Clinical Psychology and Psychotherapy
Clin. Psychol. Psychother. 18, 148–158 (2011)
Published online 25 February 2010 in Wiley Online Library (wileyonlinelibrary.com). DOI: 10.1002/cpp.684
Copyright © 2010 John Wiley & Sons, Ltd.
Dialectic Behavioural Therapy Has
an Impact on Self-Concept Clarity
and Facets of Self-Esteem
in Women with Borderline
Personality Disorder
Stefan Roepke,
1
* Michela Schröder-Abé,
2
Astrid Schütz,
2
Gitta Jacob,
3
Andreas Dams,
1
Aline Vater,
1
Anke Rüter,
1
Angela Merkl,
1
Isabella Heuser
1
and Claas-Hinrich Lammers
1
1
Department of Psychiatry, Charité-University Medicine Berlin, Campus
Benjamin Franklin, Berlin, Germany
2
Department of Psychology, Personality Psychology and Assessment,
Chemnitz University of Technology, Chemnitz, Germany
3
Department of Psychiatry and Psychotherapy, University of Freiburg Medical
Centre, Hauptstrasse, Freiburg, Germany
Identity disturbance and an unstable sense of self are core criteria of
borderline personality disorder (BPD) and signifi cantly contribute
to the suffering of the patient. These impairments are hypothesized
to be refl ected in low self-esteem and low self-concept clarity. The
objective of this study was to evaluate the impact of an inpatient dia-
lectic behavioral therapy (DBT) programme on self-esteem and self-
concept clarity. Forty women with BPD were included in the study.
Twenty patients were treated with DBT for 12 weeks in an inpa-
tient setting and 20 patients from the waiting list served as controls.
Psychometric scales were used to measure different aspects of self-
esteem, self-concept clarity and general psychopathology. Patients in
the treatment group showed signifi cant enhancement in self-concept
clarity compared with those on the waiting list. Further, the scales
of global self-esteem and, more specifi cally, the facets of self-esteem
self-regard, social skills and social confi dence were enhanced signifi -
cantly in the intervention group. Additionally, the treatment had a
signifi cant impact on basic self-esteem in this group. On the other
hand, the scale of earning self-esteem was not signifi cantly abased
in patients with BPD and did not show signifi cant changes in the
intervention group. Our data provide preliminary evidence that DBT
has an impact on several facets of self-esteem and self-concept clarity,
and thus on identity disturbance, in women with BPD. Copyright ©
2010 John Wiley & Sons, Ltd.
* Correspondence to: Dr Stefan Roepke, Department of Psychiatry, Charité-University Medicine Berlin, Campus Benjamin
Franklin, Berlin, Germany.
E-mail: stefan.roepke@charite.de

Impact of DBT on identity disturbance in BPD
149
Copyright © 2010 John Wiley & Sons, Ltd.
Clin. Psychol. Psychother. 18, 148–158 (2011)
DOI
: 10.1002/cpp
Key Practitioner Message:
• Self-concept clarity, which refers to the BPD criterion identity dis-
turbance, and facets of self-esteem, are impaired in patients with
BPD compared with reference data from healthy controls.
• Our study replicates that depressive symptoms and general psycho-
pathology are improved after a 12-week DBT programme in BPD
patients compared with a waiting list.
• The 12-week inpatient DBT treatment programme shows signifi cant
enhancement in self-concept clarity and facets of self-esteem com-
pared with the waiting list.
• Thus, in BPD patients, self-esteem and the diagnostic criteria iden-
tity disturbance, captured by self-concept clarity, can be infl uenced
with short-term psychotherapy.
Keywords:
Self-Esteem, Self-Concept Clarity, Borderline Personality
Disorder, Dialectic Behavioural Therapy, Identity Disturbance
INTRODUCTION
Borderline personality disorder (BPD) is character-
ized by a pervasive pattern of instability in inter-
personal relationships, self-image and affect as
well as by marked impulsivity (APA, 1994). Iden-
tity disturbance and an unstable sense of self con-
stitute one of the nine criteria for BPD in DSM-IV
(APA, 1994). The criterion of identity disturbance
is based on the psychoanalytic theory of identity
diffusion in borderline personality organization
(Kernberg, 1975). There is little empirical research
on the criterion of identity disturbance in BPD. The
few existing studies focus on whether this crite-
rion is specifi c to BPD (for a review see Jørgensen,
2006). In our study, we empirically measured
aspects of identity and related constructs of the
‘self’ in BPD patients (see also Schröder-Abé et al.,
under submission), and empirically assessed the
impact of an evaluated psychotherapeutic treat-
ment programme for BPD on these measures.
As existing theories vary in describing the term
‘self’, we followed the concept as defi ned by
Baumeister (1999; see Schütz, 2005, for a review)
describing the self-concept as ‘your ideas about
yourself’, identity as ‘who you are’, and self-esteem
(SE) as ‘how you evaluate yourself’. More specifi -
cally, self-concept is defi ned as a cognitive schema,
an organized knowledge structure that contains
traits, values and episodic and semantic memories
about the self, and that controls the processing of
self-relevant information (e.g., Greenwald & Prat-
kanis, 1984). Self-concept clarity (SCC) overlaps
with the construct of identity and refers to the
structural aspect of the self-concept: the extent to
which the contents of an individual’s self-concept
are clearly and confi dentially defi ned, internally
consistent and temporally stable (Campbell et al.,
1996). However, identity comprises more complex
sets of elements than SCC. They are rather dif-
fi cult to assess empirically (Campbell et al., 1996).
Thus, SCC is characteristic of people’s beliefs about
themselves and may be considered an empirically
assessable aspect of identity (Campbell et al., 1996).
Self-esteem is the evaluative dimension of the self-
concept, the ‘positivity of a person’s evaluation of
self’ (Baumeister, 1998). Various constructs are used
to describe different aspects of SE. In terms of ana-
lytical theories, basic self-esteem can be compared
with an individual’s ego-integrated libidinous and
aggressive drives as well as their derivates (Forsman
& Johnson, 1996). The concept is free of references
to perceived skills, competencies, family relations
or others’ appraisal. Instead, it refers to attitudes
that are regarded as the end result of the success-
ful merging of libidinous and aggressive emotions
into the ego, for example, warm and gratifying rela-
tions with others, the freedom to experience and
express emotions, including sexual impulses and a
sense of security and integrity (Forsman & Johnson,
1996). By contrast, earning self-esteem is defi ned
as the need to earn SE by competences and others’
appraisals (Forsman & Johnson, 1996), which means
that earning SE represents a less-adaptive aspect of
SE. Individuals high in earning self-esteem experi-
ence their sense of self-esteem as being conditional,
especially upon competence and success, and upon
the praise and approval of others. They strive hard
to do well and to be perfect (Forsman & Johnson,
1996). The hierarchical facet model of SE devel-
oped by Shavelson, Hubner and Stanton (1976) and
advanced by Fleming and Courtney (1984) states
that SE is a multidimensional construct. With an
additional subdivision of social SE into social con-

150
S. Roepke et al.
Copyright © 2010 John Wiley & Sons, Ltd.
Clin. Psychol. Psychother. 18, 148–158 (2011)
DOI
: 10.1002/cpp
fi dence and social skills, Schütz and Sellin (2006)
presented a modifi ed version of the Fleming and
Courtney (1984) model and differentiated six
factors: self-regard, social skills, social confi dence,
performance SE, physical appearance and physi-
cal abilities. Measures of SE have several clinical
implications. SE is positively related to indicators of
subjective well-being and psychological health (see
Baumeister, Campbell, Krueger, & Vohs, 2003, for
a review). High SE is associated with various posi-
tive outcomes such as optimism (Taylor & Brown,
1988), life satisfaction (e.g., Diener & Diener, 1995)
and low levels of depression (e.g., Tennen & Herz-
berger, 1987; Watson, Suls, & Haig, 2002). Further-
more, emotional instability, which is characteristic
of BPD (Ebner-Priemer et al., 2007), is negatively
related to SE (Judge, Erez, Bono, & Thoresen, 2002;
Robins, Hendin, & Trzesniewski, 2001). In addi-
tion, individuals with high SE are less prone than
others to experience stress and negative affect when
confronted with negative events (Brown & Dutton,
1995; DiPaula & Campbell, 2002). Interestingly, BPD
patients show more emotional reactivity to daily life
stress (Glaser, Mengelers, & Myin-Germeys, 2007).
