A Millennium Update on Pediatric
Diarrheal Illness in the Developing World
Miguel O’Ryan, MD,* Valeria Prado, MD,* and Larry K. Pickering, MD, FAAP
†
More than one billion diarrhea episodes occur every year among children younger than 5
years of age in socioeconomically developing countries causing 2 to 2.5 million deaths.
More than twenty viral, bacterial, and parasitic enteropathogens are currently associated
with acute diarrhea. Rotavirus and diarrheagenic
Escherichia coli are the most common
pathogens responsible for acute diarrhea episodes in children;
Shigella spp., Salmonella
spp, Campylobacter jejuni/coli, Vibrio cholerae, Aeromonas spp, and Plesiomonas spp.
occur more commonly in poorer areas and infections caused by protozoa and helminthes
occur mainly in areas where environmental sanitation is significantly deteriorated. Initial
clinical assessment of a child with diarrhea should focus on obtaining an accurate evalu-
ation of hydration and nutritional status. Assessment of stool characteristics (e.g., liquid
non-bloody stools vs. dysenteric or bloody stools) is a key feature in determining potential
pathogens causing an acute diarrhea episode. Diagnostic guidelines are discussed in the
article. The major therapeutic intervention for all individuals with diarrhea consists of fluid
and electrolyte therapy. When antimicrobial therapy is appropriate, selection of a specific
agent should be made based upon susceptibility patterns of the pathogen or information on
local susceptibility patterns. Current guidelines for administering appropriate antimicrobial
treatment are provided in the article. Preventive measures include careful personal hy-
giene, especially promotion of hand washing. Immunizations currently or soon to be
available for
Salmonella serotype Typhi, cholera prevention, and rotavirus are discussed.
Semin Pediatr Infect Dis 16:125-136 © 2005 Elsevier Inc. All rights reserved.
I
n the new millennium, diarrheal disease continues to be a
significant cause of morbidity and mortality worldwide.
Information available from the 1980s to date suggests that
the overall frequency of childhood diarrhea has remained
relatively constant, but with a steady decline of diarrhea-
associated deaths.
Estimates suggest that during the 1990s,
nearly 1.4 billion diarrhea episodes occurred every year
among children younger than 5 years of age in socioeconom-
ically developing countries, of which 123.6 million episodes
required outpatient medical care and 9 million episodes re-
quired hospitalization. Approximately 2 to 2.5 million diar-
rhea-associated deaths were estimated annually in this age
group, concentrated in the most impoverished areas of the
world.
The highest age-mortality rate (8.5 per 1000/yr)
occurred in children younger than 1 year of age.
These esti-
mates are somewhat lower than the more than 3 million
deaths from diarrhea reported 10 years before, indicating
that significant advances have had a positive impact on diar-
rhea-associated outcomes.
Children living in socioeconomically underdeveloped ar-
eas will have more overall diarrhea episodes, severe episodes
with dehydration, and a higher death rate compared with
children living in more economically developed areas. These
events are a consequence of numerous conditions common
to poverty, including deficiencies in infrastructure (de-
creased accessibility to noncontaminated water and appro-
priate sewage disposal), crowding and exposure to farm an-
imals (free roaming chickens and pigs), lower standards in
food handling and hygiene, decreased accessibility to medi-
cal care, and low educational level. Malnutrition, a well-rec-
ognized risk factor for death from diarrhea, occurs more
commonly in less economically developed countries.
The concept “developing country” is an oversimplification
that tends to include a broad range of countries that have
important socioeconomic, cultural, and medical-care related
differences among them. For example, the Gross Domestic
Product (GDP) per capita/yr of “developing” regions ranges
*Microbiology and Mycology Program, Institute of Biomedical Sciences,
Faculty of Medicine, University of Chile, Santiago, Chile.
†National Immunization Program, Centers for Disease Control and Preven-
tion, Atlanta, Georgia.
Address reprint requests to: Miguel L O’Ryan, Associate Director, Institute of
Biomedical Sciences, Faculty of Medicine, University of Chile, Indepen-
dencia 1027, Santiago, Chile. E-mail: moryan@med.uchile.cl
125
1045-1870/05/$-see front matter © 2005 Elsevier Inc. All rights reserved.
doi:10.1053/j.spid.2005.12.008

from 7.374 international dollars for Latin America to 4.327 in
Asia and 1.797 in sub-Saharan Africa.
The risk of developing
gastrointestinal tract infections and severe disease in the
poorer countries will be significantly higher compared with
middle-income countries within the economically develop-
ing world. Even more, within the same continent and coun-
try there are cities where the standards are similar to those of
more developed countries. These differences need to be ac-
counted for when seeking specific information on which to
make recommendations. For example, a pediatrician in the
United States asked to recommend diarrhea prevention strat-
egies for a family moving to Santiago, Chile will make differ-
ent recommendations than for a family moving to Dhaka,
Bangladesh. General information can be obtained at specific
web sites (
), but information obtained
should be supplemented with country-specific information
when possible. The need for the best local knowledge avail-
able to support recommendations is critical.
Unfortunately, accurate information on the impact of di-
arrheal disease in most areas within the developing world is
either not available or outdated, or the collection methods
used do not permit comparisons. Taking into account these
limitations, in general, a child in the developing world will
have more diarrhea episodes than will a child living in mid-
dle- or high-income countries. The range in the number of
diarrhea episodes per child/yr is wide and will vary depend-
ing on the risk factors indicated above. An 18-month-old
child living in a small shanty town hut in Bangladesh or the
Amazon area of Brazil, with poor sanitation and no access to
sewage systems, receiving water from a well or river, lacking
adequate nutrition, and sharing a bed with two or three sib-
lings likely will have eight or more diarrhea episodes during
his or her first year of life. The same 18-month-old child
living in a rural area of Chile in a house of wood, with access
to clean water and relatively adequate disposal of sewage,
including stools, and receiving food that potentially could be
contaminated but that most probably will be cooked will
have two to three episodes of diarrhea per year.
Breast-feeding plays a key role in prevention of diarrheal
disease in infants.
Breastfed infants, especially infants
younger than 3 months of age, suffer fewer episodes of diar-
rhea than do infants who are not breastfed.
Partial breast-
feeding confers protection that is intermediate between that
gained by infants who are exclusively breastfed and that of
infants who are exclusively bottle-fed. Other measures such
as vitamin A and zinc supplementation have been shown to
have a positive impact in decreasing morbidity and mortality
associated with Shigella infections in Bangladesh.
The relative contribution of different pathogens account-
ing for diarrhea episodes will vary depending on the specific
area of residence. Children living in areas with poor sanita-
tion are at higher risk for fecal-oral transmission, and food
and water contamination will result in a higher risk of acquir-
ing infection caused by enteric bacteria and parasites. In con-
trast, in areas of better sanitary conditions, bacteria are a less
common cause of diarrhea in children, with most cases being
caused by enteric viruses.
Severe outcomes (hospitaliza-
tion and death) associated with acute diarrhea show a diver-
gent pattern in areas with different levels of economic devel-
opment. Unfortunately but not unexpectedly, 85 percent of
diarrheal deaths occur in the less privileged countries of the
world. In these low-income countries, diarrhea accounts for
as many as 21 percent of all deaths in children younger than
5 years of age.
These figures are striking when compared
with the more economically developed world, where diar-
rhea is associated with fewer than 1 percent of deaths in
children.
The leading cause of diarrhea-associated hospital-
izations and death is dehydration. The risk of having severe
dehydration increases if episodes are more frequent or are
more severe and if the possibility of appropriately managing
dehydration, including accessibility to oral rehydration solu-
tions and to emergency departments and hospitals, is not
readily available. In addition, the educational level of parents
is critical in preventing and recognizing severe illness. In this
context, children living in areas where specific pathogens
tend to cause severe diarrhea-vomiting episodes (eg, cholera)
and where accessing oral or IV rehydration is difficult will be
at the highest risk for the development of severe dehydration.
The possibility of dying will be highly concentrated in these
settings within the poorest areas of the world, mainly under-
developed areas of Asia, sub-Saharan Africa, India, and Latin
America. Hospitalization rates for acute diarrhea will not par-
allel necessarily the trend observed for mortality rates. Hos-
pitalization in many poor countries represents an opportu-
nity that is not readily available. Conversely, in more
developed countries, hospitalization often represents a safety
measure that frequently is overused. Recent estimates suggest
that hospitalization rates for acute diarrhea are higher in mid-
dle- and high-income countries than in poorer countries.
