WOUND HEALING
23
perioplic corium of dermal origin, the coronary epidermis constitutes the coronary band. Clinically, the under-
lying modifi ed subcutis, or coronary cushion, is often considered part of the coronary band.
The slow distad growth of the hoof wall (10 mm per month) results from the differences between the
primary and secondary epidermal laminae of the stratum internum. Cells of the primary epidermal laminae
progressively keratinize while moving distally with the tubules of the stratum medium. The basal cells of the
secondary lamellae, on the other hand, adhere to the lamellar corium and do not keratinize. A continuous cycle
of breaking and reforming links between the two cell populations is responsible for maintaining a very strong
attachment of the hoof wall to the parietal surface of the distal phalanx, while allowing slow distal growth of
the horn tubules.
99
Upon reaching the solar surface of the hoof, the keratinized cells of the epidermal laminae
form the junction between the hoof wall and the sole. This zone of softer and whiter horn is commonly called
the white line (Figure 1.9).
Specifi c biomechanical properties of the equine foot affect the pattern of injury but also the pattern of repair.
Any injury of suffi cient force to invade the resistant stratum corneum usually results in a full-thickness wound
(Figure 1.10). Full-thickness hoof wounds are rare but when they occur, the rigidity of the stratum corneum
usually prevents gaping of the wound margins, encourages fracture as opposed to tear of the hoof capsule, and
causes the tissues to completely avulse from the underlying structures rather than just lacerate.
100
Where the
hoof wall is thinner and less rigid, at the coronary band and at the heel, lacerations, tears, and partial-thickness
wounds are more common. For more information regarding laceration and avulsion injury of the hoof, see
Chapter 8.
A
B
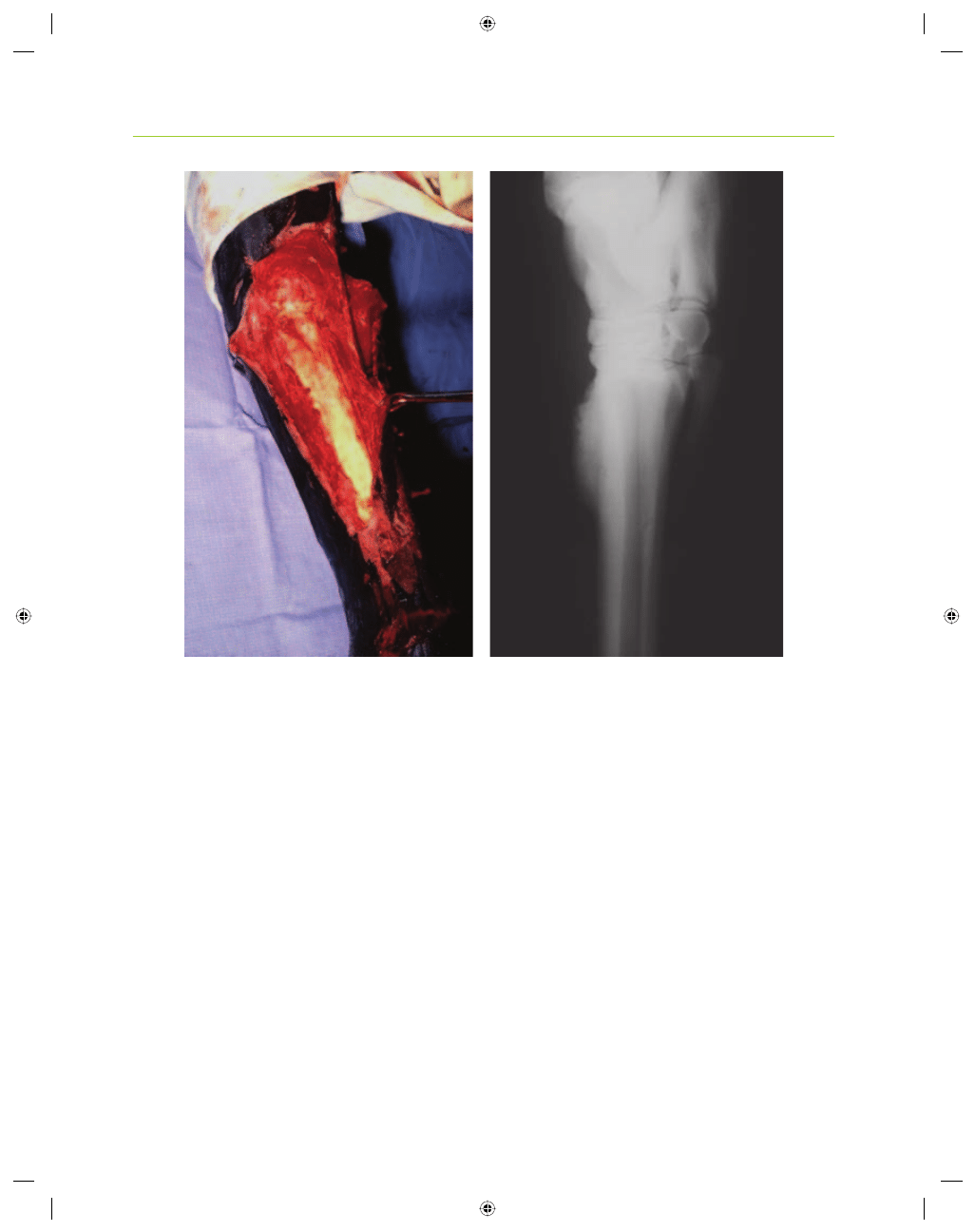
Figure 1.8. (a) Extensive avulsion injury to the dorsal metatarsal region. This picture was taken at surgery; the periosteum had been
stripped from the exposed cortex of the metatarsal bone. Following cleansing and debridement, the edges of the distal half of the
wound were apposed with sutures while the proximal half was left open to heal by second intention. A bandage cast splint that
extended from the plantar fetlock region to the caudal mid-tibial region was used to immobilize the limb. (b) Lateral radiograph taken
following complete healing of the wound. Note the mature (remodeled) exostoses that formed on the dorsal aspect of the metatarsal
bone in the region where the wound was allowed to heal by second intention. Courtesy of Dr. T. Stashak.
Wyszukiwarka
Podobne podstrony:
00037, 985992085a959304dedf013673e8b75f
00037, 1f3c8f3ec4af44a6518b642d22cd88e3
00037, dadefb7ccc3bc14e1e479cb3a9aa27cb
00037, ff7f468e251a885e8d7646553bbf787f
00037, 7e444425284193f7f492ae46d7863764
00037, 985992085a959304dedf013673e8b75f
00037, 552a98fb5414027a1c4aedc4bbdb1f3c
00037, d478e661a05b587db7ed6a357303cacf
00037, 7e444425284193f7f492ae46d7863764
00037 con other 1
00037, 2c5ca0fa46cdd4a80fa828182c266533
00037, 0d871f73d29f60403f5db6609db2f0a1
więcej podobnych podstron