
Quality of life and disparities among long-term cervical
cancer survivors
Howard P. Greenwald
&
Ruth McCorkle
&
Kathy Baumgartner
&
Carolyn Gotay
&
Anne Victoria Neale
Received: 14 July 2013 / Accepted: 13 February 2014
# Springer Science+Business Media New York 2014
Abstract
Purpose Little population-based research has been done on
social, economic, and environmental factors affecting quality
of life (QOL) among long-term cancer survivors. This re-
search assesses the impact of disease and nondisease factors
on QOL among long-term survivors of cervical cancer.
Methods In a collaborative, observational study, data were
obtained from cancer registries, interviews, and self-
administered questionnaires. Comparisons of QOL were made
between women with cervical cancer histories and women from
the general population. A total of 715 women 4
–28 years
postdiagnosis were identified from cancer registries in Con-
necticut (N=208), Detroit Metropolitan Area (N=211), New
Mexico (N=197), and Hawaii (N=99). QOL was measured
according to four SF-36 dimensions
—physical functioning,
social functioning, bodily pain, and general health status.
Results Means on SF-36 measures among women with cer-
vical cancer histories were close to or higher than women in
the general population. In a multiple regression analysis,
economic disadvantage negatively predicted physical func-
tioning (B=−13.4, SE=2.1), social functioning (B=−13.2,
SE=2.4), bodily pain (B=−12.6, SE=2.5), and general health
(B=−12.8, SE=2.1). Residence in New Mexico negatively
predicted several QOL dimensions. No impact of race was
detected when income was controlled. Disease stage did not
predict QOL.
Conclusions Cervical cancer does not generally reduce QOL
among long-term survivors. Economic disadvantage and res-
idential location affect QOL through mechanisms yet to be
determined.
Implications for Cancer Survivors Women diagnosed with
cervical cancer have good prospects for high quality of life;
socioeconomic status strongly affects quality of life over the
long term.
Keywords Survivorship . Disparities . Quality of life .
Women
’s health . Cancer
Introduction
Concern with quality of life (QOL) has grown as the life
expectancy of cancer survivors has increased. Racial and
socioeconomic factors reportedly help determine outcomes
of cancer and other diseases [
]. Research has begun to
demonstrate the existence of disparities in health-related qual-
ity of life (QOL) across several nondisease dimensions [
,
Although consequences of survivable cancers and their treat-
ment may become most apparent over the entire life course,
foregoing research has typically examined the experience of
short-term survivors. The research reported here assesses the
impact of both disease and nondisease factors, including race,
socioeconomic status, and geography, on QOL among long-
term survivors of cervical cancer.
According to the American Cancer Society, 12,340 cases of
invasive cancer of the uterine cervix were expected to occur in
the USA in 2013 [
]; an additional 50,000 noninvasive (in
situ) cases can be expected yearly. In 2013, nearly 250,000
H. P. Greenwald (
*)
Sol Price School of Public Policy, University of Southern California,
650 Childs Way, Los Angeles, CA 90089-0626, USA
e-mail: greenwa@usc.edu
R. McCorkle
Yale University, New Haven, CT, USA
K. Baumgartner
University of Louisville, Louisville, KY, USA
C. Gotay
University of British Columbia, Vancouver, BC, Canada
A. V. Neale
Wayne State University, Detroit, MI, USA
J Cancer Surviv
DOI 10.1007/s11764-014-0352-8
women in the USA were alive with histories of invasive
cervical cancer [
]. When women with histories of noninva-
sive disease are added, survivors likely totaled well over one
million. Because cervical cancer frequently occurs among
young women, it is capable of affecting QOL across a broad
range of the life course.
Researchers have reported widespread challenges to QOL
among cancer survivors [
], with low QOL more frequent
among the socially disadvantaged [
]. Several studies have
identified racial and ethnic disparities in QOL among cancer
survivors. Assessments of QOL in breast, colorectal, and pros-
tate cancer have detected poorer QOL among racial and ethnic
minorities than among Caucasian survivors [
]. A study
specifically focused on QOL among cervical cancer survivors
found disparities between Hispanic and non-Hispanic women
on social, emotional, and body image dimensions [
]. A meta-
analysis of 21 studies reported Hispanic survivors to have
significantly lower QOL than other groups [
], and a recent
literature review found African-American cancer survivors to
have lower QOL than Caucasians [
Several generations of researchers have addressed the prob-
lem of reduced QOL among cancer survivors of all back-
grounds [
]. In cervical and other gynecological malig-
nancies, survivors reportedly face special challenges such as
difficulty in marital relations, disappointment due to loss of
childbearing ability, and issues regarding sexuality, sexual
function, and sexual identity [
]. Recent studies and
commentaries have drawn particular attention to long-term
and late effects of cancer and cancer treatment [
The research reported here is intended to help build more
complete understanding of the long-term impact of cervical
cancer on QOL and the determinants of low QOL among
cervical cancer survivors. Unlike many earlier studies, this
research utilizes data drawn from population-based sources
rather than individual treatment facilities, focuses on survivor-
ship well beyond the often-cited 5-year marker, and covers
several varied geographical areas in which key minority groups
are widely represented. Representation of minorities is particu-
larly important in view of growing interest in health disparities.
Methods
Data
The investigators identified women with histories of cervical
cancer through Surveillance, Epidemiology and End Results
(SEER) registries in Connecticut, Michigan (Detroit area),
New Mexico, and Hawaii between 2000 and 2003. Led by
principal investigators at four universities (Yale, Wayne State,
University of New Mexico, and University of Hawaii), these
studies were funded independently by the National Cancer
Institute and approved by the Institutional Review Board of each
grantee organization. After deletion of individual identifiers,
data were pooled for the purpose of collaborative analysis. Data
were collected between December, 2001, and December, 2003.
