2011 Oct;50(10):1179-94. doi: 10.1111/j.1365-4632.2011.05029.x.
Treatment of acne scarring.
.
1
Department of General Practice, Monash University, South Yarra, Victoria, Australia.
gg@div.net.au
Abstract
BACKGROUND:
Post-acne scarring remains a common entity despite advances in the treatment of acne. This represents
limitations in our quality of therapy and a failure of public education. The level of severe scarring remains
as much an ongoing challenge to prevent as well as manage.
METHODS:
This review will concentrate on the methods by which acne scarring may be improved and the available
evidence for their utility. It will also rely on a grading scale of disease burden to classify patients and their
ideal therapy. New therapies allowing treatment of scarring in areas other than the face will also be
highlighted.
RESULTS:
Tabulated treatment planning will present algorithms summarizing best practice in the treatment of post-
acne scarring.
CONCLUSION:
Post-acne scarring is being better managed. Grade 1 scars with flat red, white, or brown marks are best
treated with topical therapies, fractionated and pigment or vascular-specific lasers and, occasionally,
pigment transfer techniques. Grade 2 mild scarring as seen primarily in the mirror is now the territory of
non-ablative fractionated and non-fractionated lasers as well as skin rolling techniques. Grade 3 scarring,
visible at conversational distance but distensible, is best managed by traditional resurfacing techniques or
with fractional non-ablative or ablative devices, sometimes including preparatory surgical procedures.
Grade 4 scarring, where the scarring is at its most severe and non-distensible, is most in need of a
combined approach.
© 2011 The International Society of Dermatology

Retinoic acid and glycolic acid combination in the treatment of acne
scars.
.
1
Department of Dermatology, CUTIS, Academy of Cutaneous Sciences, Bengaluru, Karnataka,
India.
Abstract
INTRODUCTION:
Acne is a prevalent condition in society affecting nearly 80-90% of adolescents often resulting in
secondary damage in the form of scarring. Retinoic acid (RA) is said to improve acne scars and reduce
postinflammatory hyperpigmentation while glycolic acid (GA) is known for its keratolytic properties and its
ability to reduce atrophic acne scars. There are studies exploring the combined effect of retinaldehyde
and GA combination with positive results while the efficacy of retinoic acid and GA (RAGA) combination
remains unexplored.
AIM:
The aim of this study remains to retrospectively assess the efficacy of RAGA combination on acne scars
in patients previously treated for active acne.
MATERIALS AND METHODS:
A retrospective assessment of 35 patients using topical RAGA combination on acne scars was done. The
subjects were 17-34 years old and previously treated for active acne. Case records and photographs of
each patient were assessed and the acne scars were graded as per Goodman and Baron's global
scarring grading system (GSGS), before the start and after 12 weeks of RAGA treatment. The differences
in the scar grades were noted to assess the improvement.
RESULTS:
At the end of 12 weeks, significant improvement in acne scars was noticed in 91.4% of the patients.
CONCLUSION:
The RAGA combination shows efficacy in treating acne scars in the majority of patients, minimizing the
need of procedural treatment for acne scars.
KEYWORDS:
Acne scars; glycolic acid; retinoic acid; retinoic acid and glycolic acid
Hyaluronic acid inhibits the glial scar formation after brain damage
with tissue loss in rats.
1
Graduate Institute of Clinical Medicine, College of Medicine, Taipei Medical University, Taipei
110, Taiwan.
Abstract
BACKGROUND:
Brain tissue scarring (gliosis) was believed to be the major cause of epileptic focus after brain injury, and
prevention of scarring could reduce the incidence of seizure. We tried the HA coating onto the cortical
brain defect of Spraque-Dawley rats to reduce the marginal glial scarring.
METHODS:
A 4 x 2 x 2 mm(3) cortical defect was created in the brain of Spraque-Dawley rats. Three percent HA gel
was coated onto the lesion for the experimental groups and normal saline solutions for the control groups.
