepregnancy
Pregnancy
Heart rate
72 (
±10 bpm)
+10–20%
Cardiac output
4.3 (
±0.9 L/min)
+30% to 50%
Blood volume
5 L
+20% to 50%
Stroke volume
73.3 (
±9 mL)
+30%
Systemic 1,530
−20%
vascular
(
±520 dyne/
resistance
cm/sec)
Oxygen 250
mL/minute
+20–30%
consumption
Table 20-1
Expected Cardiovascular Changes
in Pregnancy
Sources: Martin and Foley, 2002; Mattson and Smith, 2004;
Blackburn, 2003; Harvey, 2004.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 553
554
Unit 7
CHILDBEARING AT RISK
Table 20-2
Condition
Description
Management
Tetralogy of Fallot
Atrial septal defect
(ASD)
Ventricular septal
defect (VSD)
Patent ductus
arteriosus (PDA)
Mitral valve
prolapse
Mitral valve stenosis
Four structural anomalies: obstruction to
pulmonary flow; ventricular septal
defect (abnormal opening between
the right and left ventricles);
dextroposition of the aorta (aortic
opening overriding the septum and
receiving blood from both ventricles);
and right ventricular hypertrophy
(increase in volume of the myocardium
of the right ventricle) (O’Toole, 2003)
Congenital heart defect involving a
communication or opening between
the atria with left-to-right shunting due
to greater left-sided pressure
Arrhythmias present in some women
Congenital heart defect involving an
opening in the ventricular septum
(normal in the fetus) persisting after birth,
permitting blood flow from the left to the
right ventricle, resulting in bypassing of
the pulmonary circulation.
Complications include arrhythmias,
heart failure, and pulmonary
hypertension (Lowdermilk & Perry, 2004).
Abnormal persistence of an open lumen
in the ductus arteriosus between the
aorta and the pulmonary artery after
birth (O’Toole, 2003)
Very common in the general population,
occurring most often in younger women
Leaflets of the mitral valve prolapse into the
left atrium during ventricular contraction
The most common cause of mitral valve
regurgitation if present during
pregnancy (Martin & Foley, 2002)
Usually improvement in mitral valve
function due to increased blood volume
and decreased systemic vascular
resistance of pregnancy; most women
are able to tolerate pregnancy well.
Most common chronic rheumatic valvular
lesion in pregnancy
Causes obstruction of blood flow from the
atria to the ventricle, thereby
decreasing ventricular filling and
causing a fixed cardiac output
Resultant pulmonary edema, pulmonary
hypertension, and right ventricular
failure (Goswami & Ong, 2005)
Most pregnant women with this condition
can be managed medically.
Hospitalization and bed rest possible after
the 20th week with hemodynamic
monitoring via a pulmonary artery
catheter to monitor volume status
Oxygen therapy may be necessary during
labor and birth
Treatment with atrioventricular nodal
blocking agents, and at times with
electrical cardioversion (Wolbretta,
2003)
Rest with limited activity if symptomatic
Surgical ligation of the open ductus during
early childhood; subsequent problems
minimal after surgical correction
Most women are asymptomatic; diagnosis
is made incidentally
Occasional palpations, chest pain, or
arrhythmias in some women, possibly
requiring beta-blockers
Usually no special precautions are
necessary during pregnancy
General symptomatic improvement with
medical management involving
diuretics, beta-blockers, and
anticoagulant therapy
Activity restriction, reduction in sodium,
and potentially bed rest if condition
severe
Table 20-2
Selected Heart Conditions Affecting Pregnancy
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 554
should be consulted and should play a role in precon-
ception counseling so that risks can be discussed.
Acquired Heart Disease
Acquired heart disease is typically rheumatic in origin
(see Table 20-2). The incidence of rheumatic heart dis-
ease has declined dramatically in the past several decades
because of prompt identification of streptococcal throat
infections and treatment with antibiotics. When the heart
is involved, valvular lesions such as mitral stenosis, pro-
lapse, or aortic stenosis are common.
In addition, many women are postponing childbearing
until the fourth or fifth decade of life. With advancing
maternal age, underlying medical conditions such as hyper-
tension, diabetes, and hypercholesterolemia contributing to
ischemic heart disease become more common and increase
the incidence of acquired heart disease complicating preg-
nancy. Coronary artery disease and myocardial infarction
may result.
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
555
Table 20-2
Condition
Description
Management
Aortic stenosis
Peripartum
cardiomyopathy
Myocardial
infarction (MI)
Narrowing of the opening of the aortic
valve, leading to an obstruction to left
ventricular ejection (Lowdermilk &
Perry, 2004)
Women with mild disease can tolerate
hypervolemia of pregnancy; with
progressive narrowing of the opening,
cardiac output becomes fixed.
Diagnosis can be confirmed with
echocardiography. Most women can
be managed with medical therapy,
bed rest, and close monitoring.
Rare congestive cardiomyopathy that
may arise during pregnancy.
Multiparity, age, multiple fetuses,
hypertension, an infectious agent,
autoimmune disease, or cocaine use
may contributing to its presence (Siu &
Colman, 2004).
Development of heart failure in the last
month of pregnancy or within 5 months
of giving birth without any preexisting
heart disease or any identifiable cause
Rare during pregnancy but incidence is
expected to increase as older women
are becoming pregnant and the risk
factors for coronary artery disease
become more prevalent.
Factors contributing to MI include
family history, stress, smoking,
age, obesity, multiple fetuses,
hypercholesterolemia, and cocaine
use (Wolbretta, 2003).
Increased plasma volume and cardiac
output during pregnancy increase the
cardiac workload as well as the
myocardial oxygen demands;
imbalance in supply and demand may
contribute to myocardial ischemia.
Diagnosis confirmed with
echocardiography
Pharmacologic treatment with beta-
blockers and/or antiarrhythmic agents
to reduce risk of heart failure and/or
dysrhythmias
Bed rest/limiting activity and close
monitoring
Preload reduction with diuretic therapy
Afterload reduction with vasodilators
Improvement in contractility with inotropic
agents
Nonpharmcologic approaches include
salt restriction and daily exercise such
as walking or biking
The question of whether another
pregnancy should be attempted is
controversial due to the high risk of
repeat complications
Incorporation of usual treatment
modalities for any acute MI along with
consideration for the fetus
Anticoagulant therapy, rest, and lifestyle
changes to preserve the health of both
parties
Table 20-2
Selected Heart Conditions Affecting Pregnancy
(continued)
Sources: Goswami and Ong, 2005; Sui and Colman, 2004; Lowdermilk and Perry, 2004;
Martin and Foley, 2002; O’Toole, 2005; Wolbretta, 2003.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 555
Treatment
The woman with known cardiac disease should consult her
health care provider before becoming pregnant so that she
can determine the advisability and optimal time for a preg-
nancy, the need for and timing of diagnostic procedures,
and any medical management changes needed. If the
woman presents for care after she has become pregnant,
prenatal counseling should focus on the signs and symp-
toms of cardiac compromise, dietary and lifestyle changes
needed, and the impact of the hemodynamic changes of
pregnancy. More frequent prenatal visits (every 2 weeks
until the last month and then weekly) are usually needed to
ensure the health and safety of the mother and fetus.
Nursing Management
Nursing management of the pregnant woman with heart
disease focuses on assisting with measures to stabilize
the mother’s hemodynamic status, because a decrease in
maternal blood pressure or volume will cause blood to be
shunted away from the uterus, thus reducing placental
perfusion. Collaboration between the cardiologist, obste-
trician, perinatologist, and nurse is needed to promote
stabilization.
Assessment
Risk assessment should be completed before a woman
becomes pregnant. The data needed for risk assess-
ment can be acquired from a thorough cardiovascular
history and examination, a 12-lead electrocardiogram
(ECG), and evaluation of oxygen saturation levels by pulse
oximetry. When possible, any surgical procedures, such as
valve replacement, should be done before pregnancy to
improve fetal and maternal outcomes (Goswami & Ong,
2005).
Frequent and thorough assessments are crucial dur-
ing the antepartum period to ensure early detection and
prompt intervention should the woman experience cardiac
decompensation. Monitor the woman closely for changes
in vital signs, and auscultate heart sounds for abnormali-
ties, including murmurs. Check the client’s weight, report-
ing any weight gain outside recommended parameters.
Evaluate for edema and note any pitting.
Assess the fetal heart rate and review serial ultrasound
results to monitor fetal growth. Ask the woman about fetal
activity, and report any changes such as a decrease in fetal
movements. Ask the woman about any symptoms of pre-
term labor, such as low back pain, uterine contractions,
and increased pelvic pressure and vaginal discharge, and
report them immediately. Assess the client’s lifestyle pat-
terns and suggest realistic modifications. As the client’s
pregnancy advances, expect her functional class to be
revised based on her level of disability.
In addition, the nurse plays a major role in recogniz-
ing the signs and symptoms of cardiac decompensation.
This is vital because the mother’s hemodynamic status
determines the health of the fetus. These signs and symp-
toms include:
•
Shortness of breath on exertion
•
Cyanosis of lips and nail beds
•
Swelling of face, hands, and feet
•
Rapid respirations
•
Abnormal heartbeats, racing heart, or palpitations
•
Chest pain
•
Syncope
•
Increasing fatigue
•
Moist, frequent cough
Nursing Interventions
Nursing interventions for the woman with heart disease
include ongoing assessment of the mother and fetus to
ensure the best outcome. Additional nursing interven-
tions include:
•
Review the client’s prescribed cardiac medications;
reinforce their use and explain about their potential
side effects.
•
Outline the diagnostic tests that may be used, including
ECG and echocardiogram.
•
Advise the client to make time for rest periods in the
side-lying position.
•
Teach the woman to assess fetal activity daily and
report any changes.
•
Stress the importance of frequent prenatal visits; reinforce
the need for close medical supervision throughout
pregnancy.
•
Promote good prenatal nutrition, with a possible refer-
ral to a nutritionist.
•
Discuss the need to limit dietary sodium if indicated to
reduce fluid retention.
•
Help the client to prioritize household chores and
childcare.
•
Teach the client about signs and symptoms of cardiac
decompensation; instruct her to notify the health care
provider should any occur.
•
Explain the need for serial nonstress testing at about
32 weeks.
•
Stress the need to notify the health care professional of
any infection exposure.
•
Instruct the client about the need to consume a high-
fiber diet to prevent straining or constipation.
•
Prepare the client and family for labor and birth and the
options available.
•
Identify support systems available to the client and her
family; encourage their use.
During labor, anticipate the need for invasive hemo-
dynamic monitoring, and make sure the woman has been
prepared for this beforehand. Monitor her fluid volume
carefully to prevent overload. Anticipate the use of epidural
anesthesia if a vaginal birth is planned. After birth, assess
the client for possible fluid overload as peripheral fluids
mobilize. This fluid shift from the periphery to the central
556
Unit 7
CHILDBEARING AT RISK
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 556
circulation taxes the heart, and signs of heart failure such
as cough, progressive dyspnea, edema, palpitations, and
crackles in the lung bases may ensue before postpartum
diuresis begins. Because hemodynamics do not return to
baseline for several days after childbirth, women at inter-
mediate or high risk require monitoring for at least 72 hours
postpartum (Siu & Colman, 2004).
Women with a high-risk pregnancy involving car-
diac disease need assistance in reducing risks that would
lead to complications or further cardiac compromise.
Counseling and education are key. Assess the client’s
understanding of her condition and what restrictions
and lifestyle changes may be needed to provide the best
outcome for both her and her fetus. Ensuring a healthy
infant and mother at the end of pregnancy is the ulti-
mate goal.
Chronic Hypertension
Chronic hypertension exists when the woman has high
blood pressure before pregnancy or before the 20th week
of gestation, or when hypertension persists for more than
12 weeks postpartum (London et al., 2003). The Seventh
Report of the Joint National Committee on Prevention,
Detection, Evaluation, and Treatment of High Blood
Pressure (JNC, 2003) has classified blood pressure as
follows:
•
Normal: systolic less than 120 mm Hg, diastolic less than
80 mmHg
•
Prehypertensive: systolic 120 to 139 mm Hg, diastolic
80 to 89 mmHg
•
Mild hypertension: systolic 140 to 159 mm Hg, diastolic
90 to 99 mmHg
•
Severe hypertension: systolic 160 mm Hg or higher, dias-
tolic 100 mm Hg or higher
Chronic hypertension is typically seen in older,
obese women with glucose intolerance. The most com-
mon complication is preeclampsia, which is seen in
approximately 20% of women who enter the pregnancy
with hypertension. This preexisting condition places
the woman at greater risk for developing preeclampsia
(see Chapter 19) and fetal growth restriction during
pregnancy.
Treatment
Preconception counseling is important in fostering positive
outcomes. Typically, it involves lifestyle changes involving
diet, exercise, weight loss, and smoking cessation to mod-
ify this condition.
Treatment for women with chronic hypertension
focuses on maintaining normal blood pressure, prevent-
ing superimposed preeclampsia/eclampsia, and ensuring
normal fetal development. Once the woman is pregnant,
antihypertensive agents are typically reserved for severe
hypertension (150 to 160 mm Hg/100 to 110 mm Hg).
Methyldopa (Aldomet) is a commonly prescribed agent
because of its safety record during pregnancy. Methyldopa
(Aldomet), a slow-acting antihypertensive agent, helps
to improve uterine perfusion. Typically 1 g is given orally,
followed by a regimen of 1 to 2 g daily.
Other antihypertensive agents that can be use include
labetalol (Transdate), atenolol (Tenorium), and nife-
dipine (Procardia) (Goswami & Ong, 2005). Lifestyle
changes are needed and should continue throughout ges-
tation. The woman with chronic hypertension will be seen
more frequently prenatally (every 2 weeks until 28 weeks
and then weekly until birth) to monitor her blood pressure
and to assess for any signs of preeclampsia. At approxi-
mately 24 weeks’ gestation, the woman will be instructed
to document fetal movement. At this same time, serial
ultrasounds will be ordered to monitor fetal growth and
amniotic fluid volume. Additional tests will be included if
the client’s status changes.
Nursing Management
Preconception counseling is the ideal time to discuss
lifestyle changes to prevent or control hypertension. One
area to cover during this visit would be the Dietary
Approaches to Stop Hypertension (DASH) diet, which
contains an adequate intake of potassium, magnesium,
and calcium. Sodium is usually limited to 2.4 g. Suggest
aerobic exercise until the woman becomes pregnant,
although she should cease it once the pregnancy is con-
firmed. Encourage smoking cessation and avoidance of
alcohol. If the woman is overweight, encourage her to
lose weight before becoming pregnant, not during the
pregnancy (Dudek, 2006). Stressing the positive benefits
of a healthy lifestyle might help motivate the woman to
make the modifications and change unhealthy habits.
Encourage women with chronic hypertension to use
home blood pressure monitoring devices to document
values; any elevations should be reported. Scheduling
appointments for antepartum fetal assessment (28 to
30 weeks) and explaining the rationale for the need to
monitor fetal growth are important to gain the woman’s
cooperation in the planned regimen. Also carefully mon-
itor the woman for abruptio placentae (abdominal pain,
rigid abdomen, vaginal bleeding), as well as superimposed
preeclampsia (elevation in blood pressure, weight gain,
edema, proteinuria). Alerting the woman to these poten-
tial risks is critical to early identification of these compli-
cations and prompt intervention.
In addition, stress the importance of daily periods
of rest (1 hour) in the left lateral recumbent position to
maximize placental perfusion. Instruct the woman and
her family how to take and record a daily blood pres-
sure, and reinforce the need for her to take her med-
ications as prescribed to control her blood pressure as
well as to ensure the well-being of her unborn child.
Praising her for her efforts at each prenatal visit may
help motivate her to continue the regimen throughout
her pregnancy.
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
557
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 557
Respiratory Conditions
During pregnancy, the respiratory system is affected by
hormonal changes, mechanical changes, and prior respi-
ratory conditions. These changes can cause a woman with
a history of compromised respiration to decompensate
during pregnancy. While upper respiratory infections are
typically self-limiting, chronic respiratory conditions, such
as asthma or tuberculosis, can have a negative effect on
the growing fetus when alterations in oxygenation occur
in the mother. The outcome of pregnancy in a woman
with a respiratory condition depends on the severity of the
oxygen alteration as well as the degree and duration of
hypoxia on the fetus.
Asthma
Asthma is the most common respiratory disease compli-
cating pregnancy, affecting approximately 7% of child-
bearing women in the United States (Kazzi & Marachelian,
2004). Asthma affects 20 million Americans and is one of
the most common potentially serious medical conditions to
complicate pregnancy.
Effects of Asthma on Pregnancy
Maternal asthma is associated with an increased risk of
infant death, preeclampsia, IUGR, preterm birth, and
low birthweight. These risks are linked to the severity of
asthma: more severe asthma increases the risk (NAEPP,
2005). Asthma is also known as reactive airway disease
because the bronchioles constrict in response to allergens,
irritants, and infections. In addition to bronchoconstric-
tion, inflammation of the airways produces thick mucus
that further limits the movement of air and makes breath-
ing difficult.
The normal physiologic changes of pregnancy affect
the respiratory system. While the respiratory rate does
not change, hyperventilation increases at term by 48%
due to high progesterone levels. Diaphragmatic eleva-
tion and a decrease in functional lung residual capacity
occur late in pregnancy, which may reduce the woman’s
ability to inspire deeply to take in more oxygen. Oxygen
consumption and the metabolic rate both increase, plac-
ing additional stress on the woman’s respiratory system
(Beckmann, 2002).
A pregnant woman with asthma has a one-in-three
chance of the asthma changing, but the effect of pregnancy
on asthma is unpredictable. Studies have shown that in
one third of pregnancies the asthma will get better; in one
third it will get worse, and in the remaining third it will
remain the same. The greatest increase in asthma attacks
usually occurs between 24 and 36 weeks’ gestation; flare-
ups are rare during the last 4 weeks of pregnancy and dur-
ing labor (Blaiss, 2004).
Both the woman and her fetus are at risk if asthma is
not well managed during pregnancy. When a pregnant
woman has trouble breathing, her fetus also has trouble
getting the oxygen it needs for adequate growth and devel-
opment. Severe persistent asthma has been linked to the
development of maternal hypertension, preeclampsia, pla-
centa previa, uterine hemorrhage, and oligohydramnios.
Women whose asthma is poorly controlled during preg-
nancy are at increased risk of preterm birth, low birth-
weight, and stillbirth (Beckmann, 2003).
Treatment
Successful management of asthma in pregnancy involves
drug therapy, client education, and the elimination of
environmental triggers. Triggers provoke an exacerbation
and need to be identified and controlled. Some common
asthma triggers are listed in Box 20-2.
Asthma should be treated as aggressively in pregnant
women as in nonpregnant women because the benefits of
averting an asthma attack outweigh the risks of medica-
tions. The two major classifications of drugs used to treat
asthma are bronchodilators, such as albuterol (Proventil),
pirbuterol acetate (Maxair), and salmeterol (Serevent),
and corticosteroids, such as prednisone (Deltasone),
beclomethasone (Beclovent), and fluticasone propionate
(Flovent). Clients with asthma typically receive these med-
ications by inhalation.
