1238
C
hronic pain syndromes are reported to be a common
complication of ischemic stroke.
1
However, estimates of
the frequency from previous studies vary widely (8%–55%),
2
reflecting small sample sizes and differing patient populations,
study designs, and definitions of chronic pain.
3–14
Similarly,
the clinical consequences of chronic pain syndromes are inad-
equately understood, although they are reported to have a
negative effect on quality of life
4,5,15
after stroke.
Chronic pain syndromes may result from both central
and peripheral mechanisms and may be mediated through
nocioceptive and neuropathic processes.
1
Central poststroke
pain is a neuropathic pain syndrome, which is a direct con-
sequence of ischemic damage, and is especially challenging
to study because it usually observes an unpredictable latent
period between stroke onset and development of pain or
discomfort.
11
In contrast, most poststroke mechanical pain
syndromes have a more predictable natural history, usually
resulting from limb spasticity or shoulder subluxation. The
small sample sizes of many previous studies (<500 patients)
have also limited their ability to study pain subtypes and risk
factors for poststroke pain.
In a large cohort of patients with recent nonsevere ischemic
stroke without a history of chronic pain included in the
Prevention Regimen for Effectively avoiding Second Stroke
(PRoFESS) trial, we determined the prevalence, determinants,
and clinical consequence of new poststroke pain syndromes.
Methods
Population
PRoFESS was a randomized controlled trial that compared com-
bination aspirin (25 mg twice daily) and extended release dipyri-
damole (200 mg twice daily) versus clopidogrel (75 mg daily) and
telmisartan 80 mg daily versus placebo, in a 2×2 factorial design, in
patient
≥ 50–55 years with recent ischemic stroke (≤ 90–120 days
before randomization). The study design and primary results of the
PRoFESS trial have been published previously.
16–18
Over 34 months,
Background and Purpose—Chronic pain syndromes are reported to be common after stroke, but most previous
epidemiological studies have generally included small cohorts of patients with relatively short-term follow-up. In a
large cohort with ischemic stroke (Prevention Regimen for Effectively avoiding Second Stroke [PRoFESS] trial), we
determined the prevalence, risk factors, and clinical consequence of new poststroke pain syndromes.
Methods—Within the PRoFESS trial (mean follow-up 2.5 years), a standardized chronic pain questionnaire was administered
(at the penultimate follow-up visit) to all participants who reported chronic pain since their stroke and did not have a
history of chronic pain before their index stroke. Multivariable logistic regression analyses were used to determine risk
factors for poststroke pain (and pain subtypes), and the association between poststroke pain and cognitive (
≥3 reduction
in Mini-Mental State Examination score) and functional decline (
≥1 increase in m-Rankin).
Results—In total, 15 754 participants were included; of which 1665 participants (10.6%) reported new chronic poststroke
pain, and included 431 participants (2.7%) with central poststroke pain, 238 (1.5%) with peripheral neuropathic pain,
208 (1.3%) with pain from spasticity, and 136 participants (0.9%) with pain from shoulder subluxation. More than 1 pain
subtype was reported in 86 participants (0.6%). Predictors of poststroke pain included increased stroke severity, female
sex, alcohol intake, statin use, depressive symptoms, diabetes mellitus, antithrombotic regimen, and peripheral vascular
disease. A new chronic pain syndrome was associated with greater dependence (odds ratio, 2.16; 95% confidence interval,
1.82–2.56). Peripheral neuropathy and pain from spasticity/shoulder subluxation were associated with cognitive decline.
Conclusions—Chronic pain syndromes are common after ischemic stroke and are associated with increased functional
dependence and cognitive decline. (Stroke. 2013;44:1238-1243.)
Key Words: epidemiology
■
ischemic stroke
■
pain
Chronic Pain Syndromes After Ischemic Stroke
PRoFESS Trial
Martin J. O’Donnell, MB, PhD; Hans-Christoph Diener, MD; Ralph L. Sacco, MD; Akbar A. Panju, MD;
Richard Vinisko, MA; Salim Yusuf, MD, Dphil; On Behalf of PRoFESS Investigators
Received July 13, 2012; accepted February 19, 2013.
From the Population Health Research Group, McMaster University, Hamilton, Ontario, Canada (M.J.O'D., S.Y.); HRB-Clinical Research Facility, NUI
Galway, Galway, Ireland (M.J.O’D.); Department of Neurology, University Hospital, Essen, Germany (H.-C.D.); Miller School of Medicine, University of
Miami, Miami, FL (R.L.S.); Hamilton Health Sciences (A.A.P.) McMaster University, Hamilton, Ontario, Canada; Biostatistics Group (D.C.), Boehringer
Ingelheim Pharmaceuticals, Ridgefield, CT (R.V.).
Steven Cramer, MD, was guest editor for this article.
Correspondence to Martin O’Donnell, MD, Population Health Research Institute, DBCVS Research Institute, McMaster University, 3rd Floor, 237
Barton St E, Hamilton, Ontario, L8L 2X2, Canada. E-mail odonnm@mcmaster.ca
© 2013 American Heart Association, Inc.
Stroke is available at http://stroke.ahajournals.org
DOI: 10.1161/STROKEAHA.111.671008
2013
74
Sowmitha

O’Donnell et al Pain Syndromes After Ischemic Stroke 1239
20 332 patients were randomized from 695 centers in 35 countries
and were followed up for a mean duration of 30 months.
