
Behaviour Change | Volume 27 | Number 4 | 2010 | pp. 251–264
Dialectical Behavioural Therapy
and Borderline Personality Disorder:
Effects on Service Utilisation
and Self-Reported Symptoms
Sarah E. Williams,
1
Margaret D. Hartstone
2
and Linley A. Denson
1
1
School of Psychology, University of Adelaide, Australia
2
Central Northern Adelaide Health Service, Australia
In a pilot evaluation study, effectiveness of a 20-week dialectical behavioural ther-
apy (DBT) skills training group program was explored for adult clients with bor-
derline personality disorder (BPD; N = 140). Subjective ratings of depression,
anxiety and BPD symptomatology were obtained pre and post group therapy.
Objective measures of service utilisation levels were obtained for the 6 months
prior to group therapy, the duration of therapy, and the 6 months following ther-
apy. Group completers (n = 68) showed reductions in depression, anxiety and BPD
symptomatology, as well as in the number of emergency department attendances.
Completers with previous high service utilisation had decreases in telephone
counselling calls and inpatient days during therapy, and fewer emergency depart-
ment attendances post therapy. Completers had larger decreases in service utilisa-
tion than noncompleters (n = 72). Simultaneous engagement in individual DBT
was related to higher group completion than was individual therapy as usual, but it
did not impact on level of service utilisation or psychological functioning. This
quasi-experimental pilot study suggests that DBT groups may improve psychologi-
cal functioning and decrease service utilisation for BPD clients, particularly those
with high service utilisation. The treatment warrants systematic evaluation.
■
Keywords: borderline personality disorder, dialectical behaviour therapy, group
therapy, outpatient program, treatment, psychosocial functioning
Borderline personality disorder (BPD) has a strong impact on utilisation of health
and mental health services and is of significant interest to a wide range of clinicians
(Hulbert, Jackson & Jovev, 2008). BPD is characterised by emotional lability,
intense and unstable interpersonal relationships, fear of perceived or actual aban-
donment, recurrent suicidal and self-harming behaviours, impulsivity, identity dis-
turbances, persistent feelings of emptiness, dissociation, and/or stress-related
ideation according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-
IV; American Psychiatric Association, 2004). Occurring in approximately 1–2% of
the population in the United States (Oldham, 2004) and in Australia (Andrews,
Henderson, & Hall, 2001), BPD is associated with very high levels of use of crisis
services, with BPD clients representing 10% of outpatients and 20% of psychiatric
Address for correspondence: Dr Linley Denson, School of Psychology, University of Adelaide, North Terrace,
Adelaide SA 5005, Australia. E-mail: linley.denson@adelaide.edu.au
251

inpatients (Salsman & Linehan, 2006; Sipos & Schweiger, 2003). Approximately 8
to 10% of people with BPD commit suicide (Tanney, 2000). People with BPD usu-
ally present in late adolescence or young adulthood (McCormick, Blum, & Hansel,
2007), and BPD is three times more commonly diagnosed in females (Skodol &
Bender, 2003).
Dialectical behavior therapy (DBT) is considered an effective treatment for
BPD (Linehan & Dimeff, 2001). DBT was developed by Linehan as a team-pro-
vided psychosocial treatment for chronic parasuicidal behaviours (Linehan,
Armstrong, Suarez, Allmon, & Heard, 1991) and typically spans a period of 12
months with three simultaneous components: a weekly skills training group for 2+
hours, weekly individual therapy, and structured support phone counselling
(Linehan et al., 1991; 1993). DBT aims to help people regulate their own emotions
using cognitive, behavioural, mindfulness and acceptance techniques. These skills
are combined within a dialectical view of the world where people are encouraged to
accept and tolerate tensions that arise, while learning to change the way they think
about those tensions (Feigenbaum, 2007). The original study (Linehan et al., 1991)
randomly assigned parasuicidal women with a diagnosis of BPD to either DBT (n =
22) or treatment as usual (TAU; n = 22) for a period of 12 months. DBT comprised
individual, group and telephone support, whereas TAU involved community-pro-
vided treatment. After 12 months DBT was related to a lower number of parasuici-
dal behaviours, less severe parasuicidal behaviours, and lower number and length of
hospital inpatient admissions than TAU. Participants in DBT were more likely to
remain in therapy than those in TAU. However, DBT was no more effective in
decreasing depression symptomatology than TAU. DBT was also related to fewer
parasuicidal behaviours than TAU at 6 months post therapy, and to fewer days spent
in inpatient hospital care at 12 months post therapy.
Subsequent studies have replicated and extended the Linehan et al. (1991)
study. DBT has been found to be related to higher therapy completion rates than
TAU in randomised control trials (RCTs) (Koons et al., 2001; Linehan, Comtois, &
Murray, 2006; Verheul, van den Bosch, & Koeter, 2003) and other studies
(Prendergast & McCausland, 2007; Rathus & Miller, 2002; Sunseri, 2004).
Improvements have been found in suicidal and parasuicidal behaviours over and
above that for other therapies or expert provided therapy (Koons et al., 2001;
Linehan et al., 1991; Linehan Tutek, Heard, & Armstrong, 1994; Linehan et al.,
2006; Low & Duggan, 2001; Verheul et al., 2003). Linehan et al., (1994) replicated
their original finding that DBT and TAU were equally effective in improving psy-
chological functioning. As a result, they concluded that although clients behave
better after DBT they are still miserable. However, preliminary post-DBT data of
many subsequent studies has shown significant temporary and long-term improve-
ments in psychological functioning, including improvements in quality of life,
global functioning, depression, and global distress (Ben-Porath, Peterson, & Smee,
2004; Dams, Schommer, & Ropke, 2007; Nee & Farman, 2005; Prendergast &
McCausland, 2007) over and above that of TAU controls (Koons et al., 2001).