Nursing Management
Complete a thorough assessment of asthma triggers and
recommend strategies to reduce exposure to them, review
the client’s medication therapy, and educate her about
controlling asthma symptoms.
Assessment
Obtain a thorough history of the disease. Auscultate the
lungs and assess respiratory and heart rates. The physical
examination should include rate, rhythm, and depth of
respirations; skin color; blood pressure and pulse rate; and
evaluation for signs of fatigue. Women experiencing an
acute asthma attack often present with wheezing, chest
558
Unit 7
CHILDBEARING AT RISK
• Smoke and chemical irritants
• Air pollution
• Dust mites
• Animal dander
• Seasonal changes with pollen, molds, and spores
• Upper respiratory infections
• Esophageal reflux
• Medications, such as aspirin and nonsteroidal anti-
inflammatory drugs (NSAIDs)
• Exercise
• Cold air
• Emotional stress (Kazzi & Marachelian, 2004)
BOX 20-2
COMMON ASTHMA TRIGGERS
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 558
tightness, tachypnea, nonproductive coughing, shortness
of breath, and dyspnea. Lung auscultation findings might
include diffuse wheezes and rhonchi, bronchovesicular
sounds, and a more prominent expiratory phase of respi-
ration compared to the inspiratory phase (Blaiss, 2004). If
the pregnancy is far enough along, the fetal heart rate is
measured and routine prenatal assessments (weight, blood
pressure, fundal height, urine for protein) are completed.
Laboratory studies usually ordered include a com-
plete blood count with differential (to assess the degree
of nonspecific inflammation and identify anemia) and
pulmonary function tests (to assess the severity of an
attack and to provide a baseline to determine the client’s
response to treatment).
Nursing Interventions
Nursing interventions focus on client education to pro-
mote adherence to the treatment regimen, thereby fos-
tering the optimal environment for fetal growth and
development. Provide the client with suggestions on how
to control her environment (Teaching Guidelines 20-2).
Client education is essential to ensure that the woman
understands drug actions and interactions, the uses and
potential abuses of asthma medications, and the symptoms
that require medical evaluation. Reviewing potential peri-
natal complications with the woman is helpful in motivat-
ing her to adhere to the prescribed regimen. At each
antepartum visit, reassess the efficacy of the treatment plan
to determine whether adjustments are needed.
Taking control of asthma in pregnancy is the respon-
sibility of the client along with her health care team.
Providing the client with the knowledge and tools to mon-
itor her condition, control triggers, and use medications
to prevent acute exacerbations assists the client in taking
control. Facilitating this partnership with the woman will
improve perinatal outcomes.
When teaching the pregnant woman with asthma,
cover the following topics:
•
Signs and symptoms of asthma progression and exacer-
bation
•
Importance and safety of medication to fetus and to
herself
•
Warning signs that indicate the need to contact the
healthcare provider
•
Potential harm to fetus and self by undertreatment or
delay in seeking help
•
Prevention and avoidance of known triggers
•
Home use of metered-dose inhalers
•
Adverse effects of medications
During labor, nursing interventions focus on moni-
toring the client’s oxygenation saturation by pulse oxime-
try and providing pain management through epidural
analgesia to reduce stress, which may trigger an acute
attack. Continuously monitor the fetus for distress during
labor and assess fetal heart rate patterns for indications of
hypoxia. Assess the newborn for signs and symptoms of
hypoxia. Asthma medications can be used throughout the
pregnancy and labor and during the postpartum period to
control symptoms.
Tuberculosis
Tuberculosis (TB) is a disease that has been around
for years but never seems to go away completely. It re-
mains the most common respiratory disease in the world
(Herchline & Amorosa, 2005). Although it is not prevalent
in the United States, a resurgence was noted starting in the
mid-1980s secondary to the acquired immunodeficiency
syndrome (AIDS) epidemic and immigration. Therefore,
all nurses must be skilled in screening for and managing
this condition.
Women at risk for TB are those who are immuno-
compromised, homeless, or using injectable drugs. Women
emigrating from developing countries such as Latin
America, Asia, China, Mexico, Haiti, and Africa with high
rates of TB also are at risk.
The lung is the major site of involvement. A person
becomes infected by breathing in the infectious organism,
Mycobacterium tuberculosis, carried on a droplet nuclei
and spread by airborne transmission. Clients can remain
asymptomatic for long periods of time as the organism
may lie dormant.
Treatment
Treatment of TB during pregnancy is essentially the same
as that for the general population. Medications are the cor-
nerstone of treatment to prevent infection progression.
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
559
T E A C H I N G G U I D E L I N E S 2 0 - 2
Teaching to Control Environmental Triggers
•
Remove any carpeting in the house, especially the
bedroom, to reduce dust mites.
•
Use allergen-proof encasing on the mattress, box
spring, and pillows.
•
Wash all bedding in hot water.
•
Remove dust collectors in house, such as stuffed ani-
mals, books, knick-knacks.
•
Avoid pets in the house to reduce exposure to pet dan-
der.
•
Use a high-efficiency particulate air-filtering system in
the bedroom.
•
Do not smoke, and avoid places where you can be
exposed to passive cigarette smoke from others.
•
Stay indoors and use air conditioning when the pollen
or mold count is high or air quality is poor.
•
Wear a covering over your nose and mouth when
going outside in the cold weather.
•
Avoid exposure to persons with colds, flu, or viruses.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 559
The medical therapy for pregnant women is a combination
of medications such as isoniazid, rifampin, and ethambu-
tol, taken daily for up to 9 months. These anti-TB agents
appear to have minimal risks for the development of con-
genital anomalies and may be started as soon as the diag-
nosis of TB is made. However, extensive research has not
been done to determine the definitive safety of these drugs
(Herchline & Amorosa, 2005).
Nursing Management
Educating the client and her family about the correct
administration of medications and potential side effects is
necessary. Nursing management focuses on infection con-
trol measures and client and family education. Nurses play
a major role in TB prevention by teaching family members
how the disease is transmitted so they can protect the new-
born and other family members from airborne organisms
(McKinney et al., 2005).
Assessment
At antepartum visits, be alert for clinical manifestations of
TB, including fatigue, fever or night sweats, nonproductive
cough, slow weight loss, anemia, hemoptysis, and anorexia
(Lake, 2001). If TB is suspected or the woman is at risk for
developing TB, anticipate screening with the tuberculin
skin test. Screening is recommended for pregnant women
who fall into a high-risk group: born in a country with a
high incidence of TB, alcohol abuse, injectable drug use,
HIV infection, and immunosuppression.
Screening is done with the tuberculin skin test using
purified protein derivative (PPD), which is given by intra-
dermal injection. If the client has been exposed to TB, a
reddened induration will appear within 72 hours. A follow-
up chest x-ray with lead shielding over the abdomen and
sputum cultures will confirm the diagnosis.
Nursing Interventions
Compliance with the multidrug therapy is critical to pro-
tect the woman and her fetus from progression of TB.
Nurses can assist by first identifying high-risk women for
screening and then educating them about the disease
process, mode of transmission, prevention, potential com-
plications, and the importance of adherence to the treat-
ment regimen.
Stressing the importance of health-promotion activi-
ties throughout the pregnancy is important. Some sugges-
tions might include avoiding crowded living conditions,
avoiding sick people, maintaining adequate hydration,
eating a nutritious, well-balanced diet, keeping all pre-
natal appointments to evaluate fetal growth and well-
being, and getting plenty of fresh air by going outside
frequently. Determining the woman’s understanding of
her condition and treatment plan is important for com-
pliance. A language interpreter may be needed to vali-
date and reinforce her understanding if she does not
speak English.
Breastfeeding is not contraindicated during the
medication regimen and should in fact be encouraged.
Management of the newborn of a mother with TB involves
preventing transmission by teaching the parents not to
cough, sneeze, or talk directly into the newborn’s face.
Nurses should keep up to date with new therapies and
screening techniques to treat this centuries-old disease.
Hematologic Conditions
Anemia,
a reduction in red blood cell volume, is mea-
sured by hematocrit (Hct) or a decrease in the concentra-
tion of hemoglobin (Hgb) in the peripheral blood. This
results in reduced capacity of the blood to carry oxygen to
the vital organs of the mother and fetus. Anemia is a sign
of an underlying problem but does not indicate its origin.
In women, Hgb below 12 g/100 mL or Hct below 37%
indicates anemia (Youngkin & Davis, 2004). During preg-
nancy, anemia increases the risk of preterm birth, infec-
tions, and delayed healing.
Iron Deficiency Anemia
Iron deficiency anemia affects one in four pregnancies and
is usually caused by inadequate dietary intake of iron
(McCann, 2004). It is a very common state in pregnant
women and can be caused by a variety of factors, includ-
ing poor nutrition, hemolysis,
pica
(consuming non-food
substances), multiple gestation, limited intervals between
pregnancies, and blood loss. Anemia at term increases the
perinatal risk for both the mother and newborn. The risks
of hemorrhage (impaired platelet function) and infection
during and after birth also are increased. Anemia during
the early part of pregnancy can increase the likelihood
of preterm birth, low birthweight, and perinatal mortality
(Blackburn, 2003).
The effects of maternal iron deficiency on the fetus
and newborn have not been substantiated. Even with sig-
nificant maternal iron depletion, the fetus will receive
adequate stores, but at the cost to the mother (McKinney
et al., 2005).
Clinical Manifestations
Typically, the woman with iron deficiency anemia presents
with fatigue, weakness, malaise, anorexia, susceptibility to
infection (frequent colds), pale mucus membranes, tachy-
cardia, and pallor. Laboratory studies usually reveal low
Hgb (<11 g/dL), low Hct (<35%), low serum iron level
(<30 ug/dL), microcytic and hypochromic cells, and low
serum ferritin level (<100 mg/dL).
Treatment
The goals of treatment for iron deficiency anemia in preg-
nancy are to eliminate symptoms, correct the deficiency,
and replenish iron stores. Early and daily administration
of prenatal vitamins and iron is recommended, because
560
Unit 7
CHILDBEARING AT RISK
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 560
fulfilling maternal iron requirements solely through diet
in the face of diminished iron stores is difficult.
Nursing Management
Since the treatment of iron deficiency anemia is pharma-
cologic and dietary in nature, the nurse’s role is to encour-
age compliance with drug therapy and provide dietary
instruction about the intake of foods high in iron. Although
iron constitutes a minimal percentage of the body’s total
weight, it has several major roles: it assists in the transport
of oxygen and carbon dioxide throughout the body, it aids
in the production of red blood cells, and it plays a role in
the body’s immune response.
Stress the importance of taking the prenatal vitamin
and iron supplement consistently. Taking iron on an
empty stomach improves its absorption, but many women
cannot tolerate the gastrointestinal discomfort it causes. In
such cases, taking it with meals is advised. Adverse effects
are predominantly gastrointestinal and include gastric dis-
comfort, nausea, vomiting, anorexia, diarrhea, metallic
taste, and constipation. Taking the iron supplement with
meals and increasing intake of fiber and fluids will typically
overcome the most common side effects.
Dietary counseling includes assessing the woman’s
dietary intake as well as the quantity and timing of inges-
tion of substances that interfere with iron absorption,
such as tea, coffee, chocolate, and high-fiber foods.
Foods high in iron to recommend include dried fruits,
whole grains, green leafy vegetables, meats, peanut but-
ter, and iron-fortified cereals (Dudek, 2006). A referral
to a dietitian might be in order. Teaching Guidelines 20-3
highlights the instructions for the pregnant woman with
iron deficiency anemia.
Thalassemia
Thalassemia is a group of hereditary anemias in which
synthesis of one or both chains of the hemoglobin mol-
ecule (alpha and beta) is defective. A low Hgb and a
microcytic, hypochromic anemia result (Youngkin &
Davis, 2004). The prevalence and severity of thalassemia
depend on the population, with the type of thalassemia
seen dependent on racial background: persons of Medi-
terranean, Asian, Italian, or Greek heritage and African-
Americans are most frequently affected. Beta-thalassemia
is the most common form found in the United States
(McKinney et al., 2005).
Thalassemia occurs in two forms: minor and major.
Thalassemia minor, the heterozygous form, results from
the inheritance of one abnormal gene from either parent,
placing the offspring in a carrier trait state. These women
have little or no hematologic disease and are clinically
asymptomatic (silent carrier state). Thalassemia major is
the form involving inheritance of the gene from both par-
ents. Thalassemia major can be very severe. Genetic
counseling might be necessary when decisions about child-
bearing are being made.
Thalassemia minor has little effect on the pregnancy,
although the woman will have mild, persistent anemia.
This anemia does not respond to iron therapy, and iron
supplements should not be prescribed. Women with tha-
lassemia major do not usually become pregnant because of
lifelong severe hemolysis, anemia, and premature death
(Poole, 2003).
Diagnostic studies typically used to diagnose tha-
lassemia include a complete blood count, bone marrow
examination, peripheral blood smear, iron studies, and
Hgb (Blackburn, 2003).
Management of thalassemia during pregnancy de-
pends on the severity of the disease. Identification and
screening are important to plan care. The woman’s eth-
nic background, medical history, and blood studies are
analyzed. If the woman is determined to be a carrier,
screening of the father of the child is indicated. Knowledge
of the carrier state of each parent provides the genetic
counselor with knowledge about the risk that the fetus
will be a carrier or will have the disease (Poole, 2003).
Mild anemia may be present, and instructions to rest
and avoid infections are helpful. Nurses should provide
supportive care and expectant management throughout
the pregnancy.
Sickle Cell Anemia
Sickle cell anemia is an autosomal recessive inherited con-
dition that results from a defective hemoglobin molecule
(hemoglobin S). It is found most commonly in African-
Americans, Southeast Asians, and Middle Eastern popu-
lations. About 1 in 10 African-Americans are carriers of
the trait, while approximately 3 in 800 are affected with the
disease (McCann, 2004). People with only one gene for
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
561
T E A C H I N G G U I D E L I N E S 2 0 - 3
Teaching for the Woman with
Iron Deficiency Anemia
•
Take your prenatal vitamin daily; if you miss a dose,
take it as soon as you remember.
•
For best absorption, take iron supplement between
meals.
•
Avoid taking iron supplement with coffee, tea,
chocolate, and high-fiber food.
•
Eat foods rich in iron, such as:
••
Meats, green leafy vegetables, legumes, dried fruits,
whole grains
••
Peanut butter, bean dip, whole-wheat fortified
breads and cereals
•
For best iron absorption from foods, consume the
food along with a food high in vitamin C.
•
Increase your exercise, fluids, and high-fiber foods to
reduce constipation.
•
Plan frequent rest periods during the day.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 561
the trait (heterozygous) will have sickle cell trait without
obvious symptoms of the disease and with little effect on
the pregnancy.
In the human body, the hemoglobin molecule serves
as the oxygen-carrying component of the red blood cells.
Most people have several types of circulation hemoglobin
(HbA and HbA2) that make up the majority of their cir-
culatory system. In sickle cell disease, the abnormal hemo-
globin S (HbS) replaces HbA and HbA2. This abnormal
hemoglobin (HbS) becomes sickle-shaped when it isn’t
fully saturated with oxygen. Subsequently, it begins to
build up in the capillaries and smaller blood vessels, mak-
ing blood more viscous. These sickle cells clump together,
clogging the small blood vessels. As a result, hypoxia occurs
and leads to a crisis. In addition, sickle cells have a shorter
life span (10 to 20 days) than the normal red blood cell
(120 days). The combination of clumped red cells, fragile
cells, and shortened lifespan contribute to the severe ane-
mia (Samson & Ferguson, 2004).
Sickle cell anemia during pregnancy is associated
with more severe anemia and frequent vaso-occlusive
crises, with increased maternal and perinatal morbidity
and mortality (Mattson & Smith, 2004).
Clinical Manifestations
Women with sickle cell anemia present with anorexia, dys-
pnea, malaise, and pallor. If in sickle cell crisis, the woman
will report severe abdominal pain, muscle spasms, leg
pains, joint pain, fever, stiff neck, nausea and vomiting,
and seizures (McCann, 2004).
Treatment
Ideally, women with hemoglobinopathies are screened
before conception and are made aware of the risks of
sickle cell anemia to themselves and to the fetus. A blood
Hgb electrophoresis is done for all women from high-
risk ancestry at their first prenatal visit to determine the
types and percentages of Hgb present. This informa-
tion should help them in making future reproductive
decisions.
Treatment depends on the health status of the woman.
During pregnancy, only supportive therapy is used: blood
transfusions for severe anemia, analgesics for pain, and
antibiotics for infection.
Nursing Management
Clients require emotional support, education, and follow-
up care to deal with this chronic condition, which has a
great impact on them and their families. Nursing care of
women with sickle cell anemia includes:
•
Educate the client to avoid infection exposure, ciga-
rette smoking, alcohol consumption, and temperature
extremes.
•
Monitor laboratory test results.
•
Assess hydration status at each visit and urge the
client to drink 8 to 10 glasses of fluid daily to prevent
dehydration.
•
Monitor vital signs, fetal heart rate, weight gain, and
fetal growth.
•
Assess for early signs of crisis.
•
Schedule frequent fetal well-being assessments, such
as biophysical profiles, nonstress tests, and contraction
stress tests.
•
Encourage rest and pain management during labor.
•
Prevent infection during the postpartum period by metic-
ulous handwashing.
•
Discuss family planning options to control fertility.
Infections
A wide variety of infections can affect the progression
of pregnancy, possibly having a negative impact on the
outcome. The effect of the infection depends on the
timing of the infection, the body systems involved, and
the severity of the infection. Common viral infections
include cytomegalovirus (CMV), rubella, herpes sim-
plex, hepatitis B, varicella, parvovirus B19, and several
sexually transmitted infections (Table 20-3). Toxoplas-
mosis and group B Streptococcus are common nonviral
infections. Only the most common infections will be
discussed here.
Cytomegalovirus
Cytomegalovirus (CMV) is the most common congen-
ital and perinatal viral infection in the world, possibly
affecting up to 3% of all newborns (Damato & Winnen,
2002). Pregnant women acquire active disease primar-
ily from sexual contact, blood transfusions, kissing, and
contact with children in daycare centers. The virus can
be found in virtually all body fluids. Prevalence rates in
women in the United States range from 50% to 85%
(Damato & Winnen, 2002). CMV infection during preg-
nancy may result in abortion, stillbirth, low birthweight,
IUGR, microcephaly, deafness, blindness, mental retar-
dation, jaundice, or congenital or neonatal infection. If
the first or primary infection occurs during pregnancy,
the fetus has a 40% to 50% chance of being infected.
Primary CMV is the most dangerous to the fetus (Gibbs
et al., 2004).
