“Autism or Autistic
Disorder is a pervasive
developmental disorder
that affects all of mental
development.”
What is Autism?
Definition
Autism or Autistic Disorder is a pervasive developmental disorder that affects all of mental
development. It looks very different at different ages and certain features do not become
apparent until later. Autism is probably present at birth but is often not identified until the child
fails to develop communicative language at about 2 years of age. 70% of children with Autism
have IQ's below 70; and 11% have IQ's above 85. Those individuals who are most
developmentally delayed are usually also most autistic. As with normally developing children
no two children with Autism are alike and the differential diagnosis of such disorders as
Autism, Asperger's Syndrome, Nonverbal Learning Disability (NLD), Pervasive
Developmental Disorder (PDD), and severe communication disorder can be difficult. It is
believed by many researchers that the fundamental deficit that is seen in autistic children
is a "mind blindness" or a lack of a theory of mind or the capacity to understand that
other people think and feel the same way as they do. This deficit is believed to
contribute to the difficulty that autistic children have in imitating another person's
reactions, particularly their body movements, and particularly if the content of the
actions is affective. Several studies have also found specific deficits in autistic children's
perception and understanding of emotions.
Children with Autism have three primary distinguishing features:
·
Impairments in social interaction
(are not interested in peer interactions and
may show little eye-to-eye contact and lack of sharing with others).
·
Impairments in communication
(delays in or lack of spoken language).
·
Repetitive and stereotypic behaviours, interests and activities
(may show
behaviours such as hand flapping, spinning objects, and rituals).
Incidence
10 - 15 per 10,000 children are autistic and an additional 12 - 20 per 10,000 have autistic-like
features. Three boys to one girl have the disorder.
Diagnosis
The DSM-IV-TR (2000) has identified Autistic Disorder as one disorder under the wider category of Pervasive
Developmental Disorders. Under the broader category there are other disorders included such as Asperger's
Syndrome, Rett's Disorder, Childhood Disintegrative Disorder, and Pervasive Developmental Disorder (Not
Otherwise Specified). DSM-IV-TR has identified the following diagnostic criteria for the Autistic Disorder.
AUTISM
SYMPTOMS, CAUSES, ASSESSMENT, AND TREATMENT
1
A.
A total of six or more items from (1), (2), and (3) with at least two from (1), and one each from (2)
and (3).
(1)
qualitative impairment in social interactions, as manifested by at least two of
the following:
(a)
marked impairment in the use of multiple nonverbal behaviours
such as eye-to-eye gaze, facialexpression, body postures, and
gestures to regulate social interaction
(b)
failure to develop peer relationships appropriate to develop
mental level
(c)
a lack of spontaneous seeking to share enjoyment, interests,
or achievements with other people (e.g. by lack of showing,
bringing, or pointing out objects of interest)
(d)
lack of social or emotional reciprocity
(2)
qualitative impairment in communication as manifested by at least
one of the following:
(a)
delay in, or total lack of, the development of spoken lan
guage (not accompanied by an attempt to compensate
through alter native modes of communication such as
gestures and mime)
(b)
in individuals with adequate speech, marked impairment in
the ability to initiate or sustain a conversation with others
(c)
stereotyped and repetitive use of language or idiosyncratic
language
(d)
lack of varied, spontaneous make-believe play or social
imitative play appropriate to developmental level
(3)
restricted repetitive and stereotyped patterns of behaviour, interests, and
activities as manifested by at least one of the following:
(a)
encompassing preoccupation with one or more stereotyped and
restricted patterns of interest that isabnormal either in intensity or
focus
(b)
apparently inflexible adherence to specific, nonfunctional routines or
rituals
(c)
stereotyped and repetitive motor mannerisms (e.g. hand or finger flap
ping or twisting, or complex whole-body movements)
(d)
persistent preoccupation with parts of objects
B.
Delays or abnormal functioning in at least one of the following areas, with onset prior to age 3
years: (1) social interaction, (2) language as used in social communication, or (3) symbolic or
imaginative play
C.
The disturbance is not better accounted for by Rett's Disorder or Childhood Distintegrative
Disorder.
American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental
Disorders, 4th Edition, Text Revision (DSM-IV-TR) (p. 79).Washington, D.C.: American Psychiatric
Association.
AUTISM
Diagnostic Criteria
“10 - 15 per 10,000
children are autistic...”
2
“It is still not clear
what precise deficits
underlie Autistic
Disorders but
researchers have got
much closer to
understanding them in
the last five years.”
It is still not clear what precise deficits underlie Autistic Disorders but researchers have got much closer
to understanding them in the last five years. This has mainly occurred because the latest research has
compared autistic children to other children with the same IQ and chronological age. Deficits appear to
be very selective and are not the same in all children with Autism.
Other Symptoms That may Be Present For Some Children
·
Gross and sustained impairment of emotional relationships with people, aloofness
and/or empty symbiotic clinging.
·
Apparent unawareness of their own personal identity (e.g. posturing, self-mutilation,
and failure to use "I").
·
Obsessive use of and preoccupation with objects without regard to their functions.
·
Resistance to change in the environment and a striving to maintain sameness.
·
Excessive, diminished, or unpredictable responses to sensory stimuli.
·
Acute, excessive, and illogical anxiety especially precipitated by change.
·
Speech may have been lost or never acquired.
·
May use echolalia and certain idiosyncratic words.
·
Distortion in mobility patterns such as bizarre postures or ritualistic manner
isms, strange gestures and toe walking.
·
Serious retardation with possible islets of normal or near normal intelligence
and sometimes exceptional functioning in very isolated areas.
