
Human Papillomavirus and Cervical Cancer Knowledge,
Health Beliefs, and Preventive Practices in 2 Age Cohorts: A
Comparison Study
Kymberlee Montgomery, DrNP, MSN; and Mary Ellen Smith-Glasgow, PhD, RN
Drexel University College of Medicine and College of Nursing, Philadelphia, Pennsylvania
ABSTRACT
Background:
Genital human papillomavirus (HPV) infection is the most common sexually transmitted
infection in the United States and a known precursor of cervical cancer. Recent studies suggest a bimodal
HPV prevalence for women in 2 age groups: 19 to 26 and 40 to 70. HPV and cervical cancer knowledge has
yet to be investigated in the older population of women.
Objective:
The objective of this study was to evaluate and compare the HPV and cervical cancer
knowledge, health beliefs, and preventive practices in women in these 2 age groups.
Methods:
This study used a cross-sectional, descriptive design. A convenience sample of 300 women in
2 age groups was recruited from 3 ambulatory obstetrics and gynecology practices in Philadelphia, Pa.
Participants completed the Awareness of HPV and Cervical Cancer Questionnaire to determine their HPV
and cervical cancer knowledge, health beliefs, and preventive practices.
Results:
A total of 280 responses (131 for the age group 19 –26 years and 149 for the age group 40 –70
years) were received. Significant differences were found between the 2 groups in knowledge (P
⫽ 0.010)
only, but not health beliefs (perceived susceptibility [P
⫽ 0.111] and perceived seriousness [P ⫽ 0.266]).
Significant differences in select preventive practices were also noted between these 2 groups. These
included Pap smear (P
⫽ 0.05), use of condoms (P ⫽ 0.002), and use of oral contraception (P ⬍ 0.001).
Conclusions:
There is a remarkable need for age-appropriate HPV and cervical cancer awareness and
education for women older than the age of 40. Women’s health care providers are perfectly positioned to
act as a catalyst to improve HPV and cervical cancer knowledge, health beliefs, and preventive practice to
ensure optimal health promotion for all women. (Gend Med. 2012;9:S55–S66) © 2012 Elsevier HS Journals,
Inc. All rights reserved.
Key words:
cervical cancer, health knowledge, human papillomavirus.
Accepted for publication November 1, 2011.
doi:10.1016/j.genm.2011.11.002
© 2012 Elsevier HS Journals, Inc. All rights reserved.
1550-8579/$ - see front matter
G
ENDER
M
EDICINE
/V
OL
. 9, N
O
. 1S, 2012
S55
INTRODUCTION
Approximately 20 million Americans are currently
infected with one or more low-risk (types 6 and 11)
and/or high-risk (types 16 and 18) human papillo-
maviruses (HPVs).
Although new prevention vac-
cines are available,
⬎6 million will become newly
infected each year.
Spread mostly through skin-
to-skin contact during any type sexual contact,
HPV is the etiologic agent of genital warts and can
be isolated in 99.7% of cervical cancer cases.
Although HPV is implicated in cancers affecting
other organ sites, including vulval, oral, and anal
cancers, the study presented here focused on cer-
vical cancer risk. HPV-related cancer is the second
leading cause of cancer deaths in women world-
wide, including
⬎4200 deaths in the United States
in 2010.
Therefore, it is evident that HPV-related
cervical cancer affects millions of women and is
responsible for significant morbidity and mortality
worldwide. Cervical cancer alone contributes to
⬃300,000 lives lost annually.
Although previous studies demonstrated a de-
crease in HPV prevalence as women age, research
instead suggests that a bimodal HPV prevalence
distribution is present showing a first peak around
the age of 20 years and a second peak around the
age 40 to 50 years.
Fluctuations in relationship
infrastructure in which there are increases in di-
vorce rates and infidelity disclosures and accep-
tance of nontraditional sexual relationships place
women at age 40 and older to be at a higher risk for
sexually transmitted infection exposures. A pleth-
ora of studies demonstrated limited HPV knowl-
edge and health beliefs in both the adolescent and
college-age populations.
Multilevel educa-
tional interventions have targeted preteens, teen-
agers, and college students regarding HPV and its
relation to cancer. Women aged 40 and older are
often overlooked, despite the facts that 80% of
women will be infected with HPV by the age of 50
and 35% of cervical cancer deaths occur in women
older than the age of 65. Other HPV-related can-
cers also disproportionately affect older women.
The incidence of vulval cancer increases from 1.1
per 100,000 in women aged 25 to 39 to 3.8 in
those of ages 60 to 64. Women older than the age
of 40 may not believe themselves at risk and,
therefore, may not practice preventive measures
that can potentially save their lives. In addition,
although HPV also affects women older than the
age of 40, there are few HPV educational or pre-
vention campaigns targeting middle-age and older
adult female populations.
The purpose of this study was to determine the
differences in knowledge, health beliefs (suscepti-
bility and seriousness), and preventive practices
related to HPV and related cancers in groups of
women aged 19 to 26 and 40 to 70 years. The
research hypothesis was that women aged 40 to 70
years will have less knowledge, perceive them-
selves to be less susceptible, and report lower use of
preventive practices regarding HPV and cervical
cancer compared with women aged 19 to 26 years.
The results of this study regarding the women aged
40 and older were previously reported by Mont-
gomery et al.
Study Design
This descriptive study used a cross-sectional de-
sign to determine differences in knowledge and
health beliefs related to cervical cancer and HPV in
women aged 40 to 70 years compared with those
aged 19 to 26 years. Over a 2-month period, anon-
ymous data were collected using a self-adminis-
tered pen-and paper questionnaire.
Setting and Sample
A convenience sample of 131 women aged 19 to
26 and 149 women aged 40 to 70 years was re-
cruited from the waiting rooms of 3 ambulatory
obstetrics and gynecology offices of a large metro-
politan university hospital in Philadelphia, Pa. All
3 offices were used in an attempt to get a racially
heterogeneous sample in this urban area that has
rate of cervical cancer 1.7 times higher than the
national rate.
The inclusion criteria were women
aged 19 to 26 or 40 to 70 years presenting to their
health care provider for an annual well woman
visit and who did not have a history of HPV or
cervical cancer.
The application G*Power (Version 3.0.10, Uni-
versity of Dusseldorf, Dusseldorf, Germany) was
used to guide the power analysis for this study. The
power analysis was based on an independent sam-
Gender Medicine
S56

ple t test in which the 2 groups (women aged
19 –26 years and 40 –70 years) were to be compared
at 1 time point for the primary dependent variable:
knowledge. Small to medium effect size (0.36) was
postulated in keeping with Cohen’s recommenda-
tion for differences between cells means (Cohen’s
d).
Power was set at 0.80, meaning that there
would be an 80% probability of reaching statistical
significance if there is difference between the
groups.
In this study, for a significance level of
␣ ⫽ 0.05,
with an effect size of 0.36, to achieve a power of
0.80, a total sample size of 250 subjects with 125
subjects in each group was required. To ensure
adequate power and allow for any attrition due to
missing data, an additional 50 subjects were re-
cruited. Of the 300 women who received the study
packets, 280 respondents were eligible for analysis
and returned the completed questionnaires in
sealed envelopes; 20 questionnaires were incom-
plete and were not used in these analyses. Partici-
pants were classified into 2 groups based on their
age. The first group (group A) comprised of women
between 19 and 26 years of age (n
⫽ 131). The
second group (group B) included women between
the ages of 40 and 70 years (n
⫽ 149).