Nursing Management
Most women are asymptomatic and don’t know they have
been exposed to CMV. Symptoms of CMV in the fetus
and newborn include IUGR, microcephaly, hearing loss,
chorioretinitis, and mental retardation (London et al.,
2003). Since no therapy prevents or treats CMV infec-
tions, nurses have a responsibility for educating and sup-
porting childbearing women at risk for CMV infection
562
Unit 7
CHILDBEARING AT RISK
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 562
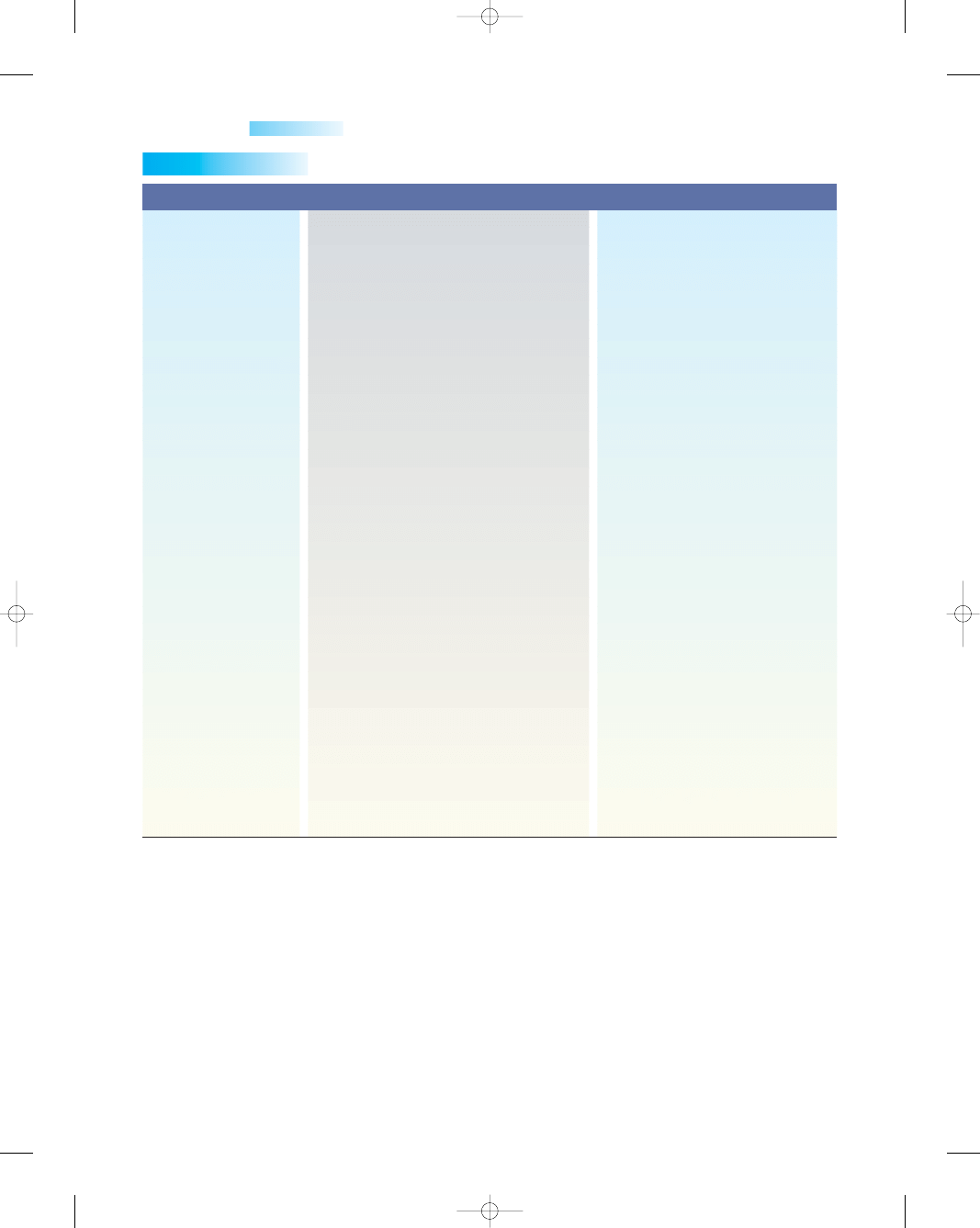
during the perinatal period. Stressing the importance of
good handwashing and use of sound hygiene practices can
help to reduce transmission of the virus to a woman who
could pass the virus on to her fetus.
Rubella
Rubella, commonly called German measles, is spread by
droplets or through direct contact with a contaminated
object. The risk of a pregnant woman transmitting this
virus through the placenta to her fetus increases the earlier
her exposure to the virus. When infections occurs within
the first month after conception, 50% of fetuses show signs
of infection; in the second month following conception,
25% of fetuses will be infected; and in the third month,
10% of fetuses will be affected (Youngkin & Davis, 2004).
Nursing Management
Ideally, all women have been vaccinated and have ade-
quate immunity against rubella. However, all women are
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
563
Table 20-3
Infection/Organism
Effect on Pregnancy and Fetus/Newborn
Implications
Syphilis (
Treponema
pallidum)
Gonorrhea (
Neisseria
gonorrhoeae)
Chlamydia (
Chlamydia
trachomatis)
Human papillomavirus
(HPV)
Trichomonas
(
Trichomonas
Vaginalis)
Maternal infection increases risk of
premature labor and birth.
Newborn may be born with congenital
syphilis—jaundice, rhinitis, anemia, IUGR,
and CNS involvement.
Majority of women are asymptomatic.
It causes ophthalmia neonatorum in the
newborn from birth through infected
birth canal.
Majority of women are asymptomatic.
Infection is associated with infertility and
ectopic pregnancy, spontaneous
abortions, preterm labor, premature
rupture of membranes, low birthweight,
stillbirth, and neonatal mortality.
Infection is transmitted to newborn through
vaginal birth.
Neonate may develop conjunctivitis or
pneumonia.
Infection causes warts in the anogenital
area, known as condylomata
acuminata.
These warts may grow large enough to
block a vaginal birth.
Fetal exposure to HPV during birth is
associated with laryngeal papillomas.
Infection produces itching and burning,
dysuria, strawberry patches on cervix,
and vaginal discharge.
Infection is associated with premature
rupture of membranes and preterm
birth.
All pregnant women should be
screened for this STI and treated
with benzathine penicillin G
2.4 million units IM to prevent
placental transmission.
All pregnant women should be
screened at first prenatal visit,
with repeat screening in the third
trimester.
All newborns receive mandatory eye
prophylaxis with tetracycline or
erythromycin within the first hour
of life.
Mother is treated with ceftriaxone
(Rocephin) 125 mg IM in single
dose before going home.
All pregnant women should be
screened at first prenatal visit and
treated with erythromycin.
Warts are treated with trichlorocetic
acid, liquid nitrogen, or laser
therapy under colposcopy.
Treatment is with a single 2-g dose of
metronidazole (Flagyl).
Table 20-3
Sexually Transmitted Infections Affecting Pregnancy
Sources: London et al, 2003; O’Toole, 2005; Youngkin and Davis, 2004; Tiller, 2002.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 563
still screened at their first prenatal visit to determine
their status. If her rubella antibody titer is 1:8 or greater,
this proves evidence of immunity. Women who are not
immune should be vaccinated during the immediate post-
partum period so they will be immune before becoming
pregnant again (CDC, 2003). Nurses need to check the
rubella immune status of all new mothers and should
make sure all mothers with a titer of less than 1:8 are
immunized prior to discharge.
Herpes Simplex Virus
Approximately 45 million people are infected with geni-
tal herpes in the United States, and 500,000 new cases
are diagnosed annually. Despite strategies designed to
prevent perinatal transmission, the number of cases of
newborn herpes simplex virus (HSV) continues to rise,
mirroring the rising prevalence of genital herpes infection
in women of childbearing age (Fischer, 2004).
HSV is a DNA virus with two subtypes: HSV-1 and
HSV-2. HSV-1 infections were traditionally associated
with oral lesions (fever blisters), whereas HSV-2 infec-
tions occurred in the genital region. Currently, either
type can be found in either location (Fischer, 2004).
Infection occurs by direct contact of the skin or
mucous membranes with an active lesion. HSV is associ-
ated with infections of the genital tract that when acquired
during pregnancy can result in severe systemic symptoms
in the mother and significant morbidity and mortality in
the newborn (Donahue, 2002). Once the virus enters the
body, it never leaves.
Infants born to mothers with a primary HSV infection
have a 30% to 50% risk of acquiring the infection via peri-
natal transmission near or during birth. Recurrent genital
herpes simplex infections carry a 1% to 3% risk of neo-
natal infection if the recurrence occurs around the time
of vaginal birth (Donahue, 2002). HSV can be vertically
transmitted to the fetus or newborn during the prenatal,
intrapartum, or postpartum periods. Most infants infected
by perinatal transmission are born to mothers with no
evidence of genital herpes lesions, so prevention is a
challenge.
Nursing Management
Nursing management for the woman with genital her-
pes in pregnancy should address the care of the preg-
nant woman as well as reducing the risk of newborn
herpes. Since the majority of newborn herpes results
from perinatal transmission of the virus during vaginal
birth, and because transmission can result in severe neu-
rologic impairment or death, treatment of the mother
with an antiviral agent such as acyclovir must be started
as soon as the culture comes back positive. Universal
screening for herpes is not economically sound, so nurses
need to remain knowledgeable about current practice
to be able to provide accurate and sensitive care to all
women.
Hepatitis B Virus
Hepatitis B virus (HBV) is one of the most prevalent
chronic diseases in the world. HBV can be transmitted
through contaminated blood, illicit drug use, blood prod-
ucts, and sexual contact. The virus is 100 times more
infectious than HIV and, unlike HIV, it can live outside
the body in dried blood for more than a week (Lin &
Kirchner, 2004).
Sexual transmission accounts for most adult HBV
infections in the United States. Acutely infected women
develop hepatitis with anorexia, nausea, vomiting, fever,
abdominal pain, and jaundice. In women with acute
hepatitis B, vertical transmission occurs in approximately
10% of newborns when infection occurs in the first
trimester and in 80% to 90% of newborns when acute
infection occurs in the third trimester (Landon, 2004).
Women at greatest risk for contracting HBV infec-
tion include those with:
•
A history of sexually transmitted infections
•
Household contacts of HBV-infected persons
•
Jobs as healthcare workers
•
Intravenous drug abuse
•
Multiple sexual partners
•
Chinese, Southeast Asian, or African heritage
•
Partners who are HBV infected (CDC, 2005)
Women who work as prostitutes or are foreign-born
also are at high risk for contracting HBV (CDC, 2005).
Hepatitis B infection during pregnancy is associated
with an increased risk of preterm birth, low birthweight,
and neonatal death. Newborns infected with HBV are
likely to become chronic carriers of the virus, becoming
reservoirs for continued infection in the population (CDC,
2005). The fetus is at risk primarily at birth because of the
possible contact with contaminated blood at this time.
Nursing Management
Screen for hepatitis B surface antigen (HbsAg) via blood
studies in all pregnant women at their first prenatal visit.
Repeat this screening later in pregnancy for women in
high-risk groups (Youngkin & Davis, 2004). If positive,
expect to administer HBV immune globulin (HBIG, Hep-
B-Gammagee) followed by HBV vaccine (Recombivax-
HB, Engerix-B) to the newborn within 12 hours of birth.
The second and third doses of the vaccine are given at
1 month and 6 months of age (CDC, 2005). The CDC
recommends routine vaccination of all newborns.
Women who are HbsAg negative may be vaccinated
safely during pregnancy. No current research supports the
use of surgical births to reduce vertical transmission of
HBV. In addition, breastfeeding by mothers with chronic
HBV infection does not increase the risk of viral transmis-
sion to their newborns (Lin & Kirchner, 2004).
HBV can be prevented through safer sex practices,
good handwashing technique, and the use of standard
564
Unit 7
CHILDBEARING AT RISK
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 564
precautions with all body fluid contact. Client educa-
tion is essential (Teaching Guidelines 20-4). Protection
can be afforded with the highly effective hepatitis B
vaccine.
Treatment for hepatitis B rarely produces permanent
remission of the disease. Therefore, the goals of therapy
are long-term suppression of viral replication and pre-
vention of end-stage liver disease. Urge the woman to
consume a high-protein diet and avoid fatigue. A healthy
lifestyle can help delay disease progression. Initiate an
open discussion about the modes of transmission and use
of condoms to prevent spread.
Varicella Zoster virus
Varicella zoster virus (VZV) is a member of the herpesvirus
family and is the virus that causes both varicella (chicken-
pox) and herpes zoster (shingles). Pregnant women are
at risk for developing varicella when they come in close
contact with children who have active infection. Maternal
varicella can be transmitted to the fetus through the pla-
centa, leading to congenital varicella, via an ascending
infection during birth, or by direct contact with infectious
lesions, leading to infection after birth. Varicella occurs in
approximately 1 to 7 of 10,000 pregnancies (Anderson &
Safdar, 2005).
Congenital varicella syndrome can occur among new-
borns of mothers infected during early pregnancy. It is
characterized by low birthweight, spontaneous abortion,
chorioretinitis, cataracts, cutaneous scarring, limb hypo-
plasia, microcephaly, ocular abnormalities, mental retar-
dation, and early death (Laartz & Gompf, 2004).
Nursing Management
Nursing management focuses on prevention of this con-
dition through preconception counseling. This counsel-
ing also should include determining the woman’s vari-
cella immunity; the vaccine is administered if needed.
Alert women in occupations that increase the risk of
exposure to the virus: daycare workers, teachers of young
children, and staff caring for children in institutional
settings.
Parvovirus B19
Parvovirus B19 is a common, self-limiting benign child-
hood virus that causes erythema infectiosum, also known
as fifth disease (McCarter-Spaulding, 2002). The preva-
lence of this virus among pregnant women and fetuses
is not known. The infection is spread transplacentally,
by the oropharyngeal route in casual contact, and through
infected blood. Approximately 50% to 65% of women
of reproductive age have developed immunity to par-
vovirus B19.
Acute infection in pregnancy can cause B19 infection
in the fetus, leading to nonimmune fetal hydrops secondary
to severe anemia or fetal loss, depending on the gestational
age at the time of infection. The risk to the fetus is greatest
when the woman is exposed and infected in the first
20 weeks of gestation. In addition to hydrops, other fetal
effects of parvovirus include spontaneous abortion, con-
genital anomalies (CNS, craniofacial, and eye), and long-
term effects such as hepatic insufficiency, myocarditis, and
learning disabilities (Cunningham & Rennels, 2004).
Clinical Manifestations
The characteristic rash starts on the face with a “slapped-
cheeks” appearance. The rash is followed by a generalized
maculopapular rash. Fever, arthralgia, and generalized
malaise are usually present in the mother.
Treatment
Generally, diagnosis of parvovirus is based on clinical
symptoms and serologic antibody testing for parvovirus
immunoglobulin G and parvovirus immunoglobulin M
(IgM). Schoolteachers, daycare workers, and women liv-
ing with school-aged children are at highest risk for being
seropositive for parvovirus B19, especially if a recent out-
break has occurred in those settings. Pregnant women who
have been exposed to or who develop symptoms of par-
vovirus B19 require assessment to determine whether they
are susceptible to infection (nonimmune). If the woman is
immune, she can be reassured that she will not develop
infection and that the virus will not adversely affect her
pregnancy. If she is nonimmune, then referral to a perina-
tologist is recommended and counseling regarding the
risks of fetal transmission, fetal loss, and hydrops is neces-
sary. The likelihood of a healthy outcome is very high after
parvovirus B19 infection in pregnancy. Because most
pregnant women who become infected are asymptomatic,
it is difficult to determine the risk of fetal infection. The
infected newborn is assessed for any anomaly and followed
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
565
T E A C H I N G G U I D E L I N E S 2 0 - 4
Teaching to Prevent Hepatitis B Virus
•
Abstain from alcohol.
•
Avoid intravenous drug exposure or sharing
of needles.
•
Encourage all household contacts and sexual
partners to be vaccinated.
•
Receive immediate treatment for any sexually
transmitted infection.
•
Know that your newborn will receive the hepatitis B
vaccine soon after birth.
•
Use good handwashing techniques at all times.
•
Avoid contact with blood or body fluids.
•
Use barrier methods such as condoms during sexual
intercourse.
•
Avoid sharing any personal items, such as razors,
toothbrushes, or eating utensils.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 565
for up to 6 years to identify any sequelae (Cunningham &
Rennels, 2004).
Nursing Management
Prevention is the best strategy. Stress the need for hand-
washing after handling children; cleaning toys and surfaces
that children have been in contact with; and avoiding the
sharing of food and drinks (McCarter-Spaulding, 2002).
Group B
Streptococcus
Group B Streptococcus is a naturally occurring bacterium
found in the human body that can cause sepsis in new-
borns. It is rarely serious in adults but can be life-
threatening to newborns. It colonizes in the rectum,
vagina, urethra, and cervix of women. Genital tract col-
onization poses the most threat to the newborn because
of exposure during birth and to the mother because of
ascending infection after the membranes rupture.
Group B Streptococcus affects about 1 in every 2,000
newborns in the United States (March of Dimes, 2004).
If a pregnant woman carries the bacterium in her vagina
or rectum during labor, there is a 1-in-100 chance that her
newborn will become ill from a group B streptococcal
infection. The risk rises to 4% if the woman has a preterm
birth, prolonged rupture of membranes (>18 hours), or
fever (100.4
°F or higher) during labor. It is thought that
newborns who become ill with group B streptococcal
infection take the bacterium into their bodies by ingesting
infected amniotic fluid or vaginal fluids during birth
(Narayanan & Ossiani, 2004).
Clinical Manifestations
Most often, women with group B streptococcal infection
are asymptomatic. However, many present with urinary
tract infections, uterine infections, and chorioamnionitis.
Newborns with early-onset (within a week after birth)
group B streptococcal infections may have pneumonia or
sepsis, whereas late-onset (after the first week) infections
often manifest with meningitis (CDC, 2002).
Treatment
Antibiotic therapy usually is effective in treating women
with infections of the urinary tract or uterus, or chorio-
amnionitis without any sequelae. According to the 2002
CDC guidelines, all pregnant women should be screened
for group B Streptococcus at 35 to 37 weeks’ gestation. The
recommendation resulted from ACOG’s review of the lat-
est data, which compared a risk-based versus a screening
approach. Vaginal and rectal specimens are cultured for
the presence of the bacterium. If positive, the woman
should be treated with intravenous antibiotics during
labor. A recent CDC study (2002) suggested that this
approach may prevent nearly 90% of early-onset group B
streptococcal infections.
Treatment of group B streptococcal infection includes
penicillin G because of its narrow spectrum, with alterna-
tive antibiotics prescribed for clients with a penicillin
allergy. The drug is usually administered intravenously at
least 4 hours before birth so that it can reach adequate lev-
els in the serum and amniotic fluid to reduce the risk of
newborn colonization. Close monitoring is required dur-
ing the administration of intravenous antibiotics because
severe allergic reactions can occur rapidly.
