3
Cytological screening for cervical cancer prevention
Lynette Denny, MBChB, MMED (O&G), FCOG (SA), PhD, Head
Department Obstetrics and Gynaecology, H 45, Old Main Building, University of Cape Town and Groote Schuur Hospital,
Observatory 7925, Cape Town, South Africa
Keywords:
screening
cervical cytology
cervical cancer
prevention
Historically, the incidence and mortality of cervical cancer has
declined in countries that have instituted and sustained mass-
organised cytology-based screening programmes. These pro-
grammes, however, required frequent repeats of the screening tests.
They also require a functioning healthcare infrastructure, with
laboratories for smear processing and interpretation, mechanisms
for quality control, referral for colposcopy, treatment of precursors,
and follow-up to detect failures of treatment. Although this
approach has been successful in preventing cervical cancer where
implemented correctly, it has proved inordinately complex and
expensive for developing countries. Consequently, no successful
screening programmes have been established in poor countries, and
cervical cancer remains the most common cancer among women in
developing countries, despite the existence of cytology and the
knowledge of cervical cancer prevention. New technologies,
speci
fically the development of liquid-based cytology, have
improved the performance of cytology as a screening test, but do not
obviate the infrastructural challenges posed to health systems by
cytology-based screening programmes. In this chapter, the history of
cytological screening and the challenges posed by secondary
prevention strategies are reviewed.
Ó 2011 Elsevier Ltd. All rights reserved.
Introduction
In 2008, an estimated 530,000 women had a diagnosis of cervical cancer and 275,000 women died
from the disease, corresponding to age-standardised incidence and mortality rates (ASIR and ASMR) of
15 and 8 per 100,000 women, respectively.
Globally, it was the third most common cancer after breast
* Tel.: þ27 21 404 4485; Fax: þ27 21 448 6921.
E-mail address:
.
Contents lists available at
Best Practice & Research Clinical
Obstetrics and Gynaecology
j o ur n a l ho m e pa g e : w w w. e l se v i e r . co m / l o ca t e / b po b g y n
1521-6934/$
– see front matter Ó 2011 Elsevier Ltd. All rights reserved.
doi:
Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) 189
cancer; however, in developing countries, where over 80% of cases are diagnosed, it was the most
common cancer in women. It was the fourth most common cause of death ranking below breast cancer
(458,000 deaths), lung cancer (427,000 deaths), and colorectal cancer (288,000 deaths).
A striking
variation of incidence of cervical cancer was reported in different regions of the world. For instance, the
lowest burden occurred in Australia and New Zealand (ASIR of 5.0 per 100,000 women and ASMR of 1.4
per 100,000 women) compared with Eastern Africa (ASIR of 34.5 per 100,000 women and ASMR of 25.3
per 100,000 women). Cervical cancer was the most common cancer cause of death in women in
Eastern Africa, South-Eastern Asia and Melanesia. Historically, the incidence and mortality rates from
cervical cancer correlate relatively well with the existence of cervical cancer prevention programmes,
largely cytology based.
History of cytology of the cervix and vagina
Cervical cytology testing involves collecting exfoliated cells from the cervix and examining these
cells microscopically. The concept of using exfoliated cells to identify women with invasive cervical
cancer was introduced by Papanicolaou and Babes in the 1920s.
Subsequently, Papanicolaou re
fined
his technique, and in 1941 published on the use of conventional cytology to identify invasive cervical
cancers. In 1954, he published on how to identify and classify cervical cancer precursors.
In the
first
paragraph of the 1941 article, the authors state:
‘The death rate from carcinoma of the female genital tract is approximately 32,000 per year in
the United States and of this
figure, four-fifths or 26,000 deaths may be said to be due to cancer
of the uterus. This rate has remained practically constant during the past twenty
five years.’
What is interesting is that, in 2011, the situation in many developing countries is not so different
from that in the USA more than 70 years ago. Even in 1941, it was noted that early diagnosis and
treatment yielded
‘a high percentage of cures in both carcinoma of the fundus and of the cervix.’ It was
not, however, until the 1960s that cervical cytology began to be used widely in many developed
countries as a tool for cervical cancer prevention.
