www.optometry.co.uk
33
Adrian Parnaby-Price MA, MB, BChir (Cantab), FRCSEd
Neurology and the eye
Case histories
Module 2 part 12 is devoted to five case histories to demonstrate the real-life
clinical presentations of neuro-ophthlamic conditions and some of the
important features to aid diagnosis and management.
The College of
Optometrists has
awarded this
article 2 CET
credits. There are
12 MCQs with a
pass mark of 60%.
The College of
Optometrists
3
A 45-year-old female barrister presented to
her optometrist with a two week history of
intermittent diplopia and mild blurring of
vision in the left eye. A friend had
commented on her small right pupil at a
barbecue party six weeks earlier, but she
had not noticed this herself. On specific
questioning, she admitted to headaches
which were either bitemporal or
occasionally felt as a sharp stab over the
left temple. She only had a three year old
pair of reading glasses with +1.50DS
correction right and left.
On examination, vision was 6/6+1 right
with a +1.25DS correction, and 6/5 left
with a +1.50/-0.50 x 85 correction. She
had no manifest squint in the primary
position. Cover testing revealed a slight
exophoria in primary position which
became manifest on right gaze. There was
anisocoria with the right pupil slightly
smaller than the left. There was no RAPD,
but the left pupil was sluggish and did not
constrict well. The media were clear and
the discs were normal. There were two dot
haemorrhages in the right mid-peripheral
retina but none in the left.
Questions
1. Which is the abnormal eye?
2. Why has this been noticed by
a friend but not by the patient?
3. What is the squint?
4. What is the significance of the retinal
haemorrhages?
5. What should the optometrist do next?
Answers
1. Which is the abnormal eye?
The left eye is abnormal. Although vision is
subjectively reduced in the left eye, in fact
the astigmatism more than accounts for
this and vision is approximately normal and
equal in both eyes with appropriate
refractive correction. There is no afferent
defect as this condition is of efferent
pathways. However, the left pupil is
abnormal and fails to respond properly to
formal pupil testing and there is an
exotropia on right gaze suggesting a left
third nerve palsy rather than an esotropia
suggestive of a right sixth nerve palsy. The
retinal haemorrhages are not directly
related to the ocular problem but may be
related to systemic disease.
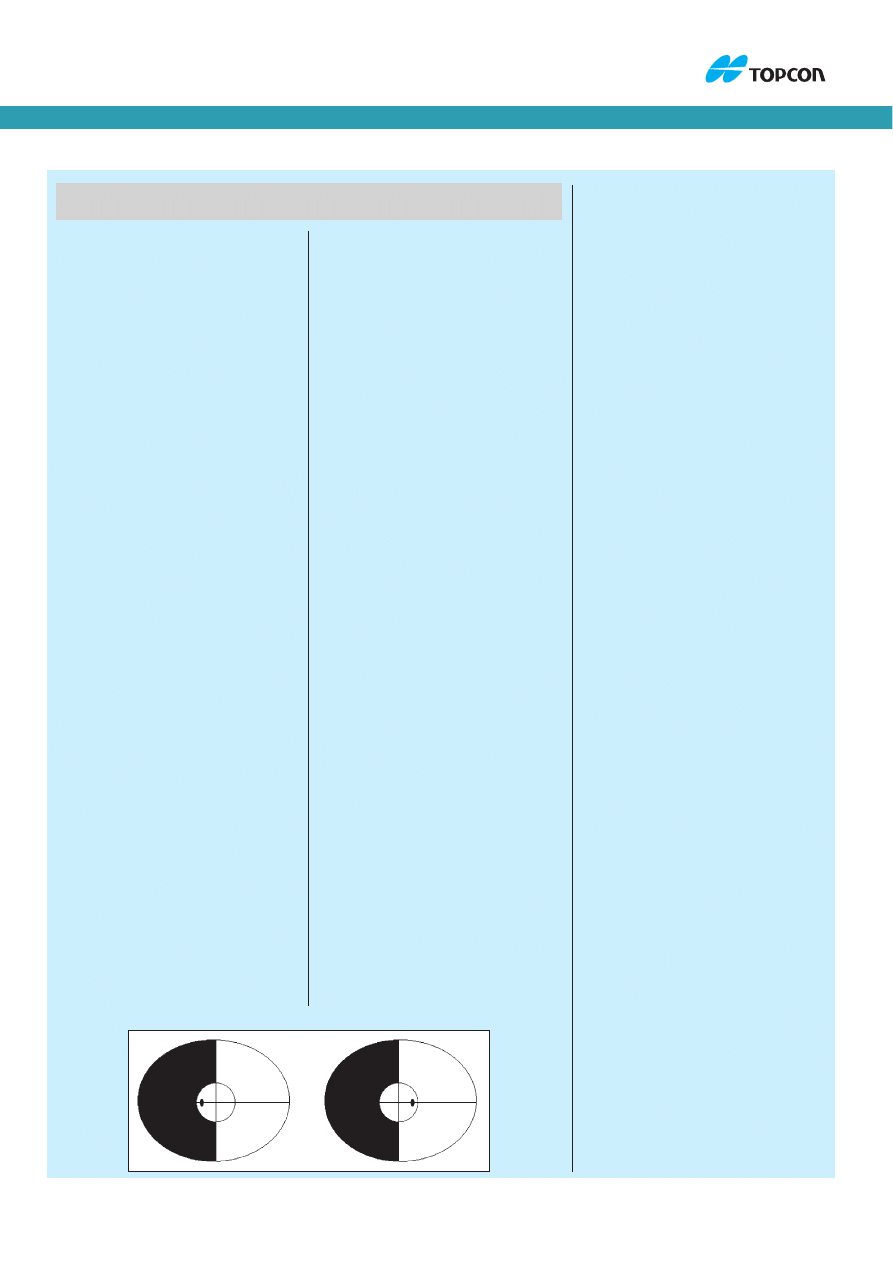
2. Why has this been noticed by
a friend but not by the patient?
The friend has noticed the anisocoria but
has mistaken the normal, smaller right
pupil as pathological instead of the larger,
abnormal left pupil. In the bright daylight
at the barbecue, parasympathetic pupil
constriction failure is more noticeable as
the affected pupil fails to constrict. In the
dimmer indoor light of the patient’s home
where she looks at herself in a mirror,
neither pupil is particularly constricted and
therefore parasympathetic anisocoria is
more difficult to see.
