
Bonding appropriately with baby
Placenta delivered
Fundus firm
Lochia small–moderate
Without clots
Perineum intact/repaired
Hemodynamically stable
EBL <500 cc
B
append
ix
Clinical Paths
Active Phase
Expulsion/Pushing
Recovery 1st Hour Post Partum
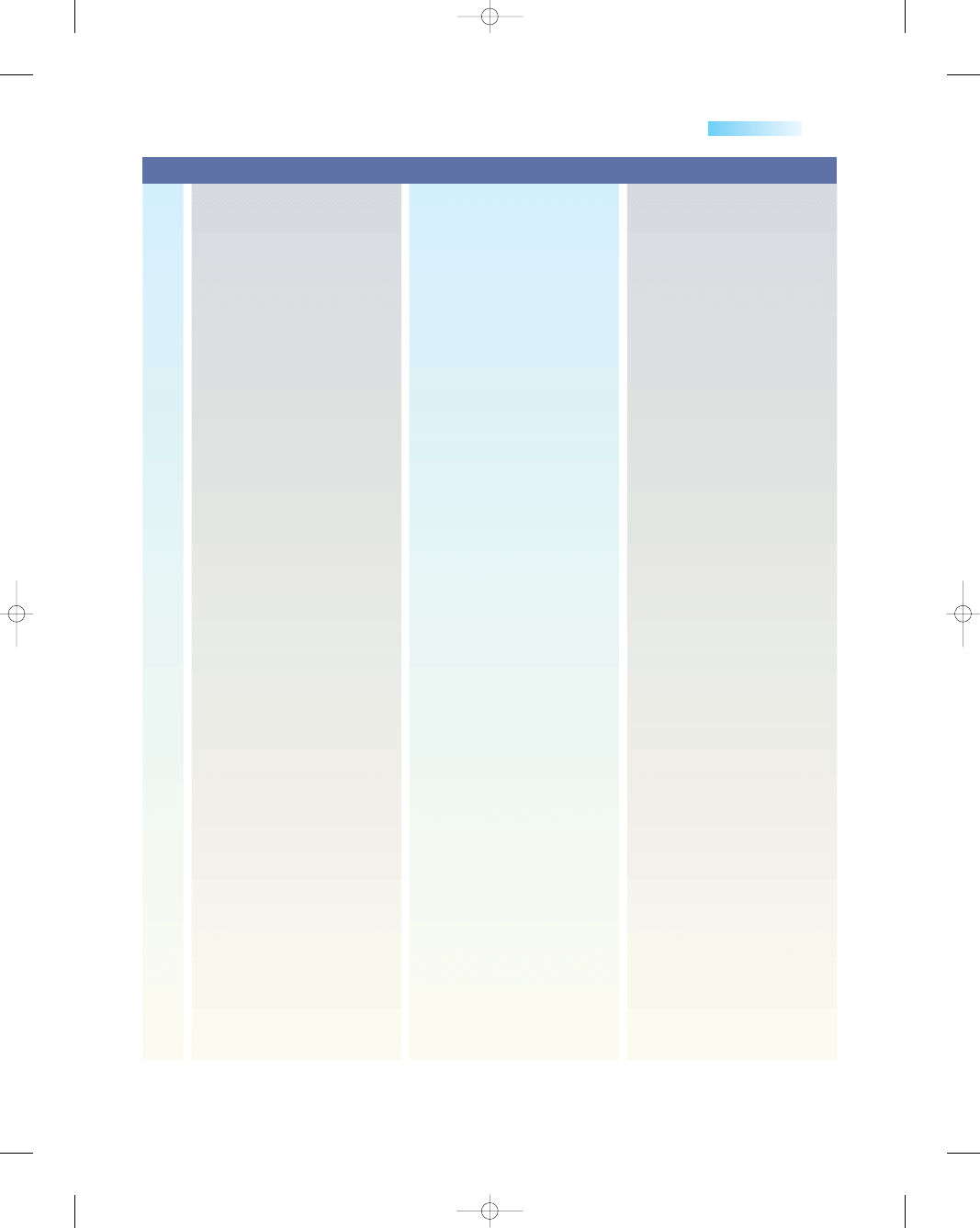
Patient coping with labor
support
Patient utilizing appropriate
labor options
Patient verbalizes satisfaction
with plan
Management interventions
Cervix dilated 5 cms-complete
Contraction regularly with
progressive cervical change.