Reductions have continued to be found in mental health service utilisation post
DBT, including number of telephone support utilisations, outpatient service utilisa-
tions, and inpatient days (Brassington & Krawitz, 2006; Prendergast &
McCausland, 2007; Rathus & Miller, 2002). Whereas the original RCT (Linehan et
al., 1991) found a decrease in annual inpatient days of up to 31 days, an uncon-
trolled trial found a decrease of 0.57 to 0.2 inpatient days per month during the 6
Sarah E. Williams, Margaret D. Hartstone and Linley A. Denson
252
Behaviour Change

months of DBT (Brassington & Krawitz, 2006). The reduction in hospital stays has
been estimated to produce savings of $US 9,000 per client per year (Gabbard, Lazar,
& Hornberger, 1997). This is important because of the high proportion of BPD clients
in the mental health system and the high level of cost associated with these services
(Gabbard et al., 1997; Salsman & Linehan, 2006; Sipos & Schweiger, 2003).
Organisations sometimes modify DBT programs, reducing costs, time, and
resources (Black, Blum, & Pfohl, 2004; Prendergast & McCausland, 2007). One ver-
sion used by organisations consists of a DBT skills-training group that is run addi-
tionally to existing treatment usual (TAU) rather than concurrently with standard
DBT individual therapy and telephone support (Black et al., 2004; Prendergast &
McCausland, 2007). Little is known about whether this single-component version of
DBT is as effective as the standard multi-component version, or whether it is effec-
tive enough to be worthwhile in organisations where resources are minimal.
However, it has been suggested that it is the whole DBT program, not its individual
components, that makes DBT effective for use with people with BPD (Black et al.,
2004). Exploration of the effectiveness of DBT groups is important so that current
patient quality of care is optimised, and so that more practical and cost-effective
methods of treatment can be made available to organisations. Some researchers have
begun to explore the benefits of DBT with fewer than the standard three compo-
nents (group, individual and telephone support). Rathus and Miller (2002) evaluated
a shortened 12-week version of DBT consisting of individual and group therapy, and
found that it was more effective than TAU in reducing service utilisation, reducing
suicidal and parasuicidal acts, and increasing completion rates of suicidal adolescents
with BPD. Soler et al. (2005) demonstrated that a 12-week version of DBT that
included DBT telephone support, group DBT, and a placebo drug, was associated
with an equal amount of improvement on self-reported depression and anxiety and
frequency of impulsive aggressive behaviours as a matched group receiving the same
psychotherapy with the addition of olanzapine, an atypical antipsychotic. However,
neither of these studies sought to isolate or explore the impact of one specific ele-
ment of standard DBT for clients with BPD. In addition, they lacked longitudinal
data to demonstrate ongoing benefits of specific DBT components.
The present study proposed that a DBT skills-training group program would be
beneficial in decreasing BPD-related symptoms and functioning, and in decreasing
longitudinal service utilisation. It was also proposed that the substitution of individ-
ual DBT therapy for individual TAU would improve retention rates, and further
improve symptoms and service utilisation post treatment, particularly in high ser-
vice utiliser subgroups.
Method
Participants
Each participant (N = 140) attended a DBT skills training group held between June
2002 and July 2008. Approximately 12 people began each group. Each participant
either commenced individual DBT sessions or continued individual treatment with
their usual therapist (individual TAU). Informed consent for participation and per-
mission for the use of self-report and service utilisation data were obtained from
clients. Research participation was voluntary and not required for admission to the
group. Conduct of the study was approved by The Queen Elizabeth Hospital
Groups for Borderline Personality Disorder
253
Behaviour Change

(Central Northern Adelaide Health Service) and University of Adelaide Research
Ethics Committees.
Design
The design was quasi-experimental with a repeated measures evaluation. One-way
ANOVA, mixed ANOVA and chi square tests were used to compare DBT group
completers and non-completers. A series of paired samples t tests, one-way ANOVA
and mixed ANOVA were used to compare high and low service utilisers, and indi-
vidual DBT and individual TAU clients, on the psychometric tests and service utili-
sation at two data-points (pre and post group therapy). The general linear model
was used to assess main and interaction effects. Several measures of effect size exist
for ANOVA (Dancey & Reidy, 1999): Cohen’s d was selected because it is often
used in clinical research.
Measures
Several self-report psychometric scales were completed at the first and final DBT
group sessions:
• The K10+ (Kessler & Mroczek, 1994) is a 14-item self-report measure (10 psy-
chological distress items and 4 impairment items) measured on a 5-point Likert
scale referring to the previous 4 weeks. It has good construct validity (Cronbach
α = 0.92) and internal consistency (Cronbach α = 0.93) and excellent reliabil-
ity for the total score although its sensitivity to change has not been formally
evaluated (Andrews & Slade, 2001; Pirkis, Burgess, Kirk, Dodson, & Coombs,
2005). There are fewer K10+ scores than for other measures because it was
included in later years of the study.
• The Behaviour and Symptom Identification Scale (BASIS-32; Eisen, Dill, &
Grob, 1994), a broad measure of wellbeing and quality of life, elicits self-report
responses on five subscales: Relation to Self/Others, Daily Living/Role
Functioning, Depression and Anxiety, Impulsive/Addictive Behavior, and
Psychosis using a 5-point Likert scale. The instrument is sensitive to change
with good concurrent and discriminant validity: scores successfully discriminate
between patients with different diagnoses, employment status and frequency of
hospitalization (Eisen, Dill, & Grob, 1994; Klinkenberg, Cho, & Vieweg; 1998;
Eisen, Wilcox, Left, Schaefer, & Culhane; 1999).
