1
Introduction to Maternity,
Newborn, and Women’s
Health Nursing
unit
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 1
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 2

Contemporary Issues and
Trends in Maternal, Newborn,
and Women’s Health
Key
TERMS
abortion
certified nurse midwife
(CNM)
doula
empowerment
ethics
family-centered care
health indicators
infant mortality rate
intrauterine fetal surgery
maternal mortality rate
nurse practice acts
Learning
OBJECTIVES
After studying the chapter content, the student should be able to
accomplish the following:
1. Define the key terms.
2. Identify the current trends in health care that affect women.
3. Outline the barriers that women have in accessing health care.
4. List three women’s health care indicators and how they are being addressed.
5. Describe the nursing implications of current trends in women’s health care.
6. Discuss the role of the nurse throughout the life cycle continuum.
Key
Learning
1
chapter
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 3

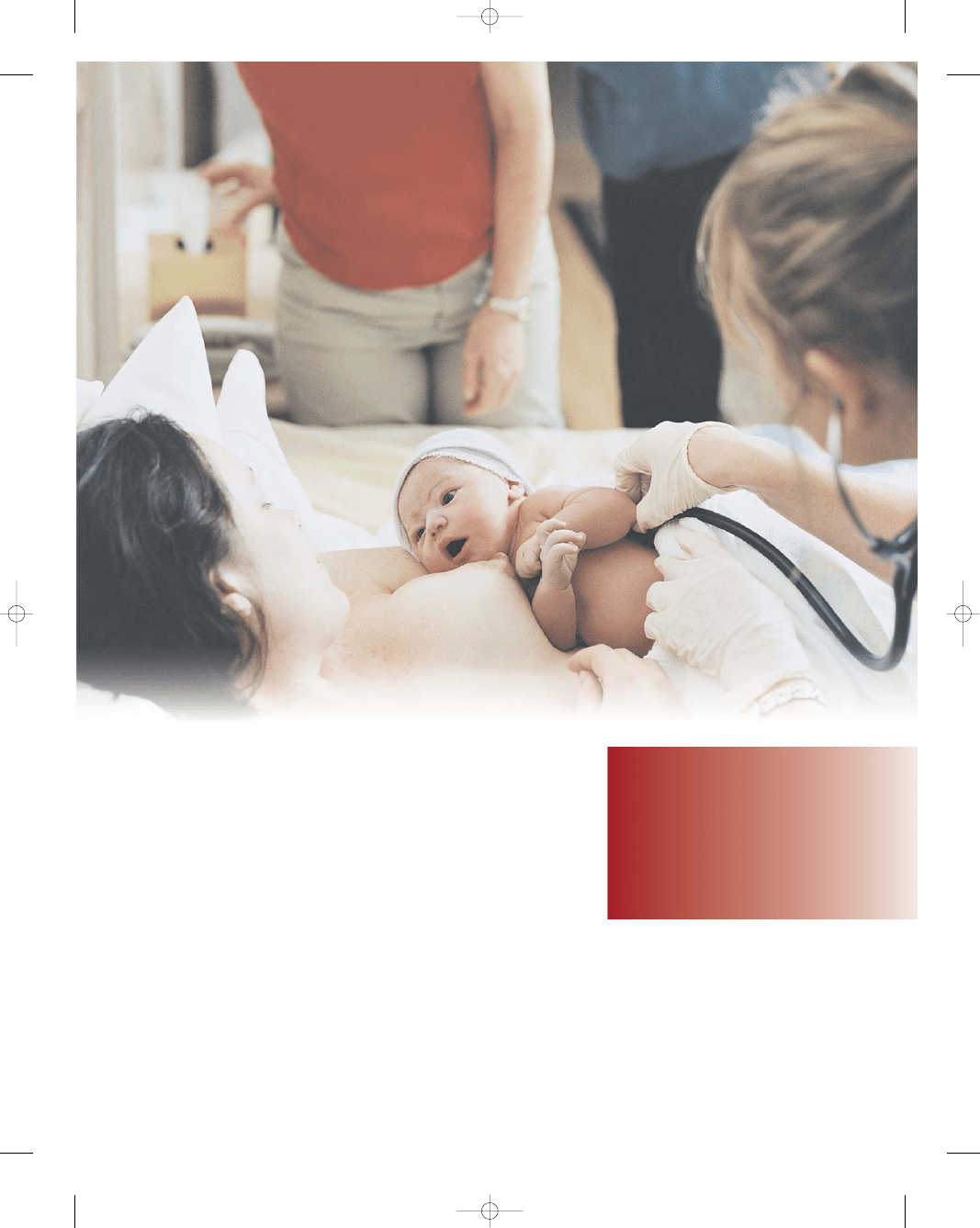
wow
person’s ability to lead a fulfilling
life and to participate fully in society depends largely on
his or her health status. This is especially true for women,
who often shoulder the combined burden of child rear-
ing, family health care, and career building. To fulfill her
responsibility to her loved ones, a woman must first care
for her own personal health.
Now more than ever, nearly every health care experi-
ence involves the contribution of a nurse. From birth to
death, and every health care emergency in between, will
likely involve the presence of a nurse. A knowledgeable,
supportive, comforting nurse often results in a superior
health care experience. Skilled nursing practice depends
on a solid base of knowledge and clinical expertise deliv-
ered in a caring, holistic manner. It is imperative that
nurses use their knowledge and passion to reach out to
their patients. They must help meet every woman’s health
care needs regardless of where a woman is in her life cycle
continuum. Nurses can help their patients to live health-
ier lives by providing emotional support, comfort, infor-
mation, advice, advocacy, support, and family counseling.
This chapter presents a general overview of issues
and trends in health care with which nurses often grapple
in caring for families with children. Nurses must know
how to approach these issues in a knowledgeable and sys-
tematic way to reduce conflict and to provide profes-
sional care.
Maternal and Women’s Health
Care Perspectives
Past Trends
Centuries ago, granny midwives handled the normal
birthing process for most women. Their training was
obtained through an apprenticeship with a more experi-
enced midwife. Most doctors only participated in child-
birth in the most extreme cases of difficulty. All births
took place in the home setting.
Childbirth in colonial America was a difficult and
sometimes dangerous experience. During the 17th and
18th centuries, women giving birth died as a result of
exhaustion, dehydration, infection, hemorrhage, or sei-
zures (Lehrman, 2003). In addition to her anxieties about
pregnancy, an expectant mother was filled with apprehen-
sions about the death of her newborn child. The death of
a child during infancy was far more common than it is
today. Approximately 50% of all children died before the
age of five (Lehrman, 2003). This can be compared with
the 0.07%
infant mortality rate
of today, which is a dra-
matic improvement (World Factbook, 2003).
During the early 1900s, physicians attended about half
the births in the United States. Midwives often cared for
women who could not afford a doctor. Most women were
attracted to hospitals because these institutions offered
pain management that was not available in home births.
Natural childbirth practices advocating birth without med-
ication and focusing on relaxation techniques were intro-
duced in the 1950s. These techniques opened the door to
childbirth education classes and helped bring the father
back into the picture. Both partners were participating
in the whole family experience by taking an active role in
pregnancy, childbirth, and parenting (Fig. 1-1).
During the 1960s, consumer organizations formed and
advocated for family-centered maternity care (FCMC).
The International Childbirth Education Association
Being pregnant and giving birth are like crossing a narrow bridge. People can accompany
you to the bridge. They can greet you on the other side. But you walk that
bridge alone. . . .
A
A
B
●
Figure 1-1
Today, fathers and partners are welcome to
take an active role in the pregnancy and childbirth experience.
(A) Couples can participate together in childbirth education
classes. (Photo by Gus Freedman.) (B) Fathers and partners
can assist the woman throughout her labor and delivery.
(Photo by Joe Mitchell.)
4
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 4
(ICEA), the American Society for Psychoprophylaxis in
Obstetrics (ASPO), and the National Association of
Parents and Professionals for Safe Alternatives in Child-
birth (NAPSAC) all stressed a strong commitment to fam-
ily values and responsibility in childbearing. In the 1970s,
female consumers and women health professionals chal-
lenged many assumptions of the obstetric system and
demanded new models of care delivery. From the 1980s
to the present, increased access to care for all women
(regardless of their ability to pay) and new hospital
redesigns (labor, delivery, and recovery [LDR] rooms;
and labor, delivery, recovery, and postpartum [LDRP]
spaces) to keep “families together” during the childbirth
experience breathed new life into FCMC (Fig. 1-2).
Family-centered care
is the delivery of safe, sat-
isfying, quality health care that focuses on and adapts to
the physical and psychosocial needs of the family. It is a
cooperative effort of families and other caregivers that
recognizes the strength and integrity of the family. The
basic principles of family-centered care are as follows:
•
Childbirth is considered a normal, healthy event in the
life of a family.
•
Childbirth affects the entire family and relationships will
change.
•
Families are capable of making decisions about their own
care if given adequate information and professional sup-
port (Murray et al., 2002).
FCMC is based on the premise that the family is the
constant. Family members support one another well
beyond the health care provider’s brief time with them
during the childbearing process. FCMC views birth as a
normal life event, rather than a medical procedure. The
core values of FCMC that need to be integrated into all
nursing care provided to families include mutual respect
and trust of all parties, “informed choice” used by the
family,
empowerment
of the family unit, collaboration
in all decision making, and flexibility, quality, and indi-
vidualized care for all family members (Phillips, 2003).
In many ways, childbirth practices in the United
States have come full circle, as we see the return of nurse
midwives and doulas.
Certified nurse midwives
(CNMs)
have postgraduate training in the care of normal
pregnancy and delivery, and are certified by the American
College of Nurse Midwives (ACNM). A
doula
is a birth
assistant who provides quality emotional, physical, and
educational support to the woman and family during
childbirth and the postpartum period. Childbirth choices
are often based on what works best for the mother, child,
and family. Box 1-1 summarizes a time line of childbirth
in America.
Current Trends
Modern women are often faced with multiple responsi-
bilities that compete for their time and attention, includ-
ing the health of their parents, their children, and their
partner. These responsibilities may decrease a woman’s
ability to tend to her own mental and physical health
(nutrition, exercise, leisure activities, and so forth). A
woman who neglects her health may have to deal with the
consequences for the remainder of her life.
Today women are part of an evolving health care
delivery system. The cost of health care is soaring and the
federal government, insurance agencies, hospitals, and
health care providers are joining together in an attempt
to bring it under control. Several changes in the health
care arena have resulted, many of which have brought
about an increasingly complex health care system. Many
people feel “lost in the maze.”