Papanicolaou separated cervical cytology
findings into five categories (classes I–V), and focused on
how closely the cells resembled truly malignant cells (
).
It has long been recognised that cervical cancer develops from histologically well-characterised
precursors. The
first evidence suggesting the existence of precursor lesions for invasive squamous
carcinoma of the cervix were observations made in the late 1800s that non-invasive epithelial
abnormalities frequently existed adjacent to invasive lesions. Schottlander and Kermauner were
quoted in Wright and Kurman as being the
first to propose the term carcinoma in-situ (CIS) to describe
these intraepithelial abnormalities.
Subsequently, a number of case-controlled studies showed that a signi
ficant proportion of women
with CIS, who were untreated, developed cervical cancer. Petersen
followed 127 women with biopsy-
con
firmed, high-grade preinvasive lesions of the cervix (epithelial hyperplasia with nuclear abnor-
malities) for a minimum of 3 years. He found that overt cervical cancer developed in 4% of women at
the end of 1 year, 11% at the end of 3 years, 22% at the end of 5 years and in 33% at the end of 9 years of
follow up. Kottmeier
found that 25 out of 34 women with CIS who were followed for 20 years or more
without treatment developed invasive cancer.
In a study by Koss et al.,
lesions of women with CIS were con
firmed histologically by biopsy and
then followed using cytology alone. Four out of 67 women (6%) developed invasive cancer between 16
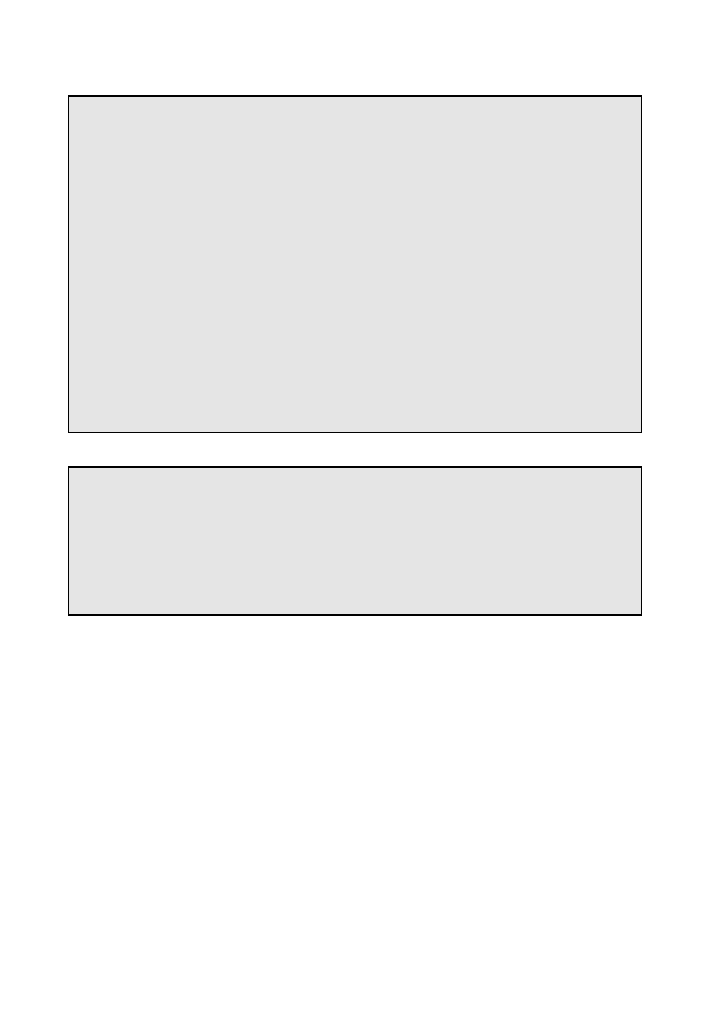
Table 1
Classi
fication of cervical cytology.