Procedure
After approval by the university’s institutional
review board, the study commenced by training a
research assistant (RA; receptionist) at each of the
3 offices. The training entailed using data on the
practice management program to identify poten-
tial eligible participants when women are checked
in for their visits, inviting potential participants,
and keeping all data anonymous by sealing all
envelopes and placing them in the research bin in
a secured drawer in the specific office. At each of
the 3 sites, there were flyers posted on the walls
and a trained RA invited participants if they met
eligibility. If the patient met 2 of the requirements
(age and the reason for the visit [well-women
check up]), she was given an additional informa-
tional sheet to read to further determine eligibility
(exclusion criteria if she had a history of HPV or
cervical cancer). After she read the sheet, the RA
asked if she was eligible. If the patient said yes, she
was given the survey packet with a cover letter that
accompanied the packet. The cover letter con-
tained a brief description of the research project,
assurance of anonymity, the voluntary nature of
participation, and institutional review board con-
tact information. Completion of the survey acted
as consent for participation. Once the survey was
completed, it was placed in a sealed envelope to be
returned to the researcher. Complete anonymity
was maintained, and no identity was disclosed.
Main Research Variables
Sociodemographic variables collected in this
study included age, race, education, health insur-
ance status, religious affiliation, marital status, and
income level.
HPV and Cervical Cancer Knowledge, Health
Beliefs, and Preventive Practices
The Awareness of HPV and Cervical Cancer
Questionnaire was used to measure knowledge,
health beliefs and perceptions, and preventive
practices related to HPV and cervical cancer.
This
self-administered, 36-item questionnaire was de-
veloped by Ingledue et al
based on the Health
Beliefs Model (HBM)
to investigate HPV/cervical
cancer knowledge, health beliefs and perception,
and preventive measures in college-age women.
This tool was selected because it was specifically
designed to measure HPV and cervical cancer
awareness, but also because it was based on the
HBM, the conceptual framework that guided this
study. Before selection, the questionnaire was re-
viewed by a panel of experts consisting of obste-
tricians/gynecologists, physicians, and nurse prac-
titioners from the university who concluded that
the questions were generalizable to women of all
age groups. Despite its original intent of targeting
college-age women, subsequent studies have used
this questionnaire in women of various age
groups, thereby validating its generalizability for
age.
The questionnaire is divided into 3 sections. The
first section consists of 15 multiple-choice questions
intended to measure knowledge of HPV and cervical
cancer. One point is awarded for each correct re-
sponse. Scores can be between 0 and 15, with higher
K. Montgomery and M. Smith-Glasgow
S57
scores indicative of higher level of HPV and cervical
cancer knowledge. The second section is intended to
measure the perceived threat portion of cervical can-
cer and consists of 15 questions, each with possible
responses using a 5-point Likert-type scale ranging
from 1 (strongly agree) to 5 (strongly disagree). Nine
of the 15 questions relate to perceived susceptibility
and have a possible subtotal score range of 9 to 45.
The remaining 6 questions relate to perceived seri-
ousness and have a potential score that ranges from
6 to 30. Higher scores denote that perceived suscep-
tibility and seriousness about HPV and cervical can-
cer are high. The final section of the questionnaire
consists of 6 questions that focus on individual sex-
ual behaviors, risk factors, and history of Pap smears.
These multiple-choice questions represent a measure
of preventive practices related to HPV and cervical
cancer.
Ingledue et al
used consensual validity via a
panel of experts who represented several health
professionals including 2 gynecologists, 2 profes-
sors of health education, and a medical profes-
sional from the Breast and Cervical Cancer
program to support content validity of the in-
strument. The authors also conducted a test-retest
reliability procedure over a 10-day period to estab-
lish the stability of the instrument over time. High
test-retest reliability was reported for knowledge (r
⫽ 0.90), perceptions and beliefs (r ⫽ 0.95), and
preventive behaviors (r
⫽ 0.90). Internal consis-
tency reliability was not reported in the study by
Ingledue et al.
For the current study, the internal
consistency reliability was adequate (Cronbach’s
␣
⫽ 0.77) for the knowledge subscale and the sus-
ceptibility subscale (
␣ ⫽ 0.66) but unacceptably
low for the seriousness subscale (
␣ ⫽ 0.20). The
low reliability for the seriousness subscale makes
any conclusion based on this subscale tentative at
best. Quantitative data were coded and entered
into the SPSS-PC program, version 16.0 (SPSS Inc.,
Chicago, Illinois) and stored on a secured com-
puter used for research purposes only.
Data Analysis
All data were collected strictly anonymously
with no identifying information or codes associ-
ated with them. Frequency distributions and mea-
sures of central tendency and variability were cal-
culated for sociodemographic and dependent
study variables. All values with missing data were
tracked and excluded from analysis. Chi-square
tests were performed to verify differences in
sociodemographic characteristics between the
groups.
To examine differences in knowledge and health
beliefs (susceptibility and seriousness) between the
younger and older groups of women, indepen-
dent-sample t tests were performed. However, ac-
cording to the HBM, knowledge, susceptibility,
and seriousness can have confounding effects on
each other and should be controlled for appropri-
ately. Therefore, to adjust for any differences in
sociodemographic characteristics as well as con-
founding effects of subdimensions of health be-
liefs (eg, knowledge and seriousness when compar-
ing susceptibility), additional ANCOVAs were
performed with the potential confounders acting
as covariates. Before analysis, the dependent vari-
ables were tested to meet the assumptions of
ANCOVA. Chi-square analyses were used to exam-
ine any differences in distribution of responses
between the groups of women for preventive prac-
tices. The Fisher exact test was used if the assump-
tions of the
2
test were not met. The level of
significance for all the tests was set at
␣ ⫽ 0.05.
RESULTS
Sociodemographic Characteristics
Sociodemographics of all the participants in this
study are detailed in
. The respondents
identified themselves as mostly white (55.4%) and
African
American
(29.6%),
college
graduates
(42.9%), Catholic (38.6%) or Christian (31.80%),
mostly single (42.9%) or married (34.3%), with an
annual income of $41,000 to $60,000 (27.4%) and
private health insurance (80%). The
2
test com-
paring the sociodemographic characteristics be-
tween the 2 groups revealed that the groups were
similar for the sociodemographic characteristics of
education (P
⫽ 0.24), type of insurance (P ⫽ 0.08),
and race (P
⫽ 0.06) but significantly different for
marital status (P
⬍ 0.001), religion (P ⫽ 0.02), and
income level (P
⬍ 0.001).
Gender Medicine
S58
As seen in
, more women in the older
group reported being married (50.30%) compared
with the younger group (16%), whereas more single
women were present in the younger group (68.7%)
than in the older group (20.10%). The number of
women reporting that their religion was Catholic
was significantly higher in the older group (43.6%)
compared with the younger group (32.8%), along
Table I. Sociodemographic characteristics of study participants (N
⫽ 280).
