1997, 35(7):1757.
J. Clin. Microbiol.
T Pal, N A Al-Sweih, M Herpay and T D Chugh
assay.
IpaC-specific enzyme-linked immunosorbent
and Shigella strains in pediatric patients by an
Identification of enteroinvasive Escherichia coli
http://jcm.asm.org/content/35/7/1757
Updated information and services can be found at:
These include:
CONTENT ALERTS
cite this article),
Receive: RSS Feeds, eTOCs, free email alerts (when new articles
http://jcm.asm.org/site/misc/reprints.xhtml
Information about commercial reprint orders:
http://journals.asm.org/site/subscriptions/
To subscribe to to another ASM Journal go to:
http://jcm.asm.org/
Downloaded from
J
OURNAL OF
C
LINICAL
M
ICROBIOLOGY
,
0095-1137/97/$04.00
10
July 1997, p. 1757–1760
Vol. 35, No. 7
Copyright © 1997, American Society for Microbiology
Identification of Enteroinvasive Escherichia coli and Shigella
Strains in Pediatric Patients by an IpaC-Specific
Enzyme-Linked Immunosorbent Assay
TIBOR PAL,
1,2
* NOURA AHMED AL-SWEIH,
3
MARIA HERPAY,
4
AND
TULSI D. CHUGH
1
Department of Microbiology, Faculty of Medicine, University of Kuwait,
1
and Mubarak Al-Kabeer Hospital,
3
Kuwait,
and Department of Microbiology, University Medical School, Pecs,
2
and Department of Bacteriology, “Bela Johan”
National Institute of Public Health, Budapest,
4
Hungary
Received 20 November 1996/Returned for modification 4 March 1997/Accepted 27 March 1997
A new method, a monoclonal antibody-based enzyme-linked immunosorbent assay (ELISA) recognizing a
secreted, invasion plasmid-coded protein antigen (IpaC), was used to identify enteroinvasive Escherichia coli
and Shigella strains among colonies from 859 cultures of fecal samples from children in Kuwait. A total of
33.8% of the samples were diarrheal. By the immunoassay, enteroinvasive E. coli strains were identified from
two diarrheal samples but from none of the samples from children without diarrhea. These strains were fully
virulent and belonged to serogroup O28ac. In addition, 26 Shigella strains were also recognized by the ELISA,
while only 23 were isolated by routine biotyping and serotyping. For two diarrheal patients, Shigella was
identified by culture only. The study showed that the IpaC-specific immunoassay is a simple and useful tool for
identifying enteroinvasive strains. Furthermore, by reporting the first enteroinvasive E. coli isolates from
Kuwait, the study indicates the presence of this group of pathogens as a potential source of diarrhea in the
region.
The microbiological diagnosis of bacillary dysentery is based
on the selective isolation and biochemical identification of the
four Shigella species, S. dysenteriae, S. flexneri, S. boydii, and S.
sonnei. The result is then confirmed and refined by determin-
ing the serotype of the isolate (3). Recently, in order to im-
prove the sensitivity, specificity, and speed of the diagnosis,
new molecular biological methods have been developed. These
techniques are based either on nucleic acid hybridization with
DNA probes specific for various virulence-related genes (2, 25)
or on a PCR technique with primers flanking these sequences
(9). Some target genes are located on the invasion plasmid (IP)
or, like the ipaH gene, on both IP and the chromosomes of
these pathogens (21, 25). These methods were successfully
used in case-control studies (5) or investigations aimed at de-
tecting posttreatment Shigella carriage (21).
A definite advantage of these molecular biological tech-
niques is that they also identify the other, often overlooked
causative agents of bacillary dysentery, enteroinvasive Esche-
richia coli (EIEC) strains carrying the same virulence-related
genes carried by shigellae (11). The enteroinvasive character
had long been recognized in some 10 E. coli serogroups (6);
however, not all members of these serogroups express the
invasive phenotype. Although invasive isolates are often non-
motile, lactose negative, and lysine decarboxylase negative
(22), the detection of these markers, similar to that of the O
antigens, is not specific or sensitive enough for diagnostic pur-
poses (3). An important reason for our rather limited under-
standing of the epidemiology of EIEC infections is the diffi-
culty in identifying these strains by simple laboratory
techniques.