• The Beck Depression Index II (BDI-II; Beck, Steer, & Brown, 1996) is a 21-item
scale examining levels of depressive symptoms and severity during the previous 2
weeks, based on a 4-point Likert scale. Validated against the BDI-I, other
depression measures and DSM-IV it has good convergent and discriminant
validity for clinical depression and anxiety, a test–retest correlation of 0.93, and
a mean coefficient alpha of 0.86 for internal consistency (Beck et al., 1996).
• The Borderline Syndrome Index (Conte, Plutchik, Karasu, & Jerrett, 1980),
designed as a quick assessment tool for clinicians, screens for global BPD-related
symptoms and criteria using 52 forced choice Yes or No questions. The initial
study found good discrimination between BPD and other syndromes and con-
trols, but subsequent research showed a correlation with mood symptoms,
detracting from its usefulness as a diagnostic tool (Marlowe, O’Neill-Byrne,
Lowe-Ponsford & Watson, 1996; Remington, 1993).
Sarah E. Williams, Margaret D. Hartstone and Linley A. Denson
254
Behaviour Change

255
• The McLean Screening Instrument for Borderline Personality Disorder (MSI-
BPD; Zanarini et al., 2003), also included in later years of the study, has 10 Yes or
No questions based on the DSM-IV criteria for BPD. It has good test–retest relia-
bility (Spearman’s rho = 0.72, p < .0001) and internal consistency (Cronbach
α
= 0.74). When diagnosing BPD in adults aged 18 to 25 using a cut-off score of 7,
it has sensitivity of 0.81 and specificity of 0.85 (Zanarini et al., 2003).
Mental health service utilisation was collected from the Community Based
Information System (CBIS) database that is used by public mental health services.
Data included number of psychiatric inpatient days, number of presentations to public
hospital emergency departments (ED), and number of telephone support calls to a 24-
hous, 7-days-per-week emergency Assessment and Crisis Intervention Service (ACIS)
6 months prior to, the duration of, and 6 months post group DBT.
The group evaluation invited responses concerning venue and time, whether the
content was useful, and whether other aspects of the group were useful or problematic.
Procedure
The group component of DBT outlined in Linehan’s Skills Training Manual for Treating
Borderline Personality Disorder (Linehan, 1993) was delivered over 20 weeks of 2-hour
sessions addressing the key components: Emotional Regulation, Interpersonal
Effectiveness, Core Mindfulness, and Distress Tolerance. Inclusion criteria were (a)
DMS-IV-TR diagnosis of borderline personality disorder made by the referring clini-
cian; (b) attendance at individual TAU or DBT therapy sessions throughout group
DBT; and (c) residence within the service catchment area, a suburban region of
South Australia, with a population of 300,000+. Criteria were reviewed by clinical
psychologists prior to group admission. Exclusion criteria were (a) current, severe and
uncontrolled psychotic illnesses; (b) severe substance abuse; and (c) significant
aggressive or antisocial traits that may compromise the group process. Group comple-
tion was defined as (a) attendance of at least 70% of sessions; (b) never missing more
than 2 consecutive sessions; and (c) attendance at the final group session.
Groups were run by a government agency providing community-based health and
mental health care to an urban and rural region of Australia. Group facilitators — clini-
cal psychologists trained in DBT — followed Linehan’s program outline. Individual
DBT therapists were also clinical psychologists trained in DBT. Individual TAU was
provided by a range of mental health professionals. Regular consultation team meetings
were held for facilitator support and development. DBT telephone support was not
available but clients were notified of the availability of ACIS for telephone support
during or post group DBT. Most clients receiving DBT individual therapy had been
referred to the community mental health service for anxiety and/or depression, and sub-
sequently identified as meeting BPD diagnostic criteria.
Minor adaptations to Linehan’s group program included discussion during the
first session about the characteristics of BPD, celebration of group completion
during the final session, and development of a crisis management plan by each
client in the final session.