Maternal/fetal well being
maintained.
Hydration maintained.
If indicated: FSE and/or IUPC
placed
IV Pitocin started
Epidural placed/WE
encouraged
Medicate with Prn pain meds
Prenatal record available after
32 weeks
Prenatal labs WNL
Pre-registered to hospital
Pediatrician identified
Support after hospitalization
identified
Discharge plan discussed with
patient/family.
Communicates understanding
of hospital and community
resources
Patient demonstrates effective
pushing technique.
Patient coping effectively with
pushing.
Support person coping
effectively with labor
Vaginal birth
Labor and Delivery Clinical Path—Labor: Expected Outcomes
PATIENT
EDUCATION
PATIENT STATUS
CONTINUUM OF CARE
3132-28_ApdxBrev.qxd 12/15/05 3:47 PM Page 772
Appendix B
773
Assess: Uterus—fundus
Vital signs
Lochia
Bladder
Perineum
Placenta
Baby status
Breast feeding
Cord blood or Rhogam workup
if appropriate
Cord blood if O
+ Mom
Ice pack to perineum
Warm blankets
Pitocin IV
Assist with ambulate to bathroom
Infant care
Assist with positioning for breast
feeding
Infant ID bands present
Interventions
Assess: Continuous EFM or
auscultation
Q 15 of 30 minutes as
indicated.
Vital signs hourly/Temp Q4 hours
if intact membranes/Q 2 hrs
if membranes ruptured
Uterine by monitor or palpation
Bladder for distention
Hydration status
Cervical dilation, effacement,
station
Reinforce comfort measures
Encourage use of labor options
Inform patient/support person
of plan of care
Hgb or Hct (if not done
recently)
T & S (if ordered)
VE as indicated
IV therapy
AROM by M.D. or CNM: assess
for color, amount and odor,
as appropriate
FSE/IUPC placement if indicated
Comfort measures/Birthing