Nursing Management
Nurses can assume the role of educator and advocate for
all women and newborns to reduce group B streptococ-
cal infections. When obtaining the woman’s prenatal his-
tory, ask about any previous infection, and document this
information to help prevent vertical transmission to the
newborn. All women with a previous group B strepto-
coccal infection during pregnancy should be treated with
intravenous antibiotics during labor. Also ensure that
pregnant women between 35 and 37 weeks’ gestation are
screened for group B streptococcal infection during their
prenatal visit. Record the results and notify the birth
attendant that the woman has tested positive for group B
Streptococcus.
Toxoplasmosis
Toxoplasmosis is a relatively widespread parasitic infec-
tion caused by a one-celled organism, Toxoplasma gondii.
When a pregnant woman is exposed to this protozoan,
the infection can pose serious risks to her fetus. Between
1 in 1,000 and 8,000 newborns are born infected with
toxoplasmosis in the United States (Gibbs et al., 2004).
It is transferred by hand to mouth after touching cat
feces while changing the cat litter box or through gar-
dening in contaminated soil. Consuming undercooked
meat, such as pork, lamb, or venison, can also transmit
this organism.
A pregnant woman who contracts toxoplasmosis for
the first time has approximately a 40% chance of pass-
ing the infection to her fetus (March of Dimes, 2005).
Although the woman typically remains asymptomatic,
transmission to her fetus can occur throughout preg-
nancy, the most severe being prior to the third trimester.
A fetus who contracts congenital toxoplasmosis typically
has a low birthweight, enlarged liver and spleen, choriore-
tinitis, jaundice, neurologic damage, and anemia (London
et al., 2003).
Treatment of the woman during pregnancy to reduce
the risk of congenital infection is a combination of pyri-
methamine and sulfadiazine. Treatment with sulfonamides
during pregnancy has been shown to reduce the risk of
congenital infection.
Nursing Management
Prevention is the key to managing this infection. Nurses
play a key role in educating the woman in measures to
prevent toxoplasmosis (Teaching Guidelines 20-5).
566
Unit 7
CHILDBEARING AT RISK
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 566
Special Populations at Risk
Every year there are an estimated 210 million pregnan-
cies worldwide, with about 6 million of them in the
United States (Alan Guttmacher Institute, 2004). Each
pregnancy runs the risk of an adverse outcome for the
mother and the baby. Risks are dramatically increased
for certain populations: adolescents, women who are HIV
positive, older women, and substance abusers. While
risks cannot be totally eliminated once pregnancy has
begun, they can be reduced through appropriate and
timely interventions.
Every woman’s experience with pregnancy is unique
and personal. The circumstances each one faces and what
pregnancy means to her involve emotions and experiences
that belong solely to her. Many women in these special
population groups go through this experience in confu-
sion and isolation, feeling desperately in need of help but
not knowing where to go. Although all pregnant women
experience these emotions to a certain extent, they are
heightened in women who have numerous psychosocial
issues. Pregnancy is a stressful time. Pregnant women face
wide-ranging changes in their lives, relationships, and
bodies as they move toward parenthood. These changes
can be challenging for a woman without any additional
stresses but are even more so in the face of age extremes,
illness, or substance abuse.
Skilled nursing interventions are essential to promote
the best outcome for the client and her baby. Timely sup-
port and appropriate interventions during the perinatal
period can have long-standing implications for the mother
and her newborn, ultimately with the goal of stability and
integration of the family as a unit.
Pregnant Adolescent
Adolescence
spans the time frame from the onset of
puberty to the cessation of physical growth, roughly from
11 to 19 years of age. Adolescents vacillate between being
children and being adults. They need to adjust to the phys-
iologic changes their bodies are undergoing and establish
a sexual identity during this time. They search for personal
identity and desire freedom and independence of thought
and action. However, they continue to have a strong
dependence on their parents (O’Toole, 2005).
Developmental Tasks of Adolescence
Certain developmental tasks need to be accomplished dur-
ing this period before an adolescent can advance to the
next stage of maturity. The developmental tasks of adoles-
cents include:
•
Seeking economic and social stability
•
Developing a personal value system
•
Building meaningful relationships with others (Fig. 20-3)
•
Becoming comfortable with their changing bodies
•
Working to become independent from their parents
•
Learning to verbalize conceptually (Bayley, 2003)
Adolescents have special needs related to their lifestyle
to accomplish their developmental tasks in making a
smooth transition to young adulthood. One of the biggest
areas of need is sexual health. Adolescents commonly lack
the information, skills, and services necessary to make
informed choices related to their sexual and reproductive
health. As a result of these issues, unplanned pregnancies
occur. When they do, achievement of their develop-
mental tasks, especially identity, often is interrupted as the
adolescent attempts to integrate the tasks of pregnancy,
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
567
T E A C H I N G G U I D E L I N E S 2 0 - 5
Teaching to Prevent Toxoplasmosis
•
Avoid eating raw or undercooked meat, especially
lamb or pork. Cook all meat to an internal
temperature of 160
°F throughout.
•
Clean cutting boards, work surfaces, and utensils with
hot soapy water after contact with raw meat or
unwashed fruits and vegetables.
•
Peel or thoroughly wash all raw fruits and vegetables
before eating them.
•
Wash hands thoroughly with warm water and soap
after handling raw meat.
•
Avoid feeding the cat raw or undercooked meats.
•
Avoid emptying or cleaning the cat’s litter box. Have
someone else do it daily.
•
Keep the cat indoors to prevent it from hunting and
eating birds or rodents.
•
Avoid uncooked eggs and unpasteurized milk.
•
Wear gardening gloves when in contact with
outdoor soil.
•
Avoid contact with children’s sandboxes, because cats
can use them as litter boxes.
●
Figure 20-3
Adolescents sharing time and developing
relationships.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 567
bonding, and preparing to care for another with the tasks
of developing self-identity and independence. The process
of learning how to separate from the parents while learn-
ing how to bond and attach to a newborn brings conflict
and stress.
Adolescents have difficulty coping with and accom-
plishing their developmental tasks of identity formation
and autonomy. Developmentally, adolescents are trying
to figure out who they are and how they fit into society.
As they mature, parents become less influential and peers
become increasingly influential. Peer pressure and the
desire to please their peers can influence adolescents to
participate in behaviors in which they might normally not
be involved. In addition, the onset of sexual maturation
and the adolescent’s belief that “it won’t happen to me”
contribute to high-risk behaviors.
The younger the adolescent is at the time of the first
pregnancy, the more likely it is that she will have another
pregnancy during her teens (Montgomery, 2003). In addi-
tion, a pregnancy can exacerbate an adolescent’s feeling of
loss of control (Youngkin & Davis, 2004). Healthcare
providers must be able to communicate with adolescents
in a manner they can understand, and respect them as
unique individuals.
Incidence of Adolescent Pregnancy
The incidence of teenage pregnancy has steadily declined
since the early 1990s, but it is still higher in the United
States than in any other industrialized country (Green &
Wilkinson, 2004). Even this reduced incidence repre-
sents what is considered an unacceptably high level of
pregnancy in an age group that is likely to suffer the social
consequences of early pregnancy most. Subsequently,
adolescent pregnancy is considered a major health prob-
lem and is addressed in Healthy People 2010.
Each year in the United States, approximately 1 mil-
lion adolescents, or 10% of girls between the ages of 15
to 19 years, become pregnant. These pregnancies, which
account for 13% of all births, are typically unintended and
occur outside of marriage (Alan Guttmacher Institute,
2004). In addition, about half of all teen pregnancies occur
within 6 months of first having sexual intercourse. Of girls
who become pregnant, one in six will have a repeat preg-
nancy within 1 year. Most of these girls are unmarried, and
many are not ready for the emotional, psychological, and
financial responsibilities of parenthood (Lowdermilk &
Perry, 2004). Adolescent pregnancy is further complicated
by the adolescent’s lack of financial resources: the income
of teen mothers is half that for women who have given
birth in their 20s (Farrington, 2003).
Impact of Pregnancy on Adolescents
Adolescent pregnancy is a complex issue. Risk factors
that contribute to adolescent pregnancy might include:
•
Early menarche
•
Peer pressure to become sexually active
•
Sexual or other abuse as a child
•
Lack of accurate contraceptive information
•
Fear of telling parents of sexual activity
•
Feelings of invulnerability
•
Poverty (85% of births occur in poor families)
•
Culture or ethnicity (high incidence in Hispanic and
African-American girls)
•
Unprotected sex
•
Low self-esteem and inability to negotiate
•
Lack of appropriate role models
•
Strong need for someone to love
•
Drug use, truancy from school, or other behavioral
problems
•
Wish to escape a bad home situation
•
Early dating without supervision (Koshar, 2001)
Adolescent pregnancy has a negative impact in terms
of both health and social consequences. For example,
seven out of ten adolescents will drop out of school. More
than 75% will receive public assistance within 5 years of
having their first child. In addition, children of adolescent
mothers are at greater risk of preterm birth, low birth-
weight, child abuse, neglect, poverty, and death (As-Sanie
et al., 2004). The psychosocial risks associated with early
childbearing often have an even greater impact on mothers,
families, and society than the obstetric or medical risks
(Pollard, 2003).
Pregnant adolescents also experience higher rates of
domestic violence and substance abuse. Those experienc-
ing abuse are more likely to abuse substances, receive in-
adequate prenatal care, and have lower pregnancy weight
compared with those who are not (Harner, 2004). More-
over, substance abuse (cigarettes, alcohol, or illicit drugs)
can contribute to low birthweight, IUGR, preterm births,
newborn addiction, and sepsis (Montgomery, 2003).
568
Unit 7
CHILDBEARING AT RISK
HEALTHY PEOPLE
2010
National Health Goals Related to
Adolescent Pregnancy
Objective
Significance
Reduce pregnancy among
adolescent females
from a baseline of
68 pregnancies per
1,000 adolescent girls to
43 pregnancies per
1,000 adolescent girls
USDHHS, 2000.
Will help to foster a
continued decline in
adolescent pregnancy
rates by focusing on
interventions related
to pregnancy preven-
tion, including safe
sex practices and
teaching about the
complications associ-
ated with adolescent
pregnancy
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 568
Although early childbearing (12 to 19 years of age)
occurs in all socioeconomic groups, it is more prevalent
among poor women and those from minority backgrounds,
who face more obstetric and newborn risks than their more
affluent counterparts (Koniak-Griffin & Turner-Pluta,
2001). Poverty often contributes to delayed prenatal care
and medical complications related to poor nutrition, such
as anemia.
The financial burden of adolescent pregnancy is high
and costs taxpayers an estimated $7 billion to $15 billion
annually in the United States (McKinney et al., 2005).
Much of the expense stems from Medicaid, food stamps,
state health department maternity clinics, Aid to Families
and Children, and direct payments to healthcare providers.
However, this amount does not address the potential
costs to society in terms of the loss of human resources
and the far-reaching intergenerational effects of adoles-
cent parenting.
For some adolescents, pregnancy may be seen as a
hopeless situation: a grim story of poverty and lost dreams,
of being trapped in a life that was never wanted. Health-
related behaviors, such as smoking, eating habits, sexual
behavior, and help-seeking behaviors, developed during
adolescence often endure into later life (Bayley, 2003).
Additionally, the consequences associated with an adoles-
cent’s less-than-optimal health status at this age due to
pregnancy can ultimately affect her long-term health and
that of her children. However, some adolescents can cre-
ate a happy, stable life for themselves and their children by
facing their challenges and working hard to beat the odds.
Nursing Management
Dealing with the complicated issues of adolescent preg-
nancy can be an emotionally charged situation, laden
with ethical dilemmas and decisions. Topics such as
abstinence, safer sex, abortion, and the decision to have
a child are sensitive issues. Adolescent pregnancy is an
area when a nurse’s moral convictions may influence the
care provided to clients. Nurses need to examine their
own beliefs about teen sexuality to identify personal
assumptions and discuss them. Putting aside one’s moral
convictions may be difficult, but it is necessary when
working with adolescents who might be making deci-
sions about their pregnancies.
Assessment
Assessment of the pregnant adolescent parallels that for
any pregnant woman. However, the nurse also needs to
address specific areas when dealing with pregnant teens.
Areas to assess include:
•
How does the girl see herself in the future?
•
Are realistic role models available to her?
•
How much does she know about child development?
•
What financial resources are available to her?
•
Does she work? Does she go to school?
•
What emotional support is available to her?
•
Can she resolve conflicts and manage anger?
•
What does she know about health and nutrition for her-
self and her child?
•
Will she need help dealing with the challenges of the new
parenting role?
•
Does she need information about community resources?
Having an honest regard for adolescents requires get-
ting to know them and being able to appreciate the impor-
tant aspects of their life. Doing so forms a basis for the
nurse’s clinical judgment and promotes care that takes
into account the concerns and practical circumstances of
the teen and her family. Skillful practice includes know-
ing how and when to advise a teen and when to listen and
refrain from giving advice. Giving advice can be misinter-
preted as “preaching,” and the adolescent will probably
ignore the information. The nurse must be perceptive,
flexible, and sensitive and must work to establish a thera-
peutic relationship.
Nursing Interventions
For adolescents, as for all women, pregnancy can be a
physically, emotionally, and socially stressful time. The
pregnancy is often both the result of and cause of social
problems and stressors that can be overwhelming to them.
Nurses must support them during the transition from
childhood into adulthood, which is complicated by their
emergence into motherhood. Stress that the girl’s physi-
cal well-being is significant for both her and her develop-
ing fetus, which depends on her for its own health-related
needs. Monitor weight gain, sleep and rest patterns,
and nutritional status to promote positive outcomes for
both. Having a healthy newborn eases the transition
to motherhood somewhat, rather than having to deal
with the added stress of caring for an unhealthy baby
(Harner, 2004).
Help the adolescent identify the options for this preg-
nancy, such as abortion, self-parenting of the child, tem-
porary foster care for the baby or herself, or placement of
the child for adoption. Explore with the adolescent why
she became pregnant. Awareness of why she decided to
have a child is necessary to help with the development of
the adolescent and her ability to parent. Identify barriers
to seeking prenatal care such as lack of transportation,
too many problems at home, financial concerns, the long
wait for an appointment, and lack of sensitivity on the
part of the healthcare system.
Key nursing activities appropriate when caring for
pregnant adolescents include:
•
Provide appropriate teaching based on the adolescent’s
developmental level.
•
Encourage the girl to return to school and further
education.
•
Make a referral for career or job counseling.
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
569
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 569

•
Identify and support family and friends who want to
become involved.
•
Assist with arranging foster care, including stress man-
agement and self-care.
•
Stress the importance of attending prenatal education
classes.
•
Monitor maternal and fetal well-being throughout
pregnancy and labor (Fig. 20-4)
•
Stress the importance of continued prenatal and follow-
up care
•
Encourage the girl to set goals and work toward them
for the future.
Nurses can also play a major role in preventing ado-
lescent pregnancies, perhaps by volunteering to talk to
teen groups. Box 20-3 highlights the key areas for teach-
ing adolescents about pregnancy prevention.
Tackling the many issues surrounding adolescent
pregnancy is difficult. Making connections with clients is
crucial regardless of how complex their situation is. The
future challenges nurses to find solutions to teenage preg-
nancies. Nurses must take proactive positions while work-
ing with adolescents, parents, schools, and communities
to reduce the problems associated with early childbearing.
The Pregnant Woman Over Age 35
The term “elderly primip” is used to describe women
ages 35 or older who are pregnant for the first time. A
few decades ago, a woman having a baby after the age of
35 probably was giving birth to the last of several children,
but today she may be having her first. With advances in
technology and the tendency of women to seek career
advancement prior to childbearing, the dramatic increase
in women having first pregnancies after the age of 35 will
likely continue.
Whether childbearing is delayed by choice or by
chance, starting a family at age 35 is different and not
without risks. Women in this age group may already have
chronic health conditions that may put the pregnancy at
risk. In addition, numerous studies have shown that
increasing maternal age is a risk factor for infertility and
spontaneous abortions, gestational diabetes, chronic
hypertension, preeclampsia, preterm labor and birth,
multiple pregnancy, genetic disorders and chromosomal
abnormalities, placenta previa, IUGR, low Apgar scores,
and surgical births (Neumann & Graf, 2003). However,
even though increased age implies increased complica-
tions, most women today who become pregnant after
age 35 have healthy pregnancies and healthy newborns
(March of Dimes, 2004).
Nursing Management
In a woman of this age, a preconception visit is impor-
tant to identify chronic health problems that might affect
the pregnancy and also to address lifestyle issues that
may take time to modify, such as cigarette smoking, poor
nutrition, overweight or underweight, alcohol use, or
illicit drug use. This visit provides the opportunity to
educate the woman about risk factors and provide infor-
mation on how to modify lifestyle habits to improve the
pregnancy outcome.
During routine prenatal visits, the nurse can play a key
role in promoting a healthy pregnancy. Social, genetic, and
environmental factors that are unique to the older preg-
nant women need to be considered and assessed, with
appropriate interventions planned. Although research has
shown increases in preterm labor and births, low-birth-
weight newborns, and operative interventions for older
570
Unit 7
CHILDBEARING AT RISK
●
Figure 20-4
A pregnant adolescent receiving care
during labor.
• High-risk behaviors that lead to pregnancy
• Involvement in programs such as Free Teens, Teen
Advisors, or Postponing Sexual Involvement
• Planning and goal setting to visualize their futures in
terms of career, college, travel, and education
• Choice of abstinence or taking a step back to become
a “second-time virgin”
• Discussions about sexuality with a wiser adult—
someone they respect can help put things in
perspective
• Protection against sexually transmitted infections and
pregnancy if they choose to remain sexually active
• Critical observation and review of peers and friends to
make sure they are creating the right atmosphere for
friendship
• Empowerment to make choices that will shape their
life for years to come, including getting control of their
own lives now
• Appropriate use of recreational time, such as sports,
drama, volunteer work, music, jobs, church activities,
and school clubs (Farrington, 2003)
BOX 20-3
TOPICS FOR TEACHING ADOLESCENTS
TO PREVENT PREGNANCY
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 570
women, many carry their pregnancies to term without
incident (Neumann & Graf, 2003).
Encourage the older woman to plan for the pregnancy
by seeing her healthcare provider before getting pregnant
to discuss preexisting medical conditions, medications,
and lifestyle choices. Also assist the woman with lifestyle
changes so that she can begin pregnancy in an optimal
state of health. For example, if the woman is overweight,
educate her about weight loss so that she can start the
pregnancy at a healthy weight. If the woman smokes,
encourage smoking cessation to reduce the effects of nico-
tine on herself and her fetus. Additional teaching topics for
the older woman to reduce her risks include:
•
Get early and regular prenatal care to ensure the best
possible outcomes.
•
Take a multivitamin containing 400 micrograms of folic
acid daily.
