225
Eating Disorders, 17:225–241, 2009
Copyright © Taylor & Francis Group, LLC
ISSN: 1064-0266 print/1532-530X online
DOI: 10.1080/10640260902848576
UEDI
1064-0266
1532-530X
Eating Disorders, Vol. 17, No. 3, March 2009: pp. 1–31
Eating Disorders
Differential Treatment Response for Eating
Disordered Patients With and Without
a Comorbid Borderline Personality
Diagnosis Using a Dialectical Behavior
Therapy (DBT)-Informed Approach
Dialectical Behavior Therapy and Eating Disorders
D. D. Ben-Porath et al.
DENISE D. BEN-PORATH
Department of Psychology, John Carroll University, Cleveland, Ohio, USA
LUCENE WISNIEWSKI and MARK WARREN
Cleveland Center for Eating Disorders, Beachwood, Ohio, USA
Studies have reported conflicting findings regarding the impact on
treatment for eating disorder patients comorbidly diagnosed with
borderline personality disorder. The current investigation sought
to investigate whether individuals diagnosed with an eating disor-
der vs. those comorbidly diagnosed with an eating disorder and
borderline personality disorder differ on measures of eating disor-
ders symptoms and/or general distress over the course of treatment.
In light of the success of DBT in treating individuals diagnosed
with borderline personality disorder, a group known to have con-
siderable difficulties in regulating affect, the current study also
sought to examine whether these two groups would differ on
expectancies to regulate affect over the course of DBT-informed
treatment. Results indicated that while a comorbid diagnosis of
borderline personality disorder did not impact eating disorder
treatment outcomes, those comorbidly diagnosed did present over-
all with higher levels of general distress and psychological distur-
bance. With respect to affect regulation, results indicated that at
the beginning of treatment, eating disordered individuals who
carried a comorbid diagnosis of BPD were significantly less able to
This project was funded by a research fellowship from John Carroll University.
The authors would like to thank the clients and their therapists for participation in this study.
Address correspondence to Denise D. Ben-Porath, Department of Psychology, John
Carroll University, 20700 North Park Blvd., University Heights, OH 44118. E-mail: dbenporath@
jcu.edu

226
D. D. Ben-Porath et al.
regulate affect than patients without a comorbid borderline diag-
nosis. However, at the end of treatment there was no statistically
significant difference between the two groups. The role of affect
regulation in treating eating disordered individuals with a comor-
bid borderline personality disorder diagnosis is discussed.
Studies investigating the prevalence of borderline personality disorder
(BPD) in women being treated for an eating disorder (ED) have produced
varying estimates ranging from as little as 2% to as high as 44% (Gwirtsman,
Roy-Byrne, Yager, & Gerner, 1983; Levin & Hyler, 1986; Pope, Frankenburg,
Hudson, Jonas, & Yurgelun-Todd, 1987; Wonderlich & Mitchell, 1997),
While estimates of prevalence rates vary, most clinicians agree that ED
patients who present with comorbid BPD (ED-BPD) are one of the most
challenging subtypes of ED individuals to treat (Johnson, Tobin, & Enright,
1989). Although the difficulties in treating those with an ED and a border-
line diagnosis are well documented (Fahy, Eisler, & Rusell, 1993; Herzog,
Keller, Lavori, Kenny, & Sacks, 1992; Johnson, Tobin, & Dennis, 1989), only
a handful of studies have specifically examined BPD comorbidity and its
impact on the course of treatment for those with eating disorders.
Johnson, Tobin and Dennis (1990) examined treatment outcomes in ED
patients with and without comorbid borderline personality 1 year after treat-
ment completion. While both groups presented initially with high levels of
ED symptoms at the initial assessment, approximately 90% of ED patients
achieved a significant reduction in ED symptoms whereas only 58% of those
diagnosed with ED-BPD achieved a significant reduction in ED symptoms.
Johnson et al. (1990) also found that ED patients with comorbid BPD pre-
sented with a more severe clinical picture at the beginning of treatment as
measured by the BDI and the SCL-90-R. While both groups reduced their
psychiatric symptomatology at similar rates over the course of treatment,
scores for the borderline patients remained at clinically significant levels
whereas the non-BPD group was largely asymptomatic.
While Steinberg, Tobin, and Johnson (1990) found that those with a
comorbid BPD diagnosis enter treatment with comparable symptom severity
on ED measures, other authors have found that ED individuals with comor-
bid borderline pathology enter treatment with a more severe clinical pic-
ture, both in terms of eating pathology and general distress. For example,
Wonderlich, Fullerton, Swift, and Kelin (1994) found that individuals diag-
nosed with ED-BPD reported a greater number of ED symptoms and higher
levels of general distress at intake. Although groups did not differ in the
amount of symptomatic change over time, symptoms in the individuals
comorbidly diagnosed remained more severe throughout treatment. Similar
to these previous findings, Zeeck et al. (2007) found that ED-BPD patients
as compared to ED-only patients reported more ED pathology as measured

Dialectical Behavior Therapy and Eating Disorders
227
by the EDI-2 and more general psychiatric symptomatology at the begin-
ning of treatment. Neither group differed in the amount of symptomatic
change on ED pathology, although scores on the EDI-2 remained consis-
tently more severe in the BPD group over the course of treatment. A similar
pattern was found on the SCL-90-R with one exception. There was a signifi-
cant interaction between time and diagnosis on the anxiety subscale of the
SCL-90-R. ED-BPD individuals had higher levels of anxiety in comparison to
the ED-only group at the beginning of treatment. However, at the end of
treatment no differences emerged.
What impact BPD has on the course of treatment for those diagnosed
with an ED remains unclear. In spite of these conflicting findings, most
researchers agree that those with BPD present with a more complicated
clinical picture, and thus, often require different levels and types of inter-
vention. Sansone, Fine and Sansone (1994) report that effective treatment
for individuals diagnosed with ED-BPD must entail an integrated and
comprehensive approach that extends to the therapeutic milieu and incor-
porates individual/group psychotherapy and consultation. Zeeck and col-
leagues (2007) suggest that borderline patients being treated for an ED
require therapies that focus not only on the ED symptoms, but also on
deficits in the areas of interpersonal skills, affect regulation, and impulse
control.
DIALECTICAL BEHAVIOR THERAPY APPLIED
TO EATING DISORDERS
Dialectical behavior therapy (DBT), is a multi-disciplinary treatment
approach that uses multiple treatment modes (e.g., individual therapy,
group skills training, telephone coaching, team consultation) to address def-
icits in interpersonal relationships, affect regulation and impulse control.
