Everyday English for International Nurses
A guide to working in the UK
C3996_00.qxd 26/02/2004 13:42 Page i
For Churchill Livingstone:
Commissioning Editor: Ninette Premdas
Development Editor: Kim Benson
Project Manager: Darren Smith
Design: Erik Bigland
C3996_00.qxd 26/02/2004 13:42 Page ii
Everyday English for
International Nurses
A guide to working in the UK
EDINBURGH
LONDON
NEW YORK
PHILADELPHIA
SAN FRANCISCO
SYDNEY
TORONTO
2004
Joy Parkinson
BA
Author and Lecturer, London, UK
Chris Brooker
BSc, MSc, RGN, SCM, RNT
Author and Lecturer, Norfolk, UK
C3996_00.qxd 26/02/2004 13:42 Page iii
CHURCHILL LIVINGSTONE
An imprint of Elsevier Limited
© 2004, Elsevier Limited. All rights reserved.
First published 2004
The right of Joy Parkinson and Chris Brooker to be identified as
authors of this work has been asserted by them in accordance with
the Copyright, Designs and Patents Act 1988.
No part of this publication may be reproduced, stored in a retrieval
system, or transmitted in any form or by any means, electronic,
mechanical, photocopying, recording or otherwise, without either the
prior permission of the publishers or a licence permitting restricted
copying in the United Kingdom issued by the Copyright Licensing
Agency Ltd, 90 Tottenham Court Road, London W1T 4LP, UK.
Permissions may be sought directly from Elsevier's Health Sciences
Rights Department in Philadelphia, USA: (+1) 215 238 7869,
fax: (+1) 215 238 2239, e-mail: healthpermissions@elsevier.com. You
may also complete your request on-line via the Elsevier Science
homepage (http://www.elsevier.com), by selecting ‘Customer Support’
and then ‘Obtaining Permissions’.
ISBN 0 443 07399 6
British Library of Cataloguing in Publication Data
A catalogue record for this book is available from the British Library.
Library of Congress Cataloging in Publication Data
A catalog record for this book is available from the Library of Congress.
Note
Medical knowledge is constantly changing. As new information
becomes available, changes in treatment, procedures, equipment and
the use of drugs become necessary. The authors/contributors and the
publishers have taken care to ensure that the information given in this
text is accurate and up to date. However, readers are strongly advised
to confirm that the information, especially with regard to drug usage,
complies with current legislation and standards of practice.
Printed in China
C3996_00.qxd 26/02/2004 13:42 Page iv
Preface
This book is designed to help the large numbers of overseas nurs-
es who have chosen to practise in the UK. The content has been
adapted from the Manual of English for the Overseas Doctor, by
Joy Parkinson. The result is a book with a uniquely nursing focus.
It can be a daunting prospect for anyone to move to another
country to nurse; not only must you become familiar with the
organisation and regulation of nursing, but you need to learn how
English is spoken by people in everyday situations. The language
spoken by clients, patients and their families in the UK is vastly
different from that used overseas. Hence a large part of the book
is concerned with the vocabulary and language used in the
nurse–patient relationship.
The first three chapters provide information about nursing in
the UK, the nursing process, professional organisations and trade
unions, registering as a nurse, adaptation programmes and career
development, and the structure of the National Health Service
and Social Services.
Chapter 4 focuses on documentation and record keeping that
are vital to good practice. This chapter also deals with written
communication in the form of letters and e-mail.
Communication in nursing is covered in Chapter 5. This
includes taking a nursing history and many case-history dialogues.
The case histories are based on the Activities of Living Model of
Nursing and provide examples of dialogue between nurses and
patients or relatives in a wide range of situations.
Chapters 6 to 8 deal with the language of spoken English (col-
loquial English, idioms and phrasal verbs). This material is based
on the book for doctors, but it has been completely updated for
the 21st century.
v
C3996_00.qxd 26/02/2004 13:42 Page v
The last three chapters provide you with more useful informa-
tion – abbreviations used in nursing, useful addresses and web
sources, and units of measurement.
Further reading suggestions and references are included in the
chapters, and a general list of further reading is provided at the
end of the book.
We hope that this new book will be of great help to you during
your nursing career in the UK.
