Pathological dissociation and
neuropsychological functioning in borderline
personality disorder
Introduction
Borderline personality disorder (BPD) is charac-
terized by disturbed relational abilities, affective
dysregulation, lack of behavior control and dis-
turbed
cognition
(1–3).
Disturbed
cognition
includes dissociative symptoms, non-delusional
suspiciousness
and
quasi-psychotic
symptoms.
Although neurocognitive impairment has been
suggested to act as a moderator in the develop-
ment of the disorder (4), only a few studies have,
with a variety of results, been devoted to the
Haaland VØ, Landrø NI. Pathological dissociation and
neuropsychological functioning in borderline personality disorder.
Objective: Transient, stress-related severe dissociative symptoms or
paranoid ideation is one of the criteria defining the borderline
personality disorder (BPD). Examinations of the neuropsychological
correlates of BPD reveal various findings. The purpose of this study
was to investigate the association between dissociation and
neuropsychological functioning in patients with BPD.
Method: The performance on an extensive neuropsychological
battery of patients with BPD with (n = 10) and without (n = 20)
pathological dissociation was compared with that of healthy controls
(n = 30).
Results: Patients with pathological dissociation were found to have
reduced functioning on every neuropsychological domain when
compared with healthy controls. Patients without pathological
dissociation were found to have reduced executive functioning, but no
other differences were found.
Conclusion: Pathological dissociation is a clinical variable that
differentiates patients with BPD with regard to cognitive functioning.
V. Ø. Haaland
1,2
, N. I. Landrø
2
1
Department of Psychiatry, Sørlandet Hospital HF,
Kristiansand, Norway and
2
Center for the Study of
Human Cognition, Department of Psychology, University
of Oslo, Oslo, Norway
Key words: personality disorders; dissociation;
cognition; cognitive science; neuropsychology
Vegard Øksendal Haaland, Sørlandet sykehus HF,
Psykiatrisk avdeling, Serviceboks 416, N-4604
Kristiansand, Norway.
E-mail: vegard.oksendal.haaland@sshf.no
Accepted for publication November 7, 2008
Significant outcomes
•
This study reports deficits in executive functioning, working memory and long-term verbal memory
performance in a subgroup of patients with BPD and pathological dissociation compared with that
in patients with BPD without pathological dissociation.
•
Patients with BPD who also show pathological dissociation seem to represent a more severely
disturbed subgroup of patients with BPD.
•
Pathological dissociation is a clinically important and relatively easily assessable psychopathological
variable.
Limitations
•
The sample is relatively small, a factor that in particular influences the size of the subgroup of
patients demonstrating pathological dissociation.
•
Dissociation is investigated both as a trait and as a categorical variable. The effect of dissociative
states per se is not studied.
Acta Psychiatr Scand 2009: 119: 383–392
All rights reserved
DOI: 10.1111/j.1600-0447.2008.01323.x
Copyright
2008 The Authors
Journal Compilation
2008 Blackwell Munksgaard
ACTA PSYCHIATRICA
SCANDINAVICA
383

neuropsychological functioning of persons with
BPD. A recent review of neuropsychological cor-
relates of BPD suggests the existence of several
neuropsychological deficits (5). These deficits are
particularly pertinent to executive functions. Still,
more research would be needed to examine vari-
able results with regard to other neuropsycholog-
ical functions.
Dissociation can be defined as a disruption in the
usually integrated functions of consciousness,
memory, identity and perception (3). The occur-
rence of Ôtransient, stress-related severe dissociative
symptoms or paranoid ideationÕ is a defining
criterion of BPD that was added to the current
version of Diagnostic and Statistical Manual
(DSM) (3). This criterion, which occurs in
around 75% of patients with BPD, shows excellent
specificity (1). According to the DSM-IV, disso-
ciative symptoms in patients with BPD are in
particular associated with situations with high
levels of stress (3), a relation that has been
demonstrated experimentally (6, 7).
Dissociative experiences also occur in the
general population (8) and measures like the
Dissociative Experiences Scale (DES) assess dis-
sociation as a continuous variable or a trait (9).
However, some studies indicate that dissociative
experiences are not uniformly distributed in
clinical groups the way a dimensional model of
dissociation would imply. Differences in mean
dissociative scores between different diagnostic
groups seem to depend on differences in the
frequency of high-dissociative individuals (10). A
taxometric analysis of dissociative experiences
revealed that two types of dissociation exists
(11). Non-pathological dissociation occurs along
a continuum and is considered a manifestation
of a dimensional construct or a dissociative
trait. Pathological dissociation is considered a
manifestation of a latent class variable or a
taxon.
Recent research has increasingly tended to
focus on associations between cognition and
dissociation. Non-pathological dissociation has
in this context been approached as a fundamen-
tal information-processing mechanism (12). Few
studies have focused on cognition and dissocia-
tion in clinical populations except for dissociative
disorders and none of those have focused on
pathological dissociation. In a sample of forensic
inpatients, a negative correlation was found
between executive test performance and dissocia-
tive symptoms (13). In patients with BPD,
dissociative
symptoms
have
been
related
to
difficulties in recalling specific autobiographic
memories (14).
Aims of the study
We sought to investigate associations between
dissociation and neuropsychological functioning
in patients with BPD. Our focus was on correla-
tions between total dissociative experiences and
neuropsychological performance, as well as on
comparison of the neuropsychological functioning
of patients with BPD with and without patholog-
ical dissociation with the performance of healthy
controls.
Material and methods
Participants with borderline personality disorder
This study was approved by the Regional Commit-
tee for Medical Research Ethics, and written
informed consent was obtained after the partici-
pants had been provided with a complete description
of the study. The sample consisted of 35 patients,
recruited through in- and outpatient settings from
different units of the Clinic for Mental Health –
Psychiatry and Dependency treatment at Sørlandet
Hospital HF – a general hospital in southern
Norway serving a population of about 265 000.
We aimed for a sample of patients with BPD who
may be considered representative of subjects in an
inpatient or outpatient setting. Knowing that com-
orbidity for axis I and axis II disorders is frequent in
patients with BPD (15, 16), we sought to limit the
exclusion criteria so as to include patients with the
most common comorbid disorders such as depres-
sion and post-traumatic stress disorder (PTSD).
Patients had to be between 18 and 40 years of age
and were required to fulfill the DSM-IV (3) criteria
for BPD. Exclusion criteria were a history of head
trauma or epilepsy, significant neurological findings,
mental retardation and ongoing substance abuse. A
total of 47 patients were recruited for evaluation; of
these, 12 did not fulfill the criteria and five had not
completed the clinical measure for dissociative
experiences (DES). These were excluded from the
study, leaving the final clinical sample with a total of
30 patients. Twenty-six patients were diagnosed
with lifetime affective disorder – 10 in remission, 16
with PTSD, 11 with an anxiety disorder other than
PTSD, 9 with another personality disorder and 6
with substance abuse. All but six patients were
taking psychotropic medications of which the most
common were SSRIs and atypical antipsychotics.