Therefore, this treatment holds considerable promise for ED individuals
diagnosed with comorbid BPD. Johnson et al. (1990) have speculated that
the one-third of patients who typically do not respond to treatment are
likely ED individuals who are also comorbidly diagnosed with BPD. This
lack of treatment response is thought, in part, to be due to the failure of
traditional cognitive behavioral interventions in addressing the affect dys-
regulation and impulsivity that accompanies ED-BPD clients.
In an effort to explore the treatment effectiveness of DBT with comor-
bidly diagnosed ED clients, Palmer and colleagues (2003), in an uncon-
trolled clinical trial, applied the DBT treatment model to seven individuals
diagnosed with an ED and BPD. Results indicated that there was a reduc-
tion in self harm as well as ED behavior. Given the treatment focus of DBT
in the area of affect regulation and reduction in self injury, this treatment
would seem highly appropriate for this comorbidly diagnosed group.

228
D. D. Ben-Porath et al.
Moreover, several researchers have stated that DBT may also be indi-
cated in the treatment of those with an ED who present without Axis II
pathology. Some theorists have argued that ED symptoms represent a mal-
adaptive method to regulate negative affect (Heatherton & Baumeister,
1991; Safer, Telch, & Agras, 2001; Telch, Agras, & Linehan, 1990, 2001). In
fact, several studies have demonstrated that negative mood states are
reduced in women after a binge eating episode (see Polivy & Herman, 1993
for a review of these studies).
To date, a handful of studies have investigated the effectiveness of DBT
and explored the role of affect regulation in treatment outcomes in those with
an ED. Telch, Agras, and Linehan (1999) conducted an uncontrolled clinical
trial on 11 women who underwent group DBT skills treatment modified for
their BED. At the end of treatment, 82% reported being abstinent from binge
eating. Furthermore, patients’ scores on the NMR scale significantly improved,
indicating that these women held stronger self expectancies for regulation of
negative mood states post-treatment as compared to pre treatment.
Following up on these findings, Telch, Agras, and Linehan (2001) con-
ducted a clinically controlled trial in which 44 women diagnosed with BED
were randomly assigned to group DBT skills modified for BED or a wait-list
control group. Results indicated that 89% of the participants in the DBT
skills group condition were abstinent from binge eating as compared with
only 12.5% in the control condition. However, no differences emerged
between the two groups on the NMR Scale, suggesting that the wait list
control did not differ significantly from the DBT group in expectancies to
regulate negative mood states.
More recently, Safer, Telch, and Agras (2001) have applied DBT treat-
ment to individuals diagnosed with binge/purge behaviors. At the end of
treatment, 28.6% in the DBT condition were abstinent from binge eating/
purging behaviors as compared with no participants in the wait-list control
condition. With respect to NMR scores, at the beginning of therapy ED indi-
viduals in the DBT condition reported significantly less expectancy to regu-
late affect as compared to ED individuals in the wait list condition.
However, at the end of treatment, there was no difference between the two
groups (Safer, Telch, & Agras, 2001).
To date, several studies have investigated the impact of a comorbid BPD
diagnosis in the treatment outcome of those diagnosed with an ED. These
studies have produced conflicting results with some suggesting that BPD has
no impact on ED symptoms (Steinberg et al., 1990) whereas other authors
have found that ED-BPD individuals enter treatment with a more severe clin-
ical picture, both in terms of eating pathology and general distress (Wonder-
lich, et al., 1994; Zeeck et al., 2007). Thus, the first goal of this study was to
investigate whether individuals diagnosed with an ED vs. those comorbidly
diagnosed with an ED and BPD differ on measures of eating disorders symp-
toms and/or general distress over the course of treatment.

Dialectical Behavior Therapy and Eating Disorders
229
A second, but equally important goal of this study was to explore the
role of affect regulation in DBT-informed treatment in individuals diagnosed
with ED vs. those diagnosed with ED-BPD. Because the previous literature
suggests that ED-BPD individuals enter treatment with higher levels of gen-
eral distress, it was predicted that those ED individuals comorbidly diag-
nosed with BPD would report lower expectancies to regulate negative affect
pre treatment as compared to their nonborderline peers. However, because
difficulties in affect regulation are central to BPD and DBT treatment specif-
ically targets affect dysregulation (Linehan, 1993), it was hypothesized that
no difference would be present in expectancies to regulate affect between
these two groups post-treatment.
METHOD
Participants
Participants in the current study were recruited over an 18-month period.
Participants were excluded from the study if they were under 18 years of
age, had been treated previously at the facility, were actively homicidal/
suicidal or met criteria for substance abuse/dependence. Additionally, indi-
viduals meeting criteria for BED did not meet the admissions criteria for par-
tial hospitalization. Therefore, they were not eligible to participate in the
current study, but rather were referred to a once-weekly outpatient group.
The initial sample consisted of 71 participants, all of whom were admit-
ted to the outpatient partial hospitalization program specializing in the treat-
ment of eating disorders. Of those, 21% (5 with a borderline diagnosis and
10 without a borderline diagnosis) dropped out of treatment prematurely
due to treatment non-compliance and an additional 16 (23%) did not have
discharge data available due to administrative error. Several one-way
ANOVAs were conducted comparing these three groups (e.g., those who
had discharge data available vs. those who dropped out of treatment pre-
maturely and did not have discharge data available, vs. those who were not
given discharge assessments due to administrative error) on the following
variables of interest: pre-treatment body mass index, age, Beck Depression
Inventory-2 (BDI-2), Beck Anxiety Inventory-2 (BAI-2), and the Eating
Disorder Examination-Questionnaire (EDE-Q). No statistically significant dif-
ferences were found on pre-treatment measures or the variables of age and
body mass index between the three groups.
The remaining sample in the current study consisted of 40 outpa-
tients (one man and 39 women) who participated in a 30 hour per week
partial hospitalization program designed specifically to treat eating disor-
ders. The mean age of the sample was 26.03 (SD = 7.92) years. The mean
body mass index for the sample at the time of admission was 21.96 (SD =
4.77). The average length of stay in the program was 73.16 (SD = 40.88) days.

230
D. D. Ben-Porath et al.
Sixteen (40%) individuals met DSM-IV-TR criteria for an ED and BPD. The
ED diagnosis was determined by a semi-structured interview by a
licensed clinician. The borderline diagnosis was determined through a
combination of the PDQ-4 and clinician confirmation of a borderline
diagnosis post discharge. Based upon these criteria, 24 (60%) individuals
met DSM-IV-R diagnostic criteria for an ED, but not BPD. Patients who
were actively psychotic, suicidal, or substance dependent were excluded
from the partial hospitalization treatment program. Table 1 presents addi-
tional demographic information for this sample, including additional Axis
I diagnoses.