Joy Parkinson and Chris Brooker
London and Norfolk 2004
PREFACE
vi
C3996_00.qxd 26/02/2004 13:42 Page vi
Acknowledgements
The authors would like to thank their families and colleagues for
their support and help.
Thanks to Gosia Brykczynska who wrote the first three chapters.
Thanks also to Annie Jennings, RGN, and Andrew Jennings,
MB, FRCS(Urol), for their help in updating the colloquial language,
to Kirsten and Stuart Dallas who offered help with one of the case
histories, and to all the staff at Elsevier who were involved in the
book – in particular, Ninette Premdas and Kim Benson for their
support and enthusiasm throughout the project.
vii
C3996_00.qxd 26/02/2004 13:42 Page vii
Contributor
Gosia Brykczynska PhD, RGN/RSCN, RNT, CertEd, Refugee Nurse
Project Officer, Royal College of Nursing, London, UK (Chs 1, 2
and 3).
C3996_00.qxd 26/02/2004 13:42 Page viii
Contents
1.
Nursing in the UK
1
2.
Registering as a nurse in the UK and career
development
13
3.
The National Health Service and Social Services
25
4.
Nursing documentation, record keeping and written
communication
37
5.
Communication in nursing
51
6.
Colloquial English
123
7.
Idioms: parts of the body
141
8.
Phrasal verbs
169
9.
Abbreviations used in nursing
193
10. Useful addresses and web sources
211
11. Units of measurement
223
General further reading suggestions
231
Index
233
ix
C3996_00.qxd 26/02/2004 13:42 Page ix
C3996_00.qxd 26/02/2004 13:42 Page x
This page intentionally left blank
Nursing in the UK
INTRODUCTION
Today nursing in the UK involves caring for the whole person
(holistic care). This includes emotional, social, psychological,
spiritual and physical factors rather than just a disease or injury.
Nursing care is based on the best evidence available (evidence-
based) and focuses on the individual needs of people using the
healthcare system. Nurses are concerned as much with helping
people to stay well, as with giving care when illness or injury
occurs. Promoting health, giving information and helping people
to learn about managing chronic illnesses is the focus of nursing
in the 21st century. The developments in medical science and
technology, and the breakdown in the traditional barriers
between the healthcare professions have meant that nurses must
now deal with many complex technical aspects of care and treat-
ment. Nursing in the UK is a regulated professional occupation
with a correspondingly thorough education system that meets the
practical and theoretical needs of a modern healthcare system.
Nurse education in the UK is designed to meet changing health-
care needs, the wishes of people needing healthcare, the growth
in complex treatments and the need for a standardised education-
al preparation resulting from membership of the European Union
(EU) (see Ch. 2).
Nurses in the UK base their practice on the systematic assess-
ment, planning, implementation and evaluation of care. In order
to do this they use the nursing process (see below) or integrated
care pathways. This is very different to task-based care, where
nursing activities were strictly allocated according to the nurse’s
seniority. The more complicated tasks, such as giving medicines,
were performed by senior nurses and simple tasks were under-
1
1
C3996-01.qxd 25/02/2004 18:20 Page 1
taken by the more junior nurses, while the most basic work such
as personal cleansing was carried out by unqualified nursing stu-
dents and nursing assistants or auxiliary nurses.
This chapter will help you to understand how nursing in the
UK is regulated, what nurses do and where they work, and how
they use the nursing process. Details about various professional
organisations and trade unions are also given.
HOW NURSING IS REGULATED IN THE UK
Nursing and midwifery are regulated by the Nursing and
Midwifery Council (NMC). The role of the NMC includes:
— Keeping a register of practitioners (656 000 qualified registered
nurses and midwives in 2003). In 2004 a new three-part regis-
ter – nursing, midwifery and specialist community public
health nursing – replaced a register with 15 parts. The nursing
part of the register has separate sections for first-level and
second-level nurses. The register also notes the particular
branch of nursing – adult, learning disability, children or men-
tal health. The second-level section of the register is for exist-
ing enrolled nurses, but this is closed to new UK applicants.
However, it must be open to existing second-level nurses who
qualified in certain other European countries in order to com-
ply with European Directives. All working nurses need to reg-
ister with the NMC to practise as qualified nurses in the UK.