Relevant Pathogens
Causing Diarrhea
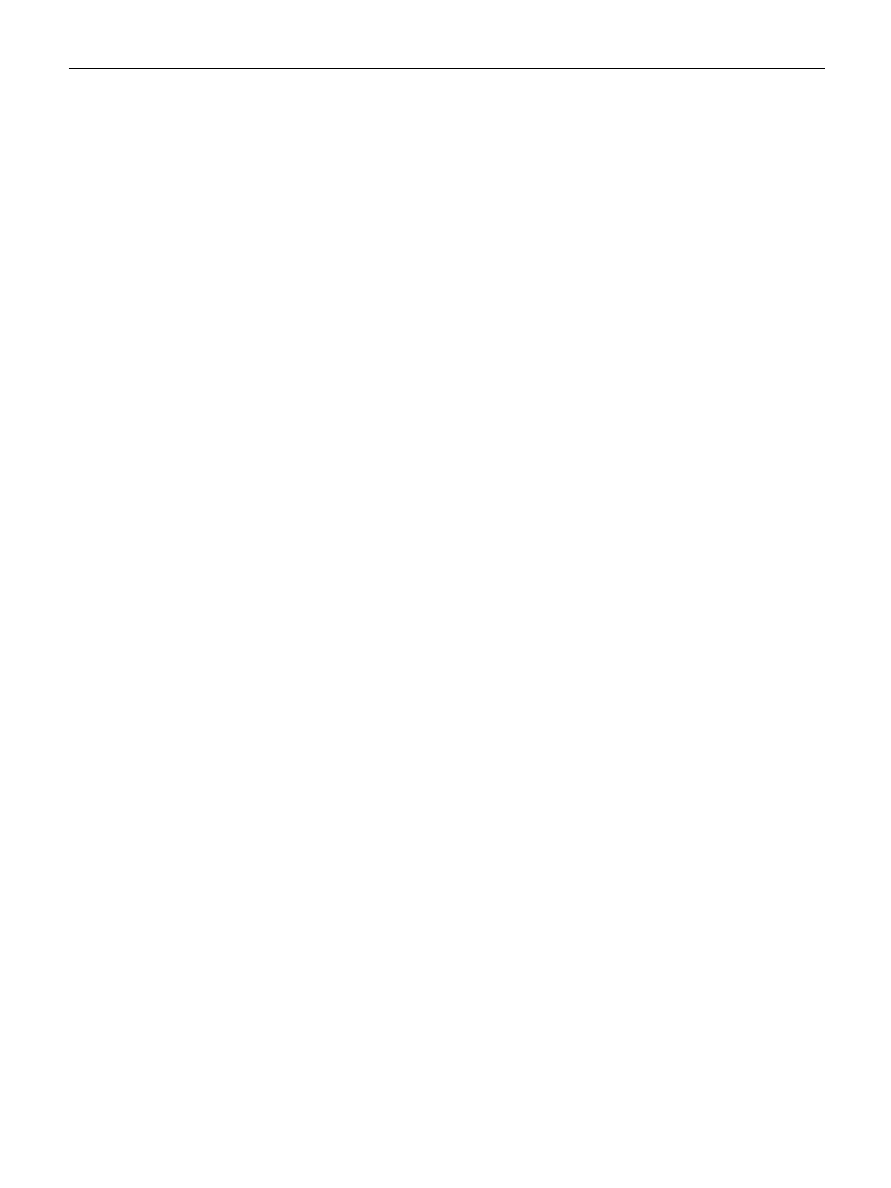
More than 20 viral, bacterial, and parasitic enteropathogens
are associated with acute diarrhea. Enteropathogens most
frequently reported are shown in
. Case-control stud-
ies required to determine the true pathogenic role of different
microorganisms are scarce in the economically developing
world. Available information is based mostly on descriptive
studies that group children younger than 5 years of age and
that do not define clearly the severity of disease nor diarrhea
characteristics (watery versus dysenteric stools). Prevalence
of specific pathogens is dependent on these variables and,
thus, proposing age-adjusted prevalence rates for specific
pathogens is difficult. Certain generalizations can be made
and are discussed in the following section.
Enteric Viruses
Four enteric viruses cause diarrhea in humans: rotavirus,
astrovirus, human caliciviruses (divided into 2 genera, noro-
virus and sapovirus), and enteric adenoviruses. Independent
of economic development, rotavirus is the most common
cause of severe, acute nondysenteric diarrhea in most areas of
the world where it has been studied. Rotavirus causes from
25 to 70 percent of cases in children of gastroenteritis severe
126
M. O’Ryan, V. Prado, and L.K. Pickering

enough to require hospitalization.
Rotavirus occurs
most commonly in children younger than 2 years of age and
uncommonly after they reach 5 years of age. In areas with low
economic development, infection occurs more commonly in
infants younger than 12 months of age compared with more
industrialized areas, where infection occurs more commonly
in children 12 to 24 months of age.
Virtually all children are
infected by the time they reach 3 years of age.
Astrovirus, human caliciviruses, and enteric adenovirus
together represent as many as 20 to 30 percent of cases of
diarrhea in areas where bacterial infections are found less
commonly. In areas with less economic development, these
viruses also infect children, but their relative contribution to
the total number of cases is diluted in lieu of the higher rate of
bacterial infections. Enteric adenoviruses belonging to sero-
types 40 and 41 have been associated with persistent diar-
rhea, generally in children younger than 4 years of age.
Noroviruses have a worldwide distribution, are genetically
and antigenetically diverse, and cause both sporadic disease
and common-source outbreaks.
Eight antigenic types
of astrovirus cause diarrhea in young children.
All enteric
viruses can cause asymptomatic infection.
Bacterial Pathogens
Diarrheagenic Escherichia coli include the following clinically
relevant pathotypes: enteropathogenic (EPEC), enterotoxi-
genic (ETEC), shigatoxin-producing (STEC), enteroaggrega-
tive (EAEC), and enteroinvasive (EIEC). As a group, diar-
rheagenic E. coli are the most common bacteria detected in
studies from economically developing countries, causing 30
to 40 percent of acute diarrhea episodes in children.
EAEC, EPEC and ETEC cause endemic watery diarrhea and
have been reported most frequently in children younger than
2 years of age.
ETEC is a common cause of traveler’s
diarrhea in economically developing countries. EIEC causes
diarrhea generally with fever and blood indistinctive from
Shigella infections in all ages. STEC has been reported as a
common cause of bloody diarrhea from some developing
countries (mainly Chile and Argentina), but these findings
have not been universal. Geographic location and methods
Table 1 Enteropathogens Frequently Associated With Acute Diarrhea in Children
Microorganisms
Highlights
Viruses
Rotavirus
Most common cause of diarrhea in children <24 months of age
Human calicivirus
Causes outbreaks and sporadic cases of gastroenteritis
Norovirus
Outbreaks occur in closed populations; common source outbreaks associated with
ingestion of contaminated food and water
Sapovirus
Less common; causes sporadic diarrhea episodes in children.
Astrovirus
Infection usually occurs in children <4 years of age.
Enteric adenovirus
Diarrhea associated mainly with serotypes 40 and 41, most often in children.
Bacteria
Diarrheagenic
E. coli
EPEC*
Acute endemic and epidemic diarrhea in infants, occasionally associated with persistent
diarrhea
ETEC
Infantile diarrhea in economically developing countries and travelers diarrhea in all ages
STEC
Bloody diarrhea and hemolytic uremic syndrome in children <5 years of age,
hemorrhagic colitis and thrombotic purpura following diarrhea in adults
EAEC
Acute and persistent diarrhea in infants
EIEC
Similar to disease caused by
Shigella, spp
Shigella spp.
Common cause of watery diarrhea and dysentery in children 12-48 months of age;
S.
flexneri is more common than S. sonnei in developing areas; significant antimicrobial
resistance worldwide
Salmonella enteritidis
Zoonotic; common cause of foodborne outbreaks
Campylobacter spp.
Zoonotic; mainly due to contact with poultry
Vibrio cholerae
Severe watery diarrhea; O1 is endemic in South Asia and Africa, and O139 is epidemic
in Asia
Parasites
Giardia lamblia
Cause of diarrhea in all ages worldwide; asymptomatic shedding is common
Entamoeba histolytica
Prevalent in economically developing countries; less common in children;
E. dispar is
not pathogenic
Cryptosporidium parvum
Associated with large waterborne outbreaks; person-to-person transmission occurs
commonly
Cyclospora cayetanensis
Outbreaks associated with food and water; direct person-to-person transmission has
not been documented
Isospora belli
Infection more common in tropical and subtropical areas and in areas of poor sanitation
*EPEC, enteropathogenic
Escherichia coli; ETEC, enterotoxigenic E. coli; STEC, Shigatoxin-producing E. coli; EIEC, enteroinvasive E. coli;
EAEC, enteroaggregative
E. coli.
Pediatric diarrheal illness in the developing world
127
used for establishing the diagnosis have an important influ-
ence on incidence and prevalence.
For instance, in the
United States, E. coli O157:H7 is the STEC most frequently
reported, whereas in Argentina and Chile other non-O157
STEC strains cause most cases of bloody diarrhea and hemo-
lytic uremic syndrome (HUS).
STEC has been established
as the main etiologic agent of HUS.
EAEC has been associ-
ated with persistent diarrhea.
Enteric infections associated with Shigella spp., Salmonella
spp., Campylobacter jejuni/coli, and other bacteria (Vibrio chol-
erae, Aeromonas spp, Plesiomonas spp.) occur more com-
monly in areas where development and hygiene are inade-
quate.
In these areas, children commonly shed these
organisms in the absence of diarrhea, confounding their
pathogenic role in acute diarrhea episodes.
Severity
of Shigella infections can increase significantly in malnour-
ished children, causing severe complications such as toxic
megacolon, intestinal perforation, and HUS associated with
S. dysenteriae type 1 infections. C. jejuni/coli is associated with
consumption of poultry and the presence of poultry in the
households; prevalence is variable among different areas,
with most cases occurring in children younger than 24
months of age. Campylobacter also can be shed asymptomat-
ically.
The principal reservoirs of nontyphoidal Salmonella organ-
isms are animals, including poultry, livestock, reptiles, and
pets. The major vehicles of transmission are foods of animal
origin, including eggs, dairy products, and poultry, and are
most significant in areas where potentially contaminated
food products (mainly derived from poultry) are processed in
large scale. Foodborne outbreaks caused by nontyphoid
Salmonella strains affect children and adults worldwide.
Differences in seasonal prevalence of specific pathogens
and epidemic curves need to be considered before proposing
probable microorganisms causing acute diarrhea in a child.
In general, rotavirus predominates during colder months,
although infection tends to occur year-round in tropical areas
and in some temperate climates. Bacterial infections predom-
inate during warmer months. Salmonella enteritidis and
C. jejuni/coli infections can be epidemic in a given area during
a defined time period.
V. cholerae needs to be considered among the possible
causes in children living in endemic areas (currently, south
Asia and Africa). V. cholerae O1, V. cholerae O139, and
S. dysenteriae 1 can cause epidemics and pandemics in areas
of extreme poverty and/or in areas with massive population
migrations associated with natural disasters or long-lasting
wars.
Mixed infections can represent as many as 15 to 20 percent
of diarrhea episodes. The possibilities of coinfections occur-
ring reflect the most common organisms circulating within a
community. Mixed infections are not necessarily more severe
compared with infections caused by a sole patho-
gen.
Parasites
Infections caused by protozoa and helminths occur mainly in
areas where potable water is not readily available and/or
where environmental sanitation is significantly deteriorated,
as occurs in markedly deprived areas of the economically
developing world. These infections decrease significantly in
areas that have solved these basic sanitary deficiencies.