Measurement of Chronic Pain
Chronic pain was measured at the penultimate visit of the trial. At that
time, participants who did not report a history of chronic pain before
their stroke (based on questionnaire) were included in the poststroke
chronic pain substudy. Each participant was asked whether they had
pain, discomfort, or unpleasant sensation for 15 days or more since
their stroke. If they answered yes, the research nurse/assistant com-
pleted a standardized worksheet assessment of the following factors:
character of pain (aching, dull, sharp, cramping, burning, shooting,
electric, and lightening), frequency of pain (every day, most days, or
less than once per week), severity of pain/discomfort (scale of 0–10),
time of onset after stroke (<1 week, 1 week-3 months, 3–6 months, or
>6 months), location of pain (anatomically and whether pain location
is in the area of weakness or sensory deficit after stroke), other associ-
ated features (hypersensitivity to touch and pain when touched), and
frequency of taking pain medications. Information from the worksheet
was kept at the local site but not included in the central database, and
therefore not reported here. After completion of the standardized as-
sessment, those participants who reported chronic pain were reviewed
by the local neurologist, who was asked to complete a form detailing
the primary pathogenesis of the chronic pain syndrome, which includ-
ed central poststroke pain, pain from shoulder subluxation, peripheral
neuropathy, pain attributable to limb spasticity, and other.
Measurement of Cognitive Function and Functional
Dependence
Cognitive function was measured with the Mini-Mental State
Examination
19
(MMSE, ranging from 0 to 30), which was completed
at 1-month and penultimate follow-up visit. A loss of
≥3 points was
considered a clinically meaningful change in cognitive function dur-
ing follow-up.
20
Dependence was measured with the modified-Rankin
scale score (range 0 to 5), which was measured at baseline and pen-
ultimate follow-up visit. A reduction of
≥1 point (from baseline to
penultimate follow-up visit) was considered a clinically meaningful
change in disability/dependence during follow-up.
Confounding Variables
All confounder variables were collected at the time of randomiza-
tion. Stroke severity was measured using the National Institutes of
Health Stroke Scale (NIHSS). Ethnicity was categorized as white
versus nonwhite. History of myocardial infarction, stroke, hyper-
tension, diabetes mellitus, hypercholesterolemia, atrial fibrillation,
congestive heart failure, and peripheral vascular disease was based
on patient report. Depression was defined as feeling sad or blue
for
≥2 weeks. Smoking was categorized as never/former (reference)
or current. Exercise was categorized as mainly nonsedentary (refer-
ence) versus sedentary (some or intense regular exercise). Alcohol
intake was categorized into never/former, current (subcategorized as
0–14 drinks per month and
≥15 drinks per month). Allocation to an-
tiplatelet regimen (aspirin/dipyridamole or clopidogrel) and telmisar-
tan or placebo was recoded at randomization. Body mass index was
recorded at baseline.
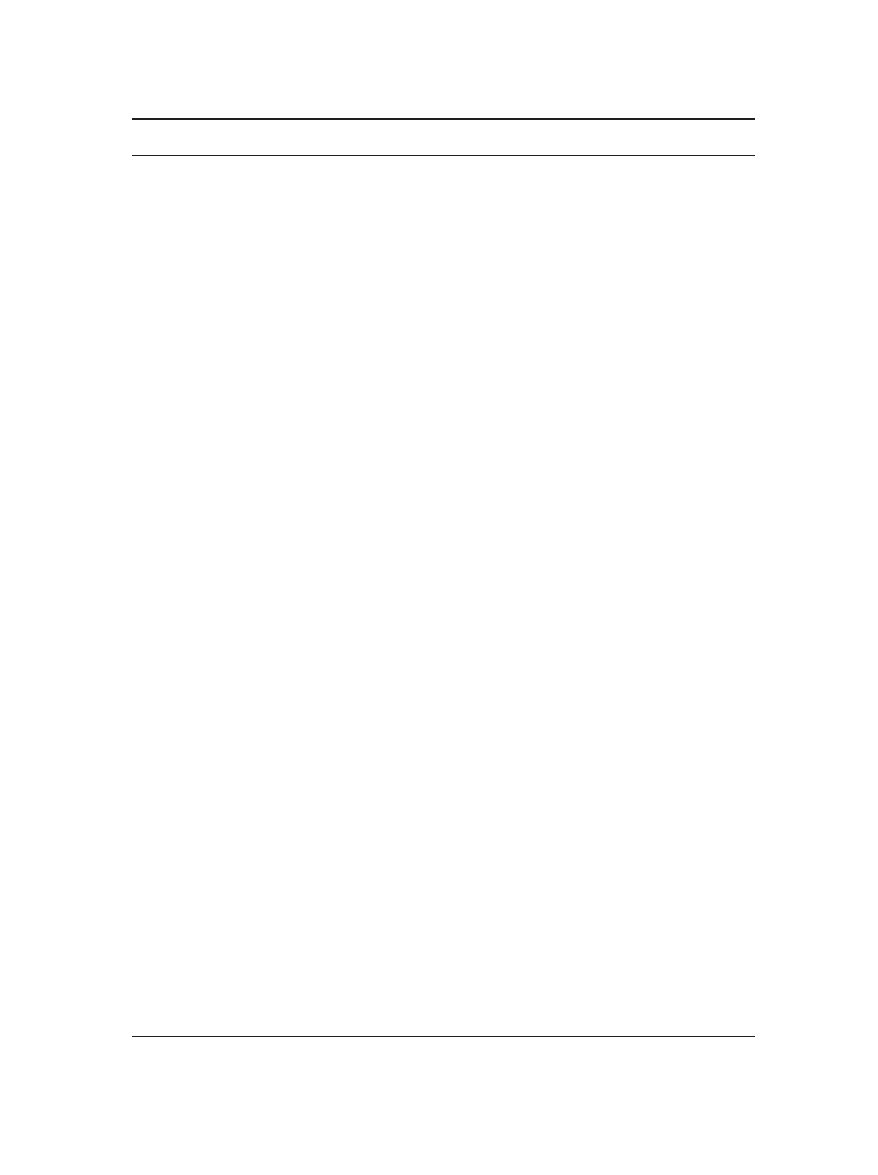
Analysis Plan
Baseline differences in characteristics between participants with and
without new chronic pain on follow-up were compared using
χ
2
and
t
test, as shown in Table 1. Risk factors for developing poststroke
pain were identified using multivariable logistic regression analysis.
