Comment
www.thelancet.com/oncology Vol 15 March 2014
249
a phase 1 study to establish the maximum tolerated
dose of the combination;
8
this phase 2/3 trial measured
progression-free survival as the primary endpoint.
Since only 267 patients were recruited—of whom
only 259 actually received the study drugs—the trial
was underpowered and thus, perhaps unsurprisingly,
there was no signifi cant diff erence in progression-
free survival between groups. Median progression-
free survival was 9·7 months (95% CI 8·1–14·5) in
the FOLFOX group, and 9·4 months (8·1–10·6) in the
fl uorouracil and cisplatin group (HR 0·93, 95% CI 0·70–
1·24; p=0·64). There were also no signifi cant diff erences
between groups in any of the secondary endpoints of
overall survival, proportion of endoscopic complete
responses, time to treatment failure, or occurrence of
grade 3 or 4 toxicities. The authors conclude that the
similar effi
cacy outcomes between the two treatment
regimens have implications for the potential use of
FOLFOX combination in cisplatin-intolerant patients.
Previously, cisplatin-intolerant patients have been
treated with radiotherapy alone, or with combinations
of radiotherapy and non-platinum-containing
regimens. However, most of these treatments have
worse survival outcomes when compared with standard
chemotherapy. Additionally, because of the high
inpatient and outpatient admission rates associated
with cisplatin as a result of patients requiring suitable
hydration, there is a potential cost benefi t to not
including cisplatin in a treatment regimen.
Thus, despite not improving progression-free
survival, this study has potentially shown an
improvement in the therapeutic ratio by increasing the
treatment options for cisplatin-intolerant patients,
and reducing the burden of treatment cost through
a less time-consuming and easier to administer
regimen—and thus, potentially, improving quality
of life for patients. I commend the authors for
completing this multicentre trial given its implications
for the future management strategies for oesophageal
cancer. It sets the scene for further randomised
trials designed to test similar endpoints with other
treatment regimens that contain platinum, such as a
regimen of carboplatin, paclitaxel, and radiotherapy,
which has been eff ective in the neoadjuvant
treatment of operable oesophageal carcinoma, and
has low toxicty.
9
Finally, I urge the authors of this trial
to publish their quality-of-life data. A study of this type
would be more complete with this additional data,
which could enhance the argument for replacement of
cisplatin with oxaliplatin.
Bryan Burmeister
Department of Radiation Oncology, Princess Alexandra Hospital,
Brisbane, QLD 4102, Australia
bryan_burmeister@health.qld.gov.au
I declare that I have no competing interests.
1
Al-Sarraf M, Martz K, Herkovic A, et al. Progress report of combined
chemoradiotherapy versus radiotherapy alone in patients with esophageal
cancer: an intergroup study. J Clin Oncol 1997; 1: 277–84.
2
Wong R, Malthaner R. Combined chemotherapy and radiotherapy (without
surgery) compared with radiotherapy alone in localized carcinoma of the
esophagus. Cochrane Database Syst Rev 2006; 1: CD002092.
3
Kohler RE, Sheets NC, Wheeler SB, et al. Two-year and lifetime
cost-eff ectiveness of intensity modulated radiation therapy versus
3-dimensional conformal radiation therapy for head and neck cancer.
Int J Radiat Oncol Biol Phys 2013; 87: 683–89.
4
Crosby T, Hurt CN, Falk S, et al. Chemoradiotherapy with or without
cetuximab in patients with oesophageal cancer (SCOPE1): a multicentre,
phase 2/3 randomised trial. Lancet Oncol 2013; 14: 627–37.
5
Conroy T, Galais M-P, Raoul J-L, et al. Defi nitive chemoradiotherapy with
FOLFOX versus fl uorouracil and cisplatin in patients with oesophageal
cancer (PRODIGE5/ACCORD17): fi nal results of a randomised, phase 2/3
trial. Lancet Oncol 2014; published online Feb 18. http://dx.doi.
org/10.1016/S1470-2045(14)70028-2.