Health care functions within the parameters of a mar-
ket setting, offering goods and services that carry cost to
health care consumers and patients. If a woman is preg-
nant, diabetic, and needs to go to an endocrinologist, she
Chapter 1
CONTEMPORARY ISSUES AND TRENDS IN MATERNAL, NEWBORN, AND WOMEN’S HEALTH
5
A
B
●
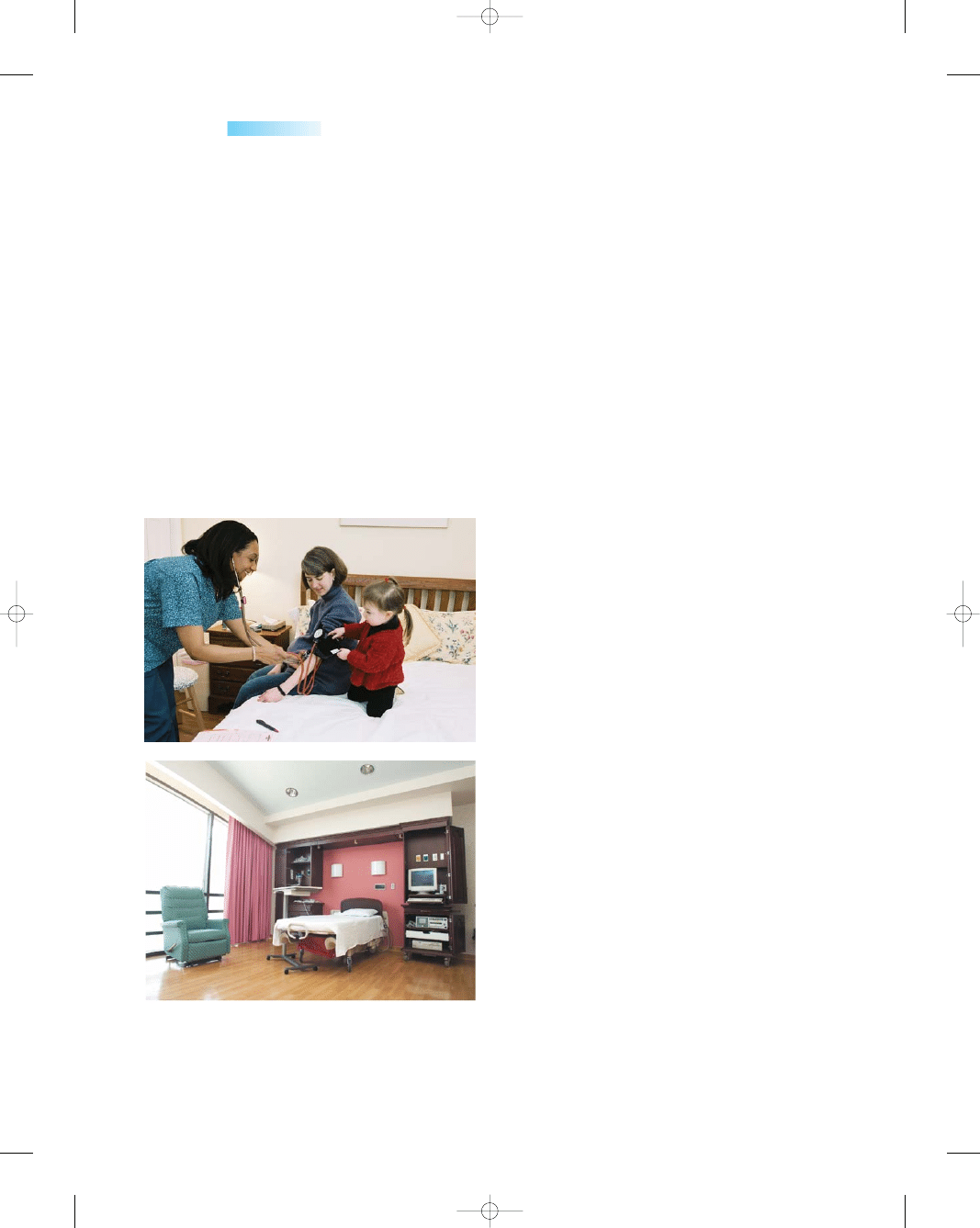
Figure 1-2
Many different settings are available for
prenatal care, labor, and delivery. (A) Birthing centers and
(B) labor, delivery and recovery (LDR) rooms have inviting,
home-like atmospheres and encourage family-centered care.
(A, Photo by Gus Freedman; B, photo by Joe Mitchell.)
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 5
has very little choice except to purchase the services needed
or go without care. In the managed care environment of
health care today, the woman will need to go through her
“primary health care professional” or “gatekeeper” to
receive a referral to a specialist. Often she must trust her
primary provider to make that choice for her, instead of
making that decision on her own.
The best managed care principles value a compre-
hensive approach with a focus on prevention, early inter-
vention, and continuity of care. The goal is to consider
the merit of services, procedures, and treatments in view
of the resources available, thus the gatekeeper role, which
ensures that care is timely and necessary. In a perfect
world, all women would receive necessary quality care
throughout their lives, but we don’t live in the perfect
managed care world. With cost-cutting strategies, there
are many implications for women:
•
Decreased length of hospital stay for newborns and
high-risk neonates, which is often met by increased at-
home care given by women as caretakers
•
Loss of continuity of care and an establishment of a
trusting relationship with her health care provider when
the insurance plan does not cover the same provider she
may have been receiving care from for years
•
Potential prohibition of OB/GYN physicians from mak-
ing referrals for specialists if they are not classified as pri-
mary physicians (gatekeepers)
•
Restricting clinical judgment that impacts quality and
individualization of care, which may potentially increase
mother and infant morbidity by dictating length of stay
in the hospital when more observation and nursing care
are needed
•
Restricting the number and type of diagnostic studies
ordered by the health care provider, which may jeopar-
6
Unit 1
INTRODUCTION TO MATERNITY, NEWBORN, AND WOMEN’S HEALTH NURSING
1700s
Men did not attend births, because it was consid-
ered indecent.
Women faced birth, not with joy and ecstasy, but
with fear of death.
Female midwives attended the majority of all
births at home.
1800s
There is a shift from using midwives to doctors
among middle class women.
The word obstetrician was formed from the Latin,
meaning “to stand before.”
Puerperal (childbed) fever was occurring in
epidemic proportions.
Louis Pasteur demonstrated that streptococci
were the major cause of puerperal fever that
was killing mothers after delivery.
The first cesarean section was performed in
Boston in 1894.
The x-ray was developed in 1895 and was used to
asses pelvic size for birthing purposes
(Feldhusen 2003).
1900s
Twilight sleep (a heavy dose of narcotics and
amnesiacs) was used on women during child-
birth in the United States.
The United States was 17th out of 20 nations in
infant mortality rates.
Fifty to 75% of all women gave birth in hospitals
by 1940.
Nurseries were started because moms could not
care for their baby for several days after receiv-
ing chloroform gas.
Dr. Grantley Dick–Reed (1933) wrote a book
entitled Childbirth Without Fear that reduced
the “fear–tension–pain” cycle women experi-
enced during labor and birth.
Dr. Fernand Lamaze (1984) wrote a book entitled
Painless Childbirth: The Lamaze Method that
advocated distraction and relaxation techniques
to minimize the perception of pain.
Amniocentesis is first performed to assess fetal
growth in 1966.
In the 1970s the cesarean section rate was about
5%. By 1990 it rose to 24%, where it stands
currently (Martin, 2002).
The 1970s and 1980s see a growing trend to return
birthing back to the basics—nonmedicated,
nonintervening childbirth.
In the late 1900s, freestanding birthing centers—
LDRPs—were designed, and the number of
home births began to increase.
2000s
One in four women undergo a surgical birth
(cesarean).
CNMs once again assist couples at home, in hos-
pitals, or in freestanding facilities with natural
childbirths. Research shows that midwives are
the safest birth attendants for most women,
with lower infant mortality and maternal rates,
and fewer invasive interventions such as epi-
siotomies and cesareans (Keefe 2003).
Childbirth classes of every flavor abound in most
communities.
According to the latest available data, the United
States ranks 21st in the world in maternal
deaths. The maternal mortality rate is approxi-
mately 7 in 1000 live births.
According to the latest available data, the United
States ranks 27th in the world in infant mortality
rates. The infant mortality rate is approximately
7 in 1000 live births (United Nations, 2003).
BOX 1-1
CHILDBIRTH IN AMERICA: A TIME LINE
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 6
dize the health and well-being of the newborn and
mother, and precludes the parents from making decisions
about future pregnancy events (Youngkin & Davis, 2004)
Other trends in the health care system include
•
Changing demographics—an aging population
•
Economic forces that affect resources
•
Profound growth of technology and information
•
Proliferation of unlicensed assistive personnel provid-
ing health care
•
Communications and cultural issues associated with
the increasingly diverse needs of multicultural patients
•
Shortages of trained health care professionals
•
Movement of health care away from acute settings into
the community
Currently, the problem surmounting all health care
considerations is cost. Although cost containment is impor-
tant to restrain spiraling health care spending, costs and
efforts to contain them should not affect the quality or
safety of care delivered. The old saying that “an ounce of
prevention is worth a pound of cure” has been shown to
lower costs significantly. Mammograms, cervical cancer
screenings, prenatal care, and smoking cessation programs
are a few examples that yield positive outcomes and reduce
overall health care costs. Using technologic advances to
diagnose and treat breast cancer early positively saves lives
as well as fiscal resources.
Nurses can be leaders in providing quality care within
a limited-resource environment by stressing to the women
for whom they care the importance of making healthy
lifestyle and food choices, seeking early interventions for
minor problems before they become major ones, and edu-
cating themselves about health-related issues that affect
them so they can select the best option for themselves
and their families. Prevention services and health edu-
cation are the cornerstones of delivering quality women’s
health care.
These are just a few of the changes in the health care
system that consumers face when they need services.
These dramatic changes present a significant opportunity
for the nursing profession. Nurses who clearly articulate
their role in this changing environment will be able to help
their patients to navigate this increasingly complicated
health care system.
Future Trends/Needs
for Women’s Health
Based on our changing demographics concerning age,
ethnic background, education, workforce participation,
and booming childbearing statistics, the future trend for
women’s health will need to
•
Broaden the focus on women’s health, not just during
pregnancy, but throughout the entire life cycle
•
Integrate women’s and perinatal health services to com-
pensate for poor coordination of services by increasing
numbers of OB/GYNs being designated primary care
providers
•
Expand comprehensive, integrated programs and ser-
vices addressing women’s unique needs across their
life span
•
Offer better provider education about the consequences
of chronic health problems as well as enlighten all women
about better lifestyle choices to prevent the progression of
chronic conditions
•
Promote social policies that ensure economic security
and health care insurance coverage for women
•
Recognize sociocultural differences that affect women’s
caregiving roles, domestic violence, access to health infor-
mation, lifestyle preferences, autonomy to make health
decisions, and learning/motivation for health prevention
and promotion activities
•
Focus scientific research for more specific drug treat-
ments for breast cancer, osteoporosis, autoimmune dis-
eases, and menopause
•
Develop better diagnostic procedures for heart disease,
diabetes, arthritis, lupus, inflammatory diseases, and
detection of genetic disorders earlier
•
Support health care educational programs to increase
entry of diverse-culture students to provide a broad
range of women’s health services
Health Care Indicators
Health indicators
are used to measure the health of
the nation. They are global in nature and provide each
country with guidelines to assess their own health sta-
tus. General global health indicators include infant mor-
tality rate, at-risk birth weight, potential years of life
lost, life expectancy, disability-free life expectancy, and
self-rated health status (Osei et al., 2003). The lead-
ing health indicators reflect the major health concerns in
the United States at the beginning of the 21st century.
These indicators were selected on the basis of their abil-
ity to motivate action, the availability of data to measure
progress, and their importance as public health issues
(Healthy People 2010). The current leading health indi-
cators include
•
Physical activity
•
Overweight and obesity
•
Tobacco use
•
Substance abuse
•
Responsible sexual behavior
•
Mental health
•
Injury and violence
•
Environmental quality
•
Immunization
•
Access to health care (Healthy People 2010)
The objectives of Healthy People 2010 are categorized
according to the health indicators. Healthy People 2010 is
a broad-based, collaborative federal and state initiative that
Chapter 1
CONTEMPORARY ISSUES AND TRENDS IN MATERNAL, NEWBORN, AND WOMEN’S HEALTH
7
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 7
has set national disease prevention and health promotion
objectives to be achieved by the end of the decade. The
initiative has two goals: to increase the quality and years
of healthy life and to eliminate health disparities among
Americans. An example of health disparity exists in peo-
ple with disabilities. Just because these individuals were
born with an impairing condition or have experienced
a disability or injury that has long-term consequences
does not negate their need for health promotion and dis-
ease prevention. In fact, their need for health-promoting
behaviors is accentuated. Many women with disabling
conditions such as lupus, rheumatoid arthritis, multiple
sclerosis, or osteoporosis do not view themselves as
disabled, despite immense physical limitations. Nurses
need to remember that wellness is the lens of their self-
perception. The accompanying Healthy People 2010
box highlights national health goals for maternal and
infant health.