·
Poor concentration, short attention span and distractibility.
·
Minimal social and self help behaviours.
·
May place him/herself in danger by, for example, not watching while crossing
the road.
·
Does not show mutual sharing of interests, activities, and emotions with others,
particularly other children.
·
Does not understand the perspective of others.
·
May be aggressive if frustrated or if a child comes too close to their space.
·
May line up toys and not be interested in their function.
·
May seem unaware of what is going on around them.
·
May wander off in shopping malls and in parking lots seemingly without a sense that
they are alone.
·
Mainly engages in interaction in order to get what they want.
·
May "use" a person's arm in order to get what they want or to do something they cannot
do. This has been called "hand leading" and is used instead of pointing.
·
Does not use the emotions of others or "social referencing" in order to decide how to act.
·
Does not follow through on the requests of others because they are really not understood and
the child is doing what he wants to do.
·
May enjoy physical contact with parents and other caregivers if it is when they want it.
·
May not seek out comfort when upset or hurt.
·
Show little desire to imitate or copy another person's behaviour.
·
May show self-injurious behaviour.
AUTISM
Diagnostic Criteria
3
Causes
Exactly what causes Autism is unknown although it is believed to be a neurological condition. Medical
conditions that could be causal are found in only about 5-10% of cases.
Genetic Component
It seems likely that a predisposition to Autism is inherited. The evidence of the heritability of
Autism comes from twin and family studies. In twin studies, unusually high rates of Autism are
found in identical twins, and very low rates in fraternal or non-identical twins. Studies of
families have indicated that 2-6% of the siblings of autistic children are also autistic, and that
8% of the extended families will include another member who is autistic. Family studies also
reveal an increased prevalence of mental retardation and cognitive difficulties in the
siblings of autistic children especially those who are mentally retarded themselves. This
suggests that what may be inherited is not an "Autism gene" but rather a nonspecific
factor which increases the likelihood of various cognitive problems including Autism.
Neurobiological Difficulties
It is believed that Autism may be related to damage to the prefrontal cortex and limbic
region of the brain and to the connections between the two regions. The most
consistent findings are of brain stem and cerebellum abnormalities. P.E.T. scans with
Autistic children show the location of problems to be in these areas of the brain. Adults
with this kind of brain damage, as a result of accident or stroke, display similar
difficulties as autistic individuals. There is some indication that the brains of children with
Autism may have increased cell density suggesting that the cells did not get pruned back
as they do in normal development. Other researchers have found that this is
particularly true within the dopamine system suggesting that there may be an excess of
dopamine which could contribute to an overactive system. Studies of glucose metabolism
and blood flow have failed to reveal consistent global or regional abnormalities, although
correlational studies do show some promise.
Developmental History
The developmental history of autistic children seldom reveals medical conditions that can be linked
to the disorder. However, certain other illnesses place children at risk for developing Autism. These
are neurofibromatosis, tuberous sclerosis, and fragile X syndrome. Many children with Autism
(approximately one fifth to one third) develop seizures. Most of these occur in lower functioning
individuals and usually develop in later childhood or adolescence. Many studies have shown that the
number of perinatal problems experienced by autistic children are exceptionally high including: difficult
delivery, infantile seizures, delayed breathing and neonatal convulsions. Some children appear to have
normal development earlier and only show the symptoms of Autism in the second year of life. There have
been two explanations given for this: (1) the child did show problems earlier but they only became obvious
when speech failed to develop and the pressure for socialization was greater, or (2) the child was born with a
vulnerability to acquiring the syndrome and it was triggered by a virus or other insult.
Environmental Factors
As mentioned previously in a very few cases of Autism a viral infection in a young child preceded the onset of
the symptoms of Autism, before which there was a period of apparently normal development. There are also
some cases where infections occurred in the mother at an early stage of pregnancy. No other links to
environmental conditions have been found.
AUTISM
Causes
“It seems likely that a
predisposition to Autism
is inherited.”
