The effects of Chinese calligraphy handwriting and relaxation training
in Chinese Nasopharyngeal Carcinoma patients: A randomized
controlled trial
Xue-Ling Yang
,
, Huan-Huan Li
, Ming-Huang Hong
, Henry S.R. Kao
a
Department of Psychology, Sun Yat-Sen University, Xin gang xi Road 135, Guangzhou 510275, Guangdong, China
b
Department of Psychology, Southern Medical University, Guangzhou, China
c
Cancer Center of Sun Yat-Sen University, Guangzhou, China
d
University of Hong Kong, Hong Kong
International Journal of Nursing Studies 47 (2010) 550–559
A R T I C L E I N F O
Article history:
Received 7 January 2009
Received in revised form 1 October 2009
Accepted 23 October 2009
Keywords:
Calligraphy
Nasopharyngeal Carcinoma
Psychological intervention
Relaxation training
A B S T R A C T
Background: Chinese calligraphy handwriting is the practice of traditional Chinese brush
writing, researches found calligraphy had therapeutic effects on certain diseases, some
authors argued that calligraphy might have relaxation effect.
Objectives: This study was to compare the effects of calligraphy handwriting with those of
progressive muscle relaxation and imagery training in Chinese Nasopharyngeal Carcinoma
patients.
Design and participants: This study was a randomized controlled trial. Two hundred and
eighty-seven Nasopharyngeal Carcinoma patients were approached, ninety (31%) patients
were recruited and randomized to one of the three treatment groups: progressive muscle
relaxation and guided imagery training group, Calligraphy handwriting group, or a Control
group. Seventy-nine (87.8%) completed all of the outcome measures.
Outcome measures: The primary treatment outcome was the changes of physiological
arousal parameters measured by pre- and post-treatment differences of heart rate, blood
pressure and respiration rate. The secondary outcomes included: modified Chinese version
of Symptom Distress Scale, Profile of Mood State-Short Form, and Karnofsky Performance
Status measured at baseline, during treatment (after the 2-week intervention), post-
treatment (after the 4-week intervention) and after a 2-week follow-up. Effectiveness was
tested by repeated measure ANOVA analyses.
Setting: Cancer centre of a major university hospital in Guangdong, China.
Results: Results showed that both of calligraphy and relaxation training demonstrated
slow-down effects on physiological arousal parameters. Moreover, calligraphy practice
gradually lowered participants’ systolic blood pressure (simple main effect of time at pre-
treatment measure, p = .007) and respiration rate (p = .000) at pre- and post-treatment
measures as the intervention proceeded, though with a smaller effect size as compared to
relaxation. Both of calligraphy and relaxation training had certain symptom relief and
mood improvement effects in NPC patients. Relaxation was effective in relieving symptom
of insomnia (p = .042) and improving mood disturbance, calligraphy elevated level of
concentration (p = .032) and improved mood disturbance.
Conclusions: Similar to the effects of relaxation training, calligraphy demonstrated a
gradually build-up physiological slow-down, and associated with heightened concentra-
tion and improved mood disturbance. Calligraphy offered a promising approach to
improved health in cancer patients.
ß
2009 Elsevier Ltd. All rights reserved.
* Corresponding author. Tel.: +86 20 84114265x807; fax: +86 20 84114266.
E-mail address:
(H.-H. Li).
Contents lists available at
International Journal of Nursing Studies
journal homepage: www.elsevier.com/ijns
0020-7489/$ – see front matter ß 2009 Elsevier Ltd. All rights reserved.
doi:

What is already known about the topic?
There were documented treatment-related symptoms
and mood disturbance in NPC patients, but less is done to
relieve their symptom distress and mood disturbance in
China.
Relaxation training was effective in reducing treatment-
related symptoms and improving patients’ mood dis-
turbance and quality of life.
Calligraphy had some therapeutic effects on certain
diseases but less is known about its applicability and
acceptability among cancer patients.
What this paper adds
Similar to the effects of progressive muscle relaxation
and guided imagery training, calligraphy handwriting
demonstrated slow-down effects on physiological arou-
sal parameters, and was effective in heightening cancer
patients’ concentration level as well as improving their
mood disturbance.
Compared to that of relaxation training, calligraphy had a
gradually build-up effect in lowering physiological
arousal, although with a smaller effect size, which was
partly due to the characteristics of calligraphy hand-
writing practice and Chinese characters.
Chinese calligraphy handwriting offers a promising
approach to improved health in cancer patients.
1. Introduction
Nasopharyngeal Carcinoma (NPC) is one of the most
common cancers in Southeast China, Taiwan and Hon-
gkong, with approximately 10–30 out of 100,000 people,
mostly men, diagnosed in Guangdong province yearly (
). NPC diagnosed at an early stage has relatively
better prognosis than most cancers due to advances in
medical care, especially in radiotherapy (RT) medicine
(
). However, high levels of depression and
anxiety in NPC patients had been observed in hospitalized
settings (
). One of the reasons was that the
acute symptoms related to intense RT treatment had
significant impact on NPC patients’ everyday experiences
(
). These distressful experiences
often involved severe pain in oral-pharyngeal cavity, dry
mouth and difficulty to swallow, noticeable alteration in
appearance,
difficulty
opening
mouth
and
hearing
damages (
).
Among psychosocial interventions for reducing treat-
ment-related symptoms and mood disturbance, relaxation
and imagery training were most investigated in controlled
trials, partly due to its low cost, ease of use and having few
if any negative side effects (
). Studies had
observed progressive muscle relaxation (PMR) and guided
imagery (GI) training could reduce anxiety and improve
quality of life among cancer patients (
), could reduce mood disturbance and emotional
suppression in breast cancer patients (
Findings of these studies conformed to the results of a
review article (
) that found relaxation
had significant beneficial effects on treatment-related
symptoms (such as nausea, pain, vomiting), emotional
adjustment (such as anxiety, depression, hostility, tension,
fatigue, confusion, vigor, overall mood), and physiological
arousal parameters (such as heart rate, blood pressure and
respiration). In view of these findings, the author
suggested that relaxation training should be implemented
into clinical routine for cancer patients in acute medical
treatment.
Art therapy, a complementary and alternative treatment
modality, had been proven to have therapeutic effects in
cancer patients (
Gotze et al., 2009; Svensk et al., 2009
).
Proponents of art therapy believed that the uninhibited
expression of feelings and emotions through art might help
to release the fear, anxiety and anger that many cancer
patients experienced. Art could also be viewed as a
distraction to the pain and discomfort of disease, allowing
patient relief from stress. Shufa, or Chinese calligraphy was
the writing of Chinese characters by hand using a soft-tipped
brush, was traditionally regarded in China as one of the fine
arts (
). To date, empirical studies on
Chinese calligraphy had been focusing mainly on how to
execute and appreciate it artistically by following the
practical experiences of the great masters. Little systematic
research had been done on the fundamental behaviors
associated with the calligraphy practice, such as visual
perception, emotions and physiological response. The
existing clinical researches on calligraphy handwriting
had found that calligraphy had treatment effects on some
behavioral and psychosomatic diseases, such as Attention
Deficit Hyperactivity Disorder (ADHD) in children (
), Alzheimer’s disease (
Kao, 2003; Kao et al., 2000a,b
),
hypertension (
Guo et al., 2001; Kao et al., 2001
) and diabetes
II (
). The authors further argued that the act
of brushing caused heightened attention and concentration
on the part of practitioners and resulted in their emotional
stabilization and physical relaxation (
The main purposes of the present study were to
compare the effects of calligraphy handwriting on NPC
patients’ physiological arousal parameters, symptom
distress, mood disturbance and functional status with
those of progressive muscle relaxation and imagery
training.
2. Methods
2.1. Study design
The study was a longitudinal, randomized, controlled
trial with 2 intervention groups and a control group. A
3 2 4 mixed-effect factorial design was used for
assessing physiological arousal parameters, and a 3 4
mixed-effect factorial design was used for assessing the
secondary outcome measures. The protocol for this study
was approved by the Review Board of the investigator’s
institution.