Entamoeba histolytica can cause acute nonbloody and bloody
diarrhea, necrotizing enterocolitis, ameboma, and liver ab-
scess and needs to be differentiated from morphologically
identical nonpathogenic strains such as Entamoeba dispar and
Entamoeba moshkovskii.
These species are excreted as cysts
and trophozoits in stools of infected people, and infection is
initiated most commonly by ingesting fecally contaminated
water or food containing E. histolytica cysts.
Giardia lamblia is a binucleate flagellated protozoan para-
site with trophozoite and cyst stages. Giardia is spread by the
fecal-oral route through ingestion of cysts, and infection is
limited to the small intestine and biliary tract. Outbreaks in
childcare centers have reflected person-to-person spread and
have demonstrated high infectivity.
Foodborne and
waterborne transmission also occur. Infection often is
asymptomatic or mildly symptomatic. Symptoms in giardia-
sis are related to the age of the patient, with diarrhea, vomit-
ing, anorexia, and failure to thrive occurring typically in the
youngest children. Infection rates in the economically devel-
oping world are high, as exemplified by a study in slum areas
of Peru, where seroprevalence reaches 40 percent by the time
infants reach the age of 6 months.
Cryptosporidium parvum is a spore-forming coccidian pro-
tozoon. Other spore-forming protozoa that cause diarrhea
are Isospora belli, Cyclospora cayetanensis, and Microsporidium
spp.
Cryptosporidium spp. are ubiquitous and, because
Cryptosporidium infects a wide variety of animal species, in-
fected individuals often have a history of animal contact.
Person-to-person spread, particularly in household contacts
and child-care centers, is well-documented and shows that
the organism is highly infectious.
Waterborne outbreaks
of cryptosporidiosis occur and can reach massive propor-
tions.
The clinical manifestations of illness in immunocom-
petent persons include watery diarrhea, abdominal pain, my-
algia, fever, and weight loss.
Infants infected early
in life may develop chronic diarrhea and malnutrition.
Cy-
closporiasis occurs worldwide but is endemic in some coun-
tries such as Peru and Haiti. Sporulation outside the host
produces infectious organisms; therefore, direct person-to-
person transmission does not occur. Outbreaks have been
associated with contaminated food and water. Clinical signs
and symptoms include watery diarrhea, which usually is self-
limited.
Isosporiasis occurs more commonly in tropical and
subtropical climates and in areas of poor sanitary conditions.
Infection occurs by the fecal-oral route and has been linked to
contaminated food and water. Oocysts are passed unsporu-
lated and require exposure to oxygen and temperature lower
than 37° C before becoming infective.
Watery diarrhea is
the most common symptom. Two microsporidia species are
important causes of chronic diarrhea in immunocompro-
mised people, especially people infected with human immu-
nodeficiency virus (HIV).
128
M. O’Ryan, V. Prado, and L.K. Pickering
Clinical Considerations
and Diagnosis
Diarrhea is a manifestation of intestinal dysfunction that re-
sults in increased stool output resulting in loss of water,
electrolytes, and/or nutrients. The most commonly used def-
inition of diarrhea is three or more loose stools during a
24-hour period, but physicians should consider the normal
regular evacuation pattern of the affected individual before
defining if he/she has diarrhea. In breastfed infants, for ex-
ample, normal stool patterns include passages of six to eight
liquid stools per day. Fever, vomiting, abdominal cramps,
and dehydration of different magnitudes can accompany di-
arrhea. High fever and intense vomiting can be present in
viral and bacterial infections and are not pathognomonic of a
given pathogen. Acute diarrhea accompanied with urgency
to defecate and tenesmus suggests an inflammatory/invasive
process of the colon as described below.
Most cases of acute diarrhea will resolve within 7 days.
Persistent diarrhea lasting longer than 14 days has been as-
sociated with several infectious and noninfectious causes,
including EAEC, Yersinia enterocolitica, enteric adenovirus,
Isospora belli, Cyclospora cayetanensis, G. lamblia, Microspo-
ridium, C. parvum, transitory lactose intolerance, and moder-
ate to severe malnutrition.
As indicated previously, the
risk of acquiring infection with several enteric pathogens in-
creases in areas where potable water is not readily available.
Initial clinical assessment of a child with diarrhea should
focus on obtaining an accurate evaluation of hydration and
nutritional status. The first is critical for management because
morbidity and mortality are associated predominantly with
dehydration. Guidelines for evaluation and quantification of
dehydration can be found elsewhere.
Malnutrition is a
risk factor for a poorer outcome, and physicians should en-
sure that appropriate actions are taken to avoid nutritional
deterioration that occurs during the acute diarrheal episode
(maintain oral protein/calorie intake). Limiting intake of milk
currently is not recommended for the great majority of chil-
dren with acute diarrhea; this measure should be considered
only if lactose malabsorption causing persistent diarrhea is
suspected.
Assessment of characteristics of the stool is a key feature in
determining potential pathogens causing an acute diarrhea
episode. Liquid nonbloody stools are associated predomi-
nantly with a secretory/small intestinal dysfunction process,
whereas dysenteric (blood and pus) or bloody stools gener-
ally are associated with an inflammatory/invasive process of
the colon. Mucous can be present in both situations and
should be differentiated from pus.
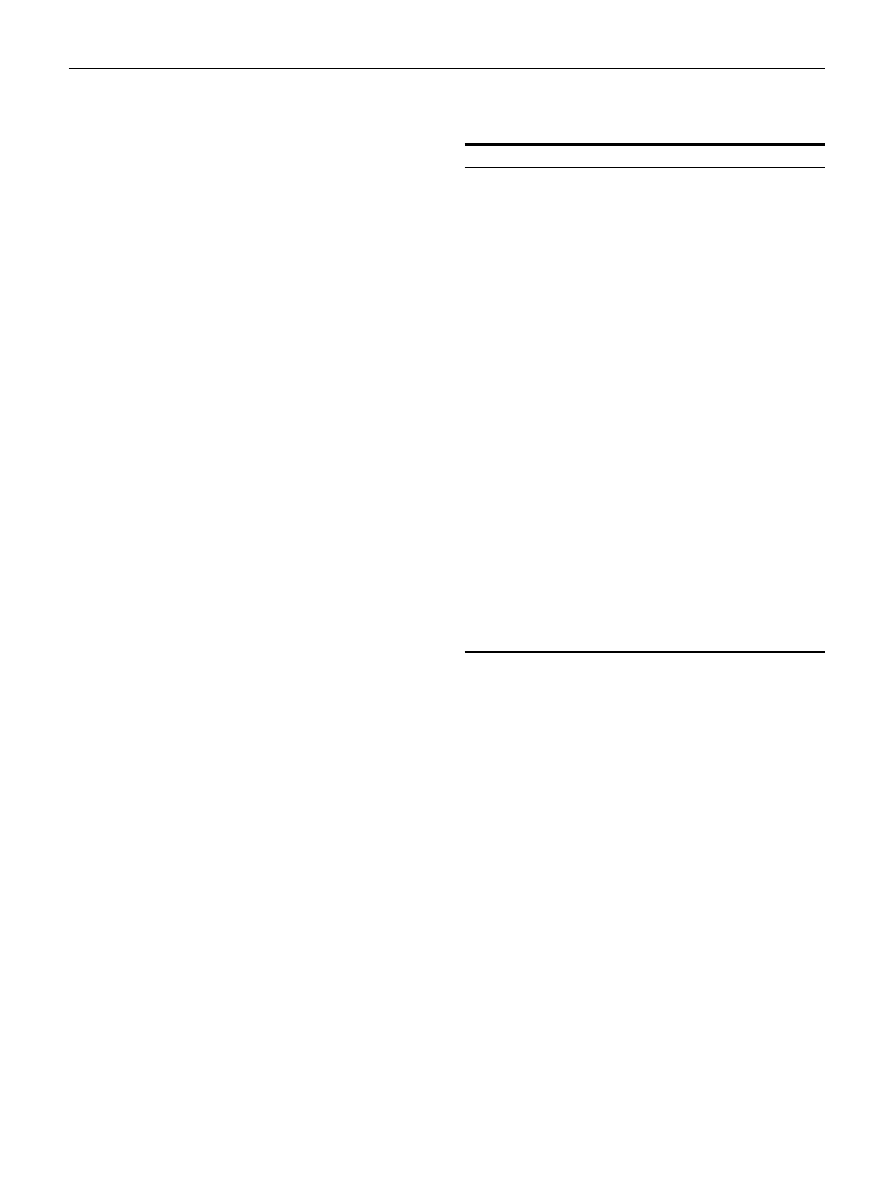
lists the pathogens
most likely to be detected in children with moderate to severe
acute endemic diarrhea living in developing areas.
The ability to obtain an etiological diagnosis in a child with
diarrhea is highly dependent on the quality of the stool sam-
ple, the experience and skill of the microbiologist, and re-
sources available for stool evaluation. Appropriate manage-
ment of the stool sample requires collection of a recently
passed sample directly from the diaper or an appropriately
obtained rectal tube or swab sample. Areas of stools with pus,
blood, or mucous are optimal for sampling. All samples
should be inoculated immediately or placed into transport
media and immediately transported to the laboratory.
Once in the laboratory, the number and types of selective
media used and the number of suspicious colonies studied
will impact the ability to identify an enteric pathogen in
stools. A universal consensus guideline for stool evaluation is
not available, and different laboratories have established their
own guidelines.
Culture techniques used in microbiology
laboratories should be able to identify Shigella, Salmonella,
Yersinia, and Campylobacter. Because selective media for
Campylobacter are expensive, identifying this microorganism
may be difficult in economically developing countries.
Identifying other enteropathogens requires additional testing
not always available in diagnostic microbiology laboratories.
Enteric viruses such as rotavirus, enteric adenovirus, astrovi-
rus, and the parasite G. lamblia can be detected by commer-
cially available techniques with acceptable sensitivity and
specificity.