Only a few studies have examined SCC and SE
in relation to features of personality disorders.
However, in normal samples, low SCC has been
shown to be related to dysfunctional personal-
ity characteristics, such as high neuroticism, low
agreeableness and low SE (Baumeister, 1998;
Campbell, 1990). Very little empirical research
has been done on the self and identity in BPD.
Wilkinson-Ryan and Westen (2000) have found a
pattern of identity disturbance that distinguishes
BPD patients from other patients and normal con-
trols. In another study, BPD patients’ mood has
been correlated with a negative view of themselves
(De Bonis, De Boeck, & Lida-Pulik, 1998). Only one
study so far has examined SCC in BPD patients.
The authors reported lower SCC in BPD patients
as compared with the general population (Pollock,
Broadbent, Clarke, Dorrian, & Ryle, 2001). In one
of our own studies, we have found the same result
of lower SCC and lower SE in women with BPD
(Schröder-Abé et al., under submission).
The present study was aimed at investigating
effects of dialectic behavioral therapy (DBT) on SE
and SCC in women with BPD. Studies investigat-
ing psychotherapeutic interventions to improve
SE in various mental disorders have yielded con-
tradictory results. Two studies (Chen, Lu, Chang,
Chu, & Chou, 2006; Knapen et al., 2005) found cog-
nitive behavioural therapy (CBT) to improve SE
in depressed patients, whereas two other studies
(Hyun, Chung, & Lee, 2005; Reynolds & Coats,
1986) found no signifi cant improvement of SE in
depressed patients. To our knowledge, however,
the possible improvement of SE and SCC through
psychotherapeutic intervention in patients with
BPD has not been studied yet. DBT was specifi cally
developed as an outpatient treatment programme
for chronically suicidal individuals meeting the cri-
teria for BPD (Linehan, Armstrong, Suarez, Allmon,
& Heard, 1991; Linehan, Heard, & Armstrong,
1993). To date, DBT has demonstrated effi cacy in
a number of randomized controlled trials for BPD
in inpatient and outpatient settings (Lynch et al.,
2007). DBT treatment strategies aim to enhance
emotion regulation by increasing awareness and
acceptance of the emotional experience, and by
changing negative affect through new learning
experiences (Linehan et al., 1993). The treatment
aims at reducing dysfunctional behaviour in four
high-priority target areas: suicidal behaviours,
intentional self-injuries, behaviours that interfere
with treatment and behaviours that prolong hospi-
talization. Randomized clinical trials revealed that
DBT reduces incidences of parasuicide and medi-
cally severe parasuicides, improves adherence to
individual therapy, and diminishes inpatients’
psychiatric days (Linehan et al., 1993).
Based on theoretical considerations and previous
empirical data, we hypothesize that DBT utilizes
different techniques that improve SE, clarify the
self-concept and thus improve identity disturbance
in BPD. Accordingly, we expected improved SCC
and SE and an overall reduction of symptoms after
12 weeks of inpatient DBT treatment in patients
with BPD.
METHOD
Participants
Forty-fi ve women with BPD were consecutively
enrolled and participated in the study. Five patients
dropped out of the study and were excluded from
analysis, two from the DBT group and three from
the waiting list group. Data from 20 patients who
completed a 12-week inpatient DBT programme
were compared with data from 20 patients from
a waiting list. All BPD patients from the interven-
tion group (DBT) were on a waiting list before
participating in the DBT programme. Patients from
the control group (waiting list) were not included
in the DBT-treatment arm of the study, but com-
pleted the DBT programme after study participa-
tion. Also, patients from the control group (waiting
Impact of DBT on identity disturbance in BPD
151
Copyright © 2010 John Wiley & Sons, Ltd.
Clin. Psychol. Psychother. 18, 148–158 (2011)
DOI
: 10.1002/cpp
list) continued treatment as usual in an outpatient
setting while waiting for the DBT programme.
Treatment as usual was not assessed more specifi -
cally. Sociodemographic characteristics, psycho-
tropic medication and comorbidity on axis I and II
of the sample are presented in Table 1.
All participants met the DSM-IV (APA, 1994)
criteria for BPD on the Structured Clinical Inter-
view for DSM-IV Personality Disorders (SCID-II;
First, Spitzer, Gibbon, Williams, & Benjamin, 1997;
Fydrich, Renneberg, Schmitz, & Witchen, 1997).
Axis I comorbidity was assessed with the Mini
International Neuropsychiatric Interview (MINI.;
Ackenheil, Stotz-Ingenlath, Dietz-Bauer, & Vossen,
1999; Sheehan et al., 1998). Lifetime diagnosis of
schizophrenia, bipolar I or II disorder, substance
abuse within the last 6 months or mental retardation
were exclusion criteria. Prior psychiatric or psycho-
therapeutic treatment was not assessed systemati-
cally and thus not included in further analyses.
Measures
Questionnaires
Psychometric Scales Assessing Self-Esteem and the
Self-Concept. Facets of self-esteem were measured
using the 32-item Multidimensional Self-Esteem
Scale (MSES; Schütz & Sellin, 2006), the modifi ed
German version of the scale by Fleming and Court-
ney (Fleming & Courtney, 1984). The question-
naire comprises six subscales: self-regard, social
skills, social confi dence, performance SE, physical
appearance and physical abilities. Two of the sub-
scales capture different aspects of SE in social con-
texts: The social skills scale captures the perception
of a person’s own capacity to interact with others,
whereas the social confi dence scale captures the
ability to handle criticism from others. The sub-
scale self-regard captures the emotional compo-
nent of SE, the emotional evaluation of the self.
The performance scale captures the perception of
technical and professional abilities. All subscales
consist of fi ve items, except for self-regard, which
consists of seven items. Additionally, the subscales
are combined to form a Global SE index, which
comprises all subscales. Responses were made on
7-point scales with endpoints labelled not at all (1)
and very much (7) or never (1) and always (7), respec-
tively. Previous research indicated internal con-
sistency reliabilities in a healthy sample between
0.75 and 0.87 (Cronbach’s alpha; Schütz & Sellin,
2006). Values for internal consistency in the present
sample are presented in Table 2. Test–retest reli-
abilities of MSES sum and subscales were between
0.46 and 0.86 (Schütz & Sellin, 2006).