The brain was retrieved 4, 8, and 12 weeks after treatment. The brains were then sectioned and
processed for H&E and GFAP staining, and the thickness of the scarring and the number of GFAP+ cells
were analyzed.
RESULTS:
The thickness of cutting marginal gliosis was significantly decreased in the HA groups. The 12-week HA
group showed the smallest thickness of gliosis, whereas the 12-week control group exhibited the largest
thickness of gliosis. The significant difference in the thickness of gliosis was also noted between the HA
and the control groups 8 weeks after treatment. The number of GFAP+ cells was also significantly
decreased in the HA groups when compared to the respective control group 4, 8, and 12 weeks after the
surgery.
CONCLUSION:
The results support the hypothesis that HA inhibits glial scarring not only by decreasing the thickness of
gliosis but also by reducing the number of the glial cells. Furthermore, our results suggest that HA might
be used to reduce glial scar formation in central nervous system surgery, which subsequently prevents
the post-operation or posttraumatic seizure incidence
2010 Sep;9(3):246-8. doi: 10.1111/j.1473-2165.2010.00513.x.
Lactic acid peeling in superficial acne scarring in Indian skin.
Abstract
INTRODUCTION:
Chemical peeling with both alpha and beta hydroxy acids has been used to improve acne scarring with
pigmentation. Lactic acid, a mild alpha hydroxy acid, has been used in the treatment of various
dermatological indications but no study is reported in acne scarring with pigmentation.
AIMS:
To evaluate the efficacy and safety of full strength pure lactic acid 92% (pH 2.0) chemical peel in
superficial acne scarring in Indian skin.
MATERIAL AND METHODS:
Seven patients, Fitzpatrick skin type IV-V, in age group 20-30 years with superficial acne scarring were
enrolled in the study. Chemical peeling was done with lactic acid at an interval of 2 weeks to a maximum
of four peels. Pre- and post-peel clinical photographs were taken at every session. Patients were followed
every month for 3 months after the last peel to evaluate the effects.
RESULTS:
At the end of 3 months, there was definite improvement in the texture, pigmentation, and appearance of
the treated skin, with lightening of scars. Significant improvement (greater than 75% clearance of lesions)
occurred in one patient (14.28%), good improvement (51-75% clearance) in three patients (42.84%),
moderate improvement (26-50% clearance) in two patients (28.57%), and mild improvement (1-25%
clearance) in one patient (14.28%).
© 2010 Wiley Periodicals, Inc.
Biweekly serial glycolic acid peels vs. long-term daily use of topical
low-strength glycolic acid in the treatment of atrophic acne scars.
1
Department of Dermatology, Faculty of Medicine, Gaziantep University, Turkey.
Abstract
BACKGROUND AND OBJECTIVE:
Treatment of atrophic acne scars is difficult and generally unsatisfactory. Although many clinical studies
have been performed to investigate the efficacy of glycolic acid in the treatment of acne vulgaris, to the
best of our knowledge no placebo-controlled study has been carried out to ascertain the effect of glycolic
acid on atrophic postacne scars.
DESIGN:
A single, blind, placebo-controlled, randomized comparative clinical study was conducted in 58 women
with atrophic acne scars. The subjects were randomly divided into three study groups. Glycolic acid peels
with 20%, 35%, 50%, and 70% concentrations were applied serially at 2-week intervals to 23 patients in
Group A. Twenty patients in Group B used a 15% glycolic acid cream once or twice daily for a period of
24 weeks. The remaining 15 patients in Group C applied a placebo cream twice daily during the same
period.
RESULTS:
The differences between the results in the different groups were statistically significant at week 24
(P<0.001). Home application of low-strength glycolic acid was better tolerated and had less side-effects
than glycolic acid peels; however, repeated short-contact 70% glycolic acid peels provided superior
results compared with the maintenance regimen (P<0.05), and apparently good responses were
observed only in the peel group (P<0.01).