ball/ambulate/telemetry/
shower
IV therapy
Amnio Infusion for Variable
decelerations
If appropriate, Pain Mgmt.
reviewed.
Antibiotics as indicated for
+ GBS
Pitocin if indicated
PRN pain medication
(Encourage WE if
requesting this).
Labor option usage
Position changes
Assess: Q 15 minutes
monitoring of fetal well
being (Low-Risk) and
Q 5 minutes (High-Risk)
Vital signs hourly Temp. Q 2–4
hrs. depending on
membrane status
Bladder for distention
Hydration status
Pushing effectiveness
Descent of presenting part
Caput
Teaching of upright pushing
positions
Discourage prolonged
maternal breath holding
Encourage to assume position
of choice
Inform patient of progress
AROM: assess for color, amount
and odor, as appropriate
Perineal massage
Warm soaks to perineal area
Allow to rest until feels urge
to push
Frequent position changes
Cool cloth/Ice chips
Pitocin if indicated
Provide wedge if supine
Promote effective position for
pushing: ie: squatting, side
lying, upright
Breathing technique
patient/support person most
comfortable with
ASSESSMENT/
TREATMENT
PATIENT
EDUCATION
TESTS/
PROCEDURES
THERAPIES
MEDS
ACTIVITY/
SAFETY
(continued)
3132-28_ApdxBrev.qxd 12/15/05 3:47 PM Page 773
1–2 days
Incision well
approximated,
without drainage
or redness
Passing flatus
Lochia sm/mod
amt
Fundus firm u/1–2
Verbalizes comfort
using pain
medication as
described
774
Appendix B
Return to previous diet
Interventions
Clear liquids
Ice chips
OTHER
Clear liquids
Ice chips
NUTRITION
UNIQUE PATIENT
NEEDS
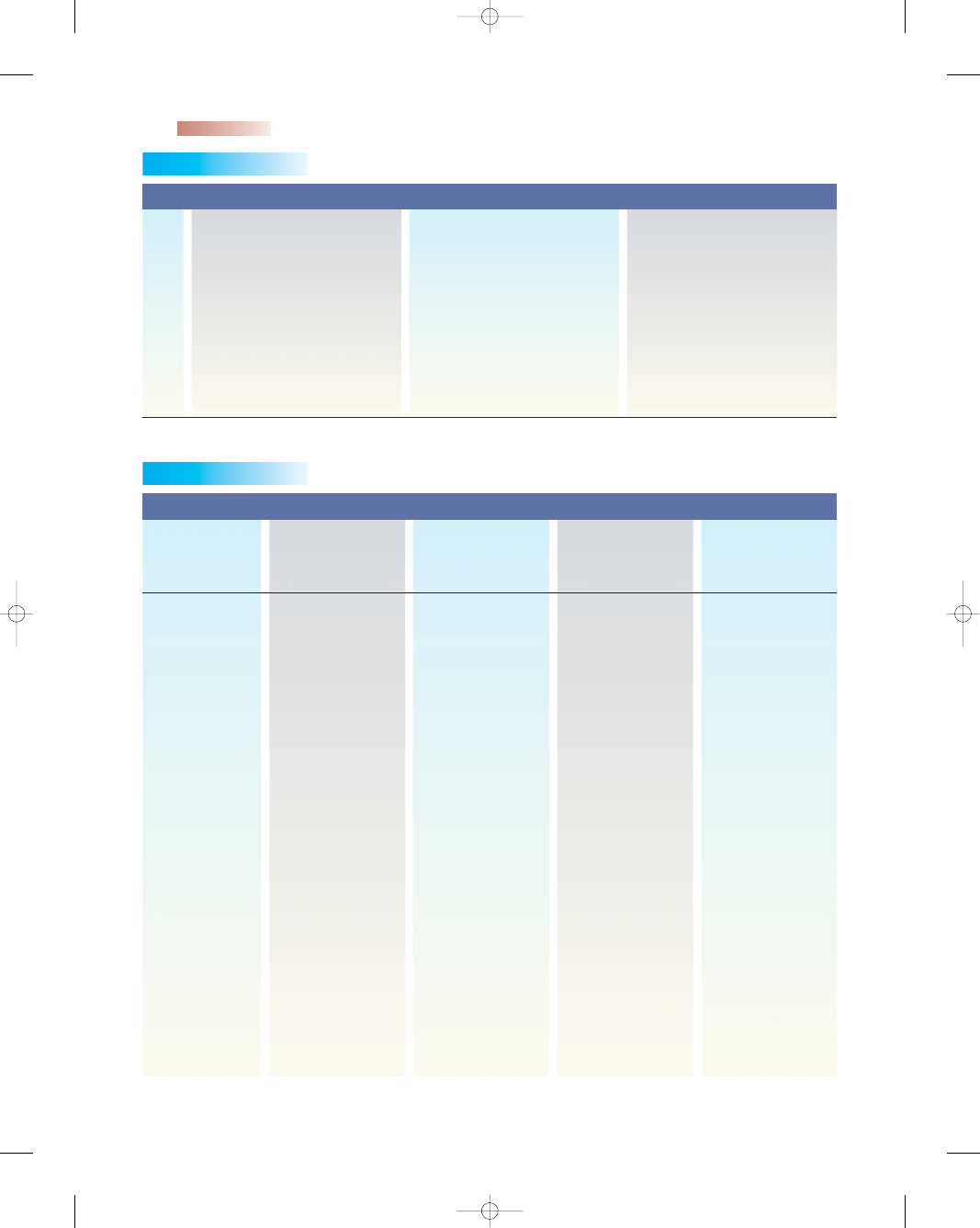
Integrated Plan of Care for Cesarean Delivery
Expected Patient Outcomes
Phase 1
Preadmission
Phase 2 Surgery/
(Cesarean
Immediate Postop/