Class
Description
I
Absence of atypical or abnormal cells
II
Atypical cytology, but no evidence for malignancy
III
Cytology suggestive of, but not conclusive for, malignancy
IV
Cytology strongly suggestive of malignancy
V
Cytology conclusive for malignancy
L. Denny / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) 189
–196
190

and 54 months after entering the study and
five out of 67 (7%) women developed possible invasion.
Hall and Walton
reported a 29% progression rate of severe dysplasia to carcinoma in situ or invasive
cancer over a 1
–14 year period.
In the 1950s, it became apparent that another large group of cervical lesions had some of the
characteristics of CIS, but to a lesser degree. Reagan et al.
first introduced the term dysplasia to
describe these lesions. Dysplasia referred to abnormalities that included a cytological and histological
spectrum of lesions intermediate between CIS and normal epithelium. The World Health Organization
introduced this terminology as
‘mild, moderate, severe dysplasia’ and CIS for ‘cytological and histo-
pathological classi
fication of cervical cancer precursors’.
The natural history of dysplasia was studied extensively in the 1950s and 1960s. Population-based
screening programmes of previously unscreened populations showed that women with mild dysplasia
were younger than women with moderate dysplasia, who in turn were younger than women with
severe dysplasia and CIS.
This age distribution suggested that mild dysplasia progressed over years to
higher grades of dysplasia and
finally to CIS. CIS was considered high risk for progression to invasive
cancer and was aggressively treated with cone biopsy or hysterectomy.
In the 1960s, Richart
introduced a classi
fication for cervical intraepithelial neoplasia (CIN).
Laboratory-based studies showed that the differences between the different grades of dysplasia were
quantitative as well as qualitative. On the basis of these studies and long-term clinical follow-up
studies, Richart
suggested that dysplasia and CIS constituted a histological continuum rather than
a series of discrete entities and introduced the term
‘cervical intraepithelial neoplasia’. In the original
CIN terminology, CIN1 corresponded to mild dysplasia, CIN 2 to moderate dysplasia and CIN3 to severe
dysplasia and CIS.
The concept of CIN was strongly in
fluenced by the results of a long-term prospective follow-up
study of 557 women who had had three previous dysplastic smears.
After study entry, the women
were prospectively followed for an average of 36 months using cytology and colposcopy without
cervical biopsy. During follow up, only 6% of the lesions spontaneously regressed and the remainder
either persisted or progressed to higher grades of dysplasia or cancer.
In an attempt to standardise cytology nomenclature, a new classi
fication of cytological reporting,
called the Bethesda system, was devised in 1988.
The Bethesda system combined clinically similar
intraepithelial diagnoses into broad categories, speci
fically low-grade squamous intraepithelial lesions
(LSIL), representing the changes of koiliocytic cytological atypia and CIN1, and high-grade SIL (HSIL),
representing the changes of CIN 2 and 3. The Bethesda system of cytological reporting was subse-
quently revised in 2001 and again in 2006 (for full classi
fication go to
).
LSIL is common and represents the usually benign cytopathological signs of human papilloma virus
(HPV) infection. In contrast, HSIL is rare and represents a truly premalignant condition. Although LSIL
can be viewed as an epidemiological exposure or risk factor for cervical cancer, HSIL can be viewed as
more closely linked to cancer outcome.
Although this conceptual distinction is clinically useful, it is not perfect. A continuum of changes
exists that encompass LSIL and HSIL without a clear end point. At a microscopic level, for example, the
characteristic cells of LSIL are abnormal but terminally differentiated. The atypical cells progress to the
surface, produce keratins, die and exfoliate as would normal cells. The gradient from LSIL to HSIL is
characterised by increasing nuclear atypia and failure of cellular differentiation in progressively more
super
ficial levels of epithelium, with CIN3 representing full-thickness replacement of the epithelium
with undifferentiated, atypical cells.