CONCLUSIONS:
Glycolic acid peeling is an effective modality for the treatment of atrophic acne scars, but repetitive peels
(at least six times) with 70% concentration are necessary to obtain evident improvement. Long-term daily
use of low-strength products may also have some useful effects on scars and may be recommended for
patients who cannot tolerate the peeling procedure.
J Cutan Aesthet Surg. 2009 Jul-Dec; 2(2): 104–106.
doi:
PMCID: PMC2918339
The Efficacy of Silicone Gel for the
Treatment of Hypertrophic Scars and
Keloids
and
Copyright and License information ►
This article has been
Abstract
Topical self drying silicone gel is a relatively recent treatment modality promoted as an
alternative to topical silicone gel sheeting. Thirty patients with scars of different types including
superficial scars, hypertrophic scars, and keloids were treated with silicon gel application. The
results of the self-drying silicone gel have been satisfactory.
Keywords: Keloids, scars, silicone
INTRODUCTION
Scars vary greatly in quality, depending on individual and racial patient features, the nature of
the trauma, and the conditions of wound healing.[
] They frequently determine aesthetic
impairment and may be symptomatic, causing itching, tenderness, pain, sleep disturbance,
anxiety, depression and disruption of daily activities. Other psychological sequelae include
posttraumatic stress reactions, loss of self esteem and stigmatization leading to a diminished
quality of life. Scar contractures also can determine disabling physical deformities.[
] All these
problems are more troublesome to the individual patient, particularly when the scar cannot be
hidden by clothes. This study was undertaken to verify the efficacy of a new topical silicone
treatment; a self-drying spreadable gel that needs no means of fixation and cannot be seen
because of complete transparency.
Silicone gel contains long chain silicone polymer (polysiloxanes), silicone dioxide and volatile
component. Long chain silicone polymers cross link with silicone dioxide. It spreads as an ultra
thin sheet and works 24 hours per day.[
] It has a self drying technology and itself dries within
4-5 minutes. It has been reported to be effective and produce 86% reduction in texture, 84% in
color and 68% in height of scars.[
] Silicon gel exerts several actions which may explain this
benefit in scars:
a. It increases hydration of stratum corneum and thereby facilitates regulation of fibroblast
production and reduction in collagen production. It results into softer and flatter scar. It
allows skin to "breathe".
b. It protects the scarred tissue from bacterial invasion and prevents bacteria-induced
excessive collagen production in the scar tissue.
c. It modulates the expression of growth factors, fibroblast growth factor β (FGF β) and
tumor growth factor β (TGF β). TGF β stimulates fibroblasts to synthesize collagen and
fibronectin. FGF β normalizes the collagen synthesis in an abnormal scar and increases
the level of collagenases which breaks down the excess collagen. Balance of fibrogenesis
and fibrolysis is ultimately restored.
d. Silicone gel reduces itching and discomfort associated with scars.
The advantages of silicon gel include easy administration, even for sensitive skin and in children.
It can be applied for any irregular skin or scar surfaces, the face, moving parts (joints and
flexures) and any size of scars. A tube of 15 gram contains enough silicone gel to treat 3-4 inches
(7.5-10 cm) scar twice a day for over 90 days.
MATERIALS AND METHODS
The study enrolled 30 patients having scars. Written informed consent was taken from all the
patients before the study. Also, prior approval of hospital ethical committee was taken before the
study. The silicone gel was applied as a thin film twice a day. It was rubbed with fingertips for 2-
3 minutes. For fresh scars, treatment was started just days after wound closure or after 5-10 days.
The scars were evaluated at monthly intervals. The appearance of scar, including scar type, scar
size and scar color was assessed by the physician. We classified hypertrophic scar as a red or
dark pink, raised (elevated) sometimes itchy scar confined within the border of the original
surgical incision, with spontaneous regression after several months and a generally poor final
appearance. A keloid is instead classified as a scar red to brown in colour, very elevated, larger
than the wound margins very hard and sometimes painful or pruritic with no spontaneous
regression.
