7578409698
in 1981.4 A lotai of 381 cases have now been documented in Canada (Laboratory Centre for Disease Control 'ffeCDCJ, Department of National Health and Welfare, Ottawa: unpublished data).4'® Infections are reported throughout the year but occur morę frequently in the summer. Some re-ports have suggested an increased incidence ratę among peoplc who are immunocompromised,® but the findings have been inconclusive.
Except for the outbreak in Nova Scotia, which involved contaminated raw cabbage, food con-sumption has not been implicated as a possiblc modę of transmission in Canada. Given the ubiqui-tous naturę of the organism, environmental or occupational exposure is usually the source of infection. Between 1971 and 1984, 28‘deaths were attributed to listeriosis, 7 being reported in 1984 (LCDC: unpublished data). There was a slight increase in the number of cases between 1982 and 1984, but this may have been due to the Nova Scotia outbreak and not a real increase in incidence. Data on the population at risk are unavaila-ble; therefore, risk-specific attack ratcs cannot yet be calculated.
The studies of Schlech and colleagues4 have suggested that L monocytogenes is carried by 5% of the generał population. Fecal carriage has been reported in 29% of poultry workers and in 77% of public health laboratory workers involved in L monocytogenes isolation.9 The public health im-portance of human fecal carriage is not known.
There are 16 recognized serotypes,10*13 given that there are at least 15 different "O" (or somatic) antigens and 5 "H" (or flagellar) antigens. Serotypes l/2a, l/2b and 4b account for morę than 90% of the cases reported worldwide.14
A phage-typing system has helped in the epidemiologie investigations of foodborne out-breaks of listeriosis. The major system now used allows Identification of 54% of the serogroup 1/2 strains and 77% of the serogroup 4 strains of L. monocytogenes.l5 However, a recent report has suggested that the phage type of a given Ustcria strain can change with time.16 Thus, the cunent phage-typing system must be modified, or an alternative to phage-typing must be developed. Several researchers at the Centers for Disease Control (CDC), Atlanta, are inve$tigating a method that involves isoenzymes to differentiate the strains.
Source
L monocytogenes can be isolated from a variety of sources: poor-quality silage, vegetation, soil, sewage, stream water, mud, slaughter-house waste, milk of normal and mastitic cows, and feces of healthy humans. In addition, the organism has been isolated from at least 37 species of mammals and 17 species of fowl, flies, ticks, fish and crustaceans.10-14
Pathogenicity
Biologie features
L monocytogenes is a gram-positive, micro-aerophilic, asporogenic badllus that has a charac-teristic tumbling motility between 20°C and 25°C and that produces slight 0-hemolysis on sheep-blood agar. It can grow at a variety of tempera-tures, from 1°C to 45°C,10 and thus can thrive in foods kept at refrigeration temperatures.
