Effect of Passive Range of Motion
Exercises on Lower-Extremity
Goniometric Measurements of
Adults With Cerebral Palsy:
A Single-Subject Design
Background and Purpose. People with spastic cerebral palsy often
receive passive stretching that is intended to maintain or increase joint
passive range of motion (PROM) even though the effectiveness of
these exercises has not been definitively demonstrated. The purpose of
this study was to determine the effect of PROM exercises on 6 adults
with spastic quadriplegia and contractures. Participants. Four men and
2 women (X
⫽31 years of age, range⫽20–44 years) who lived in an
institution for people with mental retardation participated in the study.
Methods. The authors used 2 multiple baseline designs. Three partic-
ipants (group 1) received lower-extremity PROM exercises during
phase A; PROM exercises were discontinued during phase B. Three
participants (group 2) did not receive PROM exercises during phase A;
PROM exercises were initiated during phase B. Data were analyzed
using visual analysis and the C statistic. Results. Results varied with the
method of analysis; however, phase A and phase B measurements,
overall, did not differ for either group. Discussion and Conclusion. This
study demonstrated use of a single-subject design to measure the effect
of PROM exercises on adults with cerebral palsy. The authors con-
cluded that the PROM exercise protocol did not have an effect on the
lower-extremity goniometric measurements of the participants.
[Cadenhead SL, McEwen IR, Thompson DM. Effect of passive range of
motion exercises on lower-extremity goniometric measurements of adults
with cerebral palsy: a single-subject design. Phys Ther. 2002;82:658 – 669.]
Key Words: Cerebral palsy, Contractures, Passive range of motion, Single-subject design.
Sherri L Cadenhead, Irene R McEwen, David M Thompson
658
Physical Therapy . Volume 82 . Number 7 . July 2002
Research
Report
䢇
ўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўў
ўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўў
ўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўў

C
ontractures are among the most common sec-
ondary impairments associated with cerebral
palsy, particularly for people with the spastic
type of cerebral palsy.
1
Contracture, as it relates to
cerebral palsy, has been defined in several ways, includ-
ing permanent contraction of a muscle,
2
high resistance
to passive stretch,
2
hypoextensibility,
3,4
diminished
range of passive stretch,
5
and intrinsic muscle shortening
that prevents full range of motion.
6
Many interrelated
factors have been proposed to cause contractures in
people with cerebral palsy, including more activation of
muscles on one side of a joint than on the other side,
4
changes in connective tissue and muscle length,
7,8
slow
muscle growth,
4
and positioning.
9
People with spastic
cerebral palsy who do not walk and whose voluntary
movement is restricted to the extent that they cannot
independently move their joints through the full range
of motion during daily activities are at particularly high
risk for developing a contracture.
10
Passive stretching is one physical therapy intervention
for the prevention or reduction of contractures associ-
ated with cerebral palsy.
10,11
In our experience, clini-
cians frequently advocate a prolonged stretch, with the
rationale based in part on a classic study by Tardieu
et al.
5
Tardieu and colleagues measured the amount of
time that the soleus muscles of children with cerebral
palsy were elongated beyond a minimum threshold
length throughout each day. After 7 months, contrac-
tures increased in participants whose soleus muscle was
elongated for only 2 hours per day, but these contrac-
tures did not increase in participants whose soleus
muscle was elongated for at least 6 hours a day.
Casting
12
and splinting
13,14
are 2 interventions that pro-
vide a prolonged stretch and have been shown to be
effective in preventing or reducing knee and ankle
contractures in children with cerebral palsy. Positioning,
such as lying prone, standing in standers,
15
and sitting
with the hips abducted,
16
also can provide a prolonged
SL Cadenhead, PT, MS, PCS, is Early Interventionist, Programs for Infants and Children, Anchorage, Ala. At the time the study was conducted,
she was employed at the Northern Oklahoma Resource Center, Enid, Okla.
IR McEwen, PT, PhD, is Presbyterian Health Foundation Presidential Professor, Department of Physical Therapy, University of Oklahoma Health
Sciences Center, PO Box 26901, Oklahoma City, OK 73190 (USA) (irene-mcewen@ouhsc.edu). Address correspondence to Dr McEwen.
DM Thompson, PT, MS, is Assistant Professor, Department of Physical Therapy, University of Oklahoma Health Sciences Center.
All authors provided concept/research design and data analysis. Ms Cadenhead and Dr McEwen provided writing. Ms Cadenhead provided data
collection and project management, and Dr McEwen provided fund procurement. The authors thank the occupational therapist who helped with
data collection, the physical therapist who participated in the interrater reliability study, and the participants’ physician who assisted with the study.
This study was conducted in partial fulfillment of the requirements for Ms Cadenhead’s postprofessional Master of Science degree from the
University of Oklahoma Health Sciences Center. The study was approved by the University of Oklahoma Health Sciences Center Institutional
Review Board and by the Human Rights Committee of the Northern Oklahoma Resource Center.
The study was partially supported by Preparation of Related Services Personnel grants H029F00056 and H029F30020 from the US Department of
Education, Office of Special Education and Rehabilitative Services. This article, however, does not necessarily reflect the policy of that office, and
official endorsement should not be inferred.
This article was submitted March 7, 2001, and was accepted November 13, 2001.
Physical Therapy . Volume 82 . Number 7 . July 2002
Cadenhead et al . 659
ўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўўў
ў

stretch. The effectiveness of most positioning for main-
taining or increasing range of motion of people with
cerebral palsy, however, has not been studied.
15,17
Researchers have shown that using a chair to provide a 5-
to 7-hour adductor stretch per day, along with 1 to 3
therapy sessions per week for “progressive manual
stretching,”
16(p984)
did prevent adductor muscle contrac-
tures in children with cerebral palsy.
A practical problem associated with providing a pro-
longed stretch using splints, casts, or positioning is that
adults with severe cerebral palsy often have contractures
in many joints and limitations in more than one plane of
movement. Hip motion, for example, typically is
restricted in abduction, lateral rotation, and exten-
sion.
11,16
Another problem is that the severity of the
contractures can limit positioning options, such as stand-
ing. Passive range of motion (PROM) exercises are
interventions that are used for contractures of any
severity and all limitations of joint PROM. Although
some authors have proposed that PROM exercises are
ineffective
18
(an opinion that is supported by the studies
showing prolonged elongation to be necessary
5,12–14
),
other therapists continue to use passive stretching.
10,11
In 2 studies, researchers found at least minimal benefits
to PROM exercises for young people with cerebral
palsy.
7,19
Over a 2-year period, McPherson et al
7
examined the
effects of PROM exercises and positioning on knee
flexion contractures of 4 participants between 10 to 18
years of age. During the first year of the study, the
participants received PROM exercises 3 times a day at
school and twice a week at home. During the second
year, PROM exercises at school were discontinued, and
participants were positioned in prone and supine stand-
ers for 1 hour a day. The PROM exercises continued
twice a week at home. The authors compared PROM
measurements for periods of treatment (when school
was in session) with PROM measurements for periods of
nontreatment (Christmas and summer vacations). The
participants’ PROM measurements increased during the
2 school semesters of the first year and the fall semester
of the second year, and they decreased during 3 of the 4
nontreatment periods. The average increase over the
year was 4 to 9 degrees, and the average decrease during
nontreatment times was 5 to 10 degrees.
Miedaner and Renander
19
studied 13 participants who
were 6 to 20 years of age and assigned the participants to
1 of 2 groups. For 5 weeks, one group received PROM
exercises 5 consecutive days a week, and the other group
received PROM exercises 2 nonconsecutive days a week.