4
Development
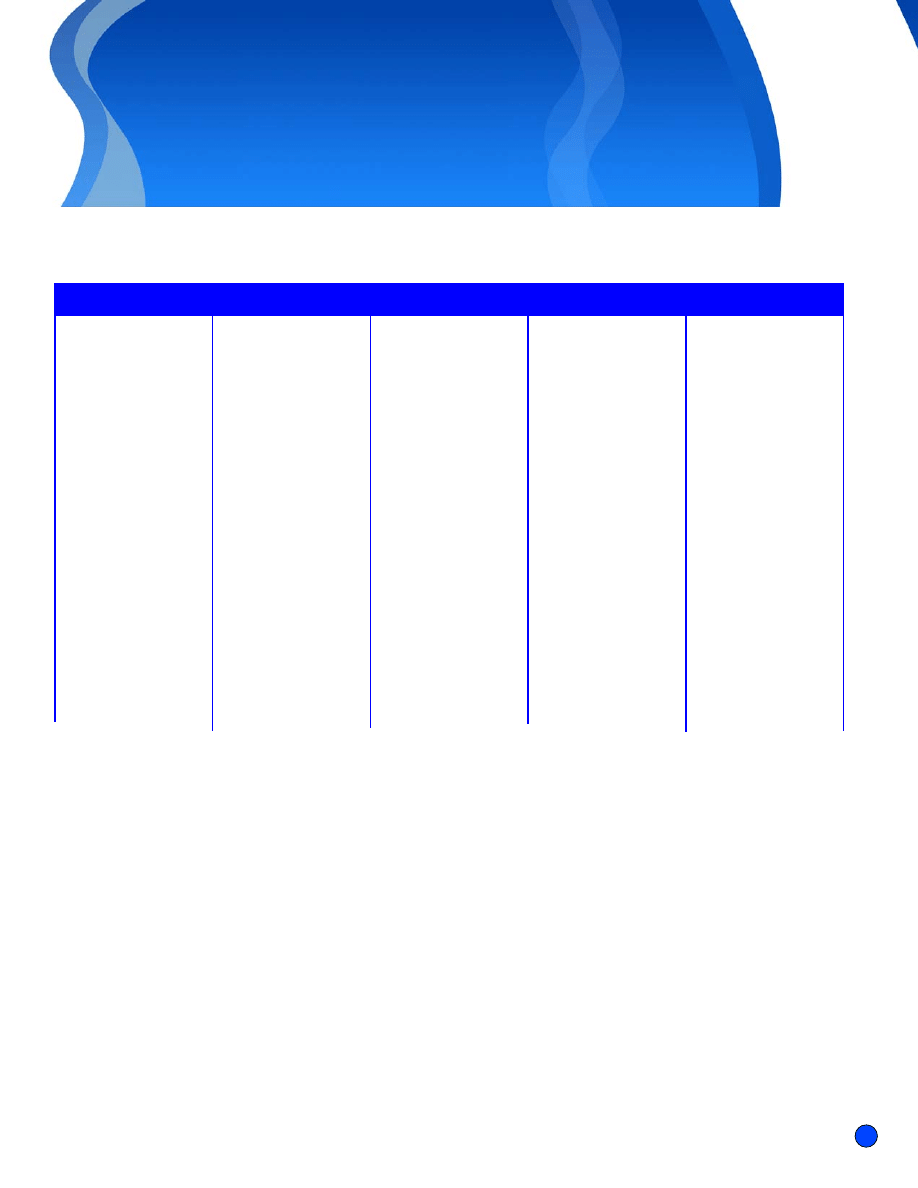
Infancy
In general, unless there is mental retardation, the signs of Autism may not be obvious until the second year of life when language
does not develop normally and the child does not show any interest in playing with other children. Stereotypic behaviours may also
develop at this time. However, even in early infancy some signs of difficulties may be observable. See the following chart for a list of
these signs
Early Childhood
It is usually in the second year of life that signs of Autism become most obvious and assessment is requested in order to determine
the reason or cause of the symptoms. Some of the signs that become obvious at this time are outlined below.
AUTISM
Development
Inactive:
· Flaccid muscle tone
· Rarely cries
Or
Irritable:
· Inconsolable
· Only soothed when
in constant motion
· Limp
Or
Motorically
disorganized:
· May be very active
· Have poor motor
planning in reaching
for objects
Unusually sensitive to
sensory stimuli
Auditory:
· Appears deaf to voice
but jolts or panics at
environmental sounds
Tactile:
· Refuses food with rough
texture
· Adverse reaction to
wool fabrics and labels,
etc.
· Prefers smooth surfaces
Visual:
· Sensitive to light
· May panic at change in
illumination
· Preoccupied in
observing own hand
and finger movements
Unresponsive:
· No social smile
· Avoidance of eye
contact when held
· Fleeting eye contact at a
distance
· Lack of anticipatory
response to being
picked up
· Seems not to like being
held or hugged
· Seems content left alone
· Does not visually follow
the coming and going
of primary caregiver
· Does not play peek-a-
boo or patty-cake or
wave bye-bye
· Fails to show normal 8-
month stranger anxiety
· Does not respond to
social bids from
caregiver
Fails to form strong
personal attachments
Delayed or absent coo or
expressive socialization
Failure to imitate sounds,
words, or gestures
Little communication or
use of gestures
Speech delayed or shows
precocious advances
followed by failure to use
previously learned words
Use eye contact when
interacting
Does not point to object
or hold up an object to
show it to caregiver
Decreased visual pursuit
of objects and people
Object permanence
develops slowly or stops
at age 2 or 3 years so
child does not develop
capacity for retaining a
memory of object or per-
son or for searching for
them
MOTOR
PERCEPTUAL
SOCIAL-EEMOTIONAL
LANGUAGE
MENTAL
REPRESENTATIONAL
Signs in Infancy (first year)
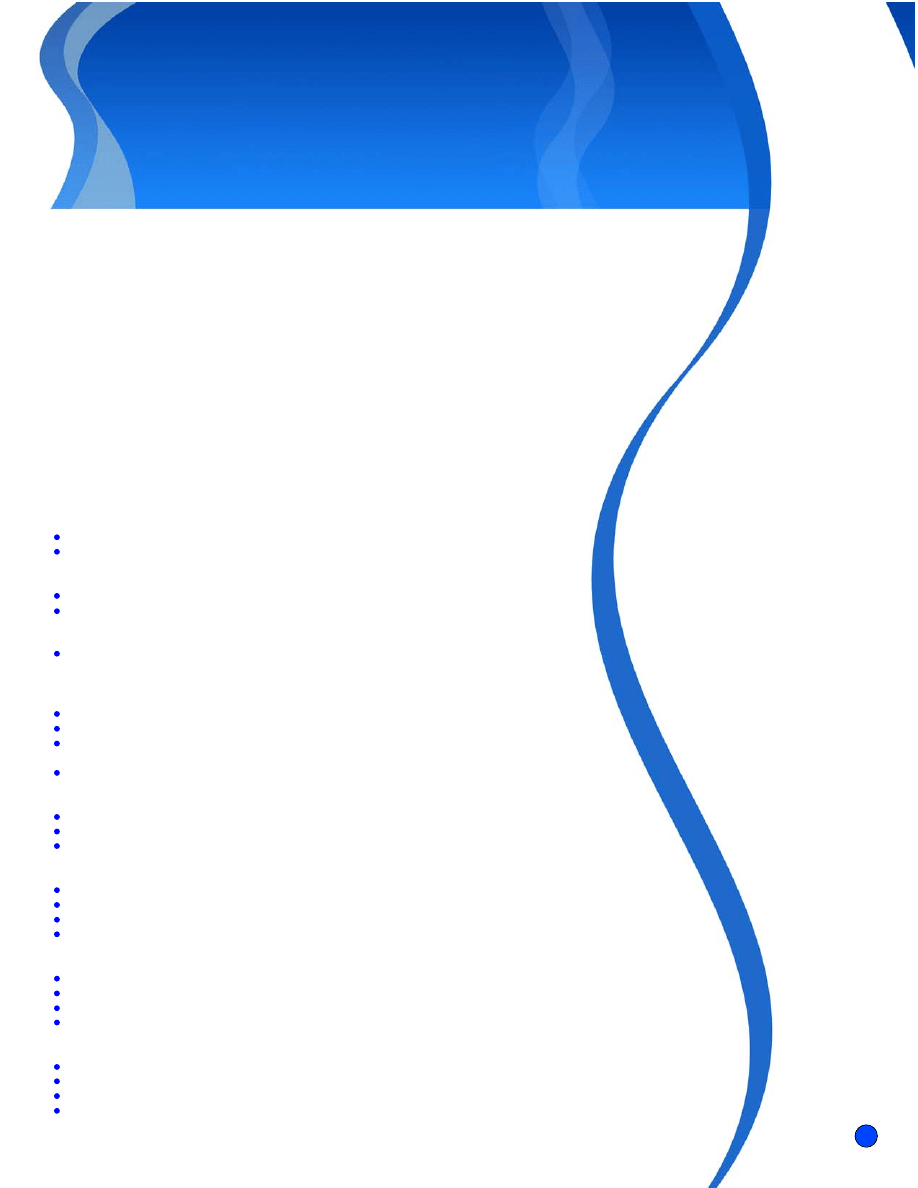
5
Toe walking
Rocking
Head banging
Whirling without dizziness
Perseverative movements
such as spinning or
finger posturing
Withdraws from
environmental stimulation
Engages in self
stimulation
Preoccupied with
spinning and shiny
objects
Suddenly ceases and
activity and stares into
space. Often with
hyperextension of the
neck
Respond inconsistently to
sounds (e.g. seems deaf)
Show unusual visual
interests (e.g.spinning
objects, "studying" objects
Moves adult's hand like a
tool
Insists on sameness and
ritualizes routines
Socialization:
· Does not respond to
social bids
· Does not smile to praise
or a smile of someone
else
· Does not engage in
reciprocal and back
and forth play
· Does not imitate the