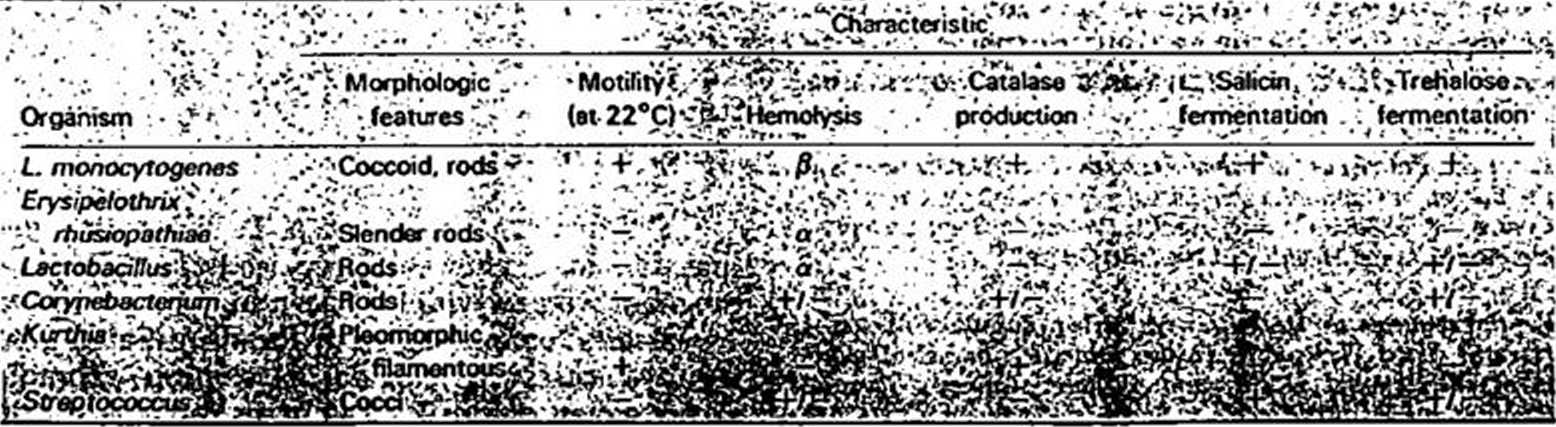
In the laboratory Usteria can frequently be missed or misidentified.,u2 One must be careful not to overlook Usteria as a contaminating organism, especially when symptoms and conditions suggest listeriosis. The characteristics that dis-tinguish Usteria from other morphologically simi-lar organisms are listed in Table 1.
The tests for pathogenidty indude the ability to cause keratoconjunctivitis in guinea pigs (Antoni test), toxirity in chick embryos and death in mice.17
Viru lence factors
Many potential virulence factors have been identified in the literaturę; these may or may not be important to the overall pathogenicity of L. monocytogenes.18 The morę important factors ap-pear to be a monocytosis-producing agent,5*19 a lipopolysaccharide-like materiał,70-21 hemoly-
.Tablel — Characteristics of Usteria nuMOcytogenesarid morphologicałly similar rnicróorganiśms k .vi^ł.WV., ;.f y .• •
• > . . r ** *. * %• •• :• ' . C* .t r
CMAJ, VOL 138, MARCH 1,1988
414
Wyszukiwarka
Podobne podstrony:
68488 skanowanie0019 (32) 2.9.2.4. Presentation of text to classical musie The students sitting in r
A number of medical milestones have recently been reached, with antibody tests approved, phase \l\ v
4. Survival mechanism of micróbes in ch/orinated water. Waterborne 2 diseases. 5. Controlling of
SPECIFICITY OF TRAINING MARINĘ ELECTRO A UTOMA TION OFFICERS A T THE ... Rys. 4. Laboratoiy stand fo
99 Seasonal and experiinental changes in Msum have also been interpreted in terms of body remodellin
IMGx48 268 The Origin of Civilisatiou Armed with the theoretical base we have now built, this concep
Testing indicates that the proportion of people who have had COVID-19 in the U.K. is Iow, but that t
dpp07 INTROOUCTION IN explanation of the title T have chosen for my book I woulil say that, above al
Topological Asymptotic Expansion of the Shape Functional Now we are in position to establish the asy
99 Seasonal and experiinental changes in Msum have also been interpreted in terms of body remodellin
38 Annex 2.1 Page 2 of 5 4. The Program has now virtually eliminated riverblindnes
You have dow nloaded a document from RE-BIIŚrepository of the Universitv of Silesia in Katowice Titl
have all been found serviceable. AU types of adapt-alions can prove successful in fact, prnviding th
CONCEPT OF THE GODDESS ŚAKTI EXPOUNDED IN THE LALITOPAKIIYANA 109 They have also been dcscribcd as b
DSCF0022 ESSAYS IN SWEDISH HISTORY it is probably still true to say that the campaign of 1633 would
The Party System in Great Britain • Asa result of t electoral system two parties have traditionally
essent?rving?62 E S S E N T I A L W O O D C A R v I N G T F. C H N I Q U E S FlG 4.18 The edges of t
więcej podobnych podstron