6
Mauer AM, Kraut EH, Krauss SA, et al. Phase II trial of oxaliplatin, leucovorin
and fl uorouracil in patients with advanced carcinoma of the esophagus.
Ann Oncol 2005; 16: 1320–25.
7
Chiarion-Sileni V, Innocente R, Cavina R, et al. Multi-center phase II trial of
chemo-radiotherapy with 5-fl uorouracil, leucovorin and oxaliplatin in
locally advanced esophageal cancer. Cancer Chemother Pharmacol 2009;
63: 1111–19.
8
Conroy T, Viret F, Francois E, et al. Phase I trial of oxaliplatin with
fl uorouracil, folinic acid and concurrent radiotherapy for oesophageal
cancer. Br J Cancer 2008; 99: 1395–401.
9
van Hagen P, Hulschof MC, van Lanschot JJ, et al. Preoperative
chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 2012;
366: 2074–84.
Published
Online
February 13, 2014
http://dx.doi.org/10.1016/
S1470-2045(14)70073-7
See
Articles
page 315
Filling a gap in cervical cancer screening programmes
Cervical screening remains important, despite the long-
term promise of human papillomavirus (HPV) vaccination.
HPV testing is more sensitive than cytology for detection
of cervical pre-cancer and cancer, providing increased
reassurance and allowing extended screening intervals.
1
Nonetheless, the pace and manner of implementation
of primary HPV testing has varied substantially. In the
USA, HPV testing is recommended in conjunction with
cytology, whereas in the Netherlands, it is recommended
as one primary test.
2,3
In many places, it is not used at all.
Comment
250
www.thelancet.com/oncology Vol 15 March 2014
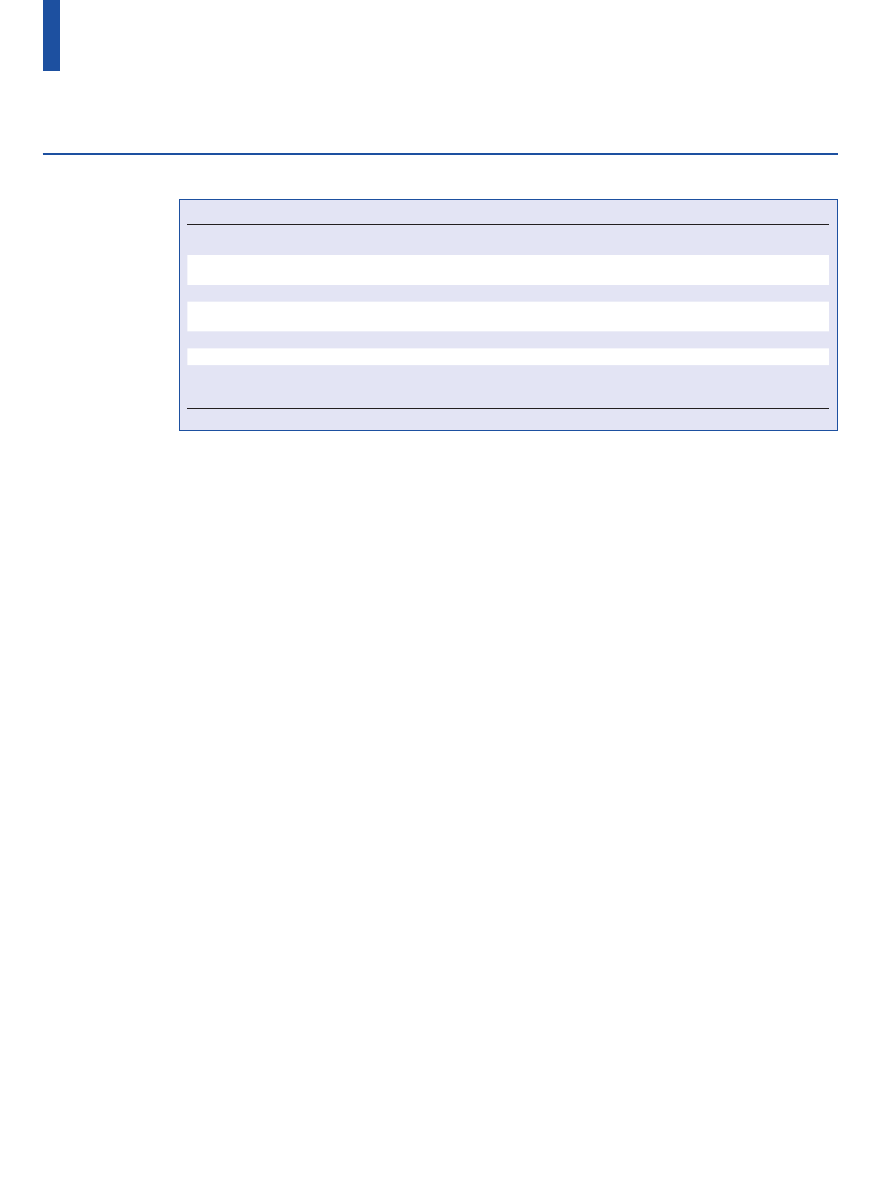
The successful introduction of HPV testing into
cervical cancer screening needs more than a sensitive
primary screening test (table). New programmes need
to be built around HPV testing. The major goal of
cervical screening programmes is to fi nd pre-cancers
that can be treated to prevent invasive cancers. A
diagnosis of pre-cancer needs colposcopic assessment
with cervical biopsies. Most HPV infections are transient;
a HPV-positive woman has a low risk of progressing
to pre-cancer and cancer. Thus, if HPV testing is used,
secondary (triage) tests are needed to decide who in
the HPV-positives needs to be referred to colposcopy. A
common suggestion is to move cytology into the role of