For the next 5 weeks, the frequency of exercise was
reversed for the 2 groups. Changes in PROM measure-
ments averaged plus or minus 2.5 degrees. Frequency of
PROM exercises made no difference in 6 of the 7
lower-extremity measurements. Straight leg raising on
the right side was greater under the 5-day-per-week
condition than under the twice-a-week condition. As was
the case in the study by McPherson et al,
7
participants
received positioning and bracing in the classroom and
PROM exercises at home throughout the study, which
makes the contribution of the PROM exercises unclear.
Although research supporting the effectiveness (or inef-
fectiveness) of PROM exercises is limited, we have
observed that PROM exercises are commonly used inter-
ventions for adults with cerebral palsy in institutions and
community-based programs. These exercises usually are
carried out by staff who have been taught by physical
therapists to do the exercises during times set aside for
exercise or during daily activities (eg, dressing, bathing).
Although the performance of PROM exercises often
continues for years, we have observed few attempts to
determine whether they are effective. A single-subject
research design is one method of gathering evidence in
clinical settings to determine whether an intervention is
effective.
20
We used a single-subject research design for
this study to examine the effect of PROM exercises on
lower-extremity PROM measurements of 6 adults with
cerebral palsy.
Method
Participants
Six adults (4 men and 2 women; X
⫽31 years of age,
range
⫽20–44 years) with spastic quadriplegic cerebral
palsy participated in the study. See Table 1 for descrip-
tions of the participants. All participants lived in a
state-operated residential facility for people diagnosed
with mental retardation. A physician and the first
author (SLC) selected participants based on 4 criteria:
(1) having a legal guardian who could be contacted and
who was willing to sign the informed consent form,
(2) presence of lower-extremity contractures measuring
20 degrees or greater in at least 3 of the joint motions
measured in the study (ie, hip extension, hip abduction,
hip lateral rotation, knee extension, and ankle dorsiflex-
ion),
13
(3) use of a wheelchair as the primary means of
mobility, and (4) current or previous participation in a
physical therapy program. Exclusion criteria were: (1) a
history of resisting PROM exercises to the extent that full
PROM was rarely, if ever, achieved, as judged by the first
author, (2) a medical condition that might have pre-
vented the participant from completing the study, (3) a
diagnosis of arthritis or other joint disease, (4) lower-
extremity orthopedic surgery within 2 years of the begin-
ning of the study, and (5) a windswept hip deformity
(limitations of adduction and medial rotation of one hip
and limitation of abduction and lateral rotation of the
660 . Cadenhead et al
Physical Therapy . Volume 82 . Number 7 . July 2002
opposite hip
21
) that prevented positioning for goniomet-
ric measurements.
We planned the study to be a single-subject, multiple-
baseline design with 6 participants, 3 of whom received
PROM exercises (group 1) and 3 of whom had not
received PROM exercises for at least 6 months before
the start of the study (group 2). All participants had
previously received PROM exercises and developmental
therapy for many years, but PROM exercises had been
discontinued for group 2 participants after they demon-
strated fairly stable PROM measurements over time, as
determined by annual physical therapy examinations.
We wanted to know whether the PROM of participants
who were receiving PROM exercises would change when
the exercises were discontinued and whether the PROM
of participants who had not been receiving the exercises
would change when exercises were provided.
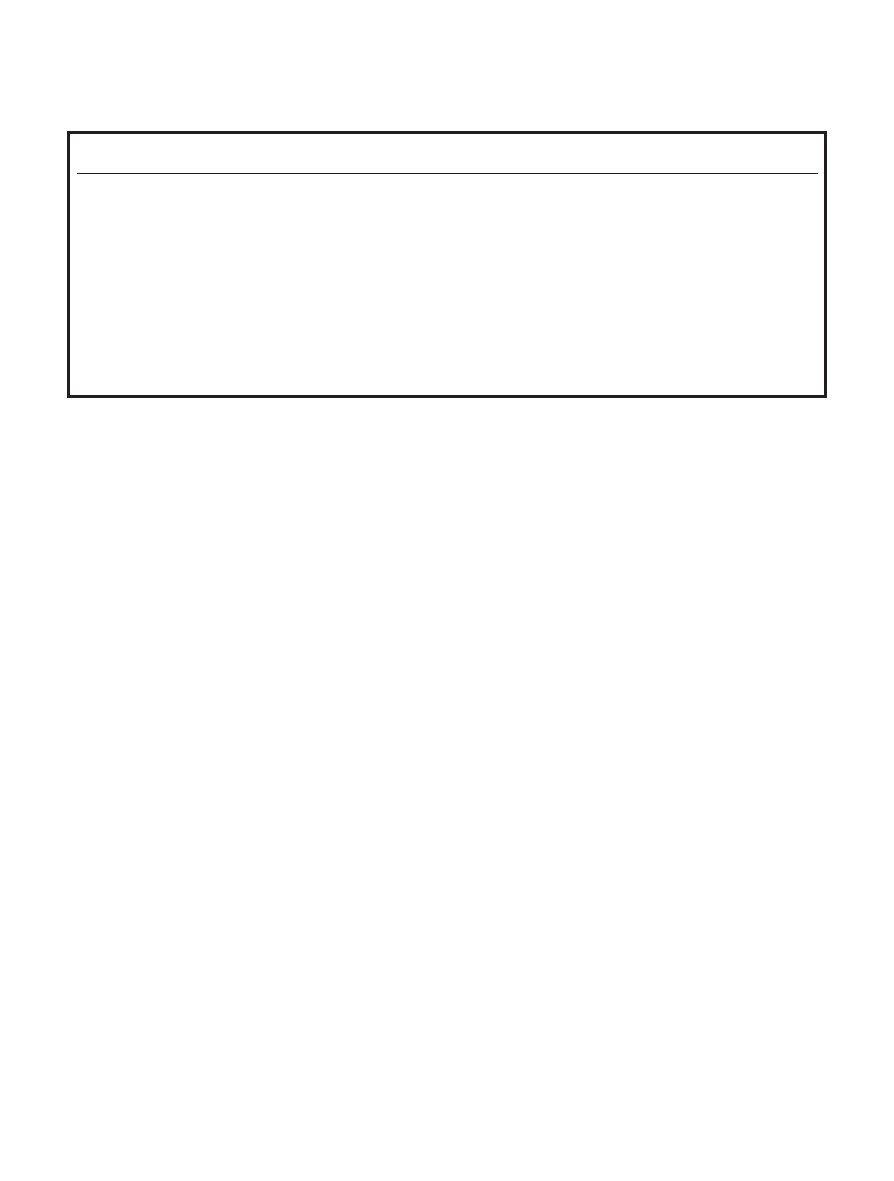
Table 1 lists characteristics of the 6 participants. All were
diagnosed as having mental retardation, but the true
abilities of people with severe cerebral palsy and limited
communication skills can be difficult to measure. The
musculoskeletal status and functional abilities of the 2
groups were similar, but the average age of the group 1
participants was 25 years (range
⫽20–32 years), and the
average age of the group 2 participants was 36 years
(range
⫽32–44 years). The older age of the group 2
participants probably contributed to the decision to
discontinue their PROM exercises, which had occurred
before the first author started working at the institution.
These 6 participants were selected for the study because
they were the first people who met the inclusion criteria
and whose legal guardians provided us with informed
consent.
Design
The study consisted of 2 multiple-baseline designs, each
with 3 participants.
22
During phase A, group 1 partici-
pants, who had been receiving PROM exercises 3 times
per week, continued to receive PROM exercises. During
phase B, PROM exercises were discontinued. Group 2
participants received no PROM exercises during phase
A, and PROM exercises were provided during phase B.
As is customary in multiple-baseline designs, the dura-
tion of each phase for each participant was individual-
ized, and the initiation of phase B was staggered across
the participants as each participant’s PROM measure-
ments became stable.