actions of others
· Does not repeat actions
to get attention or to
show off for caregivers
· Does not show interest
in other children or
want to play alongside
them
· Does not show others a
object to show interest
Echolalia or repeating
what is said
Delayed echolalia unre-
lated to social context
Pronoun reversals
Voice atonal, hollow and
arhythmic
Does not use language
or gestures to
communicate
Seems not to understand
what is being said or
gestured
Does not use eye contact
to communicate
Play:
· No imaginative play·
Little appropriate use of
toys
· Does not engage in
play sequences with
toys
· Does not play with dolls
Preoccupied with
impersonal, invariant
information (e.g.
television commercials)
May engage in repetitive
play activities (e.g. lining
up toys and opening or
closing cupboards)
MOTOR
PERCEPTUAL
SOCIAL-EEMOTIONAL
LANGUAGE
MENTAL
REPRESENTATIONAL
Signs in Second and Third Year
AUTISM
Development
Older Children, Adolescents, and Adults
IImprovements in behaviour and compliance are usually evident after 5 years of age. The biggest change is most often a decrease in
social and emotional problems. The children become more affectionate and sociable, less resistant to change, less given to needless
fears, more aware of real dangers, and somewhat better behaved in public. However, the cognitive difficulties that are a part of the
disorder usually continue although early intervention with children with the disorder has been shown to be helpful. Long term
prognosis is generally poor for children with Autism as only about 8% in most follow-up studies become employable and live
independently. The best indicators of success in later life are having an IQ of over 85, developing speech before age 5, not having
any additional identifiable neurological difficulties, and not developing seizures in late childhood or adolescence
6
“To meet criteria for a
diagnosis of Autistic
Disorder a child must
meet the 3 conditions
outlined in the
DSM-IV-TR.“
Diagnosis
To meet criteria for a diagnosis of Autistic Disorder a child must meet the 3 conditions outlined in the
DSM-IV-TR. These are: 6 items in the areas of: impairment in social interaction, communication, or in
having repetitive and stereotyped patterns of behaviour; or delays in social interaction, language, and
symbolic or imaginative play which are not accounted for by Rett's Disorder or Childhood Disintegrative
Disorder. Other observation schedules and questionnaires can also be used to make the diagnosis.
Although the symptoms of Autism are evident by 2 years of age or before, the differential diagnosis
of Autism can still be difficult especially making a distinction between such other disorders as
severe communication disorder, Pervasive Developmental Disorder, and Nonverbal Learning
Disability (NLD). Testing children with Autism can be very challenging as they are usually not
interested or able to follow or imitate the examiner's instructions and demonstrations of certain
tasks. Also if children have behavioural difficulties or find strange places upsetting they may
refuse items that they could usually complete. For this reason it is critically important to
obtain information from a variety of settings and respondents.