triage. New molecular assays such as p16/Ki-67 cytology
have higher sensitivity at comparable specifi city to
cytology.
4
Additional molecular markers such as host
methylation and HPV methylation are also being
investigated.
5–7
Irrespective of which screening and triage tests
are chosen, the crucial problem of non-participation
remains. A substantial proportion of cervical cancers in
developed countries arise in women who participate in
screening irregularly, or not at all.
8
Findings of previous
trials from the Netherlands have shown that the off er
of self-sampling for HPV testing to non-responders,
instead of an offi
ce visit, can increase participation.
9
As
with all HPV testing, women found to be HPV positive
by self-sampling need a triage test to decide who needs
colposcopy. However, self-collected samples are not
suitable for cell-based assays, such as cytology or p16/
Ki-67, so an additional collection is needed.
In The Lancet Oncology, Verhoef and colleagues
6
report the results of a randomised trial addressing
this gap in their screening programme. Investigators
enrolled initially non-participating women, found to be
HPV positive upon self-sampling, who were followed
up with two diff erent triage strategies: cytology from
physician-collected samples or methylation testing
of two genes, MAL and miR-124-2, from the self-
collected sample. The researchers found that the
clinical performance of methylation testing from the
self-collected specimen was equivalent to physician-
collected cytology. Because the assay was run from the
same specimen collected at baseline in HPV-positive
women, an additional offi
ce visit for most women
was avoided.
The Dutch team should be commended as pioneers
in the creation of an integrated HPV-based cervical
cancer screening programme. The approach described
by Verhoef and colleagues further improves the safety
net of their programme. As one possible caveat, the
participants in the trial generally reported being
screened before, and had a very high compliance
after they were included in the study, suggesting that
they were so-called soft refusers. The self-sampling
strategy might not apply as well to the fi rm refusers
who have never been screened before, putting them at
highest risk.