Detection of E. coli pathotypes and calicivi-
Table 2 Most Commonly Reported Microorganisms Associ-
ated With Acute Endemic Diarrhea in Economically Devel-
oping Areas by Age Groups and Diarrhea Characteristic*
All Episodes
Microorganisms
<
2 year
Rotavirus
EPEC, ETEC
Astrovirus, Caliciviruses, Enteric
Adenovirus
Shigella flexneri, Shigella dysenteriae
type 1†
Campylobacter jejuni‡
STEC, EAEC
2–5 years
ETEC
S. flexneri, S. dysenteriae type 1†
Rotavirus
Non-typhi
Salmonella†
Giardia lamblia
Watery/mucous
<
2 year
Rotavirus
EPEC, ETEC
Astrovirus, Caliciviruses, Enteric
adenovirus
2–5 years
ETEC
S. flexneri/S. dysenteriae type 1
Rotavirus
Dysenteric/bloody
<
2 year
S. flexneri, S. dysenteriae type 1†
STEC
C. jejuni‡
2–5 years
S. flexneri/S. dysenteriae type 1†
STEC
Non-typhi
Salmonella†
Entamoeba histolytica§
*List generated by consensus of authors based on literature review
and personal experience. The list order of the pathogens repre-
sents a gross approximation from higher to lower probability.
†In areas where infection is endemic.
‡Associated with presence of animals (poultry) in the household.
§Mainly in areas where hygiene is markedly deficient.
Pediatric diarrheal illness in the developing world
129

ruses are available in selected research or reference laborato-
ries.
Studies suggest that detection of low inoculum-
viable microorganisms such as Shigella spp. or differentiation
of E. histolytica from E. dispar can be improved significantly
by using genetic amplification techniques such as real-time
polymerase chain reaction (PCR), but the clinical and epide-
miological relevance and applicability of detection based on
gene amplification in culture-negative individuals will re-
quire further clarification.
The possibility of incorporat-
ing new molecular techniques for routine diagnostic testing
in most economically developing countries will require ap-
propriate cost-benefit analyses of these new techniques.
Most episodes of diarrhea, independent of etiology, are
mild, self-limited, and not affected by specific antimicrobial
treatment. In addition, the numbers of different pathogens
that can cause acute diarrhea are significant, and diagnostic
testing is difficult to perform and expensive. This concern is
especially important in economically developing countries
where resources are limited. In addition, in most laborato-
ries, stool culture results are reported 48 to 72 hours after
collection of the sample, a time period during which patients
with acute diarrhea may have been treated and most of whom
will have improved significantly with or without specific
treatment.
Considering the limitations of enteropathogen detection,
our current recommendation for physicians managing chil-
dren with acute diarrhea is to focus diagnostic efforts on
children in whom the likelihood of obtaining a pathogen will
be reasonable and will make a difference for the child or
his/her potential contacts. Neonates and immunocompro-
mised patients with diarrhea should be studied because they
have a higher risk for acquiring invasive or unusual patho-
gens. Individuals involved in foodborne or waterborne out-
breaks and, when possible, children in childcare centers
should be studied for epidemiological and preventive rea-
sons. Children with persistent diarrhea also should be stud-
ied, although the yield may be low. Children with moderate
to severe bloody diarrhea, especially children requiring hos-
pitalization, should be studied to detect Shigella, STEC, Sal-
monella, Campylobacter, and E. histolytica in areas where these
infections are prevalent. Appropriate case-control studies
performed on a regular basis in different areas represent the
best strategy to define the most probable microorganisms
causing disease. These studies are an invaluable aid in em-
piric management of children with diarrhea residing in these
areas.
Stool assays for rapid identification of episodes likely to be
caused by an invasive organism have been proposed. Stool
leukocytes, lactoferrin, and occult blood have been the most
common fecal screening tests evaluated.
In general, chil-
dren with diarrhea who have one or more of these elements in
stools will have a higher probability of harboring an invasive
pathogen, but the clinical usefulness of these nonspecific
tests is limited. A metanalysis concluded that these tests per-
form moderately well in suggesting invasive pathogens such
as Shigella, Salmonella, EIEC, and Campylobacter in econom-
ically developed countries but poorly in developing coun-
tries.
Considering that current guidelines support treat-
ment of moderate to severe invasive diarrhea caused by
Shigella spp. and not STEC, that the additional benefit of
microscopic over macroscopic/clinical findings in severe
cases is unclear, and that fecal screening tests do not help in
discriminating between these pathogens, we consider these
tests to be of limited benefit for most children in the econom-
ically developing world. To assist in the macroscopic evalu-
ation of a stool specimen, screening tests could be considered
in a febrile child with severe watery diarrhea if Shigella is
suspected. A positive test could favor administering antimi-
crobial treatment while awaiting culture results. In a febrile
child with grossly bloody diarrhea, these tests will not pro-
vide benefit and will increase management costs of the epi-
sode unnecessarily.
Treatment
The major therapeutic intervention for all infants, children,
adolescents, and adults with diarrhea consists of fluid and
electrolyte therapy.
Antimicrobial therapy is not indicated
for most patients with diarrhea because most enteric infec-
tions are self-limited or are caused by agents for which anti-
microbial therapy is not available or effective. In addition,
concerns inherent with antimicrobial therapy include safety
and tolerability of antimicrobial agents, particularly in immu-
nocompromised people, the young and the elderly; potential
enhancement of virulence factors; prolongation of the carrier
state; and development of resistance.
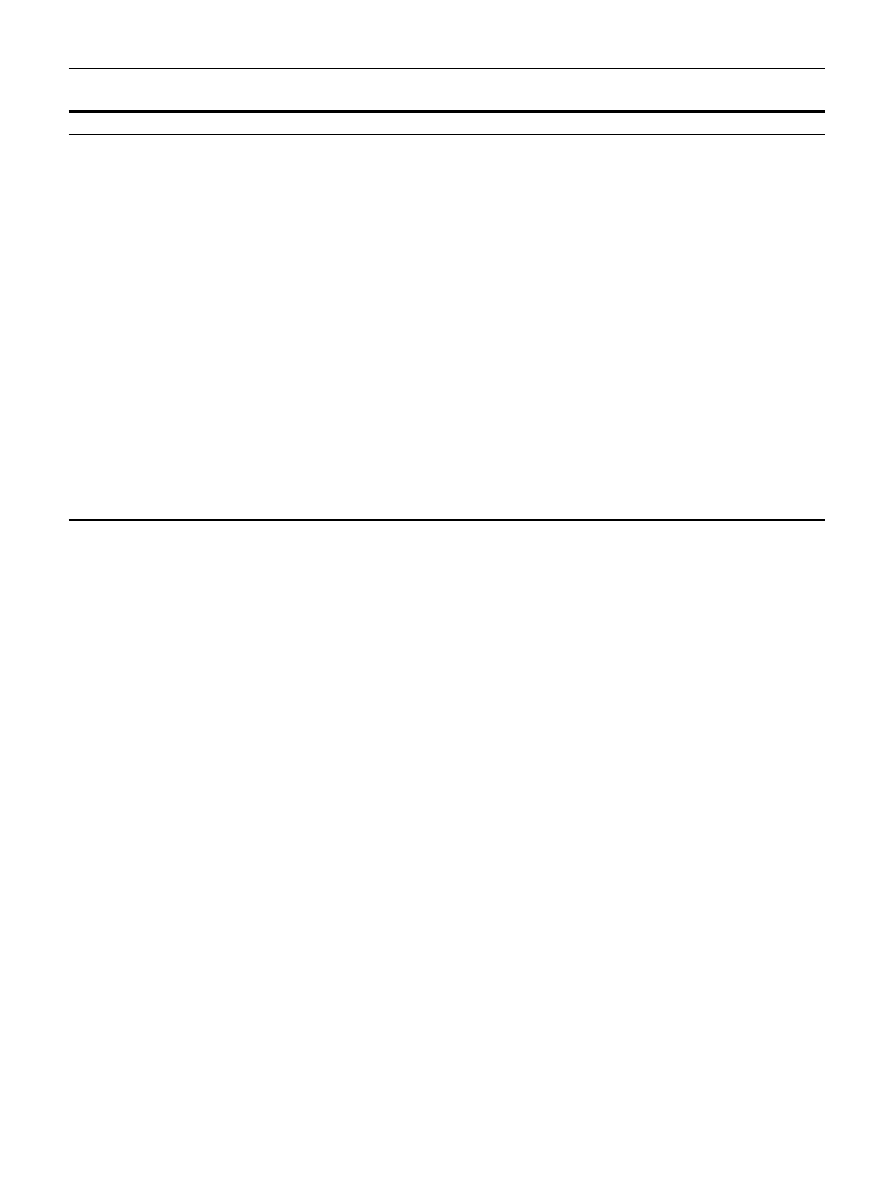
Antimicrobial agents are given to patients with diarrhea
caused by select bacterial and protozoal pathogens (Table 3).
The purpose of this therapy is to reduce signs, symptoms,
and duration of disease; prevent morbidity and mortality;
eradicate fecal shedding of the causative organism; and elim-
inate transmission. Benefits and limitations of antimicrobial
therapy should be considered when approaching a patient
with gastroenteritis. When antimicrobial therapy is appropri-
ate, selection of a specific agent should be made based on
susceptibility patterns of the pathogen or information on lo-
cal susceptibility patterns obtained from active surveillance
studies if the first is not available. Because resistance among
enteric organisms can spread rapidly, constant monitoring of
susceptibility patterns is important for selecting appropriate
agents for therapy when indicated.
Bacterial Resistance
Enteric bacterial pathogens are becoming increasingly resis-
tant to antimicrobial agents for many reasons, including in-
appropriate and excessive use of antimicrobial agents in hu-
mans
and inclusion of various classes of antimicrobial
agents as growth promoters in feeds of livestock.
Recent
use of an antimicrobial agent in a human, particularly within
the previous 4 weeks, is a documented risk factor for devel-
opment of infection or colonization with resistant bacterial
pathogens.