This registration is renewed every 3 years (see periodic regis-
tration, Ch. 2).
— Setting standards for nursing and midwifery practice.
— Protecting the public and assuring the public that only nurses
and midwives who have reached the minimum standards set
by the NMC can become registered nurses and midwives.
The NMC hears cases of alleged professional misconduct (see
nursing documentation and record keeping, Ch. 4). If the practi-
tioner is found guilty, the NMC can deal with him or her in a vari-
ety of ways, including the removal of the practitioner from the
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
2
C3996-01.qxd 25/02/2004 18:20 Page 2
professional register, which stops him or her working as a regis-
tered nurse or midwife. In this way, the NMC monitors and reg-
ulates nursing and midwifery and ensures that high standards of
professional practice are maintained.
The NMC has produced a Code of Professional Conduct that
sets out the standards of professional conduct, responsibilities
and accountability expected of a registered nurse or midwife, and
explains a person’s entitlements and reasonable healthcare
expectations about nursing care.
As part of the need to practise safely and effectively as a nurse
and to work within ethical boundaries you need to be familiar
with, to understand and to apply to your practice all parts of the
Code of Professional Conduct. The main clauses of the code are
outlined in Box 1.1, but you should read the full document which
has subclauses that give more explanation.
The Code is sent to every practising nurse in the UK, and any
nurse who does not respect the Code of Professional Conduct
will have to answer for their actions or omissions to the NMC and
others, including the hospital or care home where they work, a
court of law or the Health Service Commissioner. The British pub-
lic demand nursing care that is of a high standard and effective,
NURSING IN THE UK
3
Box 1.1
The Code of Professional Conduct (NMC, 2002)
The Code of Professional Conduct says that, ‘as a registered nurse or
midwife, you are personally accountable for your practice. In caring for
patients and clients, you must’:
— ‘respect the patient or client as an individual’
— ‘obtain consent before you give any treatment or care’ (see Ch. 4)
— ‘co-operate with others in the team’
— ‘protect confidential information’
— ‘maintain your professional knowledge and competence’
— ‘be trustworthy’
— ‘act to identify and minimise the risk to patients and clients’.
Available online: http://www.nmc-uk.org
C3996-01.qxd 25/02/2004 18:20 Page 3
and nurses are constantly trying to raise their standards of care
and to identify areas for improvement. In fact, continuing profes-
sional development (CPD) and a commitment to life-long learn-
ing are both essential if the profession is to keep ahead of the
changes that are occurring and for nurses to feel confident in the
work that they are doing. For more information about CPD, post-
registration education and practice (PREP) and periodic registra-
tion, see Chapter 2.
PROFESSIONAL ORGANISATIONS AND TRADE
UNIONS
The vast majority of practising UK nurses and midwives, and stu-
dents join a professional organisation or trade union. There are
several trade unions to choose from (Box 1.2), but the two most
popular ones with nurses are the Royal College of Nursing (RCN)
and Unison, who have about 600 000 members between them.
A trade union works hard for the welfare and best interests of
its nurse members. Trade unions also provide professional
indemnity insurance for practising nurse members, as do several
private insurance companies. Nurses who are employed are cov-
ered for acts or omissions by their employer’s vicarious liability
arrangements. Professional indemnity insurance against claims for
professional negligence is increasingly important for nurses work-
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
4
Box 1.2
Trade unions and professional organisations
— The Royal College of Nursing
— Unison
— The Royal College of Midwives (RCM)
— GMB
— Mental Health Nurses' Association
— Community Practitioners' and Health Visitors' Association
— Community and District Nurses' Association.
See Chapter 10 for useful addresses and websites.
C3996-01.qxd 25/02/2004 18:20 Page 4
ing in independent or private practice, and the NMC recommends
that these nurses should have adequate insurance.
Many trade unions provide continuing education for nurses
through study days, courses, conferences and nursing journals.
Some organisations, notably the RCN and RCM, provide extensive
libraries. Furthermore, the RCN has one of the largest non-
university affiliated nursing libraries in the world.
The National Nursing Association (NNA) in the UK is the RCN.
It is a member of the International Council of Nurses (ICN), and
is the UK representative on the Standing Committee of Nurses in
Europe.