How do these results apply to cervical cancer
screening in other places? Findings of a recent meta-
analysis
10
showed that self-sampling has slightly
lower sensitivity compared with physician-collected
samples;in most resource-rich settings, self-sampling
is not approved as a fi rst-line alternative. The off er
of self-sampling for non-responders is especially
attractive for organised screening settings, but is
diffi
cult to implement in countries with opportunistic
screening like in the USA. Moreover, the methylation
Cytology
HPV
Co-testing (cytology and HPV)
Technology
Pap smear or liquid based cytology;
manual or computer-assisted assessment
Clinician collected or self-collected
Co-collection or separate collection
Relative repeat interval
for negative screen
Shortest (lowest negative predictive
value)
Longer (greater negative predictive
value)
Longest (greatest negative predictive value)
Triage test needed
For equivocal cytology results
For all positive results
For all HPV-positive, cytology-negative results
Triage test options
HPV or repeat cytology or p16/Ki-67
Cytology or HPV genotyping or
p16/Ki-67 or methylation
Repeat co-test or HPV genotyping or
p16/Ki-67 or methylation
Triage test sampling
Refl ex triage or separate collection
Refl ex triage or separate collection
Refl ex triage or separate collection
Diagnostic test
Colposcopy and biopsy
Colposcopy and biopsy
Colposcopy and biopsy
The three major primary screening options are cytology, HPV testing, or a combination of the two (co-testing). Not considered here is visual inspection, a screening method
under consideration for low-resource regions.
Table: Options for cervical cancer screening programmes
Comment
www.thelancet.com/oncology Vol 15 March 2014
251
assay used in the present study has not been approved
for clinical use, is not available as a kit, and has not
been assessed outside of the laboratory included in the
Dutch screening trials.
Our understanding of HPV and the natural history of
cervical cancer has brought great methods for cervical
cancer prevention, including vaccines for primary
prevention, HPV testing for screening, and various
molecular assays, including methylation markers, for
detection of cervical pre-cancers. Presented with many
HPV-related preventive options, high-resource countries
are considering various combinations; no one winning
strategy has emerged. However, low-resource countries
cannot aff ord the complex programmes established or
under development in industrialised countries. A triage
test that can be done out of self-sampling material like
the methylation assay described here could extend the
options for cervical cancer screening in low-resource
settings, where cytology programmes rarely exist
and colposcopy capacity is very restricted. However,
development of a robust, cheap methylation assay is
paramount to achieve this goal.
*Nicolas Wentzensen, Mark Schiff man
Division of Cancer Epidemiology and Genetics, National Cancer
Institute, National Institutes of Health, Rockville,
MD 20892-9774, USA (NW, MS)
wentzenn@mail.nih.gov
MS has received HPV testing at no cost for NCI studies from Roche and Becton
Dickinson. NW and MS were supported by the Intramural Research Program of
the NIH, National Cancer Institute. The views expressed do not represent the
views of the US National Cancer Institute, the National Institutes of Health, the
Department of Health and Human Services, or the US Government. We declare
that we have no competing interests.
1
Katki HA, Kinney WK, Fetterman B, et al. Cervical cancer risk for women
undergoing concurrent testing for human papillomavirus and cervical
cytology: a population-based study in routine clinical practice. Lancet Oncol
2011; 12: 663–72.
2
Health Council of the Netherlands. Population screening for cervical cancer.
2011. http://www.gezondheidsraad.nl/en/publications/prevention/
population-screening-cervical-cancer (accessed Feb 7, 2014).
3
Saslow D, Solomon D, Lawson HW, et al. American Cancer Society,
American Society for Colposcopy and Cervical Pathology, and American
Society for Clinical Pathology screening guidelines for the prevention and
early detection of cervical cancer. CA Cancer J Clin 2012; 62: 147–72.
4
Wentzensen N. Triage of HPV-positive women in cervical cancer screening.
Lancet Oncol 2013; 14: 107–09.
5
Mirabello L, Schiff man M, Ghosh A, et al. Elevated methylation of HPV16
DNA is associated with the development of high grade cervical
intraepithelial neoplasia. Int J Cancer 2013; 132: 1412–22.