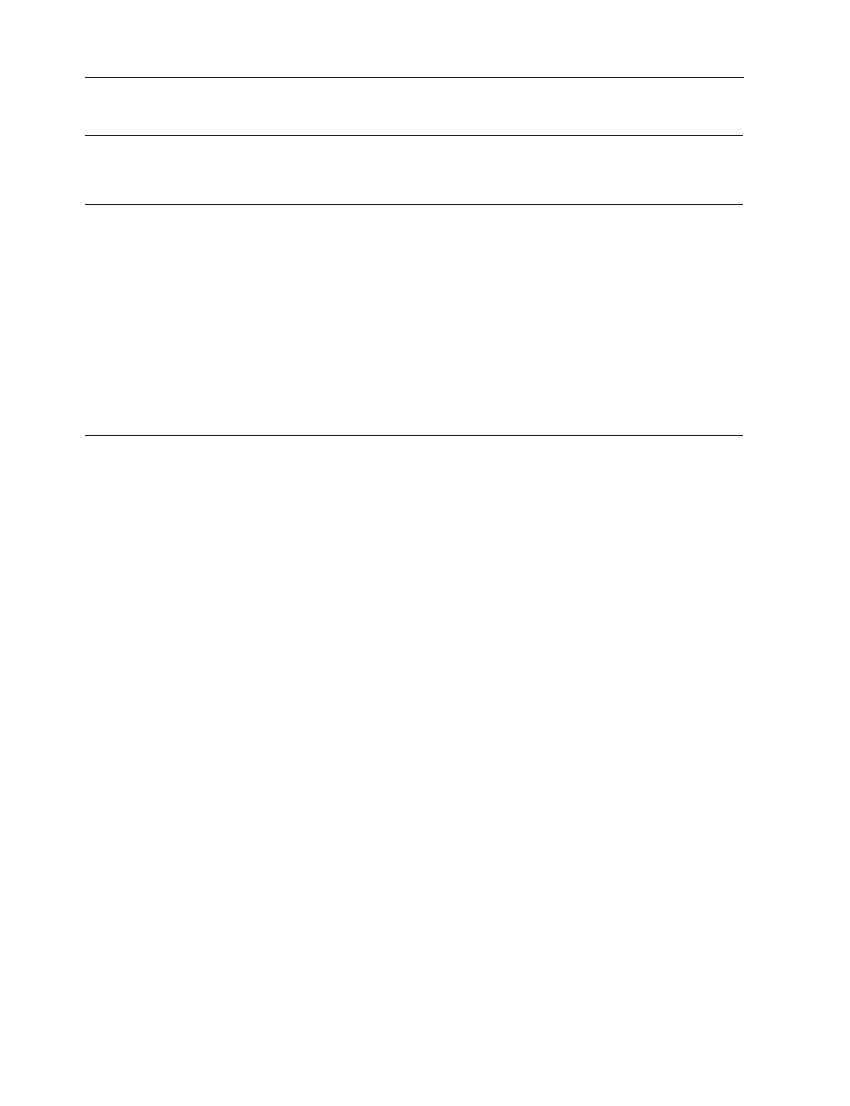
Table 1. Socioedemographic data, psychotropic medication and comorbidity of patients in the intervention group
(DBT) and control group
DBT
CG
t test
M (SD)
M (SD)
Age
27.7 (6.7)
32.5 (7.5)
t
= −2.1, df = 38, p = 0.04*
frequency (%)
frequency (%)
χ
2
-tests
Psychotropic med.
16 (80)
14 (70)
χ
2
= 0.53, df = 1, p = 0.47
SSRI
16 (80)
11 (55)
χ
2
= 2.85, df = 1, p = 0.09
aNL
6 (30)
7 (35)
χ
2
= 0.11, df = 1, p = 0.74
Axis I
Depression, lifetime
8 (40)
8 (40)
χ
2
= 0.00, df = 1, p = 1
Dysthymia
9 (45)
8 (40)
χ
2
= 0.10, df = 1, p = 0.75
PTSD
6 (30)
5 (25)
χ
2
= 0.13, df = 1, p = 0.72
Substance abuse
6 (30)
5 (25)
χ
2
= 0.13, df = 1, p = 0.72
Eating disorder
10 (50)
5 (25)
χ
2
= 2.67, df = 1, p = 0.10
Axis II
Avoidant PD
5 (25)
8 (40)
χ
2
= 1.03, df = 1, p = 0.31
Dependent PD
3 (15)
1 (5)
χ
2
= 1.11, df = 1, p = 0.29
Paranoid PD
1 (5)
3 (15)
χ
2
= 1.11, df = 1, p = 0.29
Histrionic PD
1 (5)
0 (0)
χ
2
= 1.03, df = 1, p = 0.31
* p
< 0.05.
M
= mean. SD = standard deviation. PTSD = Posttraumatic Stress Disorder. PD = Personality Disorder. SSRI = selective serotonin
reuptake inhibitor. aNL
= atypical neuroleptic. DBT = DBT intervention group (n = 20). CG = control group (n = 20).
152
S. Roepke et al.
Copyright © 2010 John Wiley & Sons, Ltd.
Clin. Psychol. Psychother. 18, 148–158 (2011)
DOI
: 10.1002/cpp
Basic self-esteem was assessed by the 38-item
Basic Self-Esteem Scale (BSE; Forsman & Johnson,
1996; e.g., ‘I can freely express what I feel’).
Responses were made on a 5-point scale, ranging
from strongly disagree (1) to strongly agree (5). Cron-
bach’s alpha internal consistency reliability was
reported as 0.92 in the validation study of the scale
(Forsman & Johnson, 1996). Internal consistency of
the scale in the present study is reported in Table 2.
Earning self-esteem was measured by the
28-item Earning Self-Esteem (ESE) Scale (Forsman
& Johnson, 1996; e.g., ‘If people say that they like
me, my self-esteem is strengthened quite a lot’).
Responses were made on a 5-point scale, ranging
from 1 (strongly disagree) to 5 (strongly agree). Inter-
nal consistency reliability was reported as 0.76
(Cronbach’s alpha) in the validation study of the
scale (Forsman & Johnson, 1996). Values for the
reliability of the present sample are reported in
Table 2. The test–retest reliabilities of ESE (0.723)
and BSE (0.735) were calculated from the control
group of the present study as data were not pro-
vided in the validation study of the scales (Forsman
& Johnson, 1996).
Self-concept clarity (SCC) was measured using
the German version of the 12-item Self-Concept
Clarity Scale (Campbell et al., 1996; Stucke, 2002).
Participants responded to each item using a 5-point
scale with endpoints 1 (strongly disagree) and 5
(strongly agree). Internal consistency reliability was
reported as 0.86 (Cronbach’s alpha) on average in
the validation study of the scale (Campbell et al.,
1996). Reliability of the scale in the present sample
is reported in Table 2. Test–retest reliability of the
scale was reported as 0.79 in the validation study
of the scale (Campbell et al., 1996).
Psychometric Scales Assessing Severity of Psycho-
pathological Symptoms. The German version of the
21-item Beck Depression Inventory (BDI; Beck,
Ward, Mendelson, Mock, & Erbaugh, 1961; Hautz-
inger, Bailer, Worall, & Keller, 1994) was employed
to assess severity of depression. Test–retest reli-
ability of the BDI was reported as 0.93 (Beck, Steer,
Ball, & Ranieri, 1996).
The SCL-90-R was used to assess current subjec-
tive experience of symptoms (Franke, 1995). The
Global Severity Index (GSI), which comprises all
subscales of the SCL-90-R, was used to measure
global psychopathological impairment. Responses
were made on 5-point scales with end points
labelled not at all (0) and very much (4). Test–retest
reliability of the GSI of the SCL-90-R was reported
as 0.92 (Franke, 1995).
Procedure
The study was conducted at the Borderline
Research Unit of the Department of Psychiatry
and Psychotherapy, Charité, University Medicine
Berlin, Campus Benjamin Franklin. The interven-
tion group was treated with a 12-week DBT pro-
gramme following Linehan’s DBT manual adapted
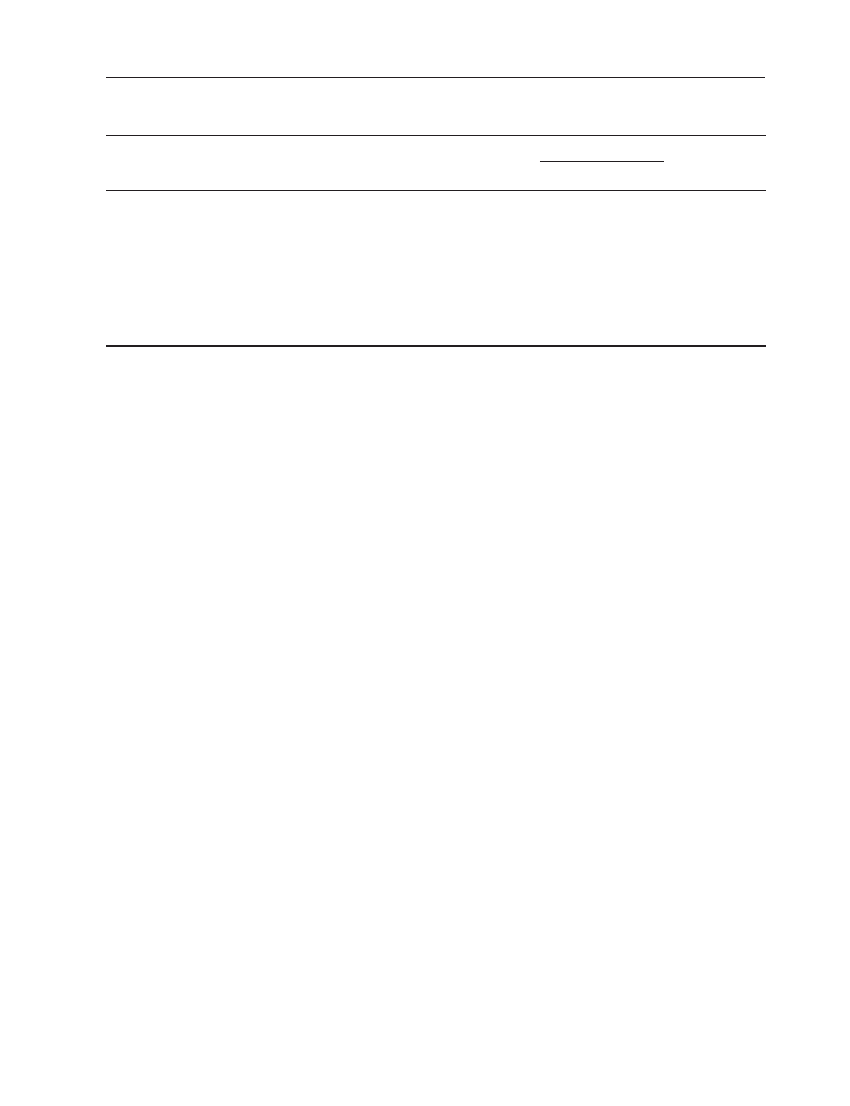
Table 2. Self-esteem and self-concept clarity in the total group of patients with BPD prior to intervention and
comparison with reference data from healthy samples
Chronbach’s
alpha
Study group,
n
= 40
M (SD)
Reference data
d-value
n
M (SD)
SCC
0.76
1.98 (0.62)
126
†
3.74 (0.94)
−2.21*
BSE
0.72
2.21 (0.34)
26
‡
3.59 (0.39)
−3.77*
ESE
0.81
3.64 (0.44)
26
‡
3.51 (0.36)
0.32, n.s.