Phase 3 Post Op
Delivery)
Day of Surgery
Day 1
N/A Date Started:
VS WNL for patient
Hgb or Hct/values
within normal
SLH antepartum
range
Up to 23 hours
VS WNL for
patient Systems
assessment:
Skin warm, dry,
Clear
➞
Alert & oriented
➞
Neg. Homan’s
sign
➞
Breast soft/nipples
intact
➞
Lungs clear
➞
Bowel sounds
present
➞
Fundus firm u/u or u
1–2 (
−/+)
Lochia sm—mod
Dsg dry and intact
No signs infiltration
IV site
Verbalizes comfort
using pain rating
scale 0–10
1 day
VS. WNL for patient
Afebrile
Voiding without
foley
➞
Passing flatus
Incision without
redness or
drainage
Lochia small amount
Fundus firm u/1–2
Verbalizes comfort
using pain scale
0–10 on oral pain
meds
Usual time in
Phase
Assessment /
Potential
Complications
Labor and Delivery Clinical Path—Labor: Expected Outcomes
(continued)
3132-28_ApdxBrev.qxd 12/15/05 3:47 PM Page 774
Appendix B
775
Date All Above Met
Verbalizes follow-
up appointment
date and time
Verbalizes proper
dosing of pain
medication
Date All Above Met
Ambulating in hall
Date All Above Met
Date All Above Met
Entire Phase
Outcomes Met;
Progress patient
to next phase
Assess pain control
0–10 scale
Incision
Volding
Fundus
lochia
Homan’s sign
IV site as needed
ID band on mother
Activity
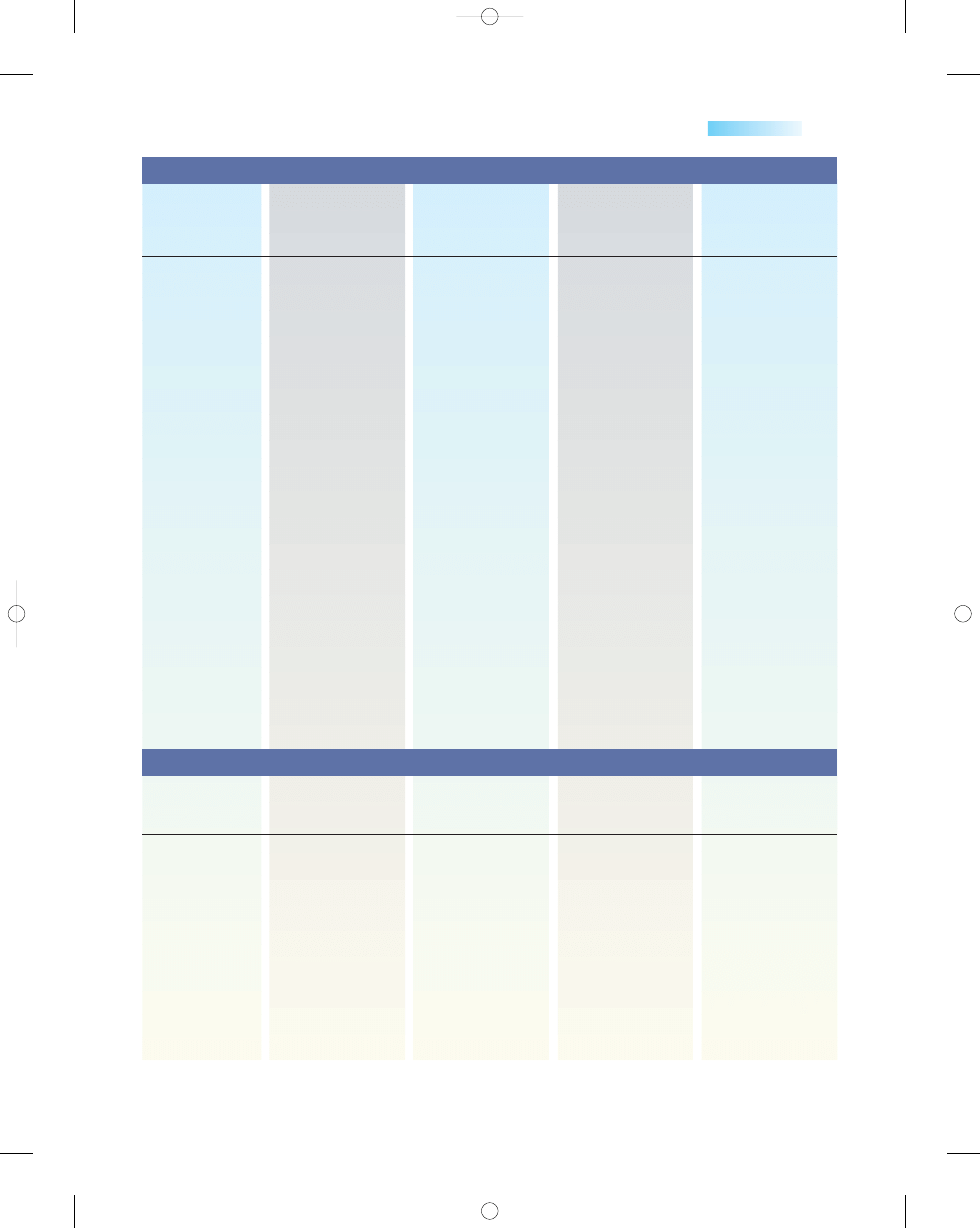
Expected Patient Outcomes
Phase 1
Preadmission
Phase 2 Surgery/
(Cesarean
Immediate Postop/
Phase 3 Post Op
Delivery)
Day of Surgery
Day 1
Date All Above Met
Verbalizes
understanding
of condition and
need for surgery
Verbalizes
understanding
of all pre-op
teaching
Date All Above Met
Verbalizes
understanding
of NPO status
Date All Above Met
Date All Above Met
Entire Phase
Outcomes Met;
Progress patient
