ORIGINAL RESEARCH—WOMEN’S SEXUAL HEALTH
Impaired Sexual Function in Patients with Borderline Personality
Disorder is Determined by History of Sexual Abuse
jsm_1422
3356..3363
Olaf Schulte-Herbrüggen, MD,* Christoph J. Ahlers, MSc,
†
Julia-Maleen Kronsbein, MD,*
Anke Rüter, MSc,* Scharif Bahri, MD,* Aline Vater, MSc,* and Stefan Roepke, MD*
*Charité-University Medicine Berlin, Campus Benjamin Franklin, Department of Psychiatry and Psychotherapy, Berlin,
Germany, EU;
†
Charité-University Medicine Berlin, Campus Mitte, Institute of Sexual Science and Sexual Medicine,
Berlin, Germany
DOI: 10.1111/j.1743-6109.2009.01422.x
A B S T R A C T
Introduction.
Patients suffering from a Borderline Personality Disorder (BPD) display altered sexual behavior, such
as sexual avoidance or sexual impulsivity, which has repeatedly been linked to the sexual traumatization that occurs
in a high percentage of BPD patients. Until now, no empirical data exists on whether these patients concomitantly
suffer from sexual dysfunction.
Aim.
This study investigates sexual function and the impact of sexual traumatization on this issue in women with
BPD as compared to healthy women.
Main Outcome Measures.
Sexual function was measured using the Female Sexual Function Index. Additionally,
diagnoses were made with SCID II Interviews for Axis II and with the Mini International Neuropsychiatric Interview
for Axis I disorders. The Post-traumatic Stress Diagnostic Scale for trauma evaluation was used. Sexual orientation
was assessed by self-evaluation.
Methods.
Forty-five women with BPD as diagnosed according to DSM-IV criteria and 30 healthy women completed
questionnaires on sexual function and sexual abuse history, as well as interviews on axis I and II disorders and
psychotropic medication.
Results.
The BPD group showed a significantly higher prevalence of sexual dysfunction. Subgroup analyses revealed
that BPD with concomitant sexual traumatization, and not BPD alone, best explains impaired sexual function. Sexual
inactivity was mainly related to current major depression or use of SSRI medication. In sexually active participants,
medication and symptoms of depression had no significant impact on sexual function.
Conclusions.
Not BPD alone, but concomitant sexual traumatization, predicts significantly impaired sexual func-
tion. This may have a therapeutic impact on BPD patients reporting sexual traumatization. Schulte-Herbrüggen
O, Ahlers CJ, Kronsbein JM, Rüter A, Bahri S, Vater A, and Roepke S. Impaired sexual function in patients
with borderline personality disorder is determined by history of sexual abuse. J Sex Med 2009;6:3356–3363.
Key Words.
Borderline Personality Disorder; Sexual Orientation; FSFI; Sexual Abuse; Sexual Dysfunction; Female
Sexual Function
Introduction
B
orderline Personality Disorder (BPD) is a
complex mental disorder characterized by a
pervasive pattern of instability in emotion regula-
tion, interpersonal relationships, self-image, and
impulse control [1]. Prevalence rates of up to 5.8%
have been found in the general population [2].
BPD is the most common personality disorder in
clinical settings and is characterized by severe
functional impairment, substantial treatment utili-
zation, and a high mortality rate [3].
Impulsivity in BPD affects multiple areas of
life such as spending money, traffic behavior,
substance abuse, eating, and sexuality [4]. Even
though clinical experience suggests impulsive
3356
J Sex Med 2009;6:3356–3363
© 2009 International Society for Sexual Medicine

sexual behavior, identity disturbance, and unstable
relationships accompanied by hyper- as well as
hypo-sexual desire disorders (often leading to
sexual avoidance or promiscuity) are frequently
seen phenomena in patients with BPD, there is not
much empirical data available regarding sexual
behavior in this group of patients. A study on 119
male and 284 female adolescents from primary
care settings reported an increased number of
unsafe sexual partners for females with elevated
Personality Disorder (PD) symptom levels.
Besides others, the BPD symptoms of “impulsiv-
ity,” “abandonment fear,” and “unstable self-
image” were associated in this study with a high
number of sexual partners [5]. Data on adolescents
are not directly applicable to adults, thus there is
little empirical evidence pointing toward increased
promiscuity and risk for unsafe sex practices in
patients with BPD [6,7]. On the other hand, there
is a study by Zanarini and colleagues [8] reporting
that 42.2% of the female BPD patients to be
avoidant of consenting sex, and 36.5% had become
symptomatic (e.g., had become dissociated, re-
ported feeling suicidal, or hurt themselves) after
consenting to sex within the last 2 years. A study by
Sansone and colleagues [9] reported earlier sexual
exposure as well as rape, but no other aspects of
sexual impulsivity, such as a larger number of
sexual partners or more frequent treatment for
sexually transmitted diseases, in their sample of 76
women with BPD symptomatology. Nevertheless,
the study did not differentiate between sexually
active and sexually inactive participants.