•
Eat a variety of nutritious foods, especially fortified cere-
als, enriched grain products, and fresh fruits and vegeta-
bles, and drink at least six to eight glasses of water daily.
•
Avoid alcohol intake during pregnancy.
•
Avoid exposure to secondhand smoke.
•
Take no drugs unless they are prescribed.
Women Who Are HIV Positive
Human immunodeficiency virus (HIV)
is a retrovirus
that is transmitted by blood and body fluids. The three
recognized modes of HIV transmission are unprotected
sexual intercourse with an infected partner, contact with
infected blood or blood products, and perinatal trans-
mission. HIV is not transmitted by doorknobs, faucets,
toilets, dirty dishes, mosquitoes, wet towels, coughing or
sneezing, shaking hands, or being hugged or by any other
indirect method. The number of people living with HIV
infection in 2004 was estimated at nearly 38 million,
including approximately 20 million women of childbear-
ing age and 2.5 million children, most of whom acquired
HIV from mother-to-child transmission (Mirochnick &
Capparelli, 2004).
The virus attacks the T4 cells, decreases the CD4
cell count, and disables the immune system. The HIV
condition can progress to a severe immunosuppressed state
termed
acquired immunodeficiency syndrome
(AIDS).
AIDS is a progressive, debilitating disease that
suppresses cellular immunity, predisposing the infected
person to opportunistic infections and malignancies. The
CDC defines AIDS as an HIV-infected person with a
specific opportunistic infection or a CD4 count of less
than 200 (Katz, 2003). Eventually, death occurs (Green
& Wilkinson, 2004). The time from infection with HIV
to development of AIDS is a median of 11 years but
varies depending on whether the patient is taking current
antiretroviral therapy (McKinney et al., 2005). Research
indicates that pregnancy does not accelerate the progres-
sion of HIV to AIDS or death (Public Health Service
Task Force, 2002).
Incidence and Prevalence
Despite the revolutionary strides that have been made in
treatment and detection and recent clinical advances and
cautious optimism associated with combination therapies
and potential vaccines, the number of individuals who
are HIV positive continues to climb worldwide. Intensive
efforts notwithstanding, there still remains no real “cure”
on the horizon (Penny, 2003).
Historically, HIV/AIDS was associated with the male
homosexual community and intravenous drug users, but
currently the prevalence of HIV/AIDS is now increasing
more rapidly among women than men (PHSTF, 2002).
Women are the fastest-growing segment of persons becom-
ing infected with HIV; transmission in women occurs
most frequently from sexual contact (64%) and from intra-
venous drug use (33%) (Koniak-Griffin et al., 2003). Most
women, a large number of whom are mothers, have
acquired the disease through heterosexual contact. The risk
of acquiring HIV through heterosexual contact is greater
for women due to exposure to the higher viral concentra-
tion in semen. In addition, sexual intercourse may cause
breaks in the vaginal lining, increasing the chances that
the virus will enter the woman’s body. Fifty percent of
all the HIV/AIDS cases worldwide occur in women. AIDS
is the third leading cause of death among all U.S. women
aged 25 to 44 years and the leading cause of death among
African-American women in this age group (CDC, 2002).
Stages of Infection
Once infected with HIV, the woman develops antibodies
that can be detected with the enzyme-linked immuno-
sorbent assay (ELISA) and confirmed with the Western
blot test. Antibodies develop within 6 to 12 weeks after
exposure, although this latent period is much longer in
some women. Table 20-4 highlights the four stages of
HIV infection according to the CDC (2002).
Perinatal Transmission
Cases of perinatal transmission (mother to fetus or child)
of HIV have decreased in the past several years in the
United States, primarily due to the use of zidovudine
(ZDV) therapy in pregnant women infected with HIV.
This has not been the case in poor countries without sim-
ilar resources. The Joint United Nations programs on
HIV/AIDS (UNAIDS) estimates that over 600,000 new
infections due to mother-to-child transmission occur
annually. This number is expected to increase rapidly as
prevalence rises in Southeast Asia (McIntyre & Gray,
2002). Perinatal transmission rates are as high as 35%
when there is no intervention (antiretroviral therapy) and
below 5% when antiretroviral treatment and appropriate
care are available.
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
571
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 571

With perinatal transmission, approximately 25% to
50% of children manifest AIDS within the first year of life,
and about 80% have clinical symptoms of the disease
within 3 to 5 years (Penny, 2003). Breastfeeding is a major
contributing factor for mother-to-child transmission, and
the infected mother must be informed about this (Bartlett
& Anderson, 2001). Given the devastating effects of HIV
infection on children, preventing its transmission is critical
(Littleton & Engebretson, 2005).
Maternal and Fetal/Newborn Risks
When a woman who is infected with HIV becomes preg-
nant, the risks to herself, her fetus, and the newborn are
great. The risks are compounded by problems such as
drug abuse, lack of access to prenatal care, poverty, poor
nutrition, and high-risk behaviors such as unsafe sex prac-
tices and multiple sex partners, which can predispose the
woman to additional sexually transmitted infections
such as herpes, syphilis, or human papillomavirus (HPV).
Subsequently, pregnant women who are HIV positive are
at risk for preterm delivery, premature rupture of mem-
branes, intrapartal or postpartum hemorrhage, post-
partum infection, poor wound healing, and genitourinary
tract infections (London et al., 2003).
The fetus and newborn also are at risk for prematurity,
IUGR, low birthweight, and infection. Prompt treatment
with antiretroviral medications for the HIV-infected infant
may slow the progression of the disease.
Screening and Diagnosis
Screening only women that are identified as high risk
based on their histories is inadequate due to the prolonged
latency period that can exist after exposure. Also, research
indicating that treatment with antiretroviral agents could
reduce vertical transmission from the infected mother
to the newborn has dramatically increased the impor-
tance of HIV antibody screening in pregnancy. As a result,
the U.S. Public Health Service (USPHS) has recom-
mended that all pregnant women be offered HIV anti-
body testing, regardless of their risk of infection, and
that testing be done during the initial prenatal evalua-
tion (Bartlett & Anderson, 2001). Testing is essential
because treatments are available that can reduce the
likelihood of perinatal transmission and maintain the
health of the woman.
All women who are pregnant or planning a pregnancy
should be offered HIV testing using ELISA. Reactive
screening tests must be confirmed by an additional test,
such as the Western blot or an immunofluorescence assay.
The Western blot is the confirmatory diagnostic test. A
positive antibody test confirmed by a supplemental test
indicates that the woman has been infected with HIV and
can pass it on to others. HIV antibodies are detectable in
at least 95% of women within 3 months after infection
(Lowdermilk & Perry, 2004).
Treatment
Women who are seropositive for HIV should be counseled
about the risk of perinatal transmission and the potential
for obstetric complications. The risk of perinatal transmis-
sion directly correlates with viral load (Minkoff, 2003). A
discussion of the options on continuing the pregnancy,
medication therapy, risks, perinatal outcomes, and treat-
ment is warranted. Women who elect to continue with the
pregnancy should be treated with antiretroviral therapy
regardless of their CD4 count or viral load.
Treatment for pregnant women infected with HIV
focuses on reducing the risk of perinatal transmission by
drug therapy. The standard treatment is oral antiretroviral
drugs given twice daily from 14 weeks’ gestation until
572
Unit 7
CHILDBEARING AT RISK
Table 20-4
Stages
Description
Clinical Picture
I
II
III
IV
Acute infection
Asymptomatic infection
Persistent generalized
lymphadenopathy
End-stage disease (AIDS)
Early stage with pervasive viral production
Flu-like symptoms 2–4 weeks after exposure
Signs and symptoms: weight loss, low-grade fever, fatigue, sore throat, night
sweats, and myalgia
Viral replication continues within lymphatics
Usually free of symptoms; lymphadenopathy
Possibly remaining in this stage for years; AIDS develops in most within
7–10 years
Opportunistic infections occur
Severe immune deficiency
High viral load and low CD4 counts
Signs and symptoms: bacterial, viral, or fungal opportunistic infections,
fever, wasting syndrome, fatigue, neoplasms, and cognitive
changes
Table 20-4
Stages of HIV Infection Outlined by the CDC
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 572
giving birth, intravenous administration during labor, and
oral syrup for the newborn in the first 6 weeks of life (Katz,
2003). The goal of therapy is to reduce the viral load as
much as possible, which reduces the risk of transmission
to the fetus.
Decisions about the birthing method to be used are
made on an individual basis based on several factors involv-
ing the woman’s health status. Some reports suggest that
cesarean birth may reduce the risk of HIV infection
(PHSTF, 2002). Efforts to reduce instrumentation, such
as avoiding the use of an episiotomy, fetal scalp electrodes,
and scalp pH, will assist in reducing the newborn’s expo-
sure to bodily fluids. The Public Health Service recom-
mends that women who are HIV positive should avoid
breastfeeding to prevent HIV transmission to the newborn.
With access to appropriate therapies, the prognosis
for pregnant women with HIV infection has improved
significantly. In addition, the newborns of women with
HIV infection who have received treatment usually do
not become infected.
Unfortunately, therapy is complicated and medica-
tions are expensive. Moreover, the medications are asso-
ciated with numerous adverse effects and possible toxic
reactions. These therapies offer a dual purpose: reduce
the likelihood of mother-to-infant transmission, and pro-
vide optimal suppression of the viral load in the mother.
The core goal of all medical therapy is to bring the client’s
viral load to an undetectable level, thus minimizing the
risk of transmission to the fetus and newborn.
Nursing Management
Women infected with HIV should have comprehensive
prenatal care, which starts with pretest and posttest coun-
seling. In pretest counseling, the client completes a risk
assessment survey and the nurse explains the meaning of
positive versus negative test results, obtains informed
consent for HIV testing, and educates the woman on how
to prevent HIV infection by changing lifestyle behaviors
if needed. Posttest counseling includes informing the
client of the test results, reviewing the meaning of the
results again, and reinforcing safer sex guidelines. All
pretest and posttest counseling should be documented
in the client’s chart.
Assessment
The usual screening tests done in normal pregnancy should
be completed, but with an emphasis on sexually trans-
mitted infections. Women infected with HIV have high
rates of sexually transmitted infections, especially HPV,
vulvovaginal candidiasis, bacterial vaginosis, syphilis, HSV,
chancroid, CMV, gonorrhea, chlamydia, and hepatitis B
(Williams, 2003). If there is no history of hepatitis B, the
woman should receive the hepatitis vaccine, as well as the
pneumococcal vaccine. Close follow-up of suspicious Pap
smear results is prudent because of the increased risk of cer-
vical changes associated with HPV and HIV (Dole, 2001).
Nursing Interventions
Pregnant clients are dealing with many issues at their first
prenatal visit. The confirmation of pregnancy may be
accompanied by feelings of joy, anxiety, depression, or
other emotions. Simultaneously, the client is given many
pamphlets and receives advice and counseling about many
important health issues (e.g., nutrition, prenatal develop-
ment, appointment schedules). This health teaching may
be done while the woman feels excited, tired, and anxious.
To expect women to understand detailed explanations of a
complex disease entity (HIV/AIDS) too may be unrealistic.
Determine the client’s readiness for this discussion.
When providing direct care, follow standard precau-
tions. Identify the client’s individual needs for teaching,
emotional support, and physical care. Approach education
and counseling of HIV-positive pregnant women in a car-
ing, sensitive manner. Address the following information:
•
Infection control issues at home
•
Safer sex precautions
•
Stages of the HIV disease process
•
Treatment modalities for each stage
•
Preventive drug therapies for her unborn infant
•
Symptoms of opportunistic infections
•
Avoidance of breastfeeding
•
Referrals to community counseling and financial aid
•
Client’s support system and potential caretaker
•
Importance of continual prenatal care
•
Well-balanced diet
•
Measures to reduce exposure to infections
Be aware of the psychosocial sequelae of HIV/AIDS. A
diagnosis of HIV can put a woman into an emotional
tailspin, where she is worried about her own health and
that of her unborn infant. She may experience grief,
fear, or anxiety about the future of her children. Along
with the medications that are so important to her health
maintenance, a woman’s mental health needs, family
dynamics, capacity to work, and social concerns also must
be addressed.
Nurses can help women face the reality of the diagno-
sis and the treatment options by first examining their own
beliefs and attitudes toward women who are HIV positive
or have AIDS. Empathy, understanding, caring, and assis-
tance are key to helping the client and her family.
Nurses also need to be informed about HIV infec-
tion and how HIV is transmitted; to share the knowl-
edge they have with all women; and to work to influence
legislators, public health officials, and the entire health
establishment toward policies to address the HIV epi-
demic. Research toward treatment and cure is tremen-
dously important, but the major key to prevention of the
spread of the virus is education. Nurses play a major role
in this education.
Current evidence suggests that cesarean birth per-
formed before the onset of labor and before the rupture
of membranes significantly reduces the rate of perinatal
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
573
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 573
transmission. ACOG recommends that women with HIV
be offered elective cesarean birth to reduce the rate of
transmission beyond that which may be achieved through
antiretroviral therapy. They further suggest that opera-
tive births be performed at 38 weeks’ gestation and that
amniocentesis be avoided to prevent contamination of
the amniotic fluid with maternal blood. Decisions con-
cerning the method of delivery should be based on the
woman’s viral load, the duration of ruptured membranes,
the progress of labor, and other pertinent clinical factors
(USPHSTF, 2004).
After the birth of the newborn, the motivation for tak-
ing antiretroviral medications may be lower, thus affecting
the woman’s compliance with therapy. Encourage the
woman to continue therapy for her own sake as well as that
of the newborn. Nurses can make a difference in helping
women to adhere to their complex drug regimens.
Reinforce family planning methods during this time,
incorporating a realistic view of her disease status. The
use of oral contraceptives with concurrent use of con-
doms is recommended (Katz, 2003). Advise the woman
that breastfeeding is not recommended. Instruct the HIV-
positive woman in self-care measures, including the proper
method for disposing of perineal pads to reduce the risk of
exposing others to infected body fluids. Adhere to standard
precautions when providing direct client care. Finally,
teach the HIV-positive woman the signs and symptoms
of infection in newborns and infants, encouraging her to
report any to the healthcare provider.
The Pregnant Woman
With Substance Abuse
The incidence of substance abuse during pregnancy is
highly variable because most pregnant women are reluc-
tant to reveal the extent of their use.
Perinatal drug
abuse
is the use of alcohol and other drugs among preg-
nant women. The National Institute on Drug Abuse esti-
mates that 6% of the women in the United States have
used illicit drugs while pregnant, including cocaine, mar-
ijuana, heroin, and psychotherapeutic drugs that were
not prescribed by a healthcare professional. More than
18% used alcohol and 21% smoked cigarettes during
their pregnancy (Carter, 2002).
The use of drugs, legal or not, increases the risk of
medical complications in the mother and poor birth out-
comes in the newborn. The placenta acts as an active
transport mechanism, not as a barrier, and thus substances
pass from a mother to her fetus through the placenta,
directly affecting its growth and development.
A woman who claims to have taken no drugs while
pregnant may be unaware that substances such as hair
dye, diet cola, paint, or over-the-counter (OTC) med-
ications for colds or headaches are still considered drugs.
Thus, it is very difficult to get a true picture of the real use
of drugs by pregnant women.
Many drugs are considered to have a teratogenic effect
on growing fetuses. A
teratogen
is any environmental
substance that can cause physical defects in the develop-
ing embryo and fetus. Pregnant women with substance
abuse commonly present with polysubstance abuse, which
is likely to be more damaging than the use of any single
substance. Thus, it is inherently difficult to ascribe a
specific perinatal effect to any one substance (Shieh &
Kravitz, 2002).
Maternal and Fetal Effects
Substance abuse during pregnancy, particularly in the
first trimester, has a negative effect on the health of the
mother and the growth and development of the fetus.
The fetus experiences the same systemic effects as the
mother, but often more severely. The fetus cannot metab-
olize drugs as efficiently as the expectant mother and
will experience the effects long after the drugs have left
the women’s system. Substance abuse during preg-
nancy is associated with preterm labor, abortion, low
birthweight, CNS and fetal anomalies, and long-term
childhood developmental consequences (Littleton &
Engebretson, 2005). Table 20-5 summarizes the effects
of selected drugs during pregnancy.
Impact of Addiction
Addiction is a multifaceted process that is affected by envi-
ronmental, psychological, family, and physical factors.
Women who use drugs, alcohol, or tobacco come from all
socioeconomic backgrounds, cultures, and lifestyles. Risk
factors associated with substance abuse during a preg-
nancy may include low self-esteem, inadequate support
systems, low self-expectations, high levels of anxiety,
socioeconomic barriers, involvement in abusive relation-
ships, chaotic familial and social systems, and a history of
psychiatric illness or depression (Lowdermilk & Perry,
2004). Women often become substance abusers to relieve
their anxieties, depression, and feelings of worthlessness
(Green & Wilkinson, 2004).
Societal attitudes regarding women and substance
abuse may prohibit them from admitting the problem and
seeking treatment. Society sanctions women for failing to
live up to expectations of how a pregnant woman “should”
behave, thereby possibly driving them further away from
the treatment they so desperately need. For many reasons,
pregnant women who abuse substances feel unwelcome in
prenatal clinics or medical settings. Often they seek pre-
natal care late or not at all. They may fear being shamed
or reported to legal or child protection authorities. A non-
judgmental atmosphere and unbiased teaching to all preg-
nant women regardless of their lifestyle is crucial. A caring,
concerned manner is critical to help these women feel
“safe” and respond honestly to assessment questions.
