Pain following stroke, initially and at 3 and 18 months after
stroke, and its association with other disabilities
D. K. Sommerfeld
a,b
and A.-K. Welmer
c
a
Department of Geriatric Medicine, Danderyd Hospital, Danderyd;
b
Division of Physiotherapy, Department of Neurobiology, Care
Sciences and Society, Karolinska Institutet, Stockholm; and
c
Department of Neurobiology, Care Sciences and Society, Aging Research
Center (ARC), Karolinska Institutet and Stockholm University, Karolinska University Hospital, Stockholm, Sweden
Keywords:
associations, disability,
pain, prevalence,
prognoses, stroke
Received 9 October 2011
Accepted 27 March 2012
Background and purpose: A general hypothesis is that pain following stroke (PFS)
causes disabilities. However, the clinical implication of PFS on other disabilities
after stroke and vice versa has not been fully investigated. The aims of this observa-
tional study were to analyze the correlation between PFS and other disabilities at
different time points after stroke, whether PFS can be a predictor of coming disabil-
ities and whether other disabilities can be predictors of coming PFS.
Methods: Patients with a first-ever stroke were assessed initially (n
= 109), and at 3
(n
= 95) and 18 months (n = 66) after stroke for PFS, mobility, self-care as well as
touch, proprioceptive, muscle tone, and movement functions.
Results:
PFS was correlated to impaired upper extremity movement function on
all occasions, while the correlations between PFS and other disabilities varied across
the three occasions. Initial PFS and PFS at 3 months did not independently predict
coming disabilities. Initial mobility limitation independently predicted PFS at
3 months and impaired touch function, initially and at 3 months, independently
predicted PFS at 18 months. No other disabilities independently predicted coming
PFS.
Conclusions: The present results do not support the hypothesis that PFS causes
other disabilities. Our results indicate that PFS is correlated to other disabilities;
however, no ultimate conclusions can be drawn on causality. PFS was not a predic-
tor of coming disabilities, while some disabilities were predictors of coming PFS.
Introduction
Pain following stroke (PFS), whether central or
peripheral, is reported to cause major problems
for the patients affected [1]. It is considered a
common impairment after stroke although there is
a great variance in reported prevalence 19
–74%
[1]. Differences in, for example, study populations,
time since stroke onset, site of assessment, and
measurements may contribute to this variance.
PFS is also considered to be associated with long-
term mortality [2]. The relationship between PFS
and other disabilities, that is, the clinical impact
of PFS on other disabilities and vice versa after
stroke has not been fully investigated. Whether
PFS causes other disabilities or whether other
disabilities cause PFS may have implications for
the treatment offered.
The aims of this preliminary observational study
were to analyze the relationship between PFS and
other disabilities and to analyze whether initial PFS
can predict other disabilities at 3 and 18 months after
stroke, whether PFS at 3 months can predict other
disabilities at 18 months after stroke, whether other
initial disabilities can predict PFS at 3 and 18 months
after
stroke,
and
whether
other
disabilities
at
3 months can predict PFS at 18 months after stroke.
Subjects and methods
The study was approved by the Regional Ethical
Review Board in Stockholm. Informed consent was
obtained from all patients or their significant others.
Patients were consecutively recruited from the
stroke unit of Danderyd Hospital in Stockholm,
Sweden. Patients ultimately enrolled in the study were
Correspondence: D. K. Sommerfeld, Department of Geriatric Medi-
cine, S-182 87 Danderyd, Sweden (tel.: +4676 234 62 13; fax: +4686
226 154; e-mail: disa.sommerfeld@sll.se).
© 2012 The Author(s)
European Journal of Neurology
© 2012 EFNS
1325
European Journal of Neurology 2012, 19: 1325–1330
doi:10.1111/j.1468-1331.2012.03747.x

those who lived in Stockholm and who presented with
an acute, first-ever stroke (subarachnoid hemorrhage
and cerebellar lesions excluded); in whom other diag-
noses affecting muscle tone were absent, and who
were conscious and agreed to participate in the study.