Empirical data point out that childhood sexual
abuse (CSA), an identified contributory variable to
BPD, is associated with sexual impulsivity, mostly
promiscuity [10,11]. Although the empirical data
are not completely consistent, hypo- and hyper-
sexual desire can be observed in CSA survivors [12].
Apart from studies on sexual behavior in BPD
patients, there is even less evidence with regard to
the extent that sexual characteristics (e.g., sexual
function) are affected for these patients [13]. Hurl-
bert and colleagues found higher levels of sexual
assertiveness, higher sexual self-esteem, greater
sexual preoccupation, more sexual boredom, and
greater sexual dissatisfaction as compared to
women without BPD [14].
In the present study, we focused on sexual func-
tion in women with BPD in a clinical sample
compared with healthy women with respect to
contributing factors such as medication, psychia-
tric comorbidity (e.g., depression), post-traumatic
stress disorder (PTSD), and history of sexual abuse.
Materials and Methods
Study Population
Forty-five patients diagnosed with BPD (accord-
ing to DSM-IV) and 30 healthy women agreed to
participate in the study. A larger number of BPD
patients was chosen to guarantee an equal number
of sexually active participants in each group. All
BPD patients were admitted to our specialized
inpatient treatment program for BPD, during
which they were consecutively recruited into the
study between October 2005 and March 2008.
Prior to admission to the inpatient program, all of
them were on a waiting list and none was admitted
for acute care. Patients were not reimbursed
for study participation. Healthy controls were
recruited via media advertisements and reim-
bursed for participation. The study was approved
by the ethics committee of the Charité-University
Medicine Berlin. All participants provided written
informed consent after having received a thorough
explanation of the study.
Axis II diagnoses were confirmed or excluded in
patients and controls with the German version of
the Structured Clinical Interview for DSM-IV
(SCID II); axis I diagnoses were assessed with the
German version of the Mini International Neu-
ropsychiatric Interview (M.I.N.I.). Exclusion cri-
teria for the patients were anorexia nervosa,
oligophrenia, schizophrenia, pregnancy, and age
younger than 18 years. Current or chronic medical
conditions in patients and controls were excluded
by a clinical interview. Any use of medication
within the prior 2 months was an exclusion crite-
rion for controls. Interviews were performed or
supervised by a senior psychiatrist. Concurrent
comorbid psychiatric diagnoses in BPD patients
included the following: major depression (actual
N = 11, 24.4%; lifetime N = 23, 51.1%), dys-
thymia
(actual
N = 10,
22.2%),
obsessive–
compulsive disorder (actual N = 4, 8.9%), PTSD
(actual N = 18, 40%), panic disorder (actual N = 5,
11.1%), alcohol use disorder (last year, N = 11,
24.5%), substance use disorder (last year, N = 15,
33.3%), bulimia (actual N = 14, 31.1%); and
among comorbid personality disorder diagnoses,
paranoid (N = 4, 8.9%), schizotypal (N = 1, 2.2%),
antisocial (N = 2, 4.4%), narcissistic (N = 1,
2.2%), histrionic (N = 2, 4.4%), avoidant (N = 8,
17.8%), obsessive–compulsive (N = 6, 13.3%).
Fourteen (31.1%) BPD patients were on atypical
neuroleptics, 25 (55.6%) on SSRIs, and 18 (40%)
were without psychotropic medication. None of
the patients took any other medication.
Sexual Function in BPD
3357
J Sex Med 2009;6:3356–3363
Assessment Instruments
The PTSD Diagnostic Scale (PDS) is a 49-item
self-report measure of PTSD that was used to
assess all six DSM-IV diagnostic criteria for PTSD
[1]. In the study, we used the instrument for assess-
ment of trauma type. Depressive symptoms were
assessed with the 17-item Hamilton Depression
Scale (HAMD). Sexual orientation was assessed by
self-evaluation of the participants.
Sexual Function
For assessment of female sexual function, the
Female Sexual Function Index (FSFI), a 19-item
self-report instrument, was applied, including six
key domains (desire, arousal, lubrication, orgasm,
satisfaction, and pain). The administration takes
about 15 minutes. Responders were asked to base
their responses on the previous 4 weeks. Subscores
are computed by item summation and by multi-
plying by a weighting factor. A total score is cal-
culated by summation of all subscores, indicating
an overall sexual function score. A total FSFI score
of 26.55 or lower has been defined as the cut-off
score for distinguishing between impaired and
intact sexual function [15]. Former studies have
described inter-item reliability values within the
acceptable range for sexually healthy women
(Cronbach’s a = 0.82–0.92) [16]. The FSFI has
been validated and culturally adapted in about 15
countries, including Germany [17].
Statistics
Statistical analysis was performed using the SPSS
(version 14) software. Before using parametric
tests,
histograms
were
graphed
and
the
Kolmogorov–Smirnov
test
was
performed.