Patients were observed and the results were compared at monthly follow up examinations.
Follow up was done for 6 months. All scars were measured and photographed before treatment
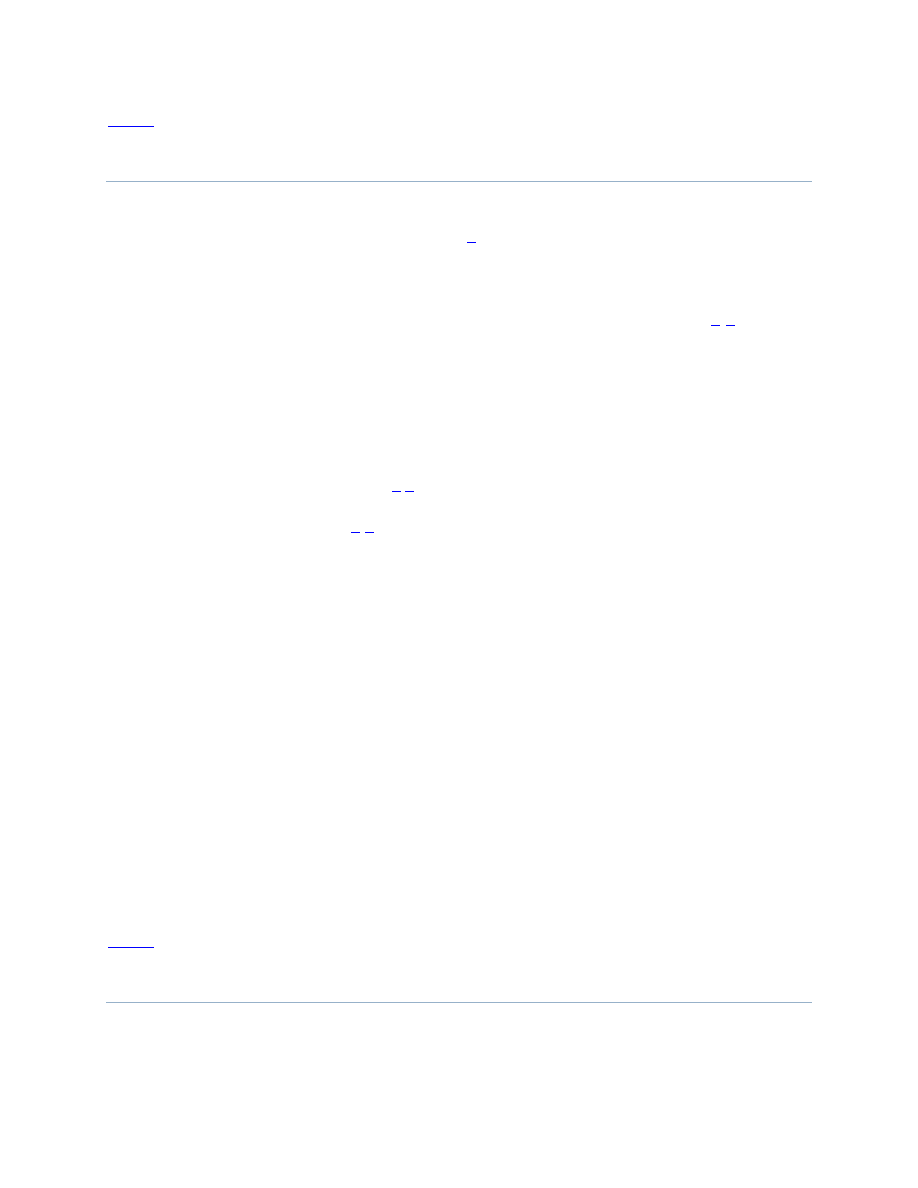
onset. Scars were graded 1 to 4 on the basis of criteria in
. Final photographs were taken
at this time.