Program Description
Individuals seeking treatment for an ED at this hospital clinic underwent a
2-hour assessment by a licensed mental health worker to determine
whether they met criteria for an ED according to DSM-IV-TR, and to deter-
mine if their symptoms warranted a partial hospitalization level of care (e.g.,
30 hours of treatment per week). Consistent with the practice guidelines put
forth by the American Psychiatric Association Work Group on Eating Disor-
ders (2006), admission to a partial hospitalization program (PHP) requires
that a patient be greater than 75% of their ideal body weight, be medically
stable, exhibit partial motivation to recover, require structured treatment,
and have limited social support.
Once clients were evaluated and determined to meet American Psychi-
atric Association (APA) criteria for a partial hospitalization level of care, they
were oriented to a DBT-informed treatment model adapted to eating disor-
ders (see Wisniewski & Kelly, 2003). All patients participated in twice
weekly DBT group skills training during which mindfulness, emotion regu-
lation, distress tolerance, and interpersonal effectiveness skills were taught
and practiced. Additional groups which incorporated DBT concepts
included a weekly group that focused on motivation and commitment, a
goal setting group, and a behavior chain analysis group. In the behavior
chain analysis group, clients provided a detailed written account of the
events, emotions, cognitions, and physical sensations leading up to, during,
and after ED behavior and/or life threatening behaviors. In addition to
behavior chain analysis, patients completed daily diary cards that were
modified to target ED behaviors as well as self injurious/suicidal behaviors.
Clients also participated in a “DBT in-action” group (a group in which par-
ticipants practiced DBT skills in order to promote generalization outside of
treatment) as well as a weekly yoga group which incorporated elements of
mindfulness to movement. The nutrition module taught patients about
healthy eating and meal planning. Lastly, in vivo exposure to food in which
clients ate healthy meals together (e.g., exposure therapy) was also part of
the DBT-informed program.
Dialectical Behavior Therapy and Eating Disorders
231
Consistent with the approach offered in standard DBT, ED clients were
offered after-hours telephone consultation to promote skills generalization
and to reduce self injurious and suicidal behaviors. However, clients were
also encouraged to call their therapist to assist in resisting urges to engage
TABLE 1 Demographic Characteristics of Participants by Diagnosis
ED-BPD
ED
Characteristic
n (%)
n (%)
Gender
Female
15 (94%)
24 (0%)
Male
1 (6.3%)
0 (100%)
Marital Status
Never Married
12 (86%)
16 (66.7%)
Married
1 (7.1%)
5 (20.8%)
Divorced
1 (7.1%)
2 (8.3%)
Widowed
0 (0%)
1 (4.2%)
Race
Caucasian
14 (100%)
22 (91.7%)
Hispanic
0 (0%)
2 (8.3%)
Level of Education
Some Graduate Training
2 (14.3%)
2 (8.3%)
Some College Education
5 (35.7%)
10 (41.7%)
High School/GED
6 (50%)
12 (50%)
Current Employment
Employed Full Time
6 (42.9%)
6 (27.3%)
Employed Part Time
1 (7.1%)
4 (18.2%)
Unemployed
3 (21.4%)
4 (18.2%)
Disabled
4 (28.6%)
7 (31.8%)
Retired
0 (0%)
1 (4.5%)
Eating Disorder Diagnosis
Anorexia Nervosa
1 (7.1%)
6 (25%)
Bulimia Nervosa
9 (64.3%)
7 (29.2%)
Eating Disorder, NOS
4 (28.6%)
11 (45.8%)
Additional Axis I Diagnosis
Depression/Dysthymia
5 (55.5%)
12 (85.7%)
Anxiety
0 (0%)
0 (0%)
Obsessive-Compulsive Disorder
1 (11.1%)
1 (7.1%)
Post Traumatic Stress Disorder
1 (11.1%)
1 (7.1%)
Attention Deficit Hyperactivity Disorder
0 (0%)
0 (0%)
Panic Disorder
1 (11.1%)
0 (0%)
Bipolar Disorder
1 (11.1%)
0 (0%)
Medications Prescribed
Anxiolytics
1 (8%)
0 (0%)
Antipsychotics
1 (8%)
3 (13%)
Mood stabilizers
0 (0%)
0 (0%)
Antidepressants
9 (69%)
10 (42%)
Note: Due to missing data, numbers may not total 40.

232
D. D. Ben-Porath et al.
in ED behaviors (see Wisniewski & Ben-Porath, 2005 for a complete
description of the DBT telephone protocol adapted to ED patients). A team
of professionals (e.g., psychologist, psychiatrist, nutritionist, social worker,
and milieu therapists) comprised the DBT consultation team. The team met
on a weekly basis to consult on cases within a DBT framework.
Unlike standard DBT treatment, individual therapy was not offered.
Third party payers are often unwilling to reimburse for individual treatment
while a patient is in higher levels of care. In an effort to compensate for this
limitation, each patient in the treatment protocol was assigned to a therapist
who met with the patient at a minimum of once weekly for 30 minutes.
During these sessions, the diary cards and behavior chain analyses were
reviewed and therapy-interfering behaviors were addressed. The assigned
therapist also validated the clients’ responses and difficulties in treatment
while also assisting them in replacing maladaptive behaviors with more
skillful behaviors. Thus, the current program employed all four modes of
standard DBT treatment. However, the time allocated to each client for indi-
vidual therapy was reduced and components of the group material were
adapted for an ED population.
Measures
E
ATING
D
ISORDER
E
XAMINATION
-Q
UESTIONNAIRE
(EDE-Q)
The EDE-Q is a questionnaire that provides information about the fre-
quency of ED behaviors over a period of the last 28 days. Questions reflect
the DSM-IV criteria for eating disorders. The EDE-Q yields four subscales.
These include dietary restraint, eating concerns, weight concerns, and shape
concerns subscales. Subscale scores can range from 0 to 6 with higher
scores indicating greater ED disturbance. The EDE-global score consists of
the four subscales. The EDE-Q has been shown to have acceptable internal
consistency with Cronbach alphas ranging from 0.78 to 0.93. Test-retest reli-
ability of the EDE-Q subscales over a two-week period yielded Pearson r
coefficients ranging from 0.81 to 0.94 (Luce & Crowther, 1999).
N
EGATIVE
M
OOD
R
EGULATION
(NMR)
SCALE
Consistent with previous research in this area, the NMR Scale was used
(Safer et al., 2001; Telch et al., 1999, 2000). The NMR is a 30-item self-report
questionnaire that assesses an individual’s expectancy to successfully regu-
late negative mood states. This measure utilizes a 5-point Likert scale format
ranging from 30 to 150 with higher scores indicating a greater expectancy
that one can regulate negative mood. The NMR demonstrated adequate tem-
poral stability of 0.74 over a 3–4 week period, adequate discriminant validity
from other measures such as the BDI, and adequate internal consistency

Dialectical Behavior Therapy and Eating Disorders
233
with alphas ranging from 0.86 to 0.92 (Catanzaro & Mearns, 1990). The NMR
yields the following three scales: (1) NMR-General which measures an indi-
vidual’s general ability to regulate mood (e.g.,” I can find a way to relax”),
(2) NMR-Cognitive which measures an individual’s ability to regulate mood
via cognitive strategies (e.g., “Planning how I’ll deal with things will help.”),
and (3) NMR-Behavioral which measures an individual’s ability to regulate
mood via behavioral strategies (e.g., “Going out with friends will help.”).