In many countries of the world, an increase in antimicro-
bial resistance patterns has occurred among the major bacte-
rial enteric pathogens, including Shigella spp, E. coli patho-
130
M. O’Ryan, V. Prado, and L.K. Pickering
types associated with diarrhea, C. jejuni/coli, and Salmonella
spp. These resistance patterns frequently have shown a pro-
gressive increase over the course of time and have demon-
strated resistance to several classes of antimicrobial agents.
Shigella Species
Shigella strains have become progressively resistant to multi-
ple antimicrobial agents since the introduction of sulfon-
amides, and multiresistance is a global problem. Resistance of
S. flexneri and S. sonnei, the most frequent causes of shigello-
sis, has developed to tetracycline, chloramphenicol, strepto-
mycin, ampicillin, kanamycin, and TMP-SMX less than 10
years after each was licensed for use in humans. Data from the
National Antimicrobial Resistance Monitoring System
(NARMS) in the United States show that in 2001 resistance of
Shigella isolates (70% of which were S. sonnei) to ampicillin
was approximately 80 percent and to TMP-SMX was 47 per-
cent.
None of the isolates was resistant to ceftriaxone, imi-
penem, or gentamicin, and only one isolate (0.3%) was resis-
tant
to
ciprofloxacin.
Susceptibility
testing
against
azithromycin was not performed. Similar resistance patterns
have been reported from England and Wales,
and Germany.
In economically developing countries, cur-
rent data from Chile indicate that most Shigella spp. are re-
sistant to ampicillin, TMP/SMX, tetracycline, and chloram-
phenicol and are susceptible to ciprofloxacin and extended
spectrum cephalosporins.
Reports from Bangladesh,
where shigellosis is highly endemic, show a similar resistance
pattern.
Outbreaks caused by multiresistant S. dysenteriae
type 1, including strains resistant to ciprofloxacin, has been
reported.
Neither ampicillin nor TMP-SMX should be
considered appropriate empiric therapy for shigellosis. Rec-
ommended therapy of people infected with Shigella includes
fluoroquinolones, azithromycin, and extended-spectrum
cephalosporins. To optimize therapy, one should know local
susceptibility patterns.
C. jejuni and C. coli
More than 16 species of Campylobacter have been identified,
but not all of them infect humans. Most episodes of Campy-
lobacter-associated diarrhea are caused by C. jejuni/coli
strains. Azithromycin, erythromycin, or fluoroquinolones
are the agents of choice for therapy of gastroenteritis caused
by C. jejuni/coli. Erythromycin resistance in most economi-
cally developed and developing countries generally is stable
at less than 5 percent,
including strains isolated from
However, in some countries, higher resistance
rates to erythromycin have been reported.
Strains that
demonstrate high-level resistance to erythromycin also man-
ifest resistance to azithromycin and clarithromycin.
Resistance to fluoroquinolones in human strains has
ranged from 3 to 96 percent. Data from NARMS in the United
States show that in 2001, 18 percent of C. jejuni/coli isolates
were resistant to ciprofloxacin.
In studies from countries
throughout the world, including Austria, Canada, Germany,
Finland, Norway, and the Netherlands, resistance has in-
creased from 9 to 30 percent.
A high frequency of cross-
resistance has been reported among the fluoroquinolo-
nes.
In
several
countries,
the
increase
in
fluoroquinolone resistance coincided with initiation of ad-
ministration of a fluoroquinolone compound to animal food
or use in veterinary animals.
These studies highlight
the importance of being familiar with local or regional resis-
tance patterns when making decisions about therapy.
Table 3 Antimicrobial Therapy for Enteric Pathogens
Organism
Drug of Choice
Alternative Drugs
Campylobacter Spp.
Azithromycin or erythromycin
Fluoroquinolone
Tetracycline
Gentamicin
Clostridium difficile
Metronidazole
Oral vancomycin
Nontyphi
Salmonella
Cefotaxime
Ceftriaxone
Fluoroquinolone
Ampicillin
TMP/SMX
Chloramphenicol
Shigella
Fluoroquinolone
Azithromycin
Nalidixic acid
TMP/SMX
Ceftriaxone
Vibrio cholerae
Doxycycline if >8 years of age
TMP/SMX
Fluoroquinolone
Chloramphenicol
Furazolidone
E. histolytica
Metronidazole followed by Iodoquinol
Tinidazole
Secnidazole
Ornidazole
G. lamblia
Metronidazole
Tinadazole
Quinacrine
Furazolidone
Paramomycin (pregnant women)
Cryptosporidium parvum
Nitazoxanide
Paramomycin
ⴙ azythromicin
Isospora belli
TMP/SMX
Cyclospora cavetanensis
TMP/SMX
Pediatric diarrheal illness in the developing world
131

Salmonella Species
The type of syndrome produced by nontyphoidal Salmonella
strains dictates the selection and duration of antimicrobial
therapy. Problems with use of antimicrobial agents among
persons who are nontyphoidal Salmonella carriers or in pa-
tients who have mild gastroenteritis are lack of clinical effec-
tiveness,
conversion of intestinal carriage to systemic dis-
ease with bacteremia,
production of bacteriologic and
symptomatic relapse,
development or selection of resis-
tant strains, and prolonged periods of fecal excretion.
In
NARMS data from the United States, the 16 most common
serotypes accounted for 80 percent of isolates that were se-
rotyped. The two serotypes most commonly identified, Ty-
phimurium (23%) and Enteritidis (20%), showed differences
in resistance to five or more antimicrobial agents, 35 percent
and 1 percent, respectively. Only 2 percent of isolates were
resistant to TMP-SMX, 2 percent to ceftriaxone, and 0.2 per-
cent to ciprofloxacin. Worldwide antimicrobial resistance to
Salmonella strains is a common finding,
but specific
serotypes responsible for causing infection and the degree of
resistance of specific serotypes differ by geographic location.
Data collected from seven cities in Argentina reported resis-
tance rates of 35 percent, 14 percent, and 42 percent against
ampicillin, chloramphenicol, and TMP/SMX, respectively.
Shiga Toxin-Producing
E. coli (STEC)
The STEC most commonly isolated in the United States is E.
coli 0157:H7. Other STEC types, such as O26:H11, O45,
O55:H7, O55:H10, O111:H8, O111:H30, O111:H34,
O113, O121, and O145, are found more commonly in other
countries.
Antimicrobial resistance patterns of various ani-
mal and human STEC strains have been reported, with resis-
tance noted to ampicillin, sulfamethoxazole, tetracycline,
streptomycin, and TMP-SMX.
Resistance is associated
with country of origin or source of the isolates tested. In the
2001 NARMS data, of 277 E. coli 0157:H7 isolates tested, 9
percent were resistant to one or more antimicrobial agents, 5
percent were multidrug-resistant, 5 percent were resistant to
sulfamethoxazole, 5 percent to tetracycline, 2 percent to am-
picillin, and 2 percent to streptomycin; none was resistant to
ceftriaxone, ciprofloxacin, amikacin, or imipenem.
Data
from Chile for O157 and non-O157 STEC isolates obtained
from clinical and food origins showed that strains were 100
percent susceptible to ampicillin, TMP/SMX, ciprofloxacin,
chloramphenicol, tetracycline, aminoglycosides, and ex-
tended spectrum cephalosporins.
Antimicrobial therapy of children infected with STEC is
not recommended because of the potential for bacteriophage
induction with enhanced cytotoxin production, leading to
development of HUS by certain classes of antimicrobial
agents.
A meta-analysis showed no benefit or increased
risk for sequelae from therapy of children with STEC intesti-
nal infection.
Effect of Resistance on Clinical
Manifestations and Treatment Options
Clinical manifestations of enteric infections include signs and
symptoms involving the gastrointestinal tract, dissemination
of organisms to sites outside the gastrointestinal tract, neu-
rologic manifestations, and immune-mediated sequelae. Peo-
ple infected with enteric pathogens that are resistant to fre-
quently used antimicrobial agents may manifest as either
clinical or bacteriologic treatment failures
and may
have an extended duration of excretion of viable organ-
isms.
Prevention
The most important aspect in control of diarrheal disease is
hygiene, both general and personal. General issues deal with
clean water, clean food, and appropriate sanitation facilities.
Despite the high-quality water and food supplies available in
the United States and other socioeconomically developed ar-
eas of the world, outbreaks of foodborne and waterborne
disease continue to occur, generally due to improper han-
dling and storage of food.
Personal measures include care-
ful personal hygiene, especially handwashing, and limited
use of antacids, antimotility drugs, and antimicrobial agents.
Promotion of handwashing has proven to be a highly effec-
tive measure in decreasing the incidence of diarrhea among
people living in high-risk areas, such as settlements in Paki-
stan.
Appropriate diaper-changing facilities and tech-
niques should be available and implemented in childcare
facilities. Breastfeeding in all areas of the world should be
promoted, implemented, and supported.
The number of immunizations available to prevent enteric
infections is scarce but expected to increase in the future with
development of new technologies including delivery mecha-
nisms (
Vaccines against Salmonella serotype
Typhi are the only vaccines against enteric diseases commer-
cially available in the United States (
). Currently, two
vaccines are licensed for cholera prevention. The oral live
Table 4 Vaccines Currently or Soon-to-Be Available to Prevent Enteric Infections
Organism
Vaccine
Type
Route of
Administration
Age
Vibrio cholerae
CVD-103HgR
Live attenuated
Oral
>
2 years
B-WC
Inactivated
Oral
all ages
Salmonella serotype typhi
Ty21A
Live attenuated
Oral
>
6 years
ViCPS
Polysaccharide
Intramuscular
>
2 years
Rotavirus
Monovalent
Live attenuated
Oral
2,4 months
Pentavalent
Live attenuated
Oral
2,4,6 months
132
M. O’Ryan, V. Prado, and L.K. Pickering

genetically attenuated CVD 103HgR (Orochol®, Berna Bio-
tech, Bern, Switzerland) has demonstrated 100 percent pro-
tection against severe cholera, but protection is not long-
lasting (14% of individuals living in endemic areas were
protected 4 years after vaccination). This vaccine is indicated
for individuals older than 2 years of age traveling to a cholera-
endemic area.