Results
Descriptive Statistics
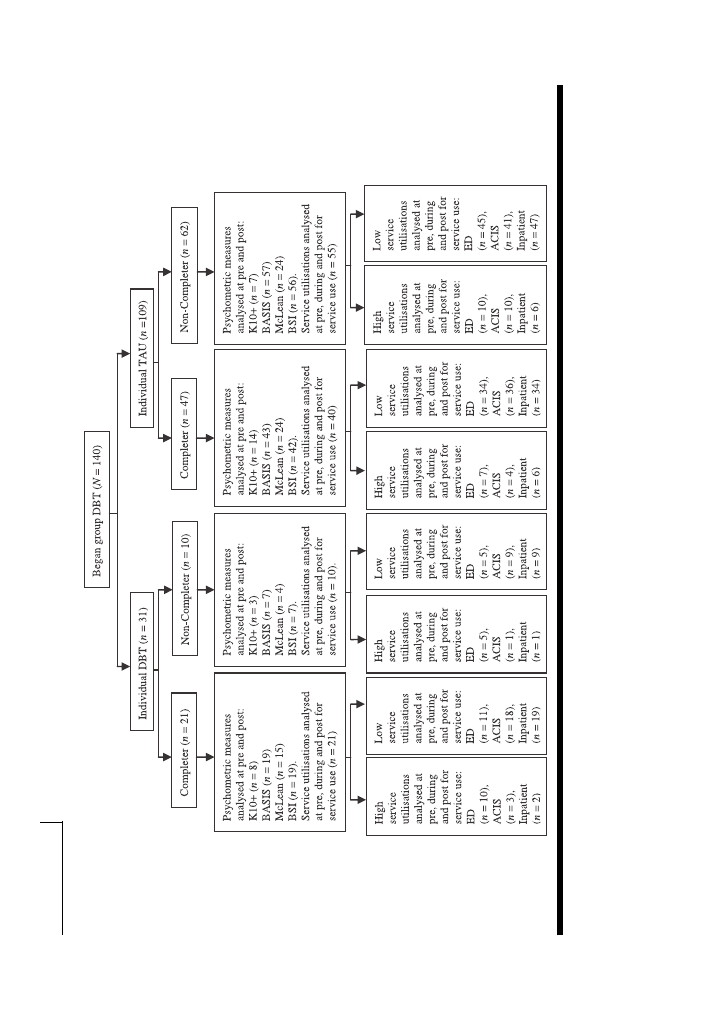
Figure 1 is a flow chart of client recruitment and study participation. Of the 140
participants, 68 completed the group program (13 males and 55 females aged
Groups for Borderline Personality Disorder
Behaviour Change
Sarah E. Williams, Margaret D. Hartstone and Linley A. Denson
256
Behaviour Change
FIGURE 1
Flow chart of participants in the study (
N
= 140).
257
between 19 and 59 years, M = 35.59, SD = 10.02). Seventy-two participants
attended at least one session but did not complete the program (7 males and 65 females
aged between 19 and 60 years, M = 36.24, SD = 11.16).
Consent to access service utilisation data was given by 127 participants. High and
low service utilisation subgroups were separated as suggested by the data distribution:
ED: low = less than 20 attendances in the previous 6 months, high = 20 or more; ACIS:
low < 3 calls in the previous 6 months, high = 3+; Inpatient days: low < 2 days in the
previous 6 months, high = 2+. During the 6 months prior to group DBT, 21% of partici-
pants spent one or more days in psychiatric inpatient care (range 1–69 days), 66% pre-
sented to an emergency department (range 1–80 attendances), and 37% of the
participants made one or more calls to ACIS (range 1–31 calls).
Completers and Non-Completers of Group Therapy
At the beginning of group therapy there were no significant differences between
completers and non-completers for age, gender, pre psychometric scores or service
utilisations in the 6 months prior to group therapy.
Changes in service utilisation during and after group therapy are summarised in
Tables 1 (for DBT group completers vs. non-completers) and 2 (for individual DBT
vs. TAU recipients).
Individual DBT was related to a higher completion rate than individual TAU,
χ
2
(1) = 5.86, p = .02, with 68% of people with individual DBT completing and 43%
of people with individual TAU completing.
ED attendances decreased during group DBT and post group DBT for non-com-
pleters with previous high service utilisation, t(14) = 2.59, p = .01, Cohen’s d = .93;
t(13) = 2.54, p = .01, d = .99.
ACIS calls decreased during group therapy for completers with high utilisation,
t(11) = 3.45, p < .01, d = 1.50. There were no significant decreases for ACIS sub-
groups at other time-points.
Groups for Borderline Personality Disorder
Behaviour Change
TABLE 1
Pre and Post Group DBT Treatment Means (M), Standard Deviations (
SD ), Relationships,
Effect Sizes, and Differential Effects for Completers and Non-Completers
Pre; Post M (
SD)
Completer
Non-completer
Differential effects
p value Cohen’s d (CI95)
p values: Time;
Cohen’s
d (CI
95
)
Time*Group
Group
ED
13.06; 7.87
9.36; 6.56
.01*; .44
(17.77; 11.26)
(14.34; 15.56)
.25
.01*
.11
.35 (-.01, .70)
.19 (-.16, .53)
ACIS
1.30; 1.54
1.77; 3.46
.12; .63
(2.50; 4.13)
(3.65; 11.44)
.31
0.14
0.12
-.07 (-.42, .29)
-.20 (-.54, .15)
Inpatient length
2.79; .81
1.38; .57
.08; .46
(10.21; 4.24)
(5.02; 1.87)
.32
0.09
0.12
Note: *
p < .05, one-tailed
Number of inpatient days decreased significantly during group DBT for com-
pleters overall, t(60) = 1.83, p = .04, d = .31, and for both completers and non-com-
pleters with high service utilization, t(10) = 2.50, p = .02, d = 1.08; t (6) = 2.36, p =
.03, d = 1.13. These decreases were significant post therapy for non-completers with
high utilisation, t(6) = 2.35, p = .03, d = 1.28, but not for other subgroups. That is,
service utilisation decreased regardless of completion or non-completion of group
DBT, but more decreases occurred for people who completed the program.
Individual DBT was related to a significant decrease in number of overall ED
attendances, t(30) = 2.93, p < .01, d = .50, especially for those with high ED utilisa-
tions, t (14) = 3.23, p < .01, d = .90. Among completers with individual TAU, high
ED service utilisers decreased their use, t(15) = 3.22, p < .01, d = 1.19, but overall
ED utilisations did not decrease significantly, t(94) = 1.38, p = .09, d = .18.
Neither type of individual therapy was related to decreases in ACIS calls, but indi-
vidual DBT and TAU were both related to significant decreases in inpatient days for
high utilisers (t (3) = 4.49, p = .01, d = 3.18; t (11) = 2.37, p = .02, d = 1.04).