T
HE
B
ECK
D
EPRESSION
I
NVENTORY
-2 (BDI-2)
Consistent with previous research in this area, the BDI-2 was used (Safer,
et al., 2001; Telch et al. 1999, 2000). The Beck Depression Inventory-2 is a
21-item scale self-report instrument used for measuring depressive symp-
toms corresponding to the criteria for major depressive disorder found in
DSM-IV (1994). Higher scores indicate greater severity of depressive symp-
tomatology. The instrument has well documented reliability and validity.
The coefficient alpha of the BDI-II for an outpatient sample was 0.92 (Beck,
Steer, & Brown, 1996).
T
HE
B
ECK
A
NXIETY
I
NVENTORY
-2 (BAI-2)
Consistent with previous research in this area, the BAI-2 was used (Safer et al.,
2001; Telch et al., 1999, 2000). The Beck Anxiety Inventory-2 is a 21-item
scale that measures severity of anxiety, with higher scores indicating greater
anxiety. The instrument has well documented reliability with Cronbach
coefficient alpha in the range of 0.92. Test retest reliability with a one week
interval was 0.75 (Beck & Steer, 1990).
P
ERSONALITY
D
ISORDER
Q
UESTIONNAIRE
-4 (PDQ-4)
The PDQ-4 is a 100-item self report, true/false questionnaire that yields
diagnoses consistent with the DSM-IV diagnostic criteria for Axis II person-
ality disorders. The PDQ-4 was selected because of its adaptability to a
clinical setting and brevity (Sansone & Levitt, 2005). Test-retest reliability for
the PDQ-4 was adequate and compared favorably with the interrater reli-
ability of a DSM-III-oriented clinical interview and the Diagnostic Interview
for Borderline Patients (DIB) (Hyler, Skodol, Kellman, Oldham & Rosnick,
1990). Levin and Hyler (1986) achieved excellent agreement for their inter-
view diagnoses with kappa coefficients of 0.92 for BPD. Based upon the
recommendations by Sansone and Levitt (2005) only individuals whose bor-
derline diagnoses were confirmed post discharge by the treating clinician
and received a score indicative of borderline personality disorder were
included in the BPD category.
234
D. D. Ben-Porath et al.
Procedure
Clients who met criteria for an ED and whose symptoms warranted the level
of care of partial hospitalization were included in the protocol. At the time
of admission and again at discharge, all participants completed the
measures above. In order to assess for borderline personality features, all
participants were administered the PDQ-4 at the time of admission.
RESULTS
A series of 2 (ED vs. ED-BPD)
× 2 (time of testing) mixed factor analyses of
variance (ANOVA) was conducted with diagnosis as a between factor and
time of testing as a within subjects factor. Scores on the NMR, BDI-II, BAI-II,
and the EDE-Q served as the dependent variables. Pre and post-treatment
means and standard deviations and significance levels for the ED and
ED-BPD groups are listed in Table 2.
Eating Disorder Examination-Questionnaire
In an effort to decrease the possibility of type 1 error, subscales for the EDE-Q
were not analyzed separately. Rather the composite scale, the EDE-global was
used. On the EDE-global scale, there was a significant main effect for time
[F (1, 37) = p = .001] with participants reporting a reduction in ED symp-
toms from Time 1 (M=, SD=) to Time 2 (M=, SD=). No significant main
effect for diagnosis or significant interaction between time and diagnosis was
found on the EDE global scale.
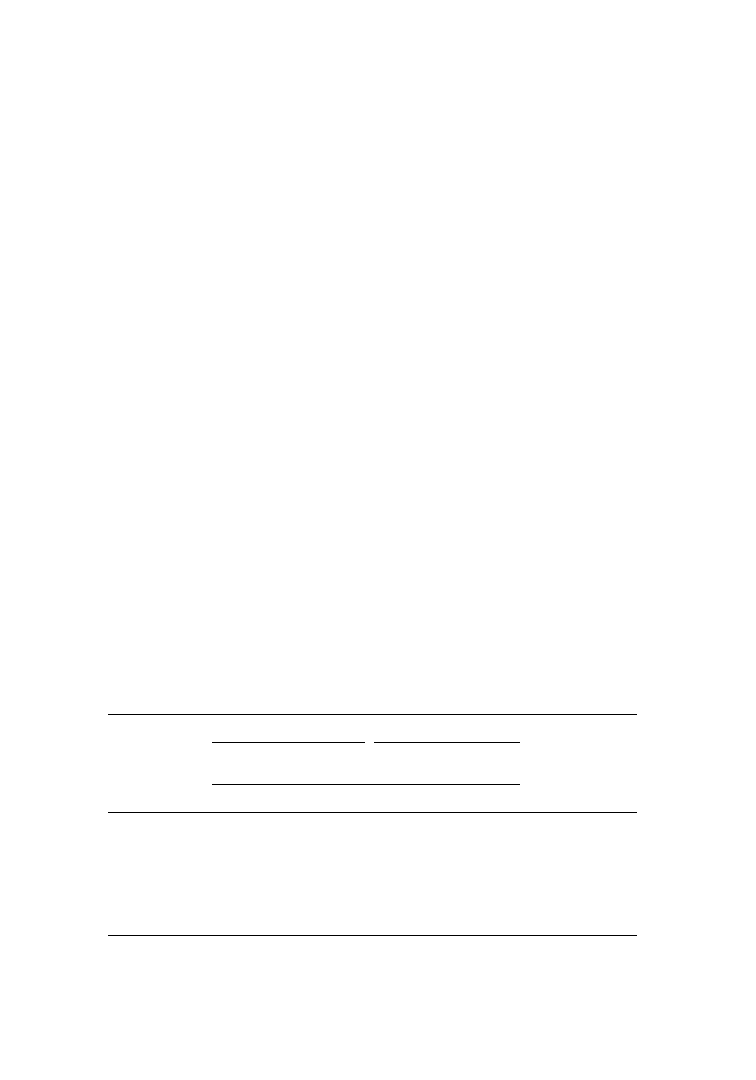
TABLE 2 Pre and Post-Treatment Means and Standard Deviations for Individuals Diagnosed
with an Eating Disorder and for Individuals Comorbidly Diagnosed with an Eating Disorder
and Borderline Personality Disorder
ED
ED-BPD
Pre-
treatment
Post-
treatment
Pre-
treatment
Post-
treatment
M (SD)
M (SD)
M (SD)
M (SD)
F
(df)
p
EDE-Q Global
Score
4.29 (.24)
3.35 (.293)
4.91 (.32)
3.66 (.39)
.314 1, 34 .579
BDI-2
24.71 (2.34) 13.80 (2.74)
37.39 (3.05) 21.15 (3.57)
1.17 1, 30 .287
BAI-2
18.09 (1.72) 13.49 (2.09)
25.79 (2.20) 15.93 (2.68)
2.17 1, 35 .15
NMR-General
31.65 (1.69) 32.45 (1.84)
23.08 (2.18) 32.79 (2.37)
7.98 1, 30 .008
NMR-Behavioral 34.35 (1.25) 35.23 (1.29)
26.00 (1.62) 32.92 (1.66) 10.56 1, 30 .003
NMR-Cognitive
31.75 (1.48) 32.85 (1.171) 22.00 (1.92) 32.67 (1.51) 11.21 1, 30 .002
Note. Due to missing data numbers may not total 40.
