Handwriting, visuomotor integration, and neurological condition at
school age
JESSIKA F VAN HOORN
1
|
CAREL GB MAATHUIS
1
|
LIEKE HJ PETERS
2
|
MIJNA HADDERS-ALGRA
2
1 Center for Rehabilitation, University Medical Center Groningen, University of Groningen, the Netherlands. 2 Department of Paediatrics, Institute of Developmental Neurology,
University Medical Center Groningen, University of Groningen, the Netherlands.
Correspondence to Dr Mijna Hadders-Algra at Department of Paediatrics, Institute of Developmental Neurology, University Medical Center Groningen, Hanzeplein 1, 9713 GZ Groningen, the Netherlands.
E-mail: m.hadders-algra@med.umcg.nl
PUBLICATION DATA
Accepted for publication 31st March 2010.
Published online 15th June 2010.
LIST OF ABBREVIATIONS
DCD
Developmental coordination
disorder
MND
Minor neurological
dysfunction
Movement ABC Movement Assessment
Battery for Children
VMI
Developmental Test of
Visual Motor Integration,
4th edition, revised
AIM
The study investigated the relationships between handwriting, visuomotor integration,
and neurological condition. We paid particular attention to the presence of minor neurological
dysfunction (MND).
METHOD
Participants were 200 children (131 males, 69 females; age range 8–13y) of whom 118
received mainstream education (mean age 10y 5mo, SD 1y 4mo) and 82 special education (mean
age 10y 8mo, SD 1y 2mo). Each child had four assessments: a neurological examination, which
paid attention to the type and severity of MND, a test to measure motor performance, a hand-
writing test, and the Developmental Test of Visual Motor Integration.
RESULTS
Dysgraphic handwriting and slow writing speed were closely related to the severity of
neurological dysfunction (both p<0.001); impaired visuomotor integration was related to the
presence of MND (p<0.001) but somewhat less to its severity. Impaired handwriting and visuomo-
tor integration were strongly related to two specific dysfunctions: fine manipulative disability and
coordination problems (both p<0.001). Impaired visuomotor integration was weakly related to
dysfunctional muscle tone regulation (p=0.009) and sensory dysfunction (p=0.042).
INTERPRETATION
Poor handwriting and impaired visuomotor integration are related to MND,
but in a differential way. Poor handwriting is related to the severity of neurological dysfunction
and to dysfunctions of complex supraspinal circuitries. Impaired visuomotor integration is associ-
ated with the presence of any of the most common types of MND.
Many children have difficulties in writing: the prevalence rates
of writing problems range from 10% to 30%.
1
Writing is an
important skill that is related to school performance and the
child’s self-esteem.
2
Deficits in handwriting performance are
also frequently encountered in children with developmental
coordination disorder (DCD).
3
Poor writing or dysgraphia
includes poor legibility and ⁄ or slow writing speed. The DSM-
IV
3
identifies dysgraphia as a ‘disorder of written expression’
as ‘writing skills that… are substantially below those expected
given the person’s… age, measured intelligence, and age-
appropriate education’. Before children can learn to write they
should have developed skills that are prerequisites for hand-
writing. These skills include understanding of directional
terms, the ability to recognize similarities and differences in
forms, a functional pencil grasp, and the ability to copy lines
and shapes. These skills require adequate performance in
visual–motor coordination, motor planning, cognitive and
perceptual skills, and accurate processing of tactile and kinaes-
thetic information.
4
The child’s neurological condition plays an important role
in the development of motor behaviour, especially in the
development of adequate complex motor skills.
5
Little is
known about the relation between neurological condition, in
particular the absence or presence of minor neurological dys-
function (MND) and writing skills. The same holds true for
the relation between neurological make-up and visual–motor
integration. Signs of MND can be determined with a stan-
dardized and age-specific assessment, such as the examination
according to Touwen.
6
Important in the interpretation of
signs of minor neurological dysfunction is the notion that a
single sign does not have clinical relevance. Signs only have
significance when they co-occur in functional domains. Basi-
cally, two forms of MND can be distinguished: simple and
complex MND.
5
The distinction between the two forms is
based on age-specific criteria. At school age it is based on the
number of domains of dysfunction. After the onset of puberty,
discrimination is based on the type of dysfunction present.
Complex MND is strongly related to pre- and perinatal adver-
sities and learning and behavioural disorders. Simple MND,
however, might reflect a normal but non-optimally developed
brain, where the ‘d’ of dysfunction rather should be inter-
preted as a ‘d’ of difference.
5
ª The Authors. Journal compilation ª Mac Keith Press 2010
DOI: 10.1111/j.1469-8749.2010.03715.x
941
DEVELOPMENTAL MEDICINE & CHILD NEUROLOGY
ORIGINAL ARTICLE
The aim of this study was to evaluate the relation between
handwriting skills and visuomotor integration on the one
hand, and the severity and type of MND on the other. We
hypothesized that children with complex MND most
frequently show difficulty in writing and visuomotor skills,
children with simple MND somewhat less often, and children
with a normal neurological condition least often. In addition,
we hypothesized that difficulties in writing and visuomotor
integration are associated with fine manipulative dysfunction
and coordination problems, as these forms of MND reflect
dysfunction in complex supraspinal circuitries. To address the
research questions we assessed neurological condition, hand-
writing, and visuomotor integration in a mixed sample of 8-
to 13-years-olds attending a mainstream school and a school
for special education.
METHOD
Participants
This study was performed between December 2005 and Feb-
ruary 2007 at two schools in Appingedam, a small, rural town
in the Netherlands. All children aged from 8 to 13 years
attending a mainstream primary school (n=132) and a school
for special education (n=120) were eligible for the study.
Thirty-four parents and ⁄ or children declined to participate
(mainstream n=12, special school n=22). Children who had
entered puberty were excluded from the study (n=18; main-
stream n=2, special school n=16), leaving 200 children (131
males, 69 females; mainstream n=118, special school n=82; see
Table I). Pubertal status was defined by the presence of the
development of secondary sexual characteristics according to
Tanner et al.
