2003;12:733-738. Published online August 13, 2003.
Cancer Epidemiol Biomarkers Prev
Philip Bretsky, Christopher A. Haiman, Shlomit Gilad, et al.
and Breast Cancer Risk : The Multiethnic Cohort
Variants
ATM
The Relationship between Twenty Missense
Updated Version
http://cebp.aacrjournals.org/content/12/8/733
Access the most recent version of this article at:
Cited Articles
http://cebp.aacrjournals.org/content/12/8/733.full.html#ref-list-1
This article cites 50 articles, 21 of which you can access for free at:
Citing Articles
http://cebp.aacrjournals.org/content/12/8/733.full.html#related-urls
This article has been cited by 6 HighWire-hosted articles. Access the articles at:
E-mail alerts
related to this article or journal.
Sign up to receive free email-alerts
Subscriptions
Reprints and
Publications Department at
To order reprints of this article or to subscribe to the journal, contact the AACR
Permissions
Department at
To request permission to re-use all or part of this article, contact the AACR Publications
The Relationship between Twenty Missense ATM Variants and Breast
Cancer Risk: The Multiethnic Cohort
1
Philip Bretsky,
2
Christopher A. Haiman, Shlomit Gilad,
Joachim Yahalom, Avital Grossman, Shoshana Paglin,
David Van Den Berg, Laurence N. Kolonel,
Rami Skaliter, and Brian E. Henderson
University of Southern California/Norris Comprehensive Cancer Center,
Department of Preventive Medicine, Keck School of Medicine of the
University of Southern California, Los Angeles, California 90033 [P. B.,
C. A. H., D. V. D. B., B. E. H.]; Quark Biotech Ltd., Nes Ziona, 70400, Israel
[S. G., A. G., R. S.]; Department of Radiation Oncology, Memorial Sloan-
Kettering Cancer Center, New York, New York 10021 [J. Y., S. P.]; and
Etiology Program, Cancer Research Center of Hawaii, University of Hawaii,
Honolulu, Hawaii 96813 [L. N. K.]
Abstract
Deficiencies in tasks of detecting and repairing DNA
damage lead to mutations and chromosomal
abnormalities, a hallmark of cancer. The gene mutated in
ataxia-telangiectasia (A-T), ATM, is a proximal
component in performing such tasks. Studies of A-T
families have suggested an increased risk of breast cancer
among obligate female heterozygous carriers of ATM
mutations. Paradoxically, studies of sporadic and familial
breast cancer have failed to demonstrate an elevated
prevalence of mutations among breast cancer cases. We
characterized the prevalence and distribution of 20 ATM
missense mutations/polymorphisms in a population-based
case-control study of 854 African-American, Latina,
Japanese, and Caucasian women aged >45 years
participating in the Multiethnic Cohort Study. The study
population included 428 incident breast cancer cases and
426 controls. The prevalence of variants ranged from 0%
to 13.6% among controls and varied by ethnicity
(0 –32.5%). Overall, these data provide little support for
an association of ATM missense mutations with breast
cancer among older women. We observed only one
sequence variation (L546V), common among African-
American women, to be overrepresented among all high-
stage breast cancer cases (odds ratio, 3.35; 95%
confidence interval, 1.27– 8.84). After correction for
multiple comparisons, this observed risk modification did
not attain statistical significance. The distribution of
ATM missense mutations and polymorphisms varied
widely across the four ethnic groups studied. Although a
single missense variant (L546V) appeared to act as a
modest predictor of risk, the remaining variants were no
more common in breast cancer cases as compared with
controls.
Introduction
A-T
3
is a pleiotropic inherited disease characterized by neuro-
degeneration, oculocutaneous telangiectases, an increased inci-
dence of cancer, immunodeficiencies, radiation sensitivity and
genetic instability (1, 2). The gene mutated in A-T, ATM, spans
more than 150 kb, is composed of 66 exons (62 coding), and
produces a 13-kb transcript encoding a protein of 3056 amino
acids (3). ATM is a member of the PI3K family as a conse-
quence of its sequence similarity to the PI3K catalytic domain
near the COOH terminus of the protein (4). Heterozygous
carriers of germ-line ATM variants are estimated to constitute
0.35–1% of the general population; the majority of these vari-
ants (
⬎70%) are predicted to lead to either truncation or altered
splicing of the protein (2, 5).
ATM plays a key and proximal role in monitoring and
responding to DNA damage; initial evidence came from case
reports of A-T patients who had fatal reactions to radiation
therapy (6 – 8). It has also been shown that cultured fibroblasts
from A-T patients are multiplicatively more sensitive to the
cytotoxic effects of ionizing radiation as compared with control
cells (9, 10). Similarly, cell lines derived from A-T patients
exhibit defects in several ionizing radiation-inducible cell cycle
checkpoints, the most critical of which is arrest in the G
1
phase
of the cell cycle (11, 12).
Recent evidence has identified ATM as an essential and
proximal component of cell cycle restriction point control. Its
scope of interaction includes the phosphorylation and activation
of p53 (13), c-Abl (14, 15), and Chk2 proteins (16, 17) as well
as the inactivation of Cdc25 (18), all of which promote either
apoptosis or cell cycle arrest. More germane to the oncogenesis
of breast cancer, however, is the recently demonstrated bio-
chemical connection between ATM and the inherited breast
cancer susceptibility gene BRCA1, wherein ATM phosphoryl-
ates BRCA1 in a cluster of residues at the COOH terminus in
response to
␥-radiation (19).
Studies of A-T families have suggested an increased risk
of breast cancer among obligate female heterozygous carriers of
A-T variants (20 –23); a meta-analysis estimated the relative
risk to be 3.9 (24). Paradoxically, studies of sporadic and
familial breast cancer have failed to consistently demonstrate an
elevated prevalence of germ-line ATM gene variants among
breast cancer cases (25, 26). To resolve these apparently dis-
parate findings, Gatti et al. (27) proposed a model for the role
of ATM heterozygosity in breast and other cancers, positing two
classes of ATM mutations: null or truncating mutations that lead
Received 11/25/02; revised 4/28/03; accepted 5/6/03.
The costs of publication of this article were defrayed in part by the payment of
page charges. This article must therefore be hereby marked advertisement in
accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
1
Supported by National Cancer Institute Grants CA 63464 and CA 54281.
2
To whom requests for reprints should be addressed, at Department of Preventive
Medicine, University of Southern California/Norris Comprehensive Cancer Cen-
ter, 1441 Eastlake Avenue, MS #44, P. O. Box 33800, Los Angeles, CA 90033.
Phone: (323) 865-3997; Fax: (323) 865-0127; E-mail: bretsky@usc.edu.