Characteristic
Total Sample
(N
⫽ 280),
100%
Group A
(Age 19-26 y, n
⫽ 131),
47%
Group B
(Age 40–70 y, n
⫽ 149),
53%
P
Age, y, mean (SD)
37.93 (14.96)
23.22 (2.3)
50.86 (7.60)
⬍0.001
Sexual partners, mean (SD)
2.62 (3.05)
3.91 (3.8)
1.45 (1.37)
⬍0.001
Race/ethnicity, n (%)
0.062
White/non-Hispanic
155 (55.40)
63 (48.10)
92 (61.70)
African American/non-Hispanic
83 (29.60)
46 (35.10)
37 (24.80)
Asian/Hawaiian/Pacific Islander
14 (5)
8 (6.10)
6 (4)
Hispanic/Latino
22 (7.90)
13 (9.90)
9 (6)
Other
6 (2.10)
1 (0.80)
5 (3.40)
Missing
0
0
0
Education
0.236
High school graduate
60 (21.40)
22 (16.80)
38 (25.50)
Some college courses
94 (33.60)
51 (38.90)
43 (28.80)
College graduate
120 (42.90)
56 (42.70)
64 (43)
Other
5 (1.80)
2 (1.50)
3 (2)
Missing
1 (0.30)
0
1 (0.70)
Marital status
⬍0.001
Single
120 (42.90)
90 (68.70)
30 (20.10)
Married
96 (34.30)
21 (16)
75 (50.30)
Widowed
7 (2.50)
0 (0)
7 (4.70)
Divorced
25 (9.00)
1 (0.80)
24 (16.10)
Living with significant other
31 (11.00)
19 (14.50)
12 (8.10)
Missing
1 (0.30)
0
1 (0.70)
Religion
0.022
Christian
89 (31.80)
48 (36.70)
41 (27.50)
Catholic
108 (38.60)
43 (32.75)
65 (43.60)
Jewish
23 (8.20)
5 (3.80)
18 (12.10)
Muslim
4 (1.40)
2 (1.50)
2 (1.30)
Other
54 (19.40)
32 (24.50)
22 (14.80)
Missing
2 (0.60)
1 (0.75)
1 (0.70)
Income level, $
⬍0.001
0–20K
26 (9.30)
16 (12.30)
10 (7.00)
21–40K
68 (24.30)
48 (36.60)
20 (13.40)
41–60K
77 (27.40)
40 (30.50)
37 (24.80)
61–80K
38 (13.40)
12 (9.20)
24 (16.20)
ⱖ80K
56 (20.00)
9 (6.80)
47 (31.60)
Missing
16 (5.60)
6 (4.60)
10 (7.00)
Health insurance
0.081
None
9 (3.20)
5 (3.80)
4 (2.70)
Private
224 (80.00)
98 (74.75)
126 (84.60)
Publicly funded
28 (10.10)
15 (11.50)
13 (8.60)
Unsure
16 (5.80)
12 (9.20)
4 (2.70)
Missing
3 (0.90)
1 (0.75)
2 (1.40)
K. Montgomery and M. Smith-Glasgow
S59
with more women in the older group identifying
their religion as Jewish (12.1% compared with 3.8%).
In contrast, there was a significantly higher percent-
age of women reporting their religion as Christian in
the younger group (36.7%) compared with the older
group (27.5%). Income levels were also significantly
higher in the older group, with 31.6% of the women
reporting a total annual household income of
ⱖ$80,000. In contrast, most respondents in the
younger group reported their annual income level to
be either between $21,000 and $40,000 (36.60%) or
$41,000 and $60,000 (30.5%). Health insurance sta-
tus was similar in the 2 groups, with the majority of
the participant’s reportedly carrying private insur-
ance. It should be noted that although race was not
significantly different (P
⫽ 0.06) between the 2
groups, the older group had more white participants
(61.7%) compared with the younger group (48.1%).
Knowledge and Health Beliefs
Results from the independent t test showed that
the groups were significantly different for knowl-
edge, t (277.55)
⫽ 3.00 (P ⫽ 0.003), and suscepti-
bility, t (227.33)
⫽ 4.21 (P ⬍ 0.001).
presents the comparison of frequency of correct
responses for the knowledge section of the ques-
tionnaire between the 2 groups, Also, as evident
from the sociodemographic differences presented
in
, the 2 groups were significantly differ-
ent in marital status, type of religion, and level of
income. These characteristics along with the re-
maining subdimensions of the HBM model acted
as covariates in the final ANCOVAs.
presents both unadjusted and ad-
justed means and variance (SD) for knowledge,
susceptibility, and seriousness for the 2 groups.
Before analysis, the data were checked and met the
following assumptions: (1) independence of obser-
vation; (2) normal distribution of the dependent
variables knowledge, susceptibility, and serious-
ness; (3) homogeneity of variance; and (D) linear
relationship between the covariates and the de-
pendent variables. Results indicate that after con-
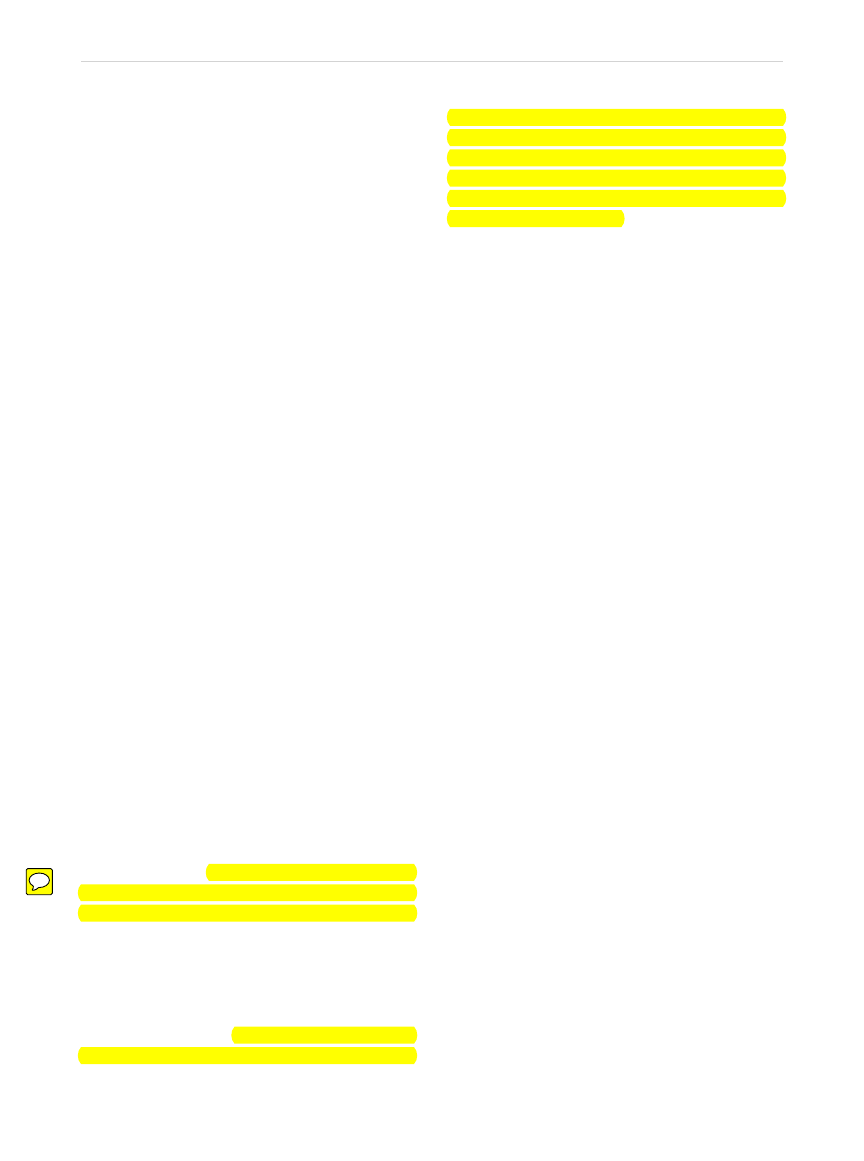
Table II. Comparison of frequencies of correct responses for multiple-choice questions regarding HPV/cervical cancer
knowledge in women aged 18 to 26 years (n
⫽ 131) and 40 to 70 years (n ⫽ 149).