3. What is the squint?
The patient is most likely to be exhibiting
the effects of a left partial third nerve
palsy for the reasons outlined earlier.
4. What is the significance
of the retinal haemorrhages?
The most common causes of retinal
haemorrhages seen as an isolated finding
are diabetes mellitus or vascular
hypertension. Both of these may be
associated with nerve lesions, in
particular third nerve palsies and pupil
abnormalities.
5. What should the
optometrist do next?
The symptoms and signs are those of a
painful third nerve palsy involving the
pupil. The most important diagnoses
include a structural/compressive lesion
such as an intracranial tumour or aneurysm
which constitute a medical emergency and
indicate immediate referral to hospital
services for an urgent CT or MRI scan.
At hospital this patient was found to be
hypertensive and had a blood pressure of
230/130. She had an aneurysm of the
carotid artery in the left cavernous sinus
which was treated neurosurgically the
morning following presentation to the
optometrist. She made an almost complete
recovery of pupil and nerve palsy and did
not suffer the potential progression of the
aneurysm to cerebro-vascular accident.
CASE 1
A 36-year-old female director of sales and
marketing presented to her General
Practitioner with a history of “droopy
eyelids” in the evenings which she first
noticed in photographs taken some 12
months earlier. This had been getting worse
for around the last 3-4 months.
She had worn soft contact lenses for
12 years without significant problems and
switched to daily disposable lenses
18 months earlier. The GP requested an
optometrist check-up to exclude lens
problems as the cause and she presented
for review early next morning before flying
to a series of business meetings in the US
later the same day.
On direct questioning she reported that
the lids might be droopy either as one or
both together and she was having
occasional blurring of vision and diplopia.
This could be remedied by putting cold
compresses over the eyes for 5 minutes.
She tended to wear her lenses from early
morning until late at night although her
optometrist had suggested at review six
months earlier that she should be cutting
down on the total wearing time due to
“minor overwear problems”. She was
otherwise well although has lost some
weight recently.
Vision was 6/5+ in both eyes with
lenses. The lenses were equivalent to
spectacle correction of –5.50/-1.00 x 60
right and –4.50/-1.50 x 100 left. There
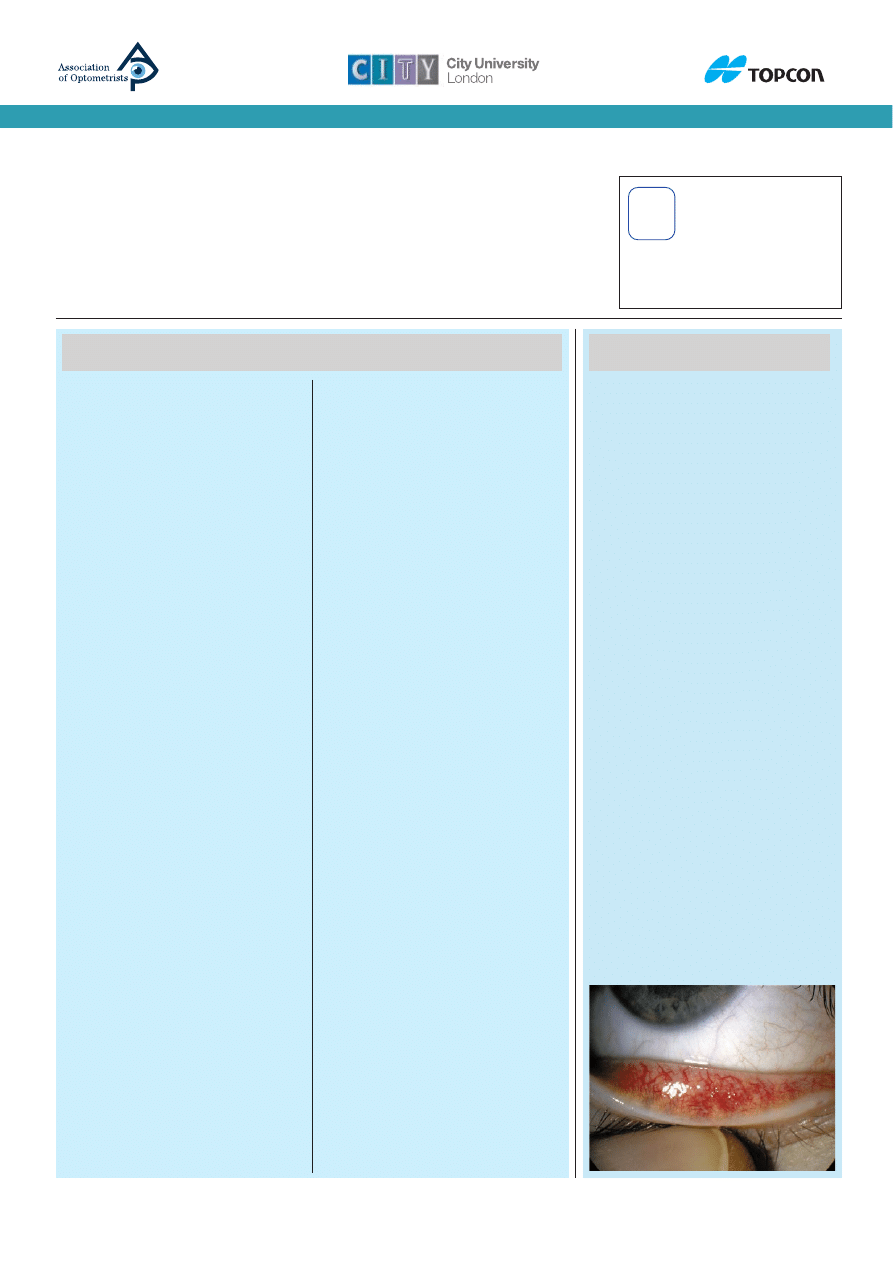
were numerous follicles and moderate
injection of the palpebral conjunctiva in
both eyes (Figure 1). Both corneae had
CASE 2
Figure 1 Conjunctival follicles
sponsored by
34
o
t
December 1, 2000 OT
www.optometry.co.uk
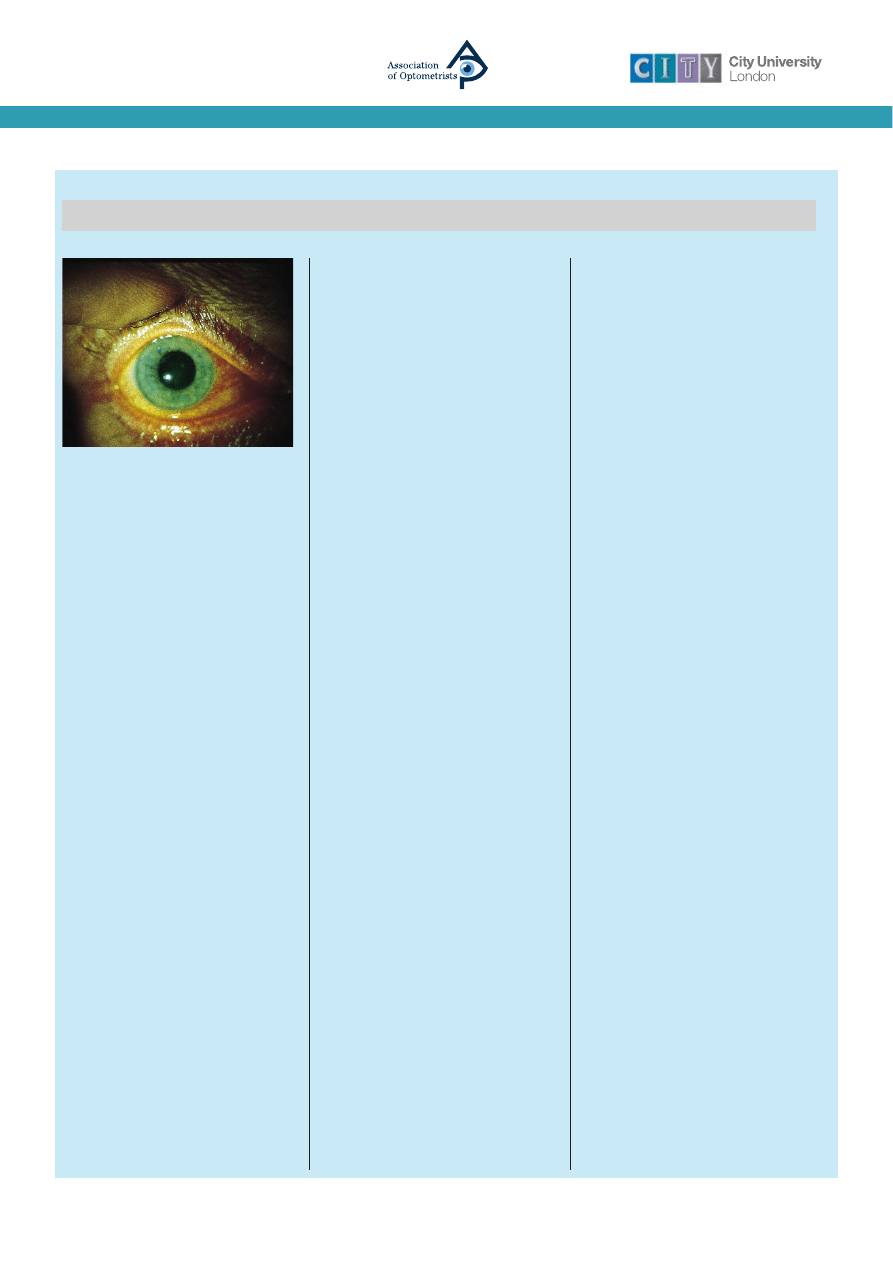
mild vessel infiltration of the cornea and
mild scleral injection consistent with
overwear (Figure 2). The eyes appeared