Healthy controls
Thirty-one non-clinical comparison subjects were
recruited among non-healthcare employees at the
Haaland and Landrø
384

hospital, students having practicum at the hospital,
through newspaper advertisement or among friends
and relatives of the staff of the hospital. In addition
to the exclusion criteria that applied to the patient
group, selection criteria for the healthy controls
were no history of availing psychiatric services, no
history of psychotropic medication and no history
which indicated psychiatric disorders.
Clinical and diagnostic assessments
Diagnoses were established using the structured
clinical interviews for DSM-IV SCID-I (17) and
SCID-II (18) conducted by one of the authors
(V.Ø.H.). Twenty of the interviews with potentially
participating patients were videotaped. The rating
was repeated by an external experienced clinical
psychologist who was unaware as to whether the
patients were included in the study or not. The
inter-rater agreement for the ratings of the nine
criteria for BPD was found to be good (average
CohenÕs j = 0.640). Depression was measured
with the Hamilton Depression Rating Scale (19),
global functioning by the Global Assessment of
Functioning Scale (GAF) (3), whereas dissociative
symptoms were measured using the Norwegian
version of the DES (9) a 28-item rating scale where
each item is scored from 0 to 100. Individuals with
pathological dissociation can be identified using
eight items from the DES, the DES-T (11).
Neuropsychological assessment
Every participant underwent an extensive battery of
intellectual and neuropsychological tests, where
most cognitive domains were covered with several
tests to obtain stable and robust measures. Domains
covered included attention, working memory, exec-
utive functions, verbal and non-verbal long-term
memory, and general cognitive abilities. The neuro-
psychological battery was administered by a test
technician or a clinical psychologist trained in
standardized assessment. Participants were tested
individually, and the total time required for testing
was about 4 h divided into two sessions. The tasks
were given in the same order, and testing was
performed at the clinic in the same location for all
participants. The neuropsychological test battery
with definitions of the variables used grouped by
cognitive domain is presented in Table 1.
Measures of attention
The Digit Symbol-Coding subtest from WAIS-III
(20) and the Conners Continuous Performance
Test II (CPT-II) (21) were used as measures of
attention. In the Digit Symbol-Coding subtest,
symbols must be matched and drawn as fast as
possible under the corresponding digit. The CPT-II
asks participants to monitor a random series of
single letters, presented continuously at different
rates on a monitor. The space bar has to be pressed
when a letter is presented except for the letter ÔxÕ.
Measures of working memory
The Digit Span subtest from WAIS-III (20), a
variant of the Paced Auditory Serial Addition Test
Table 1. Test battery used to assess neuropsychological and intellectual perfor-
mance grouped by cognitive domain
Neuropsychological domain and constituent items
Variables
Attention
Digit Symbol-Coding (WAIS-III) (20)
Total raw score
Conner Continuous
Performance Test (21)
Omissions; hit reaction time –
by block
Working memory
Digit Span (WAIS-III) (20)
Total raw score
Paced Auditory Serial Addition Test (22)
Number of correct responses
Letter Number Span (23)
Number of correct responses
n-Back (24)
Number of correct responses
in each of the 1–3 back
conditions
Executive functions
Stroop Color-Word Test (25)
Stroop interference score:
time to read incongruent
list minus time to read
congruent list
Tower of London (TOL-4) (26)
0–3 points dependent of
number of trials to solve
each problem. Total score
was the sum of points over
all 10 problems
Controlled Oral Word Association (27)
Semantic and phonetic fluency
Wisconsin Card Sorting Test (28)
Percent preservative errors
Trail Making Test (29)
Flexibility index [trail B (time)
minus trail A (time)]
Iowa Gambling Task (30)
Number of choices from the
advantageous decks minus
the number of choices from
the disadvantageous decks
Verbal long-term memory
Hopkins Verbal Learning Test (32)
Learning score: sum for trials
1–3; immediate free recall;
delayed free recall,
after 20 min
Visual long-term memory
Rey–Osterrieth Complex Figure (29)
Immediate recall; delayed
recall, after 20 min; item
recognition with
50% distractors
Kimura Recurring Recognition
Figures Test (33)
Number of correct responses
General cognitive ability
Picture Arrangement (WAIS-III) (20)
Total raw score
Block Design (WAIS-III) (20)
Total raw score
Picture Completion (WAIS-III) (20)
Total raw score
Vocabulary (WAIS-III) (20)
Total raw score
Similarities (WAIS-III) (20)
Total raw score
WAIS-III, Wechsler Adult Intelligence Scale 3 edition.
Dissociation and cognition in BPD
385

(PASAT) (22), the Letter Number Span (LNS) (23)
and the n-back task (24) were used as measures of
working memory. In the Digit Span subtest, series
of orally presented numbers must be repeated
verbatim and in reverse. In PASAT (22), 60 CD-
recorded digits are presented at a rate of 3.0 s.
Participants are required to add each number to
the one that immediately precedes it, and articulate
the new number promptly. In the LNS (23), orally
presented sequences of letters and numbers must be
sorted and presented by listing numbers in ascend-
ing order and letters in alphabetical order. In the
n
-back task (24), the numbers 2, 4, 6 or 8 are
displayed randomly on a computer screen. The
task is to respond on the keyboard with the
number presented n positions back in the sequence.
In our study, four conditions were used, 0-, 1-, 2-
and 3-back. Participants completed three trials in
each condition, with 14 stimuli per trial.
Measures of executive functions
The Stroop Color-Word Test (25), a version of the
Tower of London (TOL-4) (26), the Controlled Oral
Word Association Test (COWA) (27), the Wiscon-
sin Card Sorting Test (WCST) (28), the Trail
Making Tests (TMT) (29) and the Iowa Gambling
Task (IGT) were used (30) as measures of executive
functions. The Stroop Color-Word Test (25) con-
sists of three white cards, each containing a 6
· 8
matrix of stimulus. The critical part of the test
involves inhibition of response to color words
printed in incongruently colored inks. The TOL-4
(26) is a problem-solving task involving forward
planning to match arrangements of colored balls.