Classification of scars according to morphologic features
RESULTS
Eleven cases (36.66%) were in the age groups of 30-40 years, 8 (26.66%) cases between 20-30
years, 5 (16.66%) cases between 40-50 years, 2 (6.610%) cases between 10-20 years and 50-60
years of age each and 1 (3.33%) case of > 60 years of age and between 5 and 10 years of age
each. Male:Female ratio was 2:1. It was also seen that most (40%) of the scars were between 1
and 3 months duration, 26.6% of scars were of less than 1 month duration, 20% of scars were
between 3 and 6 months and 13.33% scars were of more than 6 months duration. The commonest
type of scars were hypertrophic scars (Grade III, 50%) followed by mildly hypertrophic scars
(Grade II, 26.6%) and keloids (Grade IV, 23.33%). Most of the scars were between 1 and 3
months duration (40%), 26.6% of scars were of less than 1 month duration, 20% of scars were
between 3 and 6 months and 13.33% scars were of more than 6 months duration,
After treatment, improvement was noted in the scars [Figures
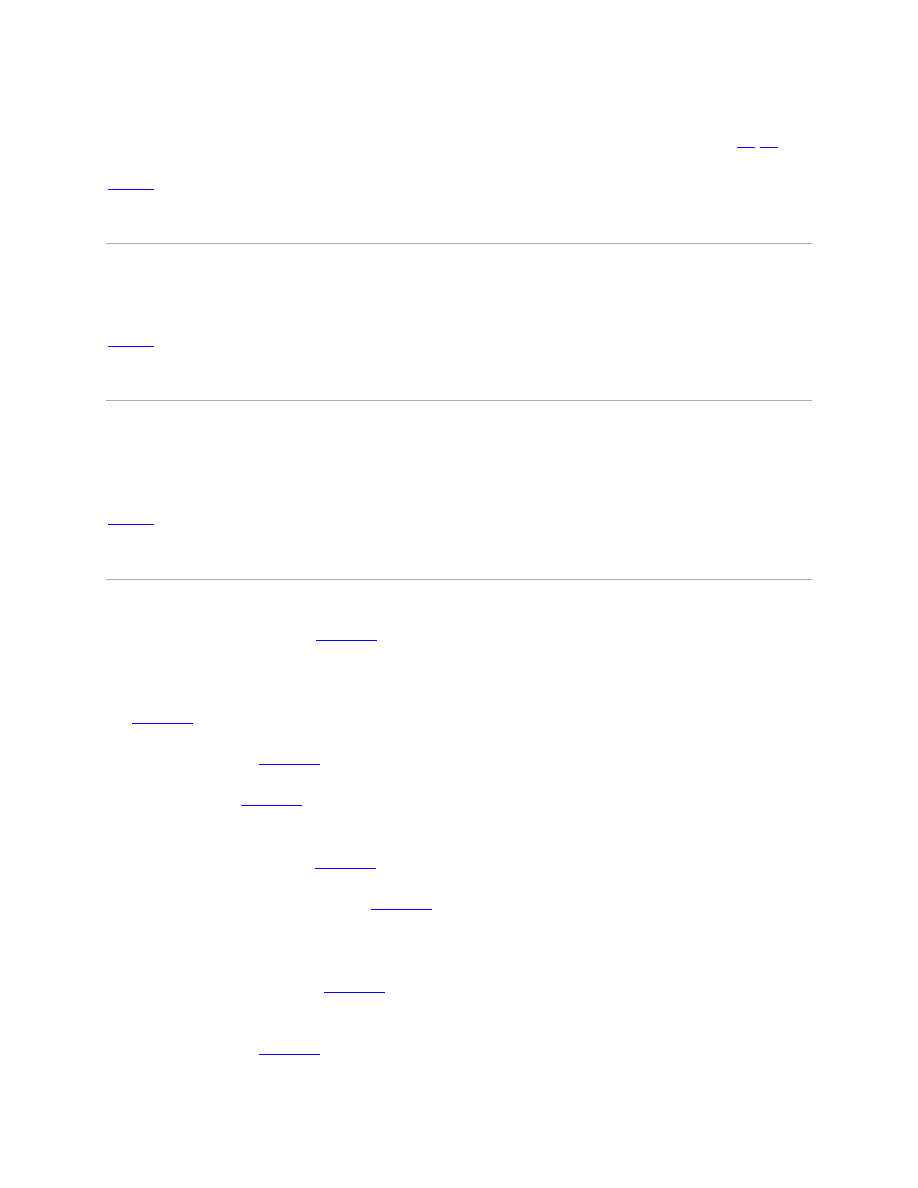
]. Sixty percent scars
were graded as normal (Grade I), while 20% were graded as mildly hypertrophic (Grade II).