2.2. Participants and setting
The study was carried out from June 2007 to March
2008 in the in-patient department of Cancer Centre of a
X.-L. Yang et al. / International Journal of Nursing Studies 47 (2010) 550–559
551
major university hospital in Guangdong, China. Patients
diagnosed with NPC based on the American Joint
Committee on Cancer Staging (
), and sched-
uled for RT, aged 18–80 were eligible for this study.
Exclusionary criteria included: patients who had finished
surgical treatment in the last 3 months; patients who were
unable to read and write Chinese with a brush (e.g.,
illiteracy or physical disability); patients with cardiovas-
cular or respiratory diseases, e.g., essential or secondary
hypertension (systolic blood pressure equal to or greater
than 140 mmHg, and/or diastolic blood pressure equal to
or greater than 90 mmHg), abnormal heart rate or
abnormal
respiration.
287
eligible
patients
were
approached and 90 (31%) consented to participate. The
major reasons for refusal included no time or interest,
feeling lack of energy and concentration.
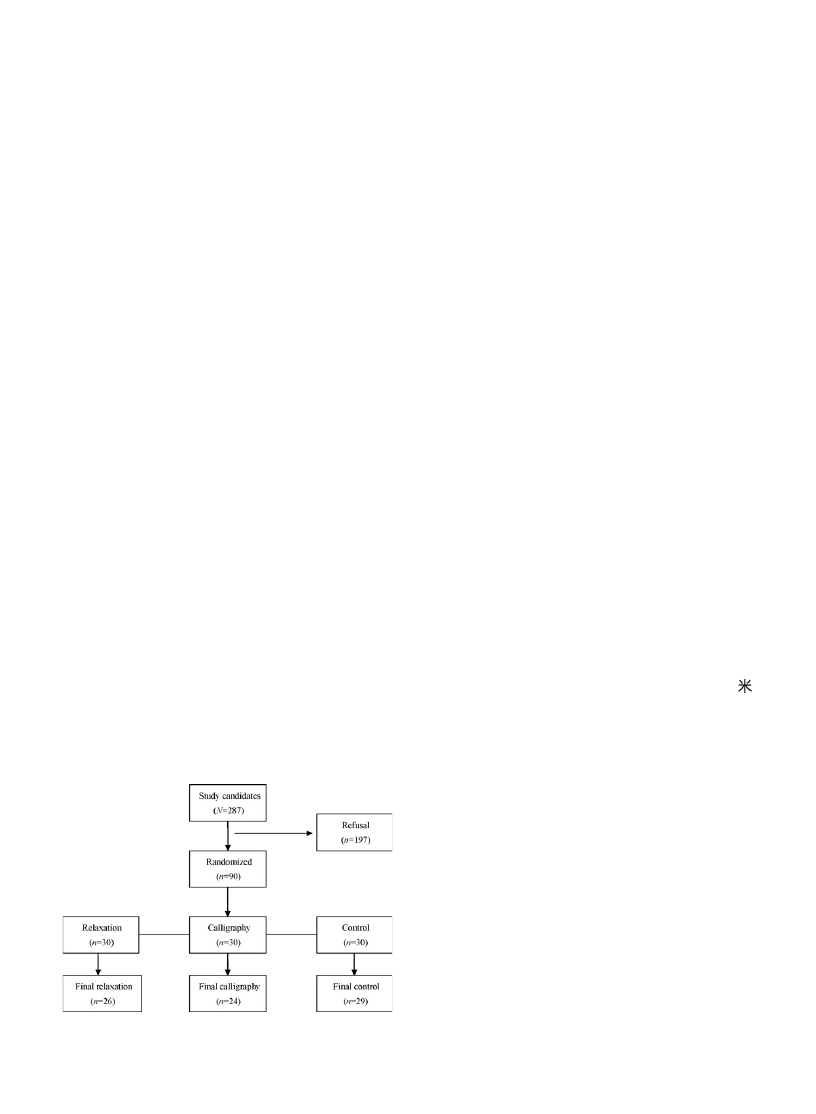
shows the flow chart of participants of this study.
90 patients who signed the informed consent were
included in the study and randomly assigned to one of
the three treatment groups: Relaxation (n = 30), Calligra-
phy (n = 30), and Control (n = 30). The randomization
procedure was accomplished by a computer-generated
table in blocks of 3 without any restriction or stratification.
By the end of the study, a total of 79 patients completed the
final assessments: Relaxation (n = 26), Calligraphy (n = 24),
Control (n = 29).
2.3. Procedures
To control for the potentially important confounding
variables that might have an impact on the outcome
measures, patients were monitored for any medication
usage, e.g., antidepressant, anti-hypertension drugs. No
such medication usage was reported. After the completion
of the final assessment, each participant was encouraged to
give feedback on effectiveness of the programs and
suggestions to improve the intervention procedure. The
reasons of participant dropout were also recorded.
2.4. Intervention
2.4.1. Relaxation training
The relaxation training lasted 30 min per day for 4
consecutive weeks; 20-min progressive muscle relaxation
(PMR) was followed by 10-min guided imagery (GI). PMR
was administered by a clinical therapist in a separate, quiet
and adequately lit inpatient ward following the abbreviated
form of Jacobsen’s procedure developed by
. For this study, the instructions led
participants in tensing and relaxing 12 major muscle groups
working from the hands and arms up to the head and down
to the feet. Participants were asked to focus on the contrast
between sensations of muscle tension and relaxation. The GI
training was delivered by a pre-recorded MP3 audio file read
by a female research associate following a script, while the
participant was in a relaxed position with the eyes closed.
The script began with suggestions for relaxation and deep
breathing, and then encouraged the participant to imagine a
pleasant special place without any pain and symptoms.
Continuous soft instrumental music provided background
to the narrator’s voice.
2.4.2. Calligraphy practice
The participants in Calligraphy Group practiced Chinese
calligraphy in a quiet, adequately lit inpatient room led by a
retired language teacher, who was a senior calligrapher. The
time duration of calligraphic writing was 30 min per day for 4
consecutive weeks as the same as that of relaxation group.
The content of Chinese calligraphy character was chosen
randomly in a handbook of calligraphy writing. To control for
the influence of emotional positiveness of the Chinese
character, rather than the calligraphy practice intervention
on outcome measures, especially on mood status ratings, 20
characters were randomly chosen in the handbook to
evaluate the emotional properties of these characters on a
5-point Likert scale (‘‘1’’ represented ‘‘very negative’’ and ‘‘5’’
represented ‘‘very positive’’) by 60 college students. The
result showed that the emotional positiveness of the sample
characters were 3.118 0.585. The calligraphic writing
involved brush handwriting by tracing the strokes and
structures of the characters displayed in a mixture of commonly
used calligraphic styles, i.e., the calligraphic brush was middle-
sized, the length of the pen was 28 cm, a 11 by 11 cm ‘‘
’’-
shaped pane was printed on the calligraphic rice paper.
2.5. Baseline and outcome measures
At baseline, demographic and clinical data were
collected either from the patients or from the medical
records prior to the interventions, and the consent to
access the patients’ medical records had been obtained
from the medical staff. Demographic information includ-
ing age, sex, education, marital status and clinical
information regarding disease and treatment modality
were collected on a demographic form.
2.5.1. Primary outcome measure
The primary outcome was the change of physiological
arousal parameters assessed by heart rate (HR), blood
pressure (BP), and respiration rate (RR), which were
measured at pre- and post-treatment per treatment day,
5 days a week (i.e., Monday to Friday), and for 4
consecutive weeks. HR and BP were measured by Omron
Upper Arm Digital Sphygmomanometer, Model HEM-
7051. The RR was counted by a clinical nurse using a
Fig. 1. Flow chart of participants.
X.-L. Yang et al. / International Journal of Nursing Studies 47 (2010) 550–559
552

stopwatch who was blind to the study hypotheses. To
avoid the impact of diurnal fluctuation of physiological
parameters, the treatments and measures were set at fixed
time period across days, i.e., 10–12 am, or 3–5 pm, or 6–
8 pm. The measures were averaged to calculate a ‘‘pre’’
(pre-treatment) and ‘‘post’’ (post-treatment) score based
on at least 4 days of measures each week, otherwise the
data would be considered invalid. To avoid the influence of
physical activity on physiological parameters, participants
were asked to sit quietly for 5 min before measurements.