7
The age of the two groups was comparable
(mainstream: mean 10y 5mo, SD 1y 4mo; special school: 10y
10mo, SD 1y 2mo).
Children of 9 years and older and parents gave informed
consent. Procedures were approved by the ethics committee of
the University Medical Center Groningen.
Assessments
Children had four assessments: a neurological examination, a
test to measure motor performance, a handwriting test, and a
test on visuomotor integration. The neurological examination
and the test to measure motor performance were performed
by one of the authors (LHJP) and assistants while the other
assessments were carried out by a different author (JFvH).
The tests on handwriting and visuomotor integration were
performed by group in the classroom; the neurological exami-
nation and the test for motor ability were performed on an
individual basis.
The children were neurologically examined according to
Touwen.
6,8
This assessment is a standardized and age-specific
assessment that pays special attention to the presence of
MND. The neurological examination addresses eight neuro-
logical domains: posture and muscle tone, reflexes, involuntary
movements, coordination and balance, fine manipulation,
associated movements, sensory systems, and cranial nerve
function. The presence of a cluster of signs of dysfunction is
essential.
6,9
This means that the presence of a single sign of
dysfunction, for example difficulty in walking on heels, does
not qualify for the label MND. The notion that the assess-
ment is age-specific does not only mean that test assignment is
adapted to the child’s age-specific behavioural characteristics,
but also that performance is assessed in an age-specific man-
ner. Performance on many items of the assessment, especially
those dealing with associated movements, fine manipulation,
and coordination on which performance depends, changes
substantially with increasing age. The assessor determines
whether performance is adequate or inadequate for age. This
age-specific classification means that performance is corrected
for age.
6
The assessment resulted in a clinical classification. Children
were classified as neurologically normal, simple MND (mean-
ing the presence of one or two clusters of dysfunction), com-
plex MND (indicating the presence of more than two clusters
of dysfunction), or neurologically abnormal. Neurologically
abnormal implied the presence of a classical combination of
Table I: Characteristics of participants
Main stream
school
(n=118) n (%)
School for
special education
(n=82) n (%)
Sex
Male
67 (57)
64 (78)
Female
51 (43)
18 (22)
Neurological classification
Normal
91 (77)
9 (11)
Simple MND
23 (20)
36 (44)
Complex MND
4 (3)
37 (45)
Cluster of dysfunction
Dysfunctional muscle
tone regulation
12 (10)
16 (20)
Reflex abnormalities
46 (39)
40 (49)
Involuntary movements
10 (9)
9 (11)
Difficulties in coordination
and balance
10 (9)
57 (70)
Fine manipulative disability
4 (3)
65 (82)
Associated movements
1 (1)
2 (2)
Sensory deficits
0
2 (2)
Cranial nerve dysfunction
1 (1)
0
Handwriting quality
Missing data
2
9
Normal handwriting
92 (79)
25 (34)
Poor handwriting
22 (19)
26 (36)
Dysgraphic
2 (2)
22 (30)
Writing speed
Missing data
2
10
Normal
83 (89)
11 (15)
Slow (
£4th decile)
33 (11)
61 (85)
VMI
Missing data
3
11
VMI median (range)
102 (75–141)
88 (57–136)
MND, minor neurological dysfunction; VMI, Visual Motor Integration
Test.
What this paper adds
•
Dysgraphic handwriting is closely related to the severity of MND.
•
Impaired visuomotor integration is more related to the presence of MND.
•
Coordination problems and fine manipulative dysfunction clearly contribute to
dysgraphic handwriting and impaired visuomotor integration; dysfunctional
regulation of posture and muscle tone and sensory dysfunction contribute
little.
942
Developmental Medicine & Child Neurology 2010, 52: 941–947
neurological signs, for example the combination of hypertonia
with brisk tendon reflexes, Babinski signs, and stereotyped
posture and movement in the case of cerebral palsy. Children
with MND do not exhibit this classical presentation of neuro-
logical signs. Reliability of the assessment according to Tou-
wen is good (j=0.76–0.83).
8
Handwriting was tested with the Concise Assessment
Method for Children’s Handwriting.
10
It is a shortened and
adapted version of the scale of dysgraphy of De Ajuriaguerra
et al.
11
It is the standard test in the Netherlands to evaluate
handwriting in clinical settings. It measures quality and speed
of handwriting during 5 minutes of writing of a standard text
that children copy on unruled paper. Handwriting quality is
rated according to 13 dysgraphic features. A total score is cal-
culated of which the minimum is 0 and the maximum is 65.
Scores of 0 to 20 are normal, scores of 21 to 28 indicate poor
handwriting, and scores above 29 are interpreted as dysgraph-
ic. This clinical classification was used for the interpretation of
the data. Copying speed is determined by counting the num-
ber of letters written by the child in 5 minutes. The score can
be translated into a decile score scaled to the norm for the
child’s school grade. Hamstra-Bletz
12
studied psychometric
details based on the handwriting of 10 children assessed by a
group of 28 assessors. She reported satisfactory results for
interrater reliability on the items (r=0.71–0.89). Comparison
of classification on the basis of the Concise Assessment
Method for Children’s Handwriting with the classification on
the basis of De Ajuriaguerra demonstrated a good validity
(r=0.72–0.83).
The Developmental Test of Visual Motor Integration
(VMI), 4th edition, revised,
13
was used to test visuomotor
skills. It is a paper and pencil task in which the child copies a
series of shapes in a test booklet. Graphic responses are scored
using the criteria listed in the manual. Shapes meeting speci-
fied criteria are accorded a score 1, non-passed items a 0.
Scoring is discontinued at three consecutive scores of 0.
The maximum score is 27. Raw scores are converted into nor-
malized scores. These normalized scores were used for the
interpretation of the data. The reliability of the VMI is
good.