Twenty percent of scars were of Grade III and IV at the end of study;10% in each grade [
]. Side effects were few. Allergic reaction to silicone gel was seen in one case and mild
desquamation was seen in 2 cases.
A patient with hypertrophic scar before and after treatment
A patient with minor keloid before and after treatment
Grading of scars after treatment
A patient with burn scar before and after treatment
DISCUSSION
Since the early 1980s, silicone gel sheeting has been widely used in the treatment of hypertrophic
scars and keloids. Several clinical studies and reviews have confirmed its efficacy.[
While many treatments have been suggested in the past for scars, only a few of them have been
supported by prospective studies with adequate control group. Only two treatments can be said to
have sufficient evidence for scar management; topical application of silicone gel sheeting and the
intralesional injection of corticosteroids.[
] The former generally is indicated as both a
preventive and the therapeutic device, the latter as a therapeutic agent only.[
] Topical silicone
gel sheeting is cumbersome to keep on the scar, and the patient compliance often is low for
lesions in visible areas.[
] Tapes or bandaging frequently is not accepted. It may also lead to
skin irritation, which can require discontinuation of treatment, especially in hot climates. Gel
sheeting is effective for scar control, but patient compliance with the method is not always
satisfactory.[
] Steroid injections are painful and may lead to skin atrophy and dyschromies.
They usually are contraindicated for large areas and for children.
Topical silicon gel application can overcome some of these limitations.
Self drying silicone gel is appealing because it is effective, no fixation is required; it is invisible
when dry; and sun blocks, makeup or both can be applied in combination.
However, on areas of the body covered by clothes, it must be perfectly dry before the patient
dresses, and this may not be always practical. All the patients felt the gel was easy to apply, but
some complained of prolonged drying time. The use of a hair dryer was recommended to
overcome this problem. When the scars are located in visible areas, especially on the face,
patients can experience psychological discomfort with the visibility of the treatment. In warm
climates, skin reactions are relatively common, often leading to treatment interruption.[
CONCLUSIONS
Topical silicon gel is safe and effective treatment for hypertrophic and keloidal scars. It is easy to
apply and cosmetically acceptable.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
1. Tuan TL, Nichter LS. The molecular basis of keloid and hypertrophic scar formation. Mol
Med Today. 1998;4:19–24. [
2. Dyakov R, Hadjiiski O. Complex treatment and prophylaxis of post-burn cicatrization in
childhood. Ann Burns Fire Disasters. 2000;13:238–42.
3. Ahn ST. Topical silicone gel: A new treatment for hypertrophic scars. Surgery. 1989;106:781–
7. [
4. Ahn ST. Topical silicone gel for the prevention and treatment of hypertrophic scar. Arch Surg.
1991;126:499–504. [
5. Beranek JT. Why does topical silicone gel improve hypertrophic scars? A hypothesis. Surgery.
1990;108:12–18. [
6. Quinn KJ. Silicone gel in the scar treatment. Burns. 1987;13:833–5.
7. Sawada Y, Sone K. Treatment of scars and keloids with a cream containing silicone oil. Br J
Plast Surg. 1990;43:683–6. [
8. Poston J. The use of the silicone gel sheeting in the management of hypertrophic and keloids
scars. J Wound Care. 2000;9:10–2. [
9. Suetake T, Sasai S, Zhen YX, Tagami H. Effects of silicone gel sheet on the stratum corneum
hydration. Br J Plast Surg. 2000;13:157–9.