to next phase
Vital Signs
Fetal status
immediately
prior to surgery
Date All Above Met
verbalizes correct
use of PCA/
Fentanyl pump
and when to
request pain
medication
Turn, Cough &
deep breath
appropriately
Date All Above Met
Able to ambulate
with minimal
assistance
Tolerating clear/full
liquid diet
Bonding observed
with newborn—
Taking-in
phase
➞
Date All Above Met
Date All Above Met
Entire Phase
Outcomes Met;
Progress patient
to next phase
VS per PACU then
q 4 hr
Systems assessment:
*Skin, LOC, FROM,
Homan’s sign,
*Breasts, Lungs,
Fundus, Incision,
*Lochia, bladder,
bowel sounds,
IV & site
Date All Above Met
can state criteria
for when to call
doctor for
problems post
discharge
➞
↑ bleeding
↑ Temperature ➞
incision redness,
odor or
drainage
➞
Date All Above Met
Ambulating without
assistance
Tolerating soft to
regular diet
Date All Above Met
Date All Above Met
Entire Phase
Outcomes Met;
Progress patient
to next phase
VS q 6 hr
Assess pain control
0–10 scale
Incision
Foley-volding
Fundus/lochia
Homan’s sign
IV site
Breasts
ID band on mother
Activity
Patient / Family
Knowledge
ADL’s / Activity
Unique Patient
Needs
Assessments
Plan of Care
# 2 Surgery/
Immediate Postop/
#3 Post Op
#4 Post Op Day 2-
#1 Preadmission
Day of Surgery
Day 1
Discharge
(continued)
3132-28_ApdxBrev.qxd 12/15/05 3:47 PM Page 775
776
Appendix B
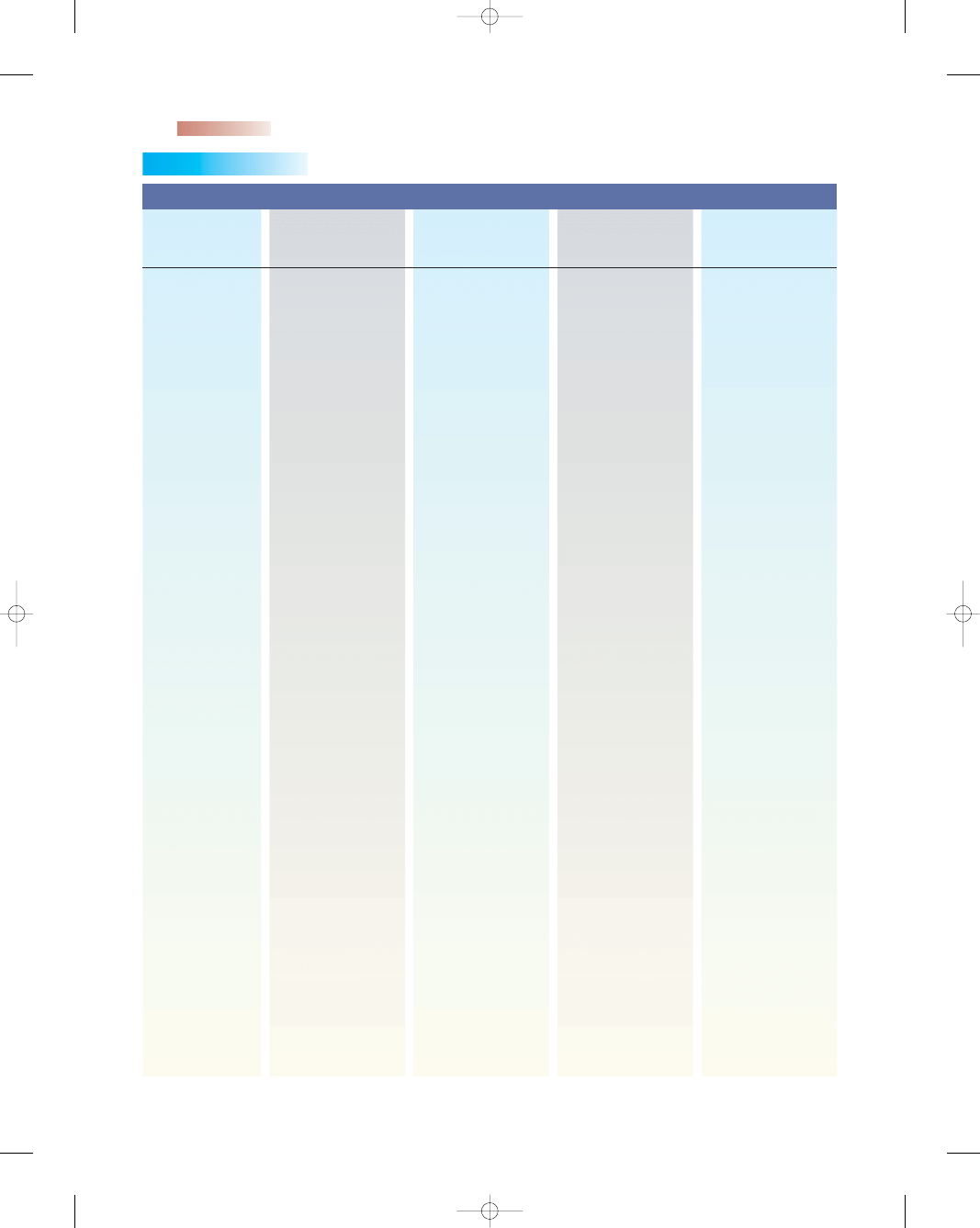
Social Work,
Lactation,
Dietitian as
needed
Verify follow-up
appointment
date and time
Activity restrictions
Follow-up for staple
removal as
needed
Offer Home follow-
up care
Discuss birth control
DC IV lock as
ordered
Plan of Care
# 2 Surgery/
Immediate Postop/
#3 Post Op
#4 Post Op Day 2-