13
The Movement Assessment Battery for Children
14
(Move-
ment ABC) was used to measure motor performance. Perfor-
mance below the 15th centile was considered a sign of risk for
DCD.
15
Reliability and validity of the Movement ABC are
good.
16,17
Information on cognitive function was obtained from the
teachers. Cognition had been tested by formal IQ tests where
there were educational concerns (n=82). The absence of the
need of IQ testing and an IQ greater than 70 were considered
as typical cognition.
Statistical analysis
Statistical analyses used SPSS software version 16.0 (SPSS Inc.
Chicago, IL, USA). For categorical data, Fisher’s exact test,
Pearson’s v
2
test, or v
2
test for trend were used when appropri-
ate. For the evaluation of the effect of type of school or neuro-
logical condition on VMI, the Mann–Whitney U and
Kruskal–Wallis tests were used. Logistic regression analysis
was applied to assess the relative contribution of the
neurological classification (normal, simple MND, complex
MND) and VMI (dichotomized as very low and low vs better)
to dysgraphic handwriting while taking into account the type
of school as confounder. The significance level was set at
p<0.05.
RESULTS
Neurological data were available for all children; for the VMI
and the handwriting test, data for 14 and 12 children were
missing (Table I). Neurological condition of children with
VMI and ⁄ or handwriting data did not differ from that of chil-
dren with missing data. Twenty-eight participants, seven in
mainstream education and 21 in special education, had the
following clinical diagnoses: attention-deficit–hyperactivity
disorder (n=5), pervasive developmental disorder not other-
wise specified (n=5), dyslexia (n=9), and multiple psychiatric
diagnoses (n=9). One hundred children (50%) had a normal
neurological condition, 59 (30%) were classified as having
simple MND, and 41 (20%) as having complex MND. Chil-
dren attending the school for special education were substan-
tially more often identified with MND; this was especially
true for complex MND (special school, 45%; mainstream
school, 3%; Table I). All types of dysfunction occurred more
frequently in children attending the school for special educa-
tion, but the differences only reached statistical significance
for coordination problems and fine manipulative dysfunction.
Children attending the school for special education also per-
formed significantly worse than the children of the main-
stream school on the tests for handwriting and visuomotor
integration (Table I).
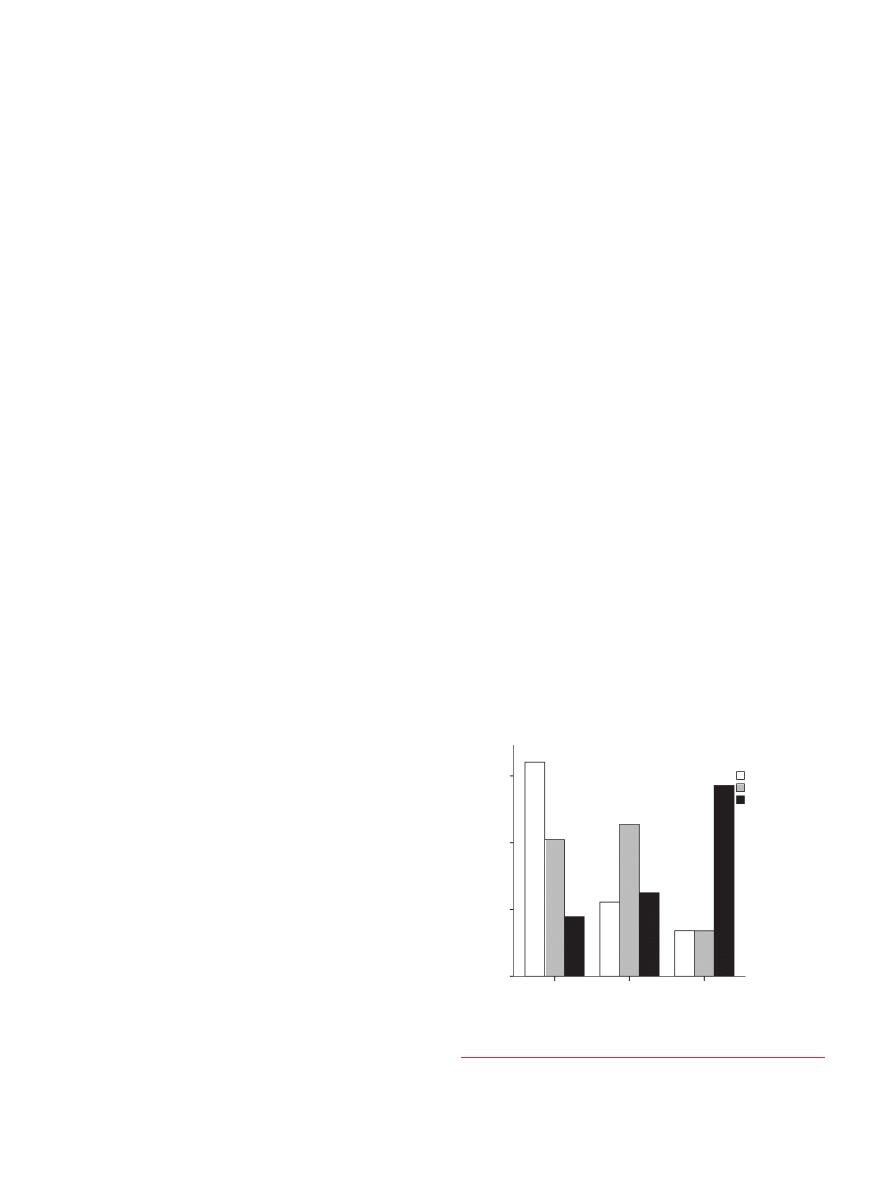
Quality of handwriting was clearly related to the pres-
ence and severity of neurological dysfunction (v
2
for
Normal
(n=98)
(n=53)
(n=38)
Simple MND Complex MND
Neurological condition
Quality of
60
40
20
0
P
e
rcentage
handwriting
Normal
Poor writing
Dysgraphia
Figure 1: Relation between quality of handwriting and neurological clas-
sification (v
2
for trend, p<0.001). MND, minor neurological dysfunction.
