F00574 019 f018
|
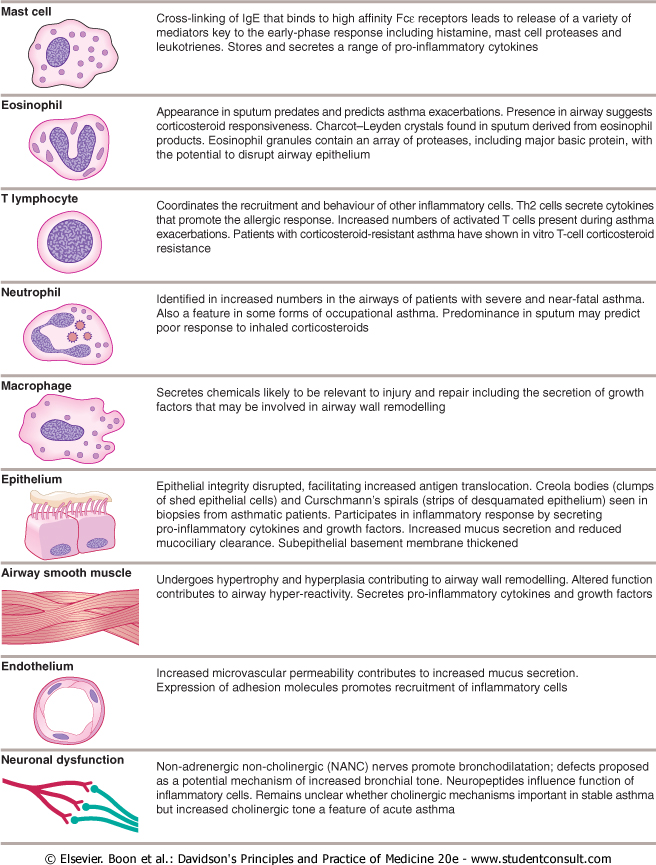
Mast celi iSjp |
Cross-linking of IgE that binds to high affinity Fcc receptors leads to release of a variety of mediators key to the earty-phase response including histaminę, mast celi proteases and leukotrienes. Stores and secretes a rangę of pro-inflammatory cytokines |
|
Eosinophil |
Appearance in sputum predates and predicts asthma exacerbations. Presence in airway suggests corticosteroid responsrveness. Charcot-Leyden crystals found in sputum derived from eosinophil products. Eosinophil granules contain an array of proteases, including major basie protein, with the potential to disrupt airway epithelium |
|
T lymphocyte |
Coordinates the reeruitment and behaviourof other inflammatory cells. Th2 cells secrete cytokines that promote the allergic response. Increased numbers of activated T cells present during asthma exacerbations. Patients with corticosterołd-resistant asthma have shown in vitro T-cell corticosteroid resistance |
|
Ncutrophil |
Identified in increased numbers in the airways of patients with severe and near-fatal asthma. Also a feature in some forms of occupational asthma. Predominance in sputum may predict poor response to inhaled corticosteroids |
|
Macrophage C ^ |
Secretes Chemicals likely to be relevant to injury and repair including the secretion of growth factors that may be involved in airway wali remodelling |
|
Epithclium |
Epithelial integrity disrupted, facilitating increased antigen translocation. Creola bodies (clumps of shed epithelial cells) and Curschmann's spirals (strips of desquamated epithelium) seen in tnopsies from asthmatic patients. Participates in inflammatory response by secreting pro-inflammatory cytokines and growth factors. Increased mucus secretion and reduced mucociliary clearance. Subepithelial basement membranę thickened |
|
Airway smooth muscle |
Undergoes hypertrophy and hyperplasia contributing to airway wali remodelling. Altered function contributes to airway hyper-reactivity. Secretes pro-inflammatory cytokines and growth factors |
|
Endothelium |
Increased microvascular permeability contributes to increased mucus secretion. Expression of adhesion molecules promotes reeruitment of inflammatory cells |
|
Neuronal dysfunction |
Non-adrenergic non-cholinergic (NANC) nerves promote bronchodilatation; defects proposed as a potential mechanism of increased bronchial tonę. Neuropeptides influence function of inflammatory cells. Remains unclear whether cholinergic mechanisms important in stable asthma but increased cholinergic tonę a feature of acute asthma |
© Elsevier. Boon et al.: Davidson's Principles and Practice of Medicine 20e - www.studentconsult.com
Wyszukiwarka
Podobne podstrony:
Schemat budowy roślinnej ściany komórkowej (II) Plant Celi Wall Structure Pectin — Cross-Linking Gly
F00574 006 f018 ^Anaerobic (_]Gram-positive
F00574 019 f010 7.0 100 90 7.1
F00574 019 f012 # Dyspnoea v_ __/ Limbie drives (emotion) Central chemoreceptors (CSF pH) Carotid
F00574 019 f016 May protect against asthma Living on farm Large families Childhood infections,&
F00574 019 f024 High-dose inhaled corticosteroids and regular bronchodilators Occasional temporary s
F00574 019 f025 MEASURE PEAK EXPIRATORY FLOW Convert PEF to % best or %
F00574 019 f026 Enlargement of mucus-secreting glands and inerease in number of goblet cells, a
F00574 019 f030 FEV, (% of value at age 25) Never smoked or not susceptible to smoke Stopped ■smokin
F00574 019 f037 Headache, vomiting, seizures. confusion Lymphocytic
F00574 019 f040a Males 600 500- 400J Ratę per 100000 900- 800- 700 45-54 55-64 65-74 75-84
F00574 019 f040b Females Ratę per 100000 1950
F00574 019 f042b Dłsplacement oł trachea, heart and other mediastinal structures to the right C
F00574 019 f043 f Lełt rll lower / ]U L-lobe ! Rlght middie lobe © Elsevier. Boon et al.:
F00574 019 f051 RESPIRATORY DISEASE Lacrimal gland enlargement Parotid gland enlargement Nasal cutan
F00574 019 g001 Face, mouth and eyes Pursed lips? Central cyanosis? Anaemia? Homer s syndrome (
F00574 019 g002 ©-© KEY FEATURES ON EXAMINATION OF COMMON RESPIRATORY CONDITIONSChronić obstructive
F00574 020 f018 Sympathetic nervous system Sympathetic nervous system I Adrenalinę Noradrenalinę (Ep
więcej podobnych podstron