††
MSES global SE
0.88
2.54 (0.72)
214
§
4.74 (0.95)
−2.61*
MSES self-regard
0.79
2.53 (0.84)
231
§
5.21 (1.11)
−2.72*
MSES social skills
0.78
2.52 (1.08)
234
§
5.01 (1.30)
−2.08*
MSES social confi dence
0.84
2.31 (1.07)
227
§
5.65 (1.42)
−2.66*
MSES performance SE
0.72
3.02 (1.18)
225
§
5.08 (1.02)
−1,87*
MSES physical appearance
0.88
2.24 (1.16)
231
§
4.51 (1.34)
−1.81*
MSES physical abilities
0.73
2.64 (1.16)
228
§
3.97 (1.36)
−1.05*
*
= p < 0.05.
†
Data from the total sample in Stucke (2002).
‡
Data from the healthy control group in Schröder-Abé et al. (unpublished data).
§
Data from the female healthy norm sample in Schütz and Sellin (2006).
††
Higher ESE values indicate a less stable self-esteem, Cronbach’s alpha: data from both groups before treatment/waiting list.
M
= mean. SD = standard deviation. SCC = Self-concept clarity. BSE = Basic Self-Esteem Scale. ESE = Earning Self-Esteem Scale.
MSES
= Multidimensional Self-Esteem Scale.

Impact of DBT on identity disturbance in BPD
153
Copyright © 2010 John Wiley & Sons, Ltd.
Clin. Psychol. Psychother. 18, 148–158 (2011)
DOI
: 10.1002/cpp
for inpatient treatment (Bohus et al., 2004). The
inpatient DBT programme included the following
components: individual therapy (1 hour/week),
group skills training (3 hours/week), mindfulness
groups (2 hours/week), group psychoeducation (1
hour/week), peer group meetings (2 hours/week),
individual body-oriented therapy (1.5 hours/
week) and therapist team consultation meetings (2
hours/week). The individual therapy, skills train-
ing, and therapist team consultation meetings fol-
lowed Linehan’s DBT manual (Linehan et al., 1993).
The psychoeducation group included instructions
in Linehan’s bio-behavioural theory of BPD com-
bined with information on theory and research
on BPD. The mindfulness group was an extended
version of the mindfulness segment of DBT skills
training. The body-oriented therapy included
education classes about psychomotor interaction
and individually tailored exercises focusing on
improvement of the body concepts. The therapists
and the staff were trained and supervised regu-
larly by a senior DBT trainer (Christian Stiglmayr).
All DBT therapists were certifi ed psychologists or
psychiatrists. All completed or were in the fi nal
course of DBT certifi cation. DBT certifi cation addi-
tionally included 96 hours of theory training in
DBT, at least one supervised therapy case (for at
least 1 year), leading a supervised skills group for
at least 6 months and a fi nal oral examination by a
senior DBT therapist.
Structured interviews (SCID II and MINI)
were administered by trained, master-level psy-
chologists, and confi rmed by a clinical inter-
view performed by the last author (CHL, senior
psychiatrist).
Patients from the intervention group adminis-
tered all self-report scales at two different times:
at admission for the 12-week DBT programme
and after 10 weeks of DBT, to avoid effects due to
hospital discharge. Patients in the control group
were also assessed twice with approximately 10
weeks in between (M
= 9.7, SD = 3.6) while they
were waiting for DBT. The study was approved by
the Ethical Committee of the Faculty of Medicine
of the Charité-University Medicine Berlin. Written
informed consent was obtained from all patients
before they entered the study.
Statistical Analyses
All analyses were conducted with the Statistical
Package for the Social Sciences SPSS, version 14.0
(SPSS, Chicago, USA). Baseline differences between
patients and the control group were analyzed with
independent t tests or chi-square tests when appro-
priate. Time and group effects were calculated with
ANCOVAs. The signifi cance level in all of the tests
was set at 0.05 (two-tailed). Effect size d for baseline
variables and references for healthy subjects from
the literature were calculated according to Cohen
(1977). Effect sizes of main effects and interactions
for ANCOVAs were reported as eta-squared. Clini-
cal signifi cance was calculated with the reliable
change index (RCI; Jacobson & Truax, 1991). RCI
>
1.96 was considered improvement.
RESULTS
Self-Concept Clarity
Women with BPD showed signifi cantly impaired
SCC compared with reference data from healthy
subjects (Table 2). The ANCOVA model for SCC
with age as a covariate revealed a signifi cant inter-
action effect between time and group, indicating
signifi cant improvement of SCC in the interven-
tion group (Table 3), but no signifi cant changes
in the waitlisted control group. The effect size for
SCC was the largest of all variables measured in
the present study. Fifteen out of 20 patients (75%)
improved as calculated by the RCI.
Self-Esteem
Measures of basic self-esteem and all six facets of
self-esteem from the MSES scale were signifi cantly
lower in the BPD sample than in healthy controls
(Table 2). The ANCOVA model for BSE revealed
a signifi cant interaction effect between group and
time, indicating signifi cant improvement in the
intervention group (Table 3), but no signifi cant
changes in the waitlisted control group. Seven out
of 20 patients (35%) improved in BSE (according
to the RCI). The ANCOVA model for the MSES
global score and the six subscales showed signifi -
cant interactions of group and time for the global
score and the subscales of self-regard, social
skills and social confi dence, indicating signifi cant
improvement in the global score and the men-
tioned subscales in BPD patients who had been
treated with DBT. As calculated by the RCI: Eight
(40%) patients improved on the global score, six
(30%) on the self-regard scale, seven (35%) on the
social skills scale, nine (45%) on the social confi -
dence scale, two (10%) on the performance scale,
two (10%) on the physical appearance scale, three
(15%) on the physical abilities scale of the MSES
out of the 20 subjects in the intervention group.
154
S. Roepke et al.
Copyright © 2010 John Wiley & Sons, Ltd.