Sarah E. Williams, Margaret D. Hartstone and Linley A. Denson
258
Behaviour Change
TABLE 3
Group Completers’ Psychometric Scores Before and After Group DBT
M (SD)
Pre
Post
p value
Cohen’s
d
CI95
K10+
34.20 (8.70)
23.73 (8.15)
< .01*
1.24
.58, 1.86
Basis 32
74.57 (24.19)
51.35 (28.42)
< .01*
.88
.51, 1.24
McLean
8.35 (2.02)
5.69 (3.30)
< .01*
.97
.49, 1.43
BSI
34.96 (8.92)
24.07 (12.27)
< .01*
1.02
.63, 1.39
BDI-II
35.11 (14.30)
24.18 (15.87)
< .01*
.72
.35, 1.09
Note: *
p < .05
TABLE 2
Service Utilisation Levels Before and After Group DBT: Means (M), standard deviations
(SD), Relationships, and Effect Sizes, by Type of Individual Therapy, and Differential Effects
Type of therapy*
Individual DBT
Individual TAU
Differential effects
utilisation M: Pre;
p-values Time;
Post (SD: Pre; Post)
Time*Group
p-value, Cohen’s d (CI
95
)
Group
ED
18.74; 10.26
8.72; 6.21
<.01*;
(19.41; 14.28)
(14.22; 13.27)
0.1
< .01*
0.09
.01*
.50 (-.01, 1.00)
.18 (-.08, .45)
ACIS
1.21; 3.29
1.58; 2.60
.11;
(1.97; 7.19)
(3.42; 9.60)
.59
0.06
0.16
.89
-.39 (-.89, .11)
-.14 (-.41, .12)
Inpatient Length
.61; .43
2.55; .77
.29;
(1.64; 2.08)
(9.14; 3.56)
.39
0.37
.04*
.23
.10 (-.40, .59)
.26 (-.01, .52)
Note: *
p < .05
259
Psychometric Test Scores for Completers
Participants reported significant symptoms associated with depression, anxiety, dis-
tress and BPD prior to attending the DBT skills group. Group completers reported
symptom reductions on all psychometric measures post therapy, as well as improved
functioning (see Table 3).
Regardless of whether participants received individual DBT or individual TAU,
their mean scores on all psychometric measures decreased (see Table 4). There were
no main effects of type of individual therapy on psychometric measures: decreases in
psychometric scores were not attributable to type of individual therapy received.
Evaluation of DBT Group
The participants’ evaluation of the group DBT program demonstrated that
Completers thought the group: was at a suitable venue (100%), suitable time
(89%), had useful content (100%), had other useful aspects (100%), and did not
have any other problems (60%). A few completers disliked the ‘slow pace’ and a few
cited disagreements between other group members as problematic.
Summary of Results
This pilot evaluation study supported the hypotheses that group DBT would be
related to decreases in psychometric scores, and that individual DBT would improve
retention rates more than individual TAU. The hypothesis that group DBT would be
related to decreases in service use was partially supported. Previous high service utilis-
ers of each service subgroup decreased service use during and/or post DBT and ED
utilisation decreased significantly for individual DBT recipients. Although Individual
DBT was associated with a higher rate of program completion, both groups showed
similar reductions in self-reported symptomatology and dysfunction.
Discussion
The pilot study aimed to explore the effects of a DBT group skills training program on
a range of variables for people with BPD. Results must be interpreted with caution,
Groups for Borderline Personality Disorder
Behaviour Change
TABLE 4
Changes in Group Completers’ Psychometric Scores by Individual Therapy Type
Individual DBT
Individual TAU
Differential effects
Pre M (SD); Post M (
SD )
Pre M (SD); Post M (
SD )
p values Time;
p value; Cohen’s d (CI95)
p value; Cohen’s d (CI
95
)
Time*Group Group
K10+
34.83 (11.84); 22.67 (6.62)
34.38 (6.84); 25.38 (9.53)
< .01*; .64
.02*; 1.27 (.31, 2.13)
.01*; 1.09 (.42, 1.71)
0.92
Basis 32
73.00 (22.59); 49.47 (21.65)
75.37 (26.77); 54.57 (32.60)
< .01*; .96
< .01*; 1.07 (.47, 1.63)
< .01*; .70 (.41, .98)
0.71
McLean
8.62 (1.33); 6.31 (3.20)
8.00 (2.50); 5.47 (3.48)
< .01*; .73
.01*; .94 (.25, 1.59)
< .01*; .84 (.41, 1.24)
0.29
BSI
34.41 (7.27); 24.88 (9.28)
35.70 (10.13); 25.20 (13.76)
< .01*; .54
< .01*; 1.14 (.54, 1.71)
< .01*; .87 (.57, 1.16)
0.95
BDI-II
32.88 (14.37); 25.24 (13.03)
37.16 (14.06); 24.81 (17.84)
< .01*; .29
.05*; .56 (-.01, 1.10)
< .01*; .77 (.48, 1.06)
0.83
Note: *
p < .05

given the study’s limitations. The design was quasi-experimental and did not include a
control group, comparison therapy, or any form of randomisation, nor were potential
clients who refused DBT group treatment followed up. Thus causality of the group
element of DBT could not be demonstrated, and it is possible (though unlikely)
that people without any form of therapy would have had the same decreases in psy-
chometric scores and service utilisation found in this sample. Also, because group
facilitators were committed to DBT therapy and to offering treatment to this
underserviced group, the study was vulnerable to allegiance factors, where a thera-
pist’s allegiance to a specific type of therapy may influence therapeutic benefits
(Luborsky et al., 1999). Third, because non-completers were no longer in therapy,
post-therapy psychometric scores were not collected. Thus it is not possible to
determine whether the amount of group DBT received was related to the levels of
improvement in psychological functioning. Lastly, although utilisation data were
obtained from public hospitals and mental health services in and surrounding the
catchment area for the study, it is possible that people also attended other services.