slightly prominent with very mild
thickening of the lids. The upper lid
margins appeared at normal position and
equal on both eyes, cutting the cornea
just below the upper limbus. There were
no afferent or efferent pupil defects.
The optometrist diagnosed a mild
overwear problem and gave appropriate
advice suggesting a review in one month’s
time.
Late in the afternoon 4 days later, she
returned to the optometrist with
significant increase in symptoms of
diplopia and lid problems since returning
to the UK the day before. She insisted
that she had reduced her lens wearing
time to only a few hours each day during
meetings.
Vision was 6/5+ in both eyes with no
pupil abnormalities. There was
improvement in the palpebral conjunctival
injection, although there were still some
follicles and the corneal vessels were less
prominent but the scleral vessels
appeared to be more full than normal,
more so on the right. The upper lids
appeared to be slightly fuller and bisected
the cornea 1.5-2mm below the upper
limbus in the right eye. Ocular motility
testing revealed diplopia in all extremes
of gaze, particularly on upgaze. There was
the suggestion of a right third nerve
weakness with abnormal abduction of the
left eye, but this was not consistent with
an internuclear ophthalmoplegia and was
not clearly apparent on cover testing. The
optometrist noted ptosis towards the end
of testing, more noticeable in the right
eye. The patient complained of discomfort
and was offered a paper napkin with cold
water to use as a compress which
appeared to reduce the ptosis and allow
re-examination after a few minutes.
Figure 2 The result of overwear
This time ocular motility appeared to
have returned to normal although
prolonged upgaze induced a slight return
of the 1-2mm ptosis of the right eyelid
which again recovered with the
application of a cold compress.
The patient was referred to a hospital
specialist for assessment.
Questions
1. What is the diagnosis and what
is the cause of the condition?
2. Why has the patient deteriorated
3. Why do the cold compresses
improve symptoms
4. What associated condition
might exhibit ocular signs?
5. What is internuclear
ophthalmolplegia?
6. What is the management
of the primary condition?
Answers
1. What is the diagnosis and what
is the cause of the condition?
Myaesthenia gravis, caused by impaired
neuromuscular transmission from the
production of auto-antibodies to
acetylcholine receptors in the motor
endplates of striated muscles.
2. Why has the patient deteriorated?
Although it is usually physical activity
which causes increase in severity of the
condition, tiredness (including that from
jet-lag) can worsen symptoms
significantly. Symptoms are characterised
by their extremely rapid variability, often
within minutes and are described by
patients as “failure to move” rather than
“tiredness and aching” such as a fatigue
following exercise.
3. Why do the cold compresses improve
symptoms?