3
The abbreviations used are: A-T, ataxia-telangiectasia; PI3K, phosphatidyli-
nositol 3
⬘-kinase; OR, odds ratio; CI, confidence interval.
733
Vol. 12, 733–738, August 2003
Cancer Epidemiology, Biomarkers & Prevention

to A-T; and missense mutations that cause cancers. Whereas
truncating mutations would block expression of ATM protein,
missense mutations could code for stable ATM proteins that are
present at normal intracellular concentrations but function ab-
normally.
To date, a confluence of evidence from epidemiological as
well as cell and animal systems has provided initial support for
this model. Indirect evidence comes from reports from cohorts
of breast cancer cases carrying missense mutations, whereas
truncating mutations are not common (28 –30). In particular,
Stankovic et al. (31) identified in two A-T families a missense
mutation in the PI3K region (T7271G or V2425G) that was
associated with a 13-fold increased risk of breast cancer. Fur-
thermore, the T7271G missense mutation appeared to be highly
penetrant for breast cancer; expression and activity studies
indicated that the mutation yielded a dominant-negative inhib-
itor of ATM (32). In addition, an inducible expression system
for ATM has been developed showing that several missense
alleles outside of the kinase domain induce a partial A-T
phenotype when introduced into normal cells also in a domi-
nant-negative fashion, perhaps through a mechanism involving
ATM-ATM interaction (33). Lastly, a knock-in mouse model of
a known A-T-causing in-frame deletion results in mice with a
significant number of solid tumors (34). This in-frame deletion
results in the production of a functionally distrupted, nearly
full-length ATM and hence has important implications for
missense mutations. Taken together, these observations provide
support for cancer predisposition among human A-T missense
carriers.
It is important to note that not all missense mutations are
equally important when considering breast cancer susceptibil-
ity. For instance, one might postulate that those mutations
disrupting conserved domains of the ATM protein (e.g., the
PI3K domain) could exert a greater effect on cancer risk as
compared with those outside such regions. To date, the precise
estimates of the risk of breast and other cancers associated with
ATM missense variants are not clearly defined, but any elevated
risk would carry with it significant clinical implications. The
prevalence of ATM missense mutations has not been compre-
hensively evaluated in a multiethnic population, although strik-
ing differences in ATM sequence diversity between African and
non-African populations have been reported (35). In this study,
we evaluated the relationship between 20 missense variants/
polymorphisms in the ATM gene and breast cancer risk in a
case-control study among African-America, Latina, Japanese,
and Caucasian women participating in the Multiethnic Cohort
Study.
Materials and Methods
Multiethnic Cohort Study Population. This nested case-
control study is part of a large, ongoing, multiethnic cohort
study in Hawaii and Los Angeles, California with an emphasis
on diet and other lifestyle characteristics in the etiology of
cancer. Aspects of this large cohort as well as details of its
design and implementation are described more fully elsewhere
(36). Briefly, participants were recruited between 1993 and
1996 from driver’s license files in Hawaii and California; the
age range at baseline was between 45 and 75 years. The focus
was on four main ethnic groups: African Americans; Japanese
Americans; Latinos/Latinas; and Caucasians. The total number
of male and female subjects who comprised the cohort was
215,251. Among women only, baseline data were collected on
22,251 African Americans, 29,957 Japanese, 26,502 Cauca-
sians, and 24,620 Latinas. Participants have completed a base-
line questionnaire designed for self-administration that in-
cluded five sections: (a) background, including medical history
and family cancer history; (b) diet history; (c) medication use;
(d) physical activity; and (e) female reproductive history, in-
cluding menstruation history, parity, age at first full-term preg-
nancy, oral contraceptive use, age at menopause, and the use of
hormones.
Eligible cases were women enrolled in the cohort and
diagnosed between 1993 and 1998 with a new primary, incident
and histologically confirmed breast cancer (International Clas-
sification of Diseases-Oncology, codes C50.0 to C50.9) iden-
tified by linkage of the cohort to population-based cancer
Surveillence, Epidemiology and End Results registries in Ha-
waii and California. Cases were contacted by letter and phone
call and agreed to provide a blood specimen. The participation
rate for providing a blood sample on request was 74% for
cancer cases. Women with carcinoma in situ (non-infiltrating
pathology) and neoplasms of the skin of the breast (Interna-
tional Classification of Diseases-Oncology code 44.5) were not
included as breast cancer cases. Information on stage of disease
was ascertained from tumor registries and used in subgroup
analyses. Stage of disease was characterized as “localized” or
“high stage,” which included regional (by direct extension
and/or lymph node involvement) or systemic disease.
For this particular effort, a nested case-control study was
designed with the intention of comprehensively analyzing the
role of rare ATM missense variants in a multiethnic, popula-
tion-based sample. Given that ATM missense mutation frequen-
cies were hypothesized to be overrepresented among breast
cancer cases, approximately 100 cases from each ethnic group
were initially selected (n
⫽ 428), and women diagnosed with
high-stage disease were oversampled (n
⫽ 222) as compared
with cases who initially presented with localized disease (n
⫽
206).
Blood samples had also been collected from an approxi-
mately 3% random sample of healthy cohort members at base-
line (37, 38). In this effort, we selected approximately 100
controls for each of the four ethnic groups (n
⫽ 426); the
participation rate for cohort controls was 66%. Only controls
with no previous diagnosis of breast cancer were included. The
study was approved by the Institutional Review Board of the
Keck School of Medicine of the University of Southern Cali-
fornia.
ATM Missense Variant Discovery. A separate sequencing
effort had previously been undertaken to discover missense
variants spanning the full-length sequence transcript of the
ATM gene. Full sequence analysis of ATM was performed on
cDNA from peripheral lymphocytes. Briefly, a nested reverse
transcription-PCR approach was used to generate overlapping,
internally labeled PCR products. These cover the entire se-
quence of ATM and were analyzed by sequencing of reverse
transcription-PCR products. All base changes were recon-
firmed. This study included a total of 274 individuals, mostly of
European descent, comprised of 94 primary breast cancer pa-
tients, 70 bilateral cases, and 63 individuals without disease
selected within a hospital-based group of breast cancer cases
from the United States. From this effort, 20 missense variants
of interest were identified; a number of the variants discovered
(but not all) had been described previously (25, 28, 35, 39, 40).