Baseline factors that were significant on univariate analysis (P<0.05),
or proposed to increase the risk of chronic pain, were included in
the multivariable model for all poststroke pain, and the same multi-
variable models were retained for individual chronic pain subtypes
(central post stroke pain, peripheral neuropathy, pain from spasticity,
or shoulder subluxation). Table 2 lists all variables included in the
final model.
The association between chronic pain and decline in MMSE score
and m-Rankin score was determined using multivariable logistic re-
gression models. For both models, we included the following vari-
ables: age, sex, modified-Rankin scale score at baseline, MMSE
score at 1 month (MMSE was not recorded at baseline), NIHSS
score at baseline, sex, previous history of stroke, ischemic stroke
subtypes (small vessel versus other), myocardial infarction and, co-
morbid risk factors, including hypertension, body mass index, atrial
fibrillation, peripheral vascular disease, congestive heart failure,
myocardial infarction, diabetes mellitus, hyperlipidemia, sedentary
lifestyle, smoking, alcohol intake, and previous history of depres-
sion. Separate models were generated for all poststroke and chronic
pain subtypes (central poststroke pain, peripheral neuropathy, pain
from spasticity, or shoulder subluxation). Estimates of association
were reported using odds ratios and 95% confidence intervals (CIs).
All analyses were conducted using SAS Version 8.2 for Unix (SAS
Institute Inc, Cary, NC).
Results
Of 20 332 patients who were randomized, 1495 patients had
died, 125 were lost to follow-up, and 2958 patients reported
previous chronic pain before their stroke or were unavailable
to complete the chronic pain questionnaire at penultimate
visit. Therefore, 15 754 participants without chronic pain
before stroke were included in this analysis. Mean NIHSS
score was 2.73 (SD 2.79).
Prevalence of Chronic Pain
In total, 1665 participants (10.6%; 95% CI, 10.1%–
11.0%) developed poststroke chronic pain, and included
431 participants (2.7%; 95% CI, 2.5–3.0%) with central
poststroke pain, 238 (1.5%; 95% CI, 1.3–1.7%) with
peripheral neuropathy, 208 (1.3%; 95% CI, 1.1–1.5%) with
pain attributable to spasticity, 136 (0.9%; 95% CI, 0.7–1.0%)
with pain attributable to shoulder subluxation, 739 (4.7%;
95% CI 4.4–5.0%) with other pain syndromes. More than
1 pain pathogenesis was reported in 86 participants (0.6%),
and the most common combinations were pain attributable to
spasticity and central pain (n=17) and the combination of pain
attributable to spasticity and shoulder pain (n=15).
Risk Factors for Poststroke Pain
On multivariable analyses, significant risk factors for all post-
stroke pain were increased stroke severity, female sex, alcohol
intake, previous depression, statin use or hyperlipidemia, dia-
betes mellitus, peripheral vascular disease, and random alloca-
tion to aspirin/dipyridamole. For central poststroke pain, the
significant predictors were younger age, previous depression,
current smoking, and increased baseline stroke severity. For
peripheral neuropathy, random allocation to aspirin/dipyridam-