The time interval between pre- and post-treatment
assessments was 30 min in 3 treatment groups.
2.5.2. Secondary outcome measures
The following secondary psychosocial outcomes were
assessed at baseline, during treatment (i.e., after 2-week
intervention), post-treatment (i.e., after the final fourth
week) and after a 2-week follow-up.
2.5.2.1. Symptom distress. Symptom distress was mea-
sured by the modified Chinese version of Symptom
Distress Scale (SDS). The SDS was one of the first scales
developed to measure the construct of symptom distress,
defined as ‘‘the degree of discomfort from the specific
symptom being experienced as reported by the patient’’
(
). Studies have shown that
levels of symptom distress could be a significant predictor
of survival in patients with variety types of cancer (
and Sloan, 1995; Frederickson et al., 1991
). The original
SDS was a 13-item self-rating scale including: frequency
and intensity of nausea, appetite, insomnia, frequency and
intensity of pain, fatigue, bowel pattern, concentration,
appearance, breathing, outlook and cough. In previous
studies, Cronbach’s
a
coefficient of the SDS ranged from
0.70 (
) to 0.92 (
). Most studies reported a Cronbach’s
a
coefficient
greater than 0.80. In the present study, Cronbach’s
a
coefficient of the modified SDS was 0.80, test–retest
reliability over 1 week interval was 0.71.
In the present study, the original SDS was firstly
translated into Chinese according to back-translation
principles (
Baldacchino and Buhagiar, 2003
), and then
modified by adding 5 items that represented NPC patients’
distressing experiences associated with radiotherapy and
chemotherapy. The procedure was performed as follows:
20 NPC patients were interviewed by the researchers to
rate for their most distressing symptoms except the 13
items of original SDS, 5 items were attained upon the 95%
patients’ congruence. The 5 items were added as follows:
dry mouth, difficulty opening mouth, oral ulcer, hearing
difficulty and skin condition.
For the current study, the modified SDS was adminis-
tered consecutive items on 2 pages. The 18 items of the
modified SDS were calibrated scores ranging from 1 (no
distress) to 5 (extreme distress) in accordance with the
original SDS of McCorkle (
2.5.2.2. Mood disturbance. The Profile of Mood State-Short
Form (POMS-SF, Chinese version) was used to assess the
patient’s negative mood states in this study. The Chinese
version of POMS-SF was developed by
,
which consists of 30 items (based on the 65-item
questionnaire in the long form) and contains the same
six subscales: Tension-Anxiety (TA), Depression-Dejection
(DD), Anger-Hostility (AH), Fatigue-Inertia (FI), Confusion-
Bewilderment (CF), and Vigor-Activity (VA). A composite
score, the total mood disturbance (TMD) score, is
computed by summing each of the individual scores for
TA, DD, AH, FI and CF, with vigor scores subtracted to
indicate patients’ total mood disturbance. Each item of the
POMS-SF is scored on a 5-point Likert scale ranging from 0
(not at all) to 4 (extremely). Cronbach’s
a
coefficient was
0.93 in a 289 hospitalized cancer sample (
). In this study, Cronbach’s
a
coefficient was 0.79.
2.5.2.3. Functional status. Karnofsky Performance Status
(KPS) provided a global indicator of functional status
(
). The scale ranges from
100 (Normal, no complaints, no evidence of disease) to 0
(Dead) with 10-point intervals, each with explicit descrip-
tors. Lower scores indicate greater symptoms and physical
restrictions. Inter-rater reliability between two indepen-
dent nurses was 0.92 in the current study.
2.6. Statistical analysis
The primary endpoint of intervention efficacy was the
change in physiological arousal parameters measured at
pre- and post-treatment, i.e., the significant interaction
effect of Prepost by Group. The secondary endpoints
included SDS scores, POMS-SF subscale scores, and KPS
rating measured at different time points, i.e., the significant
interaction effects of Group and Time.
Outcome data analyses were based on study completers
only. Baseline characteristics were compared among
groups using one-way Analysis of Variance (ANOVA) for
quantitative variables and chi-square test for qualitative
variables performed by SPSS version 11.5 (SPSS Inc.,
Chicago, IL). The intervention effects on secondary out-
come measures were determined by using two-way
mixed-effects repeated measures ANOVA (RMANOVA)
with Group as between-subjects factor and Time (Time
1, pre-treatment; Time 2, during treatment; Time 3, post-
treatment; Time 4, 2-week follow-up) as within-subject
factor. The intervention effects on physiological para-
meters were assessed by using three-way RMANOVA with
Group as between-subjects factor and Time, Prepost as
within-subject factors. Partial Eta squared values were
reported as measures of effect size. If the sphericity
assumption was not met, the Huynh-Feldt correction
would be applied. Post hoc multiple comparisons were
performed by using the Least Significant Difference (LSD)
adjustment. The Group, Time and Prepost main effect
would be interpreted in light of significant three-way and
two-way interaction and would not be described further.
3. Results
3.1. Sample characteristics
A total of 90 NPC patients meeting inclusion criteria were
recruited. The demographic and clinical characteristics of
X.-L. Yang et al. / International Journal of Nursing Studies 47 (2010) 550–559
553
the sample at baseline (n = 90) assessment were presented
in
. The mean age of the sample was 49.63 10.81,
ranging from 22 to 71 years old. The majority of patients were
male (68.9%), and married (93.3%). Only 31 (34.4%) patients
had more than 9 years of education. 41 (45.6%) patients were
diagnosed with II stage NPC, 49 (54.4%) received a diagnosis of
III stage. All patients received RT as their current treatment.
The overall mean length of hospital stay was 55 9 days. There
was no statistically significant group difference on all of the
demographical and clinical variables.79 patients (87.8%)
completed the programs and provided valid data on outcome
measures. The numbers of dropouts by treatment groups
were: Relaxation, 4; Calligraphy, 6; Control, 1. The rates of
dropout were not significantly different across groups
(p = .140). Of the 11 dropouts, 3 patients (2 in Calligraphy
and 1 in Relaxation) reported that they were too tired to
complete the program, 4 patients (2 in Relaxation and 2 in
Calligraphy) provided insufficient data on physiological
parameters, 1 patient in Calligraphy group and 1 in Control
discharged prematurely from hospital due to economic or
family issues, 2 patients (1 in Relaxation and 1 in Calligraphy)
dropped out due to diminished interest. There were no
significant differences between the completers and non-
completers on demographic and clinical characteristics except
education (non-completers had a higher percentage of
illiteracy (
x
2
(1, n = 90) = 8.39, p = .039). No significant group
difference was found on baseline assessments of physiological
measures, SDS, POMS-SF, and KPS (all p > 0.05).
3.2. Intervention effects on physiological arousal parameters
summarizes the results of repeated measures of
ANOVO. For HR, both of relaxation and calligraphy
intervention significantly lowered participants’ post-treat-
ment heart rate, but no pre-post difference was found in
the control group (Prepost by Group interaction effect,
F(2,76) = 20.67, p = .000, partial
h
2
= .35). The mean change
of Pre-post measure was
1.72 bpm in Relaxation group,
and
1.14 bpm in Calligraphy group. There was no
significant difference on the Pre-post change scores
between the two intervention groups (p > .05).
