C
LASSIFICATION BY
M
C
K
ENZIE
M
ECHANICAL
S
YNDROMES:
A S
URVEY OF
M
C
K
ENZIE-
T
RAINED
F
ACULTY
Stephen May, MSc
a
A
BSTRACT
O
bjective
:
The purpose of this survey was to identify the percentage of patients with spine pain who can be classified by
McKenzie-trained faculty as having one of either derangement, dysfunction, or postural syndromes.
M
ethods
:
McKenzie Institute International faculty members in 20 countries, who are highly trained and are experienced
users of the classification system, recorded details on 15 consecutively discharged patients.
R
esults
:
Responses were received from 57 therapists in 18 countries (89% of potential sample), and details were
collected on 607 patients with spine pain. Eighty-three percent were classified in one of the mechanical syndromes;
derangement was the most common syndrome. Therapists recorded a mechanical classification in a mean of 82%
(SD, 15.1; range, 44%-100%) of their patients with spine pain.
C
onclusions
:
For this study, the McKenzie mechanical syndromes were commonly diagnosed in a large consecutive
group of patients at multiple sites by experienced therapists. This classification system may have valuable clinical use in
managing patients with spine pain. (J Manipulative Physiol Ther 2006;29:637-642)
K
ey Indexing Terms: Pain; Classification; Prevalence; Back pain
I
n patients with low back pain, the terms dnonspecificT
or dmechanicalT back pain are used to describe an entity
whose pathoanatomical etiology is unknown.
experts argue that specific structural pathology can be
diagnosed using intra-articular or disk-stimulating injec-
tions
; however, such interventions require specialist clini-
cians and facilities and cannot realistically be made
available to all. Although some recent studies suggest that
specific structural pathology can sometimes be diagnosed
by physical examination in some patients,
such reports are
unusual. In general, attempts to search for the specific causal
mechanism for back pain have been largely inconclusive.
As a consequence, most classification systems do not use
specific pathological subgroups. Of 32 classification sys-
tems identified by a systematic review, 15 were classified by
clinical features, 7 by psychological features, 1 by work
status, 4 by health status, and only 6 by pathoanatomy.
general, the critical appraisal found the pathoanatomical
classification systems to be among the weaker systems
according to the criteria used.
A number of classification systems for spinal problems
have been described.
Classification systems provide
several advantages.
They help in making clinical
decisions; they may help in establishing prognosis and are
likely to lead to more effective treatment if patients are
treated with regard to classification. There is initial evidence
that has begun to show that patients treated in accordance
with their classification have better outcomes than patients
who are treated with what is considered best practice
according to contemporary guidelines
dence for the value of the McKenzie classification system.
Classification systems also aid in communication between
clinicians; they could improve our understanding of differ-
ent subgroups and should be used in the conduct of audit
and research. Unfortunately, there exist a wide variety of
spinal pain classifications from which to choose,
more systems continue to appear. Discussion about the
strengths and weaknesses of different types of classification
systems is provided in these reviews.
For a classification system to be of clinical use, it must
have certain characteristics.
First, different clinicians must
be able to reliably classify patients into the different
subgroups so that we can be certain that they actually
exist. Second, it must be verified that the classification
system has clinical application in a significant proportion
of the patient population. Finally, the value of the
classification system needs to be determined by under-
taking efficacy studies with and without classification. The
first stage requires reliability studies; the second stage,
cross-sectional prevalence studies; and the third stage,
637
a
Faculty of Health and Wellbeing, Sheffield Hallam University,
Collegiate Crescent Campus, Sheffield, UK.
Submit requests for reprints to: Stephen May, MSc, Faculty of
Health and Wellbeing, Sheffield Hallam University, Collegiate
Crescent Campus, S10 2BP Sheffield, UK
(e-mail: s.may@shu.ac.uk).
Paper submitted November 24, 2005; in revised form April 21,
2006; accepted June 11, 2006.