Genotyping. Genomic DNA was purified from the buffy coats
of peripheral blood samples for all cases and controls using the
Puregene DNA Isolation protocol and kit (Gentra Systems,
Minneapolis, MN). Single nucleotide polymorphism genotyp-
ing was performed using the fluorogenic 5
⬘ nuclease assay
734
ATM Variants and Breast Cancer
(TaqMan Assay; Ref. 41). The TaqMan assay was performed
using a TaqMan PCR Core Reagent Kit (Applied Biosystems)
according to manufacturer’s instructions in a final volume of 20
l. Using a fluorescent dye-labeled probe specific for each
allele, the profile of each well was measured in a Sequence
Detection System (model 7700 or model 7900HT; Applied
Biosystems), and the results were analyzed with Sequence
Detection Software (Applied Biosystems).
Statistical Analysis. Data management and descriptive and
univariate analyses were performed using SAS statistical soft-
ware version 8.01 (SAS Institute, Cary, NC). The EpiLog
software system (EpiCenter Software, Pasadena, CA) was used
to estimate ORs and 95% CIs by unconditional logistic regres-
sion while adjusting for ethnicity. The Bonferroni correction for
multiple comparisons was used to define the
␣ level of signif-
icance to avoid spurious positive results. This
␣ critical value
for these analyses is
ⱕ0.0025 (0.05/20). Given this level of
significance, this study, as designed, has 80% power to detect
a relative risk of 1.8 for a 25% minor allele, 2.2 for a 10% minor
allele, 2.8 for a 5% minor allele, and 6.5 for a 1% minor allele.
Results
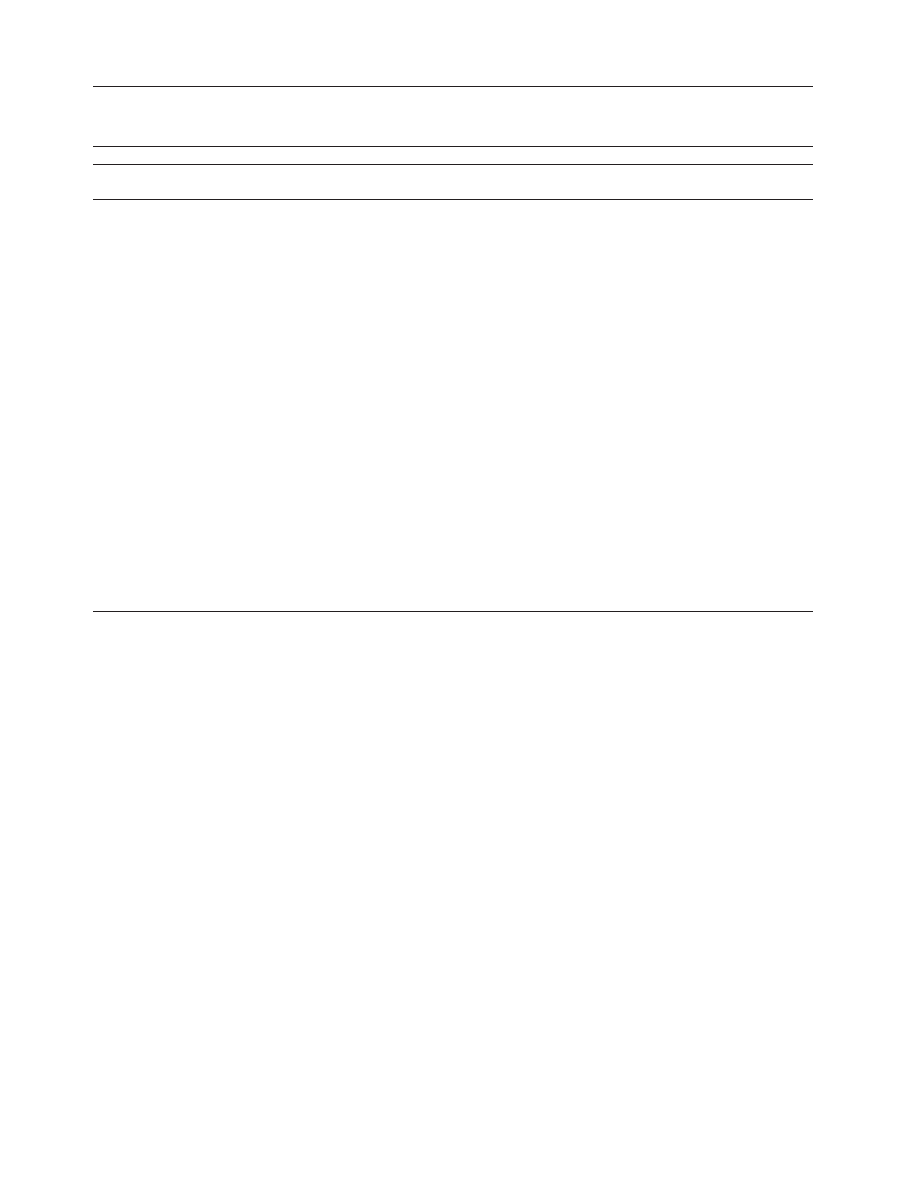
We characterized the prevalence and distribution of 20 ATM
missense mutations/polymorphisms in a case-control study of
854 African-American, Latina, Japanese, and Caucasian
women aged
ⱖ45 years participating in the Multiethnic Cohort
Study. Associations between established reproductive breast
cancer risk factors and breast cancer risk were generally con-
sistent with expectation in all ethnic groups among cases and
controls (Table 1). For instance, cases more often reported a
family history of breast cancer (18.0% of cases versus 9.9% of
controls; P
⫽ 0.01) and tended to have a later first full-term
pregnancy (after age 30 years, 12.2% versus 6.7%; P
heterogeneity
⫽ 0.04).