The COWA (27) is a measure of phonetic and
semantic verbal fluency requiring the ability to
generate words beginning with the letters F, A and S
and words in the categories of animals and cloths,
each in 1 min. In the WCST (28) the principles
according to which a deck of cards must be sorted
has to be discovered. In TMT-A (29), lines have to
be drawn sequentially connecting 25 encircled
numbers distributed on a sheet of paper. In TMT-
B, the participants must alternate between numbers
and letters. A computerized version of IGT was used
(30). IGT is a decision-making task under condi-
tions of limited knowledge about reward and
penalty, involving choices from advantageous and
disadvantageous decks of cards.
Measures of verbal long-term memory
The Hopkins Verbal Learning Test – Revised
(HVLT-R) (31, 32) was used as a measure of verbal
long-term memory. This is a classical word list
learning task with a 12-item list, and three succes-
sive learning trials.
Measures of visual long-term memory
The Kimura Recurring Recognition Figures Test
(33) and the Rey Complex Figure Test (RCFT) (29)
were used as measures of visual long-term memory.
The Kimura (33) is a continuous recognition task
that involves recognizing 20 cards containing previ-
ously learned drawn figures among 100 cards which
are presented one by one. The RCFT (29) was used
along with a recognition task. It involves copying
and recalling a complex geometric figure. The
scoring of the figures followed the 36-point scoring
system described by Lezak (29).
Measures of general cognitive ability
The Vocabulary, Block Design, Picture Completion,
Picture Arrangement and the Similarities subtests
from WAIS-III (20) were used as measures of
general cognitive ability. In the subtest Picture
Arrangement, cartoon-type pictures must be rear-
ranged to make a logical story sequence. In Block
Design, a set of blocks has to be arranged to replicate
various patterns. In Picture Completion, the most
important part missing in each of a set of color
pictures has to be identified. The Vocabulary subtest
asks participants to define orally and visually
presented words, whereas in the Similarities subtest
they are asked to explain the similarity between pairs
of words. The original scoring procedure was used.
Statistical analysis
Data analysis was completed by means of spss 16.0
(SPSS Inc., Chicago, IL, USA). The DES-T (11)
score was computed and the clinical sample was
divided into a group belonging to the pathological
dissociation taxon and a group not belonging to
the pathological dissociation taxon. Pathological
taxon membership was determined by calculating
Bayesian posterior taxon membership probabilities
according to procedures described by Waller and
Ross (34). Analyses of variance (anova) and chi-
squared tests were used to compare the three
groups regarding demographic variables whereas
t
-tests and chi-squared tests were used to compare
the two clinical groups regarding clinical variables.
For the purpose of analysis, all neuropsycholog-
ical scores were transformed into standardized
scores based on the mean values and standard
deviations of the whole clinical sample. The stan-
dardized measures were grouped into five different
cognitive domains and summary scores were
Haaland and Landrø
386

computed. Prorated IQ was computed using the
sum of the scaled scores of those five subtests
multiplied with 11
⁄ 5 as raw score. Table 1 presents
the constituent test scores in each cognitive
domain. The correlations between the neuropsy-
chological domains and the DES and DES-T
scores in the clinical group were computed using
PearsonÕs r. The pathological taxon group and the
non-pathological taxon group were compared with
healthy controls with respect to neuropsychologi-
cal performance by the use of a multivariate
analysis of variance (manova) followed up with
anova
s. Where significant effects were demon-
strated, post hoc pairwise comparisons were con-
ducted using Bonferroni adjustments in order to
correct for multiple comparisons. Effect sizes were
also computed for those differences.
Results
Taxon membership
The computation of Bayesian posterior taxon
membership probabilities resulted in 10 taxon
members with pathological dissociation and 20
non-members among the patients with BPD. One
healthy control participant was also identified as a
taxon member and was excluded from further
analysis. The probability for every participant in
the remaining healthy control group was 0.04%
(the lowest possible value) indicating no scores
above cut-off for any of the DES-T items for any of
the participants. For the non-member patient
group, the average membership probability was
1.9% (range 0.04–7.0%), and for the member
group 89% (range 72.5–100%), indicating no
uncertainty with respect to membership status.
Demographic characteristics
Table 2 displays the mean values and standard
deviations in demographic and clinical variables
for the three groups including results of statistical
comparisons. The groups were statistically similar
in terms of all demographic variables except for
participantsÕ educational level. Post hoc tests
(Scheffe´) indicated that both the taxon member
group (P = 0.004) and the non-taxon member
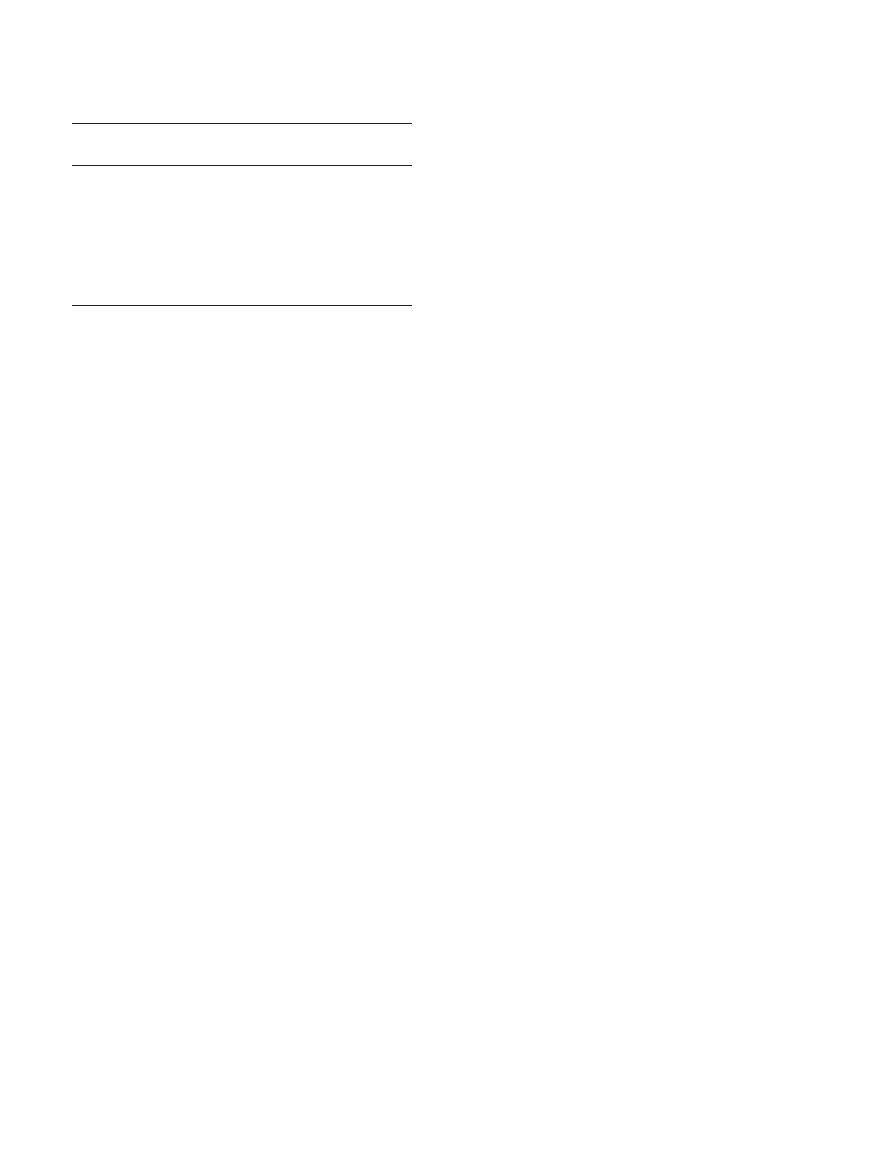
Table 2. Demographic and clinical characteristics, and neuropsychological test performance of patients with borderline personality disorder with and without pathological
dissociation, and healthy controls
BPD Non-DES-T
(n = 20)
BPD DES-T
(n = 10)
Healthy controls
(n = 30)
Analysis
Mean
SD
Mean
SD
Mean
SD
F
d.f.