In order to offer a specific and simple technique for the
microbiological diagnosis of enteroinvasive infections, we de-
veloped an enzyme-linked immunosorbent assay (ELISA) that
can be used to identify EIEC and Shigella strains (17). In the
original form of the method, an absorbed rabbit antiserum
recognizing IP-coded antigens (tentatively called virulence
marker antigen [VMA]) was used (17). Although the proce-
dures for the preparation and standardization of the absorbed
sera were cumbersome, the VMA ELISA proved the feasibility
of this approach (24). Recently, the assay was further devel-
oped and simplified by introducing a monoclonal antibody
(MAIC-1) specific for IpaC (8), a component of the tentative
VMA (19). While growing in the microcultures of the wells of
the ELISA plate, enteroinvasive bacteria secrete IpaC (1), thus
sensitizing the plate for antigen detection by the monoclonal
antibody (8). So far, however, the specificity and sensitivity of
this assay have been assessed with a panel of selected invasive
and noninvasive strains only (8), but they have not been eval-
uated with clinical material. Here we report the results of the
first clinical application of the MAIC-1 ELISA to the identi-
fication of EIEC and Shigella strains in pediatric patients.
MATERIALS AND METHODS
Patients.
A total of 859 fecal samples received from pediatric patients pre-
senting at the Mubarak Al-Kabeer Hospital, Kuwait, were investigated. All fecal
samples received were included in the investigation, no preliminary criteria
concerning the clinical diagnosis or the symptoms of the patients being used. No
special cautions were exercised to exclude from the study samples sent repeat-
edly from the same patients.
Routine bacteriology, biotyping, and serotyping.
The fecal samples were pro-
cessed in the Microbiology Laboratory of Mubarak Al-Kabeer Hospital accord-
ing to the guidelines for public health laboratories in Kuwait (13) for common
bacterial enteric pathogens, i.e., Shigella, Salmonella, Campylobacter, and enter-
opathogenic E. coli. The macroscopic appearance of the specimen was recorded
as formed, loose, or watery, and the presence of blood or mucus was noted.
Loose and watery samples were microscopically examined for the presence of
erythrocytes and leukocytes (RBCs and WBCs, respectively). For the isolation of
Shigella, MacConkey (MC) (Oxoid, Unipath Ltd., Basingstoke, United King-
dom) and salmonella-shigella (SS) (Difco Laboratories, Detroit, Mich.) agar
plates were inoculated before and after Selenite-F broth (Mast Laboratories
Ltd., Herseyside, United Kingdom) enrichment. The plates were investigated by
the technical personnel of the Microbiology Laboratory of Mubarak Al-Kabeer
* Corresponding author. Present address: Department of Microbi-
ology, University Medical School, H-7643 Pecs, Hungary. Phone: 36
(72) 324122. Fax: 36 (72) 315799. E-mail: paltib@apacs.pote.hu.
1757
http://jcm.asm.org/
Downloaded from
Hospital. Colonies suspected of being Shigella were isolated on Kligler’s iron
agar slopes (KIA; Mast Laboratories Ltd.) and urea broth. On the next day, KIA
cultures showing reactions typical of Shigella were serotyped with a set of Shigella
typing sera (Murex Diagnostic Ltd., Dartford, England). The species was con-
firmed in the Vitek automatic system by using the Vitek GNI card (bioMerieux,
Marcy l’Etoile, France). Agglutination of eight to nine colonies from the MC
agar plate for samples from patients younger than 2 years of age was done with
Murex diagnostic pooled sera 2, 3, and 4 for pathogenic E. coli. Serotyping of
suspected EIEC isolates identified by MAIC-1 ELISA (see below) were carried
out with diagnostic sera produced at the Department of Bacteriology, “Bela
Johan” National Institute of Public Health, Budapest, Hungary.
MAIC-1 ELISA.
After isolating colonies for biotyping and serotyping, MC and
SS agar plates with primary cultures were used to pick colonies for the MAIC-1
ELISA. A person unaware of the culture results selected three colonies, possibly
with different morphologies and lactose fermentation patterns, from each plate.
The only restriction in choosing various colony types for the immunoassay was
that colonies with signs of H
2
S production on the SS plate were left untouched.
Altogether, six colonies from each patient’s sample were individually inoculated
into 6 wells of a 96-well sterile tissue culture plates (Nunclon Delta; Nunc,
Roskilde, Denmark) (hereafter referred to as ELISA plate) filled with 200
ml of
tryptic soy broth. Simultaneously, these colonies were also inoculated onto a
Congo red (CR) plate (15) as macrocolonies.