#1 Preadmission
Day of Surgery
Day 1
Discharge
Anesthesia
— Need for surgery
— Review Cesarean
Delivery
— Review
procedure,
postop
expectations
— Demonstrate/
Discuss
equipment—
PCA, Fentanyl
pump
— Tour of OR area
& Nsy
PAT; Hgb or Hot (if
not done
recently—within
one month)
T & S (if ordered)
*I & O q shift
*Assess pain control
0–10 scale
*Assess Rhogam
status
*Assess Rubella titer
status
*ID band on
mother
Social Work as
needed,
Anesthesia,
Lactation,
Dietitian as
needed
Review post-op
expectations
Review equipment
us prn
Instruct pt on:
Hospital/Infant
security systems
Unity orientation
Newborn
orientation/care
/feeding (if
breastfeeding
problems see
decision trees)
IV fluids as ordered
Pain control: PCA,
Fentanyl pump,
IM to PO
Social Work,
Lactation,
Dietitian as
needed
Review dietary
needs post
surgery
Review Bleeding/
Lochia
Precautions post
cesarean
delivery
Review follow-up
care and doctor
Appointments
Review incision
care, peri care
Infant care
Infant feeding
IV lock
PO pain meds
Give Rhogam if
indicated
Give Rubella if
indicated
Consults
Patient / Family
Education
Discharge
Planning
Tests and
Procedures
Pharmacologic
Needs
Integrated Plan of Care for Cesarean Delivery
(continued)
3132-28_ApdxBrev.qxd 12/15/05 3:47 PM Page 776
Appendix B
777
Ambulate in halls
without
assistance
Plan of Care
# 2 Surgery/
Immediate Postop/
#3 Post Op
#4 Post Op Day 2-
#1 Preadmission
Day of Surgery
Day 1
Discharge
Patients usual
Change position
q 2 hr while in
bed, OOB stand
at bedside post-
op night/dangle
and transfer to
chair
Progress to pt.
endurance
Observe bonding
with infant
Observe family
support system
(if inadequate
consult SW)
NPO then clear