Between-groups comparisons were done with two-
tailed t-tests. The distribution of sexual orienta-
tion in the two study groups was assessed with
cross tabulations and analyzed with chi-square
tests. Further analyses were performed with linear
regression models, multiple analyses of covariance
(MANCOVA), and Pearson’s correlation coeffi-
cients. All significance levels were set to 0.05. All
means and standard deviations were presented
when appropriate.
Results
Self-Reported Sexual Orientation
Self-evaluation of sexual orientation revealed
24.4% bisexual and 6.7% homosexual BPD
patients, and 6.7% bisexual and 13.3% homo-
sexual healthy controls. All others reported
heterosexual
orientation.
Nevertheless,
the
distribution of sexual orientation did not differ
significantly between the two groups (Table 1).
Sexual Activity and Major Depression
Twenty-six (57.8%) of the BPD patients and 10
(33.3%) of the control women reported no sexual
activity during the 4 weeks prior to the interview.
These distribution differences were statistically
significant (c
2
(1)
=
4.31, P = 0.04). To investigate
whether lack of sexual activity within the last 4
weeks might be an effect of medication or depres-
sive symptomatology, comorbid axis I disorder, or
history of sexual abuse, which have repeatedly
Table 1
Sociodemographic data and psychometric measures in patients with Borderline Personality Disorder and
healthy controls
BPD patients
N
= 45, mean (SD)
Healthy controls
N
= 30, mean (SD)
Statistics
Age
28.2 (7.2)
27.7 (4.2)
T
= 0.30
HAMD total score
11.4 (4.8)
1.9 (1.7)
T
= 10.4**
Sexual orientation
Heterosexual
31, 68.9%
24, 80%
c
2
(2)
= 4.44
Homosexual
3, 6.7%
4, 13.3%
P
= 0.11
Bisexual
11, 24.4%
2, 6.7%
FSFI
N
= 19
†
N
= 20
†
Total score
24.1 (5.1)
30.8 (2.8)
T
= -5.1** df = 37
Desire
3.5 (1.8)
3.9 (1.0)
T
= -1.1 df = 37
Arousal
4.1 (1.3)
5.3 (0.5)
T
= -4.0** df = 23.7
Lubrification
5.0 (1.1)
5.7 (0.5)
T
= -2.5* df = 25.0
Orgasm
3.3 (1.2)
5.2 (0.9)
T
= -5.6** df = 37
Satisfaction
3.8 (1.7)
5.1 (0.9)
T
= -3.0** df = 26.7
Pain
4.5 (1.2)
5.7 (0.5)
T
= -4.1** df = 23.5
*P
< 0.05; **P < 0.01.
†
Sexually active within the last 4 weeks.
BPD
= Borderline personality disorder; df = degrees of freedom; FSFI = Female Sexual Function Index; HAMD = 17-item Hamilton depression scale;
SD
= standard deviation.
3358
Schulte-Herbrüggen et al.
J Sex Med 2009;6:3356–3363
been shown to reduce sexual desire and function
[12,18,19], a stepwise forward logistic regression
analysis predicting sexual inactivity was per-
formed, including HAMD score, treatment with
atypical neuroleptics, SSRI use, sexual traumatiza-
tion (item 5 or 6 of the PDS), dysthymia, and
PTSD as covariates. Accordingly, only inclusion of
SSRI medication (B = -1.5, P = 0.025) resulted
in a significant model (Nagelkerke’s R
2
=
0.17)
explaining sexual abstinence. Actual major depres-
sive episode (MDE) could not be included in the
regression model as only one patient (5.3% of the
sexually active patients) in the MDE group was
sexually active. Thus, the distribution of sexually
active vs. non-sexually active was significantly dif-
ferent in the group with comorbid MDE versus no
comorbid MDE (c
2
(1)
=
6.55, P = 0.01). Seven
patients with comorbid MDE were taking an SSRI
(representing 63.6% of patients with comorbid
MDE), and 18 patients without comorbid MDE
were taking an SSRI (representing 52.9% of
patients without comorbid MDE); this distribu-
tion was not significantly different (c
2
(1)
=
0.39,
P = 0.54), indicating that actual MDE and SSRI
medication were two independent variables influ-
encing sexual abstinence.