Initially, 109 patients
– 67 women and 42 men – med-
ian age 79 years (inter quartile range [IQR] 73
–84),
were enrolled in the study. Ninety-five patients
– 60
women and 35 men, median age 80 years (IQR 73
–85)
– were still enrolled in the study at 3 months, and 66
patients
– 44 women and 22 men, median age
78.5 years (IQR 72
–83) – at 18 months. The present
study is a complement to a previous study [3] that
was originally designed to describe the prevalence of
spasticity after stroke [3, 4] and a full description of
the inclusion procedure has been presented previously
[4]. The present study mainly focuses on the patients
with PFS.
The patients were assessed initially and at 3 and
18 months after acute stroke, with regard to the
parameters described below. All tests were performed
either in the hospital/institution or in the patient’s
home by four purpose-trained physiotherapists.
Pain was assessed through a structured interview
and by asking the patients whether they perceived any
pain. The pain was adjudged to be stroke-related
(PFS) if it occurred after the stroke as, for example,
pain on the affected side and headache. The pain was
adjudged to be not stroke related if it occurred before
the stroke, in the form of rheumatoid arthritis, arthro-
sis and migraine but had another obvious cause rather
than stroke, for example, fracture and wound and
pain on the non-affected side, if it occurred after the
stroke. When the cause was not obvious, the pain was
adjudged to be stroke related.
Touch function was determined by testing the
patient’s ability to perceive light touch (cotton wool)
on the upper arm, forearm, hand, thigh, calf and dor-
sal foot with their eyes closed. If the patient was
unable to perceive light touch in one location or
more, the test result was defined as impaired touch
function for the upper or the lower extremity. The test
is frequently used and is considered to be of satisfac-
tory reliability for stroke patients [5].
Proprioceptive function, that is, sensing the relative
position of body parts, was tested with the Thumb
localizing test [6]. The arm on the affected side is posi-
tioned passively and the patient is asked to pinch its
thumb with the opposite thumb and index finger; this
is repeated four times. Proprioceptive function is con-
sidered normal if the patient is able to locate the
thumb on the affected side with their eyes closed in
three of four tests. The test is considered valid [6] for
stroke patients but has not been tested for reliability.
Muscle tone function
– spasticity – was assessed by
the Modified Ashworth Scale (MAS) [7]. Possible scores
on the MAS are 0 (normal or lowered muscle tone), 1, 1
+, 2, 3 and 4 (passive movements are not possible). The
MAS is considered fairly reliable [8] and is regarded as
one of the best clinical measures of spasticity [9]. The
muscle groups evaluated were the following: arm adduc-
tors, elbow flexors and extensors, wrist flexors and ex-
tensors, and finger flexors (tested in the sitting position,
if possible), and hip adductors, knee flexors and exten-
sors, and plantar-flexors (tested in the supine position).
Severe spasticity was defined as the upper quartile of the
highest MAS score at 3 months post-stroke in any mus-
cle group, or inexhaustible plantar-flexor clonus.
Control
of
voluntary
movement
function
was
assessed using part 1 of the 7-part Lindmark Motor
Assessment Scale (LMAS) [10] (upper extremity move-
ments, 0
–57 points and lower extremity movements, 0
–36 points; the higher the score, the better). The
LMAS is considered valid [11] and reliable [12] for
stroke patients.
Mobility was assessed with the Rivermead Mobility
Index (RMI) [13] (possible range 0
–15 points). The
RMI is considered valid [14], reliable [15], and sensi-
tive to change [14, 16] for stroke patients.
Self-care, that is, activities of daily living (ADL),
was assessed using the Barthel Index (BI) [17] (possi-
ble range 0
–100 points). The BI is widely used and is
considered valid, reliable, and sensitive to change for
stroke patients [17, 18].