Pregnancy can be a motivator for some who want to
try treatment. The goal of therapy is to help the client deal
574
Unit 7
CHILDBEARING AT RISK
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 574
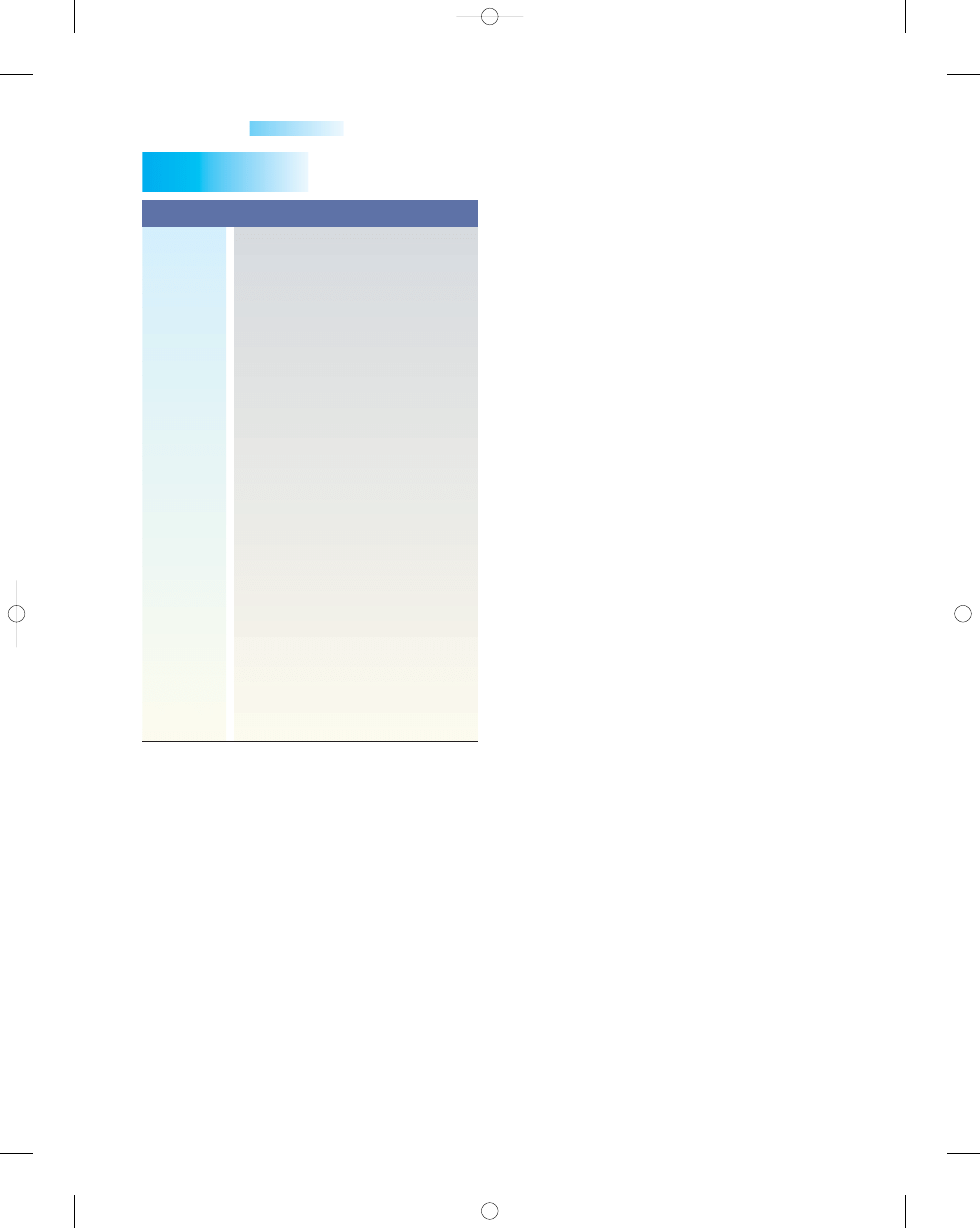
with pregnancy by developing a trusting relationship.
Providing a full spectrum of medical, social, and emotional
care is needed.
Common Substances
Abused During Pregnancy
Alcohol
Alcohol abuse is a major public health issue in the United
States. Alcohol is a teratogen, a substance known to be
toxic to human development. Approximately 10% of preg-
nant women report alcohol consumption (CDC, 2004).
Theoretically, no mother would give a glass of wine, beer,
or hard liquor to her newborn, but when she drinks, her
embryo or fetus is exposed to the same blood alcohol con-
centration as she is. The teratogenic effects of heavy mater-
nal drinking have been recognized since 1973, when fetal
alcohol syndrome was first described. Fetal alcohol syn-
drome is now a classification under the broader term
of
fetal alcohol spectrum disorder;
this disorder
includes the full range of birth defects, such as structural
anomalies and behavioral and neurocognitive disabilities
caused by prenatal exposure to alcohol (Eustace et al.,
2003; Hoyme et al., 2005). Fetal alcohol spectrum disor-
der is completely preventable and is the leading cause of
mental retardation (CDC, 2004).
Not every woman who drinks during pregnancy will
give birth to an affected child. Based on the best research
available, the following is known about alcohol consump-
tion during pregnancy:
•
Intake increases the risk of alcohol-related birth defects,
including growth deficiencies, facial abnormalities,
CNS impairment, behavioral disorders, and intellectual
development.
•
No amount of alcohol consumption is considered safe
during pregnancy.
•
Damage to the fetus can occur at any stage of preg-
nancy, even before a woman knows she is pregnant.
•
Cognitive defects and behavioral problems resulting
from prenatal exposure are lifelong.
•
Alcohol-related birth defects are completely preventable
(USDHHS, 2005).
Risk factors for giving birth to an alcohol-affected
newborn include maternal age, socioeconomic status, eth-
nicity, genetic factors, depression, family disorganization,
unplanned pregnancy, and maternal metabolism (Mattson
& Smith, 2004). Identification of risk factors strongly asso-
ciated with alcohol-related birth outcomes could help
identify high-risk pregnancies requiring intervention.
Characteristics of fetal alcohol spectrum disorder
include craniofacial dysmorphia, IUGR, microcephaly,
and congenital anomalies such as limb abnormalities
and cardiac defects. Long-term sequelae include post-
natal growth restriction, attention deficits, delayed reaction
time, and poor scholastic performance (NoFAS, 2003).
The complex neurobehavioral problems typically manifest
themselves insidiously. Common cognitive and behavioral
problems are listed in Box 20-4.
The child with fetal alcohol spectrum disorder pre-
sents with characteristic facial features (Fig. 20-5) that
include a small head circumference, short palpebral fis-
sures, and small eye openings, a thin upper lip, a receding
jaw, a short nose, a low nasal bridge, a groove between the
nose and the upper lip, skin folds at the corner of the eye
(epicanthal folds), and a small, flat midface area. Minor
ear abnormalities also may be noted (Hoyme et al., 2005).
One of the biggest challenges in determining the true
prevalence of fetal alcohol spectrum disorder is how to rec-
ognize the syndrome, which depends in part on the age
and physical features of the person being assessed.
Difficulty in identifying alcohol abuse is due to the client’s
denial of alcohol use, unwillingness to report alcohol
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
575
Table 20-5
Substance
Effect on Pregnancy
Alcohol
Caffeine
Nicotine
Cocaine
Marijuana
Narcotics
Sedatives
Spontaneous abortion, inadequate
weight gain, IUGR, fetal alcohol
spectrum disorder, the leading
cause of mental retardation
Vasoconstriction and mild diuresis in
mother; fetal stimulation, but
teratogenic effects not
documented via research
Vasoconstriction, reduced
uteroplacental blood flow,
decreased birthweight, abortion,
prematurity, abruptio placentae,
fetal demise
Vasoconstriction, gestational
hypertension, abruptio placentae,
abortion, “snow baby syndrome,”
CNS defects, IUGR
Anemia, inadequate weight gain,
“amotivational syndrome,”
hyperactive startle reflex, newborn
tremors, prematurity, IUGR
Maternal and fetal withdrawal,
abruptio placentae, preterm labor,
premature rupture of membranes,
perinatal asphyxia, newborn sepsis
and death, intellectual impairment,
malnutrition
CNS depression, newborn
withdrawal, maternal seizures in
labor, newborn abstinence
syndrome, delayed lung maturity
Table 20-5
Effects of Selected Drugs
on Pregnancy
Sources: Youngkin and Davis, 2004; McKinney et al., 2005;
London et al., 2003.
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 575
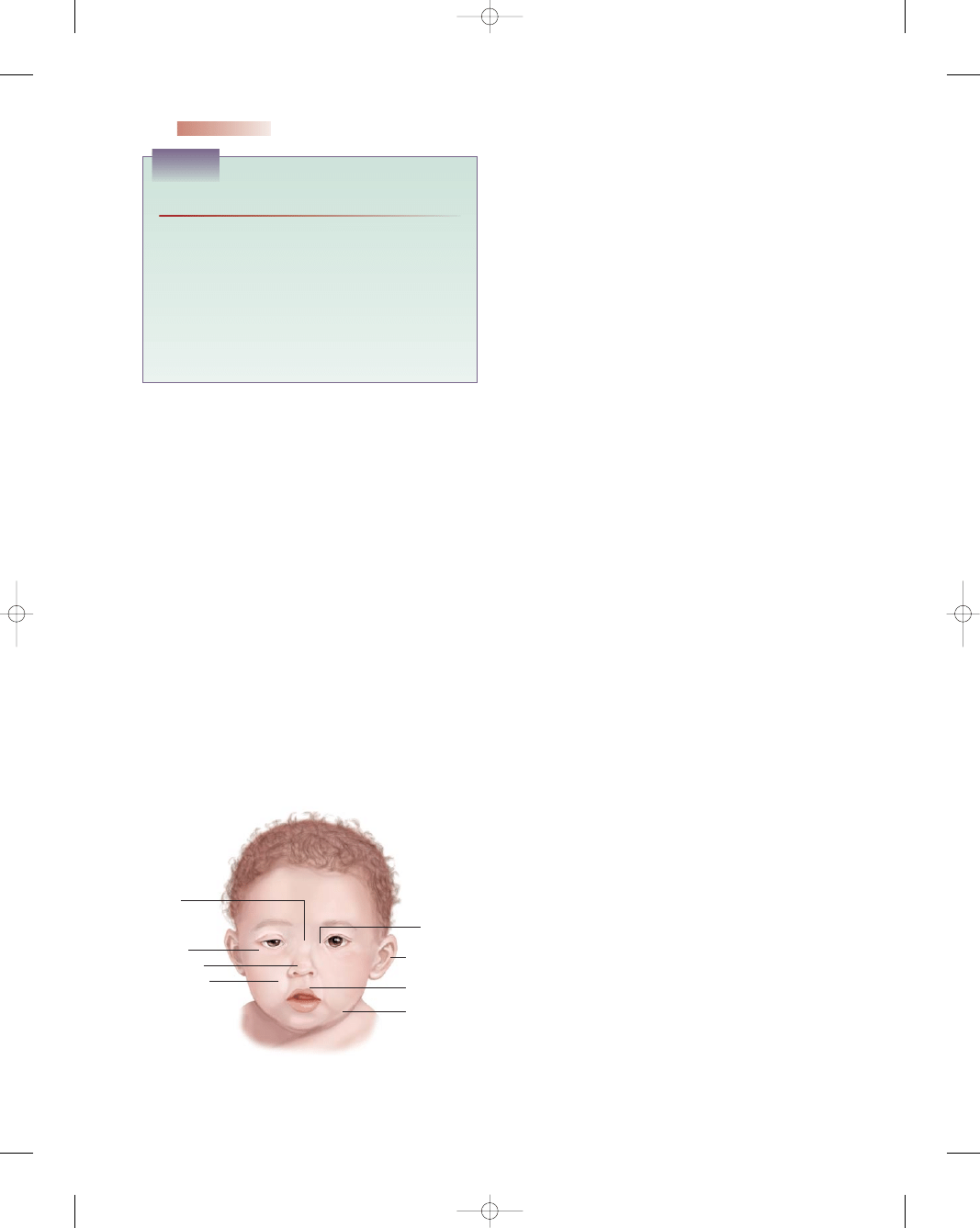
screening questionnaires, such as the Michigan Alcoholism
Screening Test (MAST) and the CAGE Questionnaire,
are not sensitive enough to detect low levels of alcohol
consumption among women. Several challenges remain
for the future in preventing birth defects due to alcohol
consumption:
•
Ways to improve clinical recognition of high-risk women
who drink alcohol
•
Ways to intervene more effectively to modify drinking
behaviors
•
In utero approaches to prevent or minimize fetal injury
•
Strategies to address the neurodevelopmental problems
of children affected by maternal alcohol ingestion
Caffeine
Caffeine is a CNS stimulant and is present in varying
amounts in such common products as coffee, tea, colas,
and chocolate. It is also in cold remedies and analgesics.
Birth defects have not been linked to caffeine consump-
tion, but maternal coffee consumption decreases iron
absorption and may increase the risk of anemia during
pregnancy. The FDA recommends that pregnant women
eliminate or limit their consumption of caffeine to less than
300 mg/day (three cups of coffee or cola) (Lowdermilk &
Perry, 2004).
Nicotine
Nicotine, found in cigarettes, is another substance that is
harmful to the pregnant women and her fetus. Nicotine,
which causes vasoconstriction, transfers across the pla-
centa and reduces blood flow to the fetus, contributing to
fetal hypoxia. When compared with alcohol, marijuana,
and other illicit drug use, tobacco use is less likely to
decline as the pregnancy progresses (Wang, 2004).
Women who smoke during the pregnancy also con-
tinue to smoke after giving birth, and thus the infant will
be exposed to nicotine after birth. This environmental or
passive exposure has an impact on the child’s development
and increases the risk of childhood respiratory disorders.
Smoking increases the risk of spontaneous abortion,
preterm labor and birth, maternal hypertension, placenta
previa, and abruptio placentae. The perinatal death rate
among infants of smoking mothers is 20% to 35% higher
(Gabbe et al., 2002). It has also been considered an impor-
tant risk factor for low birthweight; sudden infant death
syndrome (SIDS); and cognitive deficits, especially in lan-
guage, reading, and vocabulary, as well as poorer perfor-
mances on tests of reasoning and memory. Researchers
have also reported behavior problems, such as increased
activity, inattention, impulsivity, opposition, and aggres-
sion (Wang, 2004).
Cocaine
Cocaine use is second only to marijuana in women who
abuse drugs during pregnancy. The incidence of cocaine
576
Unit 7
CHILDBEARING AT RISK
• Attention-deficit/hyperactivity disorder (ADHD)
• Inability to foresee consequences
• Inability to learn from previous experience
• Lack of organization
• Learning difficulties
• Poor abstract thinking
• Poor impulse control
• Speech and language problems
• Poor judgment
BOX 20-4
COMMON COGNITIVE AND BEHAVIORAL PROBLEMS
ASSOCIATED WITH FETAL ALCOHOL SPECTRUM DISORDER
Low nasal
bridge
Short palpebral
fissures
Short nose
Flat midface
Epicanthal
folds
Minor ear
abnormalities
Thin upper lip
Receding jaw
●
Figure 20-5
Facial characteristics in a newborn with FASD.
consumption, underreporting, and limited ability to recol-
lect the frequency, quantity, and type of alcohol consumed.
This makes it difficult to identify women who are drinking
during pregnancy, institute preventive measures, or refer
them for treatment.
Women who drink excessively while pregnant are at
high risk for giving birth to children with birth defects.
Thus, to prevent these defects, women should stop drink-
ing during all phases of a pregnancy. Unfortunately, many
women continue to drink during their pregnancy despite
warnings from professionals.
Currently, it is not known whether there is a minimal
amount of alcohol safe to drink during pregnancy; an occa-
sional glass of wine might be harmless or might not be.
Therefore, eliminating alcohol consumption during preg-
nancy is the ultimate goal to prevent fetal alcohol spectrum
disorder. Most women know they shouldn’t drink during
pregnancy, but the “window of vulnerability”—the time
lag between conception and the discovery of pregnancy—
may put substantial numbers of children at risk. A multi-
disciplinary approach is key.
A key challenge in screening pregnant women for
alcohol use arises from the fact that traditional alcohol-
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 576
exposure in utero is 1 to 10 per 1,000 live births (Weekes
& Lee, 2004).
Cocaine is a psychoactive drug derived from the leaves
of the coca plant, which grows in the Andes Mountains of
Peru, Ecuador, and Bolivia. The freebase form, called
“crack” because of the cracking or popping noise made in
its preparation, is less expensive, easily made, and smok-
able. Cocaine is a powerful vasoconstrictor. When sniffed
into the mucous membranes of the nose, it produces an
intense “rush” that some have compared to an orgasmic
experience (Sloane, 2002). Smoked crack is absorbed
rapidly by the pulmonary vasculature and reaches the
brain’s circulation in 6 to 8 seconds (Weekes & Lee, 2004).
Cocaine use produces vasoconstriction, tachycardia,
and hypertension in both the mother and the fetus
(Weekes & Lee, 2004). Uteroplacental insufficiency may
result from reduced blood flow and placental perfu-
sion. Chronic use can result in low birthweight, the most
common effect of cocaine use in pregnancy (Littleton &
Engebretson, 2005).
Studies suggest that perinatal cocaine use increases
the risk of preterm labor, abortion, abruptio placentae,
IUGR, intrauterine fetal distress and demise, seizures,
withdrawal, and cerebral infarcts. Cocaine may increase
the risk of uterine rupture and congenital anomalies
(London et al., 2003). Some infants exposed to cocaine
in utero show increased irritability and are difficult to
calm and soothe to sleep.
Other fetal anomalies associated with cocaine use in
early pregnancy involve neurologic problems such as neural
tube defects and microcephaly; cardiovascular anomalies
such as congenital heart defects; genitourinary condi-
tions such as prune belly syndrome, hydronephrosis, and
ambiguous genitalia; and gastrointestinal system problems
such as necrotizing enterocolitis (Mattson & Smith, 2004).
Marijuana
Marijuana is the most commonly used illicit drug in
America, with about 83 million people having tried it at
least once. It is often called pot, reefer, grass, weed, herb,
Mary Jane, or MJ (Mattson & Smith, 2004). Marijuana is
a preparation of the leaves and flowering tops of Cannabis
sativa, the hemp plant, which contains a number of phar-
macologically active agents. Tetrahydrocannabinol (THC)
is the most active ingredient of marijuana. With heavy
smoking, THC narrows the bronchi and bronchioles
and produces inflammation of the mucous membranes.
Smoking marijuana causes tachycardia and a reduction
in blood pressure, resulting in orthostatic hypotension.
Marijuana is not considered teratogenic, but many
newborns display altered responses to visual stimuli,
increased tremulousness, and a high-pitched cry, which
might indicate CNS insults (Wang, 2004). The effects of
marijuana smoking on pregnancy are not yet fully under-
stood because there are very few studies on its long-term
effects on child development. One can speculate that the
effects of marijuana on the immature nervous system may
be subtle and not detected until more complex functions
are required, usually in a formal educational setting. There
is some evidence that marijuana increases the risk of
spontaneous abortion and preterm delivery (O’Toole,
2003). Use of marijuana is highly correlated with use of
alcohol and cigarettes.
Opiates and Narcotics
Opiates and narcotics include opium, heroin (known
as horse, junk, smack, downtown), morphine, codeine,
hydromorphone (Dilaudid; little D), oxycodone (Per-
codan, perkies), meperidine (Demerol, demise), and
methadone (meth, dollies). These drugs are CNS depres-
sants that soothe and lull. They may be used medically
for pain, but all have a high potential for abuse. Most
cause an intense addiction in both mother and newborn.
Narcotic dependence is particularly problematic in
pregnant women. It leads to medical, nutritional, and
social neglect by the woman due to the long-term risks of
physical dependence, malnutrition, compromised immu-
nity, hepatitis, and fatal overdose (Alexander et al., 2004).
Taking opiates or narcotics during pregnancy places the
woman at increased risk for preterm labor, IUGR, and
preeclampsia (Wang, 2004).