The comprehensiveness of the utilisation data is not guaranteed. Nevertheless,
this exploratory and naturalistic pilot study produced some interesting findings,
suggesting directions for future research and practice.
The overall retention rate was 49%, lower than those found by authors using
the standard multicomponent DBT approach, that is, 100% in Linehan et al.’s
(1991) original study, 77% by Koons et al. (2001), and 70% by Soler et al. (2005).
Retention rates were higher for clients receiving individual DBT (68%) than for
those receiving individual TAU (43%). These results support previous findings
(Koons et al., 2001; Linehan et al., 1991; Linehan et al., 2006; Prendergast &
McCausland, 2007; Rathus & Miller, 2002; Sunseri, 2004; Verheul, van den
Bosch, & Koeter, 2003). The proportion of males among participants was higher
than in some other studies, perhaps because participants with some other Axis II
diagnoses were not excluded and because some studies only included female partic-
ipants (Prendergast & McCausland, 2007; Linehan et al., 1991; Verheul, van den
Bosch, & Koeter, 2003). However, the proportion of males included in the current
study (17%), and particularly the proportion of males who completed group treat-
ment (24%), were reasonable reflections of the number of males diagnosed with
BPD in the general population (25%; Skodol & Bender, 2003).
There were no significant differences in age, gender, psychometric scores, or
levels of service utilisation between group DBT completers and non-completers
prior to group commencement. These results suggest that the individual therapy
component of standard DBT contributes to retention and completion rates for
group DBT.
There was a decrease in self-reported symptoms of depression, anxiety and BPD
post DBT group completion. Individual DBT was not superior to individual TAU
in decreasing these symptoms. These findings support previous studies that have
demonstrated that modified DBT programs consisting of fewer than the standard
three elements of DBT (group, individual and telephone support) can be effective
in reducing self-reported psychological and behavioural dysfunction (Rathus &
Miller, 2002; Soler et al., 2005). The findings call into question Black’s (2004)
suggestion that it is the whole DBT program, not its individual components, that
make DBT effective for use with people with BPD. The next step would be an
RCT design to test this assumption.
Sarah E. Williams, Margaret D. Hartstone and Linley A. Denson
260
Behaviour Change

261
There was a significant reduction in ED attendances for completers 6 months
post group therapy (13.06 to 7.87 attendances), especially for high ED service
utilisers (35.53 to 14 attendances). Non-completers did not have a significant
decrease in ED attendances overall, but the high ED service utiliser subgroup of
non-completers significantly decreased their ED use post therapy (33.40 to 16.47
attendances).
Completers with high ACIS service utilisations had a significant decrease in
ACIS calls during the DBT group (5.33 to 1.25 calls), but not post therapy (5.30
to 2.40 calls). This result may be because clients were encouraged to call ACIS,
which is set up specifically for emergency mental health assistance, rather than
overloading ED or inpatient services.
There was a significant decrease in number of inpatient days during group ther-
apy for group completers (2.79 to .57 days). This was accounted for by a significant
decrease in the number and length of hospital stays for previous high service utilis-
ers (16.18 to 1.36 days). In the 6 months post group this decrease in days, though
large from the perspective of cost savings, merely approached statistical signifi-
cance (17.56 to 3.33 days; p = .06).
The addition of individual DBT was not superior to the addition of individual
TAU in reducing levels of service utilisation for either high or low ACIS or inpa-
tient service utiliser subgroups, but was superior in reducing overall ED atten-
dances. Given the greater number of decreases in service utilisation during group
DBT, it is important for organisations to consider the possibility of having booster
sessions for group completers because this may help individuals to retain signifi-
cant decreases in service utilisations post group therapy.
The finding that group DBT completion is related to improvements in the
number of outpatient, telephone support, and inpatient service utilisations during
or post therapy is consistent with the literature (Brassington & Krawitz, 2006;
Linehan et al., 1991; Prendergast & McCausland, 2007; Rathus & Miller, 2002;
Sunseri, 2004). The finding that completers had a larger decrease in service utili-
sations than non-completers is not surprising given that they had more exposure
to group skills training. There were no differences between the completers and
non-completers on baseline psychometric scores or service utilisation, suggesting
that the group component itself impacted these decreases. However, other partici-
pant attributes could have accounted for this difference, including motivation and
endurance.
Participants perceived the group DBT program as being at a suitable venue, at
a suitable time, useful in content, and useful in ‘other areas’. Although 40% of
people mentioned in the ‘other problems’ section of the questionnaire that they
had some issue with the group, only a few described the problem. This often
related to personal difficulties with the communication styles or opinions of other
group members, which is unsurprising because one symptom of BPD is intense and
unstable interpersonal relationships.
In the absence of higher levels of evidence, this pilot evaluation supports fur-
ther clinical practice and evaluation research. It suggests that DBT skills-training
group programs may improve psychological functioning and decrease symptoms for
individuals with a diagnosis of BPD, and decrease service utilisation, especially for
high service utilisers. These results suggest that individual DBT may improve com-
pletion rates for the group DBT program more than individual TAU, albeit alloca-
tion to DBT and TAU was naturalistic and non-random. Group completion is
Groups for Borderline Personality Disorder
Behaviour Change

important because decreases in service utilisation appear to be related to the
amount of exposure to group DBT.