Any lid swelling due to contact lens
problems will be aided by cold but in this
case it is more likely that simply the
resting of the extra-ocular muscles during
eye closure allowed recovery. The extreme
variability of phorias or tropias during the
same examination is very suggestive of
myaesthenia. Myaesthenia gives rise to
generalised muscle weakness, which can
mimic any of the patterns of the ocular
nerve palsies or central lesions including
gaze palsies, INO and nystagmus but the
pupils are not affected.
4. What associated condition might
exhibit ocular signs?
Patients with myaesthenia gravis have an
increased risk of other autoimmune
diseases and thyroid dysfunction is
present in 5-8% of myaesthenic patients.
Other features of thyroid eye disease
include prominent globes and orbital
congestion with injection of conjunctival
and scleral vessels and mild lid swelling
with ptosis. Extraocular muscle
involvement can mimic mild or early
nerve palsies.
5. What is internuclear
ophthalmolplegia?
Internuclear ophthalmoplegia is caused by
a lesion in the medial longitudinal
fasciculus (a neural tract running through
the brainstem carrying impulses from the
vestibular nuclei to the cranial nuclei). It
is characterised by limitation of adduction
in one eye with ataxic nystagmus in the
abducting eye and may be bilateral. The
pupils are not involved in the lesion.
Causes of lesions in this area include
multiple sclerosis, tumours and vascular
events.
6. What is the management of the
primary condition?
Ocular involvement is present in 90% of
myaesthenic patients and is the
presenting complaint in 75% with most
progressing to systemic symptoms within
two years. Diagnosis is made by
identifying acetylcholine receptor
antibodies in the blood although only
30% of myaesthenic patients have these.
If indicated, intravenous edrophonium
chloride (Tensilon) relieves symptoms and
signs immediately (particularly of ptosis)
and is diagnostic. Electromyelography can
be helpful but is rarely used in clinical
practice.
Ocular myaesthenia alone may be
managed by ocular occlusion, prism
spectacles, oral pyridostigmine and
systemic steroids. Surgical thymectomy
may be indicated and plasmaphoresis
has been used. It is important to
monitor thyroid status after
diagnosis.
In this patient treatment with oral
pyridostigmine and reduction in contact
lens wear time did not significantly
improve the scleral and episcleral
injection although the corneal vessels
regressed somewhat. Symptoms of
diplopia were completely alleviated
and the ptosis has resolved. She
remains well two years after initial
presentation.
CASE 2
continued
www.optometry.co.uk
35
Module 2 Part 12
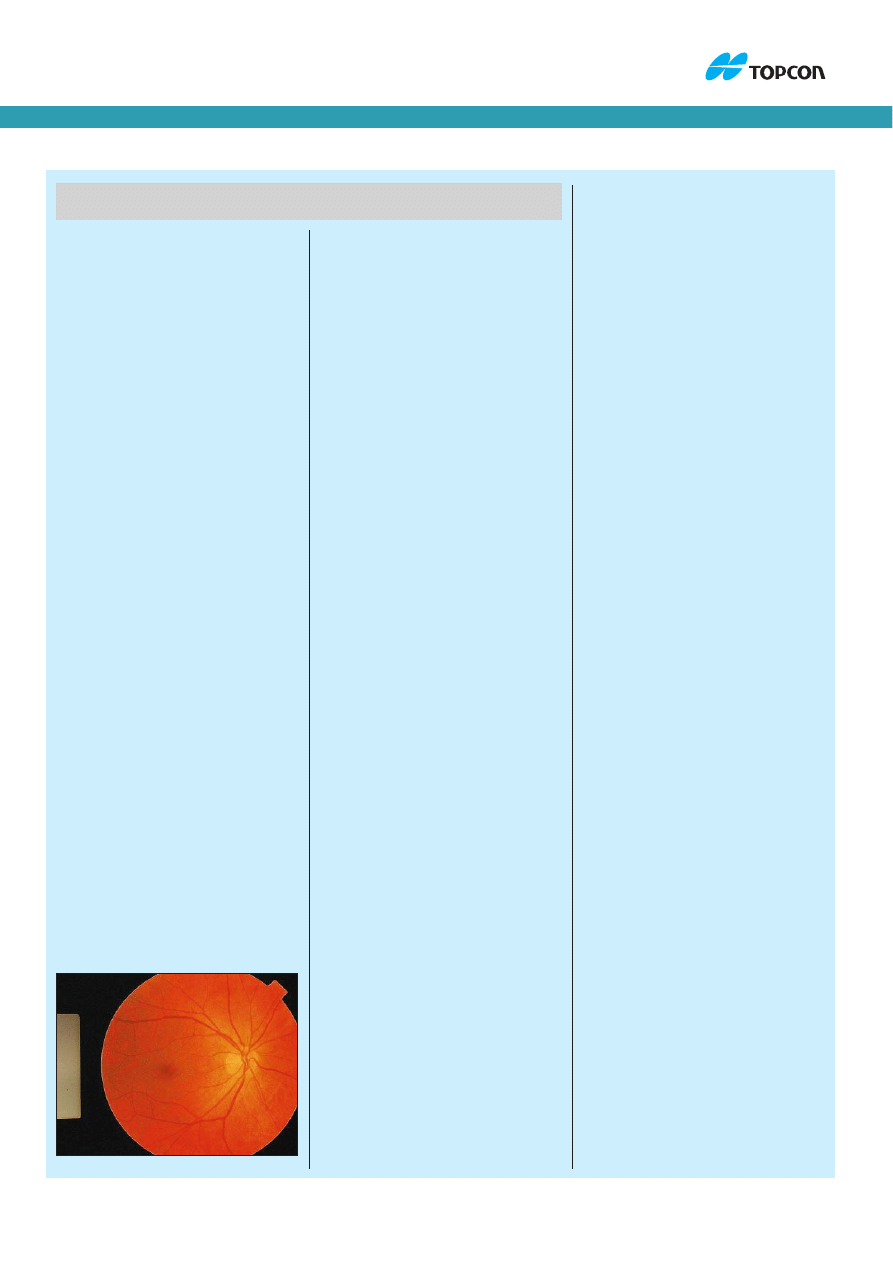
Figure 3 Optic atrophy
A 23-year-old fifth year medical student
presented to his ophthalmology lecturer
during a clinical attachment. He complained
of a left retrobulbar ache over the previous
four days and some blurring of vision in the
left eye over the last 24-48 hours. He was
otherwise fit and well.