Handwriting and MND Jessika F Van Hoorn et al.
943
trend=90.6, degrees of freedom [df]=1, p<0.001; Fig. 1) and
specifically to fine manipulative disability (v
2
=29.8, df=1,
p<0.001)
and
coordination
problems
(v
2
=25.2,
df=1,
p<0.001; Table II). Writing speed was also significantly
related to the severity of neurological condition (Mann–
Whitney U test=1524.0, z=
)4.9, p<0.001; Fig. 2) and to
fine manipulative disability and coordination problems
(Mann–Whitney U test=2054.0, z=
)5.9, p<0.001, and
Mann–Whitney U test=2242.0, z=
)5.3, p<0.001 respec-
tively). These relationships between handwriting (quality
and speed) and neurological condition remained statistically
significant when the analyses were restricted to (1) children
who performed below the 15th centile of the Movement
ABC (Table II) or (2) children with a typical cognition
(n=184; data not shown). In the children with typical cogni-
tion, a less clear relation was found between an excessive
amount of associated movements and dysgraphia (normal
or poor handwriting n=1 [33%], dysgraphic handwriting
n=2 [67%]; Fisher’s exact test, p=0.042).
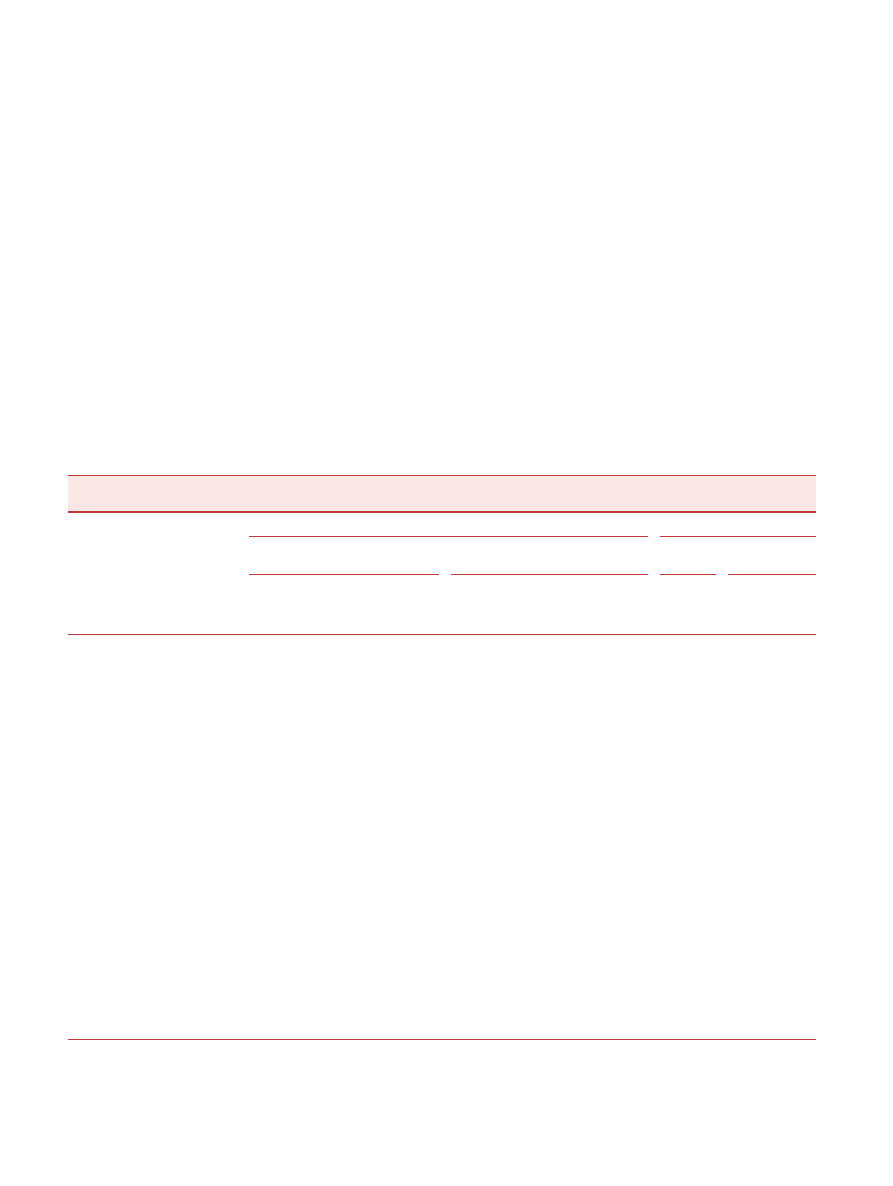
Poor visuomotor integration was related to the presence of
MND (Mann–Whitney U test=1653.5 z=
)3.8 p<0.001;
Table II). Raw scores were only related to the presence of
MND, not its severity (Table II and Fig. 3), but a low or very
low performance showed a statistically significant association
with complex MND (v
2
, p=0.01).
Poor visuomotor integration was associated with fine
manipulative disability (Mann–Whitney U test=1925.0,
z=
)5.4, p<0.001), coordination problems (Mann–Whitney U
test=2078.0, z=
)4.9, p<0.001), dysfunctional muscle tone regu-
lation (Mann–Whitney U test=1419.5, z=
)2.6, p=0.009), and
to sensory dysfunction (Mann–Whitney U test=30.0, z=
)2.0,
p=0.042). These associations remained statistically significant
when the analysis was restricted to children with typical cogni-
tion (n=184; data not shown). The associations between VMI
and fine manipulative disability and coordination problems
also remained statistically significant when the analyses were
restricted to the children who performed below the 15th cen-
tile of the Movement ABC (Mann–Whitney U test=743.0,
z=
)0.4, p<0.001, and Mann–Whitney U test=842.5, z=)2.6,
p=0.01). Associations between VMI and dysfunctional muscle
tone
regulation
and
sensory
dysfunction
disappeared
(Table II).