Effect of cervical cytology-based screening programmes
Until recently, no randomised-controlled trials had been conducted to evaluate the effect of
cytologically-based cervical cancer screening on cervical cancer incidence and mortality, and all data
on the effect of screening came from cohort and case-controlled studies. The marked reduction in the
incidence of, and mortality from, cervical cancer before and after the introduction of screening pro-
grammes in a variety of developed countries, was interpreted as strong non-experimental support for
organised cervical cancer screening programmes.
L. Denny / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) 189
–196
191

The International Agency for Research on Cancer conducted a comprehensive analysis of data from
several of the largest screening programmes in the world in 1986, and showed that well-organised
cytology-based screening programmes were effective in reducing the incidence of, and mortality
from, cervical cancer.
In the Nordic countries, after the introduction of nationwide screening in the
1960s, cumulative mortality rates of cervical cancer showed a falling trend. The greatest fall was in
Iceland (84% from 1965 to 1982) where the screening interval was the shortest and the target age
range the widest. The smallest reduction in cumulative mortality (11%) was in Norway, where only 5%
of the population had been part of organised screening programmes.
The decline in Finland,
Sweden and Denmark were 50%, 34% and 27%, respectively. The highest reduction in cervical cancer
incidence was among women aged 30 and 49 years, where the focus of screening was the most
intense.
The association between mortality trends and the extent of coverage of the population by organised
screening was most pronounced when the proportional reductions in the age-speci
fic rates were
related to the target ages of the screening programmes. The age-speci
fic trends indicated that the
‘target age range’ of a screening programme was a more important determinant of risk-reduction than
the
‘frequency’ of screening within the defined age range. This finding was in agreement with the
estimates of the International Agency for Research on Cancer working group, that for inter-screen
intervals of up to 5 years, the protective effect of organised screening was high throughout the tar-
geted age group (over 80%).
It is apparent, therefore, that the extent to which screening programmes
have succeeded or failed to reduce incidence of, and mortality from, cervical cancer is largely re
flected
in (1) the extent of coverage of the population at risk by screening; (2) the target age of women
screened; and (3) the reliability of cytology services in that programme.
The contrast between Finland, which had an organised screening programme, and Norway, where
an equivalent number of smears were carried out opportunistically, indicated another important
aspect of screening. Even though the difference in the total number of smears taken in the two
countries was not great, the reduction in mortality was substantial for all ages in Finland, whereas in
Norway, only women aged 30
–49 years showed a fall in mortality rates: even for that age group, the fall
was half that shown in Finland. These data suggest that spontaneous or opportunistic screening fail to
reach the most at-risk women in the population; that is, middle-aged and older women of high relative
risk and therefore has far less of an effect on the incidence of, and mortality from, cervical cancer. Other
reasons for the failure of opportunistic screening to reduce cervical cancer mortality include sub-
optimal follow up and management of women with abnormal smears, and the lack of a co-
ordinated campaign of informing and educating women about cervical cancer prevention. This
results in women at high risk of disease being excluded from screening.
The Canadian experience provides further evidence of the effect of screening. A 20-year screening
programme was carried out in British Columbia between the 1960s and 1980s.
The incidence of
cervical cancer dropped from 28.4 to 6.9 and mortality from 11.4 to 3.3 per 100,000 women over that
period.
Mortality from cervical cancer in the UK fell by 30% after the introduction of screening in the 1960s;
however, some of this decline was attributed to falling rates in older women, and could have been
a cohort effect unrelated to screening.
The need for an effectively managed national programme in
the UK was realised by the mid 1980s, which led to the introduction of a computerised call and recall
system for women aged between 20 and 64 years. The invitation-based system, together with target
payments for general practitioners, improved population coverage from 40
–60% in 1989, to 80% in
1992 and to 83% in 1993. In an audit of this programme in 24 self-selected districts in the UK by Sasieni
et al.,
it was estimated that the number of cases of cervical cancer in the participating districts would
have been 57% (95% con
fidence interval (CI) 28–85%) greater had there had been no screening. They
also estimated that screening prevented between 1100 and 3900 cases of invasive cervical cancer in the
UK.
Experience from countries that have successfully maintained cervical cancer screening programmes
indicate that instituting mass cervical screening requires a complex network of parallel factors.