Vision was 6/12 right, 6/9 left unaided
with no improvement in acuity with pinhole.
Subjective red appreciation was reduced in
the right eye but normal in the left. Ishihara
colour vision was 10/16 + test plate right,
16/16 + test plate left. Ocular movements
were full with no diplopia or obvious
restriction of movement although there was
a slight increase in the retrobulbar ache in
the left eye on extreme version. The right
eye was white with no anterior segment
pathology, but there was moderate injection
of the scleral and conjunctival vessels of the
left eye with cells and flare in the anterior
chamber. There was a right RAPD. After
dilation, the right optic disc was pale
(Figure 3) although the left disc was
normal.
After more careful questioning, the
patient gave a history of a temporary loss of
vision in the right eye some 4 years earlier
which had apparently recovered without
treatment. The ophthalmologist who had
seen him during that episode at the
student’s home town had not offered a
specific diagnosis but seemed confident that
there would be no sequelae. He also reported
an episode of mild weakness of his left hand
and lower arm about six months earlier
which had again resolved after 2-3 weeks for
which he did not seek medical advice. On
physical examination the tendon reflexes of
the arms were asymmetrical with increased
responses on the left (upper motor neurone
pattern).
Questions
1. What is the diagnosis in the left eye?
2. What is the treatment
for this condition?
3. What is the likely pathology
in the right eye?
CASE 3
4. Are the two conditions associated?
5. What investigations might be
helpful in establishing a diagnosis
for the right eye?
6. What are the management options for
the right eye and was the previous
ophthalmologist justified in not
venturing likely underlying diagnostic
possibilities?
Answers
1. What is the diagnosis in the left eye?
Anterior uveitis (iritis)
2. What is the treatment for this
condition?
Topical steroids to suppress inflammation
and mydriatics to relieve pain and prevent
posterior synaechiae. Posterior synaechiae
results in a ‘fixed’ pupil caused by leakage of
protein-rich serum and cells into the
aqueous blocking the area between the pupil
margin and the anterior lens.
3. What is the likely pathology in the
right eye?
Optic atrophy. In view of the suspicion of
other neurological abnormalities in this age
group the most likely underlying diagnosis is
multiple sclerosis suggesting that the optic
atrophy is secondary to old optic neuritis.
Optic neuritis can affect any part of the
optic nerve but will only produce clinical
changes if the portion immediately adjacent
to the globe is involved. This is only the
case in a minority of cases. In an acute
attack, macular exudates are relatively
frequent if the disc is involved as protein
and lipid-rich fluid leaks through diseased
vessel walls, forming linear streaks (macular
star) as deposits track along the nerve fibre
layer. In addition, the cerebrospinal fluid
(CSF) may contain inflammatory cells.
Other important differential diagnoses in
this patient include other inflammatory
conditions such as Behcet’s disease,
congenital and hereditary optic atrophy (but
not likely in view of the recovery of this eye
and the normal fellow eye), choroiditis and
retinitis pigmentosa (again, unlikely in view
of the absence of other findings). Optic
nerve compression of the right eye and toxic
or infective conditions also seem unlikely.
4. Are the two conditions associated?
Yes. Demyelinating disease (multiple
sclerosis) is the result of aberrant leucocyte
activity in the CNS, which is embryologically
and immunologically similar to the eye.
Uveitis and multiple sclerosis are therefore
likely to represent differing targets of a
similar malfunction in the immune system
and there is a strong association of uveitis
in patients with multiple sclerosis. Because
uveitis can be treated and can result in
severe ocular pathology, it is very important
to actively exclude uveitis in any patient
with multiple sclerosis who complains of
visual loss, even in those with previous optic
neuritis and during relapses at other sites.
5. What investigations might be helpful
in establishing a diagnosis for the right
eye?
During acute CNS inflammation, lumbar
puncture to obtain CSF samples can show
antibodies and cells characteristic of disease.
In old disease or in remission this is unlikely
to yield a positive result. MRI scanning will
show current or old areas of demyelination
and is the most reliable diagnostic tool.
What are the management options for the
right eye and was the previous
ophthalmologist justified in not venturing
likely underlying diagnostic possibilities?
Up to approximately 60% of patients with
optic neuritis will go on to develop other
clinical signs of multiple sclerosis in later
life. However, the diagnosis of multiple
sclerosis is made only when two or more CNS
lesions can be demonstrated, separated by
time and anatomical site. In this patient, a
single episode of optic neuritis does not
meet the diagnostic requirements and even
speculation must be restricted. Even when
clearly diagnosed, use of specific
prophylactic and acute anti-inflammatory
treatments in multiple sclerosis is extremely
limited. During acute relapse, high dose
intravenous steroids will shorten the
duration of the attack but have no influence
on the severity of residual disability later on.
Interferon may influence the incidence of
relapse in certain subtypes of multiple
sclerosis in specific patients but there is
currently no clinical test to identify whether
a patient would benefit and the potential
costs and side-effects currently limit its use.
In this patient it would not be reasonable to
commence prophylactic interferon treatment
on the basis of a single episode of optic
neuritis.
In the absence of a firm diagnosis and in
the absence of a reliable prophylactic
treatment, the first ophthalmologist was
probably fully justified in not discussing the
potential underlying condition.
Six months later this patient suffered an
acute episode of paralysis of the right leg at
which time an MRI scan revealed multiple
areas of demyelination throughout the CNS.
He was not treated for the acute attack but
was subsequently commenced on interferon.
He has had specific career counselling and is
continuing with his career in medicine but
has decided to enter radiology as a speciality
as it was considered to be the area in which
any physical disability is least likely to affect
his career.
sponsored by
A 52 year old company director presented to
his optometrist with a two week history of
“blurring” of vision on looking to the right.
The optometrist noted that this was not
causing significant symptoms but suspected
that the patient was adopting a head turn
to the right to compensate. The optometrist
advised the patient to visit his GP as soon
as possible and gave a referral letter to the
patient to take with him which is
summarised as follows:
Vision right 6/12 unaided improving to
6/6 with +0.50/+0.50 x 75. Vision left 6/9
unaided improving to 6/6 with 0.00/+0.50 x
100. There is a right sixth nerve weakness
giving horizontal diplopia of two weeks’
duration. History of hypertension – on
treatment. Suggest urgent referral to
ophthalmologist for assessment.