Frequency (%)
Group A (18–26 y), n
⫽ 131
Group B (40–70 y), n
⫽ 149
1. The virus associated with cervical cancer
is transmitted by
102 (77.9)
66 (44.3)
2. Cervical cancer and precancerous cells
are associated with the presence of
105 (80.2)
402 (26.8)
3. Cervical cancer can be diagnosed by
107 (81.7)
32 (21.5)
4. Prevention of cervical cancer may require
84 (64.1)
84 (56.6)
5. HPV can cause
74 (56.5)
98 (65.8)
6. HPV can live in the skin without causing
growths or changes
88 (67.7)
82 (55.8)
Risk factors (yes or no)
7. Multiple sex partners
104 (79.4)
100 (67.1)
8. Having genital warts
77 (58.8)
76 (51.7)
9. Sexual intercourse before 18
65 (49.6)
75 (50.3)
10. Taking illegal drugs
20 (15.3)
27 (18.1)
11. Having contracted any STIs
98 (76)
85 (57.8)
12. Smoking cigarettes
31 (23.7)
33 (22.3)
13. Poor diet or nutrition
69 (53.1)
79 (53.4)
14. Using tampons
86 (65.6)
101 (67.8)
15. Use of oral contraceptives (birth
control pills)
13 (10.2)
13 (8.8)
HPV
⫽ human papillomavirus; STIs ⫽ sexually transmitted infections.
Gender Medicine
S60
trolling for all the sociodemographic characteris-
tics and pertinent subdimensions of the HBM,
there was a significant difference between the
groups for knowledge only (F
1,265
⫽ 6.80, P ⫽
0.01), but not for susceptibility (F
1,265
⫽ 2.55, P ⫽
0.11). As evident in
, the differences in
adjusted means for knowledge are similar after
controlling for sociodemographic characteristics
and subdimensions, whereas that of susceptibility
and seriousness are lower.
It should be noted that the younger group of
women have a higher level of knowledge and
health belief scores compared with the older
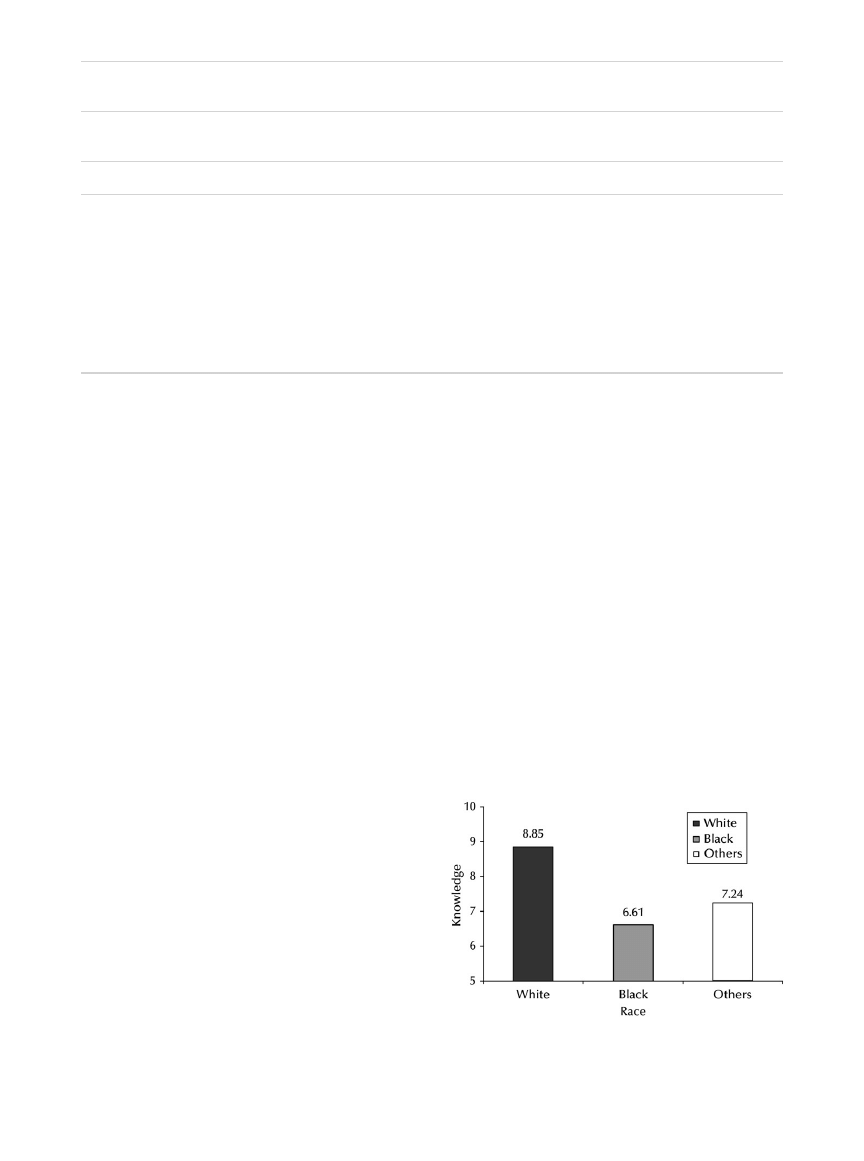
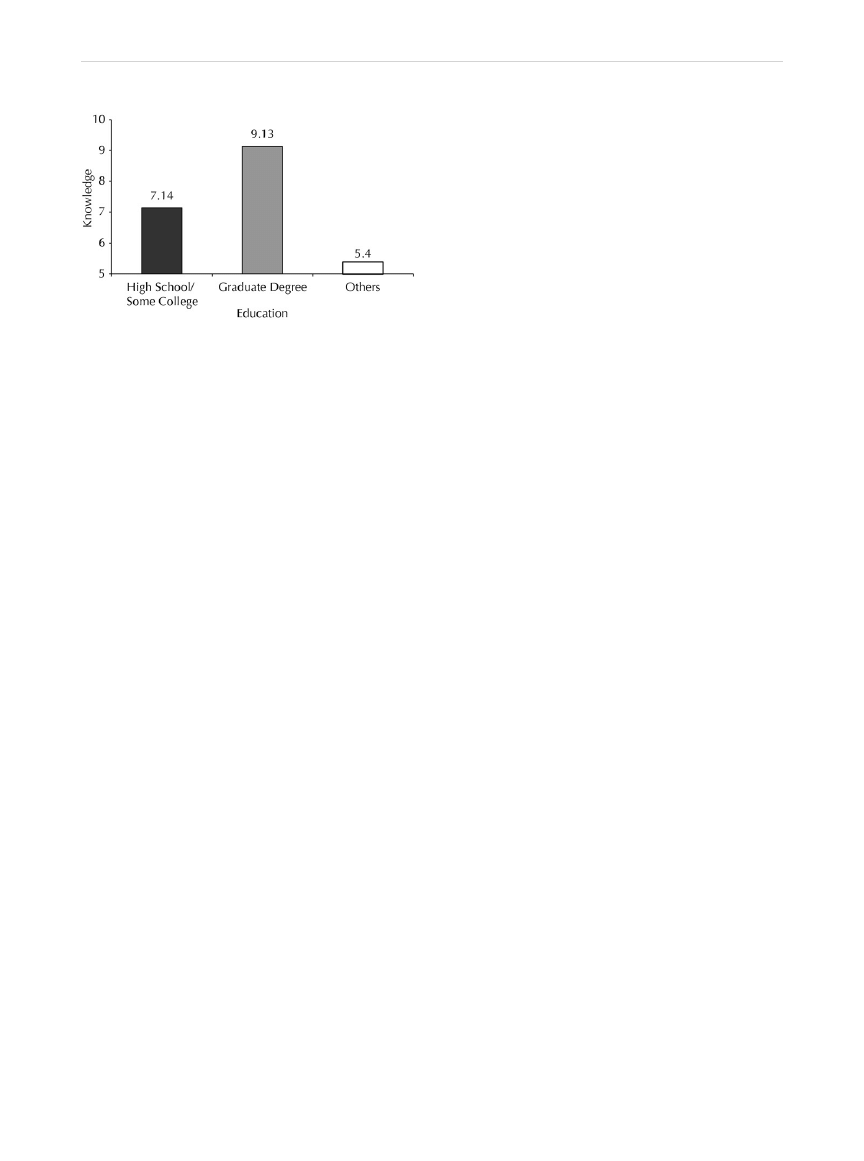
group. Moreover, the ANCOVA revealed that the
sociodemographic covariates race and education
led to significant difference in knowledge. Based
on this finding, knowledge levels for different race
and education levels were plotted in separate
graphs (
and
Preventive Practices