P
Age (years)
25.5
5.6
23.7
4.8
25.9
6.4
0.52
2
0.597
Education (years)
12.9
2.6
12.0
1.6
14.8
2.1
8.18
2
0.001
MotherÕs education (years)
11.3
3.0
10.8
2.9
13.0
3.1
2.55
2
0.088
FatherÕs education (years)
12.9
4.5
12.2
3.5
13.8
3.0
0.77
2
0.471
t*
d.f.
P
Hamilton DRS
11.4
6.0
14.4
4.9
1.8
2.6
1.32
28
0.197
GAF
42.1
5.2
38.8
7.7
88.5
5.5
1.37
28
0.181
DES – total score
14.9
9.0
38.5
15.5
2.2
1.9
5.28
28
<0.001
DES – pathological
dissociation score
10.5
7.2
36.3
19.8
0.5
0.9
5.24
28
<0.001
n
%
n
%
n
%
v
2
d.f.
P
Gender
Male
4
20.0
0
0.0
4
13.3
Female
16
80.0
10
100.0
26
86.6
2.308
2
0.315
Handedness
Right
18
90.0
10
100.0
27
90.0
Left
2
10.0
0
0.0
3
10.0
1.550
2
0.461
Mean
SD
Mean
SD
Mean
SD
F
d.f.
P
Neuropsychological performance
Attention
0.25
0.41
)0.44
1.29
0.59
0.59
7.27
2, 51
0.002
Working memory
0.27
0.64
)0.33
0.84
0.67
0.54
10.06
2, 51
<0.001
Executive functions
0.26
0.40
)0.40
0.69
0.68
0.32
25.19
2, 51
<0.001
Verbal long-term memory
0.24
0.67
)0.46
1.19
0.44
0.55
7.83
2, 51
0.001
Visual long-term memory
0.25
0.61
)0.10
0.61
0.60
0.53
5.67
2, 51
0.006
Prorated IQ
100.9
12.3
87.2
12.9
113.7
11.4
20.90
2, 51
<0.001
DRS, Depression Rating Scale; GAF, Global Assessment of Functioning; DES, Dissociative Experiences Scale; BPD, Borderline Personality Disorder; DES-T, Dissociative
Experiences Scale pathological dissociation Taxon member.
*Comparisons between the two clinical groups.
Dissociation and cognition in BPD
387
group (P = 0.016) had a significantly lower edu-
cational level than the healthy control group. No
differences were found between the two clinical
groups (P = 0.543).
Clinical characteristics
Between the two clinical groups, the analysis
showed no differences with respect to scores on
the Hamilton Depression Rating Scale or on the
GAF scale (Table 2). The analysis revealed signif-
icant differences between the two groups on
dissociative experiences both on the DES total
score and on the DES-T score. There were no
differences between the two clinical groups in the
frequencies of affective disorders (v
2
= 0.144;
d.f. = 1;
P
= 0.704)
or
PTSD
(v
2
= 0.268;
d.f. = 1; P = 0.605).
Overall analysis of neuropsychological performance
When comparing the two clinical groups and the
healthy control group with manova (Wilks lambda),
we found an overall group difference in neuro-
psychological test performance [F(12,92) = 4.36,
P
< 0.001]. anova revealed significant differences
between the three groups in all neuropsychological
domains (Table 2).
Neuropsychological performance of patients with BPD with
pathological dissociation
Post hoc
pairwise comparisons with Bonferroni
adjustments
revealed
significant
differences
between patients with BPD with pathological
dissociation and the healthy control group on
every cognitive domain: attention (P = 0.001),
working memory (P < 0.001), executive function-
ing (P < 0.001), verbal long-term memory (P =
0.002), non-verbal long-term memory (P = 0.004)
and general cognitive functioning (P < 0.001).