22
For the majority of the joints
measured, PROM measurements were considered stable
when they were within 5 degrees of each other
23
over a
period of at least 3 out of 4 weeks. Stability, or a stable
trend (increasing or decreasing measurements at a
constant rate of change) over a period of 3 out of 4
weeks, was the criterion for discontinuing PROM exer-
cises for group 1 participants or for beginning PROM
exercises for group 2 participants. All participants were
measured each week for 16 consecutive weeks. Phase A
measurements for group 1 participants were established
after 5 weeks for participant 1A, after 8 weeks for
participant 1B, and after 11 weeks for participant 1C. For
group 2 participants, phase A measurements were estab-
lished after 4 weeks for participant 2A, after 8 weeks for
participant 2B, and after 11 weeks for participant 2C.
Passive Range of Motion Program
The independent variable was a PROM exercise pro-
gram for the joint motions of hip extension, hip abduc-
tion, hip lateral rotation, knee extension, and ankle
dorsiflexion. The first author instructed physical therapy
aides in the PROM exercise protocol. Instruction
included verbal explanation, demonstration, observa-
Table 1.
Participant Characteristics
Participant
Age
(y)
Sex
Orthopedic
Surgery
Functional Status
1A
23
Female
Spine, hips, knees
Followed simple commands, repeatedly vocalized nonwords. Assisted minimally with
transfers and other activities of daily living (ADL). Independent wheelchair mobility
on level terrain.
1B
32
Male
None
Could not talk, but appeared to have good receptive communication. Dependent for all
ADL and wheelchair mobility.
1C
20
Male
Spine, hips, knees
Used manual signs to make requests. Independent wheelchair mobility on level terrain
with assistance with doors. Independent in some transfers and ADL.
2A
32
Male
None
Communicated with facial expressions. Dependent for all ADL and wheelchair mobility.
2B
44
Male
Spine
Laughed, screamed, and pulled others to him to communicate. Moved wheelchair short
distances and needed assistance for all ADL.
2C
33
Female
None
Communicated with facial expressions. Assisted minimally with transfers. Dependent for
ADL and wheelchair mobility.
Physical Therapy . Volume 82 . Number 7 . July 2002
Cadenhead et al . 661
ўўўўўўўўўўўўўўўўўўўўўўўў
ў

tion of the aides performing each exercise, feedback on
their performance, and written instructions with pictures
illustrating how to perform each exercise. The exercises
were based on PROM exercises published by Bezner
24
and Kisner and Colby.
25
For each of the participants, the
investigator monitored one exercise session a week
throughout the study to ensure that the physical therapy
aides adhered to the protocol.
The protocol was based on 2 studies in which the
effectiveness of PROM exercise for young people with
cerebral palsy was studied.
7,19
In both studies, the PROM
exercises consisted of moving an extremity passively to
the end of the PROM and holding this position for 20 to
60 seconds, then repeating this stretch 5 times. Research-
ers studying people with and without neuromusculo-
skeletal impairments have found that one 30-second
stretch 5 days a week is as effective in increasing ham-
string muscle length as one 60-second stretch or three
30- or 60-second stretches.
26,27
Based on our experience
with people with cerebral palsy, however, we believe that
more than one repetition is beneficial because resistance
to passive stretch seems to decrease with repetition.
The aides performed 5 repetitions of each passive joint
motion, holding the position at the end of the range for
20 seconds during each repetition. They were instructed
to move the joint only to the point of resistance and to
avoid forcing the movement. They also were given
instructions for obtaining as much motion as possible,
such as moving slowly, providing a gentle continuous
stretch, avoiding pressure on the balls of the feet or
palms of the hand, and bending an adjacent joint if
movement was difficult to initiate.
The aides could do the 5 exercises in any order that they
chose. Participants were placed in a supine position for
all exercises except hip extension. For the hip extension
exercise, participants were positioned prone with their
hips at the edge of the table. The aides’ hand placements
were done as illustrated in Bezner.
24
The PROM exercise sessions were carried out 3 times per
week. Each session lasted for approximately 30 to 45
minutes, including time for transferring, positioning,
and talking with the participant. In the studies
26,27
of
people without neuromusculoskeletal impairments, the
researchers did not examine frequencies other than 5
days per week. They provided no rationale for using this
frequency. We selected a frequency of 3 days per week
because, in our experience, it is a frequency often used
for adults with cerebral palsy living in institutions and
because Miedaner and Renander
19
found that PROM
did not differ when their participants received PROM
exercises 2 times a week or 5 times a week.
Goniometric Measurements
Our study’s dependent variables were bilateral gonio-
metric measurements of hip extension, hip abduction,
hip lateral rotation, and ankle dorsiflexion as well as 2
measurements of knee extension: one with the hip
flexed and the other with the hip extended. Measure-
ments were taken each week using a 30.48-cm (12-in)
plastic goniometer with a 360-degree scale. Although the
reliability of goniometry for measuring joint limitations
due to contractures has been questioned,
28,29
investiga-
tors often have used a goniometer to measure the joint
PROM of people with cerebral palsy.
7,19
To promote
consistency in measurements, the 16 measurement ses-
sions for each participant were done on the same day of
the week and at the same time of day, with the partici-
pant lying on a firm, vinyl-covered, high-low mat table.
Semipermanent marks were made on each participant’s
bony landmarks with a laundry marker to identify the
goniometer’s fulcrum, stationary arm, and measurement
arm positions. Color photographs of the measurement
positions and specific written instructions for the 6 joint
motions were available for the aides and therapists to
review throughout the study.
When measuring each joint motion, the first author,
designated as therapist 1, moved the extremity passively
through the full available PROM for 3 repetitions. A slow
30-second stretch was applied on the third repetition to
“differentiate a reflex or active muscle contraction from
the structural limitation of the muscle, tendon, or joint
capsule.”
29(p661)
This procedure was intended to mini-
mize resistance to passive stretch and identify the end of
the PROM. The joint PROM was measured at the end of
the 30-second stretch by an occupational therapist (ther-
apist 2). Although having someone other than the
principal investigator move the limb through the PROM
(to control for potential bias) would be the preferred
method, another person with the necessary skill was not
available for the number of measurement sessions
required. To help control for bias, therapist 2 was not
informed of the participants’ group assignments and
their progress within and between the phases of the
study.
The testing sequence was consistent for every measure-
ment session,
30
and the procedures for positioning and
hand placement were standardized for each joint
motion.
31
First, each participant’s right lower extremity
was measured in the following order: (1) knee extension
in the supine position with the hip extended
29
; (2) knee
extension in the supine position with the hip flexed to
90 degrees, as indicated by a goniometer that was fixed
at 90 degrees and positioned on the mat table at the level
of the greater trochanter
19
; (3) ankle dorsiflexion in the
supine position with the knee extended and the calca-
neus in as neutral a position as possible in an attempt
662 . Cadenhead et al
Physical Therapy . Volume 82 . Number 7 . July 2002
to distinguish between ankle and forefoot motion
29
;
(4) hip abduction in the supine position with the hip
extended and the lower leg positioned off of the end of
the table
32
; (5) hip lateral rotation in the supine position
with the lower leg positioned off of the end of the
table
28
; and (6) hip extension in the prone position with
the hips at the edge of the table, the pelvis level, and the
knee flexed.
33
While the participant was positioned
prone, left hip extension was measured. Then, the
remaining left lower-extremity joints were measured in
the same order as the joints of the right lower extremity.
Because all of the participants had knee flexion contrac-
tures and because of the importance of knee extension
with hip flexion for wheelchair seating, knee extension
was measured with the hip extended as far as possible
and with the hip flexed to 90 degrees. Flexing the hip to
90 degrees also was intended to control any effects on
knee PROM if hip extension changed over the course of
the study.