No perimeter rows or columns of the 96-well plates were used for the assays.
On each plates three wells were inoculated with a virulent (YSH 6000) and a
nonvirulent (YSH 6200) S. flexneri 2a strain (provided by C. Sasakawa, Tokyo,
Japan), serving as positive and negative controls, respectively, in the immuno-
assay.
Inoculated ELISA and CR plates were incubated overnight at 37°C. On the
next day the MAIC-1 ELISA was run as described previously (8). Briefly, the
microcultures in the wells were discarded and the free binding sites were blocked
for 1 h at room temperature with 1% bovine serum albumin (BSA) in phosphate-
buffered saline (PBS; pH 7.2). The plates were washed three times with PBS
containing 0.05% Tween 20 (PBS-Tw), and then the IpaC-specific monoclonal
antibody was added as a serum-free supernatant of the cell culture medium
(RPMI 1640; Gibco BRL, Life Technologies Ltd., Paisley, England) of the
hybridoma cell line MAIC-1 (8), which was diluted 1:250 in PBS-Tw containing
0.1% BSA (PBS-Tw-BSA). The plates were incubated for 1 h at 37°C, washed,
and reacted with anti-mouse immunoglobulin–horseradish peroxidase (P260;
Dakopatts, Copenhagen, Denmark). Reactions were developed with 1,2-phe-
nylenediamine substrate (Dakopatts), and the optical density (OD) at 490 nm
was measured on a Dynatech MR 5000 ELISA reader.
Previously (8), it was shown that a cutoff value for the positive reaction in the
ELISA, defined as the mean
1 3 standard deviations for nonvirulent isolates,
differentiated between enteroinvasive and nonenteroinvasive strains. In prelim-
inary experiments with a set of virulent and nonvirulent Shigella and EIEC strains
from our strain collection, this value was determined for the purpose of the
present study to be 0.150. In case of a positive reaction (i.e., OD
$ 0.150) the
corresponding colony taken from the CR plate was retested by the MAIC-1
ELISA. In order to recognize isolates binding to the enzyme-conjugated anti-
mouse antibodies (i.e., false-positive results), the assay was also carried out with
the anti-mouse–horseradish peroxidase conjugate only, replacing the IpaC-spe-
cific antibodies with PBS-Tw-BSA.
Clones that were saved on the CR plate and that showed a positive reaction in
the ELISA and all six selected clones from samples from which an enteroinvasive
pathogen was isolated in the hospital laboratory were also subjected to biochem-
ical and serological identification, as described above.
Confirmatory assays for enteroinvasiveness.
All Shigella and E. coli isolates
recognized by the MAIC-1 ELISA were tested for their capacity to invade HEp-2
cells (10). After Giemsa staining of the infected tissue cultures, the invasive
potentials of the strains were calculated as the number of infected cells of 200
cells examined and was expressed as the percentage of that for the positive
control strain, strain YSH 6000. The E. coli isolates exhibiting a positive reaction
in the immunoassay were also investigated for the expression of the characteristic
pattern of invasion plasmid-coded proteins detected by sera from convalescent-
phase dysenteric patients (16) received from Alf A. Lindberg, Stockholm, Swe-
den. The extraction of bacteria, polyacrylamide gel electrophoresis, and Western
blotting (immunoblotting) were carried out as described previously (19). As
ultimate proof of the enteroinvasive character, E. coli isolates positive by the
assays described above were subjected to the Sereny test (i.e., the guinea pig
keratoconjunctivitis assay) (20).
RESULTS
Altogether, 859 samples were included in the study. On the
basis of macroscopic observations, 33.8% of the samples were
scored as loose or watery, of which 8.2% contained macro-
scopic blood. Microscopically, RBCs were detected in 23.4% of
the diarrheal samples and WBCs were detected in 27.5% of the
diarrheal samples. Sixty-eight nontyphoid Salmonella and 12
Campylobacter jejuni strains were isolated. One patient ex-
creted both Salmonella enteritidis and C. jejuni. From the pa-
tients younger than 2 years of age, 11 E. coli strains belonging
to enteropathogenic E. coli serogroups were isolated.