Bias-corrected (HedgesÕ gˆ) effect sizes with 95%
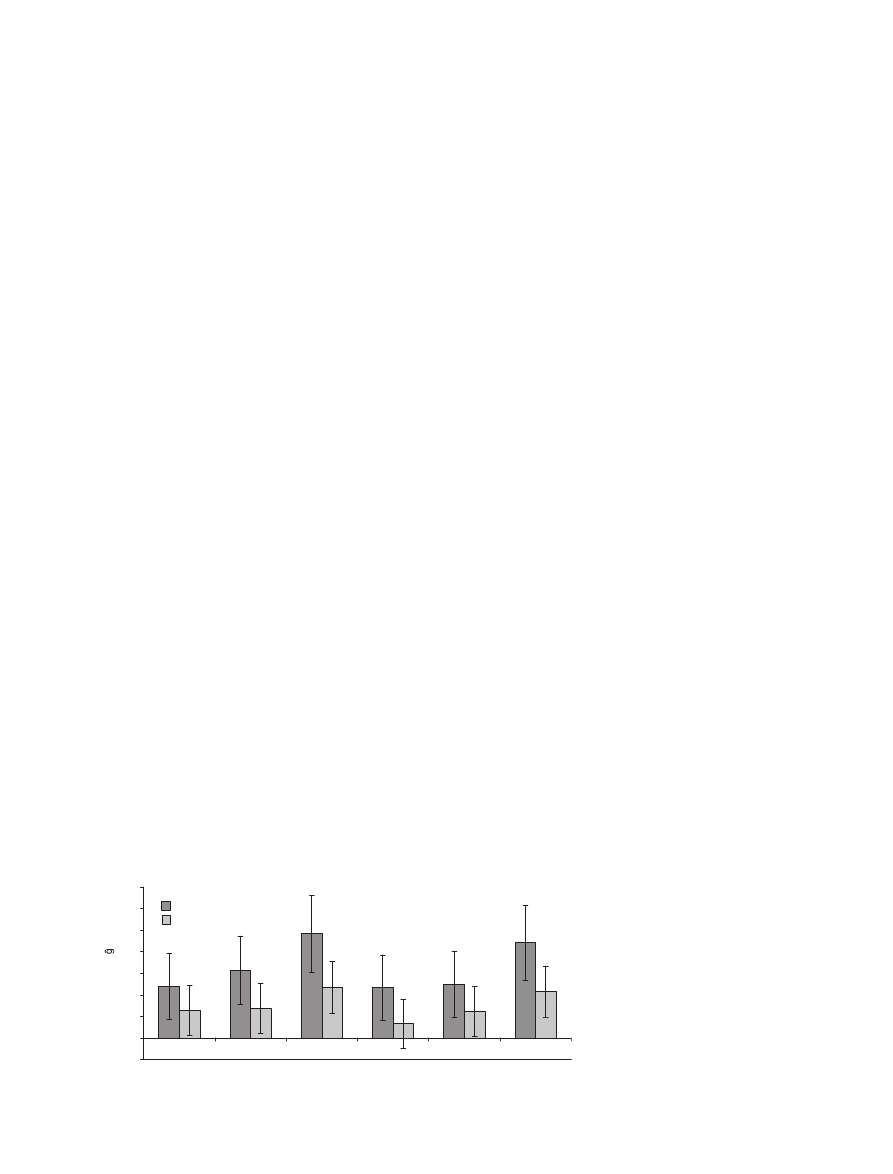
confidence intervals are presented in Fig. 1.
Neuropsychological performance of patients with BPD without
pathological dissociation
We found a significant difference between the
healthy controls and patients with BPD without
pathological dissociation on measures of executive
functioning (P = 0.004), but not on measures of
the other domains: attention (P = 0.388), working
memory (P = 0.307), verbal long-term memory
(P = 1.000),
non-verbal
long-term
memory
(P = 0.927) or general cognitive functioning
(P = 0.057). Bias-corrected (HedgesÕ gˆ) effect
sizes with 95% confidence intervals are presented
in Fig. 1.
Differences in neuropsychological performance between the
clinical groups
Patients with BPD without pathological dissocia-
tion showed better performance than patients with
BPD with pathological dissociation on measures of
working memory (P = 0.027), executive function-
ing (P = 0.002), verbal long-term memory (P =
0.002)
and
general
cognitive
functioning
(P = 0.001). No differences were found between
the two groups on measures of attention (P = 0.097)
or non-verbal long-term memory (P = 0.092).
Correlations between neuropsychological performance and
dissociation
In the combined clinical samples, there were
significant negative correlations between DES
total score and attention (r =
)0.56, P = 0.001),
and
between
DES-T
score
and
attention
(r =
)0.53, P = 0.003) and verbal long-term
memory (r =
)0.41, P = 0.025). Correlations
between the dissociation score and the other
–0.5
0
0.5
1
1.5
2
2.5
3
3.5
Attention Working
memory
Executive
functions
Verbal LTM
Visual LTM
IQ
Effect sizes, Hedges (adjusted)
BPD/DES-T
BPD/NON-DES-T
Fig. 1.
Effect sizes (with error bars
indicating 95% CIs) of the differences
between the groups of patients with
BPD with and without pathological
dissociation and the healthy control
group on every cognitive domain.
Haaland and Landrø
388
neuropsychological domains and between the dif-
ferent domains are presented in Table 3.
Discussion
The association between pathological dissociation and
neuropsychological performance
To our knowledge, this is the first study that
explores associations between pathological disso-
ciation as a categorical variable and neuropsycho-
logical performance in patients with BPD. Patients
with BPD and pathological dissociation were
found to have reduced executive functioning,
working memory and long-term verbal memory
performance when compared with patients with
BPD without pathological dissociation. With
regard to the neuropsychological domains of
attention and long-term non-verbal memory, no
differences were found between the two groups.
When compared with healthy controls, patients
with BPD with pathological dissociation showed
reduced performance on every cognitive domain,
whereas patients with BPD without pathological
dissociation showed only reduced executive func-
tioning. The only neuropsychological domain that
seems to be consistently impaired in patients with
BPD, regardless of pathological dissociation, is the
executive one; a finding that concurs with previous
research (5).
This study contributes to the understanding of
cognitive functioning of patients with BPD. Path-
ological dissociation might be a clinical variable
that differentiates patients with BPD with regard to
cognitive functioning. These results elaborate the
findings from earlier examinations of executive
functioning,
working
memory
and
long-term
verbal memory in BPD (35–44). Different propor-
tions of pathological dissociative patients in differ-
ent study samples may be one factor that accounts
for the variability of the findings. This clinical
characteristic may also plausibly account for the
fMRI findings which connect specific frontolimbic
neural substrates to behavioral dyscontrol in
patients with BPD (45).
The two groups also differed with respect to
general intellectual abilities. The score of the
group with pathological dissociation was more
than 1 SD lower than the group without
pathological dissociation. This is a crucial finding
that, along with the results regarding the other
cognitive domains, allow for several hypotheses.
First, one could argue that reduced cognitive
abilities enhance the probability of pathological
dissociation. Second, one could hypothesize that
there is a common factor to reduced cognitive
abilities and pathological dissociation; it could be
a question of traumatic experiences that, at a
certain stage, would effect neurobiological devel-
opment. Third, it is, of course, possible that the
pathological dissociative phenomena per se cause
reduced test performance, i.e. pathological disso-
ciation during test uptake conflicts with the tasks
solved. Nonetheless, pathological dissociation and
reduced working memory, executive functions,
long-term verbal memory performance and IQ
seem to be co-occurring in patients with BPD.
Correlations between non-pathological dissociation and
neuropsychological performance
When using a dimensional model of dissociation,
we found a significant negative correlation between
the total DES score and performance in the
attention domain, but not between DES score
and
performance
on
the
neuropsychological
domains of working memory, executive functions,
long-term verbal memory, long-term non-verbal
memory or IQ. When treating the DES-T as a
dimensional variable, it was found to be signifi-
cantly negatively correlated with attention as well
as with verbal long-term memory, but not with
performance on the other domains. These findings
are crucial for two reasons:
First, we found different associations between
dissociation and neuropsychological performance
when applying a dimensional model compared
with the results when applying a categorical model.