0161-4754/$32.00
Copyright
D 2006 by National University of Health Sciences.
doi:10.1016/j.jmpt.2006.08.003

randomized controlled trials. Reliability is necessary to
ensure consistent identification between clinicians. How-
ever, if reliability were perfect but the classification system
only applied to a small proportion of all potential patients,
its clinical use would be limited. For a system to be
clinically useful, it must be able to incorporate a substantial
proportion of all potential patients.
first described a classification system as it
applied to the lumbar spine, then related the same
classification system to the cervical and thoracic spines,
and finally to extremity musculoskeletal problems.
lowing wide usage, minor modifications were made to
the classification system,
which included further detail
on nonmechanical problems that did not fit one of the
mechanical syndromes. The McKenzie classification of
Mechanical Diagnosis and Therapy is now commonly used,
as documented from the United Kingdom and the United
States.
The system involves the use of 3 mechanical
syndromes that are distinguished by their different symptom
and mechanical responses to repeated end-range movement
or sustained postures: derangement, dysfunction, and
postural syndromes.
Derangement is identified by a report of centralization,
abolition, or decrease of symptoms and an increase in range
of movement in response to repeated movements or
sustained postures. Dysfunction is identified by intermittent
pain consistently produced at a restricted end-range with no
rapid change of symptoms or range. Adherent nerve root is a
particular type of dysfunction following a history of
radicular pain, with intermittent pain in the limb. Postural
syndrome is identified by intermittent pain produced only
by sustained sitting, which is abolished by posture
correction, with the rest of the physical examination being
normal.
Patients that do not show responses that permit
classification in one of the mechanical syndromes are
classified as dotherT or nonmechanical syndrome. This
includes patients with the following problems: chronic pain
state, mechanically inconclusive, stenosis, trauma, sacroiliac
joint, dred flagT pathology, and after surgery.
Regarding the clinical use of the system, a number of
studies involving patients with lumbar and cervical spine
problems have established the reliability of categorization or
components of categorization, such as centralization.
Education and familiarity with the system may be important
in the therapists’ ability to use the system reliably. Separate
studies have shown those who have limited exposure to
Mechanical Diagnosis and Therapy show no or moderate
reliability,
whereas well-trained therapists show good
to excellent reliability.
However, this has not been di-
rectly investigated.
The extent to which the classification system is
applicable to patient populations can be indirectly deter-
mined from cohort and reliability studies. Centralization,
which is only found in derangement syndrome, has been
commonly described in patients with back pain, reported in
70% of 731 patients with subacute back pain and in 52% of
325 patients with chronic back pain across 9 studies.
derangement syndrome is described as the most common of
the mechanical syndromes.
A directional preference,
found in the derangement syndrome, has been elicited in
74% of subjects in a randomized controlled trial.
reliability studies, the proportion of patients that could be
classified in one of the mechanical syndromes has varied in
different studies but has been generally high: 68%,
Only one study has directly
looked at the question; it attempted to classify a cohort of
patients with back pain into the McKenzie categories.
522 new patients referred, 307 (58%) were classified into
McKenzie syndromes, whereas 215 (42%) were not.
Consequently, it seemed valuable to determine the
number of patients who can be categorized within the
McKenzie mechanical syndromes and to do this with
therapists who are trained and are familiar with the
system. Therefore, a survey of mechanical and nonmechan-
ical diagnoses was made of the McKenzie teaching faculty,
all who have passed the diploma exam, which is the
highest attainment within the McKenzie educational pro-
gram. Classification is used to guide treatment and is stable
once made; however, at the initial appointment, a provi-
sional classification is made, which is confirmed on
subsequent visits. Therefore, the information was collected
at discharge. The aim of the study was to identify the
percentage of patients with spine pain that can be classified
by McKenzie-trained faculty as having one of the mechan-
ical syndromes.
M
ETHODS
Therapists
Only faculty members of the McKenzie Institute Interna-
tional were recruited for the survey. This group was
experienced with the system of mechanical diagnosis and
therapy, and all had achieved a diploma in mechanical
diagnosis and therapy, which is the highest award in the
educational system. This group was chosen because the
literature suggested that reliability of assessment would be
high in this group.