Statistical analysis
Descriptive analyses were used to present the numbers
of patients with PFS and non-stroke-related pain as
well as the location of PFS at each assessment. Spear-
man’s rank correlation was used for the cross-sectional
relationship between PFS and initial functioning scores
at 3 and 18 months after stroke. Logistic regression
analyses were conducted to estimate the associations
between initial functioning scores after stroke as inde-
pendent variables and PFS at 3 and 18 months after
stroke, respectively, as dependent variables and func-
tioning scores 3 months after stroke as independent
variables and PFS at 18 months after stroke as depen-
dent variable. Logistic regression analyses were also
conducted to estimate the associations between initial
PFS as the independent variable and functioning scores
at 3 and 18 months after stroke, respectively, as depen-
dent variables; and PFS at 3 months as the indepen-
dent variable, and functioning scores at 18 months
after stroke as dependent variables. Owing to the low
number of patients in the study, scores for the upper
and lower extremities, respectively, in PFS, muscle
© 2012 The Author(s)
European Journal of Neurology
© 2012 EFNS European Journal of Neurology
1326
D. K. Sommerfeld and A.-K. Welmer
tone, touch, and proprioceptive functions were merged
for the regression analyses. Scores for the upper and
lower extremities were significantly correlated for all
variables (Spearman’s rho
>0.5, P < 0.001). Ordinal
scales were dichotomized according to known criteria,
when available, or according to the lower quartile of all
patients. The analyses were adjusted for age, gender,
and each of the other functioning/disability variables.
Data were analyzed using STATISTICA 7.0 for Win-
dows
(StatSoft
Scandinavia
AB,
Klostergatan,
Uppsala, Sweden).
Results
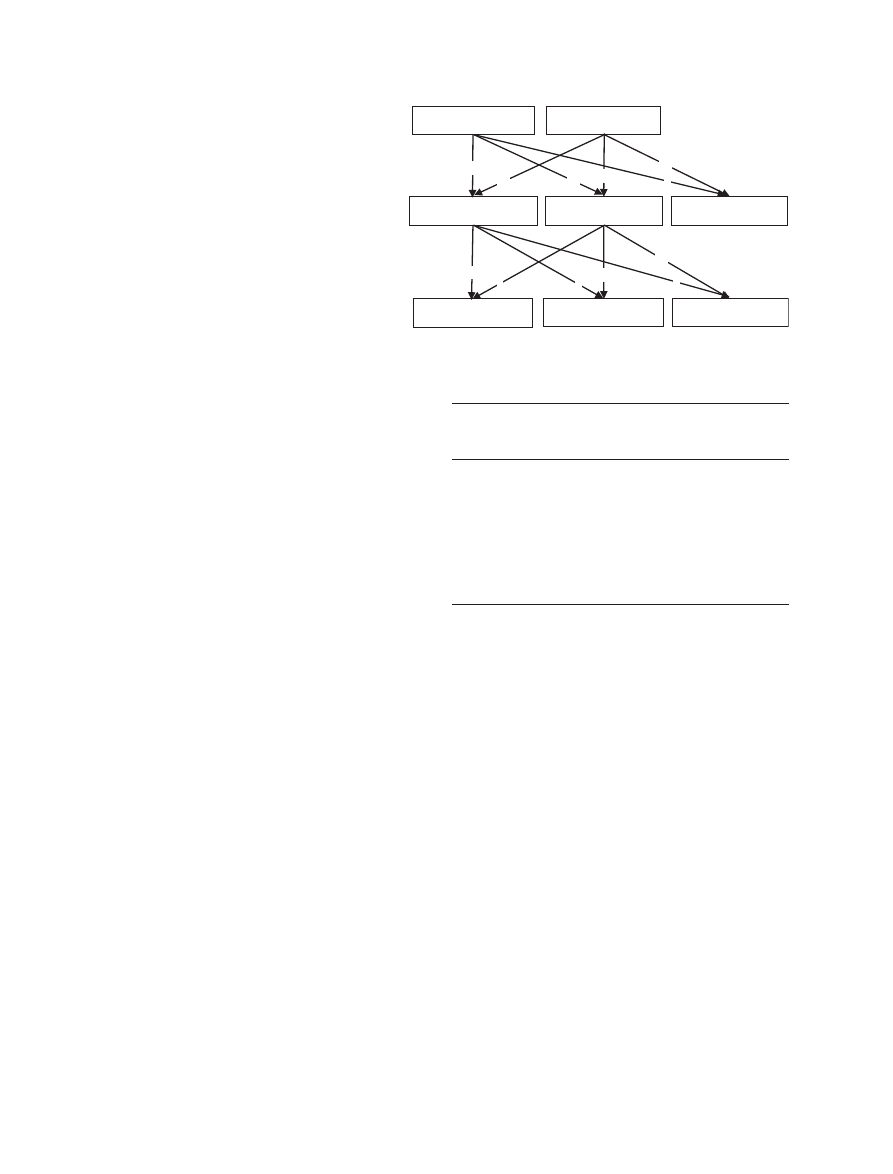
Initially after stroke, eight men and 10 women (17%)
of 109 patients had PFS; at 3 months, 10 men and 10
women (21%) of 95 patients had PFS; and at
18 months, five men and six women (17%) of 66
patients had PFS (Fig. 1). On all occasions, the PFS
in the upper and lower extremities that was most com-
monly described was unspecified pain in the arm or
leg (Table 1).