The
following factors are considered important in ensuring the success of cytologically-based screening
programmes: (1) adequate
field facilities with appropriately trained health personnel to carry out
quality cervical smears; (2) wide coverage of the target population (at least 70%) at regular intervals:
L. Denny / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) 189
–196
192

a minimum of 3 years between smears and mechanisms for contacting women on an individual basis
(e.g. through personally addressed letters); (3) an ef
ficient health infrastructure with functioning
management and information systems; (4) a cytology service with built-in quality assurance, ongoing
training of cytotechnicians, and regular audit of performance of laboratories; (5) an accessible and
functional referral system for colposcopic assessment of women with abnormal smears; (6) adequate
diagnosis, treatment and follow up of women with abnormal smears, and follow up of women who
have been treated for preinvasive disease of the cervix; (7) community understanding and accept-
ability; (8) screening programmes should be planned at national level, and they should be organised to
encompass a call and recall system; (9) a cancer registry to monitor the effect of the screening
programmes.
These factors require a relatively sophisticated health infrastructure, and implementation is not
feasible in developing countries with limited resources. This explains the failure of cytology-based
screening programmes in large parts of the world and the large discrepancy in incidence of, and
mortality from, cervical cancer in different regions of the world.
New technologies
Despite the success of some well-executed conventional cytology-based screening programmes,
when the performance of cervical cytology was scrutinised, the accuracy of cytology was brought into
question. Fahey et al.
conducted a meta-analysis of 62 studies comparing Pap tests with histology,
and found that the estimates of sensitivity of cytology ranged from 11
–99% and specificity from 14–
97%. Both were highly negatively correlated, with Pap tests being unable to achieve concurrently high
sensitivity and speci
ficity. The average sensitivity of cytology was 57%.
Liquid-based cytology (LBC) was introduced in the mid 1990s in an attempt to improve the
performance of conventional cytology. LBC involves immersing the spatula used to obtain the smear
into a liquid preservative solution that is then transported to the laboratory where the slide is
prepared through an automated process. The process involves the breaking up of cells and mucus by
mechanical agitation, followed by
filtering of the liquid solution through a membrane filter with
a pore size designed to trap epithelial cells while allowing contaminating blood and in
flammatory
cells to pass through. The epithelial cells are collected on the membrane and then transferred onto
a glass slide and stained. LBC is reported to have a number of advantages over conventional cytology,
which include the following: (1) more representative transfer of cells from the collection device to
the glass slide; (2) reduction in the number of unsatisfactory cells; (3) higher detection rates of
cellular abnormalities; (4) availability of residual cellular material for molecular testing; (5) reduction
of screening time and greater ease of screening; and (6) possibility for automated interpretation of
slides.
Liquid-based cytology currently accounts for more than 90% of Pap smears carried out in the
USA and UK. Data on trials using LBC have generated considerable controversy owing to the
heterogenous design of studies, the use of split-sample techniques without histological veri
fica-
tion, and failure to con
firm cytological diagnoses with histology. Karnon et al.
reviewed the
effectiveness and cost-effectiveness of LBC in 2004. They concluded that, from the evidence
available, it is likely that LBC will reduce the number of false-negative tests, and this in turn would
reduce the incidence of invasive cervical cancer. In addition, their analysis supported the
contention that LBC is associated with reduced number of unsatisfactory smears and a decrease in
time needed to screen the smears. These bene
fits translated into significantly greater cost-
effectiveness of LBC over conventional cytology; it was on this basis that the National Health
Service of the UK introduced LBC nationally.
By contrast, Arbyn et al.
reported on an analysis of 109 studies that described test positivity,
adequacy rates, or both, in conventional and LBC. In only six studies, however, were all the cytology
results veri
fied with the standard reference test of histopathology. The pooled sensitivity for HSIL
detected by LBC in those studies with complete gold standard veri
fication was 57% and 55.2% for
conventional cytology, with speci
ficities of 97 and 96.7%, respectively. With the cut-off at atypical
squamous cells of undetermined signi
ficance for both methods, the pooled sensitivities were 90.4%
and 88.2%, respectively, with speci
ficities of 64.6 and 71.3%, respectively. They concluded that LBC
L. Denny / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) 189
–196
193

was neither more sensitive nor more speci
fic for detection of HSIL compared with conventional
cytology.