Results of the analysis revealed significant differ-
ences between the groups for use of condoms (P
⬍
0.002), oral contraceptives (P
⬍ 0.001), Pap smear
(P
⬍ 0.048), and family member diagnosed with
HPV (P
⬍ 0.05), but not for cigarette smoking (P ⫽
1.00) and sexual involvement (P
⫽ 0.164) (
). Although 34.7% of the women in the younger
group reported using condoms regularly (usually
and always), only 18.4% of the women in the older
group reported doing so. The use of condoms was
low in the older age group, with 59.2% of the
women never using a condom during sexual activity,
compared with only 34.6% in the younger age
group. Almost half the women in the younger group
(43.8%) reported using oral contraceptives. In con-
trast, more women in the older age group (86.3%)
did not use oral contraceptives at the time of partic-
ipation. In response to the question of whether the
women knew anyone in the family with a history of
HPV/cervical cancer, a higher percentage (72.5%) of
women in the older age group reported not knowing
one compared with the younger age group (58.8%).
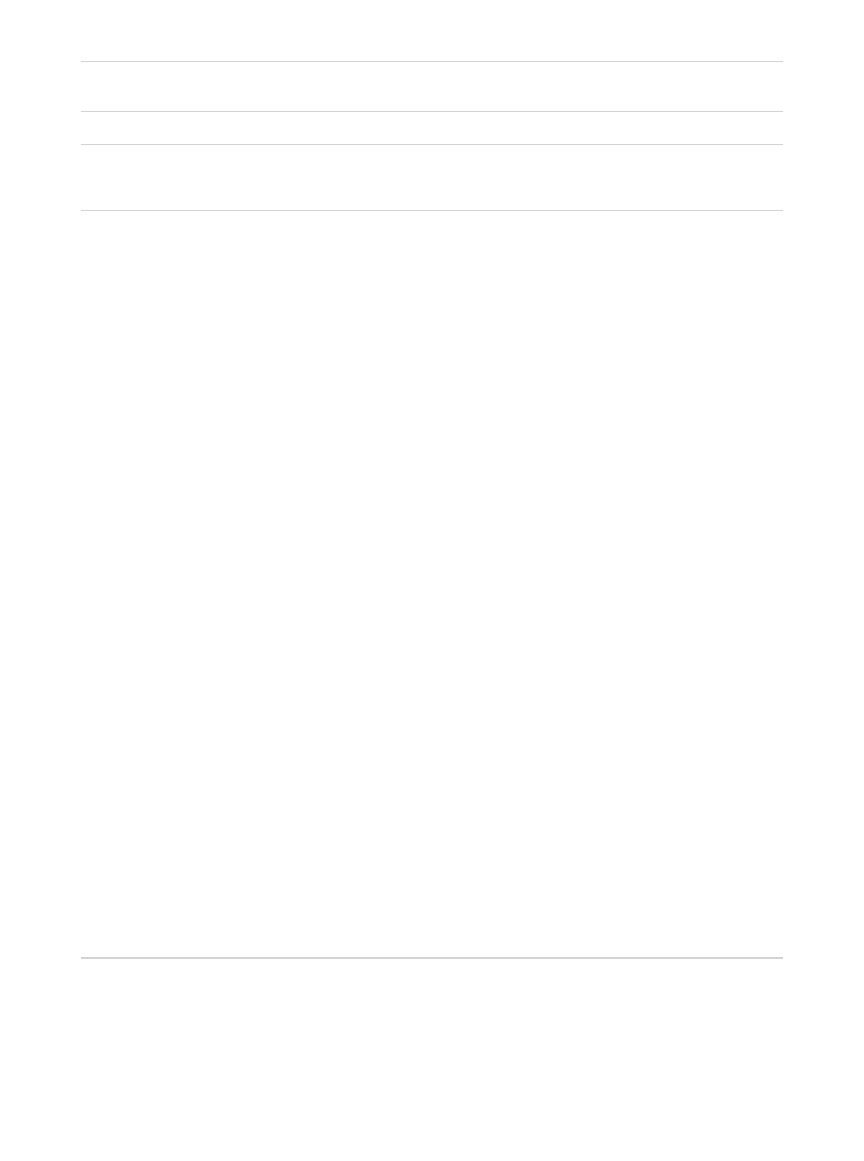
Table III. Adjusted and unadjusted mean (SD) for knowledge, susceptibility, and seriousness for younger and older groups
of women using sociodemographic factors as a covariate.
n
Unadjusted, Mean (SD)
P
Adjusted,* Mean (SD)
P
Knowledge
0.003
†
0.010
†
Group A (19–26 y)
129
8.57 (3.14)
8.57 (3.41)
Group B (40–70 y)
146
7.44 (3.41)
7.43 (3.38)
Susceptibility
⬍0.001
†
0.111
Group A (19–26 y)
129
29.09 (6.53)
28.12 (4.63)
Group B (40–70 y)
146
26.03 (4.63)
26.88 (5.88)
Seriousness
0.097
0.266
Group A (19–26 y)
129
20.26 (2.76)
20.19 (3.02)
Group B (40–70 y)
146
19.69 (2.78)
19.76 (2.98)
*
Adjusted means are based on ANCOVA analyses with the following covariates: race, education, marital status, religion, income, and
subdimensions.
†
P
⬍ 0.05; the P values for the unadjusted means are calculated for the t test and the P values for the adjusted means are calculated for
the ANCOVA.