Non-stroke-related pain was present in: six men and
13 women (17%) of 109 patients initially; one man and
16 women (18%) of 95 patients at 3 months; five men
and 18 women (35%) of 66 patients at 18 months. The
occurrence of pain, both stroke-related and non-stroke-
related pain, was initially 37 (34%), 37 (39%) at
3 months and 34 (52%) at 18 months.
The majority of patients with any spasticity had PFS.
All patients with severe spasticity initially (n
= 1) and
at 3 months (n
= 5) had PFS, while six of 10 patients
with severe spasticity at 18 months had PFS.
Age was significantly correlated with PFS at 3 and
18 months, while gender was not correlated with PFS
on any occasion. Impaired upper extremity movement
function was significantly correlated with PFS on all
occasions, while the significance of the correlations
between PFS and other disabilities varied across the
three occasions (Table 2).
Results from the logistic regression models showed
that initial worse mobility score was significantly asso-
ciated with PFS at 3 months (P
< 0.05), and initially
impaired touch function was significantly associated
with PFS at 18 months (P
< 0.05). Impaired touch
function at 3 months was also significantly associated
with PFS at 18 months (P
< 0.05). No other disabili-
ties
were
significantly
associated
with
PFS
at
3 months, when the findings were adjusted for demo-
graphics and initial mobility score, or with PFS at
18 months when the findings were adjusted for demo-
graphics and initial touch function. Initial PFS was
not significantly associated with any disabilities at 3
and 18 months, when the findings were adjusted for
age and gender. PFS at 3 months was not significantly
associated with functioning at 18 months when adjust-
ment was made for age, gender, and functioning.
Discussion
This preliminary observational study describes the
relationship
between
PFS
and
other
disabilities
(impaired touch, proprioceptive, muscle tone, and
movement functions; mobility and self-care limitations)
Patients without PFS
n = 91
Patients with PFS
n = 18
Patients without PFS
n = 75
Patients with PFS
n = 20
Not followed up
n = 14
Patients without PFS
n = 55
Patients with PFS
n = 11
Not followed up
n = 29
Initially after
stroke n = 109
3 months after
stroke n = 95
18 months after
stroke n = 66
11
1
13
14
9
6
6
23
6
64
5
46
Figure 1 Number of patients with pain
following stroke (PFS) as well as those
patients in which PFS persisted,
appeared or disappeared at respective
assessment point.