Heroin is the most common illicitly used opioid. It
is derived from the seeds of the poppy plant and can be
sniffed, smoked, or injected. It crosses the placenta via
simple diffusion within 1 hour of maternal consumption
(Moran, 2004). Use of heroin during pregnancy is believed
to affect the developing brain of the fetus and may cause
behavioral abnormalities in childhood (Alexander et al.,
2004).
The most common harmful effect of heroin on new-
borns is withdrawal, or
neonatal abstinence syn-
drome
(see Chapter 24). This collection of symptoms
may include irritability, hypertonicity, a high-pitched cry,
vomiting, diarrhea, respiratory distress, disturbed sleep-
ing, sneezing, diaphoresis, fever, poor sucking, tremors,
and seizures (Littleton & Engebretson, 2005).
Withdrawal from opiates during pregnancy is
extremely dangerous for the fetus, so a prescribed oral
methadone maintenance program combined with psy-
chotherapy is recommended. This closely supervised
treatment program reduces withdrawal symptoms and
exposure to HIV and other sexually transmitted infec-
tions because she is no longer injecting drugs. However,
methadone has the same withdrawal consequences for
women and newborns as heroin does.
Sedatives
Sedatives relax the CNS and are used medically for induc-
ing relaxation and sleep, relieving tension, and treating
seizures. Sedatives easily cross the placenta and cause birth
defects and behavioral problems. Infants born to mothers
who abuse sedatives during pregnancy may be physically
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
577
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 577
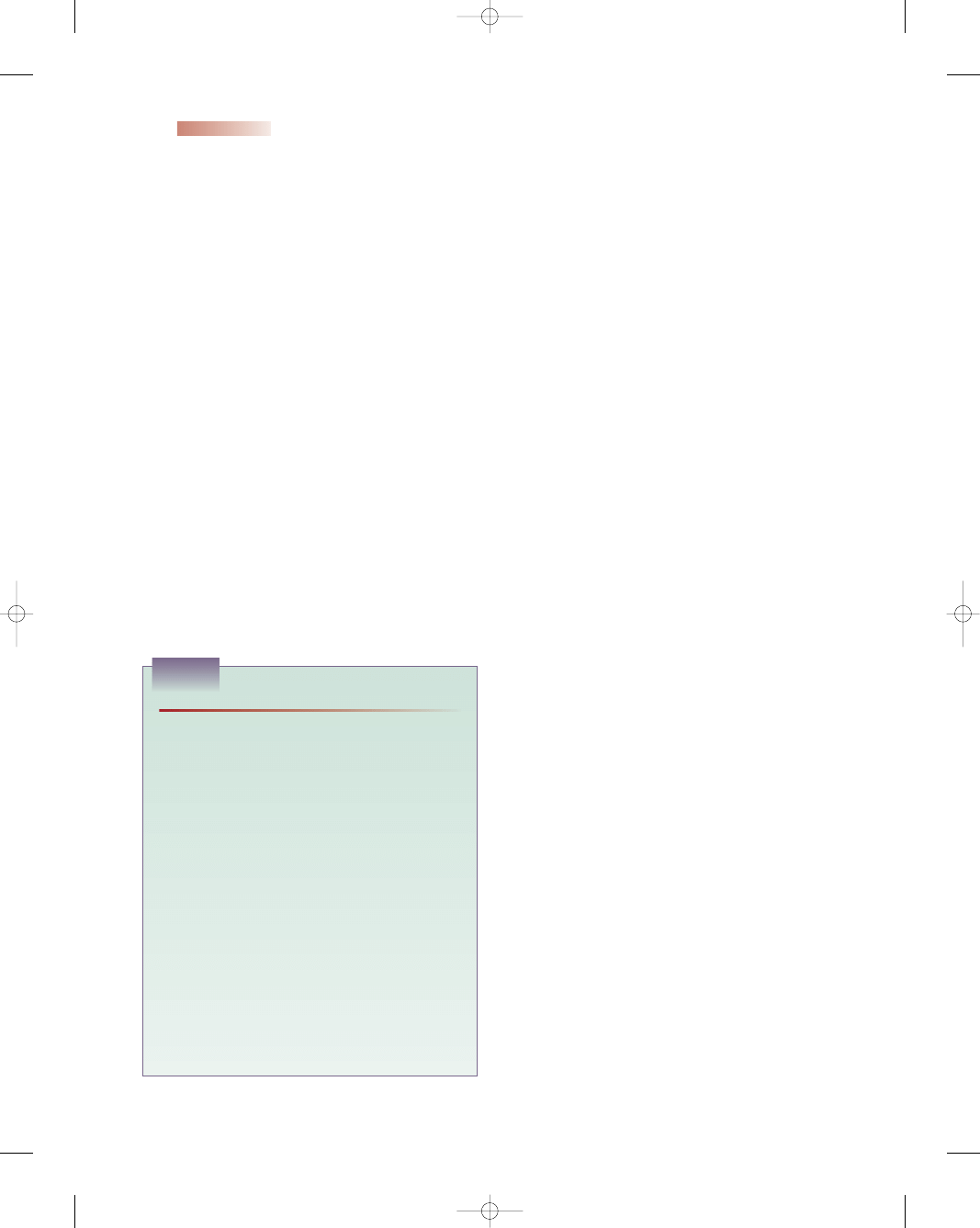
dependent on the drugs themselves and are more prone to
respiratory problems, feeding difficulties, disturbed sleep,
sweating, irritability, and fever (Alexander et al., 2004)
Nursing Management
Substance abuse during pregnancy remains a huge prob-
lem in our society. The maternal and fetal consequences
are still underestimated and more research is needed to
validate its impact. Nursing management emphasizes
screening and prevention to reduce the high incidence
of obstetric and medical complications among users, as
well as the morbidity and mortality among their passively
addicted infants.
Assessment
Substance abuse screening in pregnancy is done to detect
the use of any substance known or suspected to exert a
deleterious effect on the client or her fetus. Routinely ask
about substance abuse with all women of childbearing
age, inform them of the risks involved, and advise them
against continuing. Screening questionnaires are helpful in
identifying potential users, may reduce the stigma of asking
clients about substance abuse, and result in a more accu-
rate and consistent evaluation. The questions in Box 20-5
may help assess a client who is at risk for substance abuse
during pregnancy. Using accepting terminology may
encourage honest answers without fear of reproach.
A urine toxicology screen may also be helpful in deter-
mining drug use, although a urine screen identifies only
recent or heavy use of drugs. The length of time a drug is
present in urine is as follows:
•
Cocaine: 24 to 48 hours in an adult, 72 to 96 hours in
an infant
•
Heroin: 24 hours in an adult, 24 to 48 hours in an infant
•
Marijuana: 1 week to 1 month in an adult, up to a month
or longer in an infant
•
Methadone: up to 10 days in an infant (Wang, 2004)
A positive drug screen in a newborn warrants an inves-
tigation by the state protection agency. In the interim, the
newborn’s comfort is paramount; environmental control
will help reduce the stress and stimuli (see Chapter 24 for
a more in-depth discussion).
A positive screen is an opportunity for the nurse and
the client to discuss prenatal exposure to substances that
may be harmful. The discussion may lead the nurse to
refer the client for a diagnostic assessment or identify
an intervention such as counseling that may be helpful.
Being nonjudgmental is a key to success; a client is more
apt to trust and reveal patterns of abuse if the nurse does
not judge the client and her lifestyle choices.
Nursing Interventions
Nursing interventions must be provided in a supportive,
proactive, and accepting fashion. Assure women with sub-
stance abuse problems that sharing information of a con-
fidential nature with healthcare providers will not render
them liable to criminal prosecution. Perform counseling
and education, emphasizing the following:
•
Education about the effects of substance exposure on
the fetus
•
Interventions to improve mother–child attachment and
improve parenting
•
Psychosocial support if treatment is needed to reduce
substance abuse
•
Referral to outreach programs to improve access to
treatment facilities
•
Hazardous legal substances to avoid during pregnancy
•
Follow-up of children born to substance-dependent
mothers
•
Dietary counseling to improve the pregnancy outcome
for both mother and child
•
Drug screening to identify all drugs a client is using
•
More frequent prenatal visits to monitor fetal well-being
•
Maternal and fetal benefits of remaining drug-free
•
Cultural sensitivity
•
Coping skills, support systems, and vocational assistance
Substance abuse is a complex problem that requires
sensitivity to each woman’s unique situation and con-
tributing factors. Be sure to address individual psycholog-
ical and sociocultural factors to help the woman to regain
control of her life. Treatment must combine different
approaches and provide ongoing support for women learn-
ing to live drug-free. Developing personal strengths,
578
Unit 7
CHILDBEARING AT RISK
• Have you ever used recreational drugs? If so, when
and what?
• Have you ever taken a prescription drug other than as
intended?
• What are your feelings about drug use during preg-
nancy?
• How often do you smoke cigarettes? How many per
day?
• How often do you drink alcohol?
If the assessment reveals substance use, obtain addi-
tional information by using the RAFFT questions,
which are a sensitive screening instrument for identify-
ing substance abuse (Weekes & Lee, 2004):
R: Do you drink or take drugs to Relax, improve your
self-image, or fit in?
A: Do you ever drink or take drugs while Alone?
F: Do you have any close Friends who drink or take
drugs?
F: Does a close Family member have a problem with
alcohol or drugs?
T: Have you ever gotten in Trouble from drinking or
taking drugs?
BOX 20-5
SAMPLE QUESTIONS FOR ASSESSING SUBSTANCE USE
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 578
such as communication skills and assertiveness, and self-
confidence will help the woman to resist drugs. Encourage
the use of appropriate coping skills. Enhancing self-esteem
also helps provide a foundation to avoid drugs.
K E Y C O N C E P T S
●
Preconception counseling for the woman with
diabetes is helpful in promoting blood glucose
control to prevent congenital anomalies.
●
The classification system for diabetes commonly
used is based on disease etiology and not pharmacol-
ogy management; the classification includes type 1
diabetes, type 2 diabetes, gestational diabetes,
and impaired fasting glucose and impaired glucose
tolerance.
●
A functional classification for heart disease during
pregnancy is based on past and present disability:
class I, asymptomatic with no limitation of physical
activity; class II, symptomatic (dyspnea, chest pain)
with increased activity; class III, symptomatic
(fatigue, palpitation) with normal activity; and class
IV, symptomatic at rest or with any physical activity.
●
Chronic hypertension exists when the woman has a
blood pressure of 140/90 mm Hg or higher before
pregnancy or before the 20th week of gestation or
when hypertension persists for more than 12 weeks
postpartum.
●
Successful management of asthma in pregnancy
involves elimination of environmental triggers, drug
therapy, and client education.
●
Ideally, women with hematologic conditions are
screened before conception and are made aware of
the risks to themselves and to a pregnancy.
●
A wide variety of infections, such as rubella, herpes
simplex, hepatitis B, varicella, parvovirus B19, and
many sexually transmitted infections can affect the
pregnancy, having a negative impact on its outcome.
●
The younger the adolescent is at the time of the first
pregnancy, the more likely it is that she will have
another pregnancy during her teens. About 1 million
teenagers between the ages of 15 and 19 become
pregnant each year; about half give birth and keep
their infants.
●
The nurse’s role in caring for the pregnant adoles-
cent is to assist her in identifying the options for this
pregnancy, including abortion, self-parenting of the
child, temporary foster care for the baby or herself,
or placement for adoption.
●
The prevalence of HIV/AIDS is increasing more
rapidly among women then men: half of all the
HIV/AIDS cases worldwide now occur in women.
There are only three recognized modes of HIV
transmission: unprotected sexual intercourse with
an infected partner, contact with infected blood or
blood products, and perinatal transmission.
Breastfeeding is a major contributing factor in
mother-to-child transmission of HIV.
●
Cases of perinatal AIDS have decreased in the past
several years in the United States, primarily because
of the use of zidovudine (ZDV) therapy in pregnant
women with HIV. The U.S. Public Health Service
recommends that all pregnant women should be
offered HIV antibody testing regardless of their risk
of infection, and that testing should be done during
the initial prenatal evaluation.
●
Pregnant women with substance abuse problems
commonly abuse several substance, making it diffi-
cult to ascribe a specific perinatal effect to any one
substance. Societal attitudes regarding pregnant
women and substance abuse may prohibit them
from admitting the problem and seeking treatment.
●
Substance abuse during pregnancy is associated with
preterm labor, abortion, low birthweight, CNS and
fetal anomalies, and long-term childhood develop-
mental consequences.
●
Fetal alcohol spectrum disorder is a lifelong yet
completely preventable set of physical, mental, and
neurobehavioral birth defects; it is the leading cause
of mental retardation in the United States.
●
Nursing management for the woman with substance
abuse focuses on screening and preventing substance
abuse to reduce the high incidence of obstetric and
medical complications as well as the morbidity and
mortality among passively addicted newborns.
References
Alan Guttmacher Institute (2004). In the know about pregnancy,
contraception and abortion. [Online] Available at: http://www.
guttmacher.org/in-the-know/pregnancy.html
Alexander, L. L., LaRosa, J. H., Bader, H., & Garfield, S. (2004).
New dimensions in women’s health (3rd ed.). Sudbury: Jones &
Bartlett Publishers.
American Diabetes Association (ADA) (2004). Gestational diabetes
mellitus. Diabetes Care, 27, S88–S90.
American Heart Association (2003). Heart disease and stroke statistics,
2003 update. Dallas: American Heart Association.
Anderson, W. E., & Safdar, A. (2005). Varicella-zoster virus.
EMedicine. [Online] Available at: http://emedicine.com/med/
topic2361.htm.
As-Sanie, S., Gantt, A., & Rosenthal, M. S. (2004) Pregnancy
prevention in adolescents. American Family Physician, 70(8),
1517–1524.
Barbour, L. A. (2003) New concepts in insulin resistance of preg-
nancy and gestational diabetes: long-term implications for mother
and offspring. Journal of Obstetrics and Gynecology, 23(5), 545–549.
Bartlett, J. G., & Anderson, J. R. (2001). Updated guidelines for
managing HIV in pregnancy for the USPHS Task Force. The
Hopkins HIV Report [Online]. Available at: http://www.
hopkins-aids.edu/publications/report/may01_1.html
Bayley, O. (2003). Improvement of sexual and reproductive health
requires focusing on adolescents. Lancet, 362(9386), 830–832.
Beckmann, C. A. (2002). Women’s perceptions of their asthma dur-
ing pregnancy. MCN, 27(2), 98–102.
Beckmann, C. A. (2003). The effects of asthma on pregnancy and
perinatal outcomes. Journal of Asthma, 40(2), 171–180.
Blackburn, S. T. (2003). Maternal, fetal, & neonatal physiology: a
clinical perspective. Philadelphia: Saunders.
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
579
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 579
Blaiss, M. S. (2004). Managing asthma during pregnancy.
Postgraduate Medicine, 115(5), 55–63.
Carter, C. S. (2002). Perinatal care for women who are addicted:
implications for empowerment. Health and Social Work, 27(3),
166–175.
CDC (2002). Semiannual HIV/AIDS surveillance report, 13(2)
[Online]. Available at: www.cdc.gov/hiv/stats/htm
CDC (2002). Prevention of perinatal group B streptococcal disease:
revised guidelines from CDC. Morbidity and Mortality Weekly
Report, 51(RR-11), 1–28.
CDC (2003). Rubella [Online] Available at: www.cdc.gov/nip/
publications/pink/rubella.pdf
CDC (2004). Alcohol consumption among women who are pregnant
or who might become pregnant, United States, 2002. Morbidity
and Mortality Weekly Report, 53(50), 1178–1181.
CDC (2005). Fact sheet: viral hepatitis B. [Online] Available at:
http://www.cdc.gov/ncidod/diseases/hepatitis/b/fact.htm
Criteria Committee of the New York Heart Association (1994).
Nomenclature and criteria for diagnosis of diseases of the heart and
great vessels (9th ed.). Dallas: American Heart Association.
Cunningham, D., & Rennels, M. B. (2004). Parvovirus B19 infection.
eMedicine. [Online] Available at: http://www.emedicine.com/ped/
topic192.htm
Cunningham, F. G., Gant, N. F., Leveno, K. J., et al. (2001).
Williams obstetrics (21st ed.). New York: McGraw-Hill.
Damato, E. G., & Winnen, C. W. (2002). Cytomegalovirus infection:
perinatal implications. JOGNN, 31(1), 86–92.
Dole, P. J. (2001). Primary care of HPV management in HIV-
infected women. Nurse Practitioner Forum, 12(4), 214–222.
Donahue, D. B. (2002). Diagnosis and treatment of herpes simplex
infection during pregnancy. JOGNN, 31(1), 99–106.
Dornhorst, A., & Frost, G. (2002). The principles of dietary manage-
ment of gestational diabetes: reflection on current evidence.
Journal of Human Nutrition & Dietetics, 15, 145–156.
Dudek, S. G. (2006). Nutrition essentials for nursing practice (5th ed.).
Philadelphia: Lippincott Williams & Wilkins.
Eustace, L. W., Kang, D. H., & Coombs, D. (2003). Fetal alcohol
syndrome: a growing concern for health care professionals.
JOGNN, 32(2), 215–221.
Expert Committee on the Diagnosis and Classification of Diabetes
Mellitus (2003). Report of the Expert Committee on the
Diagnosis and Classification of Diabetes Mellitus. Diabetes Care,
26(suppl 1), S5–S20.
Farrington, J. (2003). The realities of teen parenting. Current Health 2
(Human Sexuality Supplement), 29(7), 1–5.
Feig, D. S., & Palda, V. A. (2003). Type 2 diabetes in pregnancy:
a growing concern. Lancet, 359, 1690–1692.
Fischer, R. (2004). Genital herpes in pregnancy. EMedicine. [Online]
Available at: http://www.emedicine.com/med/topic3554.htm
Gabbe, S. G., & Graves, C. R. (2003). Management of diabetes
mellitus complicating pregnancy. Obstetrics and Gynecology, 102,
857–868.
Gabbe, S., Niebyl, J., & Simpson, J. (2002). Obstetrics: normal and
problem pregnancies. Philadelphia: Churchill Livingstone.
Gibbs, R. S., Sweet, R. L., & Duff, W. P. (2004). Maternal and infec-
tious diseases. In R. K. Creasy, R. Resnik, & J. D. Iams (Eds.),
Maternal-fetal medicine: principles and practice (5th ed., pp.
741–801). Philadelphia: Saunders.
Gilbert, E., & Harmon, J. (2003) Manual of high-risk pregnancy and
delivery (3rd ed.). St. Louis: Mosby.
Goswami, G., & Ong, K. (2005). Cardiovascular disease and preg-
nancy. EMedicine. [Online] Available at: http://www.emedicine.
com/med/topic3251.htm
Green, C. J., & Wilkinson, J. M. (2004). Maternal newborn nursing
care plans. St. Louis: Mosby.
Harner, H. M. (2004). Domestic violence and trauma care in teenage
pregnancy: does paternal age make a difference? JOGNN, 33(3),
312–319.