ole, increased body mass index, small-vessel stroke, current
smoking, diabetes mellitus, and previous history of depres-
sion were all significantly associated. For the composite of
pain from spasticity/shoulder subluxation, younger age, lower
body mass index, previous history of depression, and increased
stroke severity were all significantly associated (Table 2).
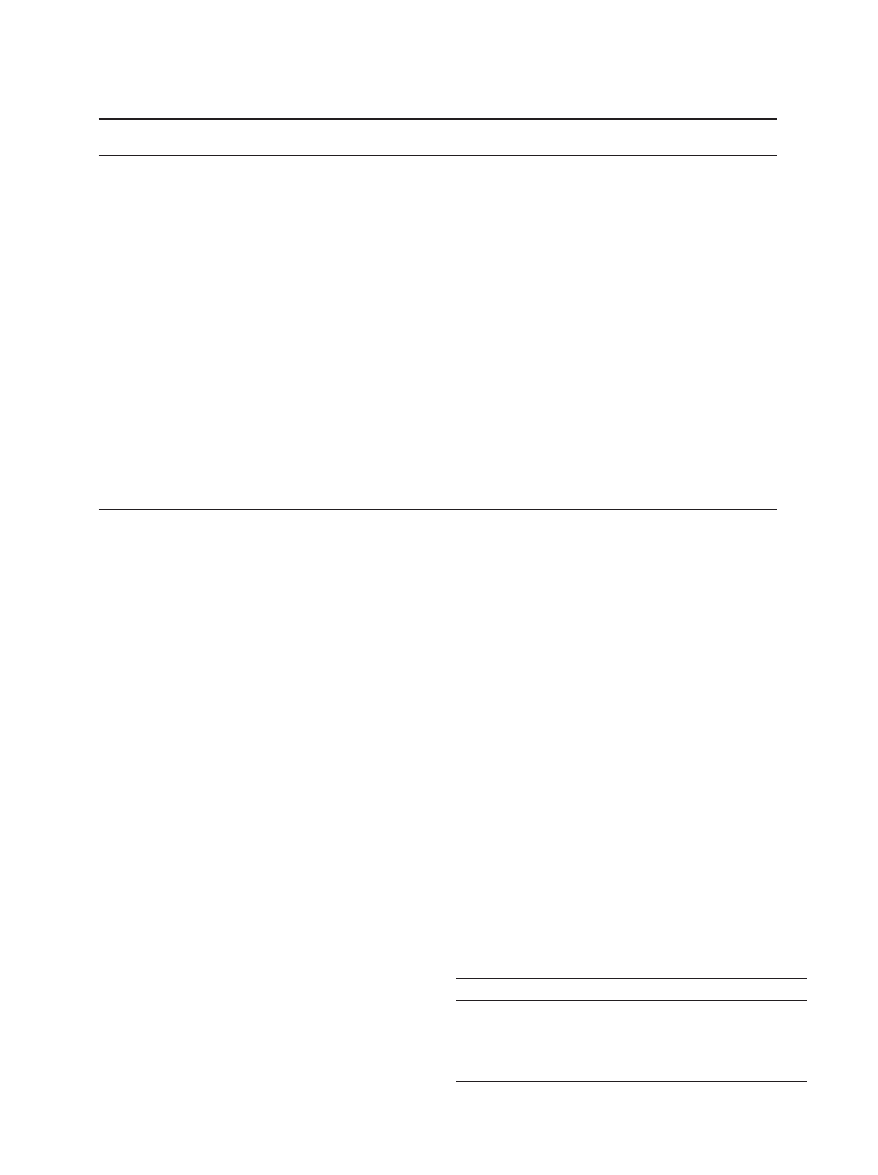
Poststroke Pain, Cognitive Decline, and Disability
Dependence
A decline in MMSE (
≥3 points) occurred in 8.8% of patients
who did not develop chronic poststroke pain compared with
1240 Stroke May 2013
Table 1. Descriptive Variables (No Poststroke Pain Compared With Poststroke Pain)
Characteristics
No PSP
(N=14 089)
PSP
(N=1665)
All Trial
(N=15 754)
P Value*
Age (mean, SD)
65.8 (8.4)
65.1 (8.3)
65.8 (8.4)
0.002
Female (N, %)
4785 (34.0)
624 (37.5)
5409 (34.3)
0.004
Baseline NIHSS (mean, SD)
2.67 (2.76)
3.23 (2.95)
2.73 (2.79)
<0.0001
m-Rankin (baseline, N, %)
<0.0001
0
2067 (14.7)
155 (9.3)
2222 (14.1)
1
5504 (39.1)
545 (32.7)
6049 (38.4)
2
3507 (24.9)
449 (27.0)
3956 (25.1)
3–5
3011 (21.4)
516 (31.0)
3527 (22.4)
MMSE (mean, SD) 1-month
27.14 (3.92)
27.04 (4.00)
27.13 (3.93)
0.34
TOAST classification
0.48
Large-artery (N, %)
4059 (28.8)
491 (29.5)
4550 (28.9)
Cardioembolism (N, %)
246 (1.7)
21(1.3)
267 (1.7)
Small-artery occlusion (N, %)
7360 52.2
883 53.0
8243 (52.3)
Other determined (N, %)
285 (2.0)
34 (2.0)
319 (2.0)
Undetermined (N, %)
2130 (15.1)
235 (14.1)
2365 (15.0)
Previous stroke/TIA (N, %)
3354 (23.8)
416 (25.0)
3770 (23.9)
0.27
Myocardial infarction (N, %)
841(6.0)
125 (7.5)
966 (6.1)
0.01
CHF (N, %)
320 (2.3)
45 (2.7)
365 (2.3)
0.27
PVD (N, %)
346 (2.5)
62 (3.7)
408 (2.6)
0.002
Atrial fibrillation (N, %)
344 (2.4)
31 (1.9)
375 (2.4)
0.14
Diabetes mellitus (N, %)
3745 (26.6)
515 (30.9)
4260 (27.0)
0.0002
Hypertension (N, %)
10 368 (73.6)
1242 (74.6)
11 610 (73.7)
0.38
Hyperlipidemia (N, %)
6438 (45.7)
849 (51.0)
7287 (46.3)
<0.0001
Previous depression (N, %)
2102 (14.9)
396 (23.8)
2497 (15.9)
<0.0001
Ethnicity (N, %)
<0.0001†
White
7986 (56.7)
981 (58.9)
8967 (56.9)
Chinese
2768 (19.6)
305 (18.3)
3073 (19.5)
South Asian
1234 (8.8)
98 (5.9)
1332 (8.5)
Other
2101 (14.9)
281 (16.9)
2382 (15.1)
BMI (mean, SD)
26.7 (4.8)
27.1 (5.0)
26.7 (4.8)
0.002
Alcohol use (N, %)
0.02
0 drinks
8948 (63.5)
1020 (61.3)
9968 (63.3)
1–14 drinks
4264 (30.3)
515 (30.9)
4779 (30.3)
≥15 drinks
781 (5.5)
118 (7.1)
899 (5.7)
Missing
96 (0.7)
12 (0.7)
108 (0.7)
Smoker (current)
2990 (21.2)
376 (22.6)
3366 (21.4)
0.102
Exercise (N, %)
0.016
Sedentary
4738 (33.6)
612 (36.8)
5350 (34.0)
Some
4585 (32.5)
494 (29.7)
5079 (32.2)
Intense
4687 (33.3)
544 (32.7)
5231 (33.2)
Missing
79 (0.6)
15 (0.9)
94 (0.6)
Clopidogrel (N, %)
7108 (50.5)
774 (46.5)
7882 (50.0)
0.002
Aggrenox (N, %)
6981 (49.5)
891 (53.5)
7872 (50.0)
Telmisartan (N, %)
7036 (49.9)
837 (50.3)
7873 (50.0)
0.8
Placebo (N, %)
7053 (50.1)
828 (49.7)
7881 (50.0)
BMI indicates body mass index; CHF, congestive heart failure; NIHSS, National Institutes of Health Stroke Scale; PSP, poststroke pain; PVD,
peripheral vascular disease; and TIA, transient ischemic attack.