The results of the isolation and identification of enteroinva-
sive bacteria are presented in Table 1. Shigella species were
identified either by culture or by ELISA in 28 samples, all from
different patients. All 28 samples were marked as loose or
watery (3.25% of the total and 9.62% of the diarrheal sam-
ples). Twenty-six of these samples contained RBCs and WBCs,
and 8 of the samples were macroscopically bloody. By bio-
chemical and serological assays, Shigella organisms were iden-
tified, all from the primary culture plates, in 23 samples, and no
further strains were found after enrichment in Selenite-F
broth. By MAIC-1 ELISA, members of the genus were de-
tected among colonies from 26 samples. In four of the five
samples in which Shigella strains were missed by routine cul-
ture, the pathogen grew as a few colonies of non-lactose fer-
menters (NLF) on the MC agar plate only in a heavy lactose
fermenter background. In the fifth case a few NLF colonies of
S. dysenteriae were also missed on the SS plate in a similar
background.
The MAIC-1 ELISA did not detect one S. sonnei isolate and
one S. flexneri isolate from diarrheal patients in whom the
pathogen was identified by culture (Table 1). By microscopy,
RBCs and WBCs were detected in both mucoid samples, while
no macroscopic blood was seen. Reinvestigating the colonies
tested by ELISA from the S. sonnei-infected patient revealed
that two of the six colonies (both taken from the MC agar
plate) were biochemically S. sonnei, indeed, agglutinating in
the phase I and II typing sera. However, both clones were CR
negative and lost their invasive capacity, as tested on tissue
culture cells, indicating the loss of the IP coding for the target
antigen of the immunoassay (data not shown). No phase I,
CR-positive, invasive, ELISA-positive colonies were found on
reinvestigations of 20 S. sonnei colonies from the MC and SS
agar plates. In the sample from the other patient excreting
Shigella but in which Shigella was not identified by the immu-
noassay, two of the six colonies tested proved to be S. flexneri.
The colonies were taken from MC and SS agar plates, respec-
tively. Similar to the S. sonnei isolate, these colonies did not
bind to CR and they were noninvasive (data not shown). How-
ever, after reinvestigating the SS and MC agar plates contain-
ing the sample from this patient, 5 ELISA-positive, invasive
colonies of 20 colonies tested were found.
By the MAIC-1 ELISA we could identify two E. coli strains
secreting the IpaC antigen. They expressed the O28ac cell wall
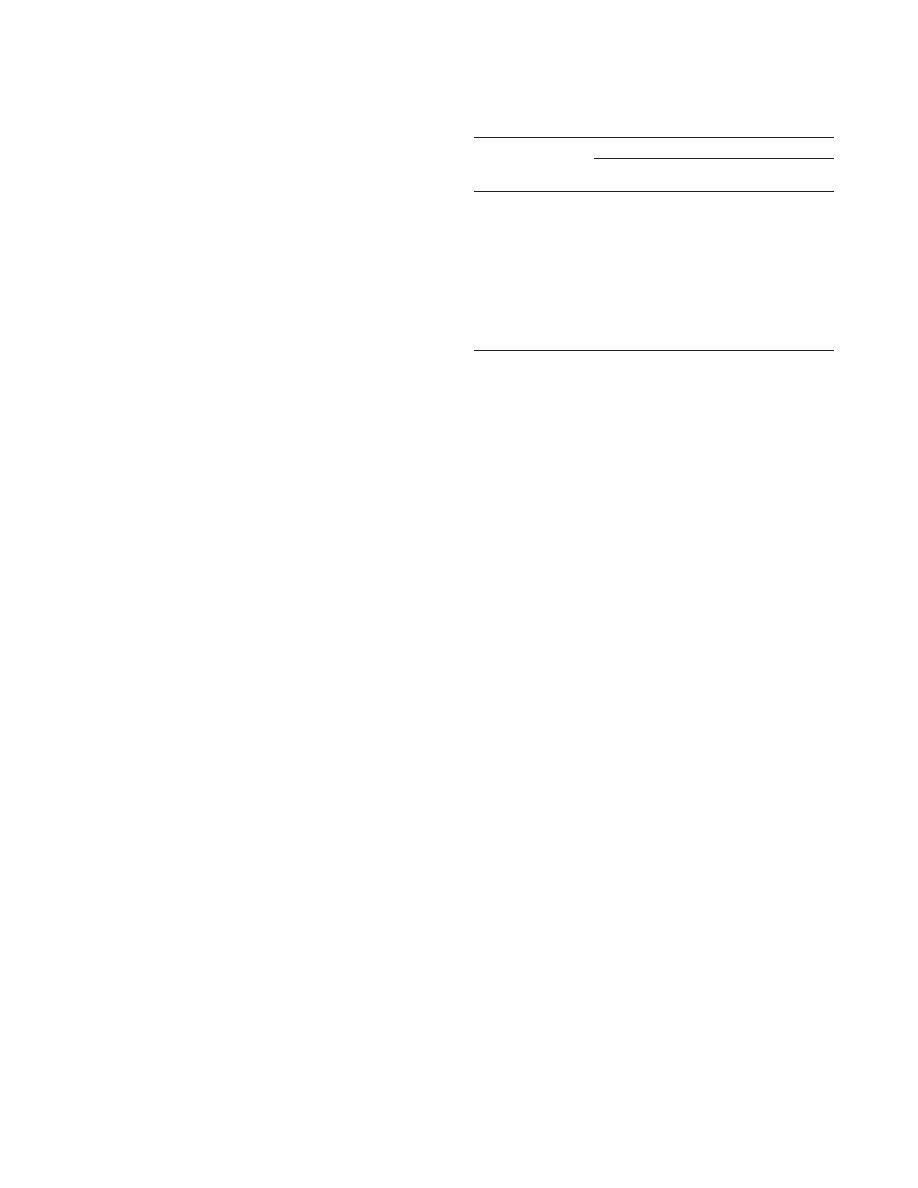
TABLE 1. Identification of enteroinvasive bacteria among colonies
isolated from 859 fecal samples
Species
No. of strains identified
By ELISA
By biotyping
and serotyping
Total
a
S. dysenteriae
1
0
1
S. flexneri
13
12
14
S. boydii
0
0
0
S. sonnei
12
11
13
All Shigella
26
23
28
EIEC
2
0
2
Total
28
23
30
a