SEER is a population-based cancer surveillance program
supported by the National Cancer Institute. The completeness
and reliability of SEER registries has been widely researched
[
]. SEER records include dates of diagnosis and treat-
ment, stage, basic demographics, and geographic information.
Individuals identified through SEER were contacted by per-
sonnel associated with each individual SEER registry and
interviewed in person or via telephone or sent mail question-
naires. Similar procedures were used at all sites to obtain
physician permission to contact cervical cancer survivors.
Assessments of potential response bias in these data are
reported in publications based on data from two research sites.
In Connecticut, a response rate of 85 % was obtained, and the
respondents did not differ by statistically significant margins
from all cervical cancer survivors in the registry in age, stage,
and county of residence [
]. Metropolitan Detroit reported a
response rate of 62 %, but age and stage of survey respondents
did not differ from those of nonrespondents [
]. The re-
sponse rates for Hawaii and New Mexico were 34 and
16 %, respectively. Comparison of respondents in Hawaii
and New Mexico with 2010 census data suggests overrepre-
sentation of Caucasians at both sites.
Subject selection for the study differed across the four
research sites. The Connecticut protocol restricted accrual to
women with histories of invasive cancer. Research teams
using the other registries accrued both in situ and invasive
cases. At the Connecticut, New Mexico, and Hawaii sites,
research teams interviewed all individuals in the registries
who met the study criteria, whose physicians gave consent,
who could be reached during the study period, and who were
willing to be interviewed. In the Detroit area, an identical
recruitment procedure was used, except that a random sample
of potential subjects was selected and approached. The sam-
pling method and rationale are described elsewhere [
]. A
total of 715 observations were obtained.
To compare cervical cancer patients with national QOL-
related norms, the researchers utilized data from the National
Survey of Functional Health Status (NHS). Conducted in
1990, the NHS was a cross-sectional survey designed to
obtain national normative data for the SF-36, a measure which
will be described below. The sampling frame for the NHS was
drawn from the 1989 and 1990 sampling frames of the Gen-
eral Social Survey, an annual survey of non-institutionalized
adults in the USA. Conducted via telephone and mail, the
NHS oversampled individuals over age 65; 2,474 responses
were obtained, a response rate of 77 % [
Although the NHS and the study of cervical cancer survi-
vors reported here were carried out approximately a decade
apart, comparison of means from the two data sources remains
valid. Strong differences in women
’s health did not seem to
J Cancer Surviv

have developed across this interval. Data on related metrics
for comparable intervals are available from the National
Health Interview Survey. Among women interviewed in
1991, 2000, and 2003, 10.1, 9.3, and 9.6 % reported that their
health status was fair or poor (as opposed to excellent, very
good, or good). Among women interviewed in 1990, 2001,
and 2002, 13.0, 11.9, and 12.3 % reported limitations on
activity caused by chronic disease (as opposed to no such
limitations) [
,
].
Measures
Quality of life among cervical cancer survivors was assessed
according to four composite indicators from the SF-36
—
physical functioning, social functioning, bodily pain, and
general health. The SF-36, perhaps the world
’s most widely
used instrument for assessing health-related quality of life,
consists of eight scales measuring various dimensions of
functional health status [
]. The SF-36 has undergone
extensive reliability and validity testing and assessment of
differences between telephone and mail responses [
Although questions comprising all eight were administered
in the data collection procedure described above, only four are
reported here. Two of the research teams (Yale and University
of Hawaii) used version 1 of the SF-36 instrument, while two
(Wayne State and the University of New Mexico) used version
2, which contains minor modifications of wording for some
items and, for some items, a different number of response
options. Both SF-36 versions continue in widespread use. For
the four dimensions used here, all component items and asso-
ciated response options on versions 1 and 2 of the SF-36
instruments are identical.
The SF-36 physical functioning scale is based on ten
questions asking subjects about their ability to perform activ-
ities such as walking, lifting, bathing, or dressing. The social
functioning scale comprises two questions regarding the fre-
quency and extent to which health problems have interfered
with social activities. The bodily pain scale includes two
items, one focusing on amount of pain experienced in the past
4 weeks, the other on the degree to which pain interfered with
the subject
’s normal work. The general health scale is based
on five questions about the subject
’s self-perceived current
health status and expectations regarding future health.
Analysis
Data analysis focused on testing of four hypotheses. Three are
based on the literature summarized above:
H
1
—Cervical cancer survivors will have lower QOL than
comparable women assumed not to have histories of
cervical cancer.
H
2
—Black and Latina cervical cancer survivors will have
lower QOL than Caucasian survivors.
H
3
—Economically disadvantaged cervical cancer survi-
vors will have lower QOL than non-disadvantaged
survivors.
A final hypothesis was based on the general expectation
that more extensive disease would result in lower QOL:
H
4
—Cervical cancer survivors with histories of invasive
disease will have lower QOL than women diagnosed with
in situ disease; among women with invasive disease,
those with histories of higher stage cancer will have lower
QOL than those at lower stage.
To test H
1
, means on the SF-36 physical functioning, social
functioning, bodily pain, and general health scales were com-
puted, and comparison made with means on these indicators
obtained from the NHS [
]. This procedure was intended to
assess whether QOL of the cervical cancer survivors in this
study differed from the general population of women. In view
of the prevalence of cancer history of any kind among adult
women in the USA during the data collection period (about
6.5 million) [
] in an adult female population approximat-
ing103 million), this procedure compared cervical cancer
survivors with women largely without histories of cancer.