Despite these controversial interpretations of the data, LBC has been approved by the US Food and
Drug Administration, is widely used throughout the developed, and is likely to stay as the recom-
mended method of screening in these countries. Molecular testing to improve the performance of
cervical cytology has been intensively investigated in high-income countries as an adjunct or
complementary screening test to cytology. In developing countries, molecular testing combined with
treatment of positive tests has been extensively investigated in low-income countries as an alternative
to, and replacement for, cervical cytology, as discussed in the Chapters entitled
“HPV DNA Testing in
Developed countries
” and “HPV DNA testing in Developing Countries”. The molecular test of particular
signi
ficance is testing for high-risk types of HPV. These chapters will explore the data and evidence for
the introduction of HPV DNA testing in both high- income and low-income settings.
Katki et al.,
reported on a large programme of co-testing (LBC and HPV DNA testing) for cervical
cancer risk that was introduced into a health-maintenance organization for women over the age of 30
years between 2003 and 2005. The study included 331,818 women. Higher rates of disease were
reported in women positive for HPV at enrolment compared with women positive for Pap for CIN 2
(78% v 53%), CIN 3 or adenocarcinoma in situ (84% v 53%), adenocarcinoma in situ (80% v 40%), total
cancers (69% v 51%) and adenocarcinoma (78% v 15%); all outcomes highly statistically signi
ficant. In
addition, they identi
fied higher percentages of disease outcomes in women who were positive by
HPV and negative by Pap than vice versa. Enrolment HPV testing distinguished future risk of CIN 3 or
worse more clearly than enrolment cytology. Women who were negative for HPV testing had half the
5-year risk of invasive cervical cancer than women negative by Pap (3.8 v 7.5 per 100,000 women per
year). The importance of this study is that it allows an evaluation of the real-world clinical effec-
tiveness of concurrent testing with HPV and cytology. A single negative HPV test ensured that
a woman remained low risk for CIN 3 or cancer for at least 5 years; however, negative cytology
provided no additional reassurance against cancer beyond that provided by a negative HPV test.
Further, testing for HPV predicted future disease much more accurately than cytology. This study
con
firms the superior test performance of HPV testing in clinical practice and that cytology as a co-
test adds little value. Cytology as a post-HPV DNA test most likely has higher value of reducing the
referral rate for colposcopy.
Ronco et al.
randomly assigned women aged 25
–60 years to conventional cytology or to HPV
testing in combination with LBC or alone in 2004. Overall, 47,001 women were assigned to the cytology
group and 47,369 were assigned to the HPV testing group. Although the detection of invasive cancers
was the same in the
first round of screening in the two groups, no cancers were detected in the second
round of screening in the HPV group compared with nine in the cytology group. Further, for women
aged greater than 35 years, the detection of CIN 2 and CIN 3 in the HPV group was signi
ficantly higher
than in the cytology group, with a detection ratio of 2.03 (95% CI 1.60 to 2.57). Conversely, in the second
round of screening, the detection of CIN 2 and 3 was signi
ficantly lower than in the cytology group.
These data support the superiority of HPV testing as a screening test compared with cytology, and the
authors recommend using HPV testing as a primary screen and to reserve cytology for the triage of
HPV-positive women.
Conclusion
Correctly implemented cytology-based screening programmes have had a major effect on reducing
cervical cancer incidence and mortality. The test, however, requires frequent repetition to achieve
acceptable longitudinal sensitivity. Current technologies, such as LBC, offer advantages over conven-
tional cytology; however, they do not obviate the complexity of the infrastructure required to maintain
effective cytology-based screening programmes. HPV testing has been subjected to numerous clinical
trials and has been shown to be superior in sensitivity to cytology, although less speci
fic. Large
randomised-controlled trials, however, have shown signi
ficantly improved detection of cervical cancer
precursors and reduction in cervical cancer in women tested with HPV and treated appropriately.