Dialectical Behavior Therapy and Eating Disorders
235
Beck Depression and Beck Anxiety Inventories
On the BDI-II, there was a significant main effect for time with participants
reporting a reduction in depression from Time 1 (M = 28.41, SD = 12.60) to
Time 2 (M = 16.49, SD = 13.75) [F (1, 37) = 26.03, p = .001]. In addition,
there was a main effect for diagnosis [F (1, 37) = 8.09 p = .007] with ED
individuals with a comorbid borderline diagnosis (M = 28.25, SD = 2.62)
presenting overall with more depression as compared to those with only
an ED diagnosis (M = 18.67, SD = 2.12). No interaction between diagnosis
and time was found on the BDI-II. Results for the BAI-2 followed the same
pattern.
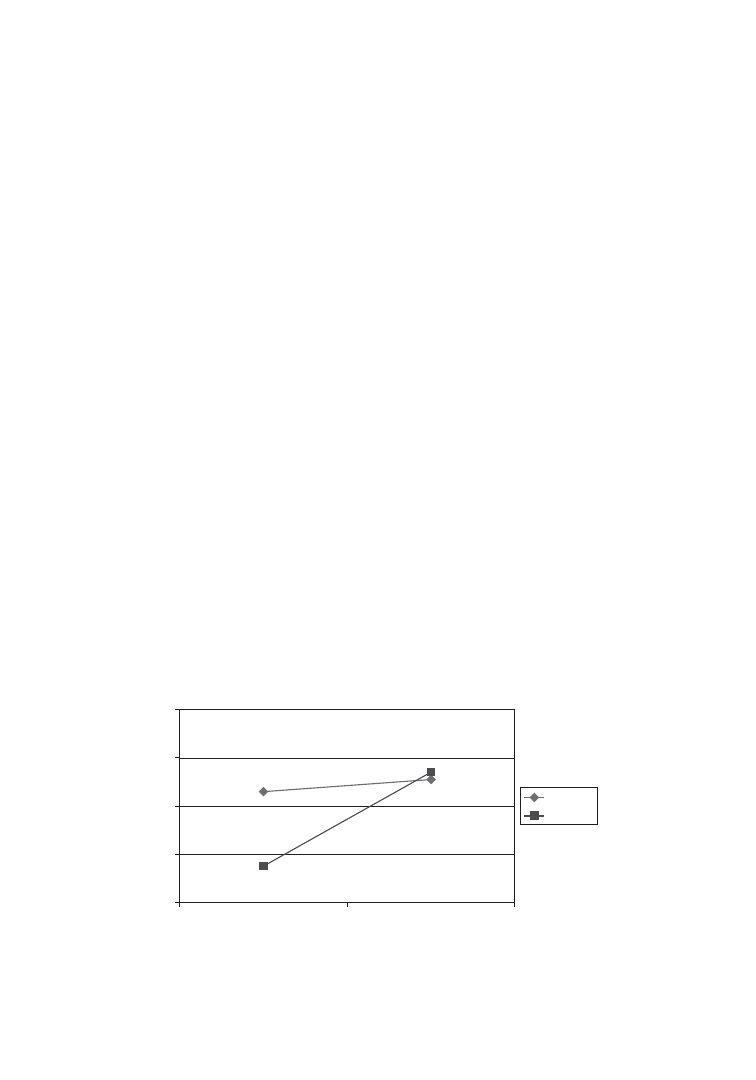
Negative Mood Regulation Scale
Because there is no composite score on the NMR, each scale was analyzed
separately. Thus, a bonferroni correction was done to control for multiple
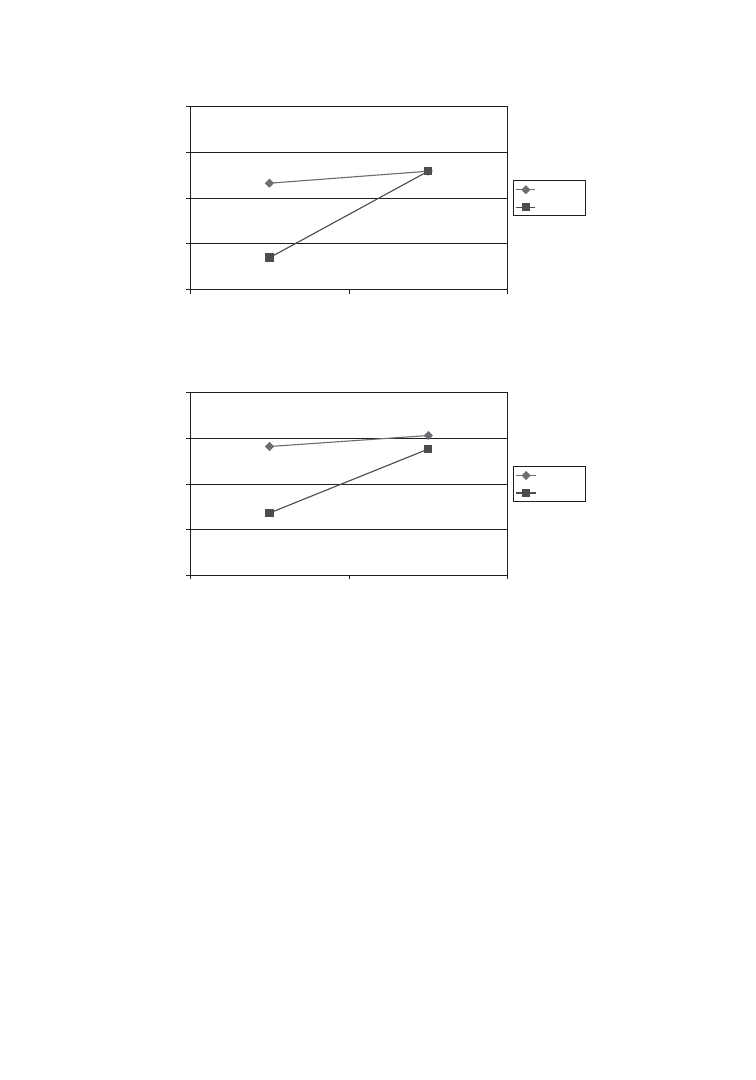
comparisons with alpha being set at 0.016 As can be seen in Figure 1, on
the NMR-general scale there was a significant main effect for time [F (1, 33) =
14.33, p = .001] but not diagnosis. This main effect must be interpreted in
light of a significant interaction [F (1, 33) = 8.43, p = .007]. At the beginning
of treatment ED individuals who carried a comorbid diagnosis of BPD
reported significantly less ability to regulate affect on the NMR-general
scale (M = 23.79, SD = 4.71) than patients without a comorbid borderline
diagnosis (M = 31.48, SD = 8.62). However, at the end of treatment there
was no difference between the ED-BPD (M = 33.54, SD = 6.91) and
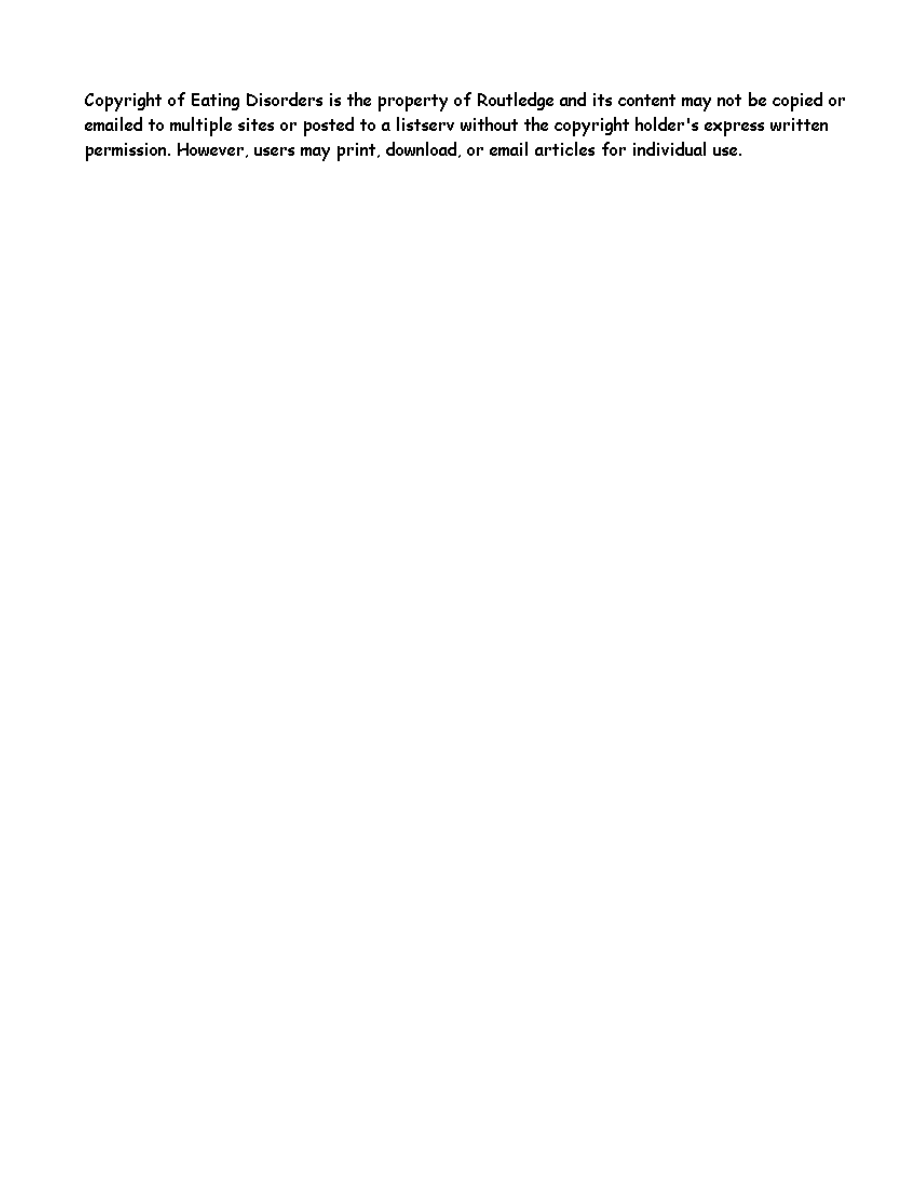
ED-only (M = 32.76, SD = 8.71) groups. As can be seen in Figures 2 and 3,
results for the NMR-cognitive and NMR-behavior scale followed the same
pattern.
FIGURE 1 NMR-General scores for ED and ED/BPD patients pre and post-treatment.
20
25
30
35
40
Time1
Time2
ED
ED/BPD
236
D. D. Ben-Porath et al.
DISCUSSION