Statistical significance of differences between means on the
sample of cervical cancer survivors and subjects in the nation-
al survey were assessed via z scores.
Cervical cancer survivors were compared with women in the
NHS first for all cervical cancer survivors and then for nonmi-
nority (Caucasian) subjects only. Although limited in scope, a
comparison of nonminority subjects with the national sample
may be more valid than a comparison of all cervical cancer
survivors with the national survey. In the cervical cancer survi-
vor sample as a whole, African-Americans, a key disadvan-
taged group, were underrepresented. Percentages of Asian-
Americans and Latinas in the cervical cancer survivor sample
approximated their percentage in the USA population as a
whole. But most Latinas and Asian-Americans in the cervical
cancer sample resided, respectively, in New Mexico and Ha-
waii, and their responses to a history of cervical cancer may
differ from those of their counterparts in other locations.
The investigators assessed H
2
through H
4
through multiple
regression (OLS) equations predicting the SF-36 variables.
Ethnic category was entered into regression equations as di-
chotomous variables for African-American, Asian-American,
and Hispanic, with Caucasian omitted as a referent. Economic
disadvantage was conceptualized as relatively low income, and
represented in the equations as a dichotomous variable indicat-
ing lowest income quartile among subjects from each catch-
ment area. Lowest income quartile was used as an index of
economic disadvantage rather than a specific dollar figure to
J Cancer Surviv
adjust for differences in income distribution and cost of living
across the four study catchment areas. Locale was represented
as dichotomous variables representing Detroit, New Mexico,
and Hawaii, with Connecticut omitted as a referent.
Separate sets of regressions were computed for all women
in the sample and women diagnosed with invasive diseases. In
the first of these analyses, stage was represented as a dichot-
omous variable (in situ vs. invasive), and in the second as a
continuous three-degree variable (stages I, II, and III). In all
equations, time since diagnosis and age at interview were
entered as contextual variables.
Results
Women accrued in the study were 4
–28 years post-diagnosis;
their ages at time of interview ranged from 26 to 92 years.
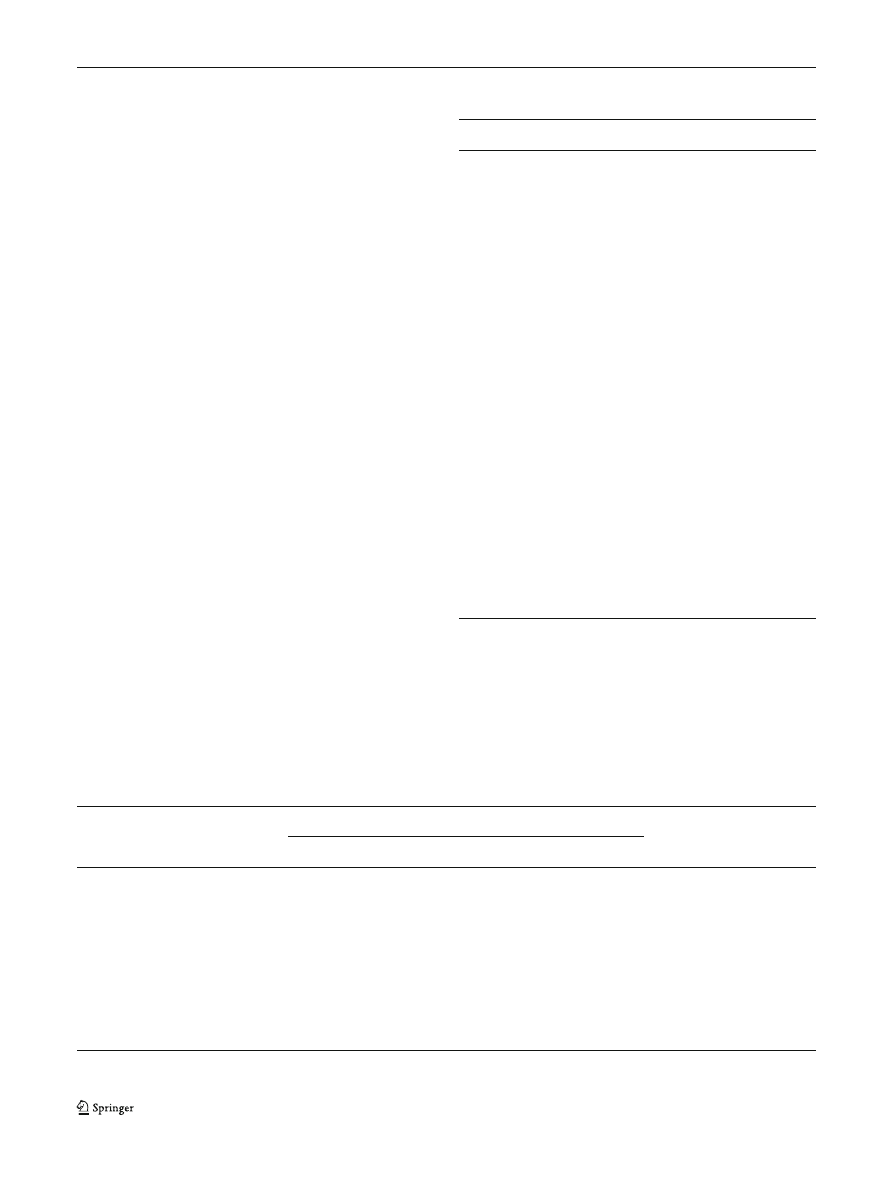
Table
compares the characteristics of the samples obtain-
ed from the Connecticut, Detroit, New Mexico, and Hawaii
registries. Demographic features of each sample reflect differ-
ences in the populations of each SEER site. In addition,
differences across sites are visible in extent of initial disease
(in situ vs. invasive), a consequence of the differences in data
collection protocols of each group of investigators.