6
Verhoef VMJ, Bosgraaf RP, van Kemenade FJ, et al. Triage by
methylation-marker testing versus cytology in women who test
HPV-positive on self-collected cervicovaginal specimens (PROHTECT-3):
a randomised controlled non-inferiority trial. Lancet Oncol 2014; published
online Feb 13. http://dx.doi.org/10.1016/S1470-2045(14)70019-1.
7
Wentzensen N, Sun C, Ghosh A, et al. Methylation of HPV18, HPV31, and
HPV45 genomes and cervical intraepithelial neoplasia grade 3.
J Natl Cancer Inst 2012; 104: 1738–49.
8
Spence AR, Goggin P, Franco EL. Process of care failures in invasive cervical
cancer: systematic review and meta-analysis. Prev Med 2007; 45: 93–106.
9
Gok M, Heideman DA, van Kemenade FJ, et al. HPV testing on self collected
cervicovaginal lavage specimens as screening method for women who do
not attend cervical screening: cohort study. BMJ 2010; 340: 1040.
10 Arbyn M, Verdoodt F, Snijders PJ, et al. Accuracy of human papillomavirus
testing on self-collected versus clinician-collected samples: a meta-analysis.
Lancet Oncol 2014; 15: 172–83.
Melanoma as a model for precision medicine in oncology
Published
Online
February 7, 2014
http://dx.doi.org/10.1016/
S1470-2045(14)70059-2
See
Articles
page 323
Steve
Gschmeissner/Science Photo Library
Advances in the understanding of the molecular profi le
of tumour cells and progress in systems biology and
bioinformatics have led to the promise of precision
medicine for treatment of human cancer. Melanoma
has provided an opportunity for insights into both the
potential benefi t and limitations of precision medicine
for cancer.
In 2002, half of all human melanoma cells were
shown to harbour mutations in the BRAF gene,
1
the
product of which has an important role in cell division,
diff erentiation, and secretion through the MAPK or
RAS-RAF-MEK-ERK pathways. Mutations in BRAF
result in constitutive MAPK signalling and have been
associated with a number of tumour types. The ability
to detect mutations in BRAF from tumour biopsy
specimens and the availability of highly specifi c BRAF
inhibitors have begun to change the notion of the
clinical management of patients with melanoma.
In 2011, the BRIM-3 phase 3 trial,
2
comparing the
oral BRAF inhibitor vemurafenib with dacarbazine in
675 patients with BRAF-mutated metastatic melanoma,
was reported. Vemurafenib was associated with a
signifi cant reduction in the risk of death (hazard ratio
[HR] 0·37, 95% CI 0·26–0·55; p<0·001).
2
Common
treatment-related adverse events included arthralgia,
rash, fatigue, keratocanthoma, and squamous-cell
carcinomas, with 38% of patients requiring dose
modifi cation. The results of this trial led to approval of
vemurafenib by the US Food and Drug Administration
(FDA) for patients with metastatic melanoma whose
Document Outline
Wyszukiwarka
Podobne podstrony:
European transnational ecological deprivation index and index and participation in beast cancer scre
Trend in cervical cancer screening in Spain
Increasing participation in cervical cancer screenin Telephone contact
Lower utilization of cervical cancer screening by nurses in Taiwan
New technologies for cervical cancer screening
Menagement Dile in cervical cancer
Alternative approaches to cervical cancer screening — kopia
New technologies for cervical cancer screening
Cost effectiveness of cervical cancer screening
Knowledge of cervical cancer and screening practices of nurses at a regional hospital in tanzania
Morbidity and mortality due to cervical cancer in Poland
The present ways in prevention of cervical cancer
Cytological screening for cervical cancer prevention — kopia
Perceived risk and adherence to breast cancer screening guidelines
Human Papillomavirus and Cervical Cancer Knowledge health beliefs and preventive practicies
In vitro cytotoxicity screening of wild plant extracts
Fantasy and Reality in Nazi Work Creation Programs, 1933 1936
więcej podobnych podstron