At the time the survey was conducted, the international
teaching faculty numbered 70 individuals in 20 countries.
Up to 3 repeat e-mailings were conducted over a 6-month
period between October 2003 and March 2004. There was
failure of delivery (3), change of status (3), or unclear results
(2) in 8 individuals and no data from 5 individuals.
Responses were received from 57 faculty members in 18
countries—81% of total population and 89% of potential
population who could be contacted and were still working
as part of McKenzie Institute International. The details
about therapists’ age, sex, experience, practice setting, and
patient referral pattern are provided in
.
638
Journal of Manipulative and Physiological Therapeutics
May
October 2006
McKenzie Classification
Data
Anonymity of patient data was retained at all times, as
participating therapists extracted data from their patient
notes on to the data collection sheets at discharge, with the
researcher never having access to individual patients’ notes.
The McKenzie assessment sheet allows for recording of the
items requested; hence, data extraction was straightforward.
Participants were instructed to provide data on the next 15
consecutive patients discharged from receipt of request for
data. The importance of capturing all consecutive patients
was stressed to all participants. They were asked for the
following information:
! Information about therapist (
)
! Demographic information about patients (
)
! Site of symptoms
! Mechanical or nonmechanical diagnosis
Data collection forms were provided to clarify the type of
data that was required.
Participants were asked to provide basic demographic
data about the patients: age, sex, work status, acuity/
chronicity. Four respondents failed to provide these data;
consequently, the numbers for demographic details are less
than diagnostic information. Mechanical or nonmechanical
diagnosis was collected on a sheet that allowed classifica-
tion to be matched with the site of problem. The end-result
matched site and mechanical or nonmechanical syndrome
(eg, back/derangement, indicating that the patient had back
pain and was classified mechanically and treated as a
derangement). Not all participants returned details on
15 patients. There were data on 849 patients, of which
607 had spinal pain and 242 did not. This article describes
only the consecutive patients with spinal pain.
The operational definitions and descriptions for the