*P value relates to comparison between patients with and without PSP.
†P value for comparison of White/European, Chinese, South Asian, Other Asian, African, Native Latin, and other.
O’Donnell et al Pain Syndromes After Ischemic Stroke 1241
10.7% of patients who developed chronic poststroke pain. On
multivariate analysis, peripheral neuropathy (odds ratio, 1.80;
1.24–2.62) and shoulder spasticity (odds ratio, 1.44; 1.02–2.02)
were associated with cognitive decline. A decline in m-Rankin
(
≥1 points) occurred in 8.7% of patients who did not develop
chronic poststroke pain compared with 13.7% of patients who
developed chronic poststroke pain. All chronic pain syndromes
(odds ratio, 2.16; 1.82–2.56) were associated with an increase
in disability/dependence on follow-up (Table 3).
Recurrent Major Vascular Events
Recurrent stroke was reported in 142 patients (8.5%) who
developed chronic pain and in 1030 patients (7.3%) who did
not develop chronic pain (P=0.07). Myocardial infarction
was reported in 30 patients (1.8%) who developed chronic
pain and in 180 patients (1.3%) who did not develop chronic
pain (P=0.08).
Discussion
We found that new chronic pain syndromes were common
after nonsevere ischemic stroke, affecting
≈1 in 10 patients.
Within stroke-specific pain subtypes, central pain was the
most common, and accounted for one quarter of all chronic
pain syndromes in this population. Increased stroke sever-
ity and previous depression were the most robust risk factors
for all stroke syndromes. The development of chronic pain
was associated with greater cognitive decline and functional
dependence on follow-up.
Our study is the largest to determine the prevalence of
chronic pain syndromes after ischemic stroke. Our estimate of
10.6% is lower than the prevalence reported in most previous
studies, which have reported varying rates of between 8%
and 55% in cohorts of patients after stroke, and definitions of
chronic pain (and methods of assessment) may vary between
studies.
3–14
In many of the previous studies that reported high
rates of chronic pain, populations were patients admitted to
hospital or a rehabilitative facility,
3,4,8–10,13
and would there-
fore have included a patient population with more severe
stroke, contrasting those included in the PRoFESS trial, in
which >85% had a baseline NIHSS score of
≤5.
16
Another
contributing factor that may explain our lower estimates com-
pared with most studies is that we excluded all patients with
a previous history of chronic pain, which would have resulted
in a lower prevalence of overall chronic pain compared with
previous studies. New poststroke pain accounted for
≈40%
of all chronic pain syndromes reported in 2 studies that dis-
tinguished stroke-associated pain from other chronic pain.
5,8
In our study, exclusion of patients with a previous history of
chronic pain allowed us to determine the frequency of chronic
pain that was most likely to be related to ischemic stroke.
Our findings show that new chronic pain syndromes are an
important long-term complication of ischemic stroke, even
Table 2. Risk Factor for Poststroke Pain and Individual Subtypes
Risk Factors
All PSP
N=1665 OR (95% CI)
CPSP
N=431 OR (95% CI)
Peripheral Neuropathy
N=238 OR (95% CI)
Spasticity or Subluxation
N=344 OR (95% CI)
Clopidogrel vs Aggrenox
0.84 (0.76–0.93)
1.00 (0.82–1.21)
0.76 (0.58–0.98)
0.90 (0.72–1.13)
Age
0.99 (0.99–1.00)
0.98 (0.97–0.99)
0.98 (0.96–1.00)
0.98 (0.96–0.99)
Male
0.84 (0.75–0.94)
0.85 (0.69–1.06)
1.05 (0.78–1.42)
0.93 (0.72–1.20)
Nonwhite
0.92 (0.82–1.04)
0.94 (0.76–1.16)
0.92 (0.69–1.23)
1.12 (0.87–1.44)
BMI
1.01 (1.00–1.02)
1.02 (1.00–1.04)
1.03 (1.01–1.06)
0.96 (0.93–0.99)
Alcohol
1–14
1.13 (1.00–1.28)
1.04 (0.83–1.32)
0.89 (0.65–1.22)
1.23 (0.95–1.60)
≥15
1.37 (1.11–1.70)
1.31 (0.88–1.95)
1.59 (0.99–2.54)
1.26 (0.79–1.99)
Current smoking
1.07 (0.94–1.23)
0.89 (0.69–1.15)
1.43 (1.05–1.94)
1.11 (0.84–1.45)
Sedentary
1.06 (0.95–1.18)
1.00 (0.81–1.23)
1.04 (0.79–1.36)
0.88 (0.69–1.12)
Statin
1.14 (1.02–1.28)
1.02 (0.82–1.27)
1.00 (0.75–1.33)
1.12 (0.87–1.43)
Previous stroke
1.09 (0.96–1.25)
1.19 (0.93–1.52)
1.07 (0.77–1.49)
1.00 (0.75–1.33)
PVD
1.44 (1.09–1.91)
1.36 (0.79–2.37)
1.31 (0.66–2.59)
1.48 (0.81–2.69)
Diabetes mellitus
1.18 (1.05–1.33)
0.96 (0.77–1.20)
1.99 (1.52–2.61)
1.12 (0.87–1.44)
Hyperlipidemia
1.12 (1.00–1.26)
0.81 (0.65–1.01)
0.97 (0.73–1.30)
0.99 (0.77–1.28)
Depressìon (baseline)
1.67 (1.47–1.89)
1.38 (1.08–1.76)
1.76 (1.30–2.38)
1.52 (1.15–2.01)
NIHSS
1.07 (1.05–1.09)
1.09 (1.05–1.12)
1.03 (0.98–1.07)
1.18 (1.14–1.21)
Small-vessel stroke
1.09 (0.98–1.21)
1.21 (1.00–1.48)
1.35 (1.03–1.76)
0.88 (0.70–1.11)
BMI indicates body mass index; CI, confidence interval; CPSP, central poststroke pain; NIHSS, National Institutes of Health Stroke Scale; OR, odds ratio;
PSP, Poststroke pain; and PVD, peripheral vascular disease.