For systolic blood pressure (SBP), relaxation and
calligraphy intervention significantly lowered partici-
pants’ post-treatment SBP, but no pre-post difference
was found in the control group (Prepost by Group
interaction
effect,
F(2,76) = 35.99,
p = .000,
partial
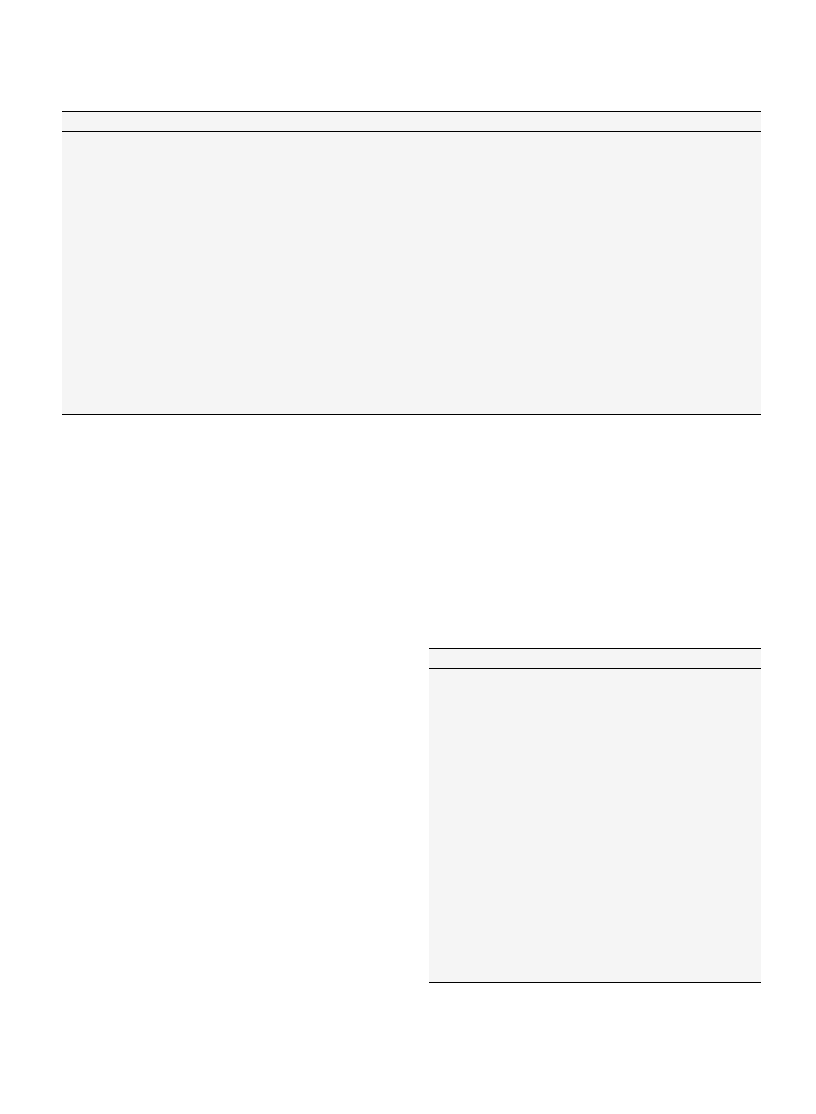
Table 1
Demographic and clinical characteristics of the sample at baseline measures.
Relaxation
Calligraphy
Control
F
p
Age
0.01
.995
30 or younger
1
2
1
31–55 years
17
15
18
56 years or older
12
13
11
Gender
0.05
.952
Male
21
20
20
Female
9
10
10
Marital status
1.48
.233
Single (divorced)
0
3
2
Married
30
27
28
Education
0.36
.700
6 years or less
7
7
6
7–9 years
13
11
13
More than 9 years
10
12
11
Stage of cancer
0.40
.673
I
0
0
0
II
14
11
14
III
16
19
16
IV
0
0
0
Table 2
Multivariate test of RMANOVA on significant physiological arousal
parameters.
Effects
F
df
p
Partial
h
2
HR
Prepost
81.31
1,76
.000
.517
Prepost Group
20.67
2,76
.000
.352
SBP
Time
8.68
3,74
.000
.260
Prepost
207.58
1,76
.000
.732
Prepost Group
35.99
2,76
.000
.486
Time Prepost
5.51
3,74
.002
.183
DBP
Time
11.67
3,74
.000
.321
Time Group
3.50
6,146
.003
.126
Prepost
355.44
1,76
.000
.824
Prepost Group
80.16
2,76
.000
.678
Time Prepost
6.89
2,74
.000
.218
Time Prepost Group
2.36
6,146
.033
.088
RR
Time
13.73
3,74
.000
.358
Time Group
5.21
6,146
.000
.176
Prepost
331.21
1,76
.000
.813
Prepost Group
95.56
2,76
.000
.715
Time Prepost
4.60
3,74
.005
.157
Time Prepost Group
5.56
6,146
.000
.186
Note: RMANOVA: repeated measure analysis of variance.
HR: heart rate; SBP: systolic blood pressure; DBP: diastolic blood
pressure; RR: respiration rate.
Partial
h
2
: effect size estimate.
X.-L. Yang et al. / International Journal of Nursing Studies 47 (2010) 550–559
554
h
2
= .49). The mean change of Pre-post measure was
1.68 mmHg in Relaxation group,
1.41 mmHg in Calli-
graphy, and
.23 mmHg in Control. There was no
significant difference on the change scores between the
two intervention groups (p > .05). Post hoc comparison
revealed that calligraphy not only significantly lowered the
post-treatment SBP, but also gradually lowered the pre-
treatment SBP (simple main effect of Time at pre-
treatment measure in Calligraphy group, p = .007), while
relaxation only had treatment effect on post-treatment
measures (p < .05). Regardless of group status, the Pre-post
change score was gradually increased as the intervention
program went on, as was shown by a significant Prepost by
Time interaction (F(3,74) = 5.51, p = .002, partial
h
2
= .18).
For diastolic blood pressure (DBP), the two intervention
groups had different impact on post-treatment measures,
and as the intervention proceeded, the treatment effects
had a trend to increase, indicated by a significant three-
way interaction effect (F(6,218) = 2.28, p = .040, partial
h
2
= .09) and all of the two-way interaction effect (all
p < .05). The mean change of Pre-post measure was
1.76 mmHg in Relaxation group,
1.46 mmHg in Calli-
graphy group, and
.099 mmHg in Control.
For RR, different groups exhibited different patterns of
treatment effect as the intervention proceeded, as indi-
cated
by
the
significant
three-way
interaction,
F(6,228) = 7.10, p = .000, partial
h
2
= .06. Relaxation train-
ing
significantly
lowered
post-treatment
RR
(F(1,76) = 433.41, p = .000, partial
h
2
= .85), the mean Pre-
post change was
1.14 breath per minute, and the change
became larger with the proceeding of intervention,
F(3,74) = 11.83, p = .000, partial
h
2
= .32. In Calligraphy
group, the Pre-post change was significant (F(1,76) = 69.26,
p = .000, partial
h
2
= .48), although with a less magnitude of
.47 breath per minute, and interestingly, the pre-
treatment RR gradually slowed down across time points
(F(3,74) = 8.25, p = .000, partial
h
2
= .06). No two-way
interaction or their main effect was found in Control group.