10. Baum TM, Busuito MJ. Use of glycerine-based gel sheeting in scar management. Adv
Wound Care. 1998;11:40–3. [
11. Niessen FB. The use of silicone occlusive sheeting (Sil-K) and silicone occlusive gel
(Epiderm) in the prevention of hypertrophic scar formation. Plast Reconstr Surg.
1998;102:1962–72. [
12. Mustoe TA, Cooter RD, Gold MH, Hobbs FD, Ramelet AA, Shakespeare PG, et al.
International clinical recommendations on scar management. Plast Reconstruc Surg.
2002;110:560–3. [
13. Berman B, Flores F. Comparison of a silicone gel filled cushion and silicone gel sheeting for
the treatment of hypertrophic or keloid scars. Dermatol Surg. 1999;25:484–90. [
14. Carney SA, Cason CG, Gowar JP. Cica care gel sheeting in the management of hypertrophic
scarring. Burns. 1994;20:163–7. [
15. Perkins K, Davey RB, Wallis KS. Silicone gel: A new treatment for burn scars contractures.
Burns Incl Therm Inj. 1983;9:201–6. [
16. Mercer NS. Silicone gel in the treatment of keloid scars. Br J Plast Surg. 1989;42:83–8.
[
17. Dockery GL. Treatment of hypertrophic and keloid scars with silastic gel sheeting. J Foot
Ankle Surg. 1994;33:110–9. [
18. Cruz-Korchin NI. Effectiveness of silicone sheets in the prevention of hypertrophic breast
scars. Ann Plast Surg. 1996;37:345–8. [
19. Gibbons M, Zuker R, Brown M, Candlish S, Snider L, Zimmer P. Experience with silastic
gel sheeting in pediatric scarring. J Burn Care Rehabil. 1994;15:69–73. [
20. Borgognoni L, Martini L, Chiarugi C, Gelli R, Reali UM. Hypertrophic scars and keloids:
Immunophenotypic features and silicone sheets to prevent recurrences. Ann Burns Fire
Disasters. 2000;8:164–6.
21. Nikkonen MM, Pitkanen JM, Al Qattan MM. Problems associated with the use of silicone
gel sheeting for hypertrophic scars in the hot climate of Saudi Arabia. Burns. 2001;27:498–500.
[
Articles from Journal of Cutaneous and Aesthetic Surgery are provided here courtesy of
Medknow Publications
Wyszukiwarka
Podobne podstrony:
A review of the use of adapalene for the treatment of acne vulgaris
Atrophic Acne Scarring A Review of Treatment Options
Effective Treatments of Atrophic Acne Scars
Magnetic Treatment of Water and its application to agriculture
Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syn
Diagnosis and Treatment of Autoimmune Hepatitis
Introduction to the Magnetic Treatment of Fuel
65 935 946 Laser Surface Treatment of The High Nitrogen Steel X30CrMoN15 1
APA practice guideline for the treatment of patients with Borderline Personality Disorder
Flashback to the 1960s LSD in the treatment of autism
The term therapeutic relates to the treatment of disease or physical disorder
Friday's Treatment of Social Issues
Treatments of Alcoholism
Presentation 5 Psychological Aspects of Treatment of the S
7 77 93 Heat and Surface Treatment of Hot Works for Optimum Performance
Drugs for treatment of malaria
Periacetabular osteotomy for the treatment of dysplastic hip with Perthes like deformities
14 Treatment of Strokes
więcej podobnych podstron