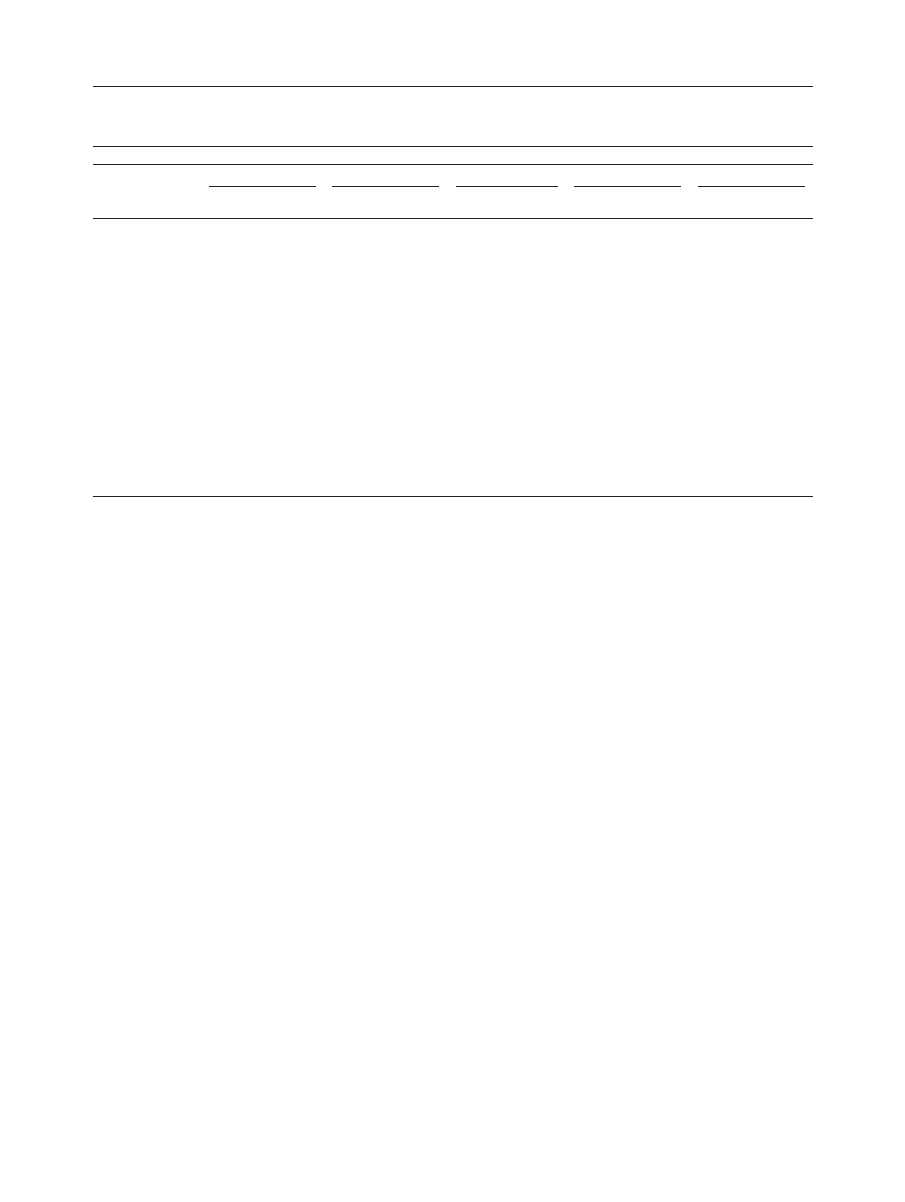
The prevalence of variants ranged in frequency from 0% to
13.6% among controls for all ethnicities combined and varied
widely by ethnicity (0 –33.0%; Table 2). Two of the missense
variants (D126E and D1853N) are previously described com-
mon polymorphisms (35) and are present in equal frequencies
among cases and controls (Table 2). Most of the other missense
variants were uncommon and did not appear to be overrepre-
sented among breast cancer cases as compared with controls
(data not shown).
We did observe an exon 13 missense variant (L546V) to
be modestly overrepresented among all breast cancer cases as
compared with controls (OR
crude
, 2.44; 95% CI, 0.91– 6.54).
This association, however, was limited to African-American
women as the L546V variant was relatively common within this
group [7.7% overall; 10.3% among all cases (12.1% among
those with high-stage disease) and 5.1% among controls]. The
L546V missense mutation was also seen in two Latina cases but
was not seen among any of the Japanese or Caucasian study
participants.
Discussion
Studies of A-T families have documented an increased risk of
breast cancer among both presumptive and obligate heterozy-
gous carriers of ATM gene mutations (21, 22). Whereas this
Table 1
Descriptive statistics of subjects stratified by case or control status (total observations with percentage in parentheses)
Variable
Cases
(n
⫽ 428)
Controls
(n
⫽ 426)
Total
(n
⫽ 854)
P
a
Age at entry (yrs)
⬍50
58 (13.5)
86 (20.2)
144 (16.9)
50–54
61 (14.3)
76 (20.2)
137 (16.0)
55–59
65 (15.2)
65 (15.3)
130 (15.2)
60–64
79 (18.5)
59 (13.9)
138 (16.2)
65–69
90 (21.0)
83 (19.5)
173 (20.3)
70–74
69 (16.1)
51 (12.0)
120 (14.1)
ⱖ75
6 (1.4)
6 (1.4)
12 (1.4)
0.05
Ethnicity
African American
117 (27.3)
117 (27.5)
234 (27.4)
Japanese
100 (23.4)
100 (23.5)
200 (23.4)
Latina
101 (23.6)
99 (23.2)
200 (23.4)
White
110 (25.7)
110 (25.8)
220 (25.8)
0.9995
Family history of breast cancer
Reported
77 (18.0)
42 (9.9)
119 (13.9)
0.0090
Any
⬍50 yrs
33 (7.7)
17 (4.0)
50 (5.9)
0.0015
Family history of ovarian cancer
19 (4.4)
21 (4.9)
40 (4.7)
0.8594
Age at first menstrual period (yrs)
⬍13
229 (54.1)
211 (49.9)
440 (52.0)
13
194 (45.9)
212 (50.1)
406 (48.0)
0.2420
No. of children
None
29 (7.8)
25 (6.7)
54 (7.5)
1–2
79 (21.2)
104 (27.9)
183 (25.3)
2–3
129 (34.6)
141 (37.8)
270 (37.3)
4 or more
114 (30.6)
103 (27.6)
217 (30.0)
0.2475
Age of first full-term pregnancy (yrs)
b
⬍20
108 (29.3)
129 (34.6)
237 (32.1)
21–25
129 (34.9)
141 (37.8)
270 (36.5)
26–30
87 (23.6)
78 (20.9)
162 (21.9)
31
45 (12.2)
25 (6.7)
70 (9.5)
0.0356
a
P was calculated by the
2
test for heterogeneity (categorical variables) comparing cases with controls.
b
Among parous women.
735
Cancer Epidemiology, Biomarkers & Prevention
observation has been corroborated by a Dutch study (42), to
date, most other case-control studies have failed to support the
hypothesis that ATM variant carriers are at an increased risk of
breast cancer (25, 26, 43– 47). Initial surveys, guided by the
suggestion that most “at risk” A-T alleles were truncating or
null mutations (5), relied on methods that identify aberrant
pre-mRNA splice variants, namely, protein truncation test and
single-strand conformational polymorphism methods. The pro-
tein truncation test method would necessarily overlook rare
missense variants, and although the single-strand conforma-
tional polymorphism method is sensitive to missense mutations,
early studies often only considered truncating mutations.