Clin. Psychol. Psychother. 18, 148–158 (2011)
DOI
: 10.1002/cpp
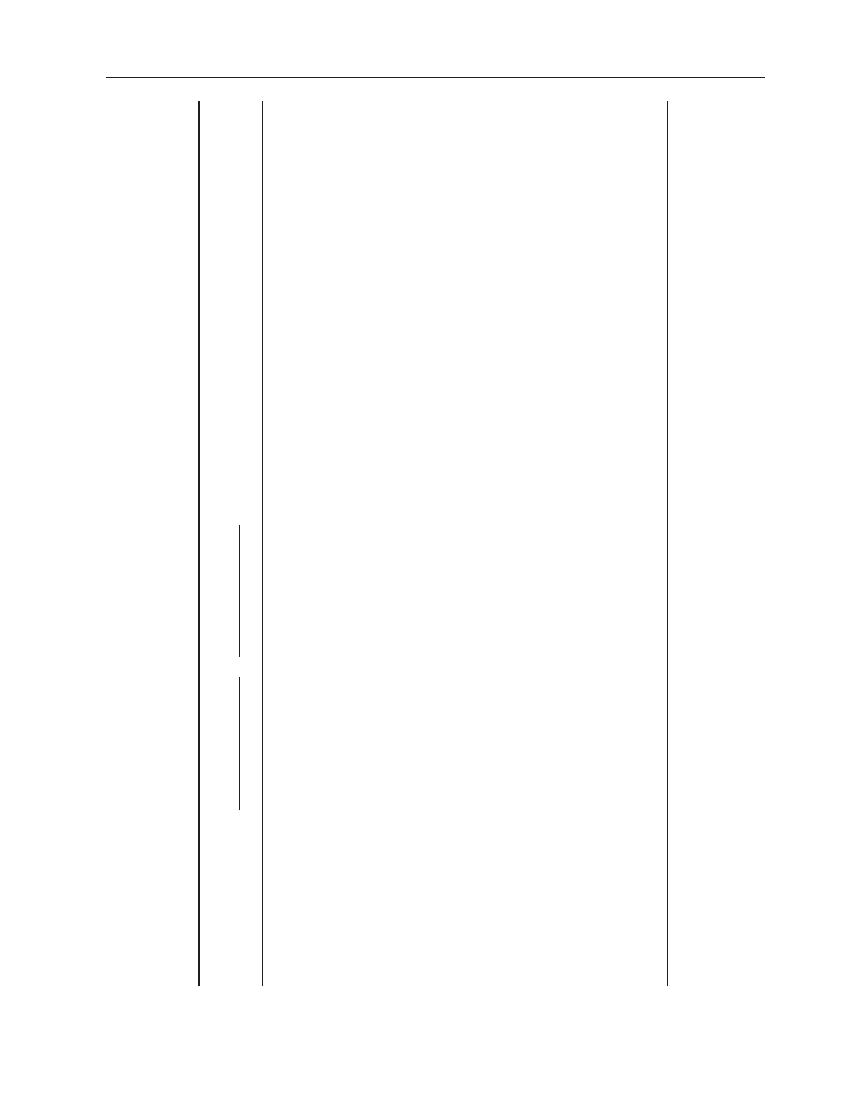
T
able 3.
Means and standar
d deviations of all outcome variables and
ANCOV
A
r
esults with all outcome measur
es as dependent varia
bles and age as
covariate
Pr
e
M (SD)
Post
M (SD)
ANCOV
A
IG
CG
IG
CG
Main ef
fect gr
oup
Main ef
fect time
Interaction gr
oup*time
SCC
1.95 (0.64)
2.02 (0.60)
3.35 (1.92)
1.92 (0.67)
F
=
18.0;
df
=
1, 36;
p
< 0.001**,
η
p
2
=
0.33
F
=
0.02;
df
=
1, 36;
p
= 0.89,
η
p
2
=
0.001
F
=
30.4;
df
=
1, 36;
p
< 0.001**,
η
p
2
=
0.46
BSE
2.21 (0.34)
2.20 (0.36)
2.60 (0.49)
2.18 (0.40)
F
=
2.44;
df
=
1, 36;
p
= 1.22,
η
p
2
=
0.06
F
=
0.16;
df
=
1, 36;
p
= 0.69,
η
p
2
=
0.01
F
=
14.0;
df
=
1, 36;
p
= 0.001*,
η
p
2
=
0.28
ESE
3.71 (0.41)
3.57 (0.47)
3.60 (0.26)
3.56 (0.50)
F
=
0.67;
df
=
1, 35;
p
= 0.42,
η
p
2
=
0.02
F
=
0.63;
df
=
1, 35;
p
= 0.43,
η
p
2
=
0.02
F
=
2.5;
df
=
1, 35;
p
= 0.12,
η
p
2
=
0.07
MSES global SE
2.46 (0.45)
2.62 (0.92)
2.90 (0.80)
2.45 (0.94)
F
=
0.09,
df
=
1, 37;
p
= 0.77,
η
p
2
=
0.002
F
=
0.01;
df
=
1, 37;
p
= 0.93,
η
p
2
=
0.00
F
=
9.6;
df
=
1, 37;
p
= 0.004*,
η
p
2
=
0.21
MSES self-r
egar
d
2.62 (0.51)
2.44 (1.08)
2.96 (0.77)
2.24 (1.03)
F
=
1.2;
df
=
1, 37;
p
= 0.28,
η
p
2
=
0.03
F
=
0.19;
df
=
1, 37;
p
= 0.67,
η
p
2
=
0.005
F
=
4.9;
df
=
1, 37;
p
= 0.033*,
η
p
2
=
0.12
MSES social skills
2.49 (1.09)
2.54 (1.09)
3.16 (1.22)
2.51 (1.10)
F
=
0.94;
df
=
1, 37;
p
= 0.34,
η
p
2
=
0.03
F
=
0.29;
df
=
1, 37;
p
= 0.59,
η
p
2
=
0.008
F
=
4.9;
df
=
1, 37;
p
= 0.034*,
η
p
2
=
0.12
MSES social confi
dence
1.99 (0.80)
2.64 (1.23)
2.93 (1.16)
2.57 (1.61)
F
=
0.1
1;
df
=
1, 35;
p
= 0.75,
η
p
2
=
0.003
F
=
0.9;
df
=
1, 35;
p
= 0.77,
η
p
2
=
0.002
F
=
10.0;
df
=
1, 35;
p
= 0.003*,
η
p
2
=
0.22
MSES performance SE
2.86 (0.92)
3.17 (1.40)
2.93 (1.10)
2.75 (1.51)
F
=
0.01;
df
=
1, 37;
p
= 0.92,
η
p
2
=
0.000
F
=
0.07;
df
=
1, 37;
p
= 0.79,
η
p
2
=
0.002
F
=
1.8;
df
=
1, 37;
p
= 0.19,
η
p
2
=
0.045
MSES physical apperar
ence
2.22 (0.96)
2.25 (1.37)
2.59 (1.34)
2.19 (1.16)
F
=
0.02;
df
=
1, 36;
p
= 0.89,
η
p
2
=
0.001
F
=
0.92;
df
=
1, 36;
p
= 0.34,
η
p
2
=
0.025
F
=
3.3;
df
=
1, 36;
p
= 0.076,
η
p
2
=
0.085
MSES physical abilities
2.52 (0.95)
2.75 (1.34)
2.82 (1.38)
2.44 (1.1
1)
F
=
0.002;
df
=
1, 36;
p
= 0.97,
η
p
2
=
0.000
F
=
0.6;
df
=
1, 36;
p
= 0.45,
η
p
2
=
0.02
F
=
1.6;
df
=
1, 36;
p
= 0.22,
η
p
2
=
0.04
BDI
32.2 (9.23)
33.6 (1
1.5)
20.9 (12.0)
32.7 (1
1.5)
F
=
2.1;
df
=
1, 35;
p
= 0.16,
η
p
2
=
0.06
F
=
6.2;
df
=
1, 35;
p
= 0.02*,
η
p
2
=
0.15
F
=
7.3;
df
=
1, 35;
p
= 0.01*,
η
p
2
=
0.17
SCL-90-R GSI
1.79 (0.52)
1.99 (0.60)
1.29 (0.72)
1.87 (0.76)
F
=
2.5;
df
=
1, 35;
p
= 0.13,
η
p
2
=
0.07
F
=
0.92;
df
=
1, 35;
p
= 0.34,
η
p
2
=
0.03
F
=
7.1;
df
=
1, 35;
p
= 0.01*,
η
p
2
=
0.17
*
p
< 0.05, **
p
< 0.001.