The inactivated whole cell vaccine with B
subunit has proven to be safe and effective up to 3 years after
vaccination in Bangladesh. Two doses conferred 70 percent
protection in adults but only 25 percent in children.
Live
genetically attenuated vaccines for Shigella are in different
stages of development. These vaccines are serotype-specific,
meaning that multivalent vaccines will be required to protect
against the most prevalent serotypes worldwide (eg, Shigella
dysenterie type 1, S. sonnei, and S. flexneri 2a, 3a, and 6
Vaccines to prevent rotavirus (RV) have been shown to be
but the association of the rhesus RV vaccine with
intussusception resulted in withdrawal of this vaccine from
the U.S. market in October 1999, following licensure in Au-
gust of 1998. This vaccine has not been licensed in any other
country of the world. A vaccine of lamb origin has been used
in China for years, but its safety and efficacy profile are un-
known. Phase III studies evaluating two new vaccines to pre-
vent infection with RV are nearing completion or have been
finalized. The efficacy of these vaccines against severe RV
gastroenteritis surpasses 80 percent and against any RV gas-
troenteritis, regardless of severity, is approximately 70 per-
cent. One vaccine is a G1 human attenuated monovalent
vaccine that has been tested in Latin America and Finland.
The other vaccine is a G1, G2, G3, G4, and P1A[8] bovine-
human reassortant pentavalent vaccine tested in the United
States, Europe, and in a few Latin American countries. The
monovalent RV vaccine has been licensed in Mexico for in-
fants and should be available in early 2005 (Vaccine Enteric
Disease Meeting, Jamaica 2004). There are no licensed vac-
cines against parasitic enteric infection. Vaccines against
other enteric pathogens and improved vaccines against
pathogens for which immunizations are available are under-
going study.
Nonspecific agents that may interfere with microbial ad-
herence or with the virulence mechanisms of toxins are being
developed and evaluated, as are compounds that will serve as
competitors for binding of organisms or toxins to receptors in
the intestine. The use of glycoconjugates and probiotics in
prevention and treatment of diarrheal disease may be bene-
ficial and is undergoing investigation.
Breastfeeding provides young infants with significant pro-
tection against morbidity and mortality due to diarrheal dis-
ease.
In part, breastfeeding protects against diarrhea
through decreased exposure of breastfed infants to organisms
present on or in contaminated bottles, food, or water. In
addition, immunologic components in human milk protect
infants against disease after exposure to an infectious agent.
References
1. Prashar U, Bresee J, Glass R: The global burden of diarrheal disease in
children. Bull World Health Organization 81:236, 2003
2. Prashar UD, Hummelman EG, Bresee J, et al: Global illness and deaths
caused by rotavirus disease in children. Emerg Infect Dis 9:565-572,
2003.
3. Kosek M, Bern C, Guerrant RL: The global burden of diarrhoeal dis-
ease, as estimated from studies published between 1992 and 2000.
Bull World Health Organ 81:197-204, 2003
4. Yoon PW, Black RE, Moulton LH, et al: The effect of malnutrition on
the risk of diarrheal and respiratory mortality in children
⬍2 y of age
in Cebu, Philippines. Am J Clin Nutr 65:1070-1077, 1997
5. Teka T, Faruqye AS, Fuch GJ: Risk factors for deaths in under-age-five
children attending a diarrhoeae treatment center. Acta Pediatr 85:
1070-1075, 1996
6. Black RE, Epstein LD, Cabrera L, et al: Effect of water and sanitation
on childhood health in a poor Peruvian peri-urban community. Lan-
cet 363:112-118, 2004
7. Luby SP, Agboatwalla M, Painter J, et al: Effect of intensive handwash-
ing promotion of childhood diarrhea in high-risk communities in
Pakistan. JAMA 2921:2547-2554, 20004
8. 2004 World Resource Institute. Earth Trends 2003. Available at
; Internet; accessed January 13, 2005.
9. Prado V, O’Ryan M: Acute Gastroenteritis in Latin America. Infect Dis
Clin North Am 8:77-106, 1994
10. Ferreccio C, Prado V, Ojeda A, et al: Epidemiologic patterns of acute
diarrhea and endemic Shigella infections in children in a Poor periur-
ban setting in Santiago, Chile. Am J Epidemiol 134:614-662, 1991
11. Popkin BM, Adair L, Akin JS, et al: Breast-feeding and diarrheal mor-
bidity. Pediatrics 86:8741990
12. Morrow AL, Pickering LK: Human milk and infectious diseases, in
Long SS, Pickering LK, Prober CG, (eds) Principles and Practice of
Pediatric Infectious Diseases. 2nd edition, New York: Churchill-Liv-
ingstone; 2003:80-87
13. Feachem RG, Koblinsky MA: Interventions for the control of diar-
rhoeal diseases among young children: promotion of breast-feeding.
Bull World Health Organ 62:271-291, 1984
14. Rahman MM, Vermund S, Wahed MA, et al: Simultaneous zinc and
vitamin A supplementation in Bangladesh children: randomized dou-
ble blind controlled trial. BMJ 323:314-318, 2001
15. O’Ryan M, Vial PA, Mamani N, et al: Norwalk virus and MX virus
seroprevalence in chilean individuals: assessment of independent risk
factors for antibody acquisition. Clin Infect Dis 27:789-795, 1998
16. Gaggero A, O’Ryan M, Noel J, et al: Prevalence of astrovirus infection
among Chilean children with acute gastroenteritis. J Clin Microbiol
36:3691-3693, 1998
17. O’Ryan ML, Mamani N, Gaggero A, et al: Human caliciviruses are a
significant pathogen of acute diarrhea in children of Santiago, Chile.
J Infect Dis 182:1519-15122, 2000
18. O’Ryan M, Pérez-Schael I, Mamani N, et al: Rotavirus-associated med-
ical visits and hospitalizations in South America: a prospective study
at three large sentinel hospitals. Pediatr Infect Dis J 20:685-693, 2001
19. Bresee J, Fang Z, Wang B, et al: First report from the Asian Rotavirus
Surveillance Network. Emerg Infect Dis 6:988-995, 2004
20. Matson DO, O’Ryan ML, Jiang X, et al: Rotavirus, enteric adenovi-
ruses, caliciviruses, astroviruses, and other viruses causing gastroen-
teritis, in Spector S, Hodinka RJ, Young SA, (eds). Clinical Virology
Manual, 3rd ed. Washington DC, ASM Press, 2000:270-294
21. Albert MJ, Faruque AS, Faruque SM, et al: Case-control study of
enteropathogens associated with childhood diarrhea in Dhaka, Bang-
ladesh. J Clin Microbiol 11:3458-3464, 1999
22. Kageyama T, Shinohara M, Uchida K, et al: Coexistence of multiple
genotypes, including new identified genotypes, in outbreaks of gas-
troenteritis due to Norovirus in Japan. J Clin Microbiol 42:2988-
2995, 2004
23. Glass RI, Noel J, Mitchell D, et al: The changing epidemiology of
astrovirus-associated gastroenteritis. Arch Virol 1996;12:287-300
(suppl)
24. Torres ME, Pirez MC, Schelotto F, et al: Etiology of children’s diarrhea
in Montevideo, Uruguay: associated pathogens and unusual isolates.
J Clin Microbiol 39:2134-2139, 2001
25. Medeiros MI, Neme S, Silva P, et al: Etiology of acute diarrhea among
Pediatric diarrheal illness in the developing world
133

children in Riberao Preto-SP, Brazil. Rev Inst Med Trop S. Paulo
43:21-24, 2001
26. Vargas M, Gascon J, Casalas C, et al: Etiology of diarrhea in children
less than five years of age in Ifkara, Tanzania. Am J Trop Med Hyg
70:536-539, 2004
27. Haque R, Mondal D, Kirckpatrick BD, et al: Epidemiologic and clini-
cal characteristics of acute diarrhea with emphasis on Entamoeba his-
tolytica infections in preschool children in an urban slum of Dhaka,
Bangladesh. Am J Trop Med Hyg 69:398-405, 2003
28. Zurawska-Olszewska J, Krzeslowska I, Dlugosz G, et al: Etiology of
acute diarrheas in children from the Lodz region. I. Occurrence of
etiologic agents. Med Dosw Mikrobiol 54:129-136, 2002
29. Youssef M, Shurman A, Bougnox M, et al: Bacterial viral, and parasitic
enteric pathogens associated with acute diarrhea in hospitalized chil-
dren from northern Jordan. FEMS Immunol Med Microbiol 28:257-
263, 2000
30. Phetsouvanh R, Midorikawa Y, Nakamura S: The seasonal variation in
the microbial agents implicated in the etiology of diarrheal diseases
among children in Lao People’s Democratic Republic. Southeast Asian
J Trop Med Public Health 30:319-323, 1999
31. Levine MM, Ferreccio C, Prado V, et al: Epidemiologic studies of
Escherichia coli diarrheal infections in a low socioeconomic level peri-
urban community in Santiago, Chile. Am J Epidemiol 128:849-869,
1993
32. López E, Prado V, O’Ryan M, et al: Shigella and shiga toxin-producing
Escherichia coli causing bloody diarrhea in Latin America. Infect Dis
Clin North Am 14:41-65, 2000
33. Prado V, Martinez J, Arellano C, et al: Variación temporal de genotipos
y serogrupos de E. coli enterohemorrágicos aislados en niños chilenos
con infecciones intestinales o síndrome hemolítico-urémico. Rev Med
Chile 125:291-297, 1997
34. Tporovsky MS, Mimica IM, Chieffi PP, et al: Diarreia aguda em crian-
cas menores de 3 anos de idade: recuperacao de enteropatogenos nas
amostras fecais de pacientes compara a grupo controle. J Pedaitr (Rio
J) 75:97-104, 1999
35. Ali AM, Qureshi AH, Rafi S, et al: Frequency of Campylobacter jejuni in
diarrhea/dysentery in children in Rawalpindi and Islamabad. J Pak
Med Assoc 52:517-520, 2003
36. Rao MR, Naficy AB, Savarino SY, et al: Pathogenicity and convalescent
excretion of Campylobacter in rural Egyptian children. Am J Epide-
miol 154:166-173, 2001
37. Alcalde Martin C, Gomez Lopez L, Carrascal A, et al: Gastroenteritis
aguda en pacientes hospitalizados. Estudio evolutivo de 14 años.