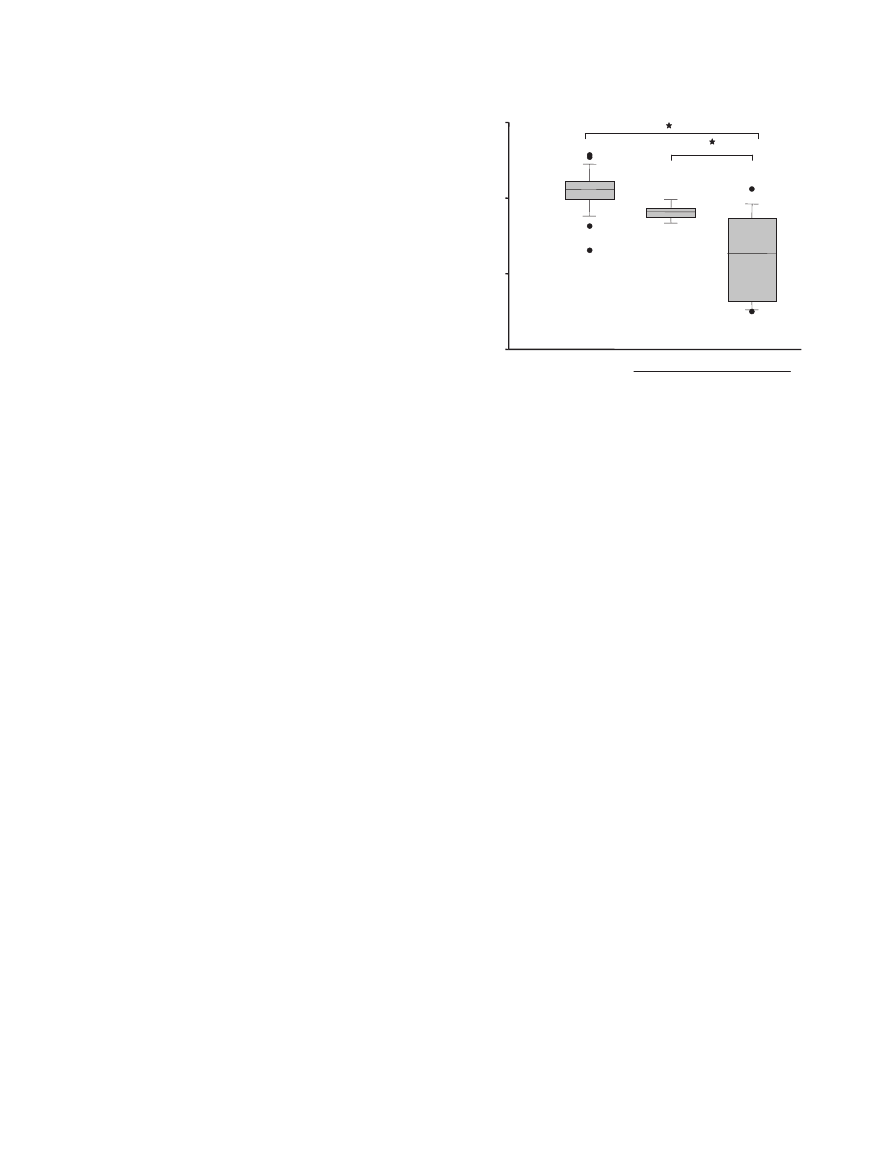
Sexual Function in Patients with BPD
Patients with BPD showed a significant reduction
of sexual function as reflected in the FSFI total
score and almost all subscores. Only the subscore
“desire” was unchanged compared to healthy
women (Table 1). Since 9 (47.4%) of the sexually
active BPD patients had FSFI total scores below
26.5 points (mean 24.1 [SD 5.1]), a remarkable
number of patients in the study group met the
criteria for “sexual dysfunction” as specified by
the validation study [15]. In the control group,
two women showed an FSFI score below 26.5
(Figure 1). Three sexually active BPD patients and
one sexually inactive BPD patient did not fill out
the PDS (assessment of trauma type) and were
excluded from the analysis of predictors of sexual
dysfunction. Seventeen (68.0%) out of 25 sexually
inactive BPD patients reported a history of sexual
traumatization. Eleven (68.8%) out of 16 sexually
active BPD patients reported a history of sexual
traumatization. All controls filled out the PDS, of
whom none reported a history of sexual traumati-
zation. Since sexual dysfunction has widely been
discussed in the context of sexual traumatization,
especially CSA, we performed subgroup analyses
using a stepwise regression model, including the
variables psychotropic medication (SSRI or atypi-
cal neuroleptics), sexual traumatization (item 5 or
6 of the PDS), and HAMD score. This statistical
approach revealed a significant model (corrected
R
2
=
0.20) with sexual traumatization (B = -5.7,
P = 0.047) as the only contributing factor. An
anova model for sexually active participants with
group (BPD with sexual traumatization, BPD
without sexual traumatization, and controls) as the
only independent variable, and FSFI sum score as
the dependent variable, revealed a significant
influence of group (P
< 0.001). Post hoc analysis
(Bonferroni-corrected) revealed a significant dif-
ference of mean FSFI score between controls
and BPD patients with sexual traumatization
(P
< 0.001) and BPD patients with and without
sexual traumatization (P = 0.03) (Figure 1). None
of the sexually active BPD patients who did not
report a history of sexual traumatization showed
an FSFI score below 26.5 (Figure 1).