IG
= Intervention gr
oup (
n
=
20). CG
= Contr
ol gr
oup (
n
=
20). M
= mean. SD
= standar
d deviation. SCC
= Self-concept clarity
. BSE
= Basic self-esteem scale. ESE
= Earning
self-esteem scale. MSES
= Multidimensional self-esteem scale. BDI
= Beck depr
ession inventory
. SCL-90-R
= Symptom checklist 90 r
evised. GSI
= Global severity index.
Impact of DBT on identity disturbance in BPD
155
Copyright © 2010 John Wiley & Sons, Ltd.
Clin. Psychol. Psychother. 18, 148–158 (2011)
DOI
: 10.1002/cpp
Scores of ESE for BPD patients were not signifi -
cantly different from those of the healthy controls
(Table 2). The ANCOVA model for ESE did not
show signifi cant main effects and no interaction
effect between time and group (Table 3), indicating
no signifi cant modifi cation of ESE in either group.
Also, no patient improved as calculated by the RCI
in the intervention group.
Changes in Psychopathology and Depression
Depressive symptoms measured by the BDI and
general psychopathology measured by the GSI
of the SCL-90-R were not signifi cantly different
between the two groups at baseline (Table 3).
The BDI and the GSI of the SCL-90-R showed a
signifi cant interaction effect of time and group
in the ANCOVA model, indicating a signifi cant
improvement after a 10-week DBT programme on
both scales (Table 3), but no signifi cant changes
in the waitlisted control group. Thirteen out of
19 patients (68%) improved as calculated by the
RCI on the BDI scale. On general psychopathol-
ogy measures (GSI), 11 out of 19 patients (58%)
improved as calculated by the RCI.
DISCUSSION
We tested the impact of a 12-week inpatient DBT
programme on SE and SCC of BPD patients. We
had hypothesized that participants treated with
the DBT programme would show (a) an enhan-
cement in SCC, and thus an improvement of
identity disturbance; (b) an enhancement in SE;
and (c) an overall reduction of psychopathological
symptoms.
Within the limitations that are discussed later, all
of our hypotheses were confi rmed. We found that
SCC was signifi cantly enhanced after 10 weeks of
DBT, 75% of patients fulfi lled criteria of clinical
improvement as calculated by the RCI. This result
is of special interest as SCC overlaps with the con-
struct of identity (Campbell et al., 1996), which
indicates that DBT directly improves the degree
of the criterion ‘identity disturbance’, in DSM-IV
(APA, 1994). To our knowledge, the present study
is the fi rst to empirically demonstrate that short-
term psychotherapy is able to improve identity
disturbance in BPD patients.
DBT comprises different strategies that are can-
didates for improving identity disturbance. Thus,
validation strategies can be conceptually under-
stood to enhance the stability of the patient’s
sense of self (Lynch et al., 2006). Validation can
be considered to be steady, self-verifying feedback
from the therapist, thus leading to a perception of
coherence (Lynch et al., 2006, Swann et al., 2003).
Further, analysis and modifi cation of dysfunctional
behaviour (e.g., by chain analysis) and cognitions
(e.g., by dialectic strategies to reduce polarization)
are hypothesized to reduce BPD symptomatology
(Lynch et al., 2006) and probably improve the sense
of self, and thus SCC and identity disturbance. Fur-
thermore, mindfulness, a technique related to the
quality of awareness within a present experience
aims to improve participating and ‘becoming one’
with experience (Chapman & Linehan, 2005) could
be a candidate to improve the experience of coher-
ence and thus identity.
DBT treatment furthermore resulted in a sig-
nifi cant increase in global and basic SE of BPD
patients. Nevertheless, only 35% of patients ful-
fi lled criteria of clinical improvement on the BSE
and 45% of patients on the MSES sum score, as
calculated by the RCI. Differentiating the facets of
SE using the MSES (Schütz & Sellin, 2006), revealed
that only self-regard and the two facets of social SE,
social skills and social confi dence, improved sig-
nifi cantly after 10 weeks of DBT. Clinical improve-
ment of these facets (RCI) was found in 30–45% of
patients in the intervention group. This result sug-
gests that the improvement of global and basic SE
can be mainly attributed to pronounced changes
within the emotional and social domains of SE.
The improvement in social SE can be explained as
an effect of the intensive training of social skills
that BPD patients receive during DBT. Social dys-
function is characteristic of BPD (Hill et al., 2008),
and without social skills it is impossible to main-
tain stable interpersonal relationships, pursue long
term goals or gain self-respect in social situations.
Therefore, an increase of social skills and compe-
tence is an important source of improved SE for
patients with BPD.
Changes in the emotional domain of SE could
be attributed to specifi c techniques used in DBT
as emotion regulation is one central focus in
that therapy and is directly linked to the bioso-
cial theory of BPD (Linehan, 1993). DBT aims to
enhance emotion regulation, and thus, the teaching
of emotion regulation skills is a core intervention
(Linehan, 1993). Further, mindfulness, conceptu-
alized as an internal state for the acquisition of
various emotional and behavioural responses
(Lynch et al., 2006), could infl uence emotional
experience. Findings of activation of brain areas
related to positive affect after mindfulness train-
156
S. Roepke et al.
Copyright © 2010 John Wiley & Sons, Ltd.
Clin. Psychol. Psychother. 18, 148–158 (2011)
DOI
: 10.1002/cpp
ing point in that direction (Davidson et al., 2003).
Also, validation strategies, as core acceptance
strategies in DBT (Linehan, 1993), possibly reduce
emotional arousal (Lynch et al., 2006). Thus, self-
regard, which is the basic emotional dimension of
SE, may have been improved through the applica-
tion of these techniques in DBT.
The lack of improvement in performance and
physical ability self-esteem may be due to the fact
that DBT does not emphasize aspects related to
performance or physical ability self-concept. As
demonstrated in previous studies (Schröder-Abé
et al., under submission) earning self-esteem was
not signifi cantly impaired in BPD patients com-
pared with healthy controls. Thus, in contrast to
the improvement of global and basic SE, earning
self-esteem was not signifi cantly modifi ed after
DBT. General psychopathology and depressive
symptoms had also improved signifi cantly after
10 weeks of inpatient DBT, which dovetails with
results from previous studies (Bohus et al., 2004;
Linehan et al., 1991). Also, the percentage of
patients that clinically improved due to RCI cri-
teria were comparable to previous results, which
revealed clinical improvement in 45% of patients
after 3 months of inpatient DBT (Kleindienst
et al., 2009).
Besides specifi c DBT techniques as emotion
regulation and mindfulness, one also has to con-
sider the impact of cognitive interventions, which
are part of DBT, on SCC and SE. Self-devaluating
and self-denigrating ideas, which are expressions
of low SE, can be considered the most frequent
cognitions underlying behaviour typical of BPD.
The therapeutic correction of these dysfunctional
cognitions is also part of the DBT programme. On
the one hand, these interventions may clarify the
self-concept of BPD patients; on the other hand,
they may increase SE by reducing self-devaluat-
ing cognitions. The data showing improved SE in
depressed patients after CBT (Chen et al., 2006;
Knapen et al., 2005) argue for a positive impact
of these more general techniques on self-esteem.
Also, the successful completion of DBT therapy
and reduction of BPD symptoms may be consid-
ered general factors that lead to modifi ed SCC
and SE.
Limitations of the Study
One limitation of our study is the lack of random-
ization between the two groups. Further, the inter-
vention group was treated as inpatients, while the
control group spent that time period at home. Thus
we cannot exclude possible effects of hospitaliza-
tion and ‘unspecifi c’ intervention. In both groups,
most patients were on psychotropic medication,
thus we did not include this factor in the statistical
analysis. The effect of concomitant psychotropic
medication has to be assessed in further research.
Also, follow-up data need to be obtained in future
research to prove stability of the improvement
in SE and SCC. Depressive symptoms after DBT
(measured by the BDI) were still higher than in
other comparable studies (Linehan et al., 1993).