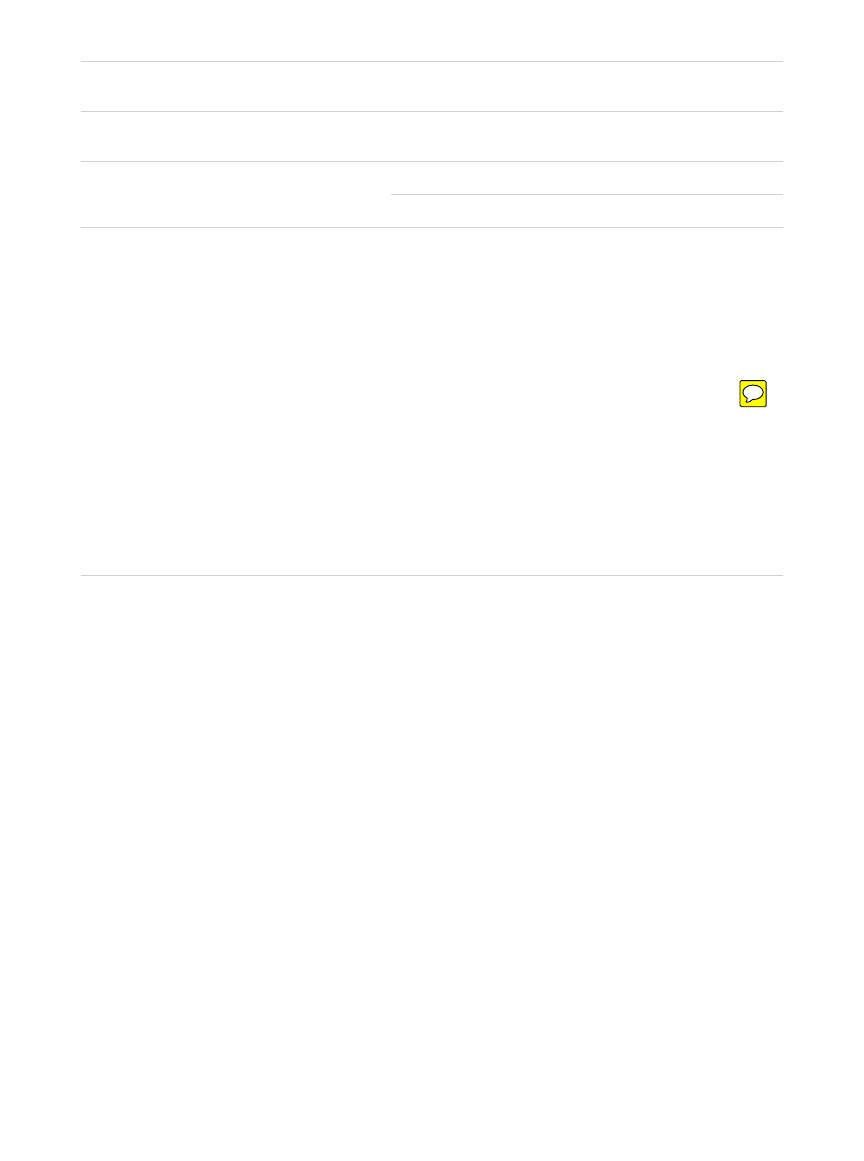
Figure 1. Means of knowledge by race for the study par-
ticipants (N
⫽ 280).
K. Montgomery and M. Smith-Glasgow
S61
DISCUSSION
This study aimed to determine the differences in
knowledge, health beliefs and perceptions, and
type of preventive practices in women aged 40 to
70 years compared with younger counterparts
aged 19 to 26 years who have typically been the
target of most national HPV public awareness and
prevention programs.
The results of this study partially support the
hypothesis that women aged 40 to 70 have less
knowledge regarding HPV and cervical cancer
knowledge, perceive themselves as less susceptible
to its acquisition, and may perceive HPV and cer-
vical cancer to be less serious than other diseases
compared with women aged 19 to 26. Although
this study demonstrated that the older age group
has less knowledge than the younger group, there
were no differences in susceptibility or seriousness
between the 2 groups.
Knowledge
Although the existence of HPV has been recog-
nized as a sexually transmitted infection for more
than half a century, discovery of HPV as a poten-
tial cause for cervical cancer that affects women
shortly after beginning their first sexual relation-
ship did not emerge until the 1970s.
The delin-
eation between the low-risk and high-risk types of
HPV was a breakthrough scientific development
⬍10 years ago.
Since then, younger women
have been the target of public health education
and prevention as well as vaccination campaigns;
therefore, it is not surprising that this study indi-
cates that older women have comparatively less
knowledge about HPV and cervical cancer than
the younger participants.
Compared with other studies, the findings of
this study regarding cervical cancer and HPV
knowledge in women aged 19 to 26 are not con-
sistent with previous findings in this population
using the same questionnaire.
The average
knowledge score reported in the study conducted
by Ingledue et al
using 428 college women was
6.8 out of 15, whereas the study by Denny-Smith
et al
reported an average score of 10.2 in women
of similar age. The study by Ingledue et al
did not
provide sufficient sociodemographic information
about their participants, whereas the study by
Denny-Smith et al
used 240 undergraduate nurs-
ing students with superior knowledge about med-
ical conditions compared with age-matched gen-
eral population. The findings from either study are
difficult to compare with these results. It should be
noted that the study by Ingledue et al
was per-
formed before the massive public educational
campaigns by the Centers for Disease Control and
Prevention and pharmaceutical companies to in-
crease awareness in the young adult population.
Finally, as suggested from
and
, knowl-
edge scores vary according to individual’s race and
education. White women appear to have higher
levels of knowledge compared with African Amer-
ican women and other minorities. Furthermore,
college graduates have greater knowledge compared
with high school graduates. It is possible that older
women whose ethnicity or educational attainment
place them in higher risk categories based on knowl-
edge of HPV and cervical cancer should be the prime
target of educational interventions involving HPV
and cervical cancer awareness.
Health Beliefs (Perceived Susceptibility and
Perceived Seriousness)
Contrary to the research hypothesis, this study
found no significant differences in perceived sus-
ceptibility to HPV and cervical cancer or in per-
ceived seriousness, after controlling for knowledge
and sociodemographic characteristics. Before con-
trolling for knowledge, the younger group of
women had a significantly higher level of per-
Figure 2. Means of knowledge for educational level of
study participants (N
⫽ 280).
Gender Medicine
S62

ceived risk than women in the older group. The
differences in knowledge may therefore be an im-
portant mediator between the 2 groups and their
perceived risk. However, the low internal consis-
tency in these measures renders any findings based
on these scales inconclusive.
Preventive Practices
The hypothesis that women aged 40 to 70 would
use preventive practices less than women aged 19
to 26 was only partially supported. As previously
described, women polled in the older age group
reported fewer sexual partners within the past 5
years and less condom use. Therefore, most sexu-
ally active women in this age group are in long-
term relationships and do not perceive themselves
at risk for a sexually transmitted disease, nor do
they appreciate the connection between HPV and
cervical cancer. Younger women, however, use
condoms more, are sexually intimate with more
sexual partners, and report a higher incidence of
oral contraceptive use than women in the older
Table IV. Comparison of frequency and percentage of participant responses to preventive practices in women aged 19 to
26 years and 40 to 70 years.