Cytology is currently recommended for use as a triage for HPV positive women or as a co-test with HPV
testing for women over the age of 30 years.
L. Denny / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) 189
–196
194
Con
flict of interest
The author has received honoraria for appearing in various speaker for GlaxoSmithKline (GSK) and
Merck/MSD. The author is the principal investigator in two studies sponsored by GSK and one by
Merck/MSD.
References
1. Arbyn M, Castellsague X, De Sanjose S et al. Worldwide burden of cervical cancer in 2008. Ann Oncol 2011. published April 6
(Epub ahead of print).
2. Papanicolaou GN. New cancer diagnosis. In: Proceedings of the Third Race Betterment conference. Battle Creek, Michigan:
Race Betterment Foundation, pp. 528
–534.
3. Papanicolaou GN & Traut HF. The diagnostic value of vaginal smears in carcinoma of the uterus. Am J Obstet Gynecol 1941;
41: 193
–206.
4. Papanicolaou GN. Atlas of exfoliative cytology. Boston, Massachusetts: Commonwealth Fund University Press, 1954.
5. Wright TC & Kurman RJ. A critical review of the morphologic classi
fication systems of preinvasive lesions of the cervix: the
scienti
fic basis for shifting the paradigm. Papillomavirus Rep 1994; 5: 175–182.
6. Petersen O. Spontaneous course of cervical precancerous conditions. Am J Obstet Gynecol 1956; 72: 1063
–1071.
7. Kottmeier HL. The development and treatment of epitheliomas [in French]. Rev Franc Gynecol 1961; 56: 821
–825.
8. Koss LG, Stewart FW, Foote FW et al. Some histological aspects of behavior of epidermoid carcinoma-in-situ and related
lesions of the uterine cervix. Cancer 1963; 16: 1160
–1211.
9. Hall JE & Walton L. Dysplasia of the cervix. A prospective study of 206 cases. Am J Obstet Gynecol 1968; 100: 662
–671.
Practice points
Cervical cancer is the most common cancer diagnosed in women living in developing
countries owing to the failure of established or sustained cervical cancer screening
programmes.
Cervical cytology-based programmes were introduced widely in the 1960s, and where
implemented correctly, resulting in a signi
ficant decrease in cervical cancer incidence and
mortality.
Key issues for implementation of cervical cancer include extent of coverage and defining
target age group, coupled with high-quality cervical cytology laboratory services and
a functioning healthcare infrastructure.
New technologies, such as LBC, have shown some advantages over conventional cytology,
particularly in reducing rate of unsatisfactory smears and quicker screening time.
Other benefits of LBC are more controversial, including the finding in some studies of
increased detection of high-grade precursors.
Randomised-controlled trials and real-life clinical screening programmes have shown that
HPV DNA testing is signi
ficantly more sensitive than cytology for detecting high-grade
cervical cancer precursors, although less speci
fic. Current recommendations from these
trials are that the best use of cytology is for the triage of HPV DNA positive women. Only if
both the HPV test and cytology are positive is the patient referred for colposcopy.
Research agenda
Effect of LBC on cervical cancer incidence and mortality as outcomes, not just detection of
high-grade cervical cancer precursors.
Accuracy of automation in interpretation of cervical cytology.
Effect of cervical cytology as a triage for positive HPV DNA testing.
Co-effectiveness of co-testing with HPV DNA testing and effect on cervical cancer prevention.
Methods for improving sensitivity of cytology.
L. Denny / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) 189
–196
195

10. Reagan JW, Seidemann IL & Sarcusa Y. Cellular morphology of carcinoma in situ and dysplasia or atypical hyperplasia of
uterine cervix. Cancer 1953; 6: 224
–235.
11. Stern E & Dixon WJ. Rate, stage, and patient age in cervical cancer; analysis of age speci
fic discovery rates for atypical
hyperplasia, in situ cancer, and invasive cancer in well population. Cancer 1959; 12: 933
–937.