More information about the services offered by individual
trade unions and professional organisations can be found in an
article by Oxtoby & Crouch (2003) and by contacting the trade
union or professional organisation.
WHERE NURSES WORK – NATIONAL HEALTH SERVICE
AND THE PRIVATE SECTOR
Most nurses and midwives (approximately 400 000) work for the
National Health Service (NHS), 80 000 work in the private sector
within independent hospitals, nursing homes, nursing agencies,
workplaces, prisons, embassies and the armed forces, and 20 000
work for general practitioners (GPs). Others work in education
institutions, in management, as independent practitioners, or as
self-employed consultants.
In the 1980s, new nurse education programmes, called Project
2000 (PK2), were introduced. This moved nurse education into
the higher education sector and nursing students were no longer
considered part of the nursing workforce, as they had been
before, and led to an increased employment of healthcare assis-
tants (HCAs) and auxiliaries. HCAs often give the ‘hands-on’ care,
and increasingly do more complex activities because the role of
nurses has expanded and changed.
Nurses today work not only in hospitals but also in the com-
munity. In fact over a third of all UK nurses work in the commu-
NURSING IN THE UK
5
C3996-01.qxd 25/02/2004 18:20 Page 5
nity – with people in their own homes and in clinics, and in the
workplace as occupational health nurses. Even when nurses are
employed in the acute healthcare sector they not only work on
the wards, but they also work in outpatient departments (OPDs)
often running and co-ordinating clinics on their own, such as in
pre-admission assessment, diabetic care, hypertension clinics,
well-men and well-women clinics, and so on. In addition, UK
nurses are increasingly taking on roles that used to be done by
doctors. This has meant that nurses can now ensure a faster and
more efficient service for people in their care.
Nurses in the UK can choose to work either for the NHS or
for the private healthcare sector. The private sector runs hospi-
tals (general and specialist), and many psychiatric hospitals and
specialist clinics (e.g. infertility clinics and drug detoxification
units). The private sector also provides much of the occupation-
al health services for industry and many private companies, and
run hundreds of nursing homes and other care facilities for older
people and other groups all over the UK. The care of older peo-
ple requires much dedication and is a difficult field of nursing,
but it can be very rewarding and certainly it is an area of nurs-
ing care that will increase in demand as more people live longer,
and proportionally more frail older people will require expert
nursing care.
Although private healthcare establishments are not bound by
NHS pay regulations, they generally pay very similar salaries and
in many instances pay slightly more. There are recruitment
guidelines and UK labour legislation helps to ensure fair and eth-
ical employment practices. Wherever a nurse works in the UK he
or she is protected by employment law and health and safety
regulations which, among other things, specify the maximum
number of hours of work to be undertaken in a specified period
of time, the minimum UK wage, and employment entitlements
and benefits.
Nursing in the UK reflects the challenges and the demands of
UK society as a whole. Nursing is considered a respected and val-
ued profession, and on the whole qualified nurses with several
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
6
C3996-01.qxd 25/02/2004 18:20 Page 6
years’ clinical experience and working full-time in a UK health-
care establishment, can expect to be adequately financially
rewarded for their expertise and practice. At the time of writing
the government is proposing a new financial package for quali-
fied nurses working in the NHS, which should redress some of
the financial problems and dissatisfactions of the past.
HIGH QUALITY CARE AND THE NURSING PROCESS
Whether you are at the beginning of your career, practising at an
advanced or specialist level, or just newly arrived to work in the
UK from abroad, all nurses must strive to achieve the five Cs of
good nursing practice:
— competent nursing
— commitment to nursing
— confidence in nursing research
— nursing compassion
— informed nursing conscience.
These aspects of caring nursing practice were first expressed by
Simone Roach, a Canadian nurse, in 1984 (Roach 1984). All five
aspects of nursing practice are needed for effective, high-quality
nursing care. It is the caring aspect of nursing work that is most
appreciated by people and their families, and nurses everywhere
are delivering good patient care by demonstrating competency,
commitment, confidence, conscience and compassion in their
work. In many parts of the world, including the UK, these aspects
of nursing care are best shown in nursing practice by using the
nursing process.