Total number of strains identified by ELISA and/or biotyping and serotyping.
1758
PAL ET AL.
J. C
LIN
. M
ICROBIOL
.
http://jcm.asm.org/
Downloaded from

antigen and fermented lactose, but they were unable to decar-
boxylate lysine. Both isolates were nonmotile. The isolates
formed red colonies on CR plates, and they were invasive in
the tissue culture invasion assay, showing 15.2 and 12.3% in-
vasive capacities compared to that of the positive control
strain. They expressed the characteristic protein pattern (i.e.,
VirG and Ipa A, B, C and D) (16) of the virulent strains when
tested with reconvalescent-phase human serum by polyacryl-
amide gel electrophoresis-Western blotting and were positive
by the Sereny test (data not shown). The two EIEC strains
were isolated from independent patients presenting with diar-
rhea at the casualty section of the hospital. The stool samples
were loose but contained no macroscopic blood. They showed
moderate numbers of RBCs and WBCs (i.e., less than 10/high-
power field).
The OD values for the Shigella strains identified by ELISA
varied between 1.405 and 2.000, while those for the two EIEC
isolates were 0.962 to 1.111. Of the total of 5,154 colonies from
the 859 samples tested by ELISA, 3 colonies from three inde-
pendent patients gave false-positive, low OD readings (0.205 to
0.322). All three isolates were shown to bind to the conjugate
in the ELISA without the monoclonal antibody, they were not
invasive, and they did not express the VirG-Ipa proteins by
Western blotting. They were identified as Serratia spp. by bio-
typing.
DISCUSSION
In some developing countries EIEC strains can be respon-
sible for 1 to 6% of cases of diarrhea or dysentery (4, 7, 23),
and an age-related isolation rate of as high as 7% was reported
for 2- to 4-year-old Thai children with diarrhea (5). EIEC
strains also can cause food- or waterborne outbreaks (14). Our
knowledge of the incidence and epidemiology of EIEC infec-
tions is mostly based on limited-scale pilot studies instead of
regular surveillance by clinical microbiology laboratories. This
is due to the fact that neither biotyping nor serotyping is
specific and sensitive enough to identify EIEC strains, and the
confirmatory assays for virulence, i.e., the guinea pig kerato-
conjunctivitis test (20), the epithelial cell invasion assay (10), or
the detection of the IP-coded proteins by Western blotting
(16), are research tools rather than techniques suited for clin-
ical laboratories. The introduction of molecular biological
techniques that detect virulence-specific plasmid or chromo-
somal genes of Shigella and EIEC (2, 3, 9, 25), while highly
sensitive and specific, may still not offer a solution for routine
work, particularly in developing countries. Recently, we pro-
posed that a simple ELISA recognizing an IP-coded antigen
(i.e., IpaC) of these pathogens could provide a highly specific
alternative for the detection of EIEC (8).