Dimensional dissociation was negatively related to
attention and verbal memory, while categorical
(pathological) dissociation was negatively related
to working memory, executive functions and verbal
memory. When taking the DES total score pri-
marily as a measure of non-pathological dissocia-
tion, this implies
that non-pathological and
pathological dissociation are related to different
Table 3. Correlations between performance on neuropsychological domains and
measures of dissociation in patients with borderline personality disorder
Working
memory
Executive
functions
Verbal
LTM
Visual
LTM
Prorated
IQ
DES
DES-T
Attention
0.41*
0.61**
0.60** 0.37
0.47**
)0.56** )0.53**
Working
memory
0.75**
0.48** 0.46**
0.74**
)0.35
)0.20
Executive
functions
0.47** 0.50**
0.65**
)0.38
)0.22
Verbal LTM
0.53**
0.58**
)0.34
)0.41*
Visual LTM
0.61**
)0.25
)0.24
Prorated IQ
)0.30
)0.25
DES
0.89**
LTM, Long-term memory, DES, Dissociative Experiences Scale – total score; DES-T
Dissociative Experiences Scale pathological dissociation score. Correlation is sig-
nificant at the *0.05 (two tailed) and **0.01 (two tailed) levels.
Dissociation and cognition in BPD
389
cognitive functions. When using the DES-T results
dimensionally, we found approximately the same
results as when we used the DES, indicating that
research based on DES-T dimensionally as a
measure of pathological dissociation may produce
different results compared with that of studies
treating pathological dissociation as a latent class
variable.
Second, these findings allow for interesting
comparisons with studies investigating the rela-
tionship between dissociation and cognition in
non-clinical samples. High-dissociative persons
have been found to have an advantage on different
cognitive tasks in some studies (12, 46–48), a
disadvantage on different cognitive tasks in other
studies (49–52), whereas some studies report no
differences between high and low dissociative
participants in tests of executive functions and
working memory (53, 54). Although not signifi-
cant, all the correlations in our sample were
negative, indicating a common direction. The
reason for this may be that we used domain results
of the neuropsychological performance rather than
results on single tests or single variables. Another
explanation may be that in a clinical sample like
ours, with high proportions of persons with patho-
logical dissociation, the possible advantageous
effect of non-pathological dissociation would be
overshadowed. Our results differ, however, from a
recent study which suggests that patients with
dissociative disorders present elevated frontal
function and enhanced working memory perfor-
mance (55). A possible, but perhaps not plausible,
explanation for this discrepancy in results could be
that dissociation is associated with reduced frontal
functions in patients with BPD, but with elevated
frontal function in patients with dissociative dis-
orders. Another possibility is that a diagnosis of
dissociative disorders not necessarily implies mem-
bership in the pathological taxon as measured with
the DES-T.
Dissociation and treatment outcome
Dissociative symptoms have been associated with
poorer outcome following psychotherapeutic treat-
ment in patients with panic disorder, agoraphobia
and obsessive–compulsive disorder, as well as in
patients with affective, anxiety or somatoform
disorders (56–58). Although these studies did not
include patients with BPD, our study may give a
hypothesis for a neuropsychological-based expla-
nation to the findings. We found both dimensional
and categorical measures of dissociation to be
associated
with
dysfunctions
in
fundamental
cognitive abilities. It may therefore not be the
dissociation per se that results in poorer outcome,
but the cognitive functioning of the patients
involved in those studies. Such a hypothesis,
however, is not entirely congruent with the results
presented in a recent study by Braakmann et al.
(59) in which no negative prognostic value was
found of dissociative symptoms on the effect of
inpatient Dialectic Behavior Therapy. The authorsÕ
hypothesis is that this is because of the specific
focus on dissociative symptoms facilitated by an
inpatient setting. Further studies on the treatment
of BPD should investigate the prognostic value of
neuropsychological variables as well as psycho-
pathological measures.
Limitations
The two groups of patients with BPD were
homogenous with respect to demographic and
clinical variables, including depressive symptoms
and GAF values, except for degree of dissociative
symptoms. One could argue that patients in the
pathological dissociation group also had a disso-
ciative disorder; however, as SCID-D was not used
in this study, we cannot give answer to this
question.
These
findings
may
therefore
be
explained by comorbidity alone, but another and
in our view more plausible explanation would be
that patients with BPD who also show pathological
dissociation represent a more severe subgroup of
patients with BPD. Such an interpretation is
supported by studies showing enhanced working
memory performance in patients with dissociative
disorders (55).
Most patients in our sample were taking psy-
chotropic medication when the tests were con-
ducted, and no steps were taken to reduce what
influences medication may have had. For SSRIs,
some positive effects have been found on neuro-
psychological performance in healthy subjects (60).
Atypical antipsychotics have been found to have
some negative effects on attention, but no effect on
executive functions in healthy subjects (61). Con-
sidering that patients in both groups used medica-
tion and that SSRIs and atypical neuroleptics were
the most frequently used medication in both
samples, it is unlikely that medication influences
would have caused the reduced neuropsychological
performance found in this study.
Given the high comorbidity of DSM-IV axis I
and II disorders in BPD (15, 16), comorbidity was
not a criterion for exclusion except for severe
ongoing substance abuse. PTSD and lifetime
affective disorders were the most frequent comor-
bid disorders. When comparing the two groups
with and without pathological dissociation, we
Haaland and Landrø
390

found no differences in frequency of those comor-
bid disorders. Average GAF scores indicated that
patients were moderately affected. Our sample may
therefore be considered representative of patients
in general clinical settings, and inferences may be
drawn from this sample to these patients, but not
necessarily to the patient group with BPD and no
comorbid disorders without psychotropic medica-
tion. Future studies should take the effect of
comorbidity and medications systematically into
consideration.
Studies similar to ours, in which neuropsycho-
logical measures and its relations to psychopatho-
logical phenomenon are investigated, may expand
our understanding of the behavioral characteristics
of various psychiatric disorders. Further studies
will have to be undertaken to specify the connec-
tions that exist between pathological dissociation
in patients with BPD, various aspects of neuro-
psychological functioning and psychosocial func-
tioning and other outcome variables.
Acknowledgements
We thank study participants, colleagues at Sørlandet Hospital
HF for assistance in recruiting the participants, Torunn
Haaland PhD for valuable language consultation, and research
nurse Gro Steensohn for assisting us with the data collection.
The study was financially supported by Sørlandet Hospital HF
and the Southern Norway Regional Health Authority. The
content of this manuscript and the manuscript itself have never
been published either electronically or in print.
Declaration of interest
None.
References
1. Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley
WJ
, Siever LJ. The borderline diagnosis I: psychopathol-
ogy, comorbidity, and personality structure. Biol Psychi-
atry 2002;51:936–950.
2. Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M.
Borderline personality disorder. Lancet 2004;364:453–461.
3. American Psychiatric Association. Diagnostic and statisti-
cal manual of mental disorders: DSM-IV-TR, 4th, text
revision edn. Washington, DC: American Psychiatric
Association, 2000.
4. Judd PH. Neurocognitive impairment as a moderator in the
development of borderline personality disorder. Dev Psy-
chopathol 2005;17:1173–1196.
5. LeGris J, van Reekum R. The neuropsychological correlates
of borderline personality disorder and suicidal behaviour.
Can J Psychiatry 2006;51:131–142.
6. Stiglmayr CE, Shapiro DA, Stieglitz RD, Limberger MF,
Bohus M
. Experience of aversive tension and dissociation
in female patients with borderline personality disorder – a
controlled study. J Psychiatr Res 2001;35:111–118.
7. Stiglmayr CE, Ebner-Priemer UW, Bretz J et al. Dissocia-
tive symptoms are positively related to stress in borderline
personality disorder. Acta Psychiatr Scand 2008;117:139–
147.
8. Ross CA, Joshi S, Currie R. Dissociative experiences in the
general population. Am J Psychiatry 1990;147:1547–1552.
9. Bernstein EM, Putnam FW. Development, reliability, and
validity of a dissociation scale. J Nerv Ment Dis 1986;
174:727–735.
10. Putnam FW, Carlson EB, Ross CA et al. Patterns of dis-
sociation in clinical and nonclinical samples. J Nerv Ment
Dis 1996;184:673–679.
11. Waller NG, Putnam FW, Carlson EB. Types of dissociation
and dissociative types: a taxometric analysis of dissociative
experiences. Psychol Methods 1996;1:300–321.
12. de Ruiter MB, Phaf RH, Elzinga BM, van Dyck R. Disso-
ciative style and individual differences in verbal working
memory span. Conscious Cogn 2004;13:821–828.
13. Cima M, Merckelbach H, Klein B, Shellbach-Matties R,
Kremer
K
. Frontal lobe dysfunctions, dissociation, and
trauma self-reports in forensic psychiatric patients. J Nerv
Ment Dis 2001;189:188–190.
14. Jones B, Heard H, Startup M, Swales M, Williams JMG,
Jones RSP
. Autobiographical memory and dissociation in
borderline personality disorder. Psychol Med 1999;29:
1397–1404.
15. Zanarini MC, Frankenburg FR, Dubo ED et al. Axis I
comorbidity of borderline personality disorder. Am J
Psychiatry 1998;155:1733–1739.
16. Becker DF, Grilo CM, Edell WS, McGlashan TH. Com-
orbidity of borderline personality disorder with other
personality disorders in hospitalized adolescents and
adults. Am J Psychiatry 2000;157:2011–2016.
17. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured
Clinical Interview for DSM-IV-TR Axis I Disorders, Re-
search Version, Patient Edition. (SCID-I
⁄ P). New York:
Biometrics Research, New York State Psychiatric Institute,
1997.
18. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured
Clinical Interview for DSM-IV Personality Disorders,
(SCID-II). Washington, DC: American Psychiatric Press,
Inc., 1997.
19. Hamilton M. Development of a rating scale for primary
depressive illness. Br J Soc Clin Psychol 1967;6:278–296.
20. Wechsler D, Nyman H, Nordvik H. Wais-III: Wechsler
Adult Intelligence Scale: manual (Norwegian edition), 3rd
edn. Stockholm: Psykologifo¨rlaget, 2003.
21. Conners CK. ConnersÕ Continuous Performance test
(CPTII). Technical guide and software manual. North
Tonawanda, NY: Multi Health Systems Inc., 2002.
22. Gronwall DM. Paced auditory serial-addition task: a
measure of recovery from concussion. Percept Mot Skills
1977;44:367–373.
23. Gold JM, Carpenter C, Randolph C, Goldberg TE, Wein-
berger
DR
. Auditory working memory and Wisconsin
Card Sorting Test performance in schizophrenia. Arch
Gen Psychiatry 1997;54:159–165.
24. Callicott JH, Ramsey NF, Tallent K et al. Functional
magnetic resonance imaging brain mapping in psychiatry:
methodological issues illustrated in a study of working
memory in schizophrenia. Neuropsychopharmacology
1998;18:186–196.
25. Lund-Johansen M, Hugdahl K, Wester K. Cognitive func-
tion in patients with ParkinsonÕs disease undergoing ste-
reotaxic thalamotomy. J Neurol Neurosurg Psychiatry
1996;60:564–571.
26. Shum D, Short L, Tunstall J et al. Performance of children
with traumatic brain injury on a 4-disk version of the
Dissociation and cognition in BPD
391

Tower of London and the Porteus Maze. Brain Cogn
2000;44:59–62.
27. Spreen O, Strauss E. A compendium of neuropsychological
tests: administration, norms, and commentary, 2nd edn.
New York: Oxford University Press, 1998.
28. Heaton RK. Wisconsin card sorting test manual. Odessa,
FL: Psychological Assessment Resources, Inc., 1981.
29. Lezak MD. Neuropsychological assessment, 3rd edn. New
York: Oxford University Press, 1995.
30. Bechara A, Damasio H, Damasio AR, Lee GP. Different
contributions of the human amygdala and ventromedial
prefrontal cortex to decision-making. J Neurosci 1999;19:
5473–5481.
31. Brandt J. The Hopkins Verbal Learning Test: development
of a new memory test with six equivalent forms. Clin
Neuropsychol 1991;5:125–142.
32. Benedict RHB, Schretlen D, Groninger L, Brandt J. Hop-
kins Verbal Learning Test – Revised: normative data and
analysis of inter-form and test-retest reliability. Clin Neu-
ropsychol 1998;12:43–55.
33. Kimura D. Right temporal-lobe damage. Perception of
unfamiliar stimuli after damage. Arch Neurol 1963;8:264–
271.
34. Waller NG, Ross CA. The prevalence and biometric
structure of pathological dissociation in the general
population: taxometric and behavior genetic findings.
J Abnorm Psychol 1997;106:499–510.
35. Lenzenweger MF, Clarkin JF, Fertuck EA, Kernberg OF.
Executive neurocognitive functioning and neurobehavioral
systems indicators in borderline personality disorder: a
preliminary study. J Personal Disord 2004;18:421–438.
36. van Reekum R, Conway CA, Gansler D, White R, Bachman
DL
. Neurobehavioral study of borderline personality dis-
order. J Psychiatry Neurosci 1993;18:121–129.