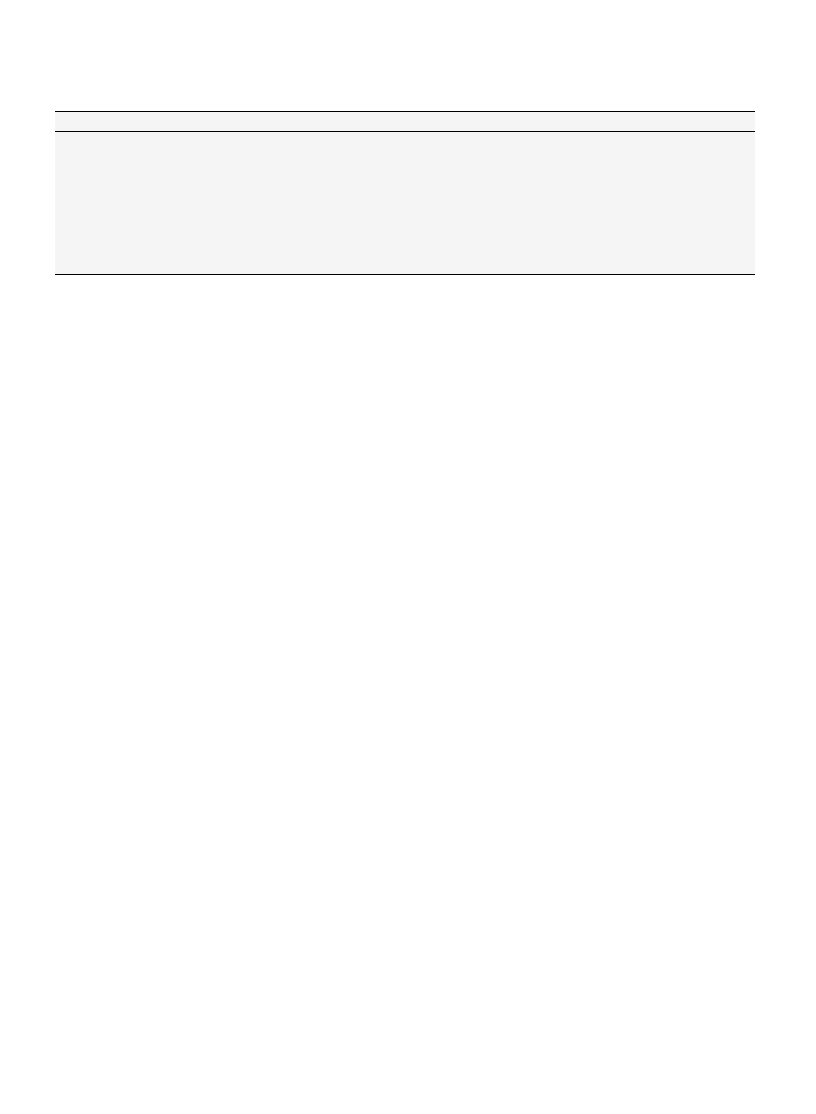
3.3. Intervention effects on symptom distress and functional
status
The two interventions had no significant effect on
average symptom distress score, which was calculated on
the basis of 18 individual items. However, the interven-
tions had different impacts on the following items of
modified SDS, as was indicated by significant Time by
Group interaction (see
): Insomnia (F(6,193) = 2.34,
p = .042), and Concentration (F(6,206) = 2.43, p = .032).
Relaxation significantly improved insomnia at Time 2
(F(2,76) = 7.56, p = .001) and Time 3 (F(2,76) = 5.97,
p = .004), and the treatment gain was maintained at 2-
week follow-up (F(2,76) = 6.38, p = .003); Calligraphy
group significantly scored lower than the other two groups
at
Time
2
(F(2,76) = 6.34,
p = .003)
and
Time
3
(F(2,76) = 3.69, p = .030) on Concentration, but the treat-
ment gain was not maintained at 2-week follow-up
(p = .066).
Relaxation and calligraphy exerted no significant
treatment effect on KPS ratings, however, patients’
functional status seemed to get better across the time
points, indicated by a significant Time main effect
(F(3,228) = 18.15, p = .000), a reflection of intervention
independent, gradual improvement of patient functioning
throughout the course of treatment.
3.4. Intervention effects on mood disturbance
As detailed in
, relaxation training and calligraphy
practice had different treatment effects on the following
subscales of POMS-SF: TA (F(6,184) = 2.75, p = .021), DD
(F(6,224) = 9.65, p = .000), AH (F(6,166) = 2.77, p = .025), FI
(F(6,174) = 4.77, p = .001), and TMD score (F(6,169) = 9.65,
p = .000), as were indicated by significant Time by Group
interaction effects. Relaxation lowered participants’ TA
score at Time 3, and maintained at follow-up; Relaxation
and Calligraphy group scored lower than Control on DD
subscale at Time 2 and Time 3, but the treatment effect was
not maintained at Time 4; Relaxation and Calligraphy group
scored lower on AH subscale than Control at Time 3, and
maintained at follow-up; Calligraphy lowered FI score at
Time 2 and Time 3, but the treatment gain diminished at
follow-up assessment.
4. Discussion
The present study tested the effects of Chinese
calligraphy handwriting practice in Chinese NPC patients,
Table 3
Significant intervention effects on items of Symptom Distress Scale (mean SD).
Measures
Relaxation
Calligraphy
Control
F
p
h
2
Insomnia
Time 1
2.08 .89
2.13 .99
2.03 .87
0.06
.938
.002
Time 2
1.81 .57
2.33 .57
2.52 .87
7.56
.001
.166
Time 3
1.46 .51
1.92 .58
1.46 .84
5.97
.004
.136
Time 4
1.23 .43
1.75 .68
1.83 .81
6.38
.003
.144
Concentration
Time 1
2.19 .75
2.12 .68
2.00 .76
0.49
.613
.013
Time 2
2.04 .53
2.04 .70
2.48 .79
6.34
.003
.143
Time 3
1.73 .67
1.54 .66
2.03 .68
3.69
.030
.088
Time 4
1.42 .64
1.21 .42
1.59 .63
2.81
.066
.069
Note: Each F tests the simple main effects of Group within each level combination of the other effects shown. These tests are based on the linearly
independent pairwise comparisons among the estimated marginal means.
Partial
h
2
: effect size estimate.
Time 1: measures at pre-treatment; Time 2: during treatment; Time 3: post-treatment; Time 4: 2-week follow-up.
X.-L. Yang et al. / International Journal of Nursing Studies 47 (2010) 550–559
555
which was compared with an established intervention
approach—progressive muscle relaxation combined with
imagery training and a control group. The primary
outcome analyses revealed that the 4-week calligraphy
practice intervention demonstrated a slow-down effect on
physiological arousal parameters (as was measured by HR,
BP, and RR) similar to those of relaxation training, though
in different patterns. The secondary outcomes analyses
revealed that calligraphy had certain symptom relief and
mood improvement effects in NPC patients, providing
further evidence on the efficacy of calligraphy practice as a
psychosocial intervention alternative.
4.1. Intervention efficacy
First of all, primary outcome analyses revealed that
similar to the effects of relaxation training, calligraphy
practice exerted short-term slow-down effects on physio-
logical arousal parameters, including slower heart rate,
decreased blood pressure, and decelerated respiration.
Moreover, calligraphy practice demonstrated gradually
build-up effects on SBP and RR measures, which were
shown by less magnitude of Pre-post change scores, and
simple main effects of time at pre-treatment measures. The
secondary outcome analyses revealed that calligraphy
improved the patients’ concentration level, reduced their
mood disturbance scores on Depression-Dejection, Anger-
Hostility and Fatigue-Inertia subscales.
Years of experimental investigation had found that
calligraphic handwriting act was capable of producing
improvements in the writer’s visual attention, physical
relaxation, emotional stabilization as well as cerebral
activation. A couple of experiments had been carried out to
assess the physiological changes of the writers during
calligraphic writing (
). Results indicated
that subjects experienced relaxation and emotional calm-
ness when they were writing Chinese calligraphy: their
respiration rate decelerated, heart rate slowed down, and
blood pressure and muscular activities dropped. On the
contrary, EEG data showed that cerebral activities
increased during Chinese calligraphy writing.
The above psychophysiological changes observed dur-
ing the process of calligraphy handwriting could be
explained by the characteristics of calligraphic practice
and Chinese character. The calligraphic writing act
involves one’s bodily function as well as one’s cognitive
activity. Motor control and maneuvering of the brush
follow the character configurations. There is, therefore, an
integration of the mind, body, and character interwoven in
a dynamic graphonomic process (
). This intimate
relationship underlies the interactive effects of Chinese
calligraphic handwriting on the mind and the body of the
writer. In addition, the Chinese character forms a perfect
geometric square pattern incorporating such features as
hole, linearity, symmetry, parallelism, connectivity, and
orientation, utilizing geometric and depth perception brain
Table 4
Significant intervention effects on subscales of POMS-SF measures (mean SD).