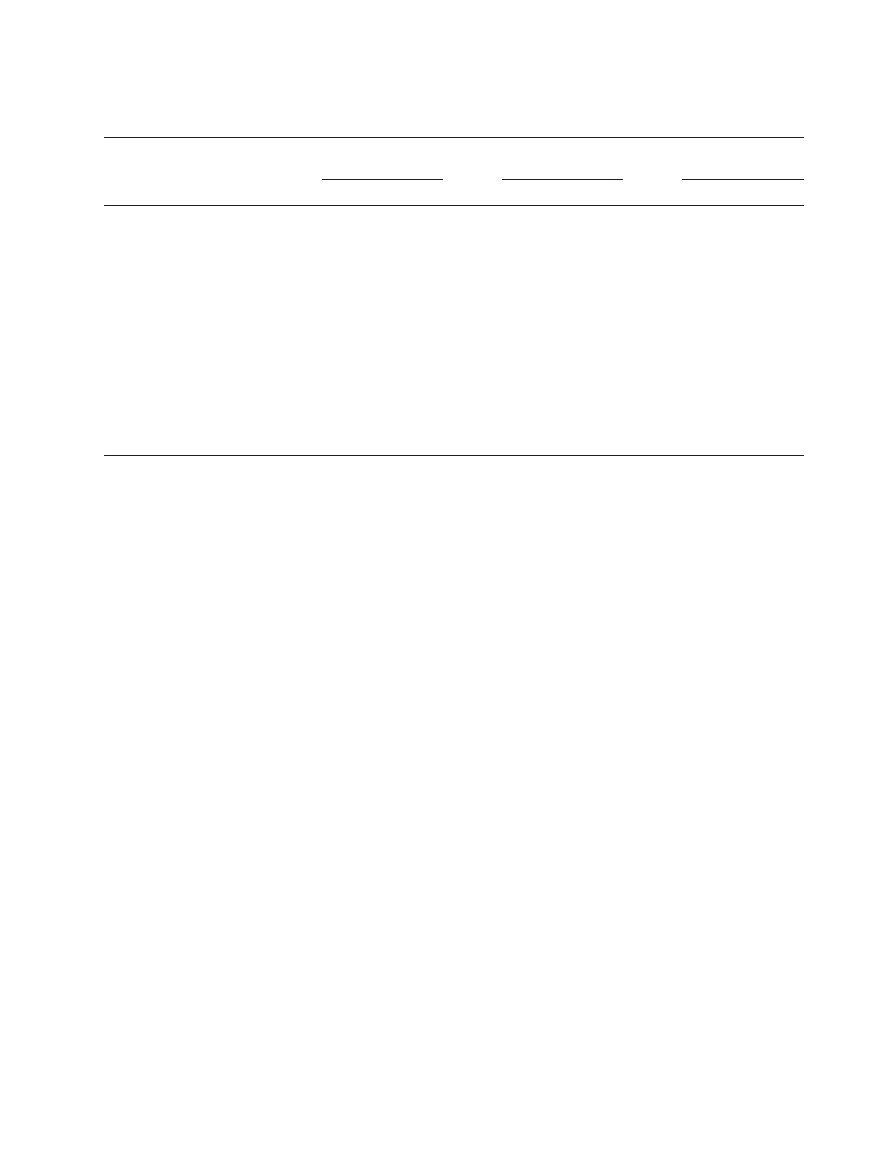
Table 1 Location of pain following stroke (PFS) as well as the
number of patients and percentage of all patients with PFS in each
location, initially and at 3 and 18 months after stroke
Initially
n
= 109 (%)
3 months
after stroke
n
= 95 (%)
18 months
after stroke
n
= 66 (%)
Face/head/neck/back
4 (4)
4 (4)
2 (3)
Upper extremity
Shoulder/chest
4 (4)
3 (3)
1 (2)
Arm (unspecified)
7 (6)
11 (12)
5 (8)
Wrist/hand
3 (3)
1 (1)
2 (3)
Lower extremity
Hip/groin
0
1 (1)
2 (3)
Leg (unspecified)
3 (3)
8 (8)
6 (9)
Foot/ankle
3 (3)
1 (1)
1 (2)
© 2012 The Author(s)
European Journal of Neurology
© 2012 EFNS European Journal of Neurology
Pain following stroke
1327
and the association between PFS and other disabilities
initially and at 3 and 18 months after stroke. Our
results indicate that initial mobility limitation indepen-
dently predicts PFS at 3 months and that impaired
touch function, initially and at 3 months, indepen-
dently predicts PFS at 18 months, while PFS does not
seem to predict disabilities on any occasion.