The patient visited his GP two days later.
The GP countersigned the referral, asked the
patient to make an appointment at the local
hospital Early Referral Clinic and checked
the blood pressure which he found to be
slightly high at 170/100. He increased the
strength of the patient’s medication and
made an appointment to re-check the blood
pressure in 3 weeks. On contacting the
hospital, the patient was given an
appointment for 10 days which he missed as
he was away on business. He was first seen
at the hospital almost a month after the
optometrist’s consultation.
The duty SHO examined the patient. The
diplopia had subjectively improved over the
previous 2-3 weeks and was not causing
significant problems. The SHO confirmed a
right sixth nerve palsy which appeared fairly
marked, but was influenced by the history
CASE 4
of recent improvement and previous
hypertension. A diagnosis of ischaemic sixth
nerve palsy secondary to hypertension was
made. His notes also recorded normal
movement in the left eye, no pupil
abnormalities and normal optic discs with a
0.3 cup to disc ratio. The patient was given
an appointment in the orthoptic clinic for a
Hess chart to quantify the defect and a
return visit to the general clinic was made
for 1 month’s time.
The Hess chart revealed a fairly marked
right abduction deficit and a mild left
adduction weakness.
At the general clinic one month later, the
patient complained of worsening diplopia
and an alteration in the appearance of the
right side of the face. The diplopia was
particularly marked on right gaze and he
was no longer able to overcome this by
head turn to the right. The ophthalmologist
on this occasion found almost complete
right sixth nerve palsy and a marked left
adduction weakness. There was a mild right
facial nerve weakness but no other cranial
nerve signs. The site of the lesion was
re-diagnosed and MRI scans and neuro-
vascular studies performed.
Questions
1. Where is the lesion?
2. Why is the left medial
rectus involved?
3. What is the likely
underlying diagnosis?
4. Why is the clinical
condition changing?
5. What should be the advice to this
patient about driving?
Answers
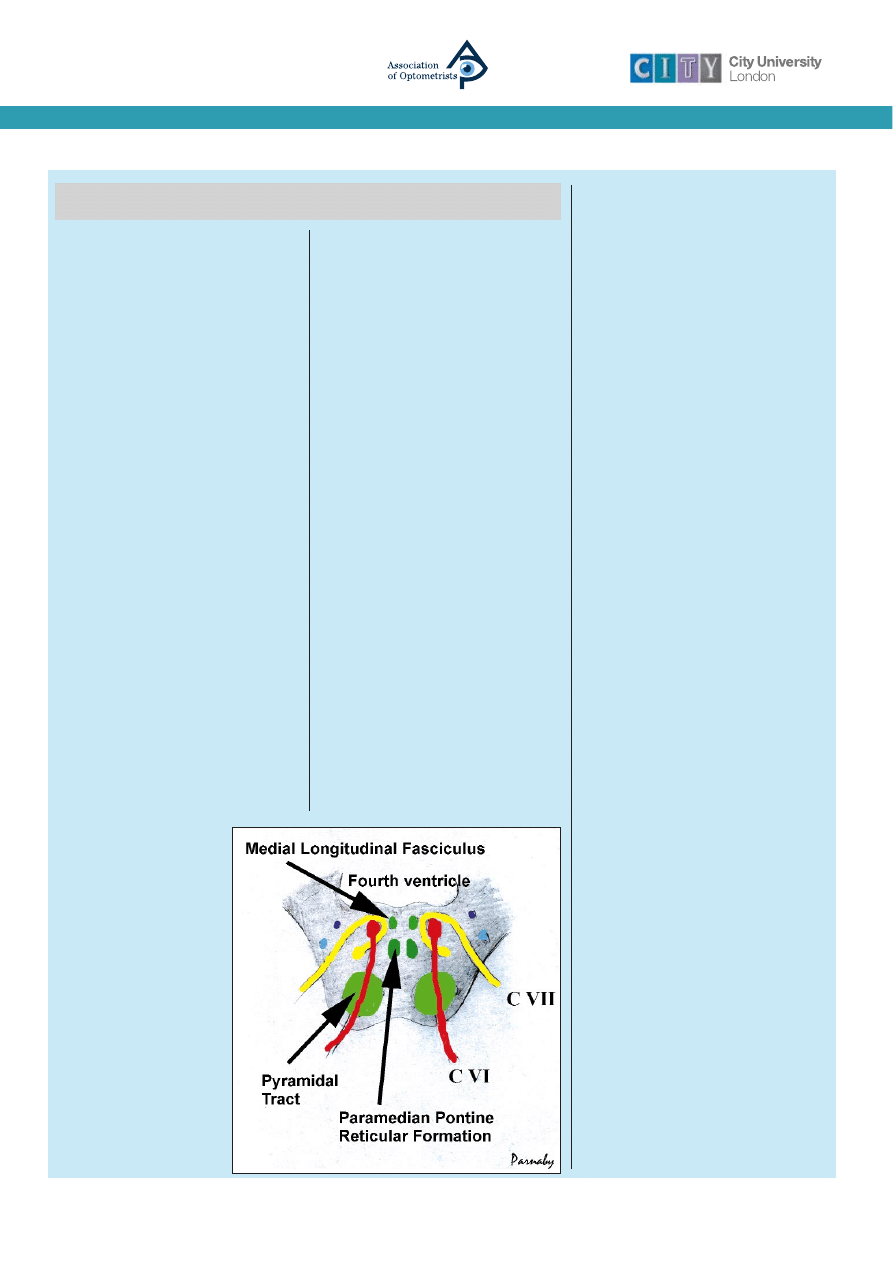
1. Where is the lesion?
Right sixth nerve nucleus. After exiting the
nucleus, there is no anatomical site which
would permit involvement of the
contralateral third nerve. The ipsilateral
seventh nerve passes backwards from its
nucleus and passes around and behind the
sixth nucleus allowing early involvement of
the seventh nerve (see Figure 4).
2. Why is the left medial rectus involved?
40% of the sixth nerve cell bodies project to
the contralateral medial rectus to cause
adduction of the fellow eye and facilitate
consensual gaze movement. Loss of this
projection therefore contributes to a gaze
palsy.
3. What is the likely underlying
diagnosis?
Ischaemia or tumour (glioma or leukaemia
deposits). In a younger age group multiple
sclerosis is also an important cause and in
children 50% of sixth nerve palsies overall
are attributable to neoplasm if trauma is
excluded.