Hence, these studies likely underestimated the prevalence of
ATM variants in breast cancer cases and controls. As a result,
few missense variants have been described or, alternatively,
may have been overlooked. Nevertheless, the T7271G missense
mutation in the PI3K region has been shown to be highly
penetrant for breast cancer, associated with an estimated 13-
fold increased risk, and yields a dominant-negative inhibitor of
ATM (32).
We characterized the prevalence and distribution of 20
ATM missense mutations/polymorphisms in a multiethnic study
population consisting of African-American, Latina, Japanese,
and Caucasian women. In the aggregate, the variants charac-
terized were rare, consistent with other ATM studies (35, 48).
Furthermore, the ethnic distribution of specific variants was
comparable with those reported in previous studies that ob-
served striking differences between African and non-African
populations (35). We also observed the D1856N variant to be
frequent among Caucasians (21.1% of controls), whereas the
D126E variant was very common among African Americans
(32.5%) but was less often observed among the other ethnic
groups. Thorstenson et al. (35) observed a similar ethnic-
specific distribution of these same two polymorphic markers
and suggest that such variation may be the result of random
genetic drift or in fact due to selective pressure.
With the exception of the L546V missense mutation, we
did not note a specific increase in the frequency of ATM
missense mutations in breast carcinoma cases as compared with
controls. However, as a consequence of testing 20 variants, we
did expect one to attain statistical significance as a consequence
of multiple hypothesis testing. As such, a Bonferroni correction
was used; no individual variant attained the critical level of
significance as determined by this procedure.
There is increasing evidence that missense variants in
ATM encode stable, functionally abnormal proteins. Overex-
pression of a mutant ATM polypeptide has previously been
shown to increase genetic instability in normal cells, thus dis-
playing a dominant-negative cellular phenotype (49); such
dominant interference has been demonstrated using an in vitro
mutagenesis approach (33). Furthermore, two ATM mutations
cosegregating with breast cancer in multiple-case families have
been shown to yield a dominant-negative inhibitor of ATM
(32). Unlike truncating variants, which act effectively as null
variants, missense variants exert distinct effects on ATM func-
tion and cancer risk (22). Furthermore, the ATM protein exists
as a component of a multiprotein complex (50); expression of
a mutated protein from even a single missense allele might
interfere with this complex.
Considerable molecular evidence places ATM as a key
and proximal component in DNA damage response, mainte-
nance of genomic integrity, and regulation of cell cycle check-
points (51). Additionally, the demonstrated functional interac-
tion of ATM with BRCA1 (19), along with an inferred
relationship with BRCA2, defines a molecular pathway that
may be disrupted in some fraction of breast cancer patients.
Based on these observations, gene-gene interactions between
ATM missense variants and variants/polymorphisms in BRCA1
and BRCA2 represent a promising avenue of further study.
This study lacked sufficient power to effectively evaluate
some ethnic-specific risks (most particularly among Japanese
and Caucasians) due to the low prevalence of the variant alleles.
However, its multiethnic design will allow us to continue to
examine these and other ATM variants in different ethnic
Table 2
Ethnic-specific distribution of missense variants in the ATM gene among breast cancer cases and controls
Site
a
Amino acid
change
All ethnicities
African American
Latina
Japanese
Caucasian
Cases
(n
⫽ 428)
Controls
(n
⫽ 426)
Cases
(n
⫽ 117)
Controls
(n
⫽ 117)
Cases
(n
⫽ 101)
Controls
(n
⫽ 99)
Cases
(n
⫽ 100)
Controls
(n
⫽ 100)
Cases
(n
⫽ 110)
Controls
(n
⫽ 110)
146
S49C
3 (0.7)
b
6 (1.4)
2 (1.7)
1 (0.9)
0
2 (2.0)
0
1 (1.0)
1 (0.9)
2 (1.8)
378
D126E
43 (10.3)
53 (12.7)
34 (29.3)
38 (32.5)
6 (6.1)
8 (8.3)
0
1 (1.1)
3 (2.9)
6 (5.6)
544
V182L
7 (1.7)
4 (1.0)
4 (3.5)
4 (3.5)
3 (3.0)
0
0
0
0
0
1636
L546V
14 (3.3)
6 (1.4)
12 (10.3)
6 (5.1)
2 (2.0)
0
0
0
0
0
2119
S707P
6 (1.5)
5 (1.2)
1 (0.9)
0
3 (3.0)
2 (2.1)
0
0
2 (1.9)
3 (2.9)
2289
F763L
2 (0.5)
0
1 (0.9)
0
1 (1.0)
0
0
0
0
0
2572
F858L
5 (1.3)
4 (1.1)
1 (0.9)
0
1 (1.1)
2 (2.1)
1 (1.1)
0
2 (2.0)
1 (1.0)
2614
P872S
8 (1.8)
8 (1.9)
7 (6.0)
6 (5.2)
1 (1.0)
0
0
0
0
2 (2.0)
2932
S978P
0
0
0
0
0
0
0
0
0
0
3118
M1040V
7 (1.7)
4 (1.0)
6 (5.2)
3 (2.7)
1 (1.0)
0
0
0
0
1 (0.9)
3161
P1054R
8 (1.9)
13 (3.1)
1 (0.9)
1 (0.9)
2 (2.0)
5 (5.1)
0
1 (1.0)
5 (4.6)
6 (5.5)
3383
Q1128R
4 (1.0)
4 (1.0)
4 (3.5)
3 (2.7)
0
1 (1.0)
0
0
0
0
4258
L1420F
4 (1.0)
7 (1.7)
0
1 (1.0)
2 (2.0)
2 (2.1)
0
1 (1.1)
2 (1.9)
3 (2.8)
5557
D1853N
47 (12.3)
47 (12.5)
9 (8.4)
8 (7.8)
13 (13.8)
13 (14.3)
2 (2.3)
5 (5.9)
23 (24.5)
21 (21.2)
5558
D1853V
2 (0.5)
1 (0.2)
0
1 (0.9)
0
0
0
0
2 (1.9)
0
6096
R2032S
0
1 (0.3)
0
1 (0.9)
0
0
0
0
0
0
6176
T2059I
2 (0.5)
2 (0.2)
2 (1.7)
2 (1.7)
0
0
0
0
0
0
6235
V2079I
3 (0.7)
6 (1.4)
1 (0.9)
2 (1.7)
1 (1.0)
3 (3.0)
0
0
1 (0.9)
1 (0.9)
6437
S2146T
2 (0.5)
2 (0.2)
1 (0.9)
2 (1.7)
1 (1.0)
0
0
0
0
0
6995
L2322F
5 (1.2)
4 (1.0)
5 (4.3)
4 (3.5)
0
0
0
0
0
0
a
Nucleotide position in GenBank (accession no. U82828).
b
Values represent number (percentage in parentheses).