Mortality Rates
The federal government has pledged to improve maternal–
child care outcomes and thus reduce the statistics of mor-
tality rates for both women and children. The
maternal
mortality rate
counts the number of deaths from any
cause during the pregnancy cycle per 100,000 live births.
In the United States, the maternal mortality rate is 7.5. The
infant mortality rate counts the number of deaths of infants
younger than one year of age per 1000 live births. In the
United States, the infant mortality rate is 7.0 (Centers for
Disease Control and Prevention [CDC], 2004, National
Center for Health Statistics [NCHS], 2005).
During the past several decades, mortality and
morbidity have dramatically decreased as a result of an
increased emphasis on hygiene, good nutrition, exercise,
and prenatal care for all women. However, women and
infants are still experiencing complications at significant
rates. The United States is one of the most medically and
technologically advanced nations and has the highest
per-capita spending on health care in the world, yet cur-
rent mortality rates in the United States indicate the
need for continued improvement.
A few facts might help present a clearer picture:
•
The current maternal mortality rate is approximately 7.5
maternal deaths per 100,000 live births (CDC, 2004).
•
The current infant mortality rate is approximately 7.0
infant deaths per 1,000 live births (CDC, 2004;
NCHS, 2005).
•
Two to three women die in the United States every day
from pregnancy complications, and more than 30% of
pregnant women (1.2 million women annually) expe-
rience some type of illness or injury during childbirth
(CDC, 2004).
•
The United States ranks 21st (below 20 other countries)
in rates of maternal deaths (deaths per 100,000 live
births).
•
The United States ranks 27th (below 26 other countries
with a population of at least 2.5 million) in rates of infant
deaths (deaths per 100,000 live births; United Nations,
2003). One reason cited for the high infant mortality rate
in the United States is the high rate of very-low-birth-
weight births in the country relative to other developed
countries (NCHS, 2005).
•
Most pregnancy-related complications are preventable.
The most common are ectopic pregnancy, preterm labor,
hemorrhage, emboli, hypertension, infection, stroke, dia-
betes, and heart disease.
•
The leading causes of pregnancy-related mortality for the
years 1991 to 1999 (the last years for which data are avail-
able) are embolism (20%), hemorrhage (17%), preg-
nancy-related hypertension (16%), and infection (13%;
CDC, 2003).
•
More than half of all infant deaths in 2002 were attribut-
able to five leading causes: congenital malformations
(20%), disorders relating to short gestation and unspeci-
8
Unit 1
INTRODUCTION TO MATERNITY, NEWBORN, AND WOMEN’S HEALTH NURSING
✓
✓
✓
✓
✓
✓
✓
✓
✓
✓
✓
✓
✓
✓
✓
✓
✓
✓
HEALTHY PEOPLE
2010
National Health Goals—Maternal and Infant Health
Goal:
Reduce fetal and infant deaths.
Goal:
Reduce maternal deaths.
Goal:
Reduce maternal illness and complications
resulting from pregnancy.
Goal:
Increase the proportion of pregnant women
who receive early and adequate prenatal care.
Goal:
Increase the proportion of pregnant women
who attend a series of prepared childbirth classes.
Goal:
Increase the proportion of very low-birth
weight (VLBW) infants born at level III hospitals or
subspecialty perinatal centers.
Goal:
Reduce cesarean births among low-risk
(full-term, singleton, vertex presentation) women.
Goal:
Reduce low birth weight (LBW) and VLBW.
Goal:
Reduce preterm births.
Goal:
Increase the proportion of mothers who
achieve a recommended weight gain during their
pregnancies.
Goal:
Increase the percentage of healthy, full-term
infants who are laid down to sleep on their backs.
Goal:
Reduce the occurrence of developmental
disabilities.
Goal:
Reduce the occurrence of spina bifida and
other neural tube defects (NTDs).
Goal:
Increase the proportion of pregnancies
begun with an optimum folic acid level.
Goal:
Increase abstinence from alcohol, cigarettes,
and illicit drugs among pregnant women.
Goal:
Reduce the occurrence of fetal alcohol
syndrome (FAS).
Goal:
Increase the proportion of mothers who
breast-feed their babies.
Goal:
Ensure appropriate newborn bloodspot
screening, follow-up testing, and referral to services.
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 8
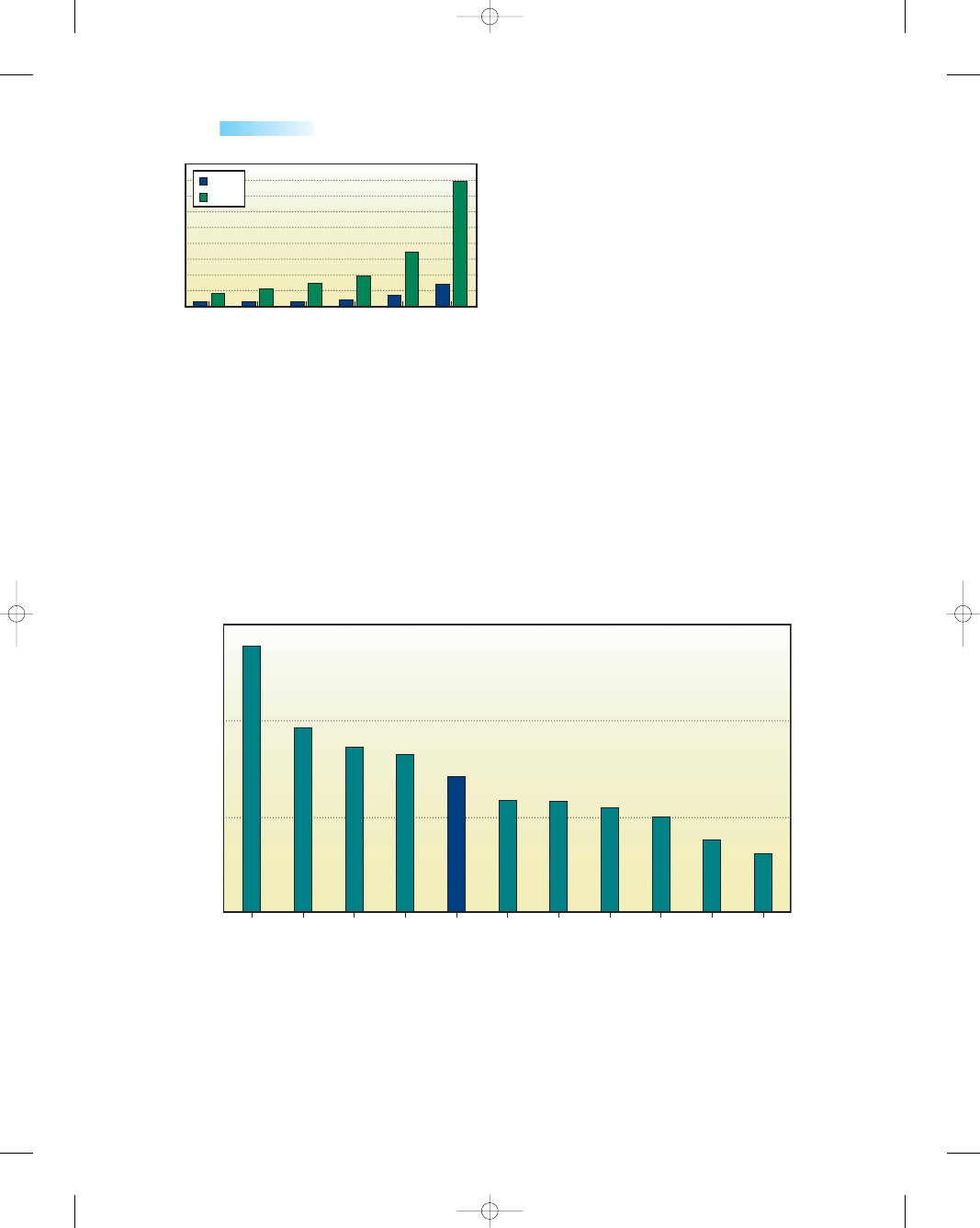
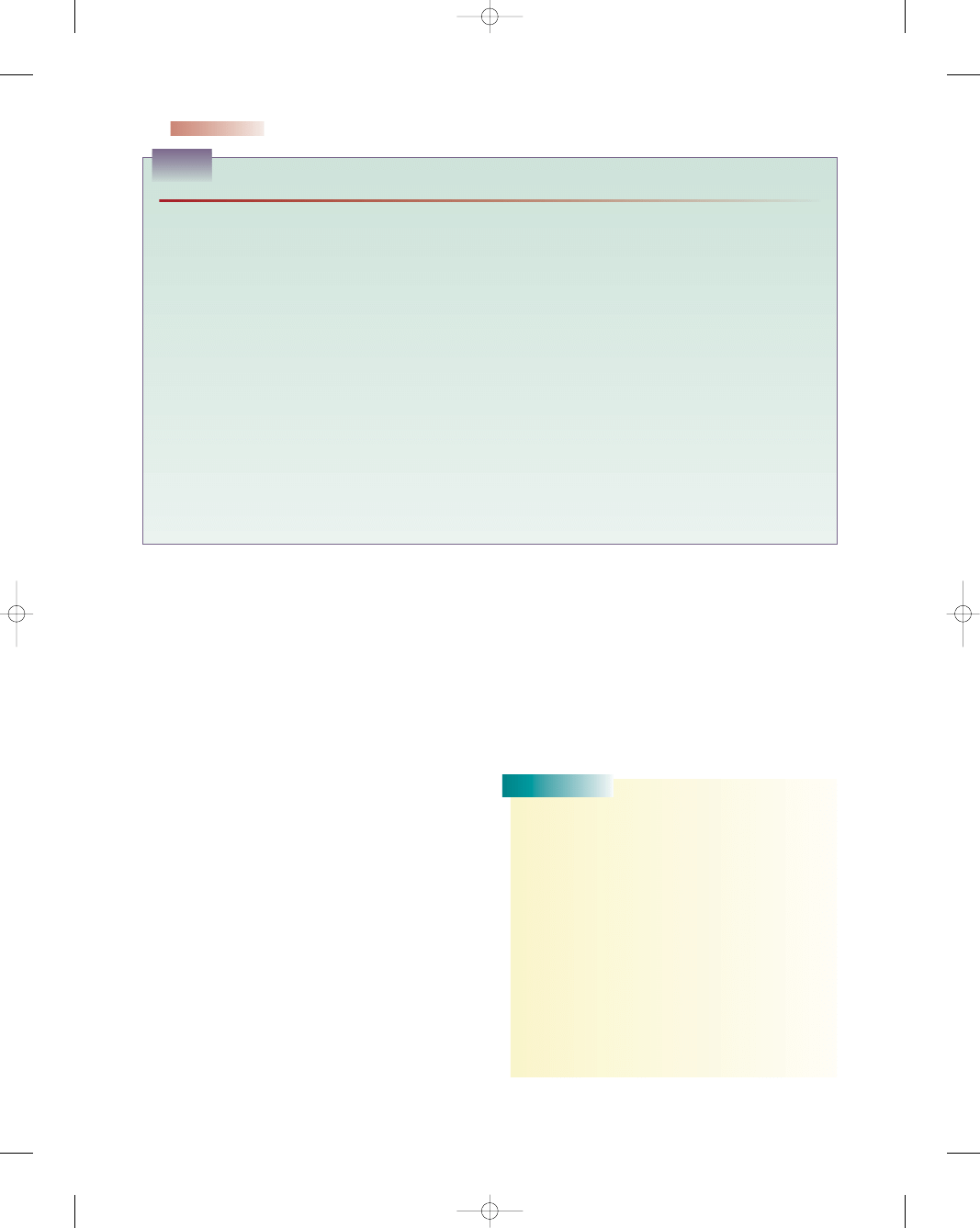
•
Infant mortality rates are higher for African-American,
Latin-American, and Native American babies. The rate
for African-American babies is twice that of white babies
(Keefe, 2003; Fig. 1-4).