Addressing hypothesis H
1
, Table
compares means on the
four SF-36 scales obtained from the cervical cancer survivors
with means from the NHS [
]. Higher scores on the SF-36
scales correspond to higher levels of health-related QOL. For
example, a high numerical score on the SF-36 bodily pain
scale would mean that the subject had, over the preceding
4 weeks, experienced little pain and when pain was experi-
enced it had little if any impact on daily activities. Because
SF-36 scores differ by age in the national sample, and because
age distribution differs across the four cervical cancer survivor
samples, comparisons in Table
are made within 10-year age
groups. Table
presents findings based on all cases accrued.
Generally, means on all four SF-36 scales were higher for
the cervical cancer survivors than the national sample. The
strongest relationships were found within the older age groups
(45 years and over). All statistically significant differences
occurred in relationships in which the cervical cancer
Table 1 Characteristics of sample
Site
Total
p
Connecticut
Detroit
New Mexico
Hawaii
Race
Caucasian (percent)
92.8
84.5
67.5
40.2
75.2
<0.001
Asian (percent)
1.9
0
0
56.7
8.3
<0.001
African-American (percent)
4.3
13.1
0
0
5.0
<0.001
Hispanic (percent)
0
0.5
32.5
0
9.1
<0.001
Age at interview (mean)
55.2
52.0
58.5
51.4
53.7
<0.001
Invasive disease (percent)
98.4
27.1
47.9
30.3
53.2
<0.001
Years since diagnosis (mean)
14.0
9.2
21.4
10.1
12.5
<0.001
Total cases
208
211
197
99
715
Percentages for
“other” or unknown race (N=17) not presented
Table 2 Means on SF-36 dimensions
—cervical cancer survivors vs.
national sample
Age group
Cervical cancer survivors National sample z-score
Dimension: physical functioning
25
–34
91.9
89.1
0.77
35
–44
89.6
88.1
0.97
45
–54
86.6
82.9
2.80**
55
–64
77.9
73.1
2.24*
65 and over 69.6
61.9
2.96**
Dimension: social functioning
25
–34
84.1
84.1
0.017
35
–44
82.7
83.1
−0.196
45
–54
80.8
82.7
−1.48
55
–64
80.9
79.4
0.735
65 and over 83.8
77.0
2.63**
Dimension: bodily pain
25
–34
82.7
79.6
0.75
35
–44
76.6
74.9
0.87
45
–54
74.4
72.1
1.57
55
–64
73.9
66.6
3.73***
65 and over 74.7
63.4
4.57***
Dimension: general health
25
–34
74.6
74.8
−0.053
35
–44
71.3
74.3
−1.71
45
–54
71.6
70.5
0.836
55
–64
68.3
62.9
3.08**
65 and over 67.1
61.6
2.70**
*p<0.05; **p<0.01; ***p<0.001
J Cancer Surviv
survivors had higher SF-36 scores than the national sample.
Differences of this kind were found for all four SF-36 scales.
Recognizing the underrepresentation of African-
Americans and potential differences between minorities
in New Mexico and Hawaii and their counterparts else-
where, comparison of SF-36 means was also made
using data only on Caucasian cervical cancer survivors.
Findings from this comparison were nearly identical
with those presented in Table
.
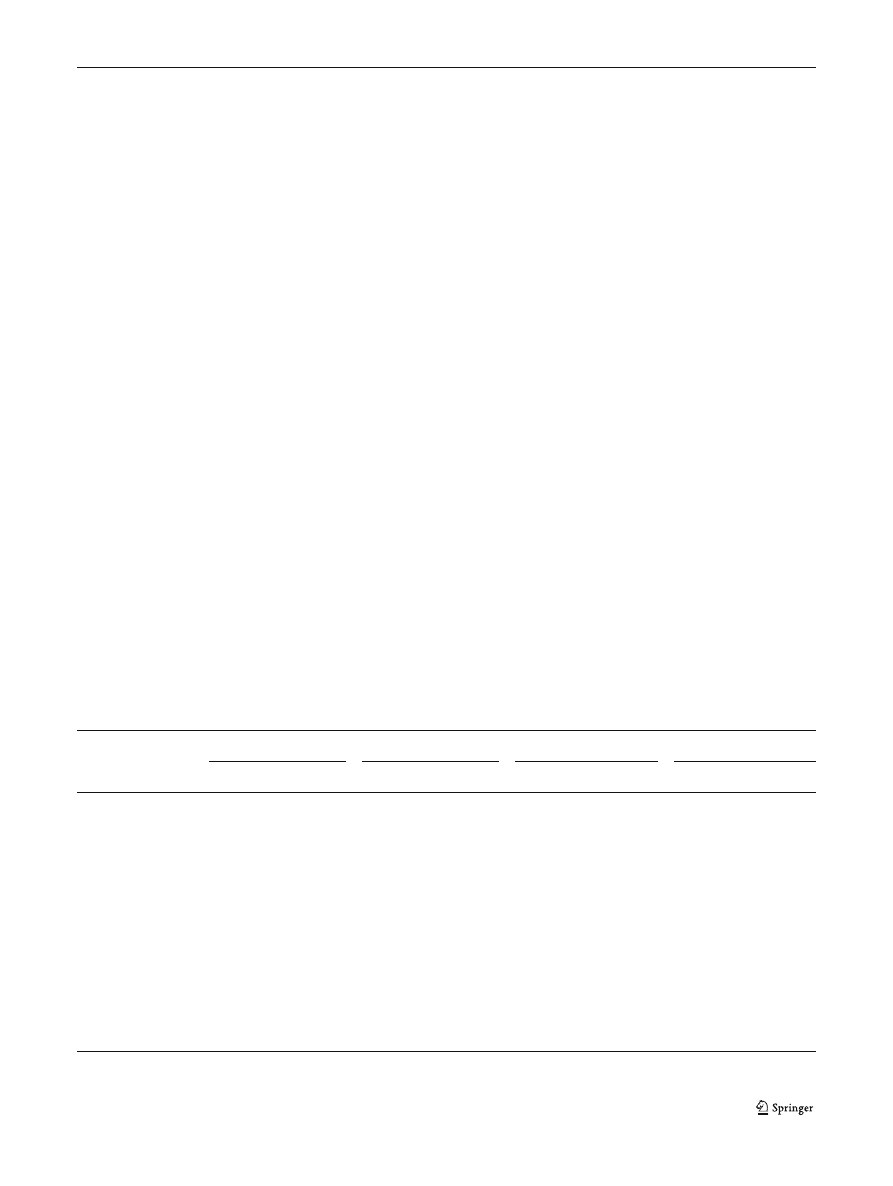
Table
presents coefficients from OLS equations testing
H
2
through H
4
. These equations predict QOL among all
individuals accrued. Age at interview significantly predicts a
lower score on the SF-36 physical functioning dimension
(p<0.001) but has no significant relations with other SF-36
scales. Neither years since diagnosis nor race predicts any of
the dependent variables. Residence in New Mexico predicts
lower scores on three of the four SF-36 dimensions (p<0.05).
Income in the lowest quartile of subjects from each site was
the strongest and most consistent predictor of SF-36 dimen-
sions, economic disadvantage according to this measure
predicting lower scores on all the SF-36 measures
(p<0.001). To aid interpretation of Table
, a table appears
in the
to this article presenting means on the depen-
dent variables by race and research site.
Notably, stage (represented as in situ vs. invasive) did not
predict QOL according to any of the SF-36 measures. The
analysis reported in Table
was repeated for only invasive
cases, the equations including a continuous variable