Harvey, E. A. (2004). Hypertensive disorders or pregnancy: patho-
physiology, symptoms and treatment. Nursing Spectrum. [Online]
Available at http://nsweb.nursingspectrum.com/ce/m23c-1.htm.
Herchline, T., & Amorosa, J. K. (2005) Tuberculosis. EMedicine.
[Online] Available at: http://www.emedicine.com/MED/
topic2324.htm
Hoyme, H. E., May, P. A., Kalberg, W. O., et al. (2005). A practical
clinical approach to diagnosis of fetal alcohol spectrum disorders:
clarification of 1996 Institute of Medicine Criteria. Pediatrics,
115(1), 39–47.
Joint National Committee (JNC). Seventh Report of the Joint National
Committee on Prevention, Detection, Evaluation, and Treatment of
High Blood Pressure. (2003). National Institutes of Health (NIH),
National Heart, Lung, and Blood Institute. NIH Publication No.
035233. Washington, D.C.: NIH.
Katz, A. (2003). The evolving art of caring for pregnant women with
HIV infection. JOGNN, 32(1), 102–108.
Katz, A. (2004). Preventing heart disease in women: new guidelines
take personal approach to preventing cardiovascular disease.
AWHONN Lifelines, 8(2), 119–120.
Kazzi, A. A., & Marachelian, A. (2004). Pregnancy, asthma. EMedicine.
[Online] Available at: http://www.emedicine.com/emerg/
topic476.htm
Kendrick, J. M. (2004). Diabetes in pregnancy. March of Dimes
Nursing Module. White Plains, NY: March of Dimes Education
and Health Promotion.
Koniak-Griffin, D., Lesser, J., Uman, G., Stein, J. A., &
Cumberland, W. G. (2003). Project CHARM: an HIV preven-
tion program for adolescent mothers. Family and Community
Health, 26(2), 94–107.
Koniak-Griffin, D., & Turner-Pluta, C. (2001). Health risks and psy-
chosocial outcomes of early childbearing: a review of the literature.
Journal of Perinatal and Neonatal Nursing, 15(2), 1–17.
Koren, G., Nulman, I., Chudley, A. E., & Loocke, C. (2003). Fetal
alcohol spectrum disorder. Journal of the Canadian Medical
Association, 169(11), 1181–1185.
Koshar, J. H. (2001). Teen pregnancy 2001: still no easy answers.
Pediatric Nursing, 27(5), 505–509.
Kuczkowski, K. M. (2004). Labor analgesia for the parturient with
cardiac disease: what does the obstetrician need to know? Acta
Obstetrics and Gynecology Scandinavica, 83, 223–233.
Laartz, B., & Gompf, S. G. (2004). Viral infections and pregnancy.
EMedicine. [Online] Available at: http://www.emedicine.com/med/
topic3270.htm
Lake, M. F. (2001). Tuberculosis in pregnancy. AWHONN Lifelines,
5(5), 35–40.
Landon, M. B. (2004) Diseases of the liver, biliary system, and pan-
creas. In R. K. Creasy, R. Resnik, & J. D. Iams (Eds.), Maternal-
fetal medicine: principles and practice (5th ed., pp. 1127–1145),
Philadelphia: Saunders.
Lin, K. W., & Kirchner, J. T. (2004). Hepatitis B. American Family
Physician, 69(1), 75–86.
Littleton, L. Y., & Engebretson, J. C. (2005). Maternity nursing care.
Clifton Park, NY: Thomson Delmar Learning.
London, M. L., Ladewug, P. W., Ball, J. W., & Bindler, R. C. (2003).
Maternal-newborn & child nursing. Upper Saddle River, NJ:
Prentice Hall.
Lowdermilk, D. L., & Perry, S. E. (2004). Maternity & women’s health
care (8th ed.). Philadelphia: Mosby.
March of Dimes (2004). Pregnancy after 35: Quick reference and fact
sheet. [Online] Available at: http://www.modimes.org/professionals/
681_1155.asp
March of Dimes (2004). Group B strep infection. March of Dimes
Birth Defects Foundation. [Online] Available at: http://www.
marchofdimes.com/professionals/681_1205.asp
March of Dimes (2005). Toxoplasmosis. March of Dimes Birth Defects
Foundation. [Online] Available at: http://www.marchofdimes.com/
printableArticles/681_1228.asp?printable
=true
Martin, J., et al. (2002). Births: final data for 2000. National Vital
Statistics Report, 50(5), 1–104.
Martin, S. R., & Foley, M. R. (2002). Adult-onset heart disease in
pregnancy. Contemporary OB/GYN, 47(11), 74–92.
Mattson, S., & Smith, J. E. (2004). Core curriculum for maternal-
newborn nursing (3rd ed.). St. Louis: Elsevier Saunders.
McCann, J. A. S. (2004). Maternal-neonatal nursing made incredibly
easy. Philadelphia: Lippincott Williams & Wilkins.
McCarter-Spaulding, D. E. (2002). Parvovirus B19 in pregnancy.
JOGNN, 31(1), 107–112.
McIntyre, J., & Gray, G. (2002). What can we do to reduce mother to
child transmission of HIV? British Medical Journal, 324(7331),
218–222.
Messner, M. G. (2004). Managing women with gestational diabetes.
Clinical Advisor, 7(11), 32–35.
580
Unit 7
CHILDBEARING AT RISK
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 580
Minkoff, H. (2003). Human immunodeficiency virus infection in
pregnancy. Obstetrics & Gynecology, 101(4), 797–811.
McKinney, E. S., James, S. R., Murray, S. S., & Ashwill, J. W.
(2005). Maternal-child nursing (2nd ed.). St. Louis: Elsevier
Saunders.
Mirochnick, M., & Capparelli, E. (2004). Pharmacokinetics of anti-
retrovirals in pregnant women. Clinical Pharmacokinetics, 43(15),
1071–1087.
Montgomery, K. S. (2003). Nursing care for pregnant adolescents.
JOGNN, 32(2), 249–257.
Moran, B. A. (2004). Substance abuse in pregnancy. In S. Mattson &
J. E. Smith, Core curriculum for maternal-newborn nursing (3rd ed.,
pp. 750–770). St. Louis: Elsevier Saunders.
Murray, S. S. & McKinney, E. S. (2006). Foundations of maternal-
newborn nursing (4th ed.) Philadelphia: W. B. Saunders.
Narayanan, S. K., & Ossiani, M. (2004). Streptococcus group B infec-
tions. eMedicine. [Online] Available at: http://www.emedicine.
com/med/topic2185.htm
National Asthma Education and Prevention Program (NAEPP)
(2005). NAEPP Expert Panel Report: managing asthma during
pregnancy. Journal of Allergy & Clinical Immunology, 115, 36–46.
Neumann, M., & Graf, C. (2003). Pregnancy after age 35.
AWHONN Lifelines, 7(5), 423–430.
NoFAS (2003). What is fetal alcohol syndrome? [Online]. Available
at: http://www.nofas.org/main/what_is_FAS.htm
O’Toole, M. T. (2005). Encyclopedia & dictionary of medicine, nursing,
& allied health, 7th ed. Philadelphia: Saunders.
Peddicord, K. (2005). Healthy hearts for women. AWHONN
Lifelines, 9(1), 35–38.
Penny, J. (2003). HIV/AIDS—2003 update. Vital Signs, 8(3), 15–19.
Pollard, T. (2003). Teenage pregnancy still a challenge for all. British
Journal of Community Health, 8(3), 102.
Poole, J. H. (2003). Thalassemia and pregnancy. Journal of Perinatal
and Neonatal Nursing, 17(3), 196–208.
Prasad, A. K., & Ventura, H. O. (2001). Valvular heart disease and
pregnancy. Postgraduate Medicine, 110(2), 69–79.
Public Health Service Task Force (PHSTF) (Feb. 4, 2002).
Recommendations for use of antiretroviral drugs in pregnant HIV-infected
women for maternal health and interventions to reduce perinatal
HIV-transmission in the United States. Washington, D.C.: Author.
Ryan, E. A. (2003). Hormones and insulin resistance during
pregnancy. Lancet, 362, 1777–1778.
Samson, L., & Ferguson, H. W. (2004). Chronic medical conditions
and pregnancy, part I. Nursing Spectrum. [Online] Available at:
http://nsweb.nursingspectrum.com/ce/m23a-1.htm
Shieh, C., & Kravitz, M. (2002). Maternal-fetal attachment in preg-
nant women who use illicit drugs. JOGNN, 31(2), 156–164.
Siu, S., & Colman, J. M. (2004). Cardiovascular problems and preg-
nancy: an approach to management. Cleveland Clinic Journal of
Medicine, 71(12), 977–985.
Sloane, E. (2002). Biology of women (4th ed.). New York: Delmar.
SmithBattle, L. (2003). Displacing the “Rule Book” in caring for teen
mothers. Public Health Nursing, 20(5), 369–376.
Tiller, C. M. (2002) Chlamydia during pregnancy: implications and
impact on neonatal outcomes. JOGNN, 31(1), 93–98.
Turok, D. K., Ratcliffe, S. D., & Baxley, E. G. (2003). Management
of gestational diabetes mellitus. American Family Physician, 68(9),
1767–1772.
U.S. Department of Health and Human Services (USDHHS) (2000)
Healthy people 2010 (Conference Edition, vol. 1). Washington, D.C.
U.S. Department of Health and Human Services (USDHHS) (2005)
U.S. Surgeon General releases advisory on alcohol use in pregnancy.
HHS Office of the Surgeon General. [Online] Available at:
http://hhs.gov/surgeongeneral/pressreleases/sg02222005.html
U.S. Preventive Services Task Force (USPSTF) (2003). Screening
for gestational diabetes mellitus: recommendation and rationale.
American Family Physician, 68(2), 331–336.
U.S. Preventive Services Task Force (USPSTF) (2004). Updated
USPHSTF recommendations for the use of antiretroviral drugs in preg-
nant HIV-1-infected women for maternal health and interventions to
reduce perinatal HIV-1 transmission in the United States. [Online]
Available at: http://aidsinfo.nih.gov
Wallerstedt, C., & Clokey, D. E. (2004). Endocrine and metabolic
disorders. In S. Mattson & J. E. Smith, Core curriculum for
maternal-newborn nursing (3rd ed., pp. 660–702). St. Louis:
Elsevier Saunders.
Wang, M. (2004). Perinatal drug abuse and neonatal withdrawal.
eMedicine. [Online] Available at: http://www.emedicine.com/ped/
topic2631.htm
Weekes, A. J., & Lee, D. S. (2004). Substance abuse: cocaine.
eMedicine. [Online] Available at: http://www.emedicine.com/ped/
topic2666.htm
Wenger, N. K. (2004). Cardiovascular disease in women: new guide-
lines stress prevention. Consultant, 44(4), 660–663.
Williams, A. (2003). Gynecologic care for women with HIV infection.
JOGNN, 32(1), 87–93.
Wolbretta, D. (2003). Treatment of arrhythmias during pregnancy.
Current Women’s Health Reports, 3, 135–139.
Youngkin, E. Q., & Davis, M. S. (2004). Women’s health: a primary
care clinical guide (3rd ed.). Upper Saddle River, NJ: Pearson
Prentice Hall.
Web Resources
Alan Guttmacher Institute: http://www.agi-usa.org
Alcoholics Anonymous: www.alcoholics-anonymous.org
American Academy of Pediatrics: www.aap.org
American College of Obstetricians and Gynecologists:
www.acog.org
American Diabetes Association: www.diabetes.org
American Lung Association: www.lungusa.org
American Medical Association HIV/AIDS Resource Center:
www.ama-assn.org/special/hiv
American Society of Addiction Medicine: www.asam.org
Association of Women’s Health, Obstetric & Neonatal Nurses:
www.awhonn.org
Association of Nurses in AIDS Care: www.anacnet.org
Asthma and Allergy Foundation of America: www.aafa.org
Allergy & Asthma Network of Mothers of Asthmatics:
www.breatherville.org
CDC National Prevention Information Network: 1-800-458-5231,
www.cdcnpin.org
HIV websites: www.hivinsite.ucsf.edu, www.hivatis.org
International Nurses Society on Addictions: www.intnsa.org
March of Dimes: www.modimes.org
Narcotics Anonymous: www.na.org
National Campaign to Prevent Teen Pregnancy:
www.teenpregnancy.org
National Clearinghouse for Alcohol and Drug Abuse Information:
www.health.org
National Heart, Lung and Blood Institute of NIH:
www.nhlbi.nih.gov
National Institute on Drug Abuse: www.nida.nih.gov
National Organization for Fetal Alcohol Syndrome: www.nofas.org
Planned Parenthood: wwwplannedparenthood.org
Sex Information and Education Council of United States:
www.siecus.org
Sidelines High Risk Pregnancy Support Office: www.sidelines.org
Tobacco Information and Prevention Source (TIPS):
www.cdc.gov/tobacco
Women for Sobriety Support Group: www.womenforsobriety.org
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
581
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 581
582
Unit 7
CHILDBEARING AT RISK
Chapter
WORKSHEET
Chapter
●
M U L T I P L E C H O I C E Q U E S T I O N S
1.
Which of the following would the nurse include when
describing the pathophysiology of gestational diabetes?
a. Pregnancy fosters the development of
carbohydrate cravings.
b. There is progressive resistance to the effects of
insulin.
c. Hypoinsulinemia develops early in the first
trimester.
d. Glucose levels decrease to accommodate fetal
growth.
2.
When providing prenatal education to a pregnant
woman with asthma, which of the following would be
important for the nurse to do?
a. Explain that she should avoid steroids during her
pregnancy.
b. Demonstrate how to assess her blood glucose
levels.
c. Teach correct administration of subcutaneous
bronchodilators.
d. Ensure she seeks treatment for any acute
exacerbation.
3.
Which of the following conditions would cause an
insulin-dependent diabetic client the most difficulty
during her pregnancy?
a. Placenta previa
b. Hyperemesis gravidarum
c. Abruptio placentae
d. Rh incompatibility
4.
Women who drink alcohol during pregnancy:
a. Often produce more alcohol dehydrogenase
b. Usually become intoxicated faster than before
c. Can give birth to an infant with fetal alcohol
spectrum disorder
d. Gain fewer pounds throughout the gestation
5.
Transmission of HIV from an infected individual to
another person occurs:
a. Only if there is a large viral load in the blood
b. Most commonly as a result of sexual contact
c. In all infants born to women with HIV infection
d. Most frequently in nurses with needlesticks
●
C R I T I C A L T H I N K I N G E X E R C I S E S
1.
A client at 26 weeks’ gestation came to the clinic to
follow up on her previous 1-hour glucose screening.
Her results had come back outside the accepted
screening range, and a 3-hour glucose tolerance test
(GTT) had been ordered. It resulted in three abnor-
mal values, confirming a diagnosis of gestational
diabetes. As the nurse in the prenatal clinic you are
seeing her for the first time.
a. What additional information will you need to
provide care for her?
b. What education will she need to address this new
diagnosis?
c. How will you evaluate the effectiveness of your
interventions?
2.
A 14-year-old white girl comes to the public health
clinic with her mother. The mother tells you that her
daughter has been “out messing around and has got
herself pregnant.” The girl is crying quietly in the
corner and avoids eye contact with you. The mother
reports that her daughter “must be following in my
footsteps” because she herself became pregnant
when she was only 15 years old. The client’s mother
goes back out into the waiting room and leaves the
client with you.
a. What is your first approach with the client to
gain her trust?
b. List the client’s educational needs during this
pregnancy.
c. What prevention strategies are needed to prevent a
second pregnancy?
3.
Linda, a 27-year-old G3, P2 is admitted to the labor
and birth suite because of preterm rupture of mem-
branes at an estimated 35 weeks’ gestation. She has
received no prenatal care and reports this was an
unplanned pregnancy. Linda appears distracted and
very thin. She reports that her two previous children
have been in foster care since birth because the child
welfare authorities “didn’t think I was an adequate
mother.” She denies any recent use of alcohol or
drugs but offers no further explanation. She has a
spontaneous vaginal birth a few hours later, produc-
ing a 4-lb boy with Apgar scores of 8 at one minute
and 9 at 5 minutes.
a. What aspects of this woman’s history make you
concerned that this infant is at risk for fetal alcohol
spectrum disorder?
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 582
Chapter 20
NURSING MANAGEMENT OF THE PREGNANCY AT RISK: PREEXISTING CONDITIONS
583
b. What additional screening or laboratory tests might
validate your suspicion?
c. What physical and neurodevelopmental deficits
might present later in life if the infant has fetal
alcohol spectrum disorder?
●
S T U D Y A C T I V I T I E S
1.
In the maternity clinic or hospital setting, interview a
pregnant woman with a preexisting medical condi-
tion (e.g., diabetes, asthma, sickle cell anemia) and
find out how this condition affects her life and this
pregnancy, especially her lifestyle choices.
2.
You have a close friend who has a problem with
drugs or alcohol but doesn’t think she has a problem.
How would you handle this situation?
3.
Should marijuana be legalized in the United States?
What impact might your view (pro or con) have on
pregnant women and their offspring?
4.
Outline a discussion you might have with an HIV-
positive pregnant woman who doesn’t see the need
to take antiretroviral agents to prevent perinatal
transmission.
5.
Which of the following conditions would not preclude
a woman from breastfeeding? Select all that apply:
a. Hepatitis B
b. Parvovirus B19
c. Herpesvirus type 2
d. HIV-positive status
e. Cytomegalovirus
f. Varicella-zoster virus
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 583
3132-20_CH20rev.qxd 12/15/05 3:37 PM Page 584
Wyszukiwarka
Podobne podstrony:
Essentials of Maternity Newborn and Women's Health 3132A 30 p780 781
Essentials of Maternity Newborn and Women's Health 3132A 29 p778 779
Essentials of Maternity Newborn and Women s Health 3132A 32 p785 808
Essentials of Maternity Newborn and Women s Health 3132A 23 p634 662
Essentials of Maternity Newborn and Women s Health 3132A 17 p428 446
Essentials of Maternity Newborn and Women s Health 3132A 16 p393 427
Essentials of Maternity Newborn and Women s Health 3132A 21 p585 612
Essentials of Maternity Newborn and Women s Health 3132A 09 p189 207
Essentials of Maternity Newborn and Women s Health 3132A 11 p235 252
Essentials of Maternity Newborn and Women s Health 3132A 08 p167 188
Essentials of Maternity Newborn and Women s Health 3132A 03 p042 058
Essentials of Maternity Newborn and Women s Health 3132A 27 p769 771
Essentials of Maternity Newborn and Women s Health 3132A 26 p729 768
Essentials of Maternity Newborn and Women s Health 3132A 28 p772 777
Essentials of Maternity Newborn and Women s Health 3132A 25 p717 728
Essentials of Maternity Newborn and Women s Health 3132A 05 p107 126
Essentials of Maternity Newborn and Women s Health 3132A 19 p496 542
Essentials of Maternity Newborn and Women s Health 3132A 22 p613 633
więcej podobnych podstron