Why is there such disparity within the United States?
The problem is multifaceted, but lack of care during preg-
nancy is a major contributing factor to a poor outcome.
Prenatal care is well known to prevent complications of
pregnancy and to support the birth of healthy infants.
Unfortunately, not all women are able to receive the same
quality and quantity of health care during a pregnancy.
More than 40% of African-American, Native American,
and Latino women do not obtain prenatal care during
their first trimester of pregnancy (Condon, 2004).
Several of the risk factors that contribute to high mor-
tality rates can be lessened or prevented with good precon-
ception and prenatal care. First, preconception screening
and counseling offer an opportunity to identify maternal
risk factors before pregnancy begins. Examples include
daily folic acid consumption (a protective factor) and alco-
hol use (a risk factor). During preconception counseling,
health care providers can also refer women for medical and
psychosocial or support services for any risk factors identi-
fied. Counseling should be culturally appropriate and lin-
guistically proficient.
Chapter 1
CONTEMPORARY ISSUES AND TRENDS IN MATERNAL, NEWBORN, AND WOMEN’S HEALTH
9
20–24
25–29
Age group (yrs)
30–34
35–39
≥
40
≤
19
0
20
40
60
80
100
120
140
160
180
White
Black
Ratio
* Deaths per 100,000 live births.
●
Figure 1-3
Pregnancy-related mortality ratios by race and
age, United States, 1991–1999. (Retrieved May 2005 from
http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5202a1.htm.)
Race/Ethnicity
Black
non-
Hispanic
Hawaiian
†
Japanese
†
Chinese
†
Cuban
§
Filipino
†
American
Indian
†
Mexican
§
Puerto
Rican
§
0
5
10
15
13.9
9.6
8.6
8.2
7.0
5.8
5.7
5.4
4.9
3.7
3.0
Ratio
Total U.S. White,
non-
Hispanic
* Per 1,000 live births.
†
Can include persons of Hispanic and non-Hispanic origin.
§
Persons of Hispanic origin may be of any race.
●
Figure 1-4
Infant mortality rates by selected racial/ethnic populations—United States,
2002. (Retrieved May 2005 from http://www.cdc.gov/mmwr/preview/mmwrhtml/
mm5405a5.htm.)
fied LBW (17%), sudden infant death syndrome (SIDS;
8%), newborns affected by maternal complications of
pregnancy (6%), and newborns affected by complications
of placenta, cord, and membranes (4%) (Martin et al.,
2005).
•
The maternal mortality and morbidity rates for African-
American women have been three to four times higher
than for whites (Chang, 2003; Fig. 1-3).
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 9
Prenatal visits offer an opportunity to provide infor-
mation about the adverse effects of substance use and
serve as a vehicle for referrals to treatment services. The
use of timely, high-quality prenatal care can help to pre-
vent poor birth outcomes and improve maternal health by
identifying women who are at particularly high risk, and
then can be used to take steps to reduce risks, such as the
risk of high blood pressure or diabetes. Interventions tar-
geted at prevention and cessation of substance use during
pregnancy may be helpful in further reducing the rate of
preterm delivery and LBW. Continued promotion of folic
acid intake can help to reduce the rate of NTDs.
In addition, providing access to quality prenatal care
for all pregnant women without ability to pay will help
reduce the mortality rates tremendously. Access to family
planning services can also play a major role in preventing
maternal deaths by reducing health risks associated with
unplanned pregnancy.
Maternal mortality rates are nearly four times higher
for women of color than for white women (Keefe, 2003).
Researchers do not entirely understand what accounts for
these disparities, but some suspected causes of higher
maternal mortality rates for minority women include low
socioeconomic status, limited or no insurance coverage,
bias among health care providers (which may foster dis-
trust), and quality of care available in the community.
Language and legal barriers may also add to the various
reasons why some immigrant women do not receive good
prenatal care.
After birth, other health promotion strategies can sig-
nificantly improve an infant’s health and chances of sur-
vival. Breast-feeding has been shown to reduce rates of
infection in infants and to improve long-term maternal
health. Emphasizing to mothers that they should place
their infants on their backs to sleep will help reduce the
incidence of SIDS. Encouraging mothers to join support
groups to prevent postpartum depression and gain assis-
tance with sound child-rearing practices will help toward
improving the health of both mothers and their infants.
The CDC has called the disparity in maternal mortal-
ity rates in women of color and white women “one of the
largest racial disparities among public health indicators”
(CDC, 1999, p. 493). They have called for more research
and monitoring to understand and address the racial dis-
parities, along with increased funding for prenatal and post-
partum care. Not enough is known about the causes of
racial disparities in maternal and infant health, so addi-
tional research is needed to identify causes and design ini-
tiatives to reduce these disparities. In addition, the CDC is
calling on Congress to expand programs to provide pre-
conception and prenatal care to underserved women to
address the racial disparities.
The Health Resources and Services Administration
(HRSA)’s Maternal and Child Health Bureau (MCHB)
has primary federal responsibility for improving the health
of mothers and children in the United States. More than
27 million infants, children, and pregnant women are
served by an MCHB program annually (Dyck et al., 2003).
A few of their programs and initiatives to improve the
health of mothers, infants, and children and to reduce
mortality rates are described in Box 1-2.
The Report Card on Women’s Health
Women of today face not only diseases of genetic origin
but also diseases that arise from poor personal habits as
well. Even though women represent 51% of the popula-
tion, only recently have researchers and the medical com-
munity focused attention on the special health needs
of women. One significant study that was published in
August 2000 assessed the overall health of women at the
state and national level. It identified an urgent need to
improve women’s access to health insurance and health
care services, place a stronger emphasis on prevention,
and invest in more research on women’s health (National
Women’s Law Center [NWLC] et al., 2000).
The study identified several health care indicators that
measure women’s access to health care services. It mea-
sured the degree to which women receive preventive health
care and engage in health-promoting activities (Box 1-3).
The report card gave the nation an overall grade of
“unsatisfactory,” and not a single state received a grade
of “satisfactory.” Among the other substandard findings
were the following:
•
No state has focused enough attention on preventive
measures, such as smoking cessation, exercise, nutri-
tion, and screening for diseases.
10
Unit 1
INTRODUCTION TO MATERNITY, NEWBORN, AND WOMEN’S HEALTH NURSING
• Healthy Start—through community outreach, home
visitation, and a network of support services, targets
the poorest neighborhoods where the likelihood of
maternal and infant mortality and LBW is highest.
• Health and Human Services (HHS) Interagency Council
on Low Birth Weight—has been established to promote
multidisciplinary research on LBW and preterm births,
scientific exchange, policy initiatives, and collaboration
among HHS agencies.
• Food fortification—along with the national campaign to
educate women about the preventive benefits of taking
folic acid, has resulted in decreases in the prevalence
of spina bifida and anencephaly.
• Increased research—concerning genetic, environmental,
and behavioral factors that have an influence on
pregnancy outcomes for mother and infant is being
undertaken.
• CDC’s Pregnancy Risk Assessment Monitoring System
(PRAMS)—is an ongoing, state-specific surveillance
system designed to identify and monitor select maternal
behaviors and experiences before, during, and after
pregnancy. PRAMS surveillance now covers approxi-
mately two thirds of all US births (Dyck et al., 2003).
BOX 1-2
MCHB PROGRAMS AND INITIATIVES
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 10

•
Too many women lack health insurance coverage.
Nationally, nearly one in seven women (14%) have no
health insurance.
•
No state has adequately addressed women’s health
needs in the areas of reproductive health, mental health,
and violence against women.
•
Limited research has been done on health conditions
that primarily affect women and that affect women dif-
ferently than men (NWLC et al., 2000).
Cardiovascular Disease (CVD)
Poor health habits affect all women. Smoking, drug abuse,
high cholesterol, and obesity lead to high mortality and
morbidity rates in our nation. CVD is the number one
cause of death of women, regardless of racial or ethnic
group. Approximately 500,000 women die annually in the
United States of CVD, equaling a rate of about one death
per minute (Alexander et al., 2004) Women who endure a
heart attack are more likely than men to die and oftentimes
are more difficult to diagnose than men because of their
vague and varied symptoms. Heart disease is still thought
of as a “man’s disease” and thus is not considered as a
diagnosis when a woman presents to the emergency room.
The common perception held by many nurses that
CVD is a man’s disease could cost women their lives.
Many nurses believe erroneously that only men need to
worry about heart attacks and stroke, but CVD is an equal-
opportunity killer. Consider these myths:
•
Breast cancer kills more women than CVD.
•
CVD is more deadly in men.
•
Men and women experience the same symptoms.
Now examine the facts about CVD:
•
CVD is the number one killer of women and stroke is
number three.
•
One in 10 women age 45 to 64 has some form of CVD.
•
CVD is more challenging to diagnose in women than
men.
•
One of two American women dies of CVD, whereas 1 in
30 dies of breast cancer.
•
Approximately 35% of heart attacks in women go unno-
ticed or unreported.
•
Health care professionals do not take CVD symptoms
seriously in women.
•
Heart attack is twice as deadly in women as men
(American Heart Association [AHA], 2004).