Assessment
Assessment needs to consider the following sources of information:
·
Clinical interviews with parents and teachers.
·
A developmental and medical history to see if there are any medical
conditions or history of medical illness that could be contributing to the
problems.
·
Assessment of hearing and vision.
·
If it has not been done a medical examination to rule out any other disorders.
If there are soft neurological signs an examination by a neurologist would be
important.
·
Tests of developmental level are important to determine the child's level of
functioning in various areas of development. Because some children are very
difficult to test, observation of their behaviours or questionnaires completed by
the parents can be essential.
·
Observations of the child in different settings or situations.
·
Observations of parent-child interactions.
·
Use of tests which have been developed specifically to evaluate the child for autistic
symptomatology.
·
Assessment for behaviour management.
Parent Interviews or Questionnaires
·
Parent Interview for Autism (for parents of children under 6 years of age)
·
Vineland Adaptive Behavior Scales
·
Autism Diagnostic Interview
Developmental Assessments
·
Diagnostic Inventory for Screening Children (D.I.S.C.)
·
Leiter International Performance Scale for children who are non-verbal
·
Bayley Scales of Infant Development
·
Wechsler Intelligence Scales can be used if the child's level of development is high enough
Direct Assessments for Children with Autism
·
Diagnostic Checklist for Behavior-Disturbed Children
·
Autism Diagnostic Inventory
·
Autism Diagnostic Observation Schedule (ADOS)
·
Psychoeducational Profile for children 1 to 12 years of age who are functioning at a preschool level
Observational Scales
·
Autism Behavior Checklist (ABC) (completed by teachers)
·
Childhood Autism Rating Scale (CARS)
·
Checklist for Autism in Toddlers
·
Behavior Observation System (free play observation procedure)
AUTISM
Diagnosis and Assessment
7
References
American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders (4th ed.).
Washington, D.C.: American Psychiatric Association.
Baron-Cohen, S., Cox, A., Baird, G., Swettenham, J., Nightingdale, N., Morgan, K., Auriol, D., &
Charman, T. (1996). Psychological markers in the detection of autism in infancy in a large
population. British Journal of Psychiatry, 168, 158-163.
Cohen, D., & Volkmar, F. (Eds.)(1997). Handbook of autism and pervasive developmental
disorder. (2nd ed.). N.Y.: John Wiley.
Kranowitz, C.S. (1998). The out-of-sync child: Recognizing and coping with sensory
integration dysfunction. New York: Perigree Book.
Lord, C., & Risi, S. (2000). Diagnosis of autism spectrum disorder in young children. In
A.M. Weterby & B.M.Prizant (Eds.). Autism spectrum disorders: A transactional
developmental perspective (pp. 11-30). Baltimore: Paul Brookes Pub. Co.
Lord, C., Rutter, M., Divare, P.C., & Risis, P. (1999). Autism Diagnosis Observation
Schedule-WPS Edition (ADOS-WPS). Los Angeles: Western Psychological Services.
Mesibov, G.B., Adams, L.W., & Klinger, L.G. (1997). Autism understanding the disorder.
New York: Plenum Press.
Rogers, S.J., & Benneto, L. (2000). Intersubjectivity in autism: The roles of imitation and
executive function. In A.M. Wetherby & B.M.Prizant (Eds.). Autism spectrum disorders: A
transactional developmental perspective (pp. 79-108). Baltimore: Paul Brookes Pub. Co.
Schopler, E., Reichler, R.J., & Renner, B. R. (1986). The Childhood Autism Rating Scale (CARS)
for diagnostic screening and classification of autism. New York: Irvington.
Siegel, B. (1996). The world of the autistic child: Understanding and treating autistic spectrum
disorders. New York: Oxford University Press.
Weatherby, A.M., & Prizant, B.M. (2000). Autism spectrum disorders: A transactional developmental
perspective. Vol. 9, Communication and Language Intervention Series. Baltimore: Paul Brookes Pub.
Co.
Wing, L. (1998). Classification and diagnosis - Looking at the complexities involved. Communication,
15-18.
ZERO TO THREE/National Center for Clinical Infant Programs (1994). Diagnostic classification 0 -3 diagnos-
tic classification of mental health and developmental disorders of infancy and early childhood. Arlington, VA:
ZERO TO THREE.
AUTISM
References
8
“Applied Behaviour
Analysis (ABA) is based
on the view that autism
is a neurological
disorder which causes a
number of deficits in
behavioural responses.”
TREATMENT
Definition
Autism or Autistic Disorder is a pervasive developmental disorder that affects all of mental
development. For further information on the diagnosis of Autism refer to the sections on
“Symptoms, Causes and Assessment”. Children with Autism have three primary distinguishing
features:
·
Impairment in social interactions.
·
Impairment in communication.
·
Repetitive and stereotypic behaviours, interests, and activities.
Treatment for children with Autism may be one or more of the following and may vary
depending on the intellectual capacity of the child. Treatments that may be used include:
·
Applied behaviour analysis (ABA)
·
Sensory integration therapy
·
Auditory integration therapy
·
Interactive approaches
·
Music therapy
·
Music interaction therapy
·
Using megavitamins
·
Medication
·
Teaching the child to mind-read
These forms of treatment are briefly described below and comments made on their
effectiveness.