mechanical and nonmechanical disorders have been pub-
lished in work that was familiar to all participants.
Up to 3
reminders were sent to maximize responses. Mailing was
done in batches, and data collection continued over a period
of 6 months. The mean time it took therapists to collect the
data was 3.4 weeks (SD, 1.5; range, 1-8). The collected data
were entered on an Excel (Microsoft Corp, Redmond, Wash,
USA) spreadsheet and presented as descriptive data. The
Sheffield Hallam University ethics committee approved the
study before data collection commenced.
R
ESULTS
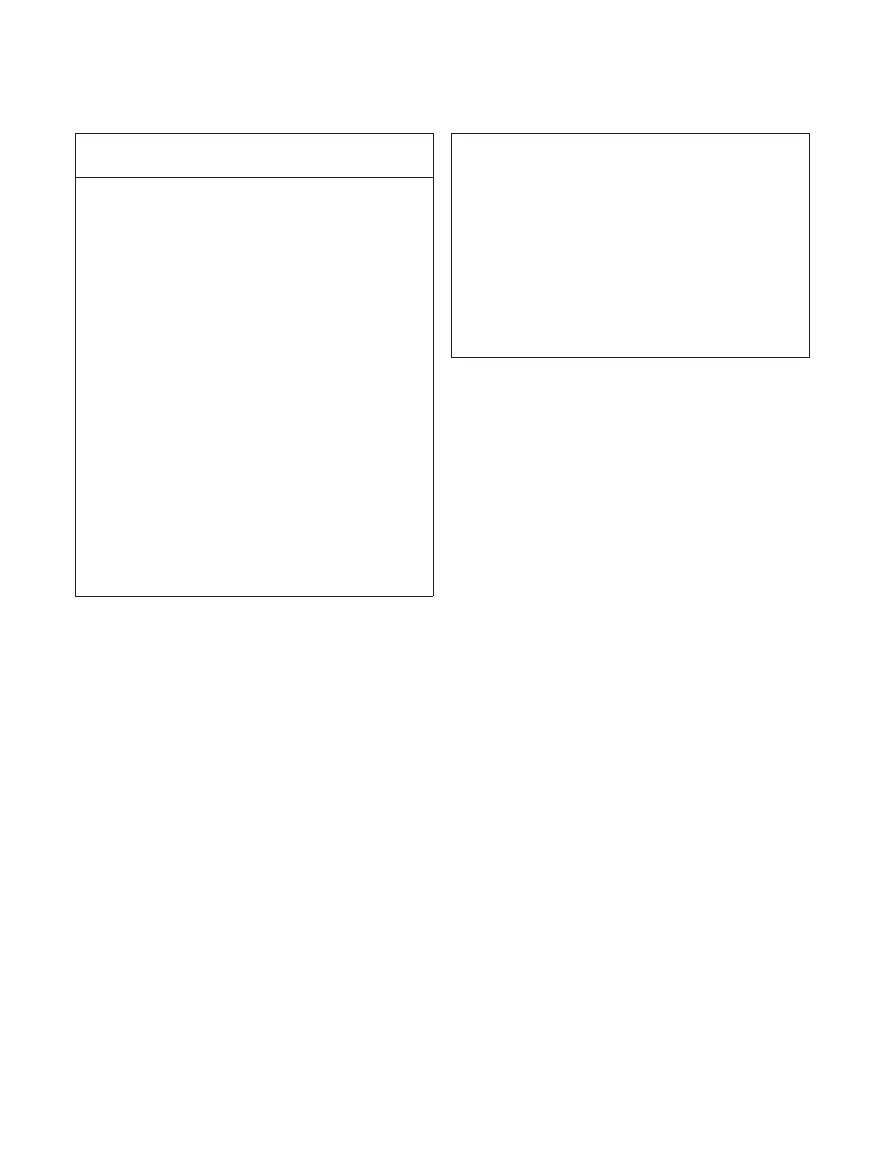
Therapist details are provided in
. Demographic
data were available on 578 patients with spine pain (
and syndrome classification was available for 607 patients
with spine pain. Therapists saw a mean of 11 patients with
spine pain (SD, 3.3; range, 4-17). Therapists recorded a spinal
mechanical classification (derangement, dysfunction, pos-
tural syndrome) in a mean of 9 patients (SD, 3.8; range, 3-17),
a spinal nonmechanical classification in a mean of 2 patients
(SD, 1.5; range, 0-5), and a nonspinal problem in a mean of
4 patients (SD, 3.2; range, 0-11). In patients with spine pain
Table 2.
Demographic and clinical details on 578
a
spinal patients
Sex, n (%)
Male
257 (44)
Female
321 (56)
Age, mean (SD)
43.2 years (13.4)
Symptom duration, n (%)
Acute (b7 d)
86 (15)
Subacute (b7 wk)
174 (30)
Chronic (N7 wk)
318 (55)
Work status, n (%)
Working
378 (65)
Working, sick
80 (14)
Retired
75 (13)
House person/student
45 (8)
Total
578
a
Missing data = 29.
Table 1.
Therapist details
Responders
(n = 57)
Nonresponders
(n = 13)
a
P
b
Sex, n (%)
Male
38 (67)
7 (64)
.445
Female
19 (33)
4 (36)
Age, mean (SD)
45 (6)
44 (7)
.473
Years since
qualification
c
,
mean (SD)
21 (7)
16 (7)
.016
Years since joining
MII faculty
c
,
mean (SD)
8 (5)
9 (7)
.770
No. of countries
d
18
7
Type of practice,
n (%)
.499
Private clinic
37 (65)
6 (55)
GP practice
2 (4)
1 (9)
Hospital outpatients
7 (12)
1 (9)
Specialist clinic
8 (14)
2 (18)
Rehabilitation center
3 (5)
Pain management
clinic
1 (9)
Main referral base
(%)
.115
Self-referral
33
18
GP
51
45
Orthopedics
10
18
Rheumatology
2
Other
4
18
MII, McKenzie Institute International; GP, general practitioner.
a
Missing data = 2.
b
Differences between responders and nonresponders tested with Mann-
Whitney U test or v
2
as appropriate.
c
At 2004.
d
Not tested for significance.