Anales Españoles de Pediatría 56:104-110, 2002
38. Patrick ME, Adcock PM, Gomez TM, et al: Salmonella enteritidis
infections, United Status 1985-1999. Emerg Infect Dis 10:1-7, 2004
39. Sack D, Sack B, Balakrish Nair G, et al: Cholera. Lancet 363:223-233,
2004
40. Haque R, Huston C, Hughes M, et al: Amebiasis. N Engl J Med 348:
1565-1573, 2003
41. Pickering LK, Woodward WE, DuPont HL, et al: Occurrence of G.
lamblia in children in day care centers. J Pediatr 104:522, 1984
42. Adam RD: The biology of Giardia spp. Microbiol Rev 55:7061991
43. Pickering LK, Engelkirk PG: Giardia lamblia. Pediatr Clin North Am
35:565, 1988
44. Miotti PG, Gilman RH, Santosham M, et al: Age-related rate of sero-
positivity and antibody to Giardia lamblia in four diverse populations.
J Clin Microbiol 24:972, 1986
45. Xiao L, Fayer R, Ryan U, et al: Cryptosporidium taxonomy: recent
advances and implications for public health. Clin Microbiol Rev 17:
72-97, 2004
46. Goodgame RW: Understanding intestinal spore-forming protozoa:
cryptosporidia, microsporidia, isospora, and cyclospora. Ann Interm
Med 124:429-441, 1996
47. Tzipori S: Cryptosporidiosis in animals and humans. Microbiol Rev
47:84, 1983
48. Navin TR: Cryptosporidiosis in humans: review of recent epidemio-
logic studies. Eur J Epidemiol 1:77, 1985
49. Alpert G, Bell LM, Kirkpatrick CE, et al: Outbreak of cryptosporidiosis
in a day care center. Pediatrics 77:152, 1986
50. Taylor JP, Perdue JN, Dingley D, et al: Cryptosporidiosis outbreak in
a day care center. Am J Dis Child 139:1023, 1986
51. Hoxie NJ, Davis JP, Vergeront JM, et al: Cryptosporidiosis-associated
mortality following a massive waterborne outbreak in Milwaukee,
Wisconsin. Am J Public Health 87:2032, 1997
52. Jokipii L, Pohiola S, Jokipii AM: Cryptosporidium: a frequent finding in
patients with gastrointestinal symptoms. Lancet 2:358, 1983
53. Current WL, Reese NC, Ernst JV, et al: Human cryptosporidiosis in
immunocompetent and immunodeficient persons: studies of an out-
break and experimental transmission. N Engl J Med 308:1252, 1983
54. Sallon S, Deckelbaum RI, Schmid II, et al: Cryptosporidium, malnutri-
tion and chronic diarrhea in children. Am J Dis Child 142:312, 1988
55. Herwaldt BL: Cyclospora cayetanensis: a review, focusing on the out-
breaks of cyclosporiasis in the 1990s. Clin Infect Dis 31:1040-1057,
2000
56. Lindsay DS, Dubey JP, Blagburn BL: Biology of Isospora spp. from
humans, nonhuman primates, and domestic animals. Clin Microbiol
Rev 10:19-34, 1997
57. Didier ES: Microsporidiosis. Clin Infect Dis 27:1-7, 1998
58. Bhan MK, Khoshoo V, Sommerfelt H, et al: Enteroaggregative Esche-
richia coli and Salmonella associated with nondysenteric persistent
diarrhea. Pediatr Infect Dis J 8:499-502, 1989
59. Bhan MK, Raj P, Levine MM, et al: Enteroaggregative Escherichia coli
associated with persistent diarrhea in a cohort of rural children in
India. J Infect Dis 159:1061-1064, 1989
60. Bhatnagar S, Bhan MK, Sommerfelt H, Sazawal S, Kumar R, Saini S:
Enteroaggregative Escherichia coli may be a new pathogen causing
acute and persistent diarrhea. Scand J Infect Dis 25:579-583, 1993
61. Fang GD, Lima AAM, Martins CV, et al: Etiology and epidemiology of
persistent diarrhea in northeastern Brazil: a hospital-based, prospec-
tive, case-control study. J Pediatr Gastroenterol Nutr 21:137-144,
1995
62. WHO/CDR/95.3 The treatment of diarrhoea: a manual for physicians
and other senior health workers. Available at:
; Internet; accessed January 13, 2005.
63. Guerrant R, Van Gilder T, Steiner T, et al: Practice guidelines for the
management of Infectious diarrhea. Clin Infect Dis 32:331-351, 2001
64. Hines J, Nachamkin I: Effective use of the clinical microbiology labo-
ratory for diagnosing diarrheal disease. Clin Infect Dis 23:1292-1301,
1996
65. Ojeda A, Marinkovic K, Prado V, et al: Rendimiento comparativo de
diferentes esquemas de trabajo para aislamiento de enteropatógenos
en coprocultivo. Rev Chile Infect 13:137-144, 1996
66. Corry JE, Post DE, Colin P, et al: Culture media for the isolation of
Campylobacter. Int J Food Microbiol 26:43-76, 1995
67. García LS, Shimizu R: Evaluation of nine immunoassay kits (enzyme
immunoassay and direct fluorescence) for detection of Giardia lamblia
and Cryptosporidium parvum in human fecal specimens. J Clin Micro-
biol 35:1526-1529, 1997
68. Gicquelais KG, Baldini MM, Martínez J, et al: Practical and economical
method for using biotinylated DNA probes with bacterial colony blots
to identify diarrhea-causing Escherichia coli. J Clin Microbiol 28:2485-
2490, 1990
69. Vidal R, Vidal M, Lagos R, et al: Multiplex PCR for diagnosis of enteric
infections associated to diarrheagenic Escherichia coli. J Clin Microbiol
42:1787-1789, 2004
70. Thiem VD, Sethabutr O, von Seidlein L, et al: Detection of Shigella by
a PCR assay targeting the ipaH gene suggests increased prevalence of
shigellosis in Nha Trang, Vietnam. J Clin Microbiol 42:2031-2035,
2004
71. Blessmann J, Buss H, Phuong A, et al: Real-time PCR for detection and
differentiation of Entoamoeba histolytica and Entoamoeba dispar in fecal
samples. J Clin Microbiol 12:4413-4417, 2002
72. Gill C, Lau J, Gorbach SL, et al: Diagnostic accuracy of stool assays for
inflammatory bacterial gastroenteritis in developed and resource-poor
countries Clin Infect Dis 37:365-376, 2003
73. Choi SW, Park CH, Silva TM, et al: To culture or not to culture: fecal
134
M. O’Ryan, V. Prado, and L.K. Pickering

lactoferrin screening for inflammatory bacterial diarrhea. J Clin
Microbiol 34:928-932, 1996
74. Ruiz-Pelaez JG, Mattar S. Accuracy of fecal lactoferrin and other stool
tests for diagnosis of invasive diarrhea at a Colombian pediatric hos-
pital Pediatr Infect Dis J 18:342-346, 1999
75. Huicho L, Campos M, Rivera J, et al: Fecal screening tests in the
approach to acute infectious diarrhea: a scientific overview. Pediatr
Infect Dis J 15:486-494, 1996
76. King CK, Glass R, Bresee JS, et al: The management of acute gastro-
enteritis in children: oral rehydration, maintenance, and nutrition
therapy. MMWR 52:1-16, 2003
77. Pickering LK, Cleary TG: Therapy for diarrheal illness in children: in
Blaser MJ, Smith, PD, Ravdin JI, et al, (eds). Infections of the Gastro-
intestinal Tract. 2nd ed. New York, Raven Press, 1223-1240:2002
78. Pickering LK: Antimicrobial resistance among enteric pathogens. Se-
min Pediatr Infect Dis 15:71-75, 2004
79. Eng JV, Marcus R, Hadler JL, et al: Consumer attitudes and use of
antibiotics. Emerg Infect Dis 9:1128-1135, 2003
80. Angulo FJ, Baker NL, Olsen SJ: Antimicrobial use in agriculture: con-
trolling the transfer of antimicrobial resistance to humans. Semin
Pediatr Infect Dis 15:78-85, 2004
81. Institute of Medicine. The Resistance Phenomenon in Microbes and
Infectious Disease Vectors Implications for Human Health and Strat-
egies for Containment-Workshop Summary (2003)
82. World Health Organization. Containing Antimicrobial Resistance Re-
view of the Literature and Report of a WHO Workshop on the Devel-
opment of a Global Strategy for the Containment of Antimicrobial
Resistance Geneva, Switzerland, February 4-5, 1999
83. National Center for Infectious Diseases. Centers for Disease Control
and Prevention. National Antimicrobial Resistance Monitoring Sys-
tem (NARMS) for Enteric Bacteria web site. Available at
; Internet; accessed January 13, 2005.
84. Cheasty T, Skinner JA, Rowe B, et al: Increasing incidence of antibiotic
resistance in shigellas from humans in England and Wales: recom-
mendations for therapy. Microb Drug Resist 4:57-60, 1998
85. Harnett N: High level resistance to trimethoprim, cotrimoxazole and
other antimicrobial agents among clinical isolates of Shigella species in
Ontario, Canada—an update. Epidemiol Infect 109:463-472, 1992
86. Aleksic S, Katz A, Aleksic V, et al: Antibiotic resistance of Shigella
strains isolated in the Federal Republic of Germany 1989-1990. Zen-
tralbl Bakteriol 279:484-493, 1993
87. Prado V, Pidal P, Arellano C, et al: Multiresistencia antimicrobiana en
cepas de Shigella sp en una comuna semirural del área norte de
Santiago. Rev Med Chile 126:1464-1471, 1988
88. Pidal P, Prado V, Trucco O, et al: Panorama de la resistencia de
Shigella sp. en 10 hospitales chilenosRev Panam Infectol 3:S18-S25,
1988 (Suppl 1)
89. Sur D, Niyogi SK, Sur S, et al: Multidrug-resistant shigella dysenteriae
type 1: forerunners of a new epidemic strain in Eastern India? Emerg
Infect Dis 9:404-405, 2003
90. Pal SC: Epidemic bacillary dysentery in West Bengal. Lancet 1:1462,
1984
91. Khan AI, Huq S, Malek MA, et al: Shigella serotypes among hospital-
ized patients in urban Bangladesh and their antimicrobial resistance.