liquids to DAT
Foley empty q shift
TCDB q 2 hr while
awake
Progress
endurance/
begin
Ambulation in hall
OOB in AM
May shower
DAT to regular or
previous diet at
home
FOLEY DC’d
Dressing removed
by MD or RN with
MD request
Activity /
Rehabilitation
Nutrition /
Elimination
Miscellaneous
Interventions
Unique Patient
Needs
3132-28_ApdxBrev.qxd 12/15/05 3:47 PM Page 777
Wyszukiwarka
Podobne podstrony:
Essentials of Maternity Newborn and Women's Health 3132A 30 p780 781
Essentials of Maternity Newborn and Women's Health 3132A 29 p778 779
Essentials of Maternity Newborn and Women s Health 3132A 32 p785 808
Essentials of Maternity Newborn and Women s Health 3132A 23 p634 662
Essentials of Maternity Newborn and Women s Health 3132A 17 p428 446
Essentials of Maternity Newborn and Women s Health 3132A 16 p393 427
Essentials of Maternity Newborn and Women s Health 3132A 21 p585 612
Essentials of Maternity Newborn and Women s Health 3132A 09 p189 207
Essentials of Maternity Newborn and Women s Health 3132A 11 p235 252
Essentials of Maternity Newborn and Women s Health 3132A 20 p543 584
Essentials of Maternity Newborn and Women s Health 3132A 08 p167 188
Essentials of Maternity Newborn and Women s Health 3132A 03 p042 058
Essentials of Maternity Newborn and Women s Health 3132A 27 p769 771
Essentials of Maternity Newborn and Women s Health 3132A 26 p729 768
Essentials of Maternity Newborn and Women s Health 3132A 25 p717 728
Essentials of Maternity Newborn and Women s Health 3132A 05 p107 126
Essentials of Maternity Newborn and Women s Health 3132A 19 p496 542
Essentials of Maternity Newborn and Women s Health 3132A 22 p613 633
więcej podobnych podstron