The occurrence of PFS was some 20%, which is in
accordance with other investigators [19] reporting PFS
in 21% of the patients 1-year-post-first-ever stroke.
PFS in the present study was most common in the
upper extremity, which is in accordance with previous
reports [19, 20]. However, in the present study, the
most commonly described PFS in the arm was
unspecified pain, which was not in accordance with
the other findings [19, 20] that report shoulder pain as
being the most common upper extremity pain.
Although the occurrence of PFS was more or less
constant over time, the occurrence of any pain, that is,
both
stroke-related
and
non-stroke-related
pain,
increased over time indicating that pain may be a related
disability caused by, for example, asymmetries, inactiv-
ity or an increased burden on the non-affected side. Our
findings are supported by some investigators [21] but
not others [20] who report decrease in non-stroke-spe-
cific pain from 40% at 4 months to 25% at 16 months
after stroke. However, in the latter study [20], only
patients still alive 16 months after stroke and only those
who were able to use the VAS are considered.
Patients with PFS were significantly younger if
compared to those without PFS at 3 and 18 months,
which has been reported earlier [2, 20]. Furthermore,
on all occasions, PFS was related to some of the other
disabilities assessed, although no conclusions can be
drawn as to the causalities.
Fifty percent of those with PFS had some spasticity.
The majority of patients with severe spasticity had
PFS, while only a small percentage of the patients with
PFS had severe spasticity. Although spasticity was sig-
nificantly correlated with PFS at 3 and 18 months,
spasticity was not independently associated with PFS
as shown by the logistic regression analyses. Our find-
ings are in accordance with others’ [19] and suggest
that further factors, such as movement limitations and
impaired sensory functions, are more important pre-
dictors of PFS if compared with spasticity. However,
it should be noted that when examining the associa-
tion between spasticity and PFS, we included patients
with any kind of spasticity, that is, both patients with
light spasticity and patients with severe spasticity. It is
possible that the association between spasticity and
PFS would have been stronger if we had analyzed the
association between severe spasticity and PFS. More-
over, the correlation between spasticity and PFS
decreased slightly between 3 and 18 months. Owing to
our small sample, these data can only be seen as preli-
minary, and more research is needed to further eluci-
date the relationships between spasticity and PFS.
Our results showing initial mobility limitations as
predicting PFS at 3 months and impaired touch func-
tion, initially and at 3 months, as predicting PFS at
18 months are partly consistent with other studies that
report stroke severity, initially impaired movement and
sensory function as predicting PFS at 6
–12 months
Table 2 The correlation (rho) between pain following stroke (PFS) and; age, gender, affected side and the other functioning/disabilities initially
and at 3 and 18 months after stroke
PFS initially after stroke
(n
= 109)
PFS 3 months after
stroke (n
= 95)
PFS 18 months after
stroke (n
= 66)
rho
P
rho
P
rho
P
Age at stroke onset
0.013
0.894
0.296
0.004
0.244
0.049
Gender (men/women)
0.054
0.577
0.141
0.173
0.115
0.358
Affected side
0.163
0.209
0.152
0.155
0.163
0.209
Activity tests
Rivermead Mobility Index
0.210
0.029
0.340
<0.001
0.134
0.285
Barthel Index
0.186
0.053
0.304
0.003
0.141
0.258
Upper extremity body function
Movement (LMAS)
0.298
0.006
0.529
<0.001
0.349
0.004
Muscle tone (MAS)
0.009
0.930
0.584
<0.001
0.421
<0.001
Light touch [normal/impaired]
0.088
0.389
0.477
<0.001
0.343
0.006
Proprioception
[normal/impaired]
0.342
<0.001
0.396
<0.001
0.151
0.245
Lower extremity body function
Movement (LMAS)
0.109
0.325
0.177
0.091
0.222
0.073
Muscle tone (MAS)
0.380
<0.001
0.116
0.264
0.361
0.003
Light touch [normal/impaired]
0.121
0.907
0.190
0.077
0.422
<0.001
LMAS, Lindmark motor assessment scale; MAS, Modifies Ashworth Scale. Bold values indicate P values < 0.05.