Applied Behaviour Analysis (ABA)
Applied Behaviour Analysis (ABA) is based on the view that autism is a neurological disorder
which causes a number of deficits in behavioural responses. Using Skinnarian operant
conditioning the approach aims to increase adaptive behaviour (such as eye contact, language,
self help skills) and decrease inappropriate behaviour (such as stereotypic behaviours and
aggression). It works through reinforcement, punishment, shaping, fading, generalizing, extinction,
etc. of the child's behaviour so he learns what is expected of him. Behaviours are broken down into
small steps, and each step is taught (usually on one-to-one) by giving the child consistent cues that are
faded out as soon as possible, so the child learns to respond to similar cues in the natural environment.
In order to enhance motivation, teaching sessions are made as much fun as possible and tangible
reinforcements are used such as toys or Smarties. The reinforcers are presented at a fast rate initially and
then faded to intermittent reinforcement in order to sustain the behaviour. As the sessions progress the
tangible reinforcements are gradually replaced by social reinforcers such as praise. Parents are included in
the treatment so it can be carried over into the home and school ensuring that children will be consistently
reinforced and will be able to able to use their new skills in different settings. Of all the interventions used with
Autism research has shown it to be the most effective, especially for young children. It has been shown to result
in integration into normal classrooms and to normal functioning for some children.
AUTISM
TREATMENT
9
“Children with Autism
have difficulty processing
stimulation from the
environment that
contributes to their over-
or under-arousal by
normal stimulation in the
environment.”
Sensory Integration Therapy
Children with Autism have difficulty processing stimulation from the environment that contributes to their
over- or under-arousal by normal stimulation in the environment. This can explain the hypersensitivities
or sensory defensiveness to touch, loud noises, bright lights, and certain food textures that are often
found with these children. These contribute to their ritualistic and stereotypic behaviours such as
body-rocking and spinning objects. It may also explain some of their withdrawal from closeness to
human contact that children with Autism display although it is not believed to be the primary
explanation. Sensory integration is a one-to-one therapy usually administered by an occupational
therapist, that involves body massaging, swinging from a hammock, rocking, jumping on
bouncy surfaces, climbing and crawling on special apparatus, or spinning on special chairs.
Another related approach that is used with children who show extreme sensory defensiveness
has been to apply rapid and firm pressure to the arms, hands, back, legs, and feet with a
non-scratching brush with many bristles. A special brush is used which is a plastic surgical
scrub brush. The brushing is followed by gentle joint compression to the shoulders,
elbows, wrists, hips, knees, ankles, and sometimes fingers and feet. It needs to be
repeated frequently throughout the day. Clear evidence for the effectiveness of the
treatment is lacking although studies by its originator A. Jean Ayres suggest that it can
reduce certain behaviours and increase some positive behaviours.
Auditory Integration Therapy
Auditory Integration Therapy (AI) assumes that sensitivity to sounds causes aggression
and impairs the Autistic child's interactions with others. The purpose of the therapy is to
reduce this sensitivity so that their learning and especially their language will improve. It
is hoped that by reducing auditory sensitivity, behaviour and learning, especially of
language will improve. The therapy is conducted over about 2 weeks and the child spends
10 hours over the 2 weeks listening to music played through a machine that filters out
frequencies to which they are sensitive. During this time it is suggested that all other
treatment be discontinued. No scientific studies have been conducted although parent
reports have indicated that children who receive the treatment have a reduced rate of
behaviour problems and understand language better than children who received a placebo.
Interactive Approaches
Stanley Greenspan and Serena Weider are the most well known advocates of using play to increase
the functioning capacity and interactions of children with Autism. Children with Autism have little
appropriate use of play objects and usually do not engage in pretend play. The treatment (called Floor
Time) can take place in a room with toys that can be used to stimulate imaginative play including cars,
animals, dolls, doll furniture, trains, etc. It can also be used throughout the day when the child is doing
something he is interested in. The child's parent is usually included in the session and is encouraged by the
therapist to carry out the following:
1.
Follow the lead of the child in whatever they are doing with the play and make it interactive. The
interaction should not be interrupted as long as the child is enjoying it and wants to continue.
2.
Treat all the child's behaviour as if it is intentional and purposeful even though it may seem random
and purposeless (e.g. the child is just picking up and dropping objects or may run around aimlessly).
3.
If the child is requesting something, indicating you do not know what he means will help extend the
AUTISM
TREATMENT
10
“Because children with
Autism enjoy music so
much it has been found
to be useful to integrate
both play and music.”
4.
Face the child and make sure that their actions are differentiated from your own and some
times put your hand over the child's to help them do something instead of encouraging the child
to lead with his hand over yours.
5.
Use surprise and novelty to capture the child's attention and interest so the child is compelled to
respond such as using a musical box or a jack-in-the-box.
6.
Pursue the child until he responds and keep trying new approaches to get interaction.
7.
Use tickling, peek-a-boo, and rhymes such as This Little Piggy, Ring Around the Rosy and
help the child join in the actions. Add new meanings to stereotypic play and add pretend
human figures such as having the lined up cars or the train which is going round and
round to pick up people and talk about the people in the train or lining up waiting for
the bus or train.
8.
If the child becomes upset empathize with the feelings but do not give up on the
interactions.
9.
Use every opportunity to expand on pretend play such as, for example, offering
pretend cups of tea or pretend keys to open doors.
Music therapy
Many children with Autism enjoy music and often enjoy dancing to it and will "sing"
along with the words. This allows the child a medium for non-verbal self-expression
and can provide a channel for communication. It can also be used to form the basis
for enjoyable interactions and a relationship.
Music Interaction Therapy
Because children with Autism enjoy music so much it has been found to be useful to
integrate both play and music. A music therapist or a musician scaffolds the interaction
between the child and his parent(s). Children who cannot speak and do not engage in
interactions with their parents are provided with prolonged exposure to preverbal play
patterns supported by the music. Through lap play, dancing together, tapping to the music,
and joint attention supported by the music the social or interactional skills and timing skills
important for language are developed.