This could refl ect general impairment in the study
population, as inpatient programmes are especially
designed for severely disturbed patients. Neverthe-
less, depressive symptoms improved signifi cantly
in the intervention group, and previous studies
have shown that depressive symptoms are related
to low SE (Chen et al., 2006; Knapen et al., 2005),
thus improvements in SE can be directly related
to the reduction of depressive symptoms. Further
research should now provide a more fi ne-grained
analysis of the effect of CBT and specifi c therapies
such as DBT on SCC and SE in patients with BPD
and patients with major depression. Future studies
should also identify specifi c effi ciency factors of
DBT that help to improve SE and SCC in BPD
patients. Also, the impact of other specifi c proto-
coled psychotherapeutic treatments of BPD, e.g.,
transference-focused psychotherapy (Kernberg,
Yeomans, Clarkin, & Levy, 2008), mentalization-
based treatment (Bateman & Fonagy, 2009) and
the systems training for emotional predictability
and problem solving (Blum et al., 2008), on self-
concept clarity and facets of self-esteem needs to
be assessed. Finally, further studies are needed to
replicate our preliminary fi ndings and, even more
importantly, follow-up examinations are needed to
prove stability of the described impact of DBT on
self-concept clarity and facets of self-esteem.
In summary, within the described limitations,
our results indicate that a 12-week inpatient DBT
programme for women with BPD provides clini-
cally signifi cant improvement in SE and SCC.
Thus, the results of the present study argue that in
BPD patients, self-esteem and the diagnostic cri-
teria identity disturbance can be infl uenced with
short-term psychotherapy.
ACKNOWLEDGEMENTS
We thank Birgit Baumkötter, Sandra Schauen,
Alisa Zukanovic and Martina Schickart for their

Impact of DBT on identity disturbance in BPD
157
Copyright © 2010 John Wiley & Sons, Ltd.
Clin. Psychol. Psychother. 18, 148–158 (2011)
DOI
: 10.1002/cpp
help with data collection. We thank Mirja Petri
for her comments on an earlier version of the
manuscript.
REFERENCES
Ackenheil, M., Stotz-Ingenlath, G., Dietz-Bauer, A., &
Vossen, A. (1999). Mini International Neuropsychiatric
Interview (MINI), German Version 5.0.0. The develop-
ment and validation of a structured diagnostic psychi-
atric interview for DSM-IV and ICD-10. Psychiatrische
Universitätsklinik, München, Germany.
American Psychiatric Association (APA) (1994). Diagnos-
tic and statistical manual of mental disorders DSM-IV.
Washington, DC: Author.
Bateman, A., & Fonagy, P. (2009). Randomized
controlled trial of outpatient mentalization-based
treatment versus structured clinical management for
borderline personality disorder. American Journal of
Psychiatry, 166, 1355–1364.
Baumeister, R. (1999). Self in social psychology: Essential
readings (Key readings in social psychology). Hove:
Psychology Press.
Baumeister, R.F. (1998). The self. In D.T. Gilbert, S.T.
Fiske, & G. Lindzey (Eds), The Handbook of social psy-
chology (pp. 339–374). New York: McGraw-Hill.
Baumeister, R.F., Campbell, J.D., Krueger, J.I., & Vohs,
K.D. (2003). Does high self-esteem cause better perfor-
mance, interpersonal success, happiness, or healthier
lifestyles? Psychological Science in the Public Interest, 4,
1–44.
Beck, A.T., Steer, R.A., Ball, R., & Ranieri, W. (1996).
Comparison of Beck Depression Inventories -IA and -II
in psychiatric outpatients. Journal of Personality Assess-
ment, 67, 588–597.
Beck, A.T., Ward, C.H., Mendelson, M., Mock, J., &
Erbaugh, J. (1961). An inventory of measuring depres-
sion. Archives of General Psychiatry, 4, 561–571.
Blum, N., St John, D., Pfohl, B., Stuart, S., McCormick, B.,
Allen, J., Arndt, S., & Black, D.W. (2008). Systems train-
ing for emotional predictability and problem solving
(STEPPS) for outpatients with borderline personality
disorder: A randomized controlled trial and 1-year
follow-up. American Journal of Psychiatry, 165, 468–478.
Bohus, M., Haaf, B., Simms, T., Limberger, M.F., Schmahl,
C., Unckel, C., Lieb, K., & Linehan, M.M. (2004). Effec-
tiveness of inpatient dialectical behavioral therapy for
borderline personality disorder: A controlled trial.
Behavior, Research and Therapy, 42, 487–499.
Brown, J.D., & Dutton, K.A. (1995). The thrill of victory,
the complexity of defeat: Self-esteem and people’s
emotional reactions to success and failure. Journal of
Personality and Social Psychology, 68, 712–722.
Campbell, J.D. (1990). Self-esteem and clarity of the self-
concept. Journal of Personality and Social Psychology, 59,
538–549.
Campbell, J.D., Trapnell, P.D., Heine, S.H., Katz, I.M.,
Lavallee, L.F., & Lehman, D.R. (1996). Self-concept
clarity: Measurement, personality correlates, and cul-
tural boundaries. Journal of Personality and Social Psy-
chology, 70, 141–156.
Chapman, A.L., & Linehan, M.M. (2005). Dialectical
behavior therapy for borderline personality disorder.
In M. Zanarini (Ed.), Borderline personality disorder (pp.
211–242). Florida: Taylor & Francis.
Chen, T.H., Lu, R.B., Chang, A.J., Chu, D.M., & Chou,
K.R. (2006). The evaluation of cognitive-behavioral
group therapy on patient depression and self-esteem.
Archives of Psychiatric Nursing, 20, 3–11.
Cohen, J. (1977). Statistical power for the behavioral sciences.
New York: Academic Press.
Davidson, R., Kabat-Zinn, J., Schumacher, J., Rosen-
kranz, M., Muller, D., Santorelli, S.F., et al. (2003).
Alternations in brain and immune function produced
by mindfulness meditation. Psychosomatic Medicine, 65,
564–570.
De Bonis, M., De Boeck, P., & Lida-Pulik, H. (1998). Self-
concept and mood: A comparative study between
depressed patients with and without borderline per-
sonality disorder. Journal of Affective Disorders, 48,
191–197.
Diener, E., & Diener, M. (1995). Cross-cultural correlates
of life satisfaction and self-esteem. Journal of Personality
and Social Psychology, 68, 653–663.
DiPaula, A., Campbell, J.D. (2002). Self-esteem and per-
sistence in the face of failure. Journal of Personality and
Social Psychology, 83, 711–724.
Ebner-Priemer, U.W., Kuo, J., Kleindienst, N., Welch,
S.S., Reisch, T., Reinhard, I., Lieb, K., Linehan, M.M.,
& Bohus, M. (2007). State affective instability in bor-
derline personality disorder assessed by ambulatory
monitoring. Psychological Medicine, 37, 961–970.
First, M.B., Spitzer, R.L., Gibbon, M., Williams, J.B.W.,
& Benjamin, L.S. (1997). Structured clinical interview
for DSM-IV personality disorders (SCID-II). Washington
DC: American Psychiatric Press.
Fleming, J.S., & Courtney, B.E. (1984). The dimension-
ality of self-esteem: II. Hierarchical facet model for
revised measurement scales. Journal of Personality and
Social Psychology, 46, 404–421.
Forsman, L., & Johnson, M. (1996). Dimensionality and
validity of two scales measuring different aspects of
self-esteem. Scandinavian Journal of Psycholology, 37,
1–15.
Franke, G.H. (1995). Die Symptom-Checkliste von Derogatis
(SCL-90-R). Göttingen: Beltz.
Fydrich, T., Renneberg, B., Schmitz, B., & Wittchen, H.U.
(1997). Strukturiertes Klinisches Interview für DSM-IV.
Achse II. Persönlichkeitsstörungen (SKID-II). Göttingen:
Hogrefe.
Glaser, J.P., Os, J.V., Mengelers, R., & Myin-Germeys, I.
(2007). A momentary assessment study of the reputed
emotional phenotype associated with borderline per-
sonality disorder. Psychological Medicine, 30, 1–9.