May
Journal of Manipulative and Physiological Therapeutics
McKenzie Classification
Volume 29, Number 8
639

only, therapists recorded a mechanical classification in a
mean of 82% of their patients (SD, 15.1; range, 44%-100%).
Five hundred four (83%) of all spinal patients were
classified in 1 of the mechanical syndromes. Derangement
was by far the commonest mechanical classification (78% of
all patients); far fewer patients were classified with dysfunc-
tion (3%), adherent nerve root (1%), or postural syndromes
(1%). Seventeen percent of all spinal patients were given a
nonmechanical classification. These 101 patients were given
the following other classifications: mechanically inconclu-
sive (6% of all patients), chronic pain state (b4%), red flags
(b1%), stenosis (N1%), sacroiliac joint (1%), trauma (N1%),
spondylolisthesis (b1%), and after surgery (b2%).
D
ISCUSSION
The principal finding of this survey of the use of the
McKenzie classification system was the high prevalence of
mechanical syndromes in the population studied; patients
that did not fit one of the mechanical syndromes were
readily classified under one of the other specific or
nonspecific categories. Extensive use of the classification
system was reflected in the overall percentage and in the
individual therapists’ use of the system. Classification of
derangement was by far the commonest classification made.
The data were collected from 57 participants in primary
care clinics and hospitals from 18 countries, ensuring
widespread and varied collection sites. There was a good
participant response and data gathered from 600 patients.
Patient data were collected at point of discharge rather than
at initial evaluation as symptom responses; therefore,
mechanical syndrome classification, if uncertain, initially
can become clear with further testing.
A classification
system has value in deciding management at initial assess-
ment, and this is the purpose of the McKenzie classification
system. However, as the initial classification is provisional
and is confirmed on subsequent visits, data were collected
retrospectively. Participants were all highly trained and
experienced in mechanical diagnosis and therapy with the
intention of ensuring the highest level of recognition of
mechanical syndromes. This level of experience of therapist
has been shown to have good reliability in classifying and
identifying key aspects of the mechanical syndromes in
patients with back
There are, however, several limitations to the survey.
Although therapists gathered data on the demographics of
the patients, these were not linked to individual patient
classifications. It is not possible, therefore, to match any
particular patient characteristics, such as age, duration of
symptoms, or sex, with particular mechanical syndromes.
Although response rates were good for this kind of survey,
there were still a number of nonresponders.
Data were gathered retrospectively at the time of dis-
charge of patients. Thus, only patients who had completed
treatment were included, which may be a source of bias.
However, details were recorded on consecutively discharged
patients, which included 101 patients who had not received
mechanical classification. So, not all discharged patients
were those who were assumed to have responded well.
The level of experience of the participating therapists
means that a direct comparison cannot be made with those
who are less familiar or experienced with the McKenzie
classification system. Years of training, experience, and
everyday use of a classification system are bound to
facilitate recognition of the classification items, a skill not
available to those less trained and experienced. Furthermore,
it should be noted that previous reliability studies relate to
the original description of the McKenzie classification
system,
whereas this survey used the revised system.
However, the revised system provides clear operational
definitions for the mechanical syndromes that make
interpretation of the system easier.
As specialist clinicians with a teaching role at post-
graduate level, it might be questioned if the patient
population is representative of normal practice. However,
although some therapists had a specialized clinic with
predominantly referrals from specialists, this was not the
case in every instance. The therapists reported that on
average, approximately 67% of their patients were self-
referred or referred from their GP, patients had a range of
symptom duration, and most were working. The practice
setting of the therapists was principally in private practice.