Table 3. Multivariable Between Poststroke Pain and MMSE
and m-Rankin Change
Risk Factors
MMSE
≥3
modified-Rankin
≥1
All poststroke pain
1.16 (0.98–1.38)
2.16 (1.82–2.56)
CPSP
1.10 (0.79–1.53)
1.66 (1.17–2.37)
Peripheral neuropathy
1.80 (1.24–2.62)
2.58 (1.77–3.76)
Spasticity/shoulder pain
1.44 (1.02–2.02)
3.19 (2.19–4.66)
CPSP indicates central poststroke pain; and MMSE, Mini-Mental State
Examination.

1242 Stroke May 2013
in a patient population with mild-to-moderate–severity isch-
emic stroke.
Of chronic pain subtypes, we recorded neuropathic pain
syndromes to be the most common primary pathogenesis,
accounting for 40% of all chronic pain. Within neuropathic
pain, central poststroke pain accounted for the majority of
cases. The predominance of neuropathic pain syndromes dif-
fers from most previous studies that reported nocioceptive
pain to be the most common pain subtype. Three factors may
account for the lower proportion of patients with musculo-
skeletal pain. First, our cohort included a low proportion of
patients with severe ischemic stroke, which would reduce the
proportion with musculoskeletal pain related to dependence.
21
We also found that small-vessel subtype had a borderline
association with central poststroke pain, which may be related
to greater prevalence of thalamic and brain stem ischemic
stroke. Second, our study had a longer duration of follow-
up than previous studies, which mostly followed patients 12
months or less after stroke. Central poststroke pain exhibits
a latent period, which may be up to 18 months after stroke
onset,
2
and short durations of follow-up will underestimate the
frequency of central pain. Third, central pain was not system-
atically measured in many previous studies, and is frequently
underdiagnosed because the presentation may be atypical, for
example, patients may not report 'pain'. In a cohort study to
complete a systematic prospective evaluation for central pain,
Andersen et al
11
reported a cumulative incidence of central
poststroke of 8% at 1 year, in a cohort of stroke patients who
survived the initial 6 months.
We found that increased stroke severity and premorbid
depressive symptoms were the most consistent risk factors
for chronic pain after stroke, which has been reported in a
number of previous studies.
3,5–7,9
As expected, increased stroke
severity was most strongly associated with pain attributable
to spasticity and subluxation. Surprisingly, increasing body
mass index was inversely associated with pain attributable to
spasticity/shoulder subluxation, which is not easily explained.
Premorbid depression was a potent risk factor for all pain
types, which may be attributable to a lower pain threshold or
tolerance rather than having a causal relationship. Younger age
was a predictor of chronic pain, which has been reported in a
previous study,
5
but it is unclear why younger age would be
associated with an increased risk of poststroke pain. The asso-
ciation between premorbid alcohol intake and chronic pain
was also consistent across pain subtypes. Although excess
alcohol intake has been associated with an increased risk of
peripheral neuropathy,
22
the association with moderate alcohol
consumption has not been reported nor an association with
other pain syndromes. It is plausible that alcohol intake may
also be a marker for other related factors, such as depression
and psychosocial stress. Diabetes mellitus and smoking were
significant predictors of peripheral neuropathic pain, but not
central poststroke pain, which suggests that these syndromes
may not share risk factors. Although we found that antiplatelet
regimen was associated with the development of chronic pain,
which was explained largely by an increased risk of peripheral
neuropathy (Table 2), it is not readily explained and may be
attributable to chance. A single observational study found that
dipyridamole, combined with
α-lipoic acid, increased pain
sensitivity in 54 patients with diabetic neuropathy.
23
Although
headache is a known side-effect of dipyridamole, it invariably
occurs at initiation of therapy and is usually short-lived, but
may be a confounding factor in our study.
All chronic pain syndromes were associated with an
increase in disability and dependence, whereas peripheral
neuropathy and pain from spasticity/shoulder subluxation
were associated with a significant decline in cognitive func-
tion (Table 3). Within pain subtypes, central poststroke pain
had the weakest association with cognition and dependence,
which may be attributable to an increased proportion of
patients with thalamic ischemic stroke in this group and our
observed association with small-vessel subtype. Differences
in magnitude of association for pain subtypes may be con-
founded by the medications used to treat poststroke pain
because approaches for their management differ by pain
subtype. Unfortunately, we are unable to report on which
medications were used to treat pain during the trial, which
would be expected to have an effect on cognitive and func-
tion, especially opiate analgesics, tricyclic antidepressants,
and antiseizure medications (which may also be used after
poststroke epilepsy).