736
ATM Variants and Breast Cancer

groups in the future. Furthermore, population stratification,
although a potential concern (52), is an unlikely explanation for
the demonstrated association in African Americans because the
observed D126E (nucleotide 378) prevalence among cases and
controls (
⬃30%) is identical to that reported among Africans in
a comprehensive survey of ATM diversity (35).
In this study, we evaluated 20 variant sites in four ethnic
groups and their association with breast carcinoma. The L546V
variant appeared to act as a modest but not statistically signif-
icant predictor of risk, although its effect was almost exclu-
sively observed among African-American women. Additional
evaluation of missense variants, particularly among younger
women reporting a family history of breast cancer, is required
to better characterize the effective contribution of this and other
ATM missense variants. The degree to which ATM heterozy-
gosity is associated with an increased risk in breast cancer
remains an open debate. Not all missense mutations will have
the same effect; hence, more research regarding the molecular
structure and function of variant ATM is required.
Acknowledgments
We thank the members of the Multiethnic Cohort Study for their participation and
cooperation and the cohort investigators in Los Angeles and Hawaii.
References
1. Boder, E. Ataxia-telangiectasia: an overview. In: R. A. Gatti (ed.), Ataxia-
Telangiectasia: Genetics, Neuropathology and Immunology of a Degenerative
Disease of Childhood, pp. 1– 63. New York: Alan R. Liss, 1985.
2. Shiloh, Y. Ataxia-telangiectasia: closer to unraveling the mystery. Eur. J.
Hum. Genet., 3: 116 –138, 1995.
3. Savitsky, K., Bar-Shira, A., Gilad, S., Rotman, G., Ziv, Y., Vanagaite, L.,
Tagle, D. A., Smith, S., Uziel, T., Sfez, S., Ashkenazi, M., Pecker, I., Frydman,
M., Harnik, R., Patanjali, S. R., Simmons, A., Clines, G. A., Sartiel, A., Gatti,
R. A., Chessa, L., Sanal, O., Lavin, M. F., Jaspers, N. G. J., Taylor, M. R., Arlett,
C. F., Miki, T., Weissman, S. M., Lovett, M., Collins, F. S., and Shiloh, Y. A
single ataxia telangiectasia gene with a product similar to PI-3 kinase. Science
(Wash. DC), 268: 1749 –1753, 1995.
4. Savitsky, K., Sfez, S., Tagle, D. A., Ziv, Y., Sartiel, A., Collins, F. S., Shiloh,
Y., and Rotman, G. The complete sequence of the coding region of the ATM gene
reveals similarity to cell cycle regulators in different species. Hum. Mol. Genet.,
4: 2025–2032, 1995.
5. Gilad, S., Khosravi, R., Shkedy, D., Uziel, T., Ziv, Y., Savitsky, K., Rotman,
G., Smith, S., Chessa, L., Jorgensen, T. J., Harnik, R., Frydman, M., Sanal, O.,
Portnoi, S., Goldwicz, Z., Jaspers, N. G. J., Gatti, R. A., Lenoir, G., Lavin, M. F.,
Tatsumi, J., Wegner, R. D., Shiloh, Y., and Bar-Shira, A. Predominance of null
variants in ataxia-telangiectasia. Hum. Mol. Genet., 3: 433– 439, 1996.
6. Morgan, J. L., Holcomb, T. M., and Morrissey, R. W. Radiation reaction in
ataxia telangiectasia. Am. J. Dis. Child., 116: 557–558, 1968.
7. Eyra, J. A., Gardner-Medwin, D., and Summerfield, G. P. Leukoencephalop-
athy after prophylactic radiation for leukaemia in ataxia telangiectasia. Arch. Dis.
Child., 63: 1079 –1080, 1988.
8. Gotoff, S. P., Amirmokri, E., and Liebner, E. J. Neoplasia, untoward response
to X-irradiation, and tuberous sclerosis. Am. J. Dis. Child., 114: 617– 625, 1967.
9. Arlett, C. F., Green, M. H., Priestley, A., Harcourt, S. A., and Mayne, L. V.
Comparative human cellular radiosensitivity. I. The effect of SV40 transforma-
tion and immortalisation on the
␥-irradiation survival of skin derived fibroblasts
from normal individuals and from ataxia-telangiectasia patients and heterozy-
gotes. Int. J. Radiat. Biol., 54: 911–928, 1988.
10. Cole, J., Arlett, C. F., Green, M. H., Harcourt, S. A., Priestly, A., Henderson,
L., Cole, H., James, S. E., and Richmond, F. Comparative human cellular
radiosensitivity. II. The survival following
␥-irradiation of unstimulated (G
0
)
T-lymphocytes, T-lymphocyte lines, lymphoblastoid cell lines and fibroblasts
from normal donors, from ataxia-telangiectasia patients and from ataxia-telangi-
ectasia heterozygotes. Int. J. Radiat. Biol., 54: 929 –943, 1988.
11. Kastan, M. B., Zhan, Q., el-Deiry, W. S., Carrier, F., Jacks, T., Walsh, W. V.,
Plunkett, B. S., Vogelstein, B., and Fornace, A. J. A mammalian cell cycle
checkpoint pathway utilizing p53 and GADD45 is defective in ataxia-telangiec-
tasia. Cell, 71: 587–597, 1992.
12. Morgan, S. E., and Kastan, M. B. p53 and ATM: cell cycle, cell death, and
cancer. Adv. Cancer Res., 71: 1–25, 1997.
13. Canman, C. E., Lim, D. S., Cimprick, K. A., Taya, Y., Tamai, K., Sakaguchi,
K., Appella, E., Kastan, M. B., and Siliciano, J. D. Activation of the ATM kinase
by ionizing radiation and phosphorylation of p53. Science (Wash. DC), 281:
1677–1679, 1998.
14. Baskaran, R., Wood, L. D., Whitaker, L. L., Canman, C. E., Morgan, S. E.,
Xu, Y., Barlow, C., Baltimore, D., Wynshaw-Boris, A., Kasta, M. B., and Wang,
J. Y. J. Ataxia telangiectasia mutant protein activates c-Abl tyrosine in response
to ionizing radiation. Nature (Lond.), 387: 516 –519, 1997.
15. Shafman, T., Khanna, K. K., Kedar, P., Spring, K., Kozlov, S., Yen, T.,
Hobson, K., Gatei, M., Zhang, N., Watters, D., Egerton, M., Shiloh, Y., Khar-
banda, S., Kufe, D., and Lavin, M. F. Interaction between ATM protein and c-Abl
in response to DNA damage. Nature (Lond.), 387: 520 –523, 1997.