Reliability
To determine interrater reliability, approximately 18%
of the measurements, including 2 or 3 measurement
sessions per participant, were repeated independently by
another physical therapist (therapist 3) throughout the
duration of the study. Therapist 3 participated only in
the reliability study and did not know the participants’
group assignments and progress. Therapist 3 followed
the measurement protocol while therapist 1 (the first
author) measured the joint PROM. Therapist 1 used a
goniometer that was masked on one side with paper to
prevent her from seeing the result until after therapist 2
(the occupational therapist) had recorded each mea-
surement.
34
Before the study was initiated, the 3 thera-
pists practiced the measurement, positioning, and
stretching techniques until they achieved agreement
within 5 degrees per joint measurement. We chose to
determine interrater reliability rather than intrarater
reliability because (1) we were concerned that memory
would affect 2 trials by one rater separated by a short
interval and (2) if interrater agreement was acceptable,
intrarater agreement also was likely to be acceptable.
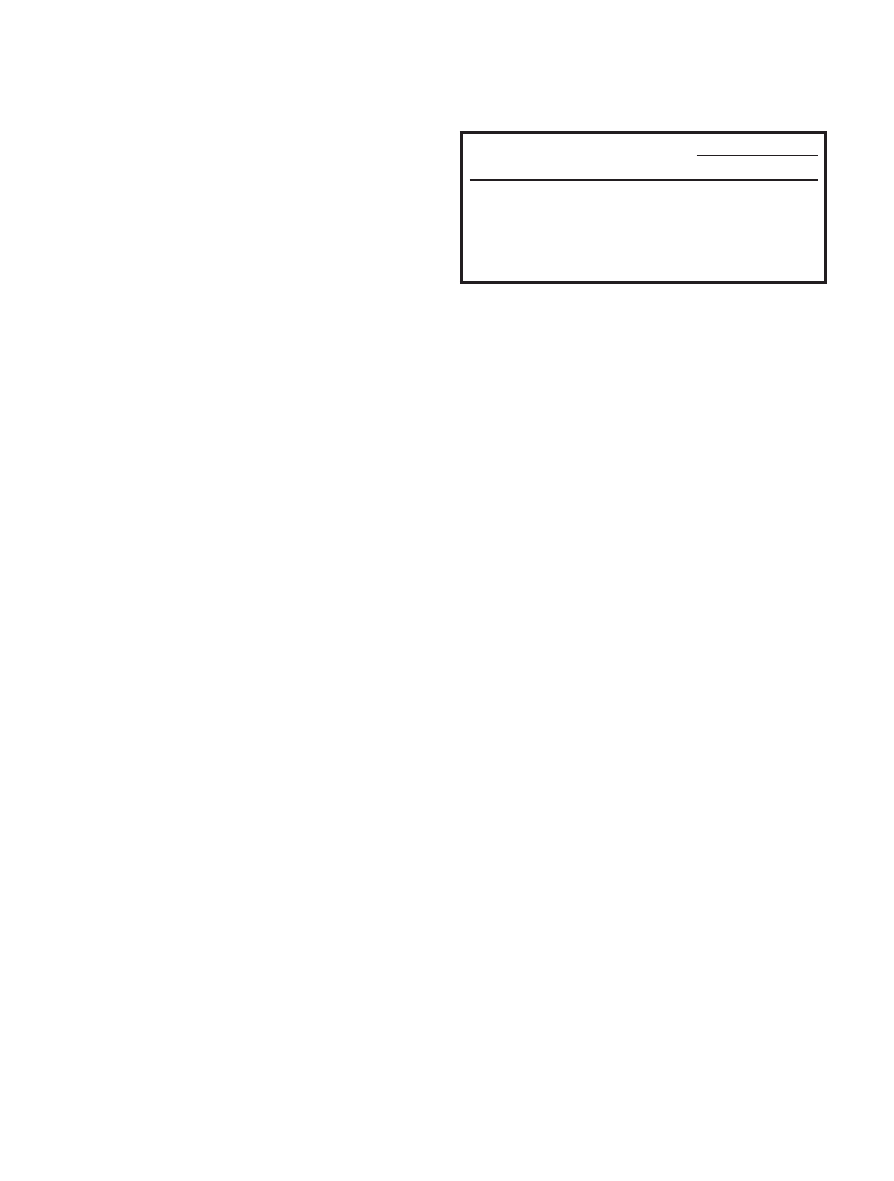
Reliability was represented by an intraclass correlation
coefficient (ICC), model 3,1.
22,35
Table 2 shows that
coefficients were between .785 for right hip lateral
rotation and .988 for right knee extension with the hip
flexed to 90 degrees.
Data Analysis
The goniometric measurements collected over the
course of the study were recorded on 12 graphs for each
participant (one graph for each of the 6 right and left
joint motions), for a total of 72 graphs. The graphs were
oriented to show an increase in PROM when the data
points went in an upward direction and a decrease in
PROM when they went in a downward direction.
We first analyzed the graphed data through visual anal-
ysis, a traditional method of interpreting single-subject
research,
36
to determine whether PROM improved,
decreased, or did not change across the 2 phases.
Through visual analysis, investigators look grossly at
level, trend, variability, and slope of the graphed data.
37
We used trend data more than level data because
changes in level (eg, rapid change in PROM) were not
expected and were due possibly to measurement error.
We also used visual analysis of trends in conjunction with
phase values and changes in slope between phases to
determine trend change scores (eg, a joint motion with
a low trend phase value [3 or less] and a low slope
[approximately 1.0 to 1.05] indicated no change). We
disregarded outlier data points (defined as a data point
that was 20 degrees greater than or less than the data
points immediately before and after it) if at least 5 other
data points were available in that phase, and we consid-
ered data that remained consistently variable across
phases to demonstrate no change.
Investigators have noted that visual analysis alone may
lead to inconsistent results.
38,39
For this reason and
because small treatment effects were expected,
37
we also
used the C statistic to further analyze the data.
40,41
Nourbakhsh and Ottenbacher
42
used 3 statistical meth-
ods for single-subject data—the split-middle method of
trend estimation, the two-standard deviation bandwidth
method, and the C statistic—to analyze the same 42
graphs. They found somewhat different results using
each method and concluded that researchers should use
several approaches to analyze single-subject data, one of
which should be visual analysis. We chose the C statistic
as the other method because many of the graphs showed
a visually obvious trend, which made the two–standard
deviation bandwidth method inappropriate,
42
and
because the split-middle method of trend estimation
often is inconsistent with visual analysis.
Table 2.
Interrater Reliability Intraclass Correlation Coefficients (ICC [3,1])
Joint Motion
ICC
Right
Left
Hip abduction
.966
.967
Hip extension
.981
.942
Hip lateral rotation
.785
.869
Knee extension, hip extended
.982
.980
Knee extension, hip flexed 90°
.988
.814
Ankle dorsiflexion
.978
.877
Physical Therapy . Volume 82 . Number 7 . July 2002
Cadenhead et al . 663
ўўўўўўўўўўўўўўўўўўўўўўўў
ў

With the C statistic, phase A data are analyzed first to
determine whether a statistically significant trend exists.
Statistical significance is determined by dividing C by its
standard error, which gives a z value that can be inter-
preted using the normal probability table for z
scores.
40,42
If a trend is not found, the phase B data are
appended to the phase A data, and the combined data
are reanalyzed using the same procedure. If a trend is
found in the phase A data, a less powerful alternative
procedure can be used to construct separate data series
from phase A and phase B data and to compare them. A
significant z score indicates that the trend in phase A and
phase B are different.
40
We used a 1-tailed test with an
alpha of .05 (z
ⱖ1.645). The unidirectional hypothesis
was that PROM would be greater during the phase in
which PROM exercises were provided.
Results
Group 1
Table 3 shows the means, standard deviations, visual
analysis results, and z values of the 36 graphs for group 1
participants. This group received PROM exercises dur-
ing phase A and PROM exercises were discontinued
during phase B.