The first goal of this study was to attempt to resolve the contradictory find-
ings in the literature pertaining to the impact of a borderline diagnosis on
treatment outcomes for those with an ED. On the EDE-Q global subscale no
differences emerged between individuals diagnosed with ED vs. those diag-
nosed with ED-BPD over the course of treatment. While the ED-BPD group
was somewhat more symptomatic pre-treatment, these differences were not
significant and there were no differences post-treatment on the EDE-Q.
These findings are consistent with former studies that suggest that a comor-
bid diagnosis of BPD has minimal impact on ED outcomes (Wonderlich
et al., 1994; Zeeck et al., 2007).
With respect to general psychopathology, findings from the current study
were consistent with past research (Johnson et al., 1990; Wonderlich, et al., 1994;
FIGURE 2 NMR-Cognitive scores for ED and ED/BPD patients pre and post treatment.
20
25
30
35
40
Time1
Time2
ED
ED/BPD
FIGURE 3 NMR-Behavioral scores for ED and ED/BPD patients pre and post treatment.
20
25
30
35
40
Time1
Time2
ED
ED/BPD

Dialectical Behavior Therapy and Eating Disorders
237
Zeeck et al., 2007). In the current investigation, the ED-BPD group demon-
strated higher levels of depression and anxiety at the beginning and end of
treatment as compared to the ED group. However, both groups made simi-
lar reductions in depressive and anxious symptomatology over the course
of treatment, suggesting that individuals with ED-BPD enter and leave treat-
ment with higher levels of distress as compared to those diagnosed with ED
alone. In sum, these findings appear to support those described by Zeeck
et al. (2007), which state that individuals with ED-BPD do not appear to dif-
fer dramatically in ED symptomatology as compared to the their ED-only
peers. However, ED-BPD clients do appear to enter and leave treatment
with higher levels of general psychopathology as compared to their ED-only
counterparts.