© 2012 The Author(s)
European Journal of Neurology
© 2012 EFNS European Journal of Neurology
1328
D. K. Sommerfeld and A.-K. Welmer

after stroke [2, 19, 22]. However, although impaired
sensory function is considered a significant predictor of
PFS, according to the present study, most patients with
initially impaired touch function will not suffer from
PFS. However, using pinprick instead of light touch
might have given a different result.
While some disabilities could be predictors of PFS,
PFS could not be a predictor of coming disabilities.
These results do not support the hypothesis that PFS
causes disabilities after stroke, but rather that other
disabilities may cause PFS.
At 18 months, only 66 patients remained to be fol-
lowed up, thus limiting the possibility of generalizing
from these results. The smallness of the sample may
also have increased the risk of Type 2 errors. Thus,
the non-significant values have to be interpreted with
caution. Another limitation is that non-stroke-related
pain on the affected side might have been considered
as PFS and thus the prevalence of PFS may have
been overestimated. Moreover, we were not able to
classify pain according to central or peripheral origin.
The estimated relationship between PFS and the other
disabilities
may have
been biased
by the
high
frequency of non-stroke-related pain.
To summarize, several disabilities were related to
PFS on all occasions. However, as to causality, no
ultimate conclusions can be drawn. Initial mobility
limitation was a predictor of PFS at 3 months and
impaired touch function, initially and at 3 months,
predicted PFS at 18 months after stroke. PFS, initially
and at 3 months, did not predict other disabilities at
18 months. Our results indicate that other disabilities
cause PFS to a larger extent than PFS causes disabili-
ties; this may have implications for the treatment of
PFS. However, our results need to be supported by a
larger and more detailed study on pain following
stroke.
Acknowledgements
The study was supported with grants from the PickUp
funding at the Stockholm County Council. We thank
the physiotherapists Elsy Eek and Helena Vesterlin
for assessing the patients.
Disclosure of conflict of interest
The authors declare no financial or other conflict of
interests.
References
1. Kim JS. Post-stroke pain. Expert Rev Neurother 2009; 9:
711
–721.
2. Naess H, Lunde L, Brogger J, Waje-Andreasses U.
Post-stroke pain on long-term follow-up: the Bergen
stroke study. J Neurol 2010; 257: 1446
–1452.
3. Sommerfeld DK, Eek E, Svensson A-K, Wide´n
Holmqvist
L,
von
Arbin
MH.
Spasticity
after
stroke, its occurence and association with motor
impairments and activity limitations. Stroke 2004;
35: 134
–140.
4. Welmer AK, von Arbin M, Wide´n Holmqvist L,
Sommerfeld DK. Spasticity and its association with
functioning
and
health-related
quality
of
life
18 months after stroke. Cerebrovasc Dis 2006; 21:
247
–253.
5. Wade DT. Measurement in Neurological Rehabilitation.
Oxford, UK: Oxford medical publications, 1992.
6. Hirayama K, Fukutake T, Kawamura M. ‘Thumb
localizing test’ for detecting a lesion in the posterior
column-medial lemniscal system. J Neurol Sci 1999; 167:
45
–49.
7. Bohannon RW, Smith MB. Interrater reliability of a
modified Ashworth scale of muscle spasticity. Phys Ther
1987; 67: 206
–207.
8. Gregson JM, Leathley MJ, Moore AP, Smith TL, Shar-
ma AK, Watkins CL. Reliability of measurements of
muscle tone and muscle power in stroke patients. Age
Ageing
2000; 29: 223
–228.
9. Pandyan AD, Johnson GR, Price CI, Curless RH,
Barnes MP, Rodgers H. A review of the properties and
limitations of the Ashworth and modified Ashworth
Scales as measures of spasticity. Clin Rehabil 1999; 13:
373
–383.
10. Lindmark B. Evaluation of functional capacity after
stroke with special emphasis on motor function and
activities of daily living. Scand J Rehabil Med Suppl
1988; 21(Suppl): 1
–40.