37. OÕLeary KM, Brouwers P, Gardner DL, Cowdry RW.
Neuropsychological testing of patients with borderline
personality disorder. Am J Psychiatry 1991;148:106–111.
38. Swirsky-Sacchetti T, Gorton G, Samuel S, Sobel R, Genetta-
Wadley A, Burleigh B. Neuropsychological function in
borderline personality disorder. J Clin Psychol 1993;49:
385–396.
39. Kunert HJ, Druecke HW, Sass H, Herpertz SC. Frontal lobe
dysfunctions in borderline personality disorder? Neuro-
psychological findings. J Personal Disord 2003;17:497–509.
40. Sprock J, Rader TJ, Kendall JP, Yoder CY. Neuropsycho-
logical functioning in patients with borderline personality
disorder. J Clin Psychol 2000;56:1587–1600.
41. Bazanis E, Rogers RD, Dowson JH et al. Neurocognitive
deficits in decision-making and planning of patients with
DSM-III-R borderline personality disorder. Psychol Med
2002;32:1395–1405.
42. Beblo T, Saavedra AS, Mensebach C et al. Deficits in visual
functions and neuropsychological inconsistency in Bor-
derline Personality Disorder. Psychiatry Res 2006;145:127–
135.
43. Haaland VØ, Landrø NI. Decision making as measured
with the Iowa Gambling Task in patients with borderline
personality disorder. J Int Neuropsychol Soc 2007;13:699–
703.
44. Stevens A, Burkhardt M, Hautzinger M, Schwarz J, Unckel
C
. Borderline personality disorder: impaired visual per-
ception and working memory. Psychiatry Res 2004;125:
257–267.
45. Silbersweig D, Clarkin JF, Goldstein M et al. Failure of
frontolimbic inhibitory function in the context of negative
emotion in borderline personality disorder. Am J Psychi-
atry 2007;164:1832–1841.
46. de Ruiter MB, Phaf RH, Veltman DJ, Kok A, van Dyck R.
Attention as a characteristic of nonclinical dissociation: an
event-related potential study. NeuroImage 2003;19:376–
390.
47. Veltman DJ, de Ruiter MB, Rombouts SA et al. Neuro-
physiological correlates of increased verbal working
memory in high-dissociative participants: a functional
MRI study. Psychol Med 2005;35:175–185.
48. DePrince AP, Freyd JJ. Dissociative tendencies, attention,
and memory. Psychol Sci 1999;10:449–452.
49. Wright DB, Livingston-Raper D. Memory distortion and
dissociation: exploring the relationship in a non-clinical
sample. J Trauma Dissociation 2002;3:97–109.
50. Kindt M, van den Hout M. Dissociation and memory
fragmentation: experimental effects on meta-memory but
not on actual memory performance. Behav Res Ther
2003;41:167–178.
51. Freyd JJ, Martorello SR, Alvarado JS, Hayes AE, Christ-
man JC
. Cognitive environments and dissociative tenden-
cies: performance on the standard Stroop task for high
versus low dissociators. Appl Cogn Psychol 1998;12:S91–
S103.
52. Giesbrecht T, Merckelbach H, Geraerts E, Smeets E. Dis-
sociation in undergraduate students: disruptions in execu-
tive functioning. J Nerv Ment Dis 2004;192:567–569.
53. Bruce AS, Ray WJ, Bruce JM, Arnett PA, Carlson RA. The
relationship between executive functioning and dissocia-
tion. J Clin Exp Neuropsychol 2007;29:626–633.
54. Wright DB, Osborne JE. Dissociation, cognitive failures,
and working memory. Am J Psychol 2005;118:103–113.
55. Elzinga BM, Ardon AM, Heijnis MK, De Ruiter MB, van
Dyck R, Veltman DJ. Neural correlates of enhanced
working-memory performance in dissociative disorder: a
functional MRI study. Psychol Med 2007;37:235–245.
56. Michelson L, June K, Vives A, Testa S, Marchione N. The
role of trauma and dissociation in cognitive-behavioral
psychotherapy outcome and maintenance for panic disor-
der with agoraphobia. Behav Res Ther 1998;36:1011–1050.
57. Rufer M, Held D, Cremer J et al. Dissociation as a pre-
dictor of cognitive behavior therapy outcome in patients
with obsessive–compulsive disorder. Psychother Psycho-
som 2006;75:40–46.
58. Spitzer C, Barnow S, Freyberger HJ, Grabe HJ. Dissociation
predicts symptom-related treatment outcome in short-term
inpatient psychotherapy. Aust N Z J Psychiatry 2007;
41:682–687.
59. Braakmann D, Ludewig S, Milde J et al. Dissoziative
Symptome im Verlauf der Behandlung der Borderline-
Perso¨nlichkeitssto¨rung [Dissociative symptoms during
treatment of borderline personality disorder]. Psychother
Psychol Med 2007;57:154–160.
60. Dumont GJH, de Visser SJ, Cohen AF, van Gerven JMA.
Biomarkers for the effects of selective serotonin reuptake
inhibitors (SSRIs) in healthy subjects. Br J Clin Pharmacol
2005;59:495–510.
61. de Visser SJ, van der Post J, Pieters MSM, Cohen AF, van
Gerven JMA. Biomarkers for the effects of antipsychotic
drugs in healthy volunteers. Br J Clin Pharmacol 2001;
51:119–132.
Haaland and Landrø
392
Wyszukiwarka
Podobne podstrony:
The Relationship Between Personality Organization, Reflective Functioning and Psychiatric Classifica
Developmental protective and risk factors in bpd (using aai)
Functional Origins of Religious Concepts Ontological and Strategic Selection in Evolved Minds
Changes in passive ankle stiffness and its effects on gait function in
Assessment of thyroid, testes, kidney and autonomic nervous system function in lead exposed workers
2010 3 MAY Immunology Function, Pathology, Diagnostics, and Modulation
Functional Origins of Religious Concepts Ontological and Strategic Selection in Evolved Minds
Changes in passive ankle stiffness and its effects on gait function in
Impaired Sexual Function in Patients with BPD is Determined by History of Sexual Abuse
Clinical and neuropsychological correlates of proton magnetic resonance spectroscopy detected metabo
Assessment of thyroid, testes, kidney and autonomic nervous system function in lead exposed workers
Curcumin improves learning and memory ability and its neuroprotective mechanism in mice
Relationship Between Dissociative and Medically Unexplained Symptoms in Men and Women Reporting Chil
Demidov A S Generalized Functions in Mathematical Physics Main Ideas and Concepts (Nova Science Pub
2008 4 JUL Emerging and Reemerging Viruses in Dogs and Cats
Angielski tematy Performance appraisal and its role in business 1
więcej podobnych podstron