The second major finding in the current investigation was that while
ED individuals comorbidly diagnosed with BPD reported lower expectan-
cies in their ability to regulate affect at the outset of treatment in comparison
to the ED-only patients, there were no statistically significant differences
between the two groups on the NMR scale at the end of treatment. These
findings are consistent with the Safer, Telch, and Agras (2001) study where
ED clients who were treated with DBT reported lower expectancies to regu-
late negative mood states on the NMR at the beginning of treatment in com-
parison to a wait list control group. However, the DBT group reported an
increase in expectancy to regulate affect such that no differences were
present post-treatment between the DBT group and the wait list control
group. Together these findings suggest that DBT treatment may play an
important role in increasing expectancies around affect regulation and may
be particularly helpful in increasing expectancies in affect regulation for
those ED patients who are comorbidly diagnosed with BPD.
While it could be argued that regression to the mean is responsible for
these findings it is unlikely. First, both the ED-BPD and the ED groups, began
with extremely low scores. For example, both groups had scores that were
more than five standard deviations from the mean of the normal sample.
However, at the end of DBT informed treatment, only the ED-BPD group
showed a statistically significant improvement in ability to regulate affect. The
score on the NMR scale for the ED group remained virtually unchanged. This
finding was consistent across all three scales of the NMR and was highly sig-
nificant even when the stringent criteria of a bonferroni correct was applied.
The findings from this study have several clinical implications. First,
with respect to affect regulation, the current investigation suggests that DBT
treatment may play a critical role in increasing ED-BPD clients expectancies
around their ability to regulate affect. While increasing and promoting cog-
nition about affect regulation does not guarantee a compatible behavioral
response, it is a necessary first step. If an individual does not have the belief
structure in place that they can indeed modulate their affective states the
behavioral response is unlikely to follow.

238
D. D. Ben-Porath et al.
Furthermore, the ability to regulate affect plays a crucial role in learn-
ing skillful behavior in DBT treatment. Baddeley (2007) has contended that
the ability to regulate affect is essential and necessary in order to process
new information. He proposes that when an individuals’ affective state
becomes overly aroused, working memory is disrupted thereby reducing
processing capacity for the task at hand. In short, the ability to learn and
process new information is impaired when emotions are highly aroused.
While more recent models of treatment (e.g., Cooper, 2005; Fairburn,
Cooper, & Shafran, 2003; Heatherton & Baumeister, 1991) have begun to
focus on the role that affect dysregulation may play in the development and
maintenance of eating disorders, it is equally important to recognize the role
that affect dysregulation may play in treatment failure. If individuals are
unable to regulate their affect sufficiently then it becomes more difficult for
them to attend to, process and subsequently utilize interventions taught in
treatment. For the ED-BPD client who exhibits considerable difficulties reg-
ulating affect, information taught in groups and individual therapy may be
impossible to process until their emotions are better managed. Because
DBT treatment has a primary focus on affect regulation, this treatment may
be particularly well suited for those with ED-BPD diagnoses.
An additional clinical implication to these findings is that they provide
direction for clinicians treating those with an ED-BPD diagnosis. It has long
been understood that those with ED-BPD present with a more complicated
clinical picture. These findings suggest that a large part of the complexity in
treating these individuals comes from higher disturbances in general psy-
chopathology (depression, anxiety, impulse control, and affect dysregula-
tion) rather than severity of ED symptoms. Therefore, treating clinicians
must be cognizant to treat symptoms of general distress in addition to the
ED pathology in those ED patients comorbidly diagnosed with BPD.
There are several limitations to the current study. First, because the
study was conducted in an applied clinical setting it was limited by practical
and ethical considerations. Although a control/wait list group would have
been desirable to determine whether changes in both groups were due to
treatment or other non-specific factors (e.g., passage of time, attention, etc.),
this was not possible due to the severity of the illness in these patients.
Recall that all patients admitted to the program met APA (2006) criteria for
partial hospitalization level of care. Thus, due to the severity of their symp-
toms and the need for immediate treatment, all patients were admitted to
the program within a week. An additional limitation of this study is the self
report measure of mood regulation. The NMR is a measure of an individ-
ual’s expectancy to regulate negative mood. While this measure was
employed so that comparisons across previous ED studies could be made
(Telch et al., 1999, 2000), it is important that studies investigate not only
perceived but actual ability to regulate affect in this population. Therefore,
future studies should employ physiological measures of affect regulation

Dialectical Behavior Therapy and Eating Disorders
239
and palm pilot methodology so that participants can rate mood states in the
moment. In addition, due to the time constraints involved in a clinical care
setting, diagnoses for borderline personality disorder were made from a self
report measures rather than a structured or semi-structured interview such
as the SCID. Finally, the current study utilized a modified DBT protocol for
eating disorders. Thus, comparisons between this study and the original
study conducted by Linehan et al. (1993) cannot be made.
In sum, the rates of comorbid BPD have been reported to be as high as
44% in those diagnosed with eating disorders (Gwirtsman et al., 1983). Thus,
there is a compelling need for therapies that address the treatment chal-
lenges associated with this subgroup. While these findings may not general-
ize to less severe ED populations, results from the current study hold out
promise by providing an effective treatment alternative for a subgroup of ED
patients that have traditionally been difficult to treat. Given the known diffi-
culties in affect regulation, increased levels of general psychiatric symptoms,
and poor therapy response in those diagnosed with ED-BPD, treatment
approaches such as DBT that address deficits in affect regulation, may be
critical to treatment success in ED clients comorbidly diagnosed with BPD.
REFERENCES
American Psychiatric Association (2006). Practice guideline for the treatment of
patients with eating disorders. APA Practice Guidelines, 3, 1–128.
Baddeley, A. (2007). Human memory: Theory and practice. Boston: Allyn & Bacon
Beck, A. T. & Steer, R. A. (1990). Manual for the Beck Anxiety Inventory-II.
San Antonio, TX: Psychological Corporation.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck Depression
Inventory-II. San Antonio, TX: Psychological Corporation.
Catanzaro, S. J., & Mearns, J. (1990). Measuring generalized expectancies for nega-
tive mood regulation: Initial scale development and implications, Journal of
Personality Assessment, 54, 546–563.
Cooper, M. (2005). A developmental vulnerability-stress model of eating disorders:
A cognitive approach. In B. L. Hankin & J. R. Z. Abela (Eds.), Development of
psychopathology: A vulnerability-stress perspective (pp. 328–354). Thousand
Oaks, CA: Sage Publications.