representing stages I through III. Stage did not predict QOL
in any of these equations; economic disadvantage and resi-
dence in New Mexico continue to strongly predict QOL on all
dimensions.
Discussion
Because this study follows survivors of cervical cancer over
an extended portion of the life course, it provides a more
comprehensive picture of the disease
’s consequences for
QOL than earlier studies. Unlike most previous studies, it
includes subjects who were treated at many different facilities
and reside in a broad range of geographic locations across the
USA. Of the four hypotheses presented above, only H
3
re-
ceived support, highlighting the importance of a key dimen-
sion of socioeconomic status in predicting quality of life
among long-term cervical cancer survivors.
The study suggests that most women who have survived
cervical cancer compare favorably with similarly aged women
in the general population, most of whom have not had cervical
cancer or other malignancies. Among the long-term cervical
cancer survivors on whom this study reports, those in higher
age categories have the most favorable scores on four key SF-
36 scales relative to their counterparts in the general population.
The study reports a strong relationship between economic
disadvantage and low QOL, as indicated by all of the four SF-
36 indicators used in this article. None of the minority groups
represented in this study differed from Caucasian subjects on
any of the four SF-36 scales after economic disadvantage,
residential location, and other background variables had been
controlled. New Mexico residents, regardless of race or eco-
nomic disadvantage, were found to have lower QOL than
cervical cancer survivors accrued elsewhere.
The observation that cervical cancer survivors in the older
age groups have higher QOL than women in the same age
ranges without histories of cervical cancer suggests that an
effective process of adaptation may take place in this disease.
Table 3 Regression of disease features, residence, race, and income quartile on SF-36 dimensions
Physical functioning
Social functioning
Bodily pain
General health
B
95 % CL
B
95 % CL
B
95 % CL
B
95 % CL
Age at interview
−0.54***
−0.72/−0.37
0.02
−0.17/0.22
−0.051
−0.26/0.16
−0.042
−0.22/0.13
Invasive disease
0.17
−4.10/4.34
−0.43
−5.03/4.44
−1.974
−7.06/3.10
−2.385
−6.66/1.89
Years since diagnosis
−0.17
−0.57/0.22
0.10
−0.35/0.55
−0.228
−0.70/0.24
−0.169
−0.56/0.23
Research site
Detroit
−3.48
−9.40/2.42
2.64
−4.10/9.38
−1.653
−8.68/5.37
−3.201
−9.11/2.71
New Mexico
−5.78
−11.56/−0.01
−8.33*
−14.97/−1.76
−7.302*
−14.15/−0.46
−6.380*
−12.15/−6.1
Hawaii
2.49
−5.91/10.89
−2.83
−12.48/6.81
0.952
−8.99/10.90
−0.868
−9.35/7.61
Race
Asian
−2.82
−11.46/5.81
5.89
−4.00/15.79
6.265
−3.95/16.48
0.545
−8.21/9.30
African-American
−1.61
−10.19/6.97
3.98
−5.79/13.77
−1.066
−11.22/9.08
−2.110
−10.65/6.43
Hispanic
−2.15
−9.12/4.81
−3.86
−11.82/4.08
−1.985
−10.29/6.32
0.222
−6.72/7.16
Lowest income quartile
−13.44*** −17.59/−9.30 −13.18*** −17.93/−8.44 −12.555*** −17.46/−7.65 −12.811*** −16.96/−8.66
R
2
0.171
0.079
0.055
0.067
*p<0.05; **p<0.01; ***p<0.001
J Cancer Surviv

Studies of survivors of cervical and other cancers provide evi-
dence that serious illness can motivate individuals to adopt
positive approaches to life and healthier lifestyles [
] and that
the survivor
’s capacity for resilience may be more important in
determining QOL than the physical features of disease [
,
In a study comparing cancer survivors with people without
cancer histories, the oldest of the survivors evidence the least
QOL impact, potentially due to a longer period of time to adapt
to long-term physical and psychological effects [
]. Alterna-
tively, this observation may be due to increasing perceived
quality of life among older women, but definitive assessment
of this possibility is beyond the scope of the present article.