Table II: Relation between specific neurological dysfunction and handwriting and visuomotor integration (VMI)
Neurological condition
Handwriting
VMI
Entire population
Movement ABC<15th centile
Entire
population
Movement
ABC<15th centile
Normal
or poor
n (%)
Dysgraphic
n (%)
Speed,
median
decile score
Normal or
poor n (%)
Dysgraphic
n (%)
Speed,
median
decile score
Median
Median
Clinical classification
Normal neurological condition
93 (95)
5 (5)
6
26 (90)
3 (10)
6
101
a
97
c
Simple MND
46 (87)
7 (13)
3
31 (86)
5 (14)
2
92
90
Complex MND
22 (58)
16 (42)
a
1
a
18 (55)
15 (45)
a
1
b
90
89
Type of dysfunction
Dysfunctional muscle tone regulation
Domain; no
141 (86)
23 (14)
5
63 (78)
18 (22)
3
98
92
Domain; yes
20 (80)
5 (20)
3
12 (71)
5 (29)
2
92
b
83
Reflex abnormalities
Domain; no
94 (87)
14 (13)
5
44 (80)
11 (20)
2
97
92
Domain; yes
67 (83)
14 (17)
4
31 (72)
12 (28)
3
97
91
Involuntary movements
Domain; no
148 (86)
24 (14)
5
68 (78)
19 (22)
3
97
93
Domain; yes
13 (76)
4 (24)
4
7 (64)
4 (36)
2
92
86
Difficulties in coordination and balance
Domain; no
121 (95)
7 (5)
6
38 (88)
5 (12)
6
100
97
Domain; yes
40 (66)
21 (34)
a
2
a
37 (67)
18 (33)
c
1
a
90
a
90
b
Fine manipulative disability
Domain; no
122 (95)
6 (5)
6
44 (94)
3 (6)
6
100
96
Domain; yes
39 (64)
22 (36)
a
1
a
31 (61)
20 (39)
a
1
a
88
a
86
a
Associated movements
Domain; no
160 (86)
26 (14)
5
74 (78)
21 (22)
3
97
92
Domain; yes
1 (33)
2 (67)
1
1 (33)
2 (67)
1
91
91
Sensory deficits
Domain; no
160 (86)
27 (14)
5
74 (77)
22 (23)
3
97
92
Domain; yes
1 (50)
1 (50)
1
1 (50)
1 (50)
1
70
c
70
Cranial nerve dysfunction
Domain; no
160 (85)
28 (15)
5
75 (77)
23 (23)
3
97
91
Domain; yes
1 (100)
0
4
0
0
NA
84
NA
Association with complex minor neurological dysfunction (MND) (vs normal condition and simple MND): v
2
or Fisher’s exact test for
dichotomized outcomes, otherwise Mann–Whitney U test:
a
p<0.001;
b
p<0.01;
c
p<0.05. Association with normal neurological condition (normal vs
simple and complex MND). Association with specific dysfunction: (v
2
or Fisher’s exact test for dichotomized outcomes, else Mann–Whitney U
test). Movement ABC, Movement Assessment Battery for Children.
944
Developmental Medicine & Child Neurology 2010, 52: 941–947
We used logistic regression analysis (n=200) to assess the
relative contribution of both neurological condition and per-
formance on the VMI to dysgraphic handwriting. This
revealed that VMI and simple MND were not related to
dysgraphic handwriting, the role of complex MND just failed
to reach statistical significance (odds ratio 2.86 [95% confi-
dence interval [CI] 0.98–8.37], p=0.055), and attending a
school for special education was the major factor contributing
to dysgraphia (odds ratio 34.53 [95% CI 5.53–215.64],
p<0.001).
DISCUSSION
The present study demonstrated that impaired handwriting
and visuomotor integration were related to MND, in particu-
lar to fine manipulative disability and coordination problems.
Poor handwriting was more closely related to the severity of
MND than impaired visuomotor integration.
The children included in the study were recruited at two
schools, a mainstream school and a school for special educa-
tion. This means that the results of the study cannot be gener-
alized to the wider population. The prevalences of MND and
difficulties in handwriting of children attending the main-
stream school resembled those of other reports,
5,12,18,19
sug-
gesting that this group may be considered representative for
the general population in these two aspects. Owing to the
inclusion of children attending a school for special education,
children with MND were overrepresented,
5,20
which can be
considered an advantage for a study on relationships between
neurological condition, handwriting, and visuomotor inte-
gration.
A limitation of our study is the lack of details on the chil-
dren’s literacy. Literacy difficulties are associated with DCD
21
and MND.
5
This means that part of the association between
dysgraphia exhibited during copying of a text and MND
might be mediated by literacy difficulties.
The strength of the study is that a relatively large group of
children was assessed with four standardized, reliable, and
valid tests. The relationships between neurological condition
and handwriting and visuomotor integration remained statisti-
cally significant when the analyses were restricted to children
with typical cognition and to children with a performance on
the Movement ABC below the 15th centile. This means that
our data may also be valid for children with DCD attending
these schools, as performance below the 15th centile on the
Movement ABC often is used as a criterion for DCD. The
diagnosis of DCD is, however, primarily based on a clinical
concern, namely parents’ and teachers’ experience that the
child’s motor function is impaired to such an extent that it
interferes with activities of daily life. In this respect, it is inter-
esting to note that when, in the present study, the results of
the child’s performance were communicated to parents and
teachers, they often expressed surprise about the findings.
Very often they were not aware of their child’s motor impair-
ment (e.g. Movement ABC score <1st centile).