Fahy, T., Eisler, I., & Rusell, G. (1993). Personality and treatment response in
bulimia nervosa. British Journal of Psychiatry, 162, 765–770.
Fairburn, C. G., Cooper, Z. & Shafran, R. (2003). Cognitive behaviour therapy for
eating disorders: A “transdiagnostic” theory and treatment. Behaviour Research
and Therapy, 41, 509–528.
Gwirtsman, H. E., Roy-Byrne, P., Yager, J., & Gerner, R. H. (1983). Neuroendocrine
abnormalities in bulimia. American Journal of Psychiatry, 140, 559–563.
Heatherton, T. F., & Baumeister, R. F. (1991). Binge eating as escape from self-
awareness. Psychological Bulletin, 110, 86–108.

240
D. D. Ben-Porath et al.
Herzog, D., Keller, M., Lavori, P., Kenny, G., & Sacks, N. (1992). The prevalence of
personality disorders in 210 women with eating disorders. Journal of Clinical
Psychiatry, 53, 147–152.
Hyler, S. E., Skodol, A .E., Kellman, H. D., Oldham, J. M., & Rosnick, L. (1990).
Validity of the Personality Diagnostic Questionnaire-Revised: Comparison with
two structured interviews. American Journal of Psychiatry, 147, 1043–1048.
Johnson, C., Tobin, D., & Dennis, A. B. (1990). Differences in treatment outcome
between borderline and nonborderline bulimics at one year follow-up.
International Journal of Eating Disorders, 9, 617–628.
Johnson, C., Tobin, D., & Enright, A. (1989). Prevalence and clinical characteristics
of borderline patients in eating-disordered population. Journal of Clinical
Psychiatry, 50, 9–15.
Linehan, M. M. (1993). Cognitive behavioral treatment of borderline personality
disorder. New York: Guilford Press.
Levin, A. P., & Hyler, S. E. (1986). DSM-III personality diagnosis in bulimia.
Comprehensive Psychiatry, 27, 47–53.
Luce, K. H., & Crowther, J. H. (1999). The reliability of the Eating Disorder Exami-
nation-Self-Report Questionnaire Version (EDE-Q). International Journal of
Eating Disorders, 25, 349–351.
Palmer, R. L., Birchall, H., Damani, S., Gatward, N., McGrain, L., & Parker, L. (2003). A
dialectical behavior therapy program for people with an eating disorder and bor-
derline personality disorder—Description and outcome. International Journal of
Eating Disorders, 33, 281–286.
Polivy, J., & Herman, C. P. (1993). Etiology of binge eating: Psychological mechanisms.
Binge eating: Nature, assessment, and treatment. New York: Guilford Press.
Pope, H. G., Frankenburg, F. R., Hudson, J. I., Jonas, J. M., & Yurgelun-Todd, D.
(1987). Is bulimia associated with borderline personality disorder? A controlled
study. Journal of Clinical Psychiatry, 48, 181–184.
Safer, D. L., Telch, C. F., & Agras, W. S. (2001). Dialectical behavior therapy for
bulimia nervosa. American Journal of Psychiatry, 158, 632–634.
Sansone, R. A., Fine, M. A., & Sansone, L. A. (1994). An integrated psychotherapy
approach to the management of self-destructive behavior in eating disorder
patients with borderline personality disorder. Eating Disorders, 2, 251–260.
Sansone, R. A., & Levitt, J. L. (2005). Borderline personality and eating disorders.
Eating Disorders, 13, 71–83.
Steinberg, S., Tobin, D. L., & Johnson, C. (1990). The role of bulimic behaviors in affect
regulation: Different functions for different patient subgroups? International Journal
of Eating Disorders
, 9, 51–55.
Telch, C. F., Agras, W. S., & Linehan, M. M. (2000). Group dialectical behavior
therapy for binge-eating disorder: A preliminary, uncontrolled trial. Behavior
Therapy, 31, 569–582.
Telch, C. F., Agras, W. S., & Linehan, M. M. (2001). Dialectical behavior therapy for
binge eating disorder. Journal of Clinical and Consulting Psychology, 69,
1061–1065.
Wisniewski, L., & Ben-Porath, D. D. (2005). Telephone skill-coaching with eating
disordered clients: Clinical guidelines using a DBT framework. European
Eating Disorders Review, 13, 344–350.

Dialectical Behavior Therapy and Eating Disorders
241
Wisniewski, L., & Kelly, E. (2003). The application of dialectical behavior therapy to
the treatment of eating disorders. Cognitive and Behavioral Practice, 10, 131–138.
Wonderlich, S. A., Fullerton, D., Swift, W. J., & Klein, M. H. (1994). Five-year out-
come from eating disorders: Relevance of personality disorders. International
Journal of Eating Disorders, 15, 233–243.
Wonderlich, S. A., & Mitchell, J. E. (1992). The comorbidity of personality disorders
in the eating disorders. In J. Yager (Ed.), Special problems in managing eating
disorders (pp. 51–86). Washington, DC: American Psychiatric Association Press.
Zeeck, A., Birindelli, E., Sandholz, A., Joos, A., Herzog, T., & Hartmann, A. (2007).
Symptom severity and treatment course of bulimic patients with and without
borderline personality disorder. European Eating Disorders Review, 15, 430–438.
Wyszukiwarka
Podobne podstrony:
Contrasting Clients in Dialectical Behavior Therapy for BPD Marie and Dean , Two Caseswith Diffe
Changes in Negative Affect Following Pain (vs Nonpainful) Stimulation in Individuals With and Withou
Making Contact with the Self Injurious Adolescent BPD, Gestalt Therapy and Dialectical Behavioral T
Stages of change in dialectical behaviour therapy for BPD
Brief Dialectical Behavior Therapy for Suicidal Behaviour and NSSI
Dialectical Behavior Therapy for BPD A Meta Analysis Using Mixed Effects Modeling
APA practice guideline for the treatment of patients with Borderline Personality Disorder
Nutrition?re for Patients With Chronic Renal?ilure
Drug and Clinical Treatments for Bipolar Disorder
Generalized Anxiety Disorder Patient Treatment Manual
Obsessive Compulsive Disorder Patient Treatment Manual
Makówka, Agnieszka i inni Treatment of chronic hemodialysis patients with low dose fenofibrate effe
Differences between the gut microflora of children with autistic spectrum disorders and that of heal
A Proton MRSI Study of Brain N Acetylaspartate Level After 12 Weeks of Citalopram Treatment in Drug
Antisocial Personality Disorder A Practitioner s Guide to Comparative Treatments (Comparative Treatm
Inne zaburzenia odżywiania - Eating Disorder Not OtherWise Specified, PSYCHOLOGIA, PSYCHODIETETYKA
więcej podobnych podstron