Nurses need to take heed and look beyond the obvi-
ous “crushing chest pain” textbook symptom that heralds
a heart attack in men, because women present much dif-
ferently and the diagnosis is missed if CVD is not on their
radar screen of possibilities. Look for the following risk
factors in women:
•
Cigarette smoking
•
Smoking and use of oral contraceptives or hormone
replacement therapy
•
Obesity
•
Consuming a diet high in saturated fats
•
Stress
•
Sedentary lifestyle
•
Hypertension
•
Hyperlipidemia
•
Strong family history
•
Diabetes mellitus
•
Postmenopausal
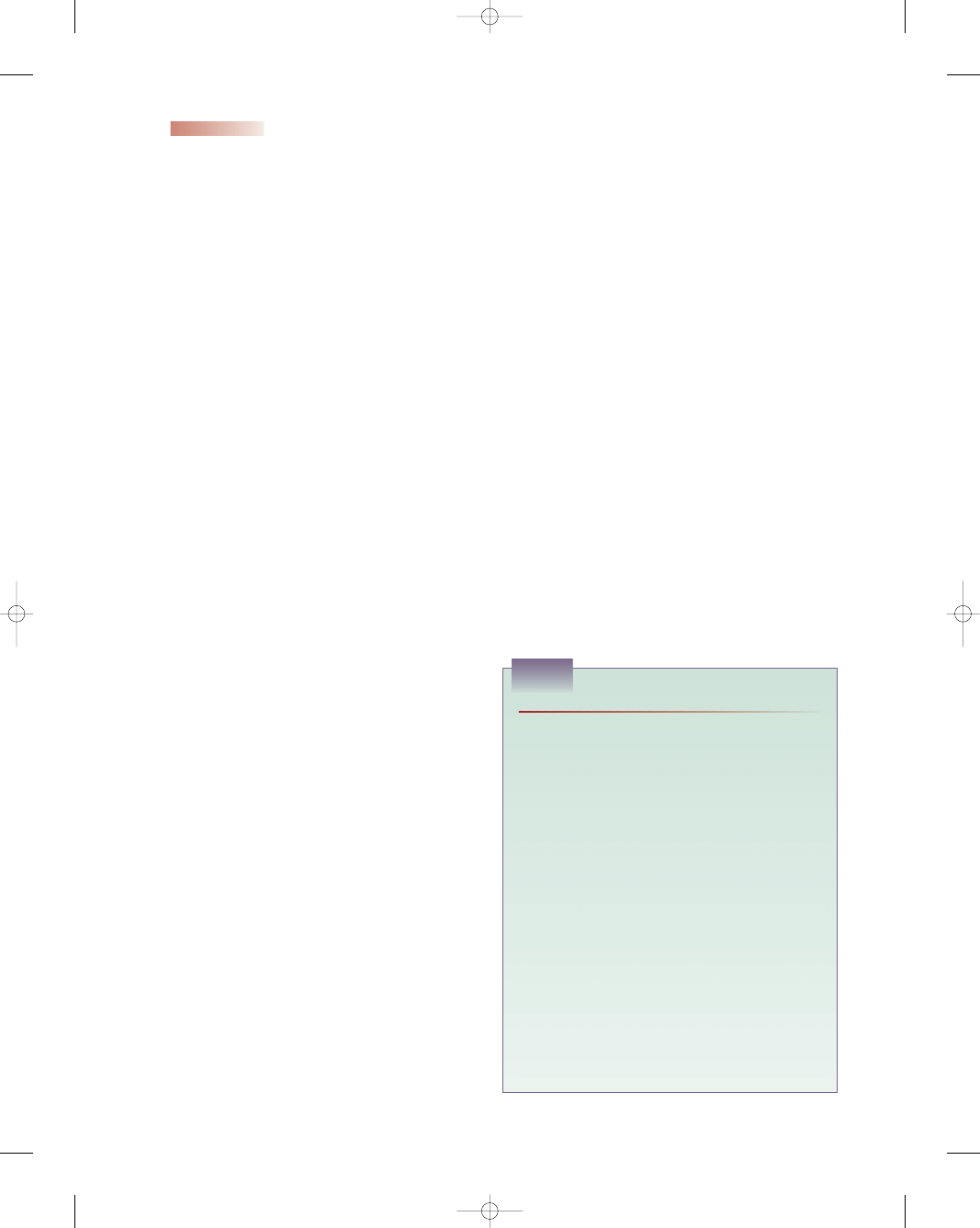
Figure 1-5 presents a sample health risk assessor to help
nurses and patients assess the patient’s risk of heart attack.
Consider CVD as a possibility in women who present
with any of the following clinical symptoms: chest dis-
comfort in the center of the chest that goes away and
comes back (can be described as pressure, squeezing,
or feeling of fullness); discomfort in one or both arms
or shoulders, the back, neck, jaw, or stomach; shortness
of breath; nausea; lightheadedness; breaking out in a cold
sweat; paleness; atypical abdominal pain; and unexplained
fatigue (AHA, 2004).
Prevention efforts to reduce the number victims of
CVD in women include
•
A low-cholesterol, low-fat diet
•
Aspirin therapy and treatment of hypertension
•
Daily exercise
•
Achieving an ideal weight
•
Smoking cessation measures
•
Cholesterol-lowering agents
•
Stress management (Condon, 2004)
Chapter 1
CONTEMPORARY ISSUES AND TRENDS IN MATERNAL, NEWBORN, AND WOMEN’S HEALTH
11
• Lung cancer death rate
• Diabetes
• Heart disease death rate
• Binge drinking
• High school completion
• Poverty
• Wage gap
• Rate of AIDS
• Maternal mortality rate
• Rate of Chlamydia infection
• Breast cancer death rate
• Heart disease death rate
• Smoking
• Being overweight
• No physical activity during leisure time
• Eating five fruits and vegetables daily
• Colorectal screening
• Mammograms
• Pap smears
• First trimester prenatal care
• Access to health insurance
BOX 1-3
THE NATIONAL INDICATORS OF WOMEN’S HEALTH
Adapted from National Women’s Law Center, FOCUS/University of
Pennsylvania, the Lewin Group. (2000). Making the grade on women’s
health: a national state-by-state report card. Washington, DC: National
Women’s Law Center.
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 11
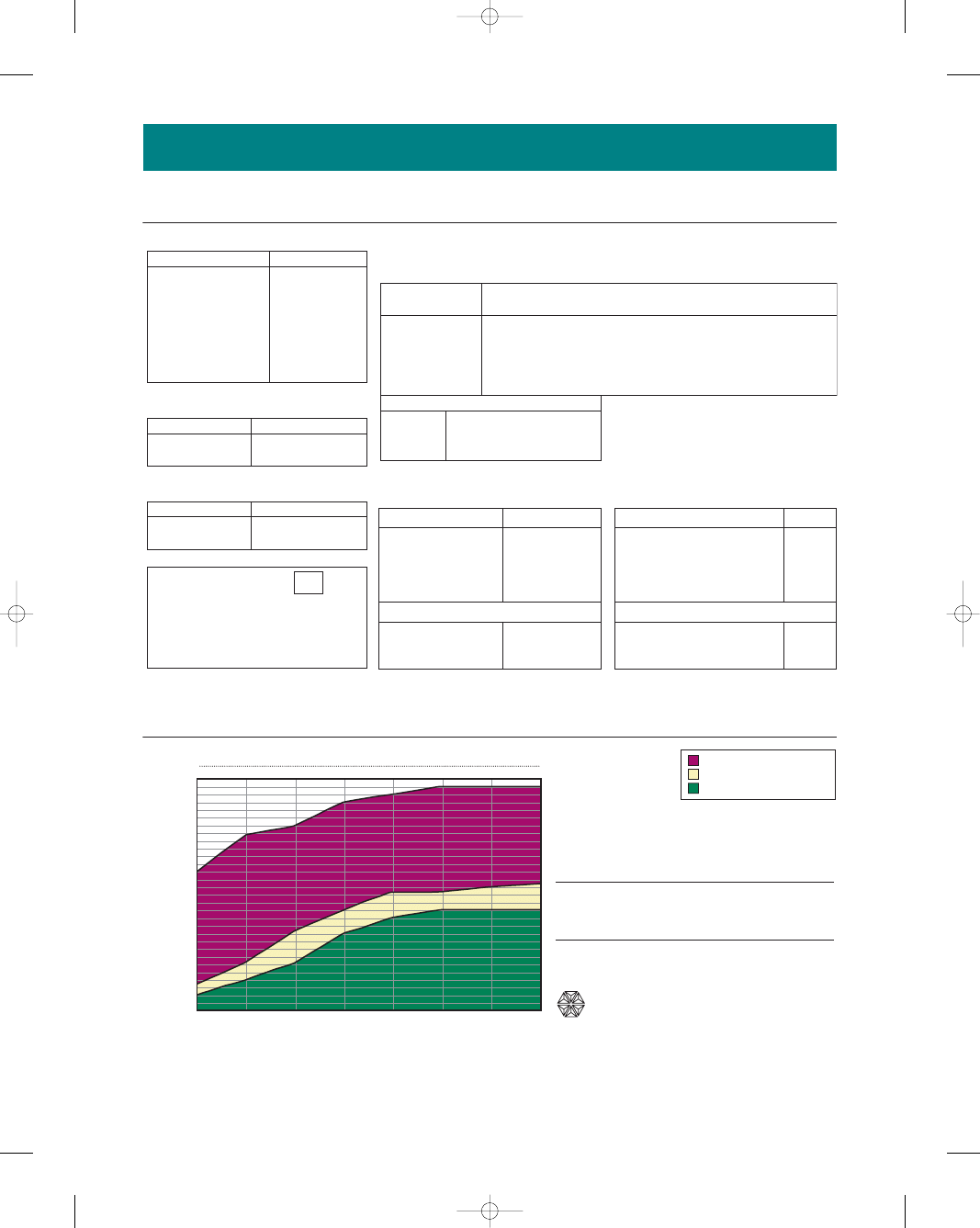
65–69
70+
D3-F091-7-99
© 1999 Bristol-Myers Squibb Company, Princeton NJ 08543
60–64
55–59
Score on Risk Assessment
50–54
45–49
40–44
Below are some easy-to-complete questions about your health and lifestyle that will help you assess your risk of a heart
attack. The questions are designed to encourage discussion with your healthcare professional. Circle your points for each
risk factor. Add them up and place your total points in the box. Then use the graph below to determine your risk.
The red zone indicates a higher than average risk for a
heart attack. The yellow zone indicates an average risk
for a heart attack. It is desirable for you to be in the
lower or green zone, which indicates a lower than
average risk of a heart attack.
1. HOW OLD ARE YOU?
2. DO YOU SMOKE?
35 – 39
120 – 129
160 – 199
35 – 44
45 – 49
50 – 59
200 – 239
240 – 279
280 and over
60 and over
Low
Low
Use the Heart Risk Assessor as a general guide. If you have already had a heart attack or have heart disease, your heart attack risk is
significantly higher. Only your healthcare professional can evaluate your risk and recommend treatment plans to reduce your risk.
If you don’t know your cholesterol level or blood pressure, ask your healthcare professional if your levels should be checked.
Normal
High
High
Average
Low
High
Average
5. WHAT IS YOUR TOTAL CHOLESTEROL
LEVEL?
Systolic
Less than 120
Less than 160
Less than 35
130 – 139
140 – 159
160 or more
40 – 44
45 – 49
50 – 54
55 – 59
60 – 64
65 – 69
70 and over
Age
Points
Points
Points
Points
Points
HDL (good) cholesterol (mg/dL)
Total cholesterol (mg/dL)
Don’t know, but I have been told it is:
Don’t know, but I have been told it is:
Don’t know, but I have been told it is:
–4
0
Heart Risk Assessor — Women
3
6
7
8
8
8
Yes
No
Yes
No
2
4
0
0
4
0
3. DO YOU HAVE DIABETES?
Now determine your risk. To do this, use
the graph. Find your score on the left,
run your finger across the line to match
your age, and place an X at this point.
Score (Total Points)
4. WHAT IS YOUR BLOOD PRESSURE?
Look up your points on the table below. Your systolic pressure (higher number) is on the
left and your diastolic pressure (the lower number) is along the top.
Diastolic
79 or less
90 – 99
100 or more
85 – 89
80 – 84
–3
–3
–2
–2
0
0
1
1
5
5
1
1
1
3
3
0
0
0
2
2
3
0
0
0
2
3
0
0
0
2
3
2
2
2
2
3
3
3
3
3
3
6. WHAT IS YOUR HDL (GOOD)
CHOLESTEROL LEVEL?
–3
–3
2
Heart Attack Risk Groups, Women Age 35 and Older
Heart Attack
Risk*
35–39
Age Group
0
5
10
20
26
–4
Higher Than Average Risk
Lower Than Average Risk
Average Risk
If you have already had a heart attack or have heart disease,
your heart attack risk is significantly higher. Only your health-
care professional can evaluate your risk and recommend
treatment plans to reduce your risk.