Epidemiol Infect 132:773-777, 2004
92. Talsma E, Goettsch WG, Nieste HL, et al: Resistance in Campylobacter
species: increased resistance to fluoroquinolones and seasonal varia-
tion. Clin Infect Dis 29:845-848, 1999
93. Engberg J, Aarestrup FM, Taylor DE, et al: Quinolone and macrolide
resistance in Campylobacter jejuni and C. coli: resistance mechanisms
and trends in human isolates. Emerg Infect Dis 7:24-34, 2001
94. Tjaniadi P, Lesmana M, Subekti D, et al: Antimicrobial resistance of
bacterial pathogens associated with diarrhea patients in Indonesia.
Am J Trop Med Hyg 68:666-670, 2003
95. Reina J, Ros MJ, Serra A: Susceptibilities to 10 antimicrobial agents of
1,220 Campylobacter strains isolated from 1987 to 1993 from feces of
pediatric patients. Antimicrob Agents Chemother 38:2917-2920, 1994
96. Chatzipanagiotou S, Papavasileiou E, Lakumenta A, et al: Antimicro-
bial susceptibility patterns of Campylobacter jejuni strains isolated
from hospitalized children in Athens, Greece. J Antimicrob
Chemother 49:803-805, 2002
97. Hoge CW, Gambel JM, Srijan A, et al: Trends in antibiotic resistance
among diarrheal pathogens isolated in Thailand over 15 years. Clin
Infect Dis 26:341-345, 1998
98. Rautelin H, Vierikko A, Hänninen JL, et al: Antimicrobial susceptibil-
ities of Campylobacter strains isolated from Finnish subjects infected
domestically or from those infected abroad. Antimicrob Agents Che-
mother 47:102-105, 2003
99. Krausse R, Ullmann U: In vitro activities of new fluoroquinolones
against Campylobacter jejuni and Campylobacter coli isolates obtained
from humans in 1980 to 1982 and 1997 to 2001. Antimicrob Agents
Chemother 47:2946-2950, 2003
100. Sam WI, Lyons MM, Waghorn DJ: Increasing rates of ciprofloxacin
resistant Campylobacter. J Clin Pathol 52:709, 1999
101. Sirinavin S, Garner P: Antibiotics for treating Salmonella gut infec-
tions. Cochrane Database Syst Rev CD001167, 2000
102. Rosenthal SL: Exacerbation of Salmonella enteritis due to ampicillin.
N Engl J Med 280:147-148, 1969
103. Neill MA, Opal SM, Heelan J, et al: Failure of ciprofloxacin to eradicate
convalescent fecal excretion after acute salmonellosis: experience during
an outbreak in health care workers. Ann Intern Med 114:195-199, 1991
104. Threlfall EJ, Ward LR: Decreased susceptibility to ciprofloxacin in
Salmonella enterica serotype Typhi, United Kingdom. Emerg Infect Dis
7:448-450, 2001
105. van Duijkeren E, Wannet WJ, Houwers DJ, et al: Antimicrobial sus-
ceptibilities of Salmonella strains isolated from humans, cattle, pigs,
and chickens in the Netherlands from 1984 to 2001. J Clin Microbiol
41:3574-3578, 2003
106. Villa L, Mammina C, Miriagou V, et al: Multidrug and broad-spectrum
cephalosporin resistance among Salmonella enterica serotype Enterit-
idis clinical isolates in southern Italy. J Clin Microbiol 40:2662-2665,
2002
107. Binsztein N, Picandet AM, Notario R, et al: Antimicrobial resistance
among species of Salmonella, Shigella, Escherichia and Aeromonas iso-
lated from children with diarrhea in 7 Argentinian centers. Rev Lati-
noam Microbiol 41:121-126, 1999
108. Schroeder CM, Meng J, Zhao S, et al: Antimicrobial resistance of
Escherichia coli O26, O103, O111, O128, and O145 from animals and
humans. Emerg Infect Dis 8:1409-1414, 2002
109. Reyes M, Durán C, Prado V: Prado V. Antimicrobial susceptibility of
Shiga toxin producing E. Coli (STEC) strains isolated from human
infections and food. Rev Méd Chile 132:1211-1216, 2004
110. Wong CS, Jelacic S, Habeeb RL, et al: The risk of hemolytic-uremic
syndrome after antibiotic treatment of Escherichia coli 0157:H7 infec-
tions. N Engl J Med 342:1930-1936, 2000
111. Zhang X, McDaniel AD, Wolf LE, Keusch GT, et al: Quinolone anti-
biotics induce shiga toxin-encoding bacteriophages, toxin produc-
tion, and death in mice. J Infect Dis 181:664-670, 2000
112. Ohara T, Kojo S, Taneike I, et al: Effects of azithromycin on shiga toxin
production by Escherichia coli and subsequent host inflammatory re-
sponse. Antimicrob Agents Chemother 46:3478-3483, 2002
113. Safdar N, Said A, Gangnon RE, et al: Risk of hemolytic uremic syn-
drome after antibiotic treatment of Escherichia coli 0157:H7 enteritis.
A meta-analysis. JAMA 288:996-1001, 2002
114. Kuschner RA, Trofa AF, Thomas RJ, et al: Use of azithromycin for the
treatment of Campylobacter enteritis in travelers to Thailand, an area
where ciprofloxacin resistance is prevalent. Clin Infect Dis 21:536-
541, 1995
115. Segreti J, Gootz TD, Goodman LJ, et al: High-level quinolone resis-
tance in clinical isolates of Campylobacter jejuni. J Infect Dis 165:667-
670, 1992
116. Helms M, Vastrup P, Gerner-Smidt P, et al: Excess mortality associ-
ated with antimicrobial drug-resistant Salmonella Typhimurium.
Emerg Infect Dis 8:490-495, 2002
117. Nakaya H, Yasuhara A, Yoshimura K, et al: Life-threatening infantile
diarrhea from fluoroquinolone-resistant Salmonella enterica Typhi-
murium with mutations in both gyrA and parC. Emerg Infect Dis
9:255-257, 2003
Pediatric diarrheal illness in the developing world
135

118. Bhutta ZA, Khan IA, Shadmani M: Failure of short-course ceftriaxone
chemotherapy for multidrug-resistant typhoid fever in children: a
randomized controlled trial in Pakistan. Antimicrob Agents Che-
mother 44:450-452, 2000
119. Olsen SJ, MacKinon LC, Goulding JS, et al: Surveillance for foodborne
disease outbreaks –United States, 1993-1997. MMWR 49:1-5, 2000
120. Luby SP, Agboatwalla M, Painter J, et al: Effect of intensive handwash-
ing promotion on childhood diarrhea in high-risk communities in
Pakistan. JAMA 291:2547-2554, 2004
121. Nataro JP, Barry EM: Diarrheal disease vaccines, in Plotkin S, Oren-
stein WA, (eds). Vaccines. 4th ed. Philadelphia: WB Saunders; 2004:
1209-1217
122. Richie EE, Punjabi NH, Sidharta YY, et al: Efficacy trial of a single-dose
live oral cholera vaccine CVD 103-HgR in North Jakarta, Indonesia, a
cholera-endemic area. Vaccine 18:2399-2410, 2000
123. Clemens JD, Sack DA, Harris JR, et al: Field trial of oral cholera
vaccines in Bangladesh: Results from three years follow-up. Lancet
355:2701990
124. Hale TL, Venkatesan MM: Vaccines against Shigella Infection. In: Le-
vine MM, Woodrow GC, Kaper JB, Cobon GS, editors. New Genera-
tion Vaccines. 2nd ed. New York: Marcel Dekker, Inc., 1997:843-852
125. American Academy of Pediatrics. Committee on Infectious Diseases:
Prevention of rotavirus disease: guidelines for use of rotavirus vaccine.
Pediatrics 102:1483-1491, 1998
126. Newburg DS: Oligosaccharides and glycoconjugates in human milk:
their role in host defense. J Mammary Gland Biol Neoplasia 1:271-
283, 1996
127. Morrow AL, Ruiz-Palacios GM, Altaye M, et al: Human milk oligosac-
charides are associated with protection against diarrhea in breast-fed
infants. J Pediatr 145:297-303, 2004
128. Pickering LK, Morrow AL, Ruiz-Palacios GM, et al: Protecting infants
through human milk. Advancing the scientific evidence. Advances in
experimental medicine and biology. New York, Kluwer Academic/
Plenum Publishers, 554:1-525, 2004
129. American Academy of Pediatrics. Policy statement. Breastfeeding and
the use of human milk. Pediatrics, 115:496-506, 2005
136
M. O’Ryan, V. Prado, and L.K. Pickering
Document Outline
- A Millennium Update on Pediatric Diarrheal Illness in the Developing World
Wyszukiwarka
Podobne podstrony:
Dell'Osso Epidemiologic and clinical updates on impulse control disorder
2003 2 MAR Update on clinical veterinary behavior
Haisch Update on an Electromagnetic Basis for Inertia, Gravitation, Principle of Equivalence, Spin
Millennium's End Terror on the Constantinople
Zinc, diarrhea, and pneumonia The Journal of Pediatrics, December 1999, Vol 135
David Icke The Illuminati Rituals On The False Millenium And Coming Age Of Light
Enteric infections, diarrhea and their impact on function and development
More on hypothesis testing
ZPSBN T 24 ON poprawiony
Fizjoterapia w pediatrii ortopedia
KIM ON JEST2
Prawne aspekty pracy pediatry
Propedeutyka Pediatrii wykłady dodatkowe
Parzuchowski, Purek ON THE DYNAMIC
Foucault On Kant
więcej podobnych podstron