In the present study we showed that the IpaC-specific im-
munoassay can indeed successfully be used to recognize EIEC
and Shigella strains among colonies grown from stool samples
from pediatric patients. By the ELISA technique, two E. coli
strains belonging to the recognized EIEC serogroup O28ac
were detected from patients in whom no enteric pathogens
were isolated by biotyping and serotyping. The enteroinvasive
character of the isolates was confirmed in the epithelial cell
invasion assay (10) as well as in the Sereny test (20). Both
strains expressed the characteristic IP-related protein profile
(16) on Western blots. Similar to other invasive isolates of the
same serogroup (3, 22), the two strains did not decarboxylate
lysine, but fermented lactose, which makes their identification
by biotyping difficult. These two EIEC strains are the first ones
ever reported from Kuwait. Together with the recent detection
of similar strains among U.S. troops stationed in the northern
region of Saudi Arabia during Operation Desert Shield (12),
this finding indicates the presence of these pathogens as a
potential cause of diarrhea in this part of the world.
More Shigella isolates were detected by the immunoassay
than by the traditional culture techniques (26 versus 23). How-
ever, in case of this genus, the immunoassay, similar to colony
hybridization with DNA probes, should not necessarily offer an
advantage. Once suspected colonies were carefully spotted on
the plates, the biological and serological identifications should
be straightforward. It should be noted that in the present study
Shigella colonies were seen only on the MC agar plates con-
taining samples from four of five patients in whom shigellae
were identified by the immunoassay only but not by culture. It
is known that for some Shigella strains, media with selective
power better than that of MC agar could be inhibitory (3). If no
NLF colonies were seen on the highly selective plates (e.g.,
agar plates), the culture could mistakenly be declared negative.
The colonies of the two Shigella strains selected for but not
identified as IpaC secretors by ELISA had lost their IpaC-
producing capacity as well as invasive capacity due to the
probable loss of or deletion from the IP. We surmise, however,
that encountering noninvasive colonies only from clinical ma-
terial should be a relatively infrequent phenomenon (one S.
sonnei isolate from the 30 patients excreting either Shigella or
EIEC in this study) due to the counterselection of the non-
virulent clones in the host. In the ELISA the problem of
plasmid instability may partially be overcome by testing larger
numbers of colonies from individual patients. This was found
to be the case for the S. flexneri-infected patient not identified
by the immunoassay, for whom, upon reinvestigation, 5 of 20 S.
flexneri colonies were still found to secrete IpaC. It should be
noted that the loss of or deletion from the IP may result in a
negative reaction with the DNA probes or by PCR as well
unless the deletion leaves the corresponding sequences intact
(18) or genes also present on the chromosome are targeted
(25).
The present study did not aim to compare the diagnostic
performances of ELISA to that of the molecular biological
techniques; therefore, no screening assays other than the
ELISA were used to identify EIEC. However, by using the
polyclonal antibody- and monoclonal antibody-based versions
of this assay, it has previously been found that of the total of ca.
5,500 E. coli strains from various strain collections tested so
far, not a single virulent EIEC strain was missed by the method
(8, 24). Therefore, we believe that among the total of 5,154
colonies tested in this study, none but those identified as Shi-
gella or EIEC expressed the IpaC antigen, i.e., were enteroin-
vasive.
Weak false-positive reactions in this assay are known to
occur rarely (8). In the present study 3 of 5,154 colonies tested
(0.058%) fell in this category, but due to their low frequency
and to the fact that they could easily be identified in repeated
or parallel assays run without the IpaC-specific antibodies, they
hardly indicate a serious diagnostic problem.
The labor requirement of this immunoassay is relatively low,
and it could provide a positive identification in 24 h. Since the
ELISA technique has been used for various purposes in many
laboratories in developing countries, the method could easily
fit into the diagnostic armory, even in clinical laboratories with
relatively low levels of technical sophistication. One could en-
vision the use of the assay as a screening method, as was done
in this study, or it could be applied only to isolates recovered
from diarrheal samples in which no other enteric pathogens
were identified.