16. Chaturvedi, P., Eng, W. K., Zhu, Y., Mattern, M. R., Mishra, R., Hurle,
M. R., Zhang, X., Annan, R. S., Lu, Q., Faucette, L. F., Scott, S. F., Li, X., Carr,
S. A., Johnson, R. K., Winkler, J. D., and Zhou, B. B. S. Mammalian Chk2 is a
downstream effector of the ATM-dependent DNA damage checkpoint pathway.
Oncogene, 18: 4047– 4054, 1999.
17. Matsuoka, S., Huang, M., and Elledge, S. J. Linkage of ATM to cell cycle
regulation by the Chk2 protein kinase. Science (Wash. DC), 282: 1893–1897,
1998.
18. Blasina, C., Van de Weyer, I., Laus, M. C., Luyten, W. H. M. L., Parker,
A. E., and McGowan, C. H. The human homologue of the checkpoint kinase Cds1
directly inhibits Cdc25 phosphatase. Cur. Biol., 9: 1–10, 1999.
19. Cortez, D., Wang, Y., Qin, J., and Elledge, S. J. Requirement of ATM-
dependent phosphorylation of Brca1 in the DNA damage response to double-
strand breaks. Science (Wash. DC), 286: 1162–1166, 1999.
20. Concannon, P., and Gatti, R. A. Diversity of ATM gene variants detected in
patients with ataxia-telangiectasia. Hum. Mutat., 10: 100 –107, 1997.
21. Swift, M., Reitnauer, P. J., Morrell, D., and Chase, C. L. Breast and other
cancers in families with ataxia-telangiectasia. N. Engl. J. Med., 316: 1289 –1294,
1987.
22. Swift, M., Morrell, D., Massey, R. B., and Chase, C. L. Incidence of cancer
in 161 families affected by ataxia-telangiectasia. N. Engl. J. Med., 325: 1831–
1836, 1991.
23. Athma, P., Rappaport, R., and Swift, M. Molecular genotyping shows that
ataxia-telangiectasia heterozygotes are predisposed to breast cancer. Cancer
Genet. Cytogenet., 92: 130 –134, 1996.
24. Easton, D. F. Cancer risks in A-T heterozygotes. Int. J. Radiat. Biol., 66
(Suppl.): S177
⫺S182, 1994.
25. Vorechovsky, I., Rasio, D., Luo, L., Monaco, C., Hammarstrom, L., Webster,
A. D. B., Zaloudik, J., Barbanti-Brodano, G., James, M., Russo, G., Croce, C. M.,
and Negrini, M. The ATM gene and susceptibility to breast cancer: analysis of 38
breast tumors reveals no evidence for mutation. Cancer Res., 56: 2726 –2732,
1996.
26. FitzGerald, M. G., Bean, J. M., Hegde, S. R., Unsal, H., MacDonald, D. J.,
Harkin, D. P., Finkelstein, D. M., Isselbacher, K. J., and Haber, D. A. Heterozy-
gous ATM mutations do not contribute to early onset of breast cancer. Nat.
Genet., 15: 307–310, 1997.
27. Gatti, R. A., Tward, A., and Concannon, P. Cancer risk in ATM heterozy-
gotes: a model of phenotypic and mechanistic differences between missense and
truncating mutations. Mol. Genet. Metab., 68: 419 – 423, 1999.
28. Dork, T., Bendix, R., Bremner, M., Rades, D., Klopper, K., Nicke, M.,
Skawran, B., Hector, A., Yamini, P., Steinmann, D., Weise, S., Stuhrmann, M.,
and Karstens, J. H. Spectrum of ATM gene mutations in a hospital-based series of
unselected breast cancer patients. Cancer Res., 61: 7608 –7615, 2001.
29. Sommer, S. S., Buzin, C. H., Jung, M., Zheng, J., Liu, Q., Jeong, S. J.,
Moulds, J., Nguyen, V. Q., Feng, J., Bennett, W. P., and Dritschilo, A. Elevated
frequency of ATM gene missense mutations in breast cancer relative to ethnically
matched controls. Cancer Genet. Cytogenet., 134: 25–32, 2002.
30. Teraoka, S. N., Malone, K. E., Doody, D. R., Suter, N. M., Ostrander, E. A.,
Daling, J. R., and Concannon, P. Increased frequency of ATM mutations in breast
carcinoma patients with early onset disease and positive family history. Cancer
(Phila.), 92: 479 – 487, 2001.
31. Stankovic, T., Kidd, A. M., Sutcliffe, A., McGuire, G. M., Robinson, P.,
Weber, P., Bedenham, T., Bradwell, A. R., Easton, D. F., Lennox, G. G., Haites,
N., Byrd, P. J., and Taylor, A. M. ATM mutations and phenotypes in ataxia-
telangiectasia families in the British Isles: expression of mutant ATM and the risk
of leukemia, lymphoma and breast cancer. Am. J. Hum. Genet., 62: 334 –345,
1998.
32. Chenevix-Trench, G., Spurdle, A. B., Gatei, M., Kelly, H., Marsh, A., Chen,
X., Donn, K., Cummings, M., Nyholt, D., Jenkins, M. A., Scott, C., Pupo, G. M.,
Dork, T., Bendix, R., Kirk, J., Tucker, K., McCredie, M. R. E., Hopper, J. L.,
Sambrook, J., Mann, G. J., and Khanna, K. K. Dominant negative ATM mutations
in breast cancer families. J. Natl. Cancer Inst. (Bethesda), 94: 205–215, 2002.
33. Scott, S. P., Bendix, R., Chen, P., Clark, R., Dork, T., and Lavin, M. F.
Missense mutations but not allelic variants alter the function of ATM by dominant
737
Cancer Epidemiology, Biomarkers & Prevention
interference in patients with breast cancer. Proc. Natl. Acad. Sci. USA, 99:
925–930, 2002.
34. Spring, K., Ahangari, F., Scott, S. P., Waring, P., Purdie, D. M., Chen, P. C.,
Hourigan, K., Ramsay, J., McKinnon, P. J., Swift, M., and Lavin, M. F. Mice
heterozygous for mutation in ATM, the gene involved in ataxia-telangiectasia,
have heightened susceptibility to cancer. Nat. Genet., 32: 185–190, 2002.
35. Thorstenson, Y. R., Shen, P., Tusher, V. G., Wayne, T. L., Davis, R. W., Chu,
G., and Oefner, P. J. Global constraint of ATM polymorphism reveals significant
functional constraint. Am. J. Hum. Genet., 69: 396 – 412, 2001.