Using Megavitamins
Megavitamins have also been used as well as different types of restricted diets such as gluten free
and restricting certain food such as sugar, milk, eggs, and chocolate. Some researchers have claimed
that the vitamins B-6 and magnesium have positive effects but there is little evidence that these
approaches are helpful.
Medication
Because Autism is a neurobiological disorder researchers have been studying the effects of medication on the
disorder. As yet, medications have been used to treat some of the symptoms of autism such as disruptive
behaviours, aggression, and stereotypic behaviours but have not been able to increase adaptive behaviours
such as language and imagination. Some medications that have been used include antipsychotics (such as
risperidone), ritalin, and anti-depressants but they have had mixed results and some have had adverse side
effects. Anti-depressants (particularly Selective Serotonin Reuptake Inhibitors, (SSRIs)) have been found to be
helpful for children with high anxiety and sensitivity to various stimuli to calm them and reduce negative
behaviours. SSRIs have also shown some benefit both in terms of reducing unwanted behaviour as well as in
increasing prosocial behaviours. However, studies have involved small numbers of children and have not been
double blind placebo controlled studies.
AUTISM
TREATMENT
11
“Children with Autism
have deficits or have not
developed a theory of
mind or the capacity for
"mind-reading" and this is
seen as at the basis of
many of their difficulties
with socialization, pretend
play, communication, and
understanding the
emotions of another
person that relate to their
beliefs.”
Teaching the Child to Mind-RRead
Children with Autism have deficits or have not developed a theory of mind or the capacity for
"mind-reading" and this is seen as at the basis of many of their difficulties with socialization, pretend
play, communication, and understanding the emotions of another person that relate to their beliefs.
This deficit can lead to insensitivity to other people's feelings, difficulty with making friends by reading
their interests and intentions, and can lead to more elaborate difficulties such as problems with
realizing they are being deceived. The program Teaching Children to Mind-Read was developed
by Howlin, Baron-Cohen, and Hadwin and research has shown that the method has been
successful in teaching children with Autism to learn specific mental state concepts and that the
improvements were maintained long after the intervention ended. The program provides the
material that can be used to teach. It involves three types of learning: (1) teaching the child
about emotions from recognizing facial expressions in photos such as happy, sad, mad,
and afraid up to being able to recognize what a person would be feeling from a sequence
of pictures, (2) teaching the child about perspective-taking and how people see things
differently both visually and on the basis of knowledge that they have, and (3) teaching
children to pretend play at increasingly complex levels.
Developmental Social-PPragmatic (DPS) Approaches To Teaching Communication
Developmental Social-Pragmatic (DPS) approaches emphasize the importance of
focusing on the child's natural attempts for communication and use more natural
activities and events as contexts to support the child's development of social
communications. In other words they do not rely on scheduled activities or programs
such as the ABA approach to enhance the behaviour. Developed by Prizant, Wetherby,
and Rydell, the approaches use interactive-facilitative strategies to carry out the therapy
and focus on aspects of both verbal and nonverbal behaviour. The interactive approach
described above is similar in the principles that underlie the approaches. In summary the
DPS approach uses the following:
·
Enhances spontaneous communication within a flexible schedule and varied
interesting activities.
·
Builds on multimodal communicative repertoires including speech, gestures, and
alternative communication methods.
·
Encourages turn taking and reciprocity in interactions.
·
Encourages the child interacting in a number of social groups.
·
Uses gestures and visual supports to help the child make sense of the communication rather
than breaking down the tasks into small pieces.
·
Emotional expression and affect sharing are seen as crucial to the interactive and learning
process.
·
The intervention starts from the developmental level that the child is at, sometimes starting from
prespeech, or echolalia, and moving to more creative levels of language.
·
Attempts are made to have the child seek out assistance in order to calm down and types of activity
are provided that can help them to regulate the emotions.
Augmentative Communication
Some children with Autism will not be learn to speak and will need to use augmentative and alternative
communication supports. Some of the common forms of augmentative communication devices are: use of
pictorial or written schedules to assist the child to understand the school schedule, teaching children manual
signs that they can use to communicate certain needs, and the use of voice-output computer programs. These
devices can all allow the child to communicate and to be communicated with.
AUTISM
TREATMENT
12
As well, treatment
needs to be ggiivveenn aass
eeaarrllyy aass ppoossssiibbllee and ttoo
bbee iinntteennssee to be
successful.
Summary and Conclusions
With so many treatments available choosing which type of treatment would benefit an individual child can
be very confusing and frustrating for parents who are often looking for a cure for their child. There are,
however, some guidelines that can be used in making decisions:
·
Treatments should start as early as possible and treatment received between 2 and 4 years
can improve a child's skills considerably.
·
Treatment needs to be different for different children depending on their IQ level (which
can range from below 50 to 120 and above), whether aggressive behaviour and other
stereotypic behaviour is a problem, whether the child has language, and their level
of socialization and their capacity for warm interactions with other children. It is,
therefore, important that the child has a thorough assessment in order to deter
mine the most appropriate treatment combination.
·
Treatment may need to be intense to begin with to get the gains that may be
possible and many improvements have occurred when treatment has been
intense.
·
All teaching in the various therapies needs to be broken down into small
steps, so that complex skills are acquired gradually, as a sequence of separate
components (see ABA and improving mind reading especially).