These findings support ‘dismantling’ trials comparing the effects of the differ-
ent elements of DBT to each other, to control groups, and to other forms of ther-
apy, as well as systematic comparisons of the separate and combined effects of
group DBT and individual DBT and TAU attempting to control for total DBT
‘dosage’. Future studies should follow up non-commencing and non-completing
individuals in an ‘intention to treat’ study design, and evaluate motivations and
barriers to therapy commencement and completion. Such studies could continue
the development of time and resource-efficient versions of DBT tailored to the
varying needs of individuals with BPD.
References
American Psychiatric Association. (2004). Diagnostic and statistical manual of mental disorders (4th
ed.). Washington, DC: Author.
Andrews, G., Henderson, S., & Hall, W. (2001). Prevalence, comorbidity, disability and service
utilisation: Overview of the Australian national mental health survey. British Journal of
Psychiatry, 178, 145–153.
Andrews, G., & Slade, T. (2001). Interpreting scores on the Kessler Psychological Distress Scale.
Australian and New Zealand Journal of Public Health, 25, 494–497.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck Depression Inventory — second edition:
Manual. San Antonio, TX: The Psychological Corporation.
Ben-Porath, D.D., Petersen, G.A., & Smee, J. (2004). Intercession telephone contact with indi-
viduals diagnosed with borderline personality disorder: Lessons from dialectical behavior ther-
apy. Cognitive and Behavioral Practice, 11, 222–230.
Black, D.W., Blum, N., & Pfohl, B. (2004). The STEPPS group treatment program for outpatients
with borderline personality disorder. Journal of Contemporary Psychotherapy, 34, 193–210.
Brassington, J., & Krawitz, R. (2006). Australasian dialectical behaviour therapy pilot outcome
study: effectiveness, utility and feasibility. Australasian Psychiatry, 14, 313–319.
Conte, H.R., Plutchik, R., Karasu, T.B., & Jerrett, I. (1980). A self-report borderline scale:
Discriminative validity and preliminary norms. The Journal of Nervous and Mental Disease, 168,
428–435.
Dams, A., Schommer, N., & Ropke, S. (2007). Skill training and the post-treatment efficacy of
dialectic behavior therapy six month after discharge of the hospital. Psychotherapie
Psychosomatik Medizinische Psychologie, 57, 19–24.
Dancey, C., & Reidy, J. (1999). Statistics without math for psychology: Using SPSS for Windows (2nd
ed). Harlow: Pearson Education.
Eisen, S.V., Dill, D.L., & Grob, M.C. (1994). Reliability and validity of a brief patient-report
instrument for psychiatric outcome evaluation. Hospital Community Psychiatry, 45, 242–247.
Eisen, S.V., Wilcox, M., Left, H.S., Schaefer, E., & Culhane, M.A. (1999). Assessing behavioral
health outcomes in outpatient programs: Reliability and validity of the BASIS-32. Journal of
Behavioral Health Services & Research, 26, 5–17.
Feigenbaum, J. (2007). Dialectical behaviour therapy: An increasing evidence base. Journal of
Mental Health, 16, 51–68.
Gabbard, O.G., Lazar, S.G., & Hornberger, J.S.D. (1997). The economic impact of psychotherapy:
A review. American Journal of Psychiatry, 154, 147–155.
Hulbert, C., Jackson, H., & Jovev, M. (2008). Personality disorders. In E. Rieger (Ed.), Abnormal
psychology: leading researcher perspectives (pp. 335–378). Sydney, Australia: McGraw-Hill.
Kessler, R., & Mroczek, D. (1994). Kessler 10 measure. Ann Arbor, MI: Survey Research Center of
the Institute for Social Research, University of Michigan.
Klinkenberg, W.D., Cho, D.W., & Vieweg, B., (1998). Reliability and validity of the interview and
self-report versions of the BASIS-32. Psychiatric Services, 9, 1229–1231.
Sarah E. Williams, Margaret D. Hartstone and Linley A. Denson
262
Behaviour Change

263
Koons, C.R., Robins, C.J., Tweed, J.L., Lynch, T.R., Gonzalez, A.M., Morse, J.Q., et al. (2001).
Efficacy of dialectical behavior therapy in women veterans with borderline personality disor-
ders. Behavior Therapy, 32, 371–390.
Linehan, M.M. (1993). Skills training manual for treating borderline personality disorder. New York:
Guilford Press.
Linehan, M.M., Armstrong, H.E., Suarez, A., Allmon, D., & Heard, H.L. (1991). Cognitive-
behavioural treatment of chronically parasuicidal borderline patients. Archives of General
Psychiatry, 48, 1060–1064.
Linehan, M.M., Comtois, K.A., & Murray, A.M. (2006). Two-year randomized controlled trial and
follow-up of dialectical behavior therapy vs. therapy by experts for suicidal behaviors and bor-
derline personality disorder. Archives of General Psychiatry, 63, 757–766.
Linehan, M.M., & Dimeff, L. (2001). Dialectical behavior therapy in a nutshell. The California
Psychologist, 34, 10–13.
Linehan, M.M., Tutek, D.A., Heard, H.L., & Armstrong, H.E. (1994). Interpersonal outcome of
cognitive behavioral treatment for chronically suicidal borderline patients. American Journal of
Psychiatry, 151, 1771–1775.
Low, G., Jones, D., & Duggan. (2001). The treatment of deliberate self-harm in borderline person-
ality disorder using dialectical behaviour therapy: A pilot study in a high security hospital
Behavioural and Cognitive Psychotherapy, 29, 85–92.