The most frequently occurring dysfunctions of the children
attending the school for special education were difficulties in
coordination, balance and fine manipulative disability, being
present in 70% and 82% of the children. Handwriting
requires a high level of coordination and high-precision force
regulation. Therefore, we hypothesized that handwriting was
related to these forms of MND, which was confirmed by
our data. Both quality of handwriting and writing speed were
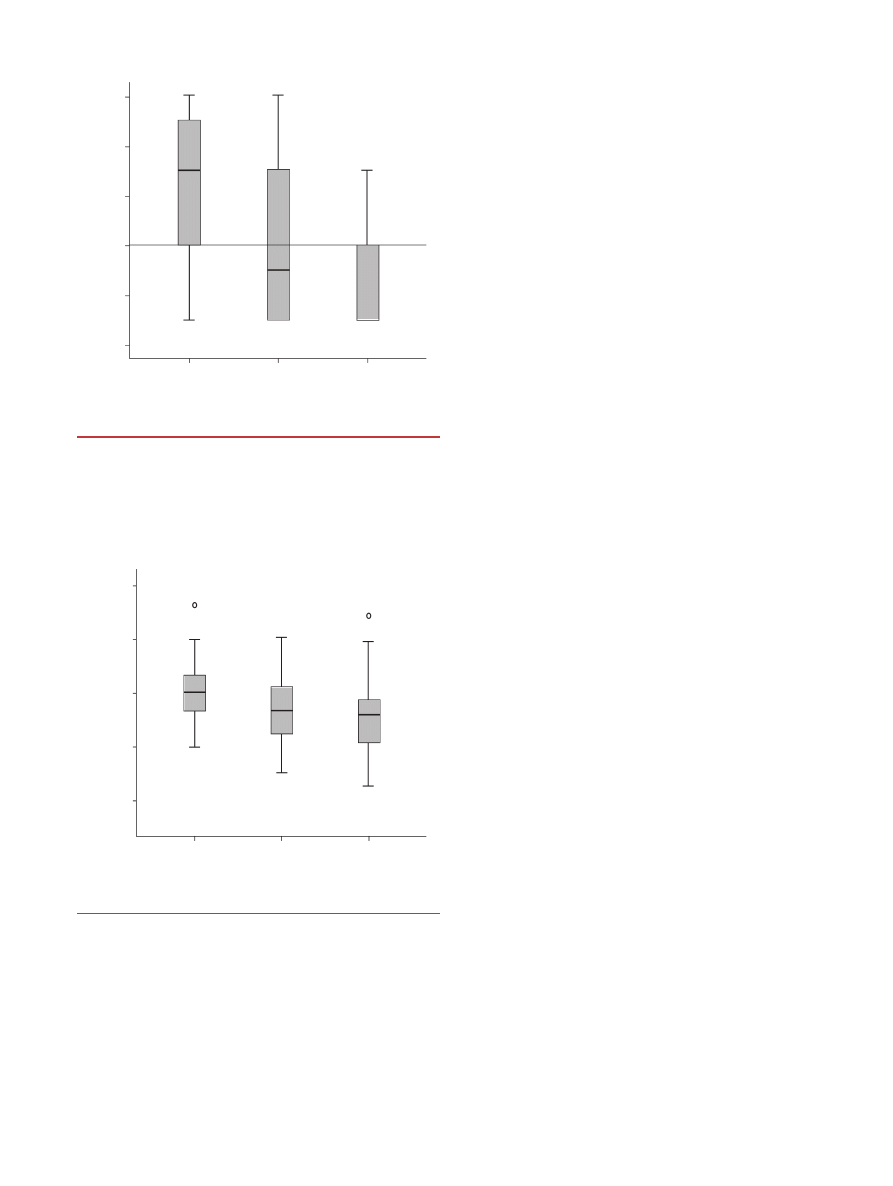
10
8
6
4
2
0
Normal
(n=98)
(n=53)
(n=37)
Simple MND
Wr
iting speed in decile score
Complex MND
Neurological condition
Figure 2: Writing speed and neurological condition. Bold horizontal lines
indicate median values; the boxes represent interquartile ranges, and the
vertical lines total ranges. The horizontal line denotes the fourth decile,
which is the cut-off for slow speed (v
2
test, linear-by-linear association,
p<0.001). MND, minor neurological dysfunction.