36. Kolonel, L. N., Henderson, B. E., Hankin, J. H., Nomura, A. M., Wilkens,
L. R., Pike, M. C., Stram, D. O., Monroe, K. R., Earle, M. E., and Nagamine, F. S.
A multiethnic cohort in Hawaii and Los Angeles: baseline characteristics. Am. J.
Epidemiol., 151: 346 –357, 2000.
37. Feigelson, H. S., McKean-Cowdin, R., Coetzee, G. A., Stram, D. O., Kolonel,
L. N., and Henderson, B. E. Building a multigenic model of breast cancer
susceptibility: CYP17 and HSD17B1 are two important candidates. Cancer Res.,
61: 785–789, 2001.
38. McKean-Cowdin, R., Feigelson, H. S., Pike, M. C., Coetzee, G. A., Kolonel,
L. N., and Henderson, B. E. Risk of endometrial cancer and estrogen replacement
therapy history by CYP17 genotype. Cancer Res., 61: 848 – 849, 2001.
39. Vorechovsky, I., Ortmann, E. K., Steinmann, D., and Dork, T. Missense
variants at ATM gene and cancer risk. Lancet, 353: 1276, 1999.
40. Stankovic, T., Weber, P., Stewart, G., Bedenham, T., Murray, J., Byrd, P. J.,
Moss, P. A., and Taylor, A. M. Inactivation of ataxia-telangiectasia mutated gene
in B-cell chronic lymphocytic leukaemia. Lancet, 353: 26 –29, 1999.
41. Lee, L., Connell, C., and Bloch, W. Allelic discrimination by nick-translation
PCR with fluorogenic probes. Nucleic Acids Res., 21: 3761–3766, 1993.
42. Broeks, A., Urbanus, J. H. M., Floore, A. N., Dahler, E. C., Klijn, J. G. M.,
Rutgers, E. J. T., Devilee, P., Russell, N. S., van Leeuwen, F. E., and van T Veer,
L. J. ATM-heterozygous germline mutations contribute to breast cancer-suscep-
tibility. Am. J. Hum. Genet., 66: 494 –500, 2000.
43. Bay, J., Uhrhammer, N., Pernin, D., Presneau, N., Tchirkov, A., Vuillaume,
M., Laplace, V., Grancho, M., Verrelle, P., Hall, J., and Bignon, Y. High
incidence of cancer in a family segregating a mutation of the ATM gene: possible
role of ATM heterozygosity in cancer. Hum. Mutat., 14: 485– 492, 1999.
44. Chen, J., Birkholtz, G. G., Lindblom, P., Rubio, C., and Lindblom, A. The
role of ataxia-telangiectasia heterozygotes in familial breast cancer. Cancer Res.,
58: 1376 –1379, 1998.
45. Bebb, D. G., Yu, Z., Chen, J., Telatar, M., Gelmon, K., Phillips, N., Gatti,
R. A., and Glickman, B. W. Absence of mutations in the ATM gene in forty-seven
cases of sporadic breast cancer. Br. J. Cancer, 80: 1979 –1981, 1999.
46. Janin, N., Andrieu, N., Ossian, K., Lauge, A., Croquette, M-F., Griscelli, C.,
Debre, M., Bressac-de-Paillerets, B., Aurias, A., and Stoppa-Lyonnet, D. Breast
cancer risk in ataxia telangiectasia (AT) heterozygotes: haplotype study in French
AT families. Br. J. Cancer, 80: 1042–1045, 1999.
47. Olsen, J., Hahnemann, J., Borresen-Dale, A-L., Brondum-Nielsen, K., Ham-
marstrom, L., Kleinerman, R., Kaariainen, H., Lonnqvist, T., Sankila, R., Seer-
sholm, N., Tretli, S., Yuen, J., Boice, J., and Tucker, M. Cancer in patients with
ataxia-telangiectasia and their relatives in the Nordic countries. J. Natl. Cancer
Inst. (Bethesda), 93: 121–127, 2001.
48. Bonnen, P. E., Story, M. D., Ashorn, C. L., Buchholz, T. A., Weil, M. M., and
Nelson, D. L. Haplotypes at ATM identify coding-sequence variation and indicate
a region of extensive linkage disequilibrium. Am. J. Hum. Genet., 67: 1437–1451,
2000.
49. Khanna, K. K. Cancer risk and the ATM gene: a continuing debate. J. Natl.
Cancer Inst. (Bethesda), 92: 795– 802, 2000.
50. Wang, Y., Cortez, D., Yazdi, P., Neff, N., Elledge, S. J., and Qin, J. BASC,
a super complex of BRCA1-associated proteins involvement in the recognition
and repair of aberrant DNA structures. Genes Dev., 14: 927–939, 2000.
51. Elledge, S. J. Cell cycle checkpoints: preventing an identity crisis. Science
(Wash. DC), 274: 1664 –1671, 1996.
52. Pritchard, J. J., and Rosenberg, N. A. Use of unlinked genetic markers to
detect population stratification in association studies. Am. J. Hum. Genet., 65:
220 –228, 1999.
738
ATM Variants and Breast Cancer
Wyszukiwarka
Podobne podstrony:
Two ATM Variants and Breast Cancer Risk
Variants in the ATM gene and breast cancer susceptibility
Testing the Relations Between Impulsivity Related Traits, Suicidality, and Nonsuicidal Self Injury
The Relationship Between Personality Organization, Reflective Functioning and Psychiatric Classifica
Ebsco Garnefski The Relationship between Cognitive Emotion Regulation Strategies and Emotional Pro
Predictors of perceived breast cancer risk and the relation between preceived risk and breast cancer
Wack, Tantleff Dunn Relationship between Electronic Game Playing, Obesity and Psychological Functio
On The Relationship Between A Banks Equity Holdings And Bank Performance
Haisch On the relation between a zero point field induced inertial effect and the Einstein de Brogl
The Relation Between Learning Styles, The Big Five Personality Traits And Achievement Motivation
2012 On the Relationship between Phonology and Phonetics
The relationship between public relations and marketing in excellent organizations evidence from the
The Roles of Gender and Coping Styles in the Relationship Between Child Abuse and the SCL 90 R Subsc
Chiodelli&Tzfadia The Multifaceted Relation between Formal Institutions and the Production of Infor
Posttraumatic Stress Symptomps Mediate the Relation Between Childhood Sexual Abuse and NSSI
Pitts, Relations between Rome and the German Kings
Losing, Collecting, and Assuming Identities The Relationships between the Ring and the Characters in
The Multiple Relations Between Creativity and Personality
The Relationship Between Community Law and National Law
więcej podobnych podstron