·
Teaching needs to pay attention to the child's interests and to build on them
(e.g. if a child loves trains use them as a subject to teach other words, math,
and reading).
·
Having a structured classroom to help contain the child's anxiety and nervous
system arousal can be very helpful.
·
Sensory integration therapy and use of exercise as a release is an important
component of treatment.
·
Using visual cues to reinforce learning as well as routines that the child follows
(e.g. have the child look at pictures of the stages of having a bath before they
have one).
·
Avoiding using long strings of verbal information as the child will probably not be
able to follow it.
·
Skills need to be reinforced by rewards but when the child finds the intervention fun and
pleasurable the influence of the rewards can be further enhanced.
·
Teaching needs to begin at the level the child is at and not a level that would be expected
given the child's age. However, for children with higher levels of functioning,individualized
rather than pre-packaged teaching methods need to be applied.
·
Family support is crucial to help parents deal with the demands of providing treatment.
In conclusion it is important to: use a combination of various treatment strategies including approaches
that build a relationship with the child and enhance parent's relating with their child and behavioural
approaches. As well, treatment needs to be given as early as possible and to be intense to be successful.
Author:
Sarah Landy Ph.D., Developmental Psychologist
We recognize and thank the Government of Ontario for its generous financial support of this publication.
AUTISM
Summary and Conclusions
13
Bebko, J.M., Perry, A., & Bryson, S. (1996). Multiple method validation study of facilitated commuication:
11. Journal of Autism and Developmental Disorders, 26, 19-42.
Cohen, D. & Volkmar, F. (Eds.). Handbook of autism and pervasive developmental disorder. (2nd ed.).
N.Y. : John Wiley and Sons.Dawn, C., Wimproy, S., & Nash, S. (1999). Musical interaction
therapy :Therapeutic play for children with autism. Child Language Teaching and Therapy,
15, 17-25.
Dawson, G., & Osterling, J. (1997). Early intervention in autism. In M. J. Guralnick (Ed.). The
effectiveness of early intervention. (pp. 307-326). Baltimore: Paul Brookes Pub.Co.
Greenspan, S.I. (1997). Developmentally based psychotherapy. Madison, CT: International
University Press.
Greeenspan, S.I., & Wieder, S. (1998) The child with special needs: Intellectual and
emotional growth. Reading, MA: Addison Wesley Longmans.
Hanna, S., & Wilford, S. Floortime: Tuning in to each child. (Book and video). New York:
Scholastic Inc.
Hodgdon, L.A. (1995). Visual strategies for improving communication: Practical
supports for school and home. Michigan: QuirkRoberts Publishing.
Howlin, P., Baron-Cohen, S., & Hadwin, J. (1999). Teaching children with autism to
mind-read: A practical guide. Chichester, West Sussex: John Wiley and Sons.
Hurth, J., Shaw, E., Izeman, S., Whaley, K., & Rogers, S.J. (1999). Areas of agreement
about effective practices among programs serving young children with autism
spectrum disorders. Infants and Young Children, 12, 17-26.
Levine, C. (1991 ). Fine motor dysfunction: Therapeutic strategies in the classroom.
Tucson, AZ: Therapy Skill Builders.
Lovass, O.I. (1981). Teaching developmentally disabled children: The "me" book. Baltimore:
University Park Press.
Lovass, O.I. (1987). Behavioral treatment and normal educational and intellectual functioning in
young autistic children. Journal of Consulting and Clinical Psychology, 55, 3-9.
Maurice, C. (1996). Behavioral interventions for young children with autism: A manual for parents
and professionals. Austin, Texas: Pro-ed.
Quill, K. (2000). Do-watch-listen-say: Social and communication intervention for children with
autism. Baltimore: Paul Brookes Pub.
Quill, K. (1995). Teaching children with autism: Strategies to enhance communication and socialization.
Baltimore: Paul Brookes Pub. Co.
Prizant, B.M., Schuler, A.L., Wetherby, A.M., & Rydell, P. (1997). Enhancing early language and
communication: Language approaches. In D. Cohen & F. Volkmar (Eds.). Handbook of autism and
pervasive developmental disorder. (2nd ed.). (pp. 572-605). New York: John Wiley & Sons.
Schwartz, S., & Miller, J.(1987). Teaching communication skills to children with special needs: A guide for
parent and teachers.
Yack, E., Sutton, S., & Aquilla, P. (1998). Building bridges through sensory integration. Weston, Ont., Canada.
AUTISM
Bibliography
14
Wyszukiwarka
Podobne podstrony:
Child Autism Treatments, Symptoms & Causes Autyzm
Young Inerner Addiction symptoms, evaluation and treatment
Osteoporosis ľ diagnosis and treatment
Diagnosis and Treatment of Autoimmune Hepatitis
Schizophrenia Explained and Treatments
Pytania i odpowiedzi ? 123 Risk Assessment and Management
Osteoporosis ľ diagnosis and treatment
Variations in Risk and Treatment Factors Among Adolescents Engaging in Different Types of Deliberate
Real Macrobiotics for Cancer Prevention and Treatment Varona
The Problem of Internal Displacement in Turkey Assessment and Policy Proposals
Ebsco Garnefski Cognitive coping strategies and symptoms of depression and anxiety a comparison be
Microsoft Assessment and Planning Toolkit 4 0 Usage Tracker Guide en
Microsoft Assessment and Planning Toolkit 4 0 Getting Started Guide en
PSYCHIC METHODS OF DIAGNOSIS AND TREATMENT IN ACUPUNCTURE …
Writing Assessment and Cognition
3 assessment and comments
BPD, Stigma, and Treatment Implications
więcej podobnych podstron