Discussion
In the present study, we analyzed sexual function
in women with BPD compared to healthy con-
trols. For the first time, we provide empirical evi-
dence for impaired sexual function in this group.
Hereby, current sexual abstinence was mainly
explained by a current episode of major depression
or concomitant medication with an SSRI. Further
Controls BPD without
BPD with
Hx of sexual abuse
FSFI sum
score
10
20
30
40
Figure 1 The figure shows the sum scores of the Female
Sexual Function Index for healthy controls (N
= 20), BPD
patients who did not reported sexual abuse (N
= 5), and
BPD patients who reported sexual abuse (N
= 11). The data
are presented as box plots displaying the median, quartiles,
and extremes. Asterisks indicate significant differences
(*P
< 0.05) that are corrected for multiple comparisons
(Bonferroni). Hx
= History.
Sexual Function in BPD
3359
J Sex Med 2009;6:3356–3363

investigation showed that in sexually active
women, BPD with concomitant sexual trauma-
tization, rather than BPD alone, is crucial for
sexual dysfunction in adulthood in these patients,
whereas co-diagnoses such as PTSD, major
depression, as well as use of medication neurolep-
tics or SSRIs) do not have a comparable impact.
Only the FSFI subscore “desire” did not differ
from healthy controls. This finding is in line with
a former study on sexuality in BPD patients reveal-
ing more positive attitudes about sex and greater
sexual preoccupation on the one hand, and sexual
dissatisfaction on the other hand [14]. The authors
suggest that a higher preoccupation with sex, com-
pared to non-borderline women is not surprising
since patients with BPD need “to bolster their
self-image, to approximate the kind of intimacy of
which they are incapable and to combat the feeling
of loneliness and boredom.” One possible expla-
nation for the fact that some studies reveal reduced
as well as increased sexual desire in BPD patients,
and the fact that in the present study, we find
unchanged sexual desire as compared to healthy
controls, may be due to the fact that BPD patients
with reduced sexual desire were not sexually active.
The FSFI is designed and validated to assess sexual
desire during sexual activity intervals, but not for
those subjects who feel sexual desire but do not
have sex. Future experimental studies are required
to elucidate the underlying mechanisms of these
findings with a focus on questions of general and
sexual identity.
This study clearly shows that sexual dysfunction
is not specific to BPD, but is often closely asso-
ciated with it since sexual traumatization is a
common but not obligatory phenomenon in these
patients. There is widely accepted evidence linking
CSA with long-term sexual dysfunction in adult-
hood in clinical samples [20–22]. Furthermore,
data from population-based studies reveal that
CSA, which is a common phenomenon, contrib-
utes to a significant impairment in the sexual func-
tioning of adults, especially in women [23]. In
contrast to that, a recent study on 699 college
students who anonymously completed question-
naires on sexuality and sexual abuse history
revealed differences between women who experi-
enced sexual abuse and non-abused controls for
sexual satisfaction, but not on the FSFI sum score
[21]. Interestingly, a meta-analytic study supports
the hypothesis that sexual dysfunction affects a
significant but quite small percentage of those who
have experienced CSA in a long-lasting and severe
manner [24].
Additional factors like better coping strategies,
personality traits [25] that may constitute a vulner-
ability to develop a personality disorder like BPD,
but also the level of ferocity and the relationship
with the abuser (e.g., a family member), may be
factors that contribute to suffering from sexual
dysfunction in adulthood.
Very little experimental data on the possible
mechanisms for how CSA may influence sexual
function in adulthood is available. An activation of
the sympathetic nervous system by physical exer-
cise did increase sexual arousal in healthy subjects,
but not in the CSA plus PTSD group [26]. More-
over, a subgroup of CSA survivors revealed in-
creased cortisol levels after exposure to a sexually
stimulating video, which may reflect an increased
automatic fear response to sexual stimuli [27]. In a
sample of 56 women with and without a history of
CSA, a study using an implicit association test
indicated a lack of excitatory cognitive and affec-
tive responses to sexual stimuli [28]. In this study,
however, sex was not more strongly associated
with an unpleasant valence compared to daily
activities. Sexual self-schemas, describing how
people make sense of the sexual self and how they
react to sexual stimuli, were investigated in CSA
survivors and controls. For cohabitating partners,
there was a significant relationship between CSA
and negative affect, which was mediated by the
“romantic/passionate” schema. This relationship
was independent from depression anxiety [29].
Thus, the first available studies on this issue point
to complex physiological but also psychological
(cognitive and emotional) changes that contribute
to impaired sexual function in CSA survivors.
Further studies are warranted to elucidate the neu-
rophysiological and sociopsychological mecha-
nisms of sexual dysfunction in this context.