Visual analysis of the data of participant 1A indicated no
change in PROM between phase A and phase B for 10 of
the 12 joints measured. The rate of increase in left hip
extension decreased during phase B and a downward
trend occurred in right ankle dorsiflexion during phase
B. Both observations were supported by the z values. The
z values also indicated a difference between phases in
bilateral hip lateral rotation and knee extension with the
hip flexed 90 degrees. Visual analysis indicated that the
reason for the discrepancy was probably the increasing
trend during the relatively short phase A, which leveled
off during phase B.
Visual analysis of participant 1B’s data identified no
change in 7 of the 12 measurements. Right and left hip
lateral rotation showed a downward trend in phase B
and ankle dorsiflexion decreased bilaterally during
phase B. Left hip abduction increased during phase B.
The z values supported a difference in these 5 measure-
ments. The z values also indicated a difference in right
and left knee extension with the hip flexed 90 degrees,
which visual analysis had not revealed. We examined the
graphs again to try to determine the reason for the
discrepancy and saw that PROM increased during phase
B (also indicated by the means), but not enough to say
with any confidence that a difference existed. The z
values could not support a difference because we used a
1-tailed test, and the direction of any difference was in
the opposite direction.
Visual analysis of participant 1C’s data showed no differ-
ence in PROM between phases for 9 of the 12 measure-
ments. During phase B, right hip lateral rotation and
right knee extension with the hip flexed 90 degrees
decreased. This finding was supported by the z values.
Visual analysis indicated that left hip abduction
increased during phase B. The visual analysis did not
support the z values, which indicated a difference in
right hip extension and left knee extension with the hip
flexed 90 degrees. Reinspection of the graphs again
indicated no change, which was supported by the mean
PROM during the 2 phases. The long baseline with an
increasing trend in the baseline data may have affected
the C statistic results.
Group 2
Table 4 shows the means, standard deviations, visual
analysis results, and z values for the 36 graphs for group
2. Group 2 participants did not receive PROM exercises
during phase A and PROM exercises were provided
during phase B.
Visual analysis of the data for participant 2A showed no
change in 7 of the 12 PROM measurements. Visual
analysis indicated an increase in 2 measurements during
phase B: left knee extension with the hip extended and
left knee extension with the hip flexed 90 degrees. The
z values supported these 2 observations and indicated no
other increases in PROM during phase B. Visual analysis
indicated a decrease in 3 measurements when PROM
exercises were provided during phase B: right hip exten-
sion, right knee extension with the hip extended, and
right ankle dorsiflexion.
Visual analysis of participant 2B’s data indicated no
change in 8 of the 12 measurements. Visual analysis
showed a negative change in 4 measurements during
phase B: bilateral hip lateral rotation and dorsiflexion.
No positive changes were identified with visual analysis
or the z values.
Visual analysis of the data of participant 2C indicated no
change in 8 of the 12 PROM measurements. A negative
change was observed during phase B in 3 PROM mea-
surements: bilateral hip lateral rotation and right ankle
dorsiflexion. Visual analysis and the z value indicated an
increase in right hip abduction during phase B.
In summary, visual analysis of the grouped data for the
subjects in group 1 showed no change in 28 of 36 joints
when PROM exercises were discontinued. Visual analysis
showed decreased PROM in 8 joints, results that the z
values supported. Visual analysis also showed an increase
in PROM for 2 of the 36 joints after PROM exercises
were discontinued. The z values indicated a decrease in
4 joint PROM measurements when PROM exercises
664 . Cadenhead et al
Physical Therapy . Volume 82 . Number 7 . July 2002
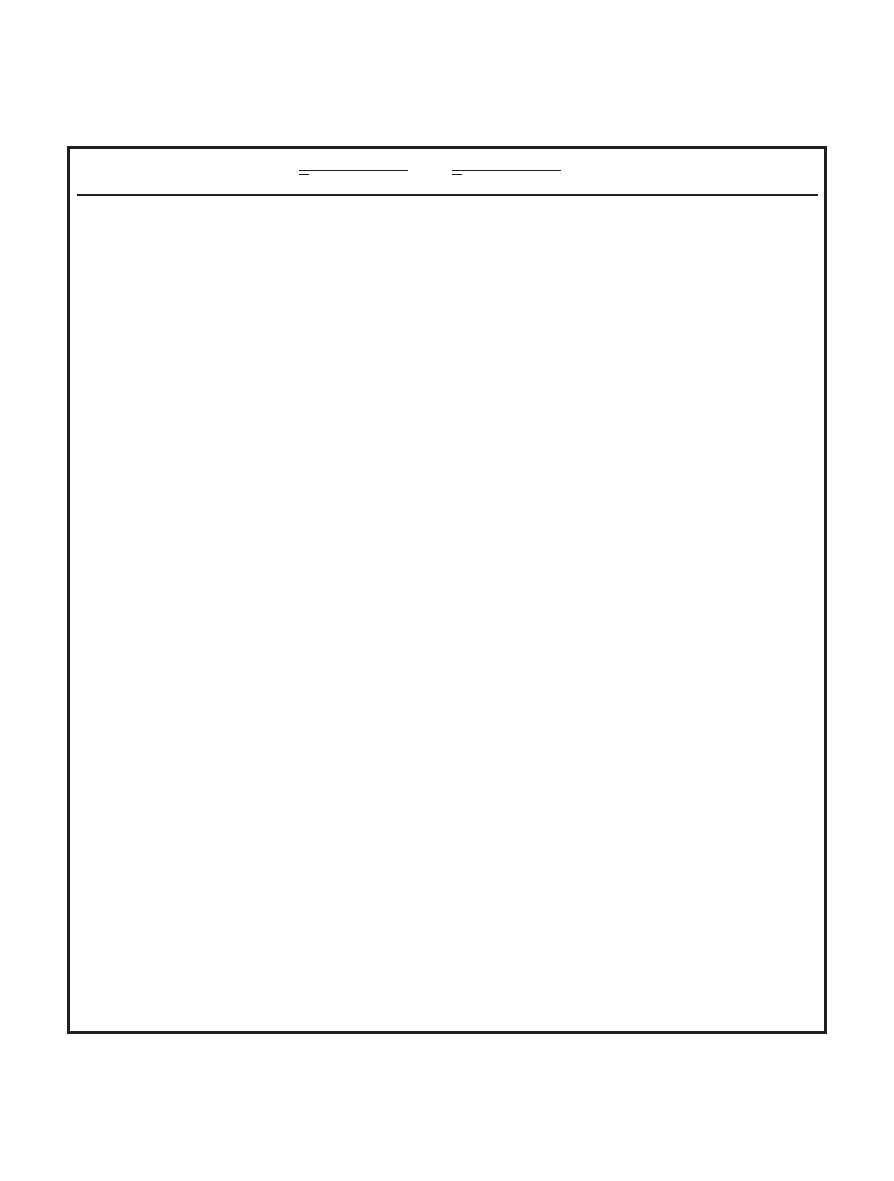
Table 3.