24–27
Our study has a number of other limitations. First, our
cohort only included patients with mild-to-moderate–sever-
ity ischemic stroke within 90 to 120 days and excluded
patients with intracerebral hemorrhage, meaning that our
findings may not be generalizable to populations with more
severe stroke or those with intracerebral hemorrhage. In the
PRoFESS trial, >85% of patients had a baseline NIHSS score
of
≤5, and 76% of patients had a baseline m-Rankin of 0 to
2. Second, we only measured poststroke pain at a single time
point (penultimate visit), which makes our study suscepti-
ble to recall bias. Recall bias may preferentially influence
certain pain syndromes that are more likely to resolve or
improve during follow-up, such as shoulder pain.
28
Another
related source of bias concerns attrition-of-the-vulnerable,
particularly those patients who died before the penultimate
visit represented, and may be a population at highest risk
of poststroke pain. Furthermore, we are unable to deter-
mine the temporal relationship between chronic pain and
cognitive and functional decline, and are therefore unable
to determine a cause and effect. Our study did not include
participants without stroke, so we are unable to report the
proportion of new-onset pain syndromes that were attribut-
able to stroke.
29
Finally, we did not measure neuroanatomi-
cal location of ischemic stroke, which is known to be an
important determinant of central poststroke pain. Strengths
of our study include the very large sample size, well-defined
population, neurologist evaluation with standardized assess-
ment and categorization of pain subtypes, and duration of
follow-up. However, the ultimate diagnosis of chronic pain,
and its subtypes, relied on clinician assessment (with stan-
dardized information), which may have resulted in between-
site variations in prevalence.
In conclusion, chronic pain syndromes are common after
ischemic stroke, and associated with cognitive decline and
increased functional dependence. Clinical trials, designed to
prevent poststroke pain syndromes, would seem to be an obvi-
ous target of future clinical research.

O’Donnell et al Pain Syndromes After Ischemic Stroke 1243
Acknowledgments
This article was submitted on behalf of the Prevention Regimen for
Effectively avoiding Second Stroke (PRoFESS) trial investigators.
Sources of Funding
This study was funded by Boehringer Ingelheim.
Disclosures
Dr Donnell has received an unrestricted educational grant from
Boehringer Ingelheim and honoraria from Boehringer Ingelheim
and Sanofi-Aventis. Dr Diener has received honoraria, consult-
ing, and lecture fees from Abbott, AstraZeneca, Bayer Vital,
Bristol Myers Squibb, Boehringer Ingelheim, D-Pharm, Fresenius,
GlaxoSmithKline, Janssen Cilag, Merck Sharpe & Dohme, Novartis,
Novo-Nordisk, Paion, Parke-Davis, Pfizer, Sanofi-Aventis, Sankyo,
Servier, Solvay, Thrombogenics, Wyeth, and Yamaguchi, and grant
support from AstraZeneca, GlaxoSmithKline, Boehringer Ingelheim,
Novartis, Janssen-Cilag, and Sanofi-Aventis. Dr Sacco has re-
ceived honoraria and consulting fees from Boehringer Ingelheim,
GlaxoSmithKline, and Sanofi-Aventis. Dr Yusuf has received hono-
raria, consulting fees, and grant support from Boehringer Ingelheim,
Bristol Myers Squibb, Servier, Sanofi-Aventis, AstraZeneca, and
GlaxoSmithKline. The other authors have no conflicts to report.
The authors had full access to the data and take responsibility
for their integrity. All authors have read and agreed to the article as
written.
The authors meet criteria for authorship as recommended by the
International Committee of Medical Journal Editors (ICMJE) and
were fully responsible for all content and editorial decisions, and were
involved at all stages of manuscript development. The authors re-
ceived no compensation related to the development of the manuscript.
This work was supported by Boehringer Ingelheim Pharmaceuticals,
Inc. (BIPI). BIPI was given the opportunity to check the data used in
the manuscript for factual accuracy only.
References
1. Chari V, Tunks E. Poststroke pain—but multiple pain mechanisms. Pain
Res Manag
. 2010;15:24–26.
2. Klit H, Finnerup NB, Jensen TS. Central post-stroke pain: clinical char-
acteristics, pathophysiology, and management. Lancet Neurol. 2009;8:
857–868.
3. Langhorne P, Stott DJ, Robertson L, MacDonald J, Jones L, McAlpine
C, et al. Medical complications after stroke: a multicenter study. Stroke.
2000;31:1223–1229.
4. Kong KH, Woon VC, Yang SY. Prevalence of chronic pain and its impact
on health-related quality of life in stroke survivors. Arch Phys Med
Rehabil
. 2004;85:35–40.
5. Jönsson AC, Lindgren I, Hallström B, Norrving B, Lindgren A. Prevalence
and intensity of pain after stroke: a population based study focusing on
patients’ perspectives. J Neurol Neurosurg Psychiatr. 2006;77:590–595.
6. Indredavik B, Rohweder G, Naalsund E, Lydersen S. Medical complica-
tions in a comprehensive stroke unit and an early supported discharge
service. Stroke. 2008;39:414–420.
7. Appelros P. Prevalence and predictors of pain and fatigue after stroke: a
population-based study. Int J Rehabil Res. 2006;29:329–333.
8. Lundström E, Smits A, Terént A, Borg J. Risk factors for stroke-related
pain 1 year after first-ever stroke. Eur J Neurol. 2009;16:188–193.
9. Sackley C, Brittle N, Patel S, Ellins J, Scott M, Wright C, et al. The
prevalence of joint contractures, pressure sores, painful shoulder, other
pain, falls, and depression in the year after a severely disabling stroke.
Stroke
. 2008;39:3329–3334.