Preventive Practices
Total Sample
(N
⫽ 280),
100%
Group A
(Age 19–26 y, n
⫽ 131),
47%
Group B
(Age 40–70 y, n
⫽ 149),
53%
P*
Sexual experience, n (%)
0.16
Currently involved
71.43
76.34
67.11
Not currently involved
26.43
21.37
30.87
Never had sexual intercourse
1.79
2.29
1.34
Missing
0.36
0.00
0.67
Use of condoms, n (%)
Always
10.36
13.74
7.38
Usually
15.00
19.85
10.74
Sometimes
10.36
10.69
10.07
Occasionally
4.64
4.58
4.70
Rarely
10.71
14.50
7.38
Never
46.79
33.59
58.39
Missing
2.14
3.05
1.34
Use of oral contraceptives, n (%)
⬍0.001
Yes
76 (27.14)
57 (43.51)
19 (12.75)
No
199 (71.07)
73 (55.73)
126 (84.56)
Don’t know
1 (0.36)
0.00
1(0.67)
Missing
4 (1.40)
1 (0.80)
3 (2.00)
Cigarette smoking, n (%)
1.00
Yes
57 (20.36)
27 (20.61)
30 (20.13)
No
222 (79.29)
104 (79.39)
118 (79.19)
Missing
1 (0.36)
0.00
1 (0.67)
Pap smear, n (%)
0.05
Never
8 (2.86)
6 (4.58)
2 (1.34)
Within the past year
194 (69.29)
97 (74.05)
97 (65.10)
Had one but not within past year
75 (26.79)
28 (21.37)
47 (31.54)
Missing
3 (1.07)
0.00
3 (2.01)
Family member diagnosed with HPV, n (%)
0.05
Yes
50 (17.86)
28 (21.37)
22 (14.77)
No
185 (66.07)
77 (58.78)
108 (72.48)
Don’t Know
39 (13.93)
23 (17.56)
16 (10.74)
Missing
6 (2.14)
3 (2.29)
3 (2.01)
*
Significance P
ⱕ 0.05.
K. Montgomery and M. Smith-Glasgow
S63
group. The qualitative study (by Vanslyke et al
of 54 women age 18 to 60 found that women
identify 3 cervical cancer preventive measures:
having regular annual examinations by a health
care provider, having a Pap smear, and having an
awareness of changes in one’s own body.
Significance to Practice
As a caring profession, nursing is dedicated to the
health and wellness of all populations and is per-
fectly positioned to act as a catalyst to improve
knowledge, health beliefs, and preventive practice to
ensure optimal health promotion for all women.
This study challenges clinical nurse practitioners to
reinforce the primary goals of Healthy People 2020
to help individuals of all ages increase life expec-
tancy and improve their quality of life, as well as
reduce the number of new cancer cases and the ill-
ness, disability, and death caused by cancer. Gaps
found throughout existing literature in women’s un-
derstanding of HPV, a potentially deadly virus, sug-
gests the need for more comprehensive education
about preventing genital HPV, its possible sequelae,
and the significance of Pap and HPV screening for
cancer detection and prevention in women of all
ages. Knowledge related to HPV, its relationship to
cervical cancer, and cervical cancer itself is low in
younger and older women. Despite national cam-
paigns to educate young women, knowledge contin-
ues to be low. Therefore, practitioners need to em-
power women with comprehensive knowledge
regarding HPV, with a focus tailored to the appropri-
ate needs of their age population. Through collabor-
ative efforts, it is paramount that the nursing com-
munity fully addresses the deficiencies in HPV/
cervical cancer knowledge, perceived risk, and
preventive practices across the life span of both
women and men. In addition, information gained
through intervention research fosters the develop-
ment of multidisciplinary and multifaceted national
education campaigns designed to educate popula-
tions of all sociodemographic backgrounds. Last,
joining forces with political action campaigns to
reach out to minorities who are at the most increased
risk for cervical cancer will result in the preservation
of human life and the promotion of healthy behav-
ior changes.
Limitations
The findings of this study should be interpreted
in light of the several existing limitations. First, the
participants of this study were mostly residents
from an urban area; consequently, the findings
may not be generalized to other populations.
Second, this study relied on self-report with no
attempt to independently verify respondents’ in-
formation. In addition, although this study used
an anonymous questionnaire, limitations of a sur-
vey study may apply. Surveys provide only real-
time descriptions of behaviors and feelings of the
respondents, and responses cannot always be
taken as accurate descriptions of what the respon-
dents actually do or feel. This is especially true for
behavior that is contrary to generally accepted
norms of society, such as information regarding
sexual activity.
Some of these women may have
been unwilling to indicate that they have engaged
in controversial behaviors, thus skewing the re-
sults (social desirability bias).
Scientific advances continue to provide clini-
cians with updated information regarding HPV
and cervical cancer. The Awareness of HPV and
Cervical Cancer Questionnaire developed
⬎5 years
ago may not represent this current scientific infor-
mation.
Revision of this tool to reflect scientific
development and cultural beliefs is crucial to gain
a better understanding of knowledge, health be-
liefs, and preventive practices in all women.
Implications for Future Research
The findings of this study provides the basis for
understanding HPV and cervical cancer knowledge,
health beliefs, and preventive practices of women of
2 high-risk age groups (19 –26 and 40 –70 years).
However, this study did not investigate age on a
continuum throughout a woman’s life span. Conse-
quently, the findings are unable to reflect the range
of ages when knowledge decreases. The next logical
step is to investigate the age threshold at which
knowledge decreases. Furthermore, the tool of this
study needs to be refined to reflect current practice
patterns and levels of HPV and cervical cancer
knowledge. Most importantly, a thorough investiga-
tion of the impact of the differences in women’s
knowledge on their health beliefs and preventive
Gender Medicine
S64

practices in populations with a high prevalence and
risk of cervical cancer is essential to combat this dis-
ease. Finally, identifying deficiencies in the current
education campaigns and redesigning culturally sen-
sitive, age-appropriate educational awareness, and
health promotion will better equip women to win
the fight against cervical cancer.
Another vital area of research involves investi-
gating current practice patterns regarding HPV and
cervical cancer knowledge of health care providers.
New evidence regarding HPV and cervical cancer is
emerging at an explosive pace, and it is challeng-
ing for health care providers to stay current with
the copious amount of information. Determining
the level of HPV and cervical cancer knowledge of
caregivers will help researchers to identify whether
patients
have
access
to
the
appropriate
information.
CONCLUSIONS
Women aged 40 to 70 have decreased HPV and cer-
vical cancer knowledge compared with women aged
19 to 26 who have been the target of substantial
national educational campaigns. Unlike the younger
group of women, women aged 40 to 70 did not have
comprehensive sex education during their formative
years. Therefore, they did not have the opportunity
to make a connection between their sexual activity
and their risk of cervical cancer. This initial defi-
ciency is further complicated by the intentional ex-
clusion of women aged 40 and older from the na-
tional education campaigns. In addition, this study
suggests that the group that has the greatest risk of
cervical cancer (African American women aged
40 –50 with low education levels) is the same group
that health care providers have failed to educate the
most. African American women are 50% more likely
to be diagnosed with cervical cancer and are twice as
likely to die of the disease compared with white
women in the United States.
Until further re-
search is completed and age-appropriate educational
materials are developed, it is crucial that health care
providers increase the HPV and cervical awareness of
all women regardless of their age and perhaps enable
women to win the battle against this potentially fatal
disease.