* Risk estimates were derived from the results of the Framingham
Heart Study
Provided as an educational service from
Bristol-Myers Squibb Company
●
Figure 1-5
Sample Health Risk Assessor form to help detect the risk for heart attack in
women. (Used with permission from Bristol-Myers-Squibb Company.)
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 12
Cancer
Cancer falls as the second leading cause of death among
women (Grantham, 2002). Women have a one in three
lifetime risk of developing cancer, and one out of every four
deaths is from cancer (Alexander et al., 2004). Although
much attention is focused on cancer of the reproductive
system, lung cancer is the number one killer of women.
This is largely the result of the higher rates of smoking by
women as well as the effects of second-hand smoke. Lung
cancer has no early symptoms, making early detection
almost impossible. Because of this, lung cancer has the
lowest survival rate of any cancer. More than 90% of peo-
ple who get lung cancer die of the disease (Breslin & Lucas,
2003).
Breast cancer occurs in one in every eight women in a
lifetime, with more than 183,000 women diagnosed annu-
ally in the United States. It is the most common malig-
nancy in women, and second only to lung cancer as a cause
of cancer mortality in women (American Cancer Society
[ACS], 2004). Although a positive family history of breast
cancer, aging, and irregularities in the menstrual cycle at
an early age are major risk factors, others include excess
weight, not having children, oral contraceptive use, exces-
sive alcohol consumption, a high-fat diet, and long-term
use of hormone replacement therapy (ACS, 2003). Early
detection and treatment appear to be the best chance for a
cure, and reducing the risk of cancer by decreasing avoid-
able risks continues to be the best preventive plan.
Improving Women’s Health
What can we do as a nation to improve the health of
women? There is no single answer to address the multi-
tude of issues that were identified in the state-to-state
study. Women’s health is a complex issue, and no single
policy is going to change the overall dismal state ratings.
Some policies may include
•
Expand health care to the uninsured
•
Overcome barriers to accessing care
•
Address the issue of violence toward women
•
Focus on wellness and prevention education programs
Although progress in science and technology have
helped reduce the incidence and improve survival rates in
several diseases, women’s health issues continue to have
an impact on our society. By eliminating or decreasing
some of the risk factors and causes for prevalent diseases
and illnesses, society and science could solve certain
chronic health problems. By focusing on the causes and
effects of particular illnesses, many women’s health issues
of today could be resolved.
Social Issues
Many social issues influence health care, including poverty,
limited access to health care (especially prenatal care), and
violence against women. These issues and possible inter-
ventions as they relate to nursing care are discussed next.
Poverty and Women
Despite many global economic gains during the last cen-
tury, poverty continues to grow, and the gap between rich
and poor is widening. Major gaps continue between the
economic opportunities and status afforded to women and
those offered to men. A disproportionate share of the bur-
den of poverty rests on women’s shoulders and under-
mines their health. For example:
•
70% of the 1.2 billion people living in poverty are female.
•
Iron deficiency anemia, which is a direct result of malnu-
trition and poverty, affects twice the number of women
compared with men.
•
Half a million women die needlessly from pregnancy-
related complications annually, the causes of which
are exacerbated by issues of poverty and geographic
remoteness.
•
On average, women are paid 30% to 40% less than
men for comparable work (World Health Organization
[WHO], 2000).
Poverty, particularly for women, is more than mone-
tary deficiency. Women continue to lag behind men in
control of cash, credit, and collateral. Other forms of
impoverishment may include deficiencies in literacy, edu-
cation, skills, employment opportunities, mobility, and
political representation, as well as pressures on their avail-
able time and energy linked to their role responsibilities.
These poverty factors may diminish a woman’s develop-
ment and affect her health status (WHO, 2000).
Barriers to Accessing Health Care
Women are the major consumers of health care services,
in many cases negotiating not only their own care, but
also that of their family members. Compared with men,
women have a greater rate of health problems, longer life
spans, and more significant reproductive health needs.
Their access to care is often complicated by their dis-
proportionately lower incomes and greater responsibil-
ities, juggling work and family concerns.
The Kaiser Women’s Health Study (Salganicoff et al.,
2002) surveyed approximately 4000 women between the
ages of 18 to 64 and found that their health care needs
were not being met, especially for women of color, those
who are poor, and those who are uninsured.
For many, affordability of care is a major concern. A
significant portion of women cannot afford to go to the
doctor and fill their drug prescriptions, even when they
have insurance coverage. Many health insurance plans do
not include prescription coverage and thus the person
must pay “out of pocket” (Box 1-4).
According to the Kaiser Women’s Health Study
(Salganicoff et al., 2002), women also have issues about
Chapter 1
CONTEMPORARY ISSUES AND TRENDS IN MATERNAL, NEWBORN, AND WOMEN’S HEALTH
13
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 13
the quality of care they receive. More than one in five
women (22%) expressed concerns about the quality of
care compared with 17% of men. This issue was a partic-
ular problem for women in fair or poor health (40%).
Almost one in five women (18%) changed providers
within the past five years because of dissatisfaction with
care and concerns over quality—twice the rate of men
(Salganicoff et al., 2002). Because access to health care is
often unstable, relationships with health care providers are
often short lived, resulting in care that can be spotty and
disjointed (Salganicoff et al., 2002).
The value of prenatal care has been extensively doc-
umented in the literature as being equated with better
pregnancy outcomes. The proportion of women begin-
ning prenatal care during the first trimester of pregnancy
remained stable at 83.2% in 2000 (US Department of
Health and Human Services, 2002). However, finances,
transportation, language and/or cultural barriers, clinic
hours, and poor attitudes of the health care workers often
limit women’s access to prenatal care.
Financial Barriers
Financial barriers are one of the most important factors
that limit care. Many women have limited or no health
care and simply cannot afford the insurance. Although
Medicaid covers prenatal care in most states, the paper-
work and enrollment process is so burdensome that many
women do not register.
Transportation
Transportation to and from appointments can be challeng-
ing for patients who do not drive or own a car or cannot use
public transportation. The frequency of prenatal health
care visits can be quite burdensome, compounding the
transportation issue. The transportation issue becomes
even more difficult if the woman has small children that she
must take along with her. These challenges can prevent the
pregnant patient from making her scheduled appointments.
14
Unit 1
INTRODUCTION TO MATERNITY, NEWBORN, AND WOMEN’S HEALTH NURSING
• Low-income women were twice as likely (23%) as those with
higher incomes (10%) to have fair or poor health status.
• Low-income women 45 to 64 years old reported
49% had arthritis
41% had hypertension
32% had anxiety or depression
• Latinos were the most likely to report poor health (29%).
• African-American women were most likely to report
activity limitations (16%).
• African-American women (45–64 years old) reported
hypertension (57%) and arthritis (40%).
• One in six Latino and African-American women
(45–64 years old) were diagnosed with diabetes during
the past five years.
• One in three low-income women have no health insurance.
• Fifty-seven percent of uninsured women work either
full- or part-time.
• Thirty-seven percent of Latino women are without
insurance coverage.
• One in seven women reported their insurance plans did not
provide adequate coverage to meet their health care needs
• One half of low-income women delayed or never
received treatment because of lack of approval for
treatment or tests.
• Seventeen percent of women did not have a regular
health provider; 46% of uninsured women did not have
a regular provider; and 31% of Latinos and 24% of low-
income women lacked a regular provider.
• Seventeen percent of women of color reported they had
difficulty communicating with their provider and left the
office.
• Latino (31%) and uninsured (24%) women experienced
access problems and barriers to care, and were least likely
to have had a doctor visit within the past year.
• Women on Medicaid (40%), Latino women (38%),
and African-American women (27%) were more likely
to rely on hospital clinics and health centers for health
care.
• Uninsured women were consistently less likely than
women with private coverage to obtain any recom-
mended preventive screening tests (Salganicoff et al.,
2002).
BOX 1-4
THE KAISER WOMEN’S HEALTH STUDY HIGHLIGHTS
Consider
THIS!
I was a 17-year-old pregnant migrant worker needing pre-
natal care. Although my English wasn’t good, I was able
to show the receptionist my “big belly” and ask for ser-
vices. All the receptionist seemed interested in was a social
security number and health insurance—neither of which I
had. She proceeded to ask me personal questions con-
cerning who the father was and commented on how
young I looked. The receptionist then “ordered” me in a
loud voice to sit down and wait for an answer by someone
in the back, but never contacted anyone that I could see.
It seemed to me like all eyes were on me while I found an
empty seat in the waiting room. After sitting there quietly
for over an hour without any attention or answer, I left.
Thoughts:
Why did she leave before receiving any
health care service? What must she have been feel-
ing during her wait? Would you come back to this
clinic again? Why or why not?
Consider
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 14
Language Barriers
Language is how people communicate with each other to
increase their understanding or knowledge base. If a
health care worker cannot speak the same language as the
client or does not have a trained interpreter available, a
barrier is created. This language barrier might prevent the
client from accessing prenatal care that could increase the
chances affecting the pregnancy outcome. Frequently,
communication between people who speak the same
language can be misinterpreted.
Cultural Barriers
Culture is the sum of the beliefs and values that are
learned, shared, and transmitted from generation to gen-
eration by a particular group. Cultural beliefs and values
vary among different groups, and nurses must be aware,
understand, and respect cultural beliefs different from
their own. Nurses who feel their cultural values and pat-
tern of behavior are superior (ethnocentrism) frequently
set up barriers that inhibit diverse cultures from receiving
prenatal health care.
Clinic Hours
Clinic hours must meet the needs of the patients, not the
health care providers who work there. Evening and/or
weekend service hours might be needed to meet the work-
ing client’s schedule. It is important to evaluate the avail-
ability and accessibility of the offered service.
Poor Attitudes of Health Care Workers
Some health care workers exhibit negative attitudes toward
poor and/or culturally diverse families, which could pro-
hibit women from seeking health care. Long delays, hur-
ried examinations, and rude comments by staff might
increase a patient’s level of discomfort with the health care
team and may discourage return appointments.
Violence and Women
Violence against women is a major health concern—one
that costs the health care system millions of dollars and
thousands of lives. Violence affects women of all ages,
ethnic backgrounds, races, educational levels, socioeco-
nomic levels, and all walks of life. Nurses often come in
contact with abused women, but fail to identify, acknowl-
edge, or report the abuse. Pregnancy is often a time when
physical abuse starts or escalates, resulting in poorer out-
comes for the mother and the baby. Assessing for abuse
carries the responsibility of listening for and following up
on a possible incidence of abuse. Nurses serve their
clients best by not trying to rescue them, but by helping
them build on their strengths, providing support, and
thereby empowering them to help themselves. All nurses
need to include “RADAR” in every client visit (Box 1-5).
For a thorough discussion of violence and women, see
Chapter 9.
Legal and Ethical Issues
Law and
ethics
are interrelated and affect the entire
nursing practice. Professional nurses must understand
the limits in their scope of practice, standards of care,
institutional or agency policies, and state laws. Every
nurse is responsible for knowing current information
regarding ethics and laws related to their practice. Three
sources of rules and regulations provide guidelines for
safe and legal nursing practice:
1. State
Nurse Practice Acts
2. Standards of Care set by the American Nurses Asso-
ciation (ANA)
3. Policies and procedures set by the employer
Ethics provide rules and principles that can be used
for resolving ethical dilemmas. The ANA recently revised
their code of ethics (ANA, 2001), which should guide
nurses in their ethical practice. Ethical decisions in mater-
nal health frequently involve maternal–fetal conflict,
in which the status of the fetus as a person is still being
debated. In maternity care, the ethical assumption is made
that the pregnant woman’s decision regarding medical
intervention will be beneficial to both the expectant mother
and her fetus. This is not always the case when the mother’s
needs or wishes may injure the fetus. Abortion, sub-
stance abuse, and fetal therapy are examples that might
bring about ethical conflict to all involved in the decisions
that influence that family unit.