In the only directly comparable study of 522 patients
with back pain, 307 (58%) were classified in one of
McKenzie mechanical syndromes after one visit.
Those
not classified in one of the mechanical syndromes had
experienced back pain for a significantly longer period.
Various significant differences were found between the
classified and unclassified group in pain and disability
scores, time off work, and general health scores. Similar
data were not gathered in the present study; hence,
comparisons cannot be made. The study has several
limitations: it is only published as an abstract; the clinician
involved had not completed the full McKenzie educational
program (only parts A-D), and his experience with the
system was unknown; and diagnosis was made on day 1
when, in fact, several sessions may be necessary to generate
a clear symptom response, especially in patients with chronic
pain. These factors may account for the lower prevalence of
mechanical syndromes.
Numerous classification systems for back problems
exist.
Some of these are in various stages of
development, with reliability and validation studies available,
whereas others are simply described. Sikorski
reported on
142 patients with back pain seen by one therapist, of which
82% were classified into 1 of 3 categories depending on
symptom response. No reliability or other studies appear to
have been performed on this classification system. Wilson
et al
reported on the reliability of a spinal classification
640
Journal of Manipulative and Physiological Therapeutics
May
October 2006
McKenzie Classification

system, which also used symptom response and symptom
location to categorize patients. Two hundred four patients
were classified according to the system; however, it
was unclear if patients were consecutive, and they were
mostly acute. The Quebec Task Force classification system
was designed so that it would be inclusive of all patients
with back pain, but some of its categories involve response
to imaging studies and treatment. Some studies have
evaluated the first 4 Quebec Task Force categories only,
which relate to area of symptoms, and not surprisingly, all
104 patients could be classified.
This classification
system does not direct management as the McKenzie system
does. Other recent classification systems
do not as yet
appear to have had validation studies, although reliability
studies have been conducted,
and one of these gives
positive agreements about classification on a consecutive
sample of patients.
This system is, in part, derived from
the McKenzie classification system, but only 45% of
their patients were classified in directly comparable mechan-
ical syndromes; however, it involves far more classifica-
tion categories.
The present study shows the wide applicability of the
McKenzie classification system to a varied patient popula-
tion among specialist McKenzie practitioners. This suggests
the system has clinical use but needs further exploration
among other patient and therapist populations. Some
preliminary studies suggest that there are effective and
ineffective methods to manage patients who are given
mechanical classifications and then randomized to different
treatments.
Further work needs to be done to substan-
tiate the classification-management link, as the ultimate
justification for any classification system must be the proof
that it improves patient management.
C
ONCLUSION
In a consecutive discharged patient population, McKenzie
mechanical syndromes were used to classify 83% of 607
spinal patients. These decisions were made by highly trained
and experienced McKenzie therapists over a 1-month period.
Although this shows common usage of the mechanical
syndromes by therapists who are expert in the McKenzie
method, external validity is limited by the specialized nature
of the participating therapists.
R
EFERENCES
1. Clinical Standards Advisory Group. Report on back pain.
London7 Her Majesty’s Stationery Office; 1994.
2. Bigos S, Bowyer O, Braen G, et al. Acute low back problems
in adults. Clinical Practice Guideline No. 14. AHCPR
Publication No. 95-0642. Rockville (Md)7 Agency for Health
Care Policy and Research, Public Health Service, U.S.
Department of Health and Human Services; 1994 [Available
from: http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=
hstat6.chapter.25870].
3. Deyo RA. Diagnostic evaluation of LBP. Reaching a specific
diagnosis is often impossible. Arch Intern Med 2002;162:
1444-8.
4. Bogduk N, Derby R, Aprill C, Lord S, Schwarzer A.
Precision diagnosis of spinal pain. In: Campbell JN, editor.
Pain 1996—an updated review; refresher course syllabus.
Seattle7 International Association for the Study of Pain Press;
1996. p. 313-22.