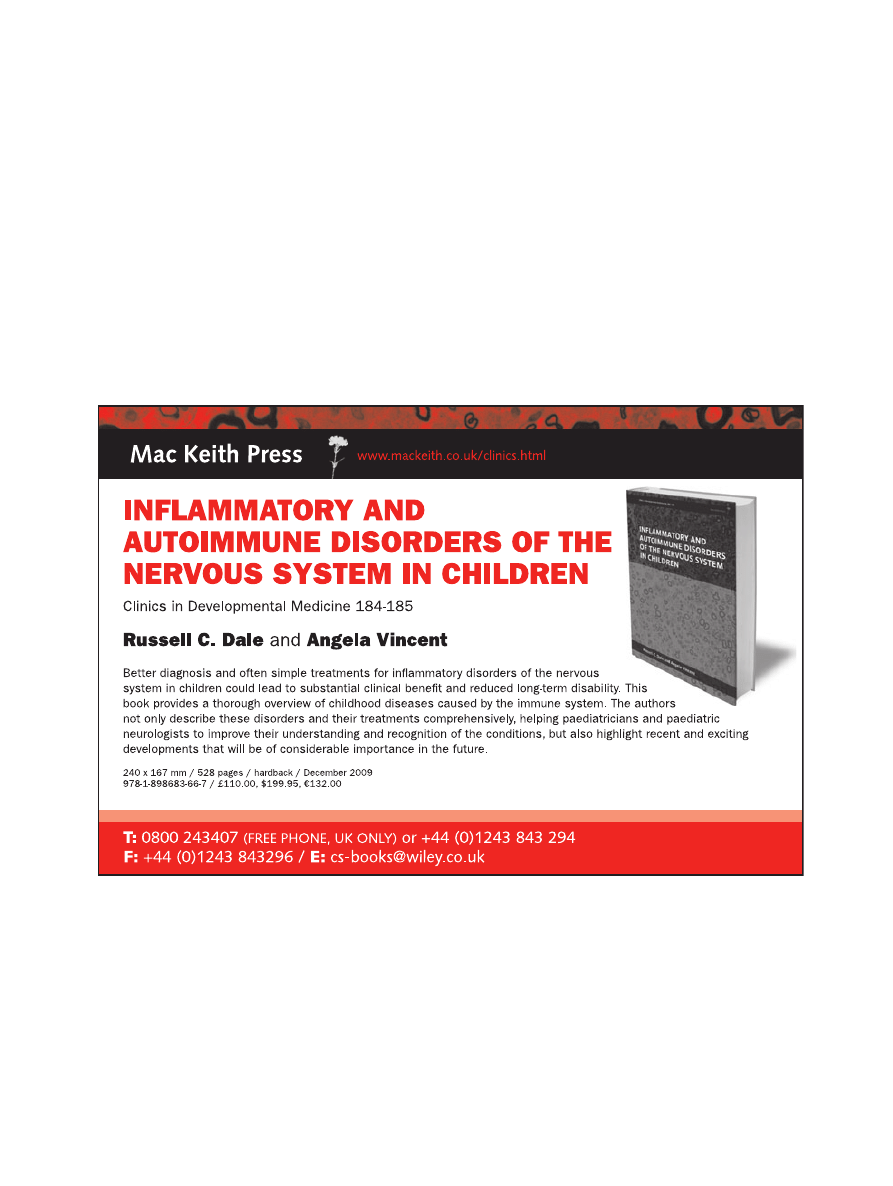
Normal
(n=96)
(n=53)
(n=37)
Simple MND
Complex MND
Neurological condition
150
125
100
75
50
Visuomotor integ
ration
Figure 3: Relation between visuomotor integration and neurological
classification (v
2
for trend, p<0.001). Bold horizontal lines indicate median
values; small circles indicate outlying values. MND, minor neurological
dysfunction.
Handwriting and MND Jessika F Van Hoorn et al.
945

closely related to coordination problems and fine manipulative
disability. Our data also fit with findings of functional MRI.
The anterior part of the left superior parietal lobule, the pos-
terior part of the middle and superior frontal gyri, and the
right cerebellum, are crucial for writing, whereas the left
premotor cortex, sensorimotor cortex, and supplementary
motor area are also involved.
22
Other dysfunctions, such as
choreiform dyskinesia and mild abnormalities in muscle tone
regulation, i.e. dysfunctions in which cortical or cerebellar
involvement is less, were not related to handwriting problems.
Impaired visuomotor integration was not only related to
coordination problems and fine manipulative disability, but
also to dysfunctional muscle tone regulation and, to a lesser
extent, to sensory dysfunction. However, in children with a
Movement ABC score below the 15th centile the latter two
dysfunctions were not related to poor visuomotor integration.
Visuomotor integration is the degree to which visual percep-
tion and finger–hand movements are coordinated. Children
can have well-developed visual and motor skills but be unable
to integrate the two.
13
It seems likely that different areas in the
brain are responsible for integrating visual information into
discrete motor plans. This conversion most likely occurs both
in motor and sensory association areas, the cerebellum, and in
subcortical nuclei in a dynamic, parallel manner. In other
words, a major part of the brain is involved in visuomotor
tasks, which might explain that it is a complex task easily ham-
pered by dysfunction of any part of the brain. This might also
explain why poor performance on the VMI was less closely
related to the severity of MND.
Children spend 30% to 60% of their school day performing
handwriting and other fine motor tasks.
23
As the presence of
handwriting problems may affect the children’s ability to func-
tion in daily life, it is essential that they are comprehensively
assessed so that meaningful intervention can be offered when
necessary. This is especially true for children with DCD and
writing problems. The child’s neurological profile may guide
the selection of the most appropriate intervention. The pres-
ence of complex MND presumably indicates that the child is
hampered by two major problems: (1) a limited repertoire of
motor strategies and (2) difficulties in adapting motor perfor-
mance to task specific requirements.
24
The presence of a lim-
ited repertoire of strategies suggests that there should be
hesitation in allowing the child to use a computer for writing
activities at school. The adaptation problems indicate that
writing performance may be enhanced by (1) ample practice
and (2) decreasing the need for adaptation to the complex task
of writing. This could be achieved, for instance, by means of
adequate writing implements and appropriate seating.
25
The
presence of simple MND denotes the presence of normal,
non-optimal brain function.
23
Writing performance of chil-
dren with simple MND may be improved by practice and sim-
plification of the writing task as indicated above.
CONCLUSION
The present study indicates that writing problems are related
to the presence and severity of MND, whereas the even more
complex tasks of visuomotor integration are easily hampered
by various forms of MND. In children with writing problems
the neurological profile may guide the choice of intervention;
children with complex MND may benefit, at school in partic-
ular, from the use of a computer, whereas for children with
any type of MND writing may improve through practice and
appropriate seating.
ACKNOWLEDGEMENTS
We acknowledge the help of Eva Kouw, Marjolein Hamming, and
Akke-Nynke van der Meer in data collection, and Michiel Schrier in
the preparation of the figures. We thank the two schools in Appinge-
dam for allowing us to assess the children. We also thank the children
and the parents who agreed to participate.
REFERENCES
1. Karlsdottir R, Stefansson T. Problems in developing func-
tional handwriting. Percept Mot Skills 2002; 94: 623–62.
2. Feder KP, Majnemer A. Handwriting development, compe-
tency, and intervention. Dev Med Child Neurol 2007; 49:
312–7.