In addition, BPD women show a trend for
describing themselves as more bisexually-oriented
as compared to healthy controls. This trend might
hypothetically reflect a part of general and sexual
identity disturbance probably due to an ambiva-
lence resulting from a heterosexual orientation
in combination with an abuse-derived coping
strategy of sexuality. In a prospective 10-year-
follow-up study investigating the prevalence of
homo- and bisexuality in 290 BPD patients, of
whom 233 were female, compared to 72 subjects
with other personality disorders, BPD patients
revealed significantly more homo- and bisexual
orientations [30]. In the present study, 13.3% of
the healthy women described themselves as homo-
sexual. Depending on the definition of homosexual
3360
Schulte-Herbrüggen et al.
J Sex Med 2009;6:3356–3363

orientation, the prevalence in large surveys of
national population-based samples in the United
States and France was approximately 11% regard-
ing “homosexual attraction but no homosexual
behavior,” and
⫾18% regarding “homosexual
attraction and behavior.” Examination of “homo-
sexual behavior separately” finds that only about
3% of the females report real homosexual contacts
[31]. In the present study, we did not differentiate
between sexual attraction, sexual self-definition,
and sexual behavior; and pre-orgasmic imagina-
tion, thus, the prevalence of sexual orientation
should be interpreted with caution, and further
research is needed to address this topic.
The concept of sexual orientation as a dimen-
sional paradigm of erotic experience (above all,
pre-orgasmic fantasies) and sexual behavior with
inexact transition between hetero-, homo-, and
bisexuality has been widely discussed [32]. The
large number of self-reports of bisexuality in BPD
may reflect identity disturbance, which is listed
in the DSM-IV [1] as a criterion for BPD, and
describes an uncertainty about sexual orientation
as a part of an indefinite sexual identity. Former
studies have repeatedly pointed to an association
between homosexuality and bisexuality, especially
in male BPD patients, compared to the prevalence
in the general population [33,34]. It has even been
suggested that homosexual orientation in a pre-
dominantly heterosexual environment increases
identity confusion, and therefore, promotes a
higher prevalence of BPD among homosexually
or bisexually oriented individuals [35]. However,
there has been controversial discussion about this
issue since research on the association between
BPD and homosexuality may have not sufficiently
taken into consideration the possible sexual orien-
tation bias in diagnoses of BPD that were based on
DSM-III and -IIIR criteria [36,37].
The DSM-IV states that patients with BPD may
experience sudden changes in sexual identity, but
takes into account that conflicts about sexual ori-
entation, especially in young adults, are a frequent
but often transient problem within healthy per-
sonality development, and therefore should not be
mistakenly diagnosed as a criterion for BPD.
Some important limitations of the present study
have to be taken into consideration. Sexual dys-
function and the type of trauma were only assessed
by questionnaires. Additional clinical exploration
of sexual problems by a senior psychiatrist as con-
ducted for the assessment of Axis I and II disorders
would have supported the clinical significance of
impaired sexual function as assessed by the FSFI.
Furthermore, the study does not include a struc-
tured clinical exploration of the reasons for the
sexual abstinence that was reported by an impor-
tant number of women in both groups. In addi-
tion, verification of reported sexual traumatization
(e.g., by asking family members or court records)
would have increased the validity of the assessment
of trauma type. Also, subthreshold PTSD and
severity of PTSD symptoms were not considered
in the present study. The study includes a small
number of women, but provides highly significant
findings. Further studies in larger samples are
needed to replicate the results. Furthermore, in
the current study we did not assess sexual dysfunc-
tion according to DSM-IV criteria. Also, medical
conditions that could influence sexual function,
libido, or sexual activity were only considered to be
absent according to clinical interview, and were
not assessed using structured methods (e.g., lab
tests).
In conclusion, sexual traumatization in women
with BPD closely determines sexual dysfunction.
In addition, current depression or SSRI medica-
tion are the main causes for sexual abstinence in
these patients. These factors are common phe-
nomena in BPD. Therefore, this may have great
impact on diagnostic procedures as well as thera-
peutic intervention in BPD patients, especially
when the issue of partnership and sexuality is con-
cerned. In our sample, an remarkable number of
the women with BPD reported themselves to be
bisexual, which might hypothetically reflect the
BPD typical identity disturbance.
Acknowledgment
The authors thank Jane Thompson for the linguistic
revision.
Corresponding Author: Stefan Roepke, MD, Depart-
ment of Psychiatry and Psychotherapy, Charité-
University
Medicine
Berlin,
Campus
Benjamin
Franklin, Eschenallee 3, D-14050 Berlin, Germany,
EU. Tel: +49-30-8445-8796; Fax: +49-30-8445-8365;
E-mail: stefan.roepke@charite.de
Conflict of Interest: None.