5. Laslett M, Young SB, Aprill CN, McDonald B. Diagnosing
painful sacroiliac joints: a validity study of the McKenzie
evaluation and sacroiliac provocation tests. Aust J Physiother
2003;49:89-97.
6. Young S, Aprill C, Laslett M. Correlation of clinical
examination characteristics with three sources of low back
pain. Spine J 2003;19:460-5.
7. Leboeuf-Yde C, Lauritsen JM, Lauritzen T. What has the
search for causes of low back pain largely been nonconclusive.
Spine 1997;22:877-81.
8. McCarthy CJ, Arnall FA, Strimpakos N, Freemont A,
Oldham JA. The biopsychosocial classification of non-
specific low back pain: a systematic review. Phys Ther
Rev 2004;9:17-30.
9. Fairbank JCT, Pynsent PB. Syndromes of back pain and their
classification. In: Jayson MIV, editor. The lumbar spine and
back pain. 4th ed. Edinburgh7 Churchill Livingstone; 1992.
10. Riddle DL. Classification and low back pain: a review of the
literature and critical analysis of selected syndromes. Phys
Ther 1998;78:708-37.
11. Petersen T, Thorsen H, Manniche C, Ekdahl C. Classification
of non-specific low back pain: a review of the literature on
classification systems relevant to physiotherapy. Phys Ther
Rev 1999;4:265-81.
12. Spitzer WO, LeBlanc FE, Dupuis M, et al. Scientific approach
to the activity assessment and management of activity-related
spinal disorders. Spine 1987;12:S1-S55.
13. Delitto A, Erhard RE, Bowling RW. A treatment-based
classification approach to low back syndrome: identifying
and staging patients for conservative treatment. Phys Ther
1995;75:470-89.
14. Long A, Donelson R, Fung A. Does it matter which exercise?
A multi-centred RCT of low back pain subgroups. Spine
2004;29:2592-602.
15. Clare HA, Adams R, Maher CG. A systematic review of
efficacy of McKenzie therapy for spinal pain. Aust J
Physiother 2004;50:209-16.
16. McKenzie RA. The lumbar spine. Mechanical diagnosis and
therapy. Waikanae (New Zealand)7 Spinal Publications; 1981.
17. McKenzie RA. The cervical and thoracic spine. Mechanical
diagnosis and therapy. Waikanae (New Zealand)7 Spinal
Publications; 1990.
18. McKenzie R, May S. The human extremities mechanical diag-
nosis and therapy. Waikanae (New Zealand)7 Spinal Publica-
tions; 2000.
19. McKenzie R, May S. The lumbar spine mechanical diagnosis
and therapy. Waikanae (New Zealand)7 Spinal Publications;
2003.
20. Battie MC, Cherkin DC, Dunn R, Ciol MA, Wheeler KJ.
Managing low back pain: attitudes and treatment preferences
of physical therapists. Phys Ther 1994;74:219-26.
21. Foster NE, Thompson KA, Baxter GD, Allen JM. Management
of nonspecific low back pain by physiotherapists in Britain and
Ireland. A descriptive questionnaire of current clinical practice.
Spine 1999;24:1332-42.
22. Gracey JH, McDonough SM, Baxter GD. Physiotherapy
management of low back pain. A survey of current practice
in Northern Ireland. Spine 2002;27:406-11.
May
Journal of Manipulative and Physiological Therapeutics
McKenzie Classification
Volume 29, Number 8
641
23. Fritz JM, Delitto A, Vignovic M, Busse RG. Interrater
reliability of judgements of the centralisation phenomenon
and status change during movement testing in patients with
low back pain. Arch Phys Med Rehabil 2000;81:57-61.
24. Kilby J, Stigant M, Roberts A. The reliability of back pain
assessment by physiotherapists, using a dMcKenzie algorithmT.
Physiotherapy 1990;76:579-83.
25. Kilpikoski S, Airaksinen O, Kankaanpaa M, Leminen P,
Videman T, Alen M. Interexaminer reliability of low back
pain assessment using the McKenzie method. Spine 2002;
27:E207-14.