3. American Psychiatric Association. Diagnostic and Statistical
Manual of Mental Disorders. 4th edn. Washington, DC:
American Psychiatric Association, 2000.
4. Maeland AE. Handwriting and perceptual motor skills in
clumsy, dysgraphic, and normal children. Percept Mot Skills
1992; 75: 1207–17.
5. Hadders-Algra M. Two distinct forms of minor neurological
dysfunction: perspectives emerging from a review of data of
the Groningen Perinatal Project. Dev Med Child Neurol
2002; 44: 561–71.
6. Touwen BCL. Examination of the child with minor neuro-
logical dysfunction. Clinics in Developmental Medicine No.
71. London: Mac Keith Press, 1979.
7. Tanner JM, Whitehouse RH, Takaishi M. Standards from
birth to maturity for height, weight height velocity and
weight velocity; British children. Arch Dis Child 1965; 41:
455–71.
8. Peters LHJ, Maathuis KGB, Kouw E, Hamming M, Had-
ders-Algra M. Test–retest, inter-assessor and intra-assessor
reliability of the Touwen examination. Eur J Paediatr Neurol
2008; 12: 328–33.
9. Hadders-Algra M. Developmental coordination disorder: is
clumsy motor behaviour caused by a lesion of the brain at
early age? Neural Plast 2003; 10: 39–50.
10. Hamstra-Bletz E, de Bie J, den Brinker BPLM. [A brief eval-
uation method for children’s handwriting]. Lisse: Swets &
Zeitlinger, 1987. (In Dutch).
11. De Ajuriaguerra J, Auzias M, Coumes F, et al. [Children’s
writing. The evolution of writing and its difficulties]. 3rd
edn. Paris: Delachaux & Niestle´, 1979. (In French).
12. Hamstra-Bletz E. [Child’s handwriting: development and
assessment]. (Thesis). University of Leiden, 1993. (In
Dutch).
13. Beery KE. Administration, Scoring and Teaching Manual for
the Beery-Buktenica Developmental Test of Visual–Motor
Integration with Supplemental Developmental Tests of
Visual Perception and Motor Coordination. New Jersey:
Modern Curriculum Press, 1997.
14. Henderson S, Sugden DA. Movement Assessment Battery
for Children. San Antonio, TX: Psychological Corporation,
1992.
15. Geuze RH, Jongmans MJ, Schoemaker MM, Smits-Engels-
man BCM. Clinical and research diagnostic criteria for devel-
opmental coordination disorder: a review and discussion.
Hum Mov Sci 2001; 20: 7–47.
16. Smits-Engelsman BCM. Nederlandse bewerking van de
Movement Assessment Battery for Children. Lisse: Swets
Test Publishers, 1998.
17. Henderson SE, Hall D. Concomitants of clumsiness in
young schoolchildren. Dev Med Child Neurol 1982; 24: 448–
60.
18. Smits-Engelsman BCM. Theory-based diagnosis of fine
motor coordination development and deficiencies using
handwriting tasks. (Thesis). University of Nijmegen, 1995.
19. Mojet JW. Characteristics of the developing handwriting skill
in elementary education. In: Wann J, Wing AM, Søvik N,
946
Developmental Medicine & Child Neurology 2010, 52: 941–947
editors. Development of graphic skills. London: Academic
Press, 1991; pp 53–75.
20. Arnaud C, Daubisse-Marliac L, White-Koning M, et al.
Prevalence and associated factors of minor neuromotor dys-
functions at age 5 years in prematurely born children: the
EPIPAGE Study. Arch Pediatr Adolesc Med 2007; 161:
1053–61.
21. O’Hare A, Khalid S. The association of abnormal cere-
bellar function in children with developmental coordina-
tion disorder and reading difficulties. Dyslexia 2002; 8:
234–48.
22. Sugihara G, Kaminaga T, Sugishita M. Interindividual uni-
formity and variety of the ‘writing center’: a functional MRI
study. Neuroimage 2006; 32: 1837–49.
23. McHale K, Cermak SA. Fine motor activities in elementary
school: preliminary findings and provisional implications for
children with fine motor problems. Am J Occup Ther 1992;
46: 898–903.
24. Hadders-Algra M. The neuronal group selection theory:
promising principles for understanding and treating develop-
mental motor disorders. Dev Med Child Neurol 2000; 42:
707–15.
25. Hadders-Algra M, Brogren Carlberg E. Postural control: a
key issue in developmental disorders. Clinics in Develop-
mental Medicine No. 179. London: Mac Keith Press,
2008.
Handwriting and MND Jessika F Van Hoorn et al.
947
Wyszukiwarka
Podobne podstrony:
JOINT CAPABILITIES INTEGRATION AND DEVELOPMENT SYSTEM
Posture and Core Conditioning
JOINT CAPABILITIES INTEGRATION AND DEVELOPMENT SYSTEM
Improving virus protection with an efficient secure architecture with memory encryption, integrity a
17 E85 Heating and Air Conditioning System
Posture and Core Conditioning
ti 1102 Transporter 2004 Heating and Air Conditioning
Rykała, Andrzej Spatial and historical conditions of the Basques aiming to obtain political indepen
integration and radiality measuring the extent of an individuals connectedness and reachability in a
Political Thought of the Age of Enlightenment in France Voltaire, Diderot, Rousseau and Montesquieu
The Dirty Truth?out The Cloud And The Digital Age
10 Integracja NT i NetWare File and Print Services for NetWare
Audel Hvac Fundamentals, Air Conditioning, Heat Pumps And Distribution Systems (Malestrom)
III dziecinstwo, Stoodley From the Cradle to the Grave Age Organization and the Early Anglo Saxon Bu
Conditioning for Sports and Martial Arts
keohane nye Power and Interdependence in the Information Age
Neurology and the eye
evolutionary psychology and conceptual integration - opracowanie, psychologia, psychologia ewolucyjn
Botox, Migraine, and the American Academy of Neurology
więcej podobnych podstron