Variation in QOL among the cervical cancer survivors studied
here may have resulted at least in part from disparities in access to
health services, unmeasured in this study. Since access to health
services is related to income, reduced access may play a part in
reducing QOL among economically disadvantaged cervical can-
cer survivors. The finding in this study, that economic disadvan-
tage predicts relatively low QOL and that race has a relatively
small impact on QOL after disadvantaged economic status has
been controlled, is consistent with earlier research [
].
Residential location has been reported as a determinant of
health-related QOL [
,
], but has not been definitively
studied. Potential explanations may lie in a relative scarcity
of resources in poor communities for health services or non-
health social support. Potentially, differences in perception
may help explain the geographical disparities reported here.
It has been reported that residents of deprived communities
are generally more likely to perceive their health as poor than
residents of nondeprived communities [
It is important to emphasize that, among many individuals
who have survived cervical cancer and other serious diseases,
QOL may be determined substantially by factors independent
of the disease history. The latter possibility is supported by the
observation here that cervical cancer survivors generally enjoy
QOL comparable to or even higher than that of women with
no such histories. Furthermore, studies in a number of fields
indicate that disadvantaged socioeconomic status reduces
levels of perceived life satisfaction and personal happiness,
dimensions akin to quality of life, within largely healthy
populations [
The possibility of sampling bias must be considered in
interpreting this study
’s results. Underrepresentation of minor-
ities (and hence lower-income women) in the sample as a
whole may have biased scores on the QOL scales upward.
Even if such bias were present, the inference would remain
valid that large numbers of women with histories of cervical
cancer enjoy QOL similar to or higher than women without
such histories. If the sample were biased in favor of the
relatively advantaged, moreover, it would seem likely that
the importance of economic disadvantage would be even
greater in a completely unbiased sample. This is because
women with the very lowest income would be the most likely
to encounter barriers to health care and other resources, and
thus be at particularly elevated risk of low QOL.
The findings reported here do not fully characterize the
long-term cervical cancer survivor. Only four of eight SF-36
scales on which data were collected were addressed in this
article. Information on emotional issues captured by two of the
scales not included in the analysis would provide a more
complete picture. In addition, data on sexual adaptation col-
lected in the study but not analyzed here would be of value.
It should in no way be inferred from this study that cervical
cancer does not represent a risk for low QOL across the life
cycle. Although successful adaptation appears to be the norm,
at least 40 % of younger women in this study scored lower on
one or more of the SF-36 scales than the national mean for
their age group. The determinants of lower QOL among these
women and the part potentially played by interaction between
disease and socioeconomic and geographical factors deserve
further investigation. But the findings reported here under-
score the importance of considering social, economic, and
place-related factors capable of reducing QOL in assessing
and treating patients with histories of cancer.
Acknowledgments
This research was supported by the following grants
and contracts: SEER Special Studies Connecticut Department of Health
2001-345, NO1-PC-65064, NO1-PC-CN 77001, and NO1-PC-67007.
Conflicts of interest
None of the authors of this article have any
conflict of interest, financial or otherwise.
Appendix
References
1. Williams DR, Mohammed SA, Leavell J. Race, socioeconomic sta-
tus, and health: complexities, ongoing challenges, and research op-
portunities. Ann NY Acad Sci. 2010;1186:69
–101.
Table 4 Means of SF-36 dimensions by race and site
Physical
functioning
Social
functioning
Bodily
pain
General
health
Race
Caucasian
83.7
82.5
75.7
70.7
Asian
79.5
86.9
82.3
72.2
African-American
74.6
86.1
70.3
64.3
Hispanic
77.3
68.6
65.7
64.2
Site
Connecticut
83.9
82.8
76.4
71.9
Detroit
83.3
86.4
76.1
70.8
New Mexico
79.5
74.0
69.7
66.1
Hawaii
82.6
85.4
80.0
72.2
J Cancer Surviv

2. Kaur JS, Coe K, Rowland J. Enhancing life after cancer in diverse
communities. Cancer. 2012;118(21):5366
–73.
3. Moadel AB, Morgan CM, Dutcher J. Psychosocial needs assessment
among an underserved, ethnically diverse cancer patient population.
Cancer. 2007;109(Supplement 2):446
–54.
4. American Cancer Society. Cancer facts and figures. Atlanta:
American Cancer Society; 2013.