Statement of Authorship
Category 1
(a) Conception and Design
Stefan Roepke; Julia-Maleen Kronsbein; Olaf
Schulte-Herbrüggen; Christoph J. Ahlers
Sexual Function in BPD
3361
J Sex Med 2009;6:3356–3363

(b) Acquisition of Data
Julia-Maleen Kronsbein; Aline Vater; Anke Rüter;
Scharif Bahri
(c) Analysis an Interpretation of Data
Stefan Roepke; Olaf Schulte-Herbrüggen; Anke
Rüter; Scharif Bahri
Category 2
(a) Drafting the Manuscript
Stefan Roepke; Olaf Schulte-Herbrüggen; Aline
Vater
(b) Revising It for Intellectual Content
Scharif Bahri; Christoph J. Ahlers; Julia-Maleen
Kronsbein
Category 3
(a) Final Approval of the Completed Manuscript
Julia-Maleen Kronsbein; Anke Rüter; Olaf Schulte-
Herbrüggen; Christoph J. Ahlers; Aline Vater;
Stefan Roepke
References
1 American Psychiatric Association. Diagnostic and
statistical manual of mental disorders. 4th edition.
American Psychiatric Association: DSM-IV; 1994.
2 Grant BF, Chou SP, Goldstein RB, Huang B,
Stinson FS, Saha TD, Smith SM, Dawson DA,
Pulay AJ, Pickering RP, Ruan WJ. Prevalence,
correlates, disability, and comorbidity of DSM-IV
borderline personality disorder: Results from the
Wave 2 National Epidemiologic Survey on Alcohol
and Related conditions. J Clin Psychiatry 2008;69:
533–45.
3 New AS, Triebwasser J, Charney DS. The case for
shifting borderline personality disorder to Axis I.
Biol Psychiatry 2008;64:653–9.
4 First MB, Spitzer RL, Gibbon M, Williams JB.
User’s guide for the structured clinical interview
for DSM-IV personality disorders (SCID II). Wash-
ington, DC: American Psychiatric Press; 1996.
5 Lavan H, Johnson JG. The association between axis
I and II psychiatric symptoms and high-risk sexual
behavior during adolescence. J Personal Disord
2002;16:73–94.
6 Hull JW, Clarkin JF, Yeomans F. Borderline per-
sonality disorder and impulsive sexual behavior.
Hosp Community Psychiatry 1993;44:1000–2.
7 Miller FT, Abrams T, Dulit R, Fyer M. Substance
abuse in borderline personality disorder. Am J Drug
Alcohol Abuse 1993;19:491–7.
8 Zanarini MC, Parachini EA, Frankenburg FR,
Holman JB, Hennen J, Reich DB, Silk KR. Sexual
relationship difficulties among borderline patients
and axis II comparison subjects. J Nerv Ment Dis
2003;191:479–82.
9 Sansone RA, Barnes J, Muennich E, Wiederman
MW. Borderline personality symptomatology and
sexual impulsivity. Int J Psychiatry Med 2008;38:53–
60.
10 Beitchman JH, Zucker KJ, Hood JE, daCosta GA,
Akman D. A review of the short-term effects of
child sexual abuse. Child Abuse Negl 1991;15:537–
56.
11 Paolucci EO, Genuis ML, Violato C. A meta-
analysis of the published research on the effects of
child sexual abuse. J Psychol 2001;135:17–36.
12 Rellini A. Review of the empirical evidence for a
theoretical model to understand the sexual problems
of women with a history of CSA. J Sex Med 2008;
5:31–46.
13 Zemishlany Z, Weizman A. The impact of mental
illness on sexual dysfunction. Adv Psychosom Med
2008;29:89–106.
14 Hurlbert DF, Apt C, White LC. An empirical
examination into the sexuality of women with
borderline personality disorder. J Sex Marital Ther
1992;18:231–42.
15 Wiegel M, Meston C, Rosen R. The female sexual
function index (FSFI): Cross-validation and devel-
opment of clinical cutoff scores. J Sex Marital Ther
2005;31:1–20.
16 Rosen R, Brown C, Heiman J, Leiblum S, Meston
C, Shabsigh R, Ferguson D, D’Agostino R Jr. The
Female Sexual Function Index (FSFI): A multidi-
mensional self-report instrument for the assessment
of female sexual function. J Sex Marital Ther 2000;
26:191–208.
17 Berner MM, Kriston L, Zahradnik HP, Härter M,
Rohde A. Validity and reliability of the German
female sexual function index (FSFI-d). Geburtshilfe
Frauenheilkd 2004:293–303.
18 Clayton AH. Female sexual dysfunction related to
depression and antidepressant medications. Curr
Womens Health Rep 2002;2:182–7.
19 Martin-Du PR, Baumann P. [Sexual dysfunctions
induced by antidepressants and antipsychotics]. Rev
Med Suisse 2008;4:758–62.
20 DiLillo D. Interpersonal functioning among women
reporting a history of childhood sexual abuse:
Empirical findings and methodological issues. Clin
Psychol Rev 2001;21:553–76.
21 Rellini A, Meston C. Sexual function and satisfac-
tion in adults based on the definition of child sexual
abuse. J Sex Med 2007;4:1312–21.
