clinical immuno final1 02
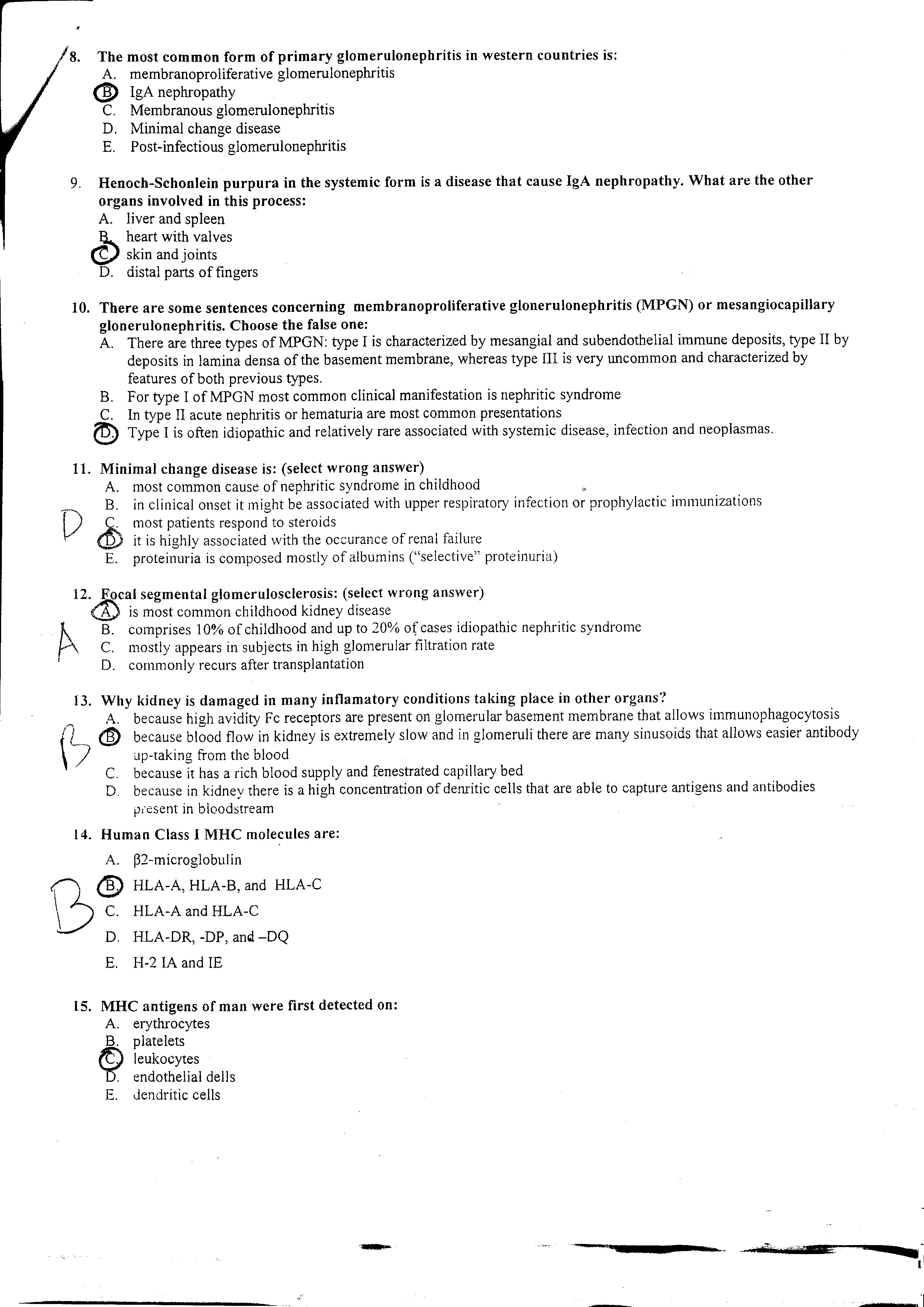
/8. The most common form of primary glomerulonephritis in western countries is:
A. membranoprołiferative glomerulonephritis d> IgA nephropathy
C. Membranous glomerulonephritis
D. Minimal change disease
E. Post-infectious glomerulonephritis
9. Henoch-Schonlein purpura in the systemie form is a disease that cause IgA nephropathy. What are the other organs involved in this process:
A. liver and spleen ĘL heart with valves (2P skin and joints D. distal parts of fmgers
10. There are some sentences concerning membranoproliferative glonerulonephritis (MPGN) or mesangiocapillary glonerulonephritis. Choose the false one:
A. There are three types of MPGN: type I is characterized by mesangial and subendothelial immune deposits, type II by deposits in lamina densa of the basement membranę, whereas type III is very uncommon and characterized by features of both previous types.