Measures
Relaxation
Calligraphy
Control
F
p
h
2
TA
Time 1
5.00 1.98
4.96 1.90
4.90 2.93
0.01
.987
.000
Time 2
4.04 1.25
4.08 1.64
4.79 2.27
1.53
.223
.039
Time 3
3.08 1.52
3.50 1.69
4.04 1.54
3.39
.039
.082
Time 4
3.19 1.13
3.19 1.61
4.48 1.99
4.61
.013
.108
DD
Time 1
5.69 1.78
5.75 2.21
5.24 2.66
0.41
.662
.011
Time 2
4.42 1.68
4.46 2.02
5.79 2.73
3.43
.038
.083
Time 3
4.04 1.54
3.79 1.91
5.76 2.78
6.66
.002
.149
Time 4
4.15 1.22
3.83 1.55
4.62 1.82
1.71
.188
.043
AH
Time 1
3.73 1.87
3.50 1.82
3.76 2.52
.098
.906
.003
Time 2
2.73 1.43
3.12 1.19
3.52 1.94
2.39
.099
.060
Time 3
2.35 1.33
2.25 1.15
3.59 1.94
6.47
.003
.147
Time 4
2.28 1.06
2.46 1.25
3.24 1.68
3.77
.028
.091
FI
Time 1
5.65 2.38
5.42 2.54
5.38 2.29
0.10
.903
.003
Time 2
5.00 1.36
4.38 1.74
5.62 1.88
3.62
.031
.087
Time 3
5.00 1.79
3.46 1.53
5.59 1.76
10.65
.000
.219
Time 4
4.69 1.35
3.96 1.37
4.90 1.68
2.82
.066
.069
TMD
Time 1
36.16 8.08
37.83 10.34
36.03 13.20
0.21
.809
.006
Time 2
31.60 6.67
32.71 6.96
36.83 9.92
3.15
.048
.078
Time 3
29.04 6.28
28.17 6.36
35.66 9.20
8.06
.001
.177
Time 4
28.00 4.72
28.21 5.76
32.59 8.94
3.89
.025
.094
Note: Each F tests the simple main effects of Group within each level combination of the other effects shown. These tests are based on the linearly
independent pairwise comparisons among the estimated marginal means.
Partial
h
2
: effect size estimate.
POMS-SF: Profile of Mood State-Short Form; TA: Tension-Anxiety; DD: Depression-Dejection; AH: Anger-Hostility; FI: Fatigue-Inertia; TMD: total mood
disturbance.
Time 1: measures at pre-treatment; Time 2: during treatment; Time 3: post-treatment; Time 4: 2-week follow-up.
X.-L. Yang et al. / International Journal of Nursing Studies 47 (2010) 550–559
556

functions. The writer must follow the pattern with
heightened alertness in the process of writing, at the
meantime, the writing act involves a cognitive facilitation
and emotional calmness process, and thus the concurrent
physiological change (
). Moreover, because
of the softness of the brush tip, the handwriting act
involves a 3-D motion, which generates a powerful source
of impact on the writer’s perceptual, cognitive, and
physiological changes during its practice (
). As
the intervention went on, the calligrapher gained more
control over their maneuvering of the brush, which in turn
induced deeper inner calmness and physiological slow-
down.
Progressive muscle relaxation is a relaxation technique
of stress management developed by American physician
Edmund Jacobson in 1934, which is focused on tensing and
releasing tensions in the 16 different muscle groups. PMR
combined with imagery training had established effects on
a variety of outcome measures in cancer patients.
found relaxation and guided imagery training
was effective in reducing treatment-related nausea and
physiological arousal (as measured by HR and BP) in
chemotherapy cancer patients.
found PMR training was associated with an improvement
on anxiety and quality of life among colorectal cancer
patients. The effectiveness of PMR and GI training on
physiological arousal parameters, as was found in the
present study, had also been established by existing
findings (
Lehrer, 1978; Sheu et al., 2003; Sung et al., 2000
and would not be discussed here. However in the current
study, relaxation was not associated with improvement of
nausea, which might due partly to the statistical floor
effect of nausea, for nausea was not a serious complaint in
patients receiving radiotherapy as their current treatment.
It was observed in the current study that relaxation had an
improvement effect on insomnia, which was consistent
with the existing findings about insomnia research (
). Relaxation training was also associated with
improved mood, including Tension-Anxiety, Depression-
Dejection, Anger-Hostility subscale and total mood dis-
turbance. The mood regulation effect found in the study
was confirmatory to the notion of
that muscular tension was usually followed as a byproduct
of anxiety, one could lower and reduce anxiety by
understanding and learning how to self relax those
muscular tension. Besides anxiety, it was found that
relaxation was also beneficial for moods of depression and
anger, as was documented in other applied researches
(
Leon-Pizarro et al., 2007; Nunes et al., 2007
4.2. Intervention feasibility
Patients in relaxation group reported that relaxation
training could make them feel calm, gain more control over
their aversive feelings, was an effective way to focus on
bodily sensation instead of a painful reality. Patients in
Calligraphy group reported that calligraphy provided a
path to calmness and relaxation of emotion, inspired an
inner motivation to pursue spiritual growth and beauty
appreciation, learned a discipline of being focused and
present in spirit, eliminated their fear of death and feeling
of worthlessness temperately. Feedback on suggestions to
improve the intervention procedure revealed: most
patients (76%) in relaxation group complained that the
program schedule was too rigid to follow, i.e., on fixed time
period of the day, 31% patients reported that practice
before bedtime was preferred; in calligraphy group, most
suggestions focused on the short length of practice, i.e.,
30 min per day, 66% patients reported that 45–60 min was
more desirable.
4.3. Study implication
Researches showed that art therapy intervention in
cancer patients could serve as a catalyst for healing, could
benefit the patients in their quality of life (
), and
demonstrated a significant symptom relieving effect
(
). Historically, Chinese calligraphy
handwriting was regarded as the most abstract and
sublime form of art in Chinese culture, many calligraphy
artists were well-known for their longevity. ‘‘Shufa’’
(calligraphy) is often thought to be most revealing of
one’s personality (examples of calligraphy art could go to
website:
http://www.chinapage.org/calligraphy.html
). To
the artist, calligraphy is a mental exercise that coordinates
the mind and the body to choose the best styling in
expressing the content of the passage. It is a most relaxing
yet highly disciplined exercise indeed for one’s physical
and spiritual well-being. Recent researches found that
calligraphy also have therapeutic values in clinical mental
health setting (
). The findings in the
current study provided further empirical evidence for the
therapeutic value of calligraphy as a form of art therapy. As
was advocated by the International Society of Calligraphy
Therapy (ISCT), calligraphy may play potentially important
role in the field of art therapy in both Chinese and non-
Chinese populations. Like Chinese handwriting, alphabetic
handwriting mostly involves the control and coordination
of the muscles of the fingers, hand and arm, subject to
visual guidance and monitoring (
). With the softness of a Chinese
brush, rather than ball pen, fountain pen, pencil, etc., the
calligraphic effect, which transforms the flat surface into
an imaginary 3-dimensional reality, could be produced.
4.4. Study limitations and future directions
One major limitation of the current study was that
although calligraphy has its roots in orient culture, there
are difficulties to generalize to other cultures, for people
who are unfamiliar with its use, may feel stressful to
conduct it. However, some pioneers in western and Arabic
culture had shown great interest in English-letter (Arabic)
calligraphy & handwriting recently (
). The second limitation was the small numbers
per group mean, so the analysis should be considered
exploratory. The third one was related to the intervention
procedure. Because we had limited knowledge regarding
whether different calligraphic character style and hand-
writing preference would be associated with different
clinical outcomes, it might be valuable to assess those
X.-L. Yang et al. / International Journal of Nursing Studies 47 (2010) 550–559
557

hypotheses in future researches. Finally, the high refusal
rate indicated that the applicability of psychotherapy in
Chinese cancer patients should be carefully considered
before the initiation of intervention programs. The reasons
of the high refusal rate in this study might be related to the
facts that the Chinese were more likely to present
emotions as physical symptoms (
), to
inhibit outward expression of negative emotions (
), and to refuse help for their psychological
problems (
), these characteristics of Chinese
cancer patients might compromise their perceived effec-
tiveness and acceptance of psychotherapy. Nevertheless,
the reasonable dropout rate suggested the programs were
easy to comply, could substantially benefit the patients
with high motives and resolution. We recommend future
researchers to test out the long-term effects of calligraphy
in terms of quality of life, spiritual well-being, and disease
progression. Furthermore, efforts also were needed to
disseminate efficacious components of calligraphy prac-
tice in future studies.