Goniometric Data (in Degrees) for Group 1 Participants Who Received Passive Range of Motion (PROM) Exercises During Phase A and Did Not
Receive PROM Exercises During Phase B
Phase A
Phase B
Visual
Analysis
a
Phase
A z
b
z
b
X
SD
X
SD
Participant A
Hip extension
Right
⫺14.2
4.4
⫺8.3
2.5
0
⫺0.36
1.55
Left
⫺35.2
12.3
⫺22.4
3.1
⫺
0.95
2.82
d
Hip abduction
Right
3.2
6.6
8.0
2.9
0
⫺0.72
0.47
Left
21.2
6.1
23.6
3.6
0
⫺0.44
⫺0.29
Hip lateral rotation
Right
34.4
10.0
48.9
2.9
0
1.43
3.37
d
Left
20.0
5.2
25.9
5.1
0
1.86
c
2.07
d
Knee extension (hip extended)
Right
⫺61.4
3.4
⫺64.3
2.0
0
⫺1.31
0.16
Left
⫺73.6
6.4
⫺66.8
3.3
0
⫺1.44
1.05
Knee extension (hip flexed 90°)
Right
⫺70.8
4.1
⫺67.6
2.5
0
1.16
1.84
d
Left
⫺67.0
1.2
⫺65.8
2.6
0
0.24
1.69
d
Ankle dorsiflexion
Right
20.4
5.3
22.8
3.6
⫺
1.79
c
1.74
d
Left
24.6
16.0
39.4
6.4
0
1.68
c
1.31
Participant B
Hip extension
Right
⫺15.0
4.8
⫺12.0
3.5
0
⫺0.63
⫺0.14
Left
⫺24.5
4.8
⫺19.5
4.5
0
⫺1.38
0.58
Hip abduction
Right
2.1
9.5
⫺7.2
3.5
0
2.21
c
2.14
d
Left
2.9
5.5
8.0
5.4
⫹
1.72
c
1.68
Hip lateral rotation
Right
27.9
5.5
27.0
9.8
⫺
2.14
c
2.40
d
Left
25.1
8.2
26.9
5.3
⫺
1.50
1.75
d
Knee extension (hip extended)
Right
⫺70.0
4.4
⫺66.0
4.7
0
⫺1.07
⫺0.92
Left
⫺67.9
5.4
⫺62.0
5.8
0
1.07
1.28
Knee extension (hip flexed 90°)
Right
⫺92.8
8.4
⫺79.8
6.1
0
1.09
2.17
d
Left
⫺88.9
9.5
⫺75.3
5.5
0
2.12
c
1.73
d
Ankle dorsiflexion
Right
48.1
6.5
44.3
6.2
⫺
1.88
c
2.50
d
Left
43.8
9.8
36.8
7.3
⫺
1.95
c
1.92
d
Participant C
Hip extension
Right
⫺17.7
4.4
⫺18.8
2.8
0
2.56
c
2.23
d
Left
⫺26.1
4.9
⫺26.4
3.4
0
1.01
1.39
Hip abduction
Right
25.0
5.9
23.6
5.7
0
0.73
0.04
Left
3.3
6.1
10.6
6.1
⫹
⫺1.76
c
⫺0.19
Hip lateral rotation
Right
39.1
11.8
39.6
12.1
⫺
2.94
c
1.88
d
Left
37.2
7.2
31.2
2.2
0
1.75
c
0.77
Knee extension (hip extended)
Right
⫺65.3
5.8
⫺63.6
2.0
0
⫺0.72
⫺0.76
Left
⫺78.2
4.4
⫺69.0
1.9
0
2.17
c
1.57
Knee extension (hip flexed 90°)
Right
⫺82.0
9.4
⫺82.6
2.1
⫺
2.11
c
2.19
d
Left
⫺81.2
6.7
⫺78.0
2.0
⫺
2.43
c
1.71
d
Ankle dorsiflexion
Right
36.0
7.7
33.0
9.6
0
2.30
c
1.41
Left
28.0
7.4
24.2
2.8
0
1.15
1.48
a
0
⫽no difference in PROM measurements between phase A and phase B, ⫺⫽negative change in PROM measurements in phase B, and ⫹⫽positive change in
PROM measurements in phase B.
b
Derived from C statistic.
c
Significant trend in phase A data (P
ⱕ.05).
d
Significant negative change in PROM in phase B (1-tailed P
ⱕ.05).
Physical Therapy . Volume 82 . Number 7 . July 2002
Cadenhead et al . 665
ўўўўўўўўўўўўўўўўўўўўўўўў
ў
Table 4.
Goniometric Data (in Degrees) for Group 2 Participants Who Did Not Receive Passive Range of Motion (PROM) Exercises During Phase A and
Received PROM Exercises During Phase B
Phase A
Phase B
Visual
Analysis
a
Phase
A z
b
z
b
X
SD
X
SD
Participant A
Hip extension
Right
⫺23.5
11.4
⫺20.7
4.3
⫺
1.01
1.00
Left
⫺27.3
7.3
⫺14.0
3.8
0
1.45
3.38
Hip abduction
Right
3.3
1.5
7.0
4.2
0
⫺1.72
c
0.14
Left
17.25
2.5
22.2
5.2
0
1.72
⫺0.03
Hip lateral rotation
Right
22.5
9.1
30.4
12.7
0
1.36
1.16
Left
27.0
7.8
36.2
12.4
0
1.63
0.91
Knee extension (hip extended)
Right
⫺53.8
3.3
⫺53.7
6.8
⫺
1.65
c
0.89
Left
⫺50.0
10.9
⫺19.8
6.0
⫹
⫺1.58
2.40
d
Knee extension (hip flexed 90°)
Right
⫺75.8
6.0
⫺61.1
3.7
0
1.66
c
0.46
Left
⫺81.5
16.8
⫺61.0
6.9
⫹
0.44
2.23
d
Ankle dorsiflexion
Right
35.0
5.6
37.6
5.9
⫺
1.19
1.68
Left
29.3
5.9
33.1
4.9
0
⫺1.07
⫺0.63
Participant B
Hip extension
Right
⫺36.6
4.0
⫺34.1
3.3
0
0.37
1.26
Left
⫺32.9
5.7
⫺25.0
3.7
0
0.92
2.13
Hip abduction
Right
⫺12.1
11.5
⫺11.3
12.6
0
0.34
0.08
Left
2.4
4.1
4.6
4.9
0
0.39
1.39
Hip lateral rotation
Right
19.0
7.3
14.9
8.3
⫺
1.31
2.69
Left
41.9
4.4
38.4
10.0
⫺
0.33
2.79
Knee extension (hip extended)
Right
⫺81.6
7.3
⫺73.0
8.0
0
⫺1.44
0.58
Left
⫺59.0
4.7
⫺55.9
3.6
0
0.18
0.77
Knee extension (hip flexed 90°)
Right
⫺81.1
4.7
⫺77.4
3.4
0
2.28
c
0.94
Left
⫺69.1
3.1
⫺66.1
3.3
0
0.13
0.38
Ankle dorsiflexion
Right
15.8
6.2
17.5
5.6
⫺
2.56
c
2.50
Left
18.8
8.5
14.6
12.2
⫺
1.93
c
0.86
Participant C
Hip extension
Right
⫺7.2
4.9
⫺5.2
2.6
0
1.37
1.51
Left
⫺23.0
4.1
⫺24.2
1.9
0
⫺1.10
⫺0.98
Hip abduction
Right
5.2
5.5
14.0
5.8
⫹
1.41
2.20
d
Left
1.9
5.3
3.2
2.9
0
2.32
c
⫺0.21
Hip lateral rotation
Right
27.0
11.9
36.8
6.1
⫺
3.09
c
1.12
Left
27.8
7.2
39.4
5.1
⫺
2.18
c
1.89
Knee extension (hip extended)
Right
⫺26.0
10.1
⫺16.8
3.9
0
2.80
c
1.72
Left
⫺73.1
10.7
⫺69.6
6.3
0
1.16
0.96
Knee extension (hip flexed 90°)
Right
⫺26.2
8.5
⫺20.6
2.2
0
1.73
c
0.52
Left
⫺62.8
9.0
⫺63.0
3.9
0
⫺0.36
⫺0.27
Ankle dorsiflexion
Right
15.0
12.6
19.6
7.9
⫺
⫺1.75
c
1.83
Left
6.5
9.2
8.0
4.5
0
⫺2.08
c
1.31
a
0
⫽no difference in PROM measurements between phase A and phase B, ⫺⫽negative change in PROM measurements in phase B, ⫹⫽positive change in PROM
measurements in phase B.
b
Derived from C statistic.
c
Significant trend in phase A data (P
ⱕ.05).
d
Significant positive change in PROM measurements in phase B (1-tailed P
ⱕ.05).