On the basis of these results we believe that the IpaC-
specific MAIC-1 ELISA offers a specific and relatively inex-
V
OL
. 35, 1997
ELISA FOR EIEC AND SHIGELLAE
1759
http://jcm.asm.org/
Downloaded from

pensive technique for the identification of enteroinvasive
strains. This is particularly true for the members of the EIEC
group, for which no other simple alternatives are available.
ACKNOWLEDGMENTS
This work was supported by grants MI O92 from Kuwait University
and T 016190 from the National Scientific Research Foundation
(OTKA), Hungary.
The skillful technical assistance of Akbar P. Kalandath is highly
appreciated.
REFERENCES
1. Andrews, G. P., A. E. Hromockyj, C. Coker, and A. T. Maurelli. 1991. Two
novel virulence loci, mxiA and mxiB, in Shigella flexneri 2a facilitate excretion
of invasion plasmid antigens. Infect. Immun. 59:1997–2005.
2. Boileau, C. R., H. M. d’Hauteville, and P. J. Sansonetti. 1984. DNA hybrid-
ization technique to detect Shigella species and enteroinvasive Escherichia
coli. J. Clin. Microbiol. 20:959–961.
3. Echeverria, P., O. Sethabutr, and C. Pitarangsi. 1991. Microbiology and
diagnosis of infections with Shigella and enteroinvasive Escherichia coli. Rev.
Infect. Dis. 13(Suppl. 4):S220–S225.
4. Echeverria, P., O. Sethabutr, O. Serichantalergs, U. Lexomboon, and K.
Tamura.
1992. Shigella and enteroinvasive Escherichia coli infections in
households of children with dysentery in Bangkok. J. Infect. Dis. 165:144–
147.
5. Echeverria, P., D. N. Taylor, U. Lexsomboon, M. Bhaibulaya, N. R. Black-
low, K. Tamura, and R. Sakazaki.
1989. Case-control study of endemic
diarrhoeal diseases in Thai children. J. Infect. Dis. 159:543–548.
6. Farmer, J. J., III., and M. T. Kelly. 1991. Enterobacteriaceae, p. 360–383. In
A. Balows, W. J. Hausler, Jr., K. L. Herrmann, H. D. Isenberg, and H. J.
Shadomy (ed.), Manual of clinical microbiology, 5th ed. American Society
for Microbiology, Washington, D.C.
7. Faundez, G., G. Figueroa, M. Troncoso, and F. C. Cabello. 1988. Charac-
terization of enteroinvasive Escherichia coli strains isolated from children
with diarrhea in Chile. J. Clin. Microbiol. 26:928–932.
8. Floderus, E., T. Pal, K. Karlsson, and A. A. Lindberg. 1995. Identification of
Shigella and enteroinvasive Escherichia coli strains by a virulence-specific,
monoclonal antibody-based enzyme immunoassay. Eur. J. Clin. Microbiol.
Infect. Dis. 14:111–117.
9. Frankel, G., L. Riley, J. A. Giron, J. Valmassoi, A. Friedmann, N. Strock-
bine, S. Falkow, and G. K. Schoolnik.
1990. Detection of Shigella in feces
using DNA amplification. J. Infect. Dis. 161:1252–1256.
10. Hale, T. L., R. E. Morris, and P. F. Bonventre. 1979. Shigella infection of
Henle intestinal epithelial cells: role of the host cell. Infect. Immun. 24:887–
894.
11. Hsia, R. C., P. L. Small, and P. M. Bavoil. 1993. Characterization of viru-
lence genes of enteroinvasive Escherichia coli by TnphoA mutagenesis: iden-
tification of invX, a gene required for entry into HEp-2 cells. J. Bacteriol.
175:
4817–4823.
12. Hyams, K. C., A. L. Bourgeois, B. R. Merrell, P. Rozmajzi, J. Escamilla, S. A.
Thornton, G. M. Wasserman, A. Burke, P. Echeverria, K. Y. Green, A. Z.
Kapikian, and J. N. Woody.
1991. Diarrheal disease during operation Desert
Shield. N. Engl. J. Med. 325:1423–1428.
13. Johny, M., A. A. Hassan, M. A. Ghafoor, K. M. Elhag, and R. Dhar. 1994.
Microbiology procedure manual, p. 40–54. Ministry of Health, Kuwait.