26. Razmjou H, Kramer JF, Yamada R. Intertester reliability of the
McKenzie evaluation in assessing patients with mechanical
low-back pain. J Orthop Sports Phys Ther 2000;30:368-89.
27. Werneke M, Hart DL, Cook D. A descriptive study of the
centralisation phenomenon. A prospective analysis. Spine
1999;24:676-83.
28. Clare HA, Adams R, Maher CG. Reliability of McKenzie
classification of patients with cervical or lumbar pain.
J Manipulative Physiol Ther 2005;28:122-7.
29. Clare HA, Adams R, Maher CG. Reliability of the McKenzie
spinal pain classification using patient assessment forms.
Physiotherapy 2004;90:114-9.
30. Dionne C, Bybee R. Interrater reliability of McKenzie assess-
ment of patients with cervical pain. Proceedings of the
McKenzie Institute 8th International Conference; 2003 Sept;
Rome. Waikanae (New Zealand)7 Spinal Publications; 2003.
31. Riddle DL, Rothstein JM. Intertester reliability of McKenzie’s
classification of the type of the syndrome types present in
patients with low back pain. Spine 1993;18:1333-44.
32. Aina A, May S, Clare H. The centralization phenomenon
of spinal symptoms—a systematic review. Man Ther 2004;9:
134-43.
33. Pinnington MA, Miller JS, Rose MJ, Stanley IM, Rose GM.
New episodes of back pain: how many patients can be
classified into McKenzie syndromes? J Bone Joint Surg
2000;82B(Supp III):211-2.
34. Werneke M, Hart DL. Discriminant validity and relative
precision for classifying patients with non-specific neck and
back pain by anatomic pain patterns. Spine 2003;28:161-6.
35. Binkley J, Finch E, Hall J, Black T, Gowland C. Diagnostic
classification of patients with low back pain: report on a survey
of physical therapy experts. Phys Ther 1993;73:138-55.
36. Sikorski JM. A rationalised approach to physiotherapy for low-
back pain. Spine 1985;10:571-9.
37. Wilson L, Hall H, McIntosh G, Melles T. Intertester reliabi-
lity of a low back pain classification system. Spine 1999;24:
248-54.
38. Van Dillen LR, Sahrmann SA, Norton BJ. Movement system
impairment-based categories for low back pain: stage 1
validation. J Orthop Sports Phys Ther 2003;33:126-42.
39. Petersen T, Laslett M, Thorsen H, et al. Diagnostic classi-
fication of non-specific low back pain. A new system
integrating patho-anatomical and clinical categories. Physi-
other Theory Pract 2003;19:213-37.
40. Loisel P, Vachon B, Lemaire J, et al. Discriminative and
predictive validity assessment of the Quebec Task Force
classification. Spine 2002;27:851-7.
41. Petersen T, Olsen S, Laslett M, et al. Inter-tester reliability of a
new diagnostic classification system for patients with non-
specific low back pain. Aust J Physiother 2004;50:85-91.
42. Van Dillen LR, Sahrmann SA, Norton BJ, et al. Reliability of
physical examination items used for classification of patients
with low back pain. Phys Ther 1998;78:979-88.
43. Fritz JM, George S. The use of a classification approach to
identify subgroups of patients with acute low back pain. Spine
2000;25:106-14.
44. Heiss DG, Fitch DS, Fritz JM, et al. The interrater reliability
among physical therapists newly trained in a classification
system for acute low back pain. J Orthop Sports Phys Ther
2004;34:430-9.
45. Schenk RJ, Jozefczyk C, Kopf A. A randomised trial
comparing interventions in patients with lumbar posterior
derangement. J Man Manip Ther 2003;11:95-1102.
642
Journal of Manipulative and Physiological Therapeutics
May
October 2006
McKenzie Classification
Document Outline
Wyszukiwarka
Podobne podstrony:
więcej podobnych podstron