666 . Cadenhead et al
Physical Therapy . Volume 82 . Number 7 . July 2002

were discontinued, which was not supported by visual
analysis.
Visual analysis of the data of all 3 subjects in group 2
showed no change in PROM for 23 of 36 joints when
PROM exercises were provided. Visual analysis and the z
values indicated an increase in PROM in 3 joints when
PROM exercises were provided during phase B. Visual
analysis indicated a decrease in 10 measurements during
phase B.
Discussion and Conclusions
For both groups of participants, our results showed no
consistent differences in lower-extremity PROM mea-
surements when the participants received and did not
receive PROM exercises. Most of the participants dem-
onstrated a gradual increase in PROM in phase A and
showed little change in motion during phase B, regard-
less of whether PROM exercises were discontinued or
provided during phase B. As a result of the study, PROM
exercises were discontinued for all participants.
The gradual increase in PROM during phase A appeared
to be the result of the participants’ increasing coopera-
tion with the person taking the PROM measurements
over the first few weeks of the study. Although an
exclusion criterion was resistance to PROM to an extent
that joint range could not be achieved, the participants
did appear to guard against full PROM initially. The
participants also demonstrated week-to-week variability
in measurements that we believe were unlikely to be
related to real change in joint PROM.
We are not aware of research that has examined consis-
tency of goniometric measurements of adults with spas-
tic quadriplegic cerebral palsy; however, Harris and
colleagues
43
found wide daily variations when measuring
a child with spastic quadriplegia, and they concluded
that a change of 10 to 15 degrees may not represent real
change. We contend that our interrater reliability esti-
mates were excellent to good; however, we assessed
reliability by having 2 therapists measure the participants
on the same day, one immediately after the other.
Day-to-day variation in participants would not have been
affected by— or detected by— our method. Future
research to examine test-retest reliability of goniometric
measurements of adults with spastic quadriplegia and
cognitive impairments, with time between measure-
ments, could be useful.
Despite the variability of our measurements, we showed
that, for the 6 adults with cerebral palsy, PROM exercises
did not appear to generally affect lower-extremity gonio-
metric measurements over a 16-week period of time. A
limitation of our study was that all participants did not
receive the same amount of PROM exercises. The stag-
gered phase A and 16-week available time frame meant
that participants received from 5 to 12 weeks of PROM
exercises. The results, however, are consistent with the
views held by some authors
18,44
that passive exercise is
not effective in the management of contractures associ-
ated with cerebral palsy. The results are not consistent
with the results of the studies by McPherson et al
7
and
Miedaner and Renander,
19
who found modest PROM
increases following PROM intervention.
One reason for the inconsistency may be the age of the
participants. Our participants were between 20 and 44
years of age, and their contractures could have been less
responsive to change than participants in the other
studies who were between 6 and 20 years of age. Another
difference in the studies is that their participants
received positioning and other co-interventions, which
our participants did not receive. These co-interventions,
rather than the PROM exercises, could have been
responsible for the change.
The studies also differed in the number of participants,
the length of the intervention, the joints investigated,
and the research design. McPherson et al
7
used a group
design to study knee extension of 4 participants over a
2-year period. Miedaner and Renander
19
also used a
group design and studied the hip, knee, and ankle
PROM of 13 participants over 10 weeks. Our study was
similar to these previous studies in the limited number
of participants, but our use of a single-subject design
enabled us to analyze the effects of intervention for each
participant, which the group designs do not permit.
Some of the participants in the previous studies may not
have benefited from the intervention, but the analyses of
group data would have obscured the individual effects.
The amount of PROM exercise also may have contrib-
uted to lack of changes in the measurements. Although
the PROM protocol was based on the literature related
to people with cerebral palsy,
7,19
research with people
without neuromusculoskeletal deficits indicate that
stretching for one 30-second stretch 5 times per week is
effective.
26,27
Although this amount cannot be general-
ized to people with neuromusculoskeletal impairments,
it may be worth investigating. Another consideration is
the length of the intervention. Our 16-week study may
not have been long enough to show an effect of PROM
exercises or an effect of discontinuing them.
The results of our study cannot necessarily be general-
ized to other adults with cerebral palsy, particularly those
with characteristics that differ from those of our partic-
ipants. The external validity of single-subject research is
demonstrated by replication,
22
and our design and
methods lend themselves well to the clinical setting and
could be used by other clinicians to determine whether
Physical Therapy . Volume 82 . Number 7 . July 2002
Cadenhead et al . 667
ўўўўўўўўўўўўўўўўўўўўўўўў
ў

PROM exercise is effective for individual clients. Repli-
cation of the study with other people with similar
characteristics also would broaden its applicability.
22
For
future studies, a larger number of data points and a
more stable baseline could improve the accuracy of the
analyses.
Measurement and treatment of contractures will con-
tinue to be important for adults with cerebral palsy to
address potential deterioration, overuse syndromes, and
joint deterioration.
1
Physical therapy programs that
focus only on PROM, however, should be reconsidered
because both the clinical usefulness and social validity
45
of this intervention are questionable. Social validity is a
term used in applied behavior analysis, from which
single-subject research developed. It refers to the social
importance of treatment goals and procedures, and the
person’s satisfaction with them. Intervention, we believe,
must go beyond the person’s secondary impairments to
address functional limitations and ability to fulfill life
roles.
46
Future research, in addition to attempting to
answer continuing questions about the effectiveness of
various techniques for increasing PROM measurements,
needs to address questions about relationships between
joint PROM and functional capabilities. Even if a tech-
nique is shown to increase PROM, we need to know
whether the increase affects the ability of an adult with
cerebral palsy to function or makes an important differ-
ence in the ease of caregiving.
References
1
Murphy KP, Molnar GE, Lankasky K. Medical and functional status of
adults with cerebral palsy. Dev Med Child Neurol. 1995;37:1075–1084.
2
Thomas CL, ed. Taber’s Cyclopedic Medical Dictionary. 18th ed. Phila-
delphia, Pa: FA Davis Co; 1997.
3
Tardieu C, Huet de la Tour E, Bret MD, Tardieu G. Muscle
hypoextensibility in children with cerebral palsy, I: clinical and exper-
imental observations. Arch Phys Med Rehabil. 1982;63:97–102.
4
Tardieu G, Tardieu C, Colbeau-Justin P, Lespargot A. Muscle hypo-
extensibility in children with cerebral palsy, II: therapeutic implica-
tions. Arch Phys Med Rehabil. 1982;63:103–107.
5
Tardieu C, Lespargot A, Tabary C, Bret MD. For how long must the
soleus muscle be stretched each day to prevent contracture? Dev Med
Child Neurol. 1988;30:3–10.
6
Cherry DB. Review of physical therapy alternatives for reducing
muscle contracture. Phys Ther. 1980;60:877– 881.
7
McPherson JJ, Arends TG, Michaels MJ, Trettin K. The range of
motion of long term knee contractures of four spastic cerebral palsied
children: a pilot study. Physical and Occupational Therapy in Pediatrics.
1984;4(1):17–34.
8
Tardieu G, Tardieu C. Cerebral palsy: mechanical evaluation and
conservative correction of limb joint contractures. Clin Orthop. 1987;
219:63– 69.
9
Fulford FE, Brown JK. Position as a cause of deformity in children
with cerebral palsy. Dev Med Child Neurol. 1976;18:305–314.
10
Holt S, Baagoe S, Lillelund F, Magnusson SP. Passive resistance of
the hamstring muscles in children with severe multiple disabilities? Dev
Med Child Neurol. 2000;42:541–544.