4. Why is the clinical condition changing?
The apparent progression of the condition
strongly suggests a progressive aetiology.
The history is consistent with an early pure
right sixth nerve palsy at the presentation to
the optometrist with an early left medial
rectus weakness by the time he was first
seen in the early referral clinic which would
reduce diplopia on right gaze. As the muscle
weakness became worse, the further
reduction in right gaze and dyskinesis caused
increased symptoms. As the nuclear lesion
enlarged, the seventh nerve has become
involved.
5. What should be the advice to this
patient about driving?
The DVLC requirements for driving stipulate
that someone with diplopia may not drive a
car in the UK. Failure to contact the DVLC
with such a condition would invalidate any
insurance policies rendering the patient
liable to legal proceedings regarding fitness
to drive and driving without insurance.
In spite of an accurate anatomical
diagnosis, MRI and neurovascular imaging
failed to identify a specific lesion. A
presumptive diagnosis was made of
brainstem microvascular occlusion (limited
cerebrovascular accident (CVA)). The patient
was treated aggressively for hypertension
and hypercholesterolaemia (a risk factor for
atherosclerosis) with dietary advice and
medication including cholesterol lowering
drugs and aspirin. Six months later there has
been a slight improvement in his condition
although he remains unable to meet the
requirements for driving.
o
t
December 1, 2000 OT
www.optometry.co.uk
Figure 4
Diagram of cross-section
through lower pons
showing relationship of
sixth and seventh cranial
nerve nuclei and fascicles
36
www.optometry.co.uk
37
Module 2 Part 12
A 74-year-old retired County Council
workman presented to an optometrist after
noticing that his vision had reduced. He had
never visited an optometrist before, but was
using a pair of his late wife’s glasses.
There was some difficulty in examining
the patient due to severe spondylosis of the
neck from ankylosing spondylitis and
apparent illiteracy, but a refraction of right
+1.50/+1.00 x 90, left +2.00 DS gave an
approximate acuity of 6/12 right, 6/24 left.
Non-contact tonometry gave a reading of
22 mmHg right, 26 mmHg left. The red
reflexes were poor and the optometrist
was unable to visualise the fundus on
ophthalmoscopy. She referred the patient to
an ophthalmologist for further assessment
re glaucoma and cataracts.
There were no previous notes available in
the clinic and a routine visual field was
performed prior to clinical assessment as
shown in Figure 5. The patient stated that
he had a “cast” in the left eye as a child, but
had not noticed any problems with his
vision. He said that he had been ‘a
sharpshooter’ in the army until about 2-3
years earlier, when he had been admitted to
hospital with an illness which had “knocked
him off his feet” for a few weeks. He took no
regular medication, smoked roll-up cigarettes
and drank around 2 pints of beer daily.
Physical examination showed a thin and
frail gentleman with severe cervical
spondylosis and deep nicotine staining of
the fingers of the right hand. Goldman
tonometry was 20 mmHg right, 24 mmHg
left with moderately deep anterior
chambers, open irido-corneal angles and no
pupil defects. There was marked nuclear
sclerotic cataract in both eyes, worse in
the left, but the optic discs appeared
normal with good neural rims and small,
non-glaucomatous cups of 0.2. There was
mild retinal pigment epithelial changes in
both maculae, but clinical assessment
showed no visual defect arising from this.
Questions
1. Does the patient have glaucoma?
2. What do the visual fields show
(Figure 5) and is this consistent with
glaucoma?
CASE 5
3. Where is the lesion and what is the
likely underlying pathology?
4. Would cataracts or amblyopia in the
left eye affect the visual fields?
5. What tests would help to assess the
foveal function?
Answers
1. Does the patient have glaucoma?
No. Glaucoma is a diagnosis reached by
considering several factors including the
intraocular pressure, the integrity of the
retinal nerve fibre layer, the optic disc
neural rim (and cup extent if neural rim is
being lost) and visual fields (dependent on
the nerve fibre integrity). However,
glaucoma can be diagnosed from the
assessment of the optic disc alone, as visual
field changes are not usually evident until
substantial changes have occurred to the
disc.
Although this patient has high
intraocular pressure, there is no apparent
damage to the optic discs and the visual
fields appear not to show any defects
consistent with glaucomatous field loss. The
diagnosis in this case is of ocular
hypertension but he has a risk of about 10%
per year of progression to outright glaucoma
and will require yearly assessment to ensure
that this does not occur.
2. What do the visual fields show
(Figure 5) and is this consistent
with glaucoma?
The fields show a left homonymous
hemianopia with sparing of the left half of
the macular fields. This appearance is not
consistent with glaucoma which typically
produces arcuate scotomata arising from the
disc (=blind spot on fields). The defects
associated with glaucoma are independent
in each eye. Disc pathology (including
glaucoma) would therefore be centered
around the blind spot and would not
specifically spare the macular field. These
fields are congruous between each eye and
observe the midline based on fixation,
consistent with CNS pathology.
3. Where is the lesion and what is the
likely underlying pathology?
The field loss is to the left consistent with a
visual pathway or cortical lesion on the
right side, behind the chiasm. The macular
sparing is the critical localising feature
suggesting that the visual cortex serving the
macula (occipital tip) is spared (i.e. the
middle cerebral artery is intact) whilst the
visual cortex serving midperipheral and
peripheral fields (mesial surface of the
occipital lobe) have been compromised.
These are supplied by the middle cerebral
and posterior cerebral artery respectively,
suggesting that this patient has experienced
occlusion of his right posterior cerebral
artery, possibly during his illness two-three
years earlier (which may have been a
stroke). Smoking is a particular risk factor
for all kinds of vascular problems and poor
healthcare suggests that hypertension and
hypercholesterolaemia need to be excluded.
4. Would cataracts or amblyopia in the
left eye affect the visual fields?
Cataracts reduce perceived brightness but
the relatively good acuity suggests that
they are not seriously interfering with vision
in this patient. In other cases, severe
cataract and amblyopia may both affect the
absolute values of the test but the relative
loss of sensitivity in the visual field of each
eye individually should be able to show
visual defects clearly. In this instance, with
dense field defects, the problem should be
easy to identify. The history of good vision
in the army previously cannot be relied
upon unless corroborated by a reliable
examiner in writing. Marksmen use their
right eyes for sighting and even a relatively
dense amblyopia in the left may be missed
completely!