B. For type I of MPGN most common clinical manifestation is nephritic syndrome
C. In type II acute nephritis or hematuria are most common presentations
© Type I is often idiopathic and relatively rare associated with systemie disease, infection and neoplasmas.
11. Minimal change disease is: (select wrong answer)
A. most common cause of nephritic syndrome in childhood
B. mc ) C. mo: ^ <£> itis
B. in clinical onset it might be associated with upper respiratory infection or prophylactic immunizations most patients respond to steroids
: is highiy associated with the occurance ofrenal failure E. proteinuria is composed mostly of albumins (“selective” proteinuria)
12
h
. Ęocal segmental glomerulosclerosis: (select wrong answer)
CAj is most common childhood kidney disease
B. comprises 10% of childhood and up to 20% of cases idiopathic nephritic syndrome
C. mostly appears in subjects in high glomerular filtration ratę
D. commonly recurs after transplantation
13. Why kidney is damaged in many inflamatory conditions taking place in other organs?
' i
A. because high avidity Fc receptors are present on glomerular basement membranę that allows immunophagocytosis d> because blood flow in kidney is extremely slow and in glomeruli there are many sinusoids that allows easier antibody up-taking from the blood
C. because it has a rich blood supply and fenestrated capillary bed
D. because in kidney there is a high concemration of denritic cells that are able to capture antigens and antibodies present in bloodstream
14.
Humań Ciass I MHC molecules are:
A. p2-microglobulin
HLA-A, HLA-B. and HLA-C
C.
D.
E.
HLA-A and HLA-C HLA-DR, -DP, and -DQ H-2 IA and IE
15. MHC antigens of man were first detected on:
B.
A. erythrocytes platelets leukocytes endothelial dells
E. dendritic cells
Wyszukiwarka
Podobne podstrony:
DSC09928 INFARCTS Local circulatory disturbances The most common form of cerebrovascular diseas
About Table Types The most common typc of table in an Oracle databasc is a relational table. which i
ESOPT State-of-the-art reportPenetration testing in IsraelA. Komornik The most common type of penetr
DSC09991 VIRAL ENCEPHAUTIS The most common cause of encephalitis Arbovirus encephalitis Herpes
There are many types of disorders affecting the blood. The most common disorder of the blood is anae
skanowanie0050 (9) disadvantages, and to work out the most effective way of their use in class, As.
clinical immuno final1 01 Clinical Immunology Finał Test 1. Which of the following diseases is organ
DSCN6628 Pneumocystosis is one of the most common infections in immunosuppressed patients with AIDS.
clinical immuno final1 04 25. Uendritic cells: (&} originate form bonę marrow B) &nb
3.Use Cases The following use cases relate to the most commonly used router configurations. The rela
The router s firmware offers presets for the most common DynDNS services plus an option to define in
some?sic preposition quiz 1 Marks: 12 You will need the most commonty used prepositbns here: in, on
UHAM066 THE CAUSES OF HEADACHE AND MIGRAINE ^ U9 Two of the most common headache-causing foods are c
91 (103) M. W. YroomFlea allergy dermatitis Flea allergy dermatitis (FAD) is the most common pruriti
Acetaminophen - poisoning o Frequency: o In the US: Acetaminophen is one of the most common pharmace
więcej podobnych podstron