5. Conclusions
Similar to the effect of relaxation training, calligraphy
demonstrated a gradually build-up physiological slow-
down, and associated with heightened concentration and
improved mood disturbance. Calligraphy was inexpensive,
easy to practice, and involved an innate art appreciation
and cognitive facilitation process. Calligraphy handwriting
offered a promising approach to improved health in cancer
patients.
Acknowledgments
This study was supported by the staff in Cancer Centre,
Sun Yat-Sen University, China. Heartfelt thanks are given
to all the men and women who participated in the study,
whose enthusiasm continues to inspire us. Special thanks
are given to Dr Ruth McCorkle, Yale University School of
Nursing, who provided the valuable user’s manual for the
Symptom Distress Scale.
Conflict of interest: None declared.
Funding: Not applicable.
Ethical approval: Ethical approval for this study was approved
by the Review Board of the investigator’s institution.
References
Baldacchino, D.R., Buhagiar, A., 2003. Psychometric evaluation of the
Spiritual Coping Strategies scale in English, Maltese, back-translation
and bilingual versions. J. Adv. Nurs. 42 (6), 558–570.
Bernstein, D.A., Borkovec, T.D., 1973. Progressive Relaxation Training: A
Manual for the Helping Professions. Research Press, Champaign, Ill.
Cao, S.M., Guo, X., Li, N.W., Xiang, Y.Q., Hong, M.H., Min, H.Q., 2006.
Clinical analysis of 1,142 hospitalized Cantonese patients with naso-
pharyngeal carcinoma. Ai Zheng 25 (2), 204–208.
Cheung, Y.L., Molassiotis, A., Chang, A.M., 2003. The effect of progressive
muscle relaxation training on anxiety and quality of life after stoma
surgery in colorectal cancer patients. Psychooncology 12 (3), 254–
266.
Cheung, Y.L., Molassiotis, A., Chang, A.M., 2001. A pilot study on the effect
of progressive muscle relaxation training of patients after stoma
surgery. Eur. J. Cancer Care (Engl.) 10 (2), 107–114.
Chi, S., Lin, W.J., 2003. The preliminary revision of Brief Profile of
Mood States (BPOMS)-Chinese Edition. Chin. J. Ment. Health 17
(11), 767–770.
Degner, L.F., Sloan, J.A., 1995. Symptom distress in newly diagnosed
ambulatory cancer patients and as a predictor of survival in lung
cancer. J. Pain Symptom Manage. 10 (6), 423–431.
Frederickson, K., Jackson, B.S., Strauman, T., Strauman, J., 1991. Testing
hypotheses derived from the Roy Adaptation Model. Nurs. Sci. Q. 4 (4),
168–174.
Gaur, A., Keith, B., 2006a. Calligraphy, East Asian. In: Encyclopedia of
Language & Linguistics, Elsevier, Oxford, pp. 177–179.
Gaur, A., Keith, B., 2006b. Calligraphy, Islamic. In: Encyclopedia of Lan-
guage & Linguistics, Elsevier, Oxford, pp. 178–179.
Gaur, A., Keith, B., 2006c. Calligraphy, Western, Modern. In: Encyclopedia
of Language & Linguistics, Elsevier, Oxford, pp. 181–187.
Gotze, H., Geue, K., Buttstadt, M., Singer, S., Schwarz, R., 2009. Art therapy
for cancer patients in outpatient care. Psychological distress and
coping of the participants. Forsch. Komplementmed. 16 (1), 28–33.
Greene, F.L., 2002. The American Joint Committee on Cancer: updating the
strategies in cancer staging. Bull. Am. Coll. Surg. 87 (7), 13–15.
Guo, N.F., Kao, H.S.R., Liu, X., 2001. Calligraphy, hypertension and the
type-A personality. Ann. Behav. Med. 23 S2001, S159.
Huang, H.Y., Wilkie, D.J., Chapman, C.R., Ting, L.L., 2003. Pain trajectory of
Taiwanese with nasopharyngeal carcinoma over the course of radia-
tion therapy. J. Pain Symptom Manage. 25 (3), 247–255.
Huang, H.Y., Wilkie, D.J., Schubert, M.M., Ting, L.L., 2000. Symptom profile
of nasopharyngeal cancer patients during radiation therapy. Cancer
Pract. 8 (6), 274–281.
Jones, G., 2000. An art therapy group in palliative cancer care. Nurs. Times
96 (10), 42–43.
Kao, H.S., Ding-Guo, G., Danmin, M., Xufeng, L., 2004. Cognitive facilitation
associated with Chinese brush handwriting: the case of symmetric
and asymmetric Chinese characters. Percept. Mot. Skills 99 (3 Pt 2),
1269–1273.
Kao, H.S.R. (Ed.), 2000. Chinese Calligraphy Therapy. Hong Kong Uni-
versity Press, Hong Kong, pp. 3–42.
Kao, H.S.R., 2003. Chinese calligraphy handwriting for health and reha-
bilitation of the elderly. In: Second World Congress of the Interna-
tional Society of Physical and Rehabilitation Medicine. Prague, May
18–22, 2003 Book of Abstracts, p. 63.
Kao, H.S.R., 2006. Shufa: Chinese calligraphic handwriting (CCH) for
health and behavioral therapy. Int. J. Psychol. 41 (4), 282–286.
Kao, H.S.R., Chen, C.C., Chang, T.M., 1997. The effect of calligraphy practice
on character recognition reaction time among children with ADHD
disorder. In: Roth, R. (Ed.), Psychologists Facing the Challenge of a
Global Culture with Human Rights and Mental Health. Proceedings of
the 55th Annual Convention of the Council of Psychologists, Graz,
Austria, July 14–18, 1997, pp. 45–49.
Kao, H.S.R., Gao, D., Wang, M., 2000a. Brush handwriting treatment of
cognitive deficiencies in Alzheimer’s disease patients. Neurobiol.
Aging 21 1s, 14.
Kao, H.S.R., Gao, D., Wang, M., Cheung, H.Y., Chiu, J., 2000b. Chinese
calligraphic handwriting: treatment of cognitive deficiencies of Alz-
heimer’s disease patients. Alzheimer’s Rep. 3, 281–287.
Kao, H.S.R., Guo, N.F., Liu, X., 2001. Effects of calligraphic practice on EEG
and blood pressure in hypertensive patients. Ann. Behav. Med. 23,
S085.
Kao, H.S.R., Hoosain, R., Van Galen, G.P. (Eds.), 1986a. Graphonomics:
Contemporary Research in Hand Writing. North-Holland, Amster-
dam, p. 403.
Kao, H.S.R., Mak, P.H., Lam, P.W., 1986b. Handwriting pressure: effects of
task complexity, control mode and orthographic differences. In: Kao,
H.S.R., van Galen, G.P., Hoosain, R. (Eds.), Graphonomics: Contempor-
ary Research in Handwriting. North-Holland, Amsterdam, pp. 47–66.
Karnofsky, D.A., Burchenal, J.H., 1949. The clinical evaluation of che-
motherapeutic agents in cancer. In: MacLeod, C.M. (Ed.), Evaluation
of Chemotherapeutic Agents. Columbia Univ Press.
Lai, Y.H., Chang, J.T., Keefe, F.J., Chiou, C.F., Chen, S.C., Feng, S.C., Dou, S.J.,
Liao, M.N., 2003. Symptom distress, catastrophic thinking, and hope
in nasopharyngeal carcinoma patients. Cancer Nurs. 26 (6), 485–493.
Lehrer, P.M., 1978. Psychophysiological effects of progressive relaxation
in anxiety neurotic patients and of progressive relaxation and alpha
feedback in nonpatients. J. Consult. Clin. Psychol. 46 (3), 389–404.