Luborsky, L., Diguer, L., Seligman, D.A., Rosenthal, R., Krause, E.D., & Johnson, S. (1999). The
researcher’s own therapy allegiances: A ‘wild card’ in comparisons of treatment efficacy.
Clinical Psychology: Science and Practice, 6, 95–106.
Marlowe, M.J., O’Neill-Byrne, K., Lowe-Ponsford, F., Watson, J.P. (1996). The Borderline
Syndrome Index: A validation study using the Personality Assessment Schedule. British Journal
of Psychiatry, 168, 72–75
McCormick, B., Blum, N., & Hansel, R. (2007). Relationship of sex to symptom severity, psychi-
atric comorbidity, and health care utilization in 163 subjects with borderline personality disor-
der. Comprehensive Psychiatry, 48, 406–412.
Nee, C., & Farman, S. (2005). Female prisoners with borderline personality disorder: Some
promising treatment developments. Criminal Behaviour and Mental Health, 15, 2–16.
Oldham, J.M. (2004). Borderline personality disorder: An overview. Psychiatric Times, 8, 1–8.
Pirkis, J., Burgess, P., Kirk, P., Dodson, S., & Coombs, T. (2005). Review of standardised measures
used in the National Outcomes and Casemix Collection (NOCC). Canberra: Australian Mental
Health Outcomes and Classification Network.
Prendergast, N., & McCausland, J. (2007). Dialectic behaviour therapy: A 12-month collaborative
program in a local community setting. Behaviour Change, 24, 25–35.
Rathus, J.H., & Miller, A.L. (2002). Dialectical behavior therapy adapted for suicidal adolescents.
Suicide and Life-Threatening Behavior, 32, 146–157.
Remington, G.J. (1993). Discriminative validity of the Borderline Syndrome Index. Journal of
Personality Disorders, 7, 312–319.
Salsman, N.L., & Linehan, M.M. (2006). Dialectical-behavioral therapy for borderline personality
disorder. Primary Psychiatry, 13, 51–58.
Sipos, V., & Schweiger, U. (2003). Inpatient treatment for men and women with borderline per-
sonality disorder and comorbidity. Verhaltenstherapie & Verhaltensmedizin, 24, 269–287.
Skodol, A.E., & Bender, D.S. (2003). Why are women diagnosed borderline more than men?
Psychiatric Quarterly, 74, 349–360.
Soler, J., Pascual, J.C., Campins, J., Barrachina, J., Puigdemont, D., Alvarez, E., et al. (2005).
Double-blind, placebo-controlled study of dialectical behavior therapy plus olanzapine for bor-
derline personality disorder. American Journal of Psychiatry, 162, 1221–1224.
Sunseri, P.A. (2004). Preliminary outcomes on the use of dialectical behavior therapy to reduce
hospitalization among adolescents in residential care. Residential Treatment for Children &
Youth, 21, 59–76.
Groups for Borderline Personality Disorder
Behaviour Change
Tanney, B.L. (2000). Psychiatric diagnoses and suicidal acts. In R. W. Maris, A. I. Berman & M.
M. Silverman (Eds.), Comprehensive textbook of suicidology (pp. 311–341). New York: Guilford
Press.
Verheul, R., van den Bosch, L.M.C., & Koeter, M.W.J. (2003). Dialectical behaviour therapy for
women with borderline personality disorder: 12-month, randomised clinical trial in The
Netherlands. British Journal of Psychiatry, 182, 135–140.
Zanarini, M.C., Vujanovic, A.A., Parachini, E.A., Boulanger, J.L., Frankenburg, F.R., & Hennen, J.
(2003). Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD): A continuous
measure of DSM-IV borderline psychopathology. Journal of Personality Disorders, 17, 233–242
Sarah E. Williams, Margaret D. Hartstone and Linley A. Denson
264
Behaviour Change

Copyright of Behaviour Change is the property of Australian Academic Press and its content may not be copied
or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission.
However, users may print, download, or email articles for individual use.
Wyszukiwarka
Podobne podstrony:
Contrasting Clients in Dialectical Behavior Therapy for BPD Marie and Dean , Two Caseswith Diffe
Dialectical Behavior Therapy for BPD A Meta Analysis Using Mixed Effects Modeling
Stages of change in dialectical behaviour therapy for BPD
Making Contact with the Self Injurious Adolescent BPD, Gestalt Therapy and Dialectical Behavioral T
Dialectic Beahvioral Therapy Has an Impact on Self Concept Clarity and Facets of Self Esteem in Wome
Changes in personality in pre and post dialectical behaviour therapy BPD groups A question of self
Brief Dialectical Behavior Therapy for Suicidal Behaviour and NSSI
Differential Treatment Response for Eating Disordered Patients With and Without a Comorbid BPD Diagn
[30]Dietary flavonoids effects on xenobiotic and carcinogen metabolism
Changes in passive ankle stiffness and its effects on gait function in
Cognitive and behavioral therapies
Heavy metal toxicity,effect on plant growth and metal uptake
33 437 452 Primary Carbides in Spincast HSS for Hot Rolls and Effect on Oxidation
49 687 706 Tempering Effect on Cyclic Behaviour of a Martensitic Tool Steel
48 671 684 Cryogenic Treatment and it's Effect on Tool Steel
Genetic and environmental effects on polyphenols
[30]Dietary flavonoids effects on xenobiotic and carcinogen metabolism
Chung, Zhao Humor effect on memory and attitude moderating role of product
więcej podobnych podstron