5. De Moor JS, Marietto AB, Parry C, Alfano MA. Cancer survivors in
the United States: prevalence across the survivorship trajectory and
implications for care. Cancer Epidemiol Biomarkers Prev.
2013;22(4):651
–70.
6. Weaver KE, Forsythe LP, Reeve BB, et al. Mental and physical
health-related quality of life among U.S. cancer survivors: population
estimates from the 2010 National Health Interview Survey. Cancer
Epidemiol Biomarkers Prev. 2012;21(11):2108
–17.
7. Richardson LC, Wingo PA, Zack MM, et al. Health-related quality of
life in cancer survivors between ages 20 and 64 years: population-
based estimates from the Behavioral Risk Factor Surveillance
System. Cancer. 2008;112(6):1380
–9.
8. Matthews AK, Tejeda S, Johnson TP, et al. Correlates of quality of
life among Africa-American and White cancer survivors. Cancer
Nurs. 2012;35(5):355
–64.
9. Ashing-Giwa KT, Lim J. Examining the impact of socioeconomic
status and socioecologic stress on physical and mental health quality
of life among breast cancer survivors. Oncol Nurs Forum. 2009;36:
79
–88.
10. Ashing-Giwa KT, Tejero JS, Kim J, et al. Cervical cancer survivor-
ship in a population based sample. Gynecol Oncol. 2009;112:358
–
64.
11. Luckett T, Goldstein D, Butlow PN, et al. Psychological morbidity
and quality of life of ethnic minority patients with cancer: a system-
atic review and meta-analysis. Lancet Oncol. 2011;12(13):1240
–8.
12. Powe BD, Hamilton J, Hancock N, et al. Quality of life of African-
American Cancer Survivors: a review of the literature. Cancer.
2007;109(Issuer Supplement 2):435
–45.
13. Davis RM, Cullin JW, Miller LS, Titus M. Physical rehabilitation. In:
Haskell WB, editor. Cancer treatment. Philadelphia: Saunders; 1986.
p. 940
–5.
14. Dobkin PL, Morrow GR. Long-term side effects in patients who have
been treated successfully for cancer. J Psychosoc Oncol. 1986;3:23
–
51.
15. Poplack DG, Brouwers P. Late CNS sequelae in long-term survivors
of childhood leukemia. Proceedings of the fifth national conference
on human values and cancer-1987. Atlanta: American Cancer
Society; 1987. p. 35
–41.
16. Bonica JJ. Importance of the problem. In: Bonica JJ, Ventafridda V,
editors. Advances in pain research and therapy. New York: Raven;
1979.
17. Daut RL, Cleeland CS. The prevalence and severity of pain in cancer.
Cancer. 1982;50:1913
–8.
18. Coyle N, Foley K. Pain in patients with cancer: profile of patients and
common pain syndromes. Semin Oncol Nurs. 1985;1:93
–9.
19. Chapman CR, Syrjala K, Sargur M. Pain as a manifestation of cancer
treatment. Semin Oncol Nurs. 1985;1:100
–8.
20. Derogatis LR, Morrow GR, Fetting J, et al. The prevalence of
psychiatric disorders among cancer patients. JAMA. 1983;249:
751
–7.
21. Kornblith AB, Anderson J, Cella DF, et al. Hodgkin disease survivors
at increased risk for problems in psychosocial adaptation. Cancer.
1992;70:2214
–24.
22. Shands ME, Lewis F, Zahlis EH. Mother and child interactions about
the mother
’s breast cancer: an interview study. Oncol Nurs Forum.
2000;27:77
–85.
23. Lewis FM, Hammond MA. Psychosocial adjustment of the family to
breast cancer: a longitudinal study. J Am Med Wom Assoc. 1996;47:
194
–200.
24. Yabroff KR, Lawrence FW, Clauser S, et al. Burden of illness in
cancer survivors: findings from a population-based national sample. J
Natl Cancer Inst. 2004;96:1322
–30.
25. Bradley CJ, Bednarek HL, Newmark D. Breast cancer survival,
work, and earnings. J Health Econ. 2003;21:757
–9.
26. Greenwald HP, Dirks SJ, Borgatta EF, et al. Work disability among
cancer patients. Soc Sci Med. 1989;29:1253
–9.
27. Corney R, Everett H, Howells A, et al. The care of patients
undergoing surgery for gynecological cancer: the need for
information, emotional support and counseling. J Adv Nurs.
1992;17:667
–71.
28. Bukovic D, Strinie T, Habek M, et al. Sexual life after cervical
carcinoma. Coll Anthropol. 2003;27:173
–80.
29. Juraskova I, Butnow P, Robertson R. Post-treatment sexual adjust-
ment following cervical and endometrial cancer: a qualitative insight.
Psycho-Oncol. 2003;12:267
–79.
30. Jensen PT, Groenvold M, Klee MC, et al. Early-stage cervical carci-
noma, radical hysterectomy, and sexual function. Cancer. 2004;100:
97
–106.
31. Elit L, Esplem MJ, Butler K, et al. Quality of life and psychosexual
adjustment after prophylactic oophrectomy for a family history of
ovarian cancer. Fam Cancer. 2001;1:149
–56.
32. Robson M, Hensley M, Barakat R, et al. Quality of life in women at
risk for ovarian cancer who have undergone risk-reducing
oophrectomy. Gynecol Oncol. 2003;89:281
–7.
33. Roussis NF, Waltrous L, Kerr A, et al. Sexual response in the patients
after hysterectomy, total abdominal versus supracervical versus vag-
inal procedure. Am J Obstet Gynecol. 2004;190:1427
–8.