Leon-Pizarro, C., Gich, I., Barthe, E., Rovirosa, A., Farrus, B., Casas, F., Verger,
E., Biete, A., Craven-Bartle, J., Sierra, J., Arcusa, A., 2007. A randomized
trial of the effect of training in relaxation and guided imagery tech-
niques in improving psychological and quality-of-life indices for
X.-L. Yang et al. / International Journal of Nursing Studies 47 (2010) 550–559
558

gynecologic and breast brachytherapy patients. Psychooncology 16
(11), 971–979.
Luebbert, K., Dahme, B., Hasenbring, M., 2001. The effectiveness of
relaxation training in reducing treatment-related symptoms and
improving emotional adjustment in acute non-surgical cancer treat-
ment: a meta-analytical review. Psychooncology 10 (6), 490–502.
Lyles, J.N., Burish, T.G., Krozely, M.G., Oldham, R.K., 1982. Efficacy of
relaxation training and guided imagery in reducing the aversiveness
of cancer chemotherapy. J. Consult. Clin. Psychol. 50 (4), 509–524.
McCallie, S.M., Blum, M.C., Hood, J.C., 2006. Progressive muscle relaxation.
J. Hum. Behav. Soc. Environ. 13 (3), 51–66.
McCorkle, R., Jepson, C., Malone, D., Lusk, E., Braitman, L., Buhler-Wilk-
erson, K., Daly, J., 1994. The impact of posthospital home care on
patients with cancer. Res. Nurs. Health 17 (4), 243–251.
McCorkle, R., Young, K., 1978. Development of a symptom distress scale.
Cancer Nurs. 1 (5), 373–378.
Monti, D.A., Peterson, C., Kunkel, E.J., Hauck, W.W., Pequignot, E., Rhodes,
L., Brainard, G.C., 2006. A randomized, controlled trial of mindfulness-
based art therapy (MBAT) for women with cancer. Psychooncology 15
(5), 363–373.
Morin, C.M., Hauri, P.J., Espie, C.A., Spielman, A.J., Buysse, D.J., Bootzin, R.R.,
1999. Nonpharmacologic treatment of chronic insomnia. An Amer-
ican Academy of Sleep Medicine review. Sleep 22 (8), 1134–1156.
Mumford, D.B., 1995. Cultural issues in assessment and treatment. Curr.
Opin. Psychiatry 8, 134–137.
Nunes, D.F., Rodriguez, A.L., da Silva Hoffmann, F., Luz, C., Braga Filho, A.P.,
Muller, M.C., Bauer, M.E., 2007. Relaxation and guided imagery pro-
gram in patients with breast cancer undergoing radiotherapy is not
associated with neuroimmunomodulatory effects. J. Psychosom. Res.
63 (6), 647–655.
Pan, J.J., Zhang, S.W., Chen, C.B., Xiao, S.W., Sun, Y., Liu, C.Q., Su, X., Li, D.M.,
Xu, G., Xu, B., Lu, Y.Y., 2009. Effect of recombinant adenovirus-p53
combined with radiotherapy on long-term prognosis of advanced
nasopharyngeal carcinoma. J. Clin. Oncol. 27 (5), 799–804.
Ragsdale, D., Morrow, J.R., 1990. Quality of life as a function of HIV
classification. Nurs. Res. 39 (6), 355–359.
Sheu, S., Irvin, B.L., Lin, H.S., Mar, C.L., 2003. Effects of progressive muscle
relaxation on blood pressure and psychosocial status for clients with
essential hypertension in Taiwan. Holist. Nurs. Pract. 17 (1), 41–47.
Su, R.V., Chen, C.C., 1979. Diagnostic and therapeutic implications of
Chinese calligraphy in psychiatric occupational therapy (author’s
transl). Taiwan Yi Xue Hui Za Zhi 78 (4), 419–432.
Sung, B.H., Roussanov, O., Nagubandi, M., Golden, L., 2000. Effectiveness
of various relaxation techniques in lowering blood pressure asso-
ciated with mental stress. Am. J. Hypertension 13 (4, Suppl. 1),
S185–S1185.
Svensk, A.C., Oster, I., Thyme, K.E., Magnusson, E., Sjodin, M., Eisemann,
M., Astrom, S., Lindh, J., 2009. Art therapy improves experienced
quality of life among women undergoing treatment for breast
cancer: a randomized controlled study. Eur. J. Cancer Care (Engl.)
18 (1), 69–77.
Van Galen, G.P., Teulings, H.L., 1983. The independent monitoring of form
and scale factors in handwriting. Acta Psychologica 54, 9–22.
Visser, A., Op’t Hoog, M., 2008. Education of creative art therapy to cancer
patients: evaluation and effects. J. Cancer Educ. 23 (2), 80–84.
Walker, L.G., Walker, M.B., Ogston, K., Heys, S.D., Ah-See, A.K., Miller,
I.D., Hutcheon, A.W., Sarkar, T.K., Eremin, O., 1999. Psychological,
clinical and pathological effects of relaxation training and guided
imagery during primary chemotherapy. Br. J. Cancer 80 (1–2), 262–
268.
Wang, J.P., Chen, H.Y., Su, W.L., 2004. Reliability and validity of Profile of
Mood State-Short Form in Chinese patients. Chin. J. Ment. Health 18
(6), 404–407.
Wen, S.L., Zhang, J.B., Ye, M.Z., Han, Z.L., Tao, J., 2000. Mental health status
of patients with nasopharyngeal carcinoma. Chin. J. Clin. Psychol. 8
(1), 52–54.
Ying, Y.W., Lee, P.A., Tsai, J.L., Yeh, Y.Y., Huang, J.S., 2000. The conception of
depression in Chinese American college students: cultural diversity
and ethnic minority. Psychology 6, 183–195.
Ying, Y., 1997. Psychotherapy for East Asian Americans with major
depression. In: Lee, E. (Ed.), Working with Asian Americans: A Guide
for Clinicians. NY7 Guilford Press, pp. 252–264.
Yoo, H.J., Ahn, S.H., Kim, S.B., Kim, W.K., Han, O.S., 2005. Efficacy of
progressive muscle relaxation training and guided imagery in redu-
cing chemotherapy side effects in patients with breast cancer and in
improving their quality of life. Support. Care Cancer 13 (10), 826–833.
Young-Mason, J., 2003. Alhabeeb’s calligraphy ‘‘Peace and beauty’’: a
bridge to understanding. Clin. Nurse Spec. 17 (2), 112–113.
X.-L. Yang et al. / International Journal of Nursing Studies 47 (2010) 550–559
559
Document Outline
- The effects of Chinese calligraphy handwriting and relaxation training in Chinese Nasopharyngeal Carcinoma patients: A randomized controlled trial
Wyszukiwarka
Podobne podstrony:
A systematic review and meta analysis of the effect of an ankle foot orthosis on gait biomechanics a
Glińska, Sława i inni The effect of EDTA and EDDS on lead uptake and localization in hydroponically
the effect of interorganizational trust on make or cooperate decisions deisentangling opportunism de
Ebsco Cabbil The Effects of Social Context and Expressive Writing on Pain Related Catastrophizing
Microwave drying characteristics of potato and the effect of different microwave powers on the dried
The Effects of Performance Monitoring on Emotional Labor and Well Being in Call Centers
the effect of sowing date and growth stage on the essential oil composition of three types of parsle
Junco, Merson The Effect of Gender, Ethnicity, and Income on College Students’ Use of Communication
On Computer Viral Infection and the Effect of Immunization
The Effects of Probiotic Supplementation on Markers of Blood Lipids, and Blood Pressure in Patients
the effect of water deficit stress on the growth yield and composition of essential oils of parsley
Kowalczyk Pachel, Danuta i inni The Effects of Cocaine on Different Redox Forms of Cysteine and Hom
The effects of handwriting experience on functional brain
The effects of plant flavonoids on mammalian cells implication for inflammation, heart disease, and
Sailing Yacht Performance The Effects of Heel Angle and Leeway Angle on Resistance
76 1075 1088 The Effect of a Nitride Layer on the Texturability of Steels for Plastic Moulds
Curseu, Schruijer The Effects of Framing on Inter group Negotiation
Evidence for the formation of anhydrous zinc acetate and acetic
więcej podobnych podstron