11
Olney SJ, Wright MJ. Cerebral palsy. In: Campbell SK, Vander
Linden DW, Palisano RJ, eds. Physical Therapy for Children. 2nd ed.
Philadelphia, Pa: WB Saunders Co; 2000:533–570.
12
Brouwer B, Davidson LK, Olney SJ. Serial casting in idiopathic
toe-walkers and children with spastic cerebral palsy. J Pediatr Orthop.
2000;20:221–225.
13
Anderson JP, Snow B, Dorey FJ, Kabo JM. Efficacy of soft splints in
reducing severe knee flexion contractures. Dev Med Child Neurol.
1988;30:502–508.
14
Hainsworth F, Harrison MJ, Sheldon TA, Roussounis SH. A prelim-
inary evaluation of ankle orthoses in the management of children with
cerebral palsy. Dev Med Child Neurol. 1997;39:243–247.
15
Stuberg WA. Considerations related to weight-bearing programs in
children with developmental disabilities. Phys Ther. 1992;72:35– 40.
16
Lespargot A, Renaudin E, Khouri N, Robert M. Extensibility of hip
adductors in children with cerebral palsy. Dev Med Child Neurol.
1994;36:980 –988.
17
Carson SJ, Ramsey C. Assistive technology. In: Campbell SK, Vander
Linden DW, Palisano, RJ, eds. Physical Therapy for Children. 2nd ed.
Philadelphia, Pa: WB Saunders Co; 2000:671–708.
18
Bleck EE. Orthopedic Management of Cerebral Palsy. Philadelphia, Pa:
WB Saunders Co; 1979.
19
Miedaner JA, Renander J. The effectiveness of classroom passive
stretching programs for increasing or maintaining passive range of
motion in non ambulatory children: an evaluation of frequency.
Physical and Occupational Therapy in Pediatrics. 1987;7(3):35– 43.
20
Patrick PD, Mozzoni M, Patrick ST. Evidence-based care and the
single-subject design. Inf Young Children. 2000;13(1):60 –73.
21
Abel MF, Blanco JS, Pavlovich L, Damiano DL. Asymmetric hip
deformity and subluxation in cerebral palsy: an analysis of surgical
treatment. J Pediatr Orthop. 1999;19:479 – 485.
22
Portney LG, Watkins MP. Foundations of Clinical Research: Applications
to Practice. 2nd ed. Upper Saddle River, NJ: Prentice Hall; 2000.
23
Wright T, Nicholson J. Physiotherapy for the spastic child: an
evaluation. Dev Med Child Neurol. 1973;15:146 –163.
24
Bezner J. Adult Exercise Instruction Sheets: Home Exercise for Rehabilita-
tion. Tucson, Ariz; Therapy Skill Builders; 1989.
25
Kisner C, Colby LA. Therapeutic Exercise: Foundations and Techniques.
Philadelphia, Pa: FA Davis Co; 1985.
26
Bandy SD, Irion JM. The effect of time on static stretch on the
flexibility of the hamstring muscles. Phys Ther. 1994;74:845– 852.
27
Bandy SD, Irion JM, Briggler M. The effect of time and frequency of
static stretching on flexibility of the hamstring muscles. Phys Ther.
1997;77:1090 –1096.
28
Ashton BB, Pickles B, Roll JW. Reliability of goniometric measure-
ments of hip motion in spastic cerebral palsy. Dev Med Child Neurol.
1978;20:87–94.
29
Stuberg WA, Fuchs RH, Miedaner J. Reliability of goniometric
measurements of children with cerebral palsy. Dev Med Child Neurol.
1988;30:657– 666.
30
Miller PJ. Assessment of joint motion. In: Rothstein JM, ed. Mea-
surement in Physical Therapy. New York, NY: Churchill Livingstone Inc;
1985:103–135.
668 . Cadenhead et al
Physical Therapy . Volume 82 . Number 7 . July 2002

31
Gajodsik RL, Bohannon RW. Clinical measurement of range of
motion: review of goniometry emphasizing reliability and validity. Phys
Ther. 1987;67:1867–1872.
32
Levitt S. Treatment of Cerebral Palsy and Motor Delay. Oxford, England:
Blackwell Scientific Publications; 1977.
33
Bartlett MD, Wolf LS. Hip flexion contractures: a comparison of
measurement methods. Arch Phys Med Rehabil. 1985;66:620 – 625.
34
Mollinger LA, Steffen TM. Knee flexion contractures in institution-
alized elderly: prevalence, severity, stability, and related variables. Phys
Ther. 1993;73:437– 444.
35
Shrout PR, Fleiss JL. Intraclass correlations: uses in assessing rater
reliability. Psychol Bull. 1979;86:420 – 428.
36
Wolery M, Harris SR. Interpreting results of single subject research
designs. Phys Ther. 1982;62:445– 452.
37
Hojem MA, Ottenbacher KJ. Empirical investigation of visual-
inspection versus trend-line analysis of single subject data. Phys Ther.
1988;68:983–988.
38
Ottenbacher KJ. Visual inspection of single-subject data: an empir-
ical analysis. Mental Retardation. 1990;28:283–290.
39
Harbst KB, Ottenbacher KJ, Harris SR. Interrater reliability of
therapists’ judgments of graphed data. Phys Ther. 1991;71:107–115.
40
Tryon WW. A simplified time-series analysis for evaluating treat-
ment interventions. J Appl Behav Anal. 1982;15:423– 429.
41
Blumberg CJ. Comments on “A simplified time-series analysis for
evaluating treatment interventions.” J Appl Behav Anal. 1984;17:
539 –542.
42
Nourbakhsh MR, Ottenbacher KJ. The statistical analysis of single-
subject data: a comparison examination. Phys Ther. 1994;74:768 –776.
43
Harris SR, Smith LH, Krukowski L. Goniometric reliability for a
child with spastic quadriplegia. J Pediatr Orthop. 1985;5:348 –351.
44
Staheli LT. Fundamentals of Pediatric Orthopedics. New York, NY:
Raven Press; 1992.
45
Wolf MM. Social validity: the case for subjective measurement or
how applied behavior analysis is finding its heart. Journal of Applied
Behavior Analysis. 1978:203–214.
46
Campbell SK. Therapy programs for children that last a lifetime.
Physical and Occupational Therapy in Pediatrics. 1997;17:1–15.
Physical Therapy . Volume 82 . Number 7 . July 2002
Cadenhead et al . 669
ўўўўўўўўўўўўўўўўўўўўўўўў
ў
Wyszukiwarka
Podobne podstrony:
Effects of a Group Exercise Program on Strength,
46 Effects of Exercise on Brain and Body
TRANSIENT HYPOFRONTALITY AS A MECHANISM FOR THE PSYCHOLOGICAL EFFECTS OF EXERCISE
Effect of long chain branching Nieznany
Effect of Kinesio taping on muscle strength in athletes
53 755 765 Effect of Microstructural Homogenity on Mechanical and Thermal Fatique
Effect of File Sharing on Record Sales March2004
31 411 423 Effect of EAF and ESR Technologies on the Yield of Alloying Elements
21 269 287 Effect of Niobium and Vanadium as an Alloying Elements in Tool Steels
(10)Bactericidal Effect of Silver Nanoparticles
Effect of?renaline on survival in out of hospital?rdiac arrest
Effects of the Great?pression on the U S and the World
4 effects of honed cylinder art Nieznany
Effects of the Atomic Bombs Dropped on Japan
Effect of aqueous extract
Effect of Active Muscle Forces Nieznany
Effects of Kinesio Tape to Reduce Hand Edema in Acute Stroke
1 Effect of Self Weight on a Cantilever Beam
effect of varying doses of caffeine on life span D melanogaster
więcej podobnych podstron