Greenwald, A.G., & Pratkanis, A.R. (1984). The self.
In R.S. Wyer, & T.K. Srull (Eds), Handbook of social
cognition (pp 129–178). Hillsdale: Erlbaum.
Hautzinger, M., Bailer, M., Worall, H., & Keller, F. (1994).
Das Beck Depressionsinventar (BDI): Testhandbuch. Bern:
Huber.
Hill, J., Pilkonis, P., Morse, J., Feske, U., Reynolds, S.,
Hope, H., Charest, C., & Broyden, N. (2008). Social
domain dysfunction and disorganization in border-

158
S. Roepke et al.
Copyright © 2010 John Wiley & Sons, Ltd.
Clin. Psychol. Psychother. 18, 148–158 (2011)
DOI
: 10.1002/cpp
line personality disorder. Psychological Medicine, 38,
135–146.
Hyun, M.S., Chung, H.I., & Lee, Y.J. (2005). The effect of
cognitive-behavioral group therapy on the self-esteem,
depression, and self-effi cacy of runaway adolescents
in a shelter in South Korea. Applied Nursing Research,
18, 160–166.
Jacobson, N.S., & Truax, P. (1991). Clinical signifi cance:
A statistical approach to defi ning meaningful change
in psychotherapy research. Journal of Consulting and
Clinical Psychology, 59, 12–19.
Jørgensen, C.R. (2006). Disturbed sense of identity in
borderline personality disorder. Journal of Personality
Disorders, 20, 618–644.
Judge, T.A., Erez, A., Bono, J.E., & Thoresen, C.J. (2002).
Are measures of self-esteem, neuroticism, locus of
control, and generalized self-effi cacy indicators of a
common core construct? Journal of Personality and Social
Psychology, 83, 693–710.
Kernberg, O.F. (1975). Borderline conditions and pathologi-
cal narcissism. Lanham: Jason Aronson.
Kernberg, O.F., Yeomans, F.E., Clarkin, J.F., & Levy, K.N.
(2008). Transference focused psychotherapy: Over-
view and update. The International Journal of Psycho-
analysis, 89, 601–620.
Kleindienst, N., Limberger, M.F., Schmahl, C., Steil, R.,
Ebner-Priemer, U.W., & Bohus, M. (2008). Do improve-
ments after inpatient dialectial behavioral therapy
persist in the long term? A naturalistic follow-up in
patients with borderline personality disorder. The
Journal of Nervous and Mental Disease, 196, 847–851.
Knapen, J., Van de Vliet, P., Van Coppenolle, H., David,
A., Peuskens, J., Pieters, G., & Knapen, K. (2005).
Comparison of changes in physical self-concept, global
self-esteem, depression and anxiety following two
different psychomotor therapy programs in nonpsy-
chotic psychiatric inpatients. Psychotherapy and Psycho-
somatics, 74, 353–361.
Linehan, M.M., Armstrong, H.E., Suarez, A., Allmon,
D., & Heard, H.L. (1991). Cognitive-behavioral treat-
ment of chronically parasuicidal borderline patients.
Archives of General Psychiatry, 48, 1060–1064.
Linehan, M.M., Comtois, K.A., Murray, A.M., Brown,
M.Z., Gallop, R.J., Heard, H.L., Korslund, K.E., Tutek,
D.A., Reynolds, S.K., & Lindenboim, N. (2006). Two-
year randomized controlled trial and follow-up of
dialectical behavior therapy vs therapy by experts for
suicidal behaviors and borderline personality disor-
der. Archives of General Psychiatry, 63, 757–766.
Linehan, M.M., Heard, H.L., & Armstrong, H.E. (1993).
Naturalistic follow-up of a behavioral treatment for
chronically parasuicidal borderline patients. Archives
of General Psychiatry, 50, 971–974.
Lynch, T.R., Trost, W.T., Salsman, N., & Linehan, M.M.
(2007). Dialectical behavior therapy for borderline
personality disorder. Annual Review of Clinical Psychol-
ogy, 3, 181–205.
Pollock, P.H., Broadbent, M., Clarke, S., Dorrian, A., &
Ryle, A. (2001). The Personality Structure Question-
naire (PSQ): A measure of the multiple self-states
model of identity disturbance in cognitive analytic
therapy. Clinical Psychology and Psychotherapy, 8, 59–
872.
Reynolds, W.M., & Coats, K.I. (1986). A comparison of
cognitive-behavioral therapy and relaxation training
for the treatment of depression in adolescents. Journal
of Consulting and Clinical Psychology, 54, 653–660.
Robins, R.W., Hendin, H.M., & Trzesniewski, K.H.
(2001). Measuring global self-esteem: Construct vali-
dation of a single item measure and the Rosenberg
Self-Esteem Scale. Personality and Social Psychology
Bulletin, 27, 151–161.
Schütz, A. (2005). Je selbstsicherer desto besser? Licht und
Schatten positiver Selbstbewertung. [Self-esteem—The
more the better? Positive and negative aspects of high self-
esteem]. Weinheim: Beltz.
Schütz, A., & Sellin, I. (2006). Die multidimensionale Selbst-
wertskala (MSWS) [The Multidimensional Self-Esteem
Scale, MSES]. Göttingen: Hogrefe.
Shavelson, R.J., Hubner, J.J., & Stanton, G.C. (1976).
Self-concept: Validation of construct interpretations.
Review of Educational Research, 46, 407–441.
Sheehan, D.V., Lecrubier, Y., Sheehan, K.H., Amorim,
P., Janavs, J., Weiller, E., Hergueta, T., Baker, R., &
Dunbar, G.C. (1998). The Mini-International Neu-
ropsychiatric Interview (MINI): The development
and validation of a structured diagnostic psychiatric
interview for DSM-IV and ICD-10. Journal of Clinical
Psychiatry, 59, 22–33.
Stucke, T.S. (2002). Investigation of a German version
of Campbell’s self-concept clarity scale. Zeitschrift für
Differentielle und Diagnostische Psychologie, 23, 475–484.
Swann, W., Rentfrow, P., & Guinn, J. (2003) Self-
verifi cation: The search for coherence. Handbook of self and
identity. New York: Guilford Press.
Taylor, S.E., & Brown, J. (1988). Illusion and well-being:
A social psychological perspective on mental health.
Psychological Bulletin, 103, 193–210.
Tennen, H.J., & Herzberger, S. (1987). Depression, self-
esteem, and the absence of self protective attributional
biases. Journal of Personality and Social Psychology, 52,
72–80.
Watson, D., Suls, J., & Haig, J. (2002). Global self-esteem
in relation to structural models of personality and
affectivity. Journal of Personality and Social Psychology,
83, 185–197.
Wilkinson-Ryan, T., & Westen, D. (2000). Identity distur-
bance in borderline personality disorder: An empiri-
cal investigation. American Journal of Psychiatry, 157,
528–541.

Copyright of Clinical Psychology & Psychotherapy is the property of John Wiley & Sons, Inc. and its content
may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express
written permission. However, users may print, download, or email articles for individual use.
Wyszukiwarka
Podobne podstrony:
Wójcik, Marcin; Suliborski, Andrzej The Origin And Development Of Social Geography In Poland, With
Winlogon Notification Packages Removed Impact on Windows Vista Planning and Deployment
M Kernis Measuring Self Esteem in Context
Alpay Self Concept and Self Esteem in Children and Adolescents
the effect of water deficit stress on the growth yield and composition of essential oils of parsley
Dialectical Behavioral Therapy and BPD Effects on Service Utilisation and Self Reported Symptoms
Extending Research on the Utility of an Adjunctive Emotion Regulation Group Therapy for Deliberate S
Making Contact with the Self Injurious Adolescent BPD, Gestalt Therapy and Dialectical Behavioral T
Changes in personality in pre and post dialectical behaviour therapy BPD groups A question of self
Pancharatnam A Study on the Computer Aided Acoustic Analysis of an Auditorium (CATT)
An Essay on Mozambique
Impact On OIC Countries id 2122 Nieznany
Fossil Fuel Consumption CO2 and its impact on Global Climate
Ferguson An Essay on the History of Civil Society
Pain has an element of blank
więcej podobnych podstron