ACKNOWLEDGMENTS
The authors thank Brian Crain for medical editing
and assistance with manuscript preparation.
Dr. Smith-Glasgow was principally responsible for
study conception and design and critical manuscript
revision. Ms. Montgomery primarily acquired and
analyzed study data, and drafted the manuscript.
CONFLICTS OF INTEREST
The symposium and publication of these proceed-
ings were supported by: The National Institutes of
Health, The Drexel University College of Medi-
cine, The Helen I. Moorehead, MD Foundation,
The Doris Willig, MD Foundation, The Institute
for Women’s Health and Leadership, and The Cen-
ter for Women’s Health Research at the Drexel
University College of Medicine.
REFERENCES
1. Centers for Disease Control and Prevention. 2009
Sexually Transmitted Disease Surveillance.
www.cdc.gov/std/stats09/exordium.htm.
Accessed
March 13, 2011.
2. Dunne EF, Unger ER, Sternberg M, et al. Preva-
lence of HPV infection among females in the
United States. JAMA. 2007;297:813– 819.
3. Parkin D. The global health burden of infection-
associated cancers in the year 2002. Int J Cancer.
2006;118:3030 –3044.
4. Muñoz N, Fransechi S, Bosetti C, et al. Role of
parity and human papillomavirus in cervical can-
cer: the IARC multicentric case-control study. Lan-
cet. 2002;359:1093–1101.
5. World Health Organization. Immunization, Vac-
cines and Biologicals. Human papillomavirus
(HPV).
http://www.who.int/immunization/topics/
Accessed March 13, 2011.
6. National Cancer Institute. A Snapshot of Cervical
Cancer.
http://www.cancer.gov/aboutnci/serving
people/snapshots/cervical.pdf.
Accessed March
13, 2011.
7. Herrero R, Hildesheim A, Bratti C, et al. A popula-
tion-based study of all grades of cervical neoplasia in
rural Costa Rica. J Natl Cancer Inst. 2000;92:6464–6473.
8. Lazcano-Ponce E, Herrero R, Muñoz N, et al. Epi-
demiology of HPV infection among Mexican
K. Montgomery and M. Smith-Glasgow
S65

women with normal cervical cytology. Int J
Cancer. 2001;91:412– 420.
9. Molano M, Posso H, Weiderpass E, et al. Preva-
lence and determinants of HPV infection among
Colombian women with normal cytology. Br J
Cancer. 2002;87:324 –333.
10. Muñoz N, Méndez F, Posso H, et al. Incidence,
duration, and determinants of cervical human
papillomavirus Infection in a cohort of Colombian
women with normal cytological results. J Infect
Dis. 2004;190:2077–2087.
11. Baer H, Allen S, Braun L. Knowledge of human
papillomavirus infection among young adult men
and women: implications for health education and
research. J Community Health 2000;25:67–78.
12. Burak LJ, Meyer M. Using the health belief model
to examine and predict college women’s cervical
cancer screening beliefs and behavior. Health
Care Women Int. 1997;18:251–262.
13. Ingledue K, Cottrell R, Bernard A. College wom-
en’s knowledge, perceptions, and preventive be-
haviors regarding HPV and cervical cancer. Am J
Health Studies. 2004;19:28 –34.
14. Vail-Smith K, White D. Risk level, knowledge, and
preventive behavior for HPV among sexually active
college women. J Am Coll Health. 1992;40:227–230.
15. Montgomery K, Rosen-Bloch J, Bhattacharya A,
Montgomery O. Human papillomavirus and cervi-
cal knowledge, health beliefs, and preventative
practices in older women. J Obstet Gynecol Neo-
natal Nurs. 2010;39:238 –249.
16. Cohen J. A power primer. Psychol Bull. 1992;112:
155–159.
17. Glanz K, Rimer BK, Lewis FM. Health Behavior and
Health Education. Theory, Research and Practice.
San Francisco, Calif: Wiley & Sons; 2002.
18. Denny-Smith T, Bairan A, Page M. A survey of
female nursing students’ knowledge, health be-
liefs, perceptions of risk, and risk behaviors
regarding human papillomavirus and cervical
cancer. J Am Acad Nurse Pract. 2006;18:62– 69.
19. Moscicki A, Hills N, Shiboski S, et al. Risks for
incident human papillomavirus infection and low-
grade squamous intraepithelial lesion develop-
ment in young females. JAMA. 2001;285:2995–3002.
20. Koutsky L, Ault K, Wheeler C, et al, Proof of Prin-
ciple Study Investigators. A controlled trial of hu-
man papillomavirus type 16 vaccine. N Engl J Med.
2002;347:1645–1651.
21. Munoz N, Bosch FX, de Sanjose S, et al. Epidemi-
ologic classification of human papillomavirus
types associated with cervical cancer. N Engl
J Med. 2003;348:518 –527.
22. Vanslyke J, Baum J, Plaza V, et al. HPV and cervical
cancer testing and prevention: knowledge, be-
liefs, and attitudes among Hispanic women. Qual
Health Res. 2008;18:584 –596.
23. US Department of Health and Human Services.
Healthy People 2020.
Accessed March 13, 2011.
24. Zia H. Asian American Dreams: The Emergence of
an American People. New York: NY: Farrar, Straus
& Giroux; 2000.
25. Centers for Disease Control and Prevention.
Quadrivalent human papillomavirus vaccine: rec-
ommendations of the Advisory Committee on Im-
munization Practices (ACIP). MMWR Morb Mortal
Wkly Rep. 2007;56:1–24.
26. American Cancer Society. Cancer Facts & Figures
2009.
http://www.cancer.org/research/cancerfacts
figures/cancerfactsfigures/cancer-facts-figures-
2009.
Accessed March 13, 2011.
27. Cates JR, Brewer NT, Fazekas K, et al. Racial differ-
ences in HPV knowledge, HPV vaccine acceptabil-
ity, and related beliefs among rural, southern
women. J Rural Health. 2009;25:93–97.
Address correspondence to:
Kymberlee Montgomery, DrNP, MSN, College of Nursing & Health Professions, 1505
Race St Ms 501, Philadelphia, PA 19102. E-mail:
kimberlee.a.montgomery@drexel.edu
Gender Medicine
S66
Document Outline
- Human Papillomavirus and Cervical Cancer Knowledge, Health Beliefs, and Preventive Practices in ...
Wyszukiwarka
Podobne podstrony:
Human Papillomavirus and Cervical Cancer Knowledge health beliefs and preventive practicies
Knowledge of cervical cancer and screening practices of nurses at a regional hospital in tanzania
Cervical Cancer Prevention and Early american cancer society
Morbidity and mortality due to cervical cancer in Poland
What do British women know about cervical cancer symptoms and the risks
Quality of life and disparities among long term cervical cancer suvarviors
Women s knowledge about cervical cancer
health behaviors and quality of life among cervical cancer s
New technologies for cervical cancer screening
Comparison of Human Language and Animal Communication
Menagement Dile in cervical cancer
Human Relations and Social Responsibility
Alternative approaches to cervical cancer screening — kopia
HUMAN RIGHTS AND THEIR IMPORTANCE goood
Papilloedema, Papillitis and Pseudopapillitis
[Mises org]Hayek,Friedrich A A Free Market Monetary System And Pretense of Knowledge(1)
Chater N , Oaksford M Human rationality and the psychology of
New technologies for cervical cancer screening
więcej podobnych podstron