14. Ke´tyi, I. 1989. Epidemiology of the enteroinvasive Escherichia coli, observa-
tions in Hungary. J. Hyg. Epidemiol. Microbiol. Immunol. 33:261–267.
15. Maurelli, A. T., B. Blackmon, and R. Curtiss III. 1984. Loss of pigmentation
in Shigella flexneri 2a is correlated with loss of virulence and virulence-
associated plasmid. Infect. Immun. 43:397–401.
16. Oaks, E. V., T. L. Hale, and S. B. Formal. 1986. Serum immune response to
Shigella protein antigens in Rhesus monkeys and humans infected with Shi-
gella spp. Infect. Immun. 53:57–63.
17. Pal, T., A. S. Pacsa, L. Emody, S. Voros, and E. Se´lley. 1985. Modified
enzyme-linked immunosorbent assay for detecting enteroinvasive Esche-
richia coli and virulent Shigella strains. J. Clin. Microbiol. 21:415–418.
18. Pal, T., P. Echeverria, D. N. Taylor, O. Sethabutr, and S. Hanchalay. 1985.
Identification of enteroinvasive Escherichia coli by indirect ELISA and DNA
hybridization. Lancet ii:785.
19. Pal, T., S. B. Formal, and T. L. Hale. 1989. Characterization of virulence
marker antigen of Shigella spp. and enteroinvasive Escherichia coli. J. Clin.
Microbiol. 27:561–563.
20. Sere´ny, B. 1955. Experimental Shigella keratoconjunctivitis. Acta Microbiol.
Acad. Sci. Hung. 2:293–296.
21. Sethabutr, O., O. Venkatesan, G. S. Murphy, B. Eampokalap, C. W. Hoge,
and P. Echeverria.
1992. Detection of shigellae and enteroinvasive Esche-
richia coli by amplification of the invasion plasmid antigen H DNA sequence
in patients with dysentery. J. Infect. Dis. 167:458–461.
22. Silva, R. M., M. R. F. Toledo, and L. R. Trabulsi. 1980. Biochemical and
cultural characteristics of invasive Escherichia coli. J. Clin. Microbiol. 11:
441–444.
23. Sunthadvanich, R., D. Chiewslip, J. Seriwatana, R. Sakazaki, and P. Echev-
erria.
1990. Nationwide surveillance program to identify diarrhea-causing
Escherichia coli in children in Thailand. J. Clin. Microbiol. 28:469–472.
24. Taylor, D. N., P. Echeverria, T. Pal, O. Sethabutr, S. Saiborisuth, S. Sric-
harmorn, B. Rowe, and J. Cross.
1986. The role of the Shigella spp., entero-
invasive Escherichia coli and other enteropathogens as causes of childhood
dysentery in Thailand. J. Infect. Dis. 153:1132–1138.
25. Venkatesan, M. M., J. M. Buyssee, and D. J. Kopecko. 1989. Use of Shigella
flexneri ipaC and ipaH gene sequences for the general identification of
Shigella spp. and enteroinvasive Escherichia coli. J. Clin. Microbiol. 27:2687–
2691.
1760
PAL ET AL.
J. C
LIN
. M
ICROBIOL
.
http://jcm.asm.org/
Downloaded from
Wyszukiwarka
Podobne podstrony:
A protocol for polymerase chain reaction detection of Enterococcus faecalis and Enterococcus faec
Shigella and enteroinvasive E coli pathogenicity factors
Identification of Shigella species
The Torbeshes of Macedonia Religious and National Identity Questions of Macedonian Speaking Muslims
Identification of inorganic pigments from paintings and ~56F
Sexualities and Identities of Minority Women
Identification of Linked Legionella pneumophila Genes Essential for Intracellular Growth and Evasion
Static detection and identification of X86 malicious executables A multidisciplinary approach
Karen The Effects on Ethnic Identification of Same and Mi
Census and Identity The Politics of Race, Ethnicity and Language in National Censuses (eds D I Kertz
Szczepanik, Renata Development and Identity of Penitentiary Education (2012)
6 6 Detection and Identification of Drugs; Summary
Insensitive Semantics~ A Defense of Semantic Minimalism and Speech Act Pluralism
Estimation of Dietary Pb and Cd Intake from Pb and Cd in blood and urine
Development of Carbon Nanotubes and Polymer Composites Therefrom
historical identity of translation
Analysis of soil fertility and its anomalies using an objective model
Modeling of Polymer Processing and Properties
więcej podobnych podstron