12. Richart RM. Natural history of cervical intrapeithelial neoplasia. Clin Obstet Gynecol 1968; 10: 748
–784.
13. Baron BA & Richart RM. A statistical model of the natural history of cervical carcinoma based on a prospective study of 557
cases. J Natl Cancer Inst 1968; 41: 1343
–1353.
14. National Cancer Workshop. The 1988 Bethesda System for reporting cervical/vaginal cytologic diagnosis. JAMA 1989; 262:
931
–934.
15. International Agency for Research on Cancer Working Group on Cervical Cancer Screening. Summary chapter. In Hakama M,
Miller AB & Day NE (eds.). Screening for cancer of the uterine cervix 1986, pp. 133
–142. Lyon.
16. Laara E, Day NE & Hakama M. Trends in mortality from cervical cancer in the Nordic countries: association with organised
screening programmes. Lancet 1987; 8544: 247
–1249.
17. IARC Working Group on Evaluation of Cervical Cancer Screening Programmes. Screening for squamous cervical cancer: the
duration of low risk after negative result of cervical cytology and its implication for screening policies. BMJ 1986; 293: 659
–
664.
18. Hakama M & Louhivuori K. A screening programme for cervical cancer that worked. Cancer Surveys 1988; 17: 403
–416.
19. International Agency for Research on Cancer. In Hakama M, Miller AB & Day NE (eds.). Screening for cancer of the uterine
cervix. Lyon: IARC Scienti
fic Publications No. 76, 1986, pp. 47–60.
20. Sasieni PD, Cuzick J, Lynch-Farmery E & The National Co-ordinating Network for Cervical Screening Working Group.
Estimating the ef
ficacy of screening by auditing smear histories of women with and without cervical cancer. Br J Cancer
1996; 73: 1001
–1005.
21. Miller AB. Cervical cancer screening programmes: managerial guidelines. Geneva: World Health Organization, 1992.
21. Fahey MT, Irwig L & Macaskill P. Meta-analysis of Pap test accuracy. Am J Epidemiol 1995; 14: 680
–689.
23. Karnon J, Peters J, Platt J et al. Liquid-based cytology in cervical screening: an updated rapid and systematic review and
economic analysis. Health Technol Assess 2004; 8: 1
–78.
24. Arbyn M, Bergeron C, Klinkhamer P et al. Liquid compared with conventional cervical cytology: a systemic review and
meta-analysis. Obstet Gynecol 2008; 111: 167
–177.
25. Katki H, Kinney W, Fetterman B et al. Cervical cancer risk for women undergoing concurrent testing for human papillo-
mavirus and cervical cytology: a population-based study in routine clinical practice. Lancet Oncol 2011; 12: 663
–672.
26. Ronco G, Giorgi-Rossi P, Carozzi F et al. Ef
ficacy of human papillomavirus testing for the detection of invasive cervical
cancers and cervical intraepithelial neoplasia: a randomised controlled trial. Lancet Oncol 2010; 11: 249
–257.
L. Denny / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) 189
–196
196
Document Outline
Wyszukiwarka
Podobne podstrony:
New technologies for cervical cancer screening
New technologies for cervical cancer screening
Cervical Cancer Prevention and Early american cancer society
Alternative approaches to cervical cancer screening — kopia
Human Papillomavirus and Cervical Cancer Knowledge health beliefs and preventive practicies
Real Macrobiotics for Cancer Prevention and Treatment Varona
Trend in cervical cancer screening in Spain
Lower utilization of cervical cancer screening by nurses in Taiwan
Reporting rates for cervical screening in the
Cost effectiveness of cervical cancer screening
The present ways in prevention of cervical cancer
Filling a gap in cervical cancer screening programmes
Increasing participation in cervical cancer screenin Telephone contact
Knowledge of cervical cancer and screening practices of nurses at a regional hospital in tanzania
[41]Hormesis and synergy pathways and mechanisms of quercetin in cancer prevention and management
Menagement Dile in cervical cancer
więcej podobnych podstron