Throughout the world, effects of violence, abuse, as
well as rape confront nurses daily in their practice settings.
Women are the primary victims of these “human crimes.”
Clearly, these acts harm women, and nurses need to look
to the ethical principle of nonmaleficence to justify action.
The principle of nonmaleficence asserts an obliga-
tion not to inflict harm on others. It is usually translated
as, “First, do no harm.” Once nurses are convinced that
these abusive acts violate the principle of nonmaleficence,
they can turn to their own ANA code of ethics for guid-
ance (ANA, 2001).
According to the ANA code of ethics, nurses have an
ethical duty to respect the dignity and human rights of
other persons and to treat them with compassion regard-
less of health condition, ethnicity, or life style (ANA, 2001,
p. 7). In addition, the nurse is to “promote, advocate, and
Chapter 1
CONTEMPORARY ISSUES AND TRENDS IN MATERNAL, NEWBORN, AND WOMEN’S HEALTH
15
R–Routinely screen every patient for abuse.
A–Ask direct, supportive, and nonjudgmental questions.
D–Document all findings.
A–Assess your client’s safety.
R–Review options and provide referrals.
BOX 1-5
RADAR
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 15
strive to protect the health and safety of the patient”
(ANA, 2001, p. 12). Ethical codes demand action and
mandate nurses do something about violation of human
rights, not only for the abused women by reporting it, but
also on the professional, local, and national levels.
Human abuse, wherever it occurs, diminishes every
human being. The challenge to all nurses is what they
can do to make a difference in abused women’s lives and
to reduce its incidence. The right ethical choice is to
move beyond ethical beliefs to ethical action (Silva &
Ludwick, 2002).
Abortion
Abortion was a volatile legal, social, and political issue even
before the Roe v. Wade decision to legalize abortion by the
Supreme Court in 1973. The term
abortion
describes
the willful or purposeful termination of a pregnancy, usu-
ally within the first three months. Each year, an estimated
46 million abortions occur worldwide. In 2000, 1.3 mil-
lion abortions took place in the United States. Forty-nine
percent of pregnancies among American women are
unintended, and 50% of them are terminated by abortion
(Alan Guttmacher Institute, 2004). The highest per-
centages of reported abortions in 2000 were for women
who were younger than 25 years of age (52%), white
(57%), and unmarried (81%). In 2000, the racial char-
acteristics of women obtaining abortions were 57%
white, 46% black, and 7% other (Whitcomb, 2004).
Abortion is one of the most common procedures per-
formed in the United States. It has become a hotly
debated political issue that separates people into two
camps: pro-choice and pro-life. The pro-choice group
supports the right of any woman to make decisions about
her reproductive functions on the basis or her own moral
and ethical beliefs. The pro-life group feels strongly that
abortion is killing and deprives the fetus of the basic right
to life. Both sides will continue to deliberate this very
emotional issue for years to come.
Today there are several modalities available to ter-
minate a pregnancy: dilation and curettage, vacuum
extraction, or medical termination by ingesting the med-
ications methotrexate/misoprostol (Cytotec) or mifepris-
tone (RU 486). When a woman chooses to terminate her
pregnancy, she now has options, depending on how far the
pregnancy has developed. For a surgical intervention she
has up to 14 weeks’ gestation; for a medical intervention
she has up to 9 weeks’ gestation (Goss, 2002). Regardless
of the method a woman chooses, all procedures require
that women have emotional support, a stable environment
in which to recover, and nonjudgmental care throughout.
Abortion is a complex issue, and the controversy lies
not only in the public arena, but many nurses struggle
with the conflict between their personal convictions and
their professional duty. Nurses are taught to be support-
ive patient advocates and interact with a nonjudgmental
attitude under all circumstances, but nurses are not
immune to having their own personal and political views,
and they may be very different from the patients’. Nurses
need to clarify their own personal values and beliefs on
this issue and be able to provide nonbiased care before
assuming responsibility for clients who might be in a
position to consider abortion. Their decision to care for
or refuse to care for the patient affects staff unity, influences
staffing decisions, and challenges the ethical concept of
duty (Marek, 2004).
The ANA’s Code of Ethics for Nurses upholds the
nurse’s right to refuse to care for a patient undergoing
an abortion if the nurse ethically opposes the procedure
(ANA, 2001). Nurses need to make their values and
beliefs known to their managers before the situation occurs
so alternate staffing arrangements can be made. Open
communication and acceptance of personal beliefs of one
another can promote a comfortable working environment.
Substance Abuse
Substance abuse can cause fetal injury and thus has legal
and ethical implications. In some instances, courts have
issued jail sentences when pregnant women caused harm
to their fetuses. Many state laws require reporting evidence
of prenatal drug exposure and might charge pregnant
women with negligence and endangerment of a child. The
punitive approach to fetal injury raises the question of how
much government control is appropriate and how much
should be allowed in the interest of child safety (Box 1-6).
Fetal Therapy
Intrauterine fetal surgery
is a procedure that involves
opening the uterus during pregnancy, performing a sur-
gery, and replacing the fetus in the uterus. The risks to the
fetus and the mother are both great, but may be used to
correct anatomic lesions (London et al., 2003). Some argue
that medical technology should not interfere with nature
and thus this intervention should not take place. Others
would vote for the better quality of life for the child made
possible with the surgical intervention. For many people,
these are ethical debates and intellectual discussions. For
nurses, these procedures may be part of a daily routine.
Nurses do play an important supportive role in caring
and advocating for their patients and their families. As
medical science expands the use of technology, frequent
ethical situations will surface that test a nurse’s belief sys-
tem. Encouraging open discussions to address potential
emotional issues and differences in opinion among staff
members is healthy and opens the door for increasing tol-
erance of differing points of view. In caring for patients
undergoing ethically sensitive procedures, the nurse can
•
Offer objective information to the woman and her family
•
Recognize and validate the woman’s myriad feelings
•
Project a nonjudgmental attitude
•
Respect the decision made by the family
•
Assess the family’s emotional support system
•
Ask questions using reflection to ascertain feelings
•
Use appropriate touch to demonstrate support
•
Make appropriate referrals for continuity of care
16
Unit 1
INTRODUCTION TO MATERNITY, NEWBORN, AND WOMEN’S HEALTH NURSING
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 16

Nursing Management
The health care system is intricately woven into the polit-
ical and social structure of society. Nurses who under-
stand social, legal, and ethical health care issues can play
an active role in meeting the health care needs of women.
Nurses striving to address these complex concerns might
want to consider the following suggestions:
1. Be aware of your own beliefs, attitudes, and miscon-
ceptions.
2. Examine and debate your feelings to validate or change
them.
3. Stay current about the impact of social/legal/ethical
issues on the family.
4. Be sensitive to different beliefs and values from your
own.
5. Stay knowledgeable about community resources for
all issues.
6. Offer your expertise on these issues to community
groups.
7. Become a client advocate by ensuring clients know all
their options.
8. Maintain your expertise in clinical practice to avoid
litigation.
9. Speak to your legislators about your opinion regarding
political action.
It is imperative that nurses take a proactive role in
advocating and empowering their clients. Nurses need to
enable women to increase control over the determinants
of health to help improve their health status. A woman
may become empowered when she develops skills not
only to cope with her environment, but also when she
works to change it. Nurses can take on that mentoring
role with women and their families, and help improve
their health outcome.
K E Y C O N C E P T S
●
Nurses need to evoke empowerment in their patients
by enabling, permitting, and investing them with the
power of knowledge.
●
Family-centered care is the delivery of safe, satisfy-
ing, quality health care that focuses on and adapts to
the physical and psychosocial needs of the family.
●
Child-birthing practices evolved from female atten-
dants at home to male physicians delivering babies
in hospitals with the use of analgesia by the early
1900s.
●
Today, freestanding birthing centers, LDRP units,
and home births are the norm.
●
Changing demographics, economics, growth of tech-
nology and information, an increasing multicultural
patient base, and a shortage of health care workforce
to meet demands have made the health care system
difficult to navigate.
●
Women with health problems, who need health care
services the most, often have the hardest time get-
ting care because of plan coverage policies, afford-
ability concerns, and limited transportation to
access that service.
●
Healthy People 2010 is a broad-based collaborative
federal and state initiative that has set national dis-
ease prevention and health promotion objectives to
be achieved by the end of the decade.
●
All states need to address disease prevention and
health promotion to make a difference in the health
status of our nation.
●
Some of the social issues affecting women’s health
care include poverty, access to health care (especially
prenatal care), and violence.
●
Every nurse is responsible for knowing current
information regarding ethics and laws related to
their practice.
Chapter 1
CONTEMPORARY ISSUES AND TRENDS IN MATERNAL, NEWBORN, AND WOMEN’S HEALTH
17
In 1992, a South Carolina court sent Cornelia Whitner,
34, who had used cocaine while pregnant, to jail for eight
years because she violated state laws regarding child
abuse and neglect. According to the court, she should
have known that cocaine use would result in the birth
of a damaged baby; therefore, she had to be punished
(Lester 1999). Ms. Whitner is an African-American
woman who was born and raised in South Carolina.
When her youngest son was born she was arrested. A test
indicated that he had been exposed to cocaine during her
pregnancy. Ms. Whitner was never counseled about her
substance abuse problem during her pregnancy and was
never offered treatment as a way to avoid arrest. When
she was indicted, there was not a single inpatient residen-
tial drug treatment program in the entire state designed
to treat pregnant drug users (Anderson 2000).
Based on the advice of her court-appointed attorney,
Ms. Whitner pled guilty to the charge of child abuse.
At her guilty plea and sentencing hearing, Ms. Whitner
admitted that she was chemically dependent and
requested help. Although Ms. Whitner and her attorney
emphasized both the need and the desire for treatment,
the court sentenced her to eight years in prison.
Author’s Note: The public’s concern for the welfare
of the child is often expressed as anger at the mother.
As a result, policy makers tend to punish these women
with jail sentences or removal of their children from
their custody. Research shows that treatment for drug
addictions is effective. The federal government spends
millions annually on services for drug-exposed children
in school. If that were spent on early intervention, we
could prevent the children’s deficits from occurring.
But to do this, we must first accept that substance
abuse by pregnant women is similar to other treatable
health problems. We must remove the societal stigma
associated with drug use and advocate treatment for
these women. Substance abuse should be viewed as a
sickness, not a crime.
BOX 1-6
PREGNANT, HOOKED, AND BOOKED
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 17
●
State nurse practice acts, standards of care, and
agency policies and procedures are three categories
of safeguards that determine the law’s view of
nursing practice. The recently revised Code of Ethics
for Nurses by the ANA should act as an ethical guide
for the practice of nursing.
●
The nurse’s role in advocating for women’s health
must encompass local, state, and national issues that
influence access to care and research.
References
Alexander, L. L., LaRosa, J. H., Bader, H., Garfield, S. (2004). New
dimensions in women’s health (3rd ed.). Sudbury, MA: Jones and
Bartlett Publishers.
American Cancer Society. (2004). Breast cancer facts and figures.
[Online] Available at www.cancer.org/docroot/STT/stt_0.asp.
American Cancer Society. (2005). What are the risk factors for breast
cancer? Cancer Reference Information. [Online] Available at
www.cancer.org/docroot/CRI/content/CRI_2_4_2X_What_are_
the_risk_factors_for_breast_cancer_5.asp?sitearea
=.