5. What tests would help to assess the
foveal function?
Foveal function is assessed by a variety of
measurements including acuity, colour vision
(including Ishihara colour charts) and
central fields. Specific tests include the
ability to see a red laser aiming dot when it
is focused on the fovea and the Watske-
Allen test where a slit lamp beam is
centered on the fovea and the subject is
asked whether it is complete or whether
there is a central break or distortion
consistent with abnormality, failure or loss
of the fovea (e.g. in macular oedema or
macular hole).
The patient proceeded to left cataract
surgery which improved acuity to 6/12
unaided at first postoperative visit. He
seemed pleased with the result although the
field loss remained. He defaulted from a
second follow-up appointment. His GP
visited him at home and wrote that the
patient has declined further ophthalmic
attention, as he is “most satisfied with his
position”.
Figure 5 Visual fields of patient of the patient
sponsored by

1. Which one of the following medical
conditions is a likely cause of a
retinal haemorrhage?
a. Diabetes mellitus
b. Diabetes insipidus
c.
Clotting factor 8 deficiency (von
Willebrand’s disease)
d. Platelet deficiency
2. Which one of the following
statements is incorrect?
Patients with myaesthenia gravis:
a. Have an increased risk of other
autoimmune diseases
b. Have antibodies against acetylcholine
receptors in the end-plates of sensory
nerve fibres
c.
May require surgery to control disease
d. Are likely to present initially to an
eye specialist
3. Which one of the following
statements is correct?
Patients with multiple sclerosis:
a. Are more likely to suffer with
episcleritis
b. May improve their prognosis with
aggressive immunosuppression during
acute attacks (relapses)
c.
May suffer peri-ocular pain during
relapses
d. Often become acutely photophobic
with acute optic neuritis
4. Which one of the following
statements is incorrect?
a. A pupil sparing third nerve palsy is
likely to be due to a compressive
lesion
b. Consensual eye movements are aided
by sixth nucleus projections to the
contralateral medial rectus
c.
An esotropia may be caused by a
sixth nerve palsy
d. A third nerve lesion with early
involvement of the pupil is likely to
be compressive
5. Which one of the following
statements is correct?
Parasympathetic anisocoria
is most easily seen:
a. in dim indoor light
b. in bright indoor light
c.
in daylight
d. at night-time
6. Which one of the following
statements is correct?
With regard to glaucoma:
a. An intraocular pressure of more than
40mmHg alone is diagnostic of
glaucoma
b. Can be diagnosed from assessment of
the optic disc alone
c.
Is unlikely to be severe if the visual
fields are unaffected
d. 1% of ocular hypertensives will
progress to outright glaucoma
7. Which one of the following
statements is incorrect?
In optic neuritis:
a. There is usually disc swelling,
hyperaemia and haemorrhages
b. There may be macular exudates
c.
The disc may be normal
d. There may be an associated
alteration in CSF composition
8. Which one of the following
statements regarding uveitis is
incorrect?
a. Uveitis can affect pupil movements
b. Uveitis is associated with multiple
sclerosis
c.
Topical steroids reduce the
inflammation that occurs in
uveitis
d. Miotics should be prescribed to
prevent posterior synaechiae
9. Which one of the following
statements regarding the seventh
nerve is incorrect?
a. Lower Motor Neurone involvement of
the seventh nerve will result in facial
hemiparesis.
b. The seventh nerve passes backwards
from its nucleus
c.
Anatomically, the seventh nerve is in
close proximity to the sixth nucleus
d. Pathology of the seventh nerve will
result in deafness
10. Which one of the following
statements is incorrect?
a. Internuclear ophthalmoplegia may be
mimicked by myaesthenia gravis
b. Multiple sclerosis is a cause of
internuclear ophthalmoplegia
c.
Pupil abnormalities are a common
feature of internuclear
ophthalmoplegia
d. The pupils are normal in myaesthenia
gravis
11. Which one of the following
statements is incorrect?
a. In children, 10% of sixth nerve palsies
are attributable to neoplasm if trauma
is excluded
b. 40% of the sixth nerve cell bodies
project to the contralateral medial
rectus
c.
Multiple sclerosis is a cause of sixth
nerve palsies
d. Disc swelling and peripapillary
haemorrhage are early features of
raised intracranial pressure
12. Which one of the following
statements is correct?
a. Macular sparing in occipital CVA
(stroke) suggests involvement of the
middle cerebral artery
b. Cataracts rarely give rise to formal
visual field defects
c.
Visual acuity is usually significantly
reduced in a CVA affecting the tip of
the right occipital lobe
d. A left hemianopia may be caused by a
glaucomatous loss of the temporal
right optic disc
Multiple choice questions -
Neurology and the eye - Case histories
An answer return form is included in this issue.
It should be completed and returned to:
CPD Initiatives (NOE12),
OT, Victoria House, 178–180 Fleet Road, Fleet,
Hampshire, GU13 8DA by January 10, 2001.
Please note there is only ONE correct answer
38
o
t
December 1, 2000 OT
www.optometry.co.uk
ABOUT THE AUTHOR
Adrian Parnaby-Price is a
Consultant in Ophthalmic Surgery
at St George’s Hospital, London
sponsored by
Wyszukiwarka
Podobne podstrony:
Botox, Migraine, and the American Academy of Neurology
Gods Eye Aerial Photography and the Katyn
Mettern S P Rome and the Enemy Imperial Strategy in the Principate
More Than Meets The Eye New Feats
Diet, Weight Loss and the Glycemic Index
Ziba Mir Hosseini Towards Gender Equality, Muslim Family Laws and the Sharia
pacyfic century and the rise of China
Danielsson, Olson Brentano and the Buck Passers
Japan and the Arctic not so Poles apart Sinclair
Pappas; Routledge Philosophy Guidebook to Plato and the Republic
Legions of the Eye
Pragmatics and the Philosophy of Language
Haruki Murakami HardBoiled Wonderland and the End of the World
SHSBC388?USE LEVEL OT AND THE PUBLIC
Doping in Sport Landis Contador Armstrong and the Tour de Fran
drugs for youth via internet and the example of mephedrone tox lett 2011 j toxlet 2010 12 014
Nouns and the words they combine with
więcej podobnych podstron