10. Kuptniratsaikul V, Kovindha A, Suethanapornkul S, Manimmanakorn
N, Archongka Y. Complications during the rehabilitation period in Thai
patients with stroke: a multicenter prospective study. Am J Phys Med
Rehabil
. 2009;88:92–99.
11. Andersen G, Vestergaard K, Ingeman-Nielsen M, Jensen TS. Incidence
of central post-stroke pain. Pain. 1995;61:187–193.
12. Bowsher D. Stroke and central poststroke pain in an elderly population.
J Pain
. 2001;2:258–261.
13. Widar M, Samuelsson L, Karlsson-Tivenius S, Ahlström G. Long-term
pain conditions after a stroke. J Rehabil Med. 2002;34:165–170.
14. Zorowitz RD, Smout RJ, Gassaway JA, Horn SD. Usage of pain medi-
cations during stroke rehabilitation: the Post-Stroke Rehabilitation
Outcomes Project (PSROP). Top Stroke Rehabil. 2005;12:37–49.
15. Widar M, Ahlström G, Ek AC. Health-related quality of life in persons
with long-term pain after a stroke. J Clin Nurs. 2004;13:497–505.
16. Yusuf S, Diener HC, Sacco RL, Cotton D, Ounpuu S, Lawton WA, et
al; PROFESS Study Group. Telmisartan to prevent recurrent stroke and
cardiovascular events. N Engl J Med. 2008;359:1225–1237.
17. Sacco RL, Diener HC, Yusuf S, Cotton D, Ounpuu S, Lawton WA, et al;
PROFESS Study Group. Aspirin and extended-release dipyridamole ver-
sus clopidogrel for recurrent stroke. N Engl J Med. 2008;359:1238–1251.
18. Diener HC, Sacco R, Yusuf S. Rationale, design and baseline data of a
randomized, double-blind, controlled trial comparing two antithrombotic
regimens (a fixed-dose combination of extended-release dipyridamole
plus ASA with clopidogrel) and telmisartan versus placebo in patients
with strokes: the Prevention Regimen for Effectively Avoiding Second
Strokes Trial (PROFESS). Cerebrovasc Dis 2007; 23:368–380.
19. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.” A practi-
cal method for grading the cognitive state of patients for the clinician. J
Psychiatr Res
. 1975;12:189–198.
20. Diener HC, Sacco RL, Yusuf S, Cotton D, Ounpuu S, Lawton WA et
al. Effects of aspirin plus extended-release dipyridamole versus clopido-
grel and telmisartan on disability and cognitive function after recurrent
stroke in patients with ischaemic stroke in the Prevention Regimen for
Effectively Avoiding Second Strokes (PROFESS) trial: a double-blind,
active and placebo-controlled study. Lancet Neurol 2008; 7:875–884.
21. Lindgren I, Jönsson AC, Norrving B, Lindgren A. Shoulder pain after
stroke: a prospective population-based study. Stroke. 2007;38:343–348.
22. Schuckit MA. Alcohol-use disorders. Lancet. 2009;373:492–501.
23. Al-Zamil MKh. [The use of dipyridamole (curantyl) in combination with
alpha-lipoic acid in the treatment of diabetic neuropathy with retinopa-
thy]. Zh Nevrol Psikhiatr Im S S Korsakova. 2008;108:23–26.
24. Conroy B, Zorowitz R, Horn SD, Ryser DK, Teraoka J, Smout RJ. An explo-
ration of central nervous system medication use and outcomes in stroke
rehabilitation. Arch Phys Med Rehabil. 2005;86(12 suppl 2):S73–S81.
25. Siniscalchi A, Gallelli L, De Sarro G, Malferrari G, Santangelo E.
Antiepileptic drugs for central post-stroke pain management. Pharmacol
Res
. 2012;65:171–175.
26. Siniscalchi A, Gallelli L, De Fazio S, De Sarro G. Psychic disturbances
associated with sodium valproate plus levetiracetam. Ann Pharmacother.
2007;41:527–528.
27. Tannenbaum C, Paquette A, Hilmer S, Holroyd-Leduc J, Carnahan R. A
systematic review of amnestic and non-amnestic mild cognitive impair-
ment induced by anticholinergic, antihistamine, GABAergic and opioid
drugs. Drugs Aging. 2012;29:639–658.
28. Gamble GE, Barberan E, Laasch HU, Bowsher D, Tyrrell PJ, Jones AK.
Poststroke shoulder pain: a prospective study of the association and risk
factors in 152 patients from a consecutive cohort of 205 patients present-
ing with stroke. Eur J Pain. 2002;6:467–474.
29. Klit H, Finnerup NB, Overvad K, Andersen G, Jensen TS. Pain following
stroke: a population-based follow-up study. PLoS ONE. 2011;6:e27607.
Wyszukiwarka
Podobne podstrony:
Chronic Prostatitis A Myofascial Pain Syndrome
Chronic Pain for Dummies
Ebsco Farezadi Chronic pain and psychological well being
combination teraphy chronic pain
Chronic Fatigue Syndrome
Chronic Fatigue Syndrome R Moss Morris, K Petrie (Routledge, 2001) WW
Pain following stroke, initially and at 3 and 18 months after stroke, and its association with other
Evidence for Therapeutic Interventions for Hemiplegic Shoulder Pain During the Chronic Stage of Stro
Pain following stroke A prospective study
excel 2013 professional plus trial
A systematic review and meta analysis of the effect of an ankle foot orthosis on gait biomechanics a
Pain Following Stroke A Population Based Follow Up Study
Lumbar lordosis and pelvic inclinations in adults with chronic lumbar pain
Serum cytokine levels in patients with chronic low back pain due to herniated disc
więcej podobnych podstron