American Heart Association. (2005). Cardiovascular disease and
women. [Online] Available at www.americanheart.org.
American Nurses Association. (2001). Code of ethics for nurses with inter-
pretive statements. Washington, DC: American Nurses Publishing.
Anderson, W. (2000). Letter to President and CEO of NAACP. South
Carolina Advocates for Pregnant Women (SCAPW). [Online]
Available at http://scapw.org/NAACPltr.htm.
Breslin, E. T., & Lucas, V. A. (2003). Women’s health nursing: toward
evidence-based practice. St. Louis, MO: WB Saunders.
Centers for Disease Control and Prevention. (2004). Safe motherhood:
promoting health for women before, during and after pregnancy.
Atlanta: CDC, Division of Reproductive Health.
Centers for Disease Control and Prevention. (2003). Fact sheet: preg-
nancy-related mortality surveillance—United States, 1991–1993.
[Online] Available at www.cdc.gov/od/oc/media/pressrel/
fs030220.htm. Accessed May 2005.
Centers for Disease Control and Prevention. (1999). State-specific
maternal mortality among black and white women—United
States, 1987–1996. MMWR, 48, 492–496. Also available at
www.cdc.gov/epo/mmwr/preview/mmwrhtm/mm4823a3.htm.
Chang, J., et al. (2003). Pregnancy-related mortality surveillance—
United States, 1991–1999. MMWR, 52 (SS02), 1–8.
Condon, M. C. (2004). Women’s health: an integrated approach to well-
ness and illness. Upper Saddle River, NJ: Prentice Hall.
Dick–Reed, G. (1933). Childbirth without fear.
Dyck, P. V., Lackritz, E., & Cordero, J. (2003). Progress review on
maternal, infant, and child health.Washington, DC: US
Department of Health and Human Services, Public Health
Service. Also available at www.cdc.gov/nchs/about/otheract/
hpdata2010/fa16/mich.htm.
Family Health International, Inc. (2005). Maternal mortality and morbid-
ity. [Online] Available at www.fhi.org/en/Topics/maternalmort.htm.
Feldhusen, A. E. (2003). The history of midwifery and childbirth in
America. [Online] Available at www.midwiferytoday.com/articles/
timeline.asp.
Goss, G. L. (2002). Pregnancy termination: understanding and
supporting women who undergo medical abortion. AWHONN
Lifelines, 6, 46–50.
Grantham, C. (2002). Women’s issues then and now. [Online]
Available at www.cwrl.utexas.edu/
∼ulrich/femhist/medicine.shtml.
Keefe, C. (2003). Overview of maternity care in the US. [Online] Available
at www.cfmidwifery.org/pdf/OverviewofMatCareApr2003.pdf.
Lamaze, F. (1984). Painless childbirth: the Lamaze method.
Lincolnwood, IL: NTC Publishers.
Lehrman, G. (2003). Childbirth in early America. [Online] Available at
www.gliah.uh.edu/historyonline/childbirth.cfm.
Lester, B. (1999). Drug-abusing moms and babies—victims of stigma.
Brown University News Service. [Online] Available at www.
brown.edu/Administration/News_Bureau/Op-Eds/Lester.html.
London, M. L., Ladewig, P. W., Ball, J. W., & Bindler, R. C. (2003).
Maternal–newborn & child nursing: family-centered care. Upper
Saddle River, NJ: Prentice Hall.
Marek, M. J. (2004). Nurses’ attitudes toward pregnancy termination
in the labor and delivery setting. JOGNN, 33, 472–479.
Martin, J., et al. (2002). Births final data for 2001. National Vital
Statistics Reports, 49(5),16.
Martin, J. A., Kochanek, K. D., Strobino, D. M., Guyer, B., &
MacDorman, M. F. (2005). Annual summary of vital statistics—
2003. Pediatrics, 115, 619–634.
Maternal Child Health Bureau. (2001). Child health USA. Rockville,
MD: Maternal Child Health Bureau, Health Resources and
Services Administration, US Department of Health & Human
Services.
Murray, S. S., McKinney, E. S., & Gorrie, T. M. (2006). Foundations
of maternal–newborn nursing (4th ed.). Philadelphia: WB Saunders.
National Center for Health Statistics. (2005). More babies born at
very low birthweight: linked to rise in infant mortality in 2002. In
NCHS news release fact sheets. [Online] Available at www.cdc.gov/
nchs/pressroom/05news/lowbirthwt.htm.
National Women’s Law Center, FOCUS/University of Pennsylvania,
and the Lewin Group. (2000). Making the grade on women’s health:
a national state-by-state report card. Washington, DC: National
Women’s Law Center.
Osei, W., Jackson, M., & Miller, S. (2003). Global health indicators for
regional health authorities. Epidemiology, research and evaluation
unit. [Online] Available at www.health.gov.sk.ca/ph_ph_ere_ghi.pdf.
Phillips, C. R. (2003). Family-centered maternity care. Sudbury, MA:
Jones and Bartlett Publishers.
Salganicoff, A., Beckerman, J. Z., Wyn, R., & Ojeda, V. D. (2002).
Women’s health in the United States: health coverage and access to
care. Report no. 6027. Menlo Park, CA: The Henry J. Kaiser
Family Foundation.
Save the Children. (2005). State of the world’s mothers (6th ed., pp.
1–52). Westport, CT: David and Lucille Packard Foundation.
Silva, M., & Ludwick, R. (2002). Ethic column: domestic violence,
nurses and ethics: what are the links? Online Journal of Issues in
Nursing. [Online] Available at www.nursingworld.org/ojin/
ethicol/ethics_8.htm.
The Alan Guttmacher Institute. (2004). Facts in brief: induced abor-
tion. [Online] Available at www.agi-usa.org/pubs/fb_induced_
abortion.html.
United Nations. (2003). United Nations demographic yearbook. New
York: United Nations.
U.S. Department of Health and Human Services. (2000). Healthy peo-
ple 2010 (2nd ed.). Washington, D.C.: U.S. Government Printing
Office.
U.S. Department of Health and Human Services. (2002). Women’s
health USA 2002. Rockville, MD: US Department of Health and
Human Services, Health Resources and Services Administration,
Maternal and Child Health Bureau. Also available at http://mchb.
hrsa.gov/data/women.htm.
Whitcomb, D. J. (2004). Abortion surveillance: trends, characteristics
and the necessity of the data collection. AWHONN Lifelines, 8,
112–114.
World Factbook. (2005). Infant mortality rate. Washington, DC:
Central Intelligence Agency.
World Health Organization. (2005). Gender, health and poverty fact
sheet. [Online] Available at www.who.int/inf-fs/en/fact251.html.
Youngkin, E. Q., & Davis, M. S. (2004). Women’s health: a primary
care clinical guide. Upper Saddle River, NJ: Pearson Prentice Hall.
Web Resources
American Dietetic Association, www.eatingright.org
American Heart Association National Center,
www.americanheart.org
Association of Reproductive Health Professionals, www.arhp.org
CancerNet, www.cancernet.nci.nih.gov
Centers for Disease Control and Prevention, www.cdc.gov
Initiative to Eliminate Racial and Ethnic Disparities in Health,
http://raceandhealth.hhs.gov
National Abortion Federation, www.naf.org
National Coalition for Women with Heart Disease,
www.womenheart.org
Office of Minority Health, www.omhrc.gov
Planned Parenthood Federation of America, www.ppfa.org
Public Health Service, www.ahcpr.gov
The Alan Guttmacher Institute, www.agi-usa.org
18
Unit 1
INTRODUCTION TO MATERNITY, NEWBORN, AND WOMEN’S HEALTH NURSING
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 18
Chapter 1
CONTEMPORARY ISSUES AND TRENDS IN MATERNAL, NEWBORN, AND WOMEN’S HEALTH
19
Chapter
WORKSHEET
Chapter
●
M U L T I P L E C H O I C E Q U E S T I O N S
1.
Most women in the 1900s were attracted to hospitals
for their child-birthing needs because they
a. Felt the sterile environment of a hospital would
reduce infections
b. Wanted analgesia to reduce the discomfort of
their labors
c. Needed to have privacy, which was not afforded
in the home
d. Sought a male physician with more experience to
deliver them
2.
The maternal mortality rate differs from the infant
mortality rate in its measurement of
a. The deaths-per-live births comparison
b. How the statistics were gathered
c. The time frame in which the data were formulated
d. The health index for the various countries
3.
The number one cause of mortality for women in the
United States is
a. Breast cancer
b. Childbirth complications
c. Injury resulting from violence
d. Heart disease
4.
Research reports that women receiving prenatal
care have better pregnancy outcomes. Why are
many women in the United States not receiving this
valuable service?
a. They don’t feel it is necessary for a normal pregnancy
b. Many use denial to cope with their pregnancy
c. No health insurance to cover the expense of care
d. Some do not trust traditional medical practices
●
C R I T I C A L T H I N K I N G E X E R C I S E
1.
As a nurse working in a federally funded low-income
clinic offering women’s health services, you are
becoming increasing frustrated with the number of
“no-shows” or appointments missed in your mater-
nity clinic. Some clients come for their initial prenatal
intake appointment and never come back. You realize
that some just forget their appointments, but most
don’t even call to notify you. Many of the clients are
high risk and thus are jeopardizing their health and
the health of their future child.
a. What changes in the clinic service hours might
address this situation?
b. Outline what you might say at your next staff
meeting to address the issue of clients making one
clinic visit and then never returning.
c. What strategies might you use to improve atten-
dance and notification?
b. Describe what cultural and customer service tech-
niques might be needed.
●
S T U D Y A C T I V I T I E S
1.
Within your clinical group discussion, debate the
following statement: Should access to health care
be a right or a privilege?
2.
List three reasons why one in four women is not
receiving prenatal care in the United States.
3.
Choose an Internet website from the ones listed here
pertaining to women’s health and select an article
from that site to discuss in your clinical group.
www.4woman.gov/
www.healthywomen.org
www.ivillage.com
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 19
10681-01_UT1-Ch01.qxd 6/19/07 2:54 PM Page 20
Wyszukiwarka
Podobne podstrony:
Essentials of Maternity Newborn and Women's Health 3132A 30 p780 781
Essentials of Maternity Newborn and Women's Health 3132A 29 p778 779
Essentials of Maternity Newborn and Women s Health 3132A 32 p785 808
Essentials of Maternity Newborn and Women s Health 3132A 23 p634 662
Essentials of Maternity Newborn and Women s Health 3132A 17 p428 446
Essentials of Maternity Newborn and Women s Health 3132A 16 p393 427
Essentials of Maternity Newborn and Women s Health 3132A 21 p585 612
Essentials of Maternity Newborn and Women s Health 3132A 09 p189 207
Essentials of Maternity Newborn and Women s Health 3132A 11 p235 252
Essentials of Maternity Newborn and Women s Health 3132A 20 p543 584
Essentials of Maternity Newborn and Women s Health 3132A 08 p167 188
Essentials of Maternity Newborn and Women s Health 3132A 03 p042 058
Essentials of Maternity Newborn and Women s Health 3132A 27 p769 771
Essentials of Maternity Newborn and Women s Health 3132A 26 p729 768
Essentials of Maternity Newborn and Women s Health 3132A 28 p772 777
Essentials of Maternity Newborn and Women s Health 3132A 25 p717 728
Essentials of Maternity Newborn and Women s Health 3132A 05 p107 126
Essentials of Maternity Newborn and Women s Health 3132A 19 p496 542
więcej podobnych podstron