34. Herzog TJ, Wright JD. The impact of cervical cancer on quality of
life
—the components and means for management. Gynecol Oncol.
2007;107:572
–7.
35. Stein KD, Syrjala KL, Andrykowski MA. Physical and psychologi-
cal long-term and late effects of cancer. Cancer. 2008;112(Issue
Supplement 11):2577
–92.
36. Ganz PA. Survivorship: adult cancer survivors. Prim Care. 2009;36:
721
–41.
37. Mettlin CJ, Menck HR, Winchester DP, et al. A comparison of breast,
colorectal, lung, and prostate cancers reported to the National Cancer
Data Base and the Surveillance, Epidemiology, and End Results
Program. Cancer. 1997;79(10):2052
–61.
38. Zippin C, Lum D, Hankey BF. Completeness of hospital cancer case
reporting from the SEER Program of the National Cancer Institute.
Cancer. 1995;76:2343
–50.
39. Greenwald HP, McCorkle R, Fennie K. Health status and adaptation
among long-term cervical cancer survivors. Gynecol Oncol.
2008;111:449
–54.
40. Bartoces MG, Severson RK, Rusin BA, et al. Quality of life and self-
esteem of long-term survivors of invasive and noninvasive cervical
cancer. J Womens Health. 2009;18(5):655
–61.
41. McHorney CA, Kosinski MA, Ware JE. Comparisons of the costs
and quality of norms for the SF-36 health survey collected by mail
versus telephone interview: results from a national survey. Med Care.
1994;32:551
–67.
42. National Center for Health Statistics. Health, United States, 1995.
Hyattsville: Public Health Service; 1996.
. Accessed 23 Dec 2013.
43. National Center for Health Statistics. Health, United States, 2005.
Hyattsville: Public Health Service; 2006.
. Accessed 23 Dec 2013.
44. Ware JE, Sherbourne CD. The MOS 36-item short form health
survey (SF-36): I. Conceptual framework and item selection. Med
Care. 1992;30:473
–83.
45. McHorney CA, Ware JE, Rachel Lu JF, et al. The MOS-36 Short
Form Health Survey (SF-36): III. Tests of data quality, scaling as-
sumptions, and reliability across diverse patient groups. Med Care.
1994;32:40
–66.
J Cancer Surviv

46. Ware JE, Kosinski MA, Gandek MA. SF-36 health survey: manual
and interpretation guide. Boston: New England Medical Center, The
Health Institute; 1993.
47. Altekruse SF, Kosary CL, Krapcho M, et al., editors. SEER Cancer
Statistics Review, 1975-2008. Bethesda: National Cancer Institute;
2008.
http://seer.cancer.gov/csr/1975_2008/
. Accessed 17 Jul 2011.
48. Greenwald HP, McCorkle R. Remedies and life changes
among invasive cervical cancer survivors. Urol Nurs.
2007;27(1):47
–53.
49. Bardwell WA, Natarajan L, Dimsdale JE, et al. Objective cancer-
related variables are not associated with depressive symptoms in
women treated for early-stage breast cancer. J Clin Oncol. 2006;24:
2420
–7.
50. Scheier MF, Helgeson VS. Really, disease doesn
’t matter? A com-
mentary on correlates of depressive symptoms in women treated for
early-stage breast cancer. J Clin Oncol. 2006;24:2407
–8.
51. Do DP, Finch BK, Basturo R, et al. Does place explain racial health
disparities? Quantifying the contribution of residential context to the
Black/White health gap in the United States. Soc Sci Med. 2008;67:
1258
–68.
52. Weaver KE, Geiger AM, Lu L, Case LD. Rural-urban disparities in
health status among US cancer survivors. Cancer. 2013;119(5):1050
–7.
53. Sathyanarayanan S, Brooks AJ, Hagen SE, et al. Multilevel analysis
of the physical health perception of employees: community and
individual factors. Am J Health Promot. 2012;26(5):e126
–36.
54. Barger SD, Donoho CJ, Wayment HA. The relative contributions of
race/ethnicity, socioeconomic status, health, and social relationships
to life satisfaction in the United States. Qual Life Res. 2009;18(2):
179
–89.
55. Yang Y. Social inequalities and happiness in the United States: 1972
–
2004: an age-period cohort analysis. Am Sociol Rev. 2008;73(2):
204
–26.
J Cancer Surviv
Document Outline
Wyszukiwarka
Podobne podstrony:
Becker The quantity and quality of life and the evolution of world inequality
health behaviors and quality of life among cervical cancer s
Quality of life of 5–10 year breast cancer survivors diagnosed between age 40 and 49
Intertrochanteric osteotomy in young adults for sequelae of Legg Calvé Perthes’ disease—a long term
Cho Chikun's encyclopedia of life and death part three a
Cho Chikun's encyclopedia of life and death part one ele
Quality of Life in Women with Gynecologic Cancer in Turkey
A Matter of Life and Death By Derdriu oFaolain
Quality of Life 100
Cho Chikun s encyclopedia of life and death part three a
Jack London Love of Life and Other Stories
89 1268 1281 Tool Life and Tool Quality Summary of the Activities of the ICFG Subgroup
Sterne The Life and Opinions of Tristram Shandy, Gentleman
Long term Management of chronic hepatitis B
THE CHEMICAL COMPOSITION AND SENSORY QUALITY OF PORK
Master Wonhyo An Overview of His Life and Teachings by Byeong Jo Jeong (2010)
Three Important Qualities Of Christ's Life
więcej podobnych podstron