22 Rumstein-McKean O, Hunsley J. Interpersonal and
family functioning of female survivors of childhood
sexual abuse. Clin Psychol Rev 2001;21:471–90.
23 Najman JM, Dunne MP, Purdie DM, Boyle FM,
Coxeter PD. Sexual abuse in childhood and sexual
dysfunction in adulthood: An Australian population-
based study. Arch Sex Behav 2005;34:517–26.
24 Rind B, Tromovitch P, Bauserman R. A meta-
analytic examination of assumed properties of child
sexual abuse using college samples. Psychol Bull
1998;124:22–53.
25 Harris JM, Cherkas LF, Kato BS, Heiman JR,
Spector TD. Normal variations in personality are
associated with coital orgasmic infrequency in
3362
Schulte-Herbrüggen et al.
J Sex Med 2009;6:3356–3363

heterosexual women: A population-based study.
J Sex Med 2008;5:1177–83.
26 Rellini AH, Meston CM. Psychophysiological
sexual arousal in women with a history of child
sexual abuse. J Sex Marital Ther 2006;32:5–
22.
27 Rellini A, Hamilton LD, Delville Y, Meston C.
Association between dissociation and cortisol
response during states of heightened physiological
sexual arousal in women with a history of child
sexual abuse. International Society for the Study of
Women’s Sexual Health 2007.
28 Rellini A, Ing D, Meston C. Implicit and explicit
cognitive processes and sexual arousal in survivors of
child sexual abuse. Meeting of the International
Society for the Study of Women’s Sexual Health
2006.
29 Meston CM, Rellini AH, Heiman JR. Women’s
history of sexual abuse, their sexuality, and sexual
self-schemas. J Consult Clin Psychol 2006;74:229–
36.
30 Reich DB, Zanarini MC. Sexual orientation and
relationship choice in borderline personality disor-
der over ten years of prospective follow-up. J Per-
sonal Disord 2008;22:564–72.
31 Sell RL, Wells JA, Wypij D. The prevalence of
homosexual behavior and attraction in the United
States, the United Kingdom and France: Results of
national population-based samples. Arch Sex Behav
1995;24:235–48.
32 Rubio-Aurioles E, Wylie K. Sexual orientation
matters in sexual medicine. J Sex Med 2008;5:1521–
33.
33 Dulit RA, Fyer MR, Miller FT, Sacks MH, Frances
AJ. Gender differences in sexual preference and sub-
stance abuse in inpatients with borderline personal-
ity disorder. J Personal Disord 1993;7:182–5.
34 Zubenko GS, George AW, Soloff PH, Schulz P.
Sexual practices among patients with borderline
personality disorder. Am J Psychiatry 1987;144:
748–52.
35 Silverstein C. The borderline personality disorder
and gay people. J Homosex 1988;15:185–212.
36 American Psychiatric Association. Diagnostic and
statistical manual of mental disorders. 3rd edition.
Washington, DC: American Psychiatric Press; 1980.
37 American Psychiatric Association. Diagnostic and
statistical manual of mental disorders. 3rd edition
rev. Washington, DC: American Psychiatric Press;
1987.
Sexual Function in BPD
3363
J Sex Med 2009;6:3356–3363

Copyright of Journal of Sexual Medicine is the property of Blackwell Publishing Limited and its content may
not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written
permission. However, users may print, download, or email articles for individual use.
Wyszukiwarka
Podobne podstrony:
A Ser49Cys Variant in the Ataxia Telangiectasia, Mutated, Gene that Is More Common in Patients with
Personality Constellations in Patients With a History of Childhood Sexual Abuse
Effects of Clopidogrel?ded to Aspirin in Patients with Recent Lacunar Stroke
Difficult airway management in a patient with traumatic asphyxia
Dialectic Beahvioral Therapy Has an Impact on Self Concept Clarity and Facets of Self Esteem in Wome
Konstatinos A Land versus water exercise in patients with coronary
Muscle Mass Gain Observed in Patients with Short Bowel Syndrome
Difficult airway management in a patient with traumatic asphyxia
Proton Magnetic Resonance Spectroscopy of the Medial Prefrontal Cortex in Patients With Deficit Schi
Serum cytokine levels in patients with chronic low back pain due to herniated disc
The Effects of Probiotic Supplementation on Markers of Blood Lipids, and Blood Pressure in Patients
Effect of high dose intravenous ascorbic acid on the level of inflammation in patients with rheumato
The relationship of Lumbar Flexion to disability in patients with low back pain
Chromatopelma cyaneopubescens First detailed breeding in captivity with notes on the species Journal
The World Is Flat Brief History of the Twenty First Century
Loyalty in National Socialism, A Contribution to the Moral History of the National Socialist Period
High Choline Concentrations in the Caudate Nucleus in Antipsychotic Naive Patients With Schizophreni
A nonsense mutation (E1978X) in the ATM gene is associated with breast cancer
Pathological dissociation and neuropsychological functioning in BPD
więcej podobnych podstron