11. Lindmark B, Hamrin E. Evaluation of functional capac-
ity after stroke as basis for active intervention. Valida-
tion of a modified chart for motor capacity assessment.
Scand J Rehabil Med
1988; 20: 111
–115.
12. Lindmark B, Hamrin E. Evaluation of functional
capacity after stroke as a basis for active intervention.
Presentation of a modified chart for motor capacity
assessment and its reliability. Scand J Rehabil Med
1988; 20: 103
–109.
13. Collen FM, Wade DT, Robb GF, Bradshaw CM. The
rivermead mobility index: a further development of the
rivermead motor assessment. Int Disabil Stud 1991; 13:
50
–54.
14. Hsieh CL, Hsueh IP, Mao HF. Validity and responsive-
ness of the rivermead mobility index in stroke patients.
Scand J Rehabil Med
2000; 32: 140
–142.
15. Chen HM, Hsieh CL, Sing Kai L, Liaw LJ, Chen
SM, Lin JH. The test-retest reliability of 2 mobility
performance tests in patients with chronic stroke.
Neurorehabil Neural Repair
2007; 21: 347
–352.
16. Sommerfeld DK, Welmer A-K, Wide´n Holmqvist L,
von Arbin M. Changes in functioning between days 5
and 10 after stroke in elderly. Phys Occup Ther Geriatr
2011; 29: 77
–89.
17. Mahoney FI, Barthel DW. Functional evaluation: the
Barthel Index. Md State Med J 1965; 14: 61
–65.
18. Collin C, Wade DT, Davies S, Horne V. The Barthel
ADL index: a reliability study. Int Disabil Stud 1988; 10:
61
–63.
© 2012 The Author(s)
European Journal of Neurology
© 2012 EFNS European Journal of Neurology
Pain following stroke
1329
19. Lundstro¨m E, Smits A, Tere´nt A, Borg J. Risk factors
for stroke-related pain 1 year after first-ever stroke. Eur
J Neurol
2009; 16: 188
–193.
20. Jo¨nsson AC, Lindgren I, Hallstro¨m B, Norrving B,
Lindgren A. Prevalence and intensity of pain after
stroke: a population based study focusing on patients’
perspectives. J Neurol Neurosurg Psychiatry 2006; 77:
590
–595.
21. Langhorne P, Stott DJ, Robertson L, et al.Medical
complications after stroke: a multicenter study. Stroke
2000; 31: 1223
–1229.
22. Appelros P. Prevalence and predictors of pain and fati-
gue after stroke: a population-based study. Int J Rehabil
Res
2006; 29: 329
–333.
© 2012 The Author(s)
European Journal of Neurology
© 2012 EFNS European Journal of Neurology
1330
D. K. Sommerfeld and A.-K. Welmer
Copyright of European Journal of Neurology is the property of Wiley-Blackwell and its content may not be
copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written
permission. However, users may print, download, or email articles for individual use.
Wyszukiwarka
Podobne podstrony:
Pain following stroke A prospective study
Pain Following Stroke A Population Based Follow Up Study
Lumiste Betweenness plane geometry and its relationship with convex linear and projective plane geo
Colin Nettelbeck French Cinema and its relations with literature from Vichy towards the New Wave
0 0 0 1 Lab Initializing and Reloading a Router and Switch
Tommy Westlund Initiation and Death
Building Autonomous Line Followers using Arduino and PID
Petasites kablikianus Tausch ex Berchtold as a pioneer species and its abilities to colonise initial
Magnetic Treatment of Water and its application to agriculture
Analysis of soil fertility and its anomalies using an objective model
Changes in passive ankle stiffness and its effects on gait function in
Extract from Armoracia rusticana and Its Flavonoid Components
[38]QUERCETIN AND ITS DERIVATIVES CHEMICAL STRUCTURE AND BIOACTIVITY – A REVIEW
Angielski tematy Performance appraisal and its role in business 1
conceptual storage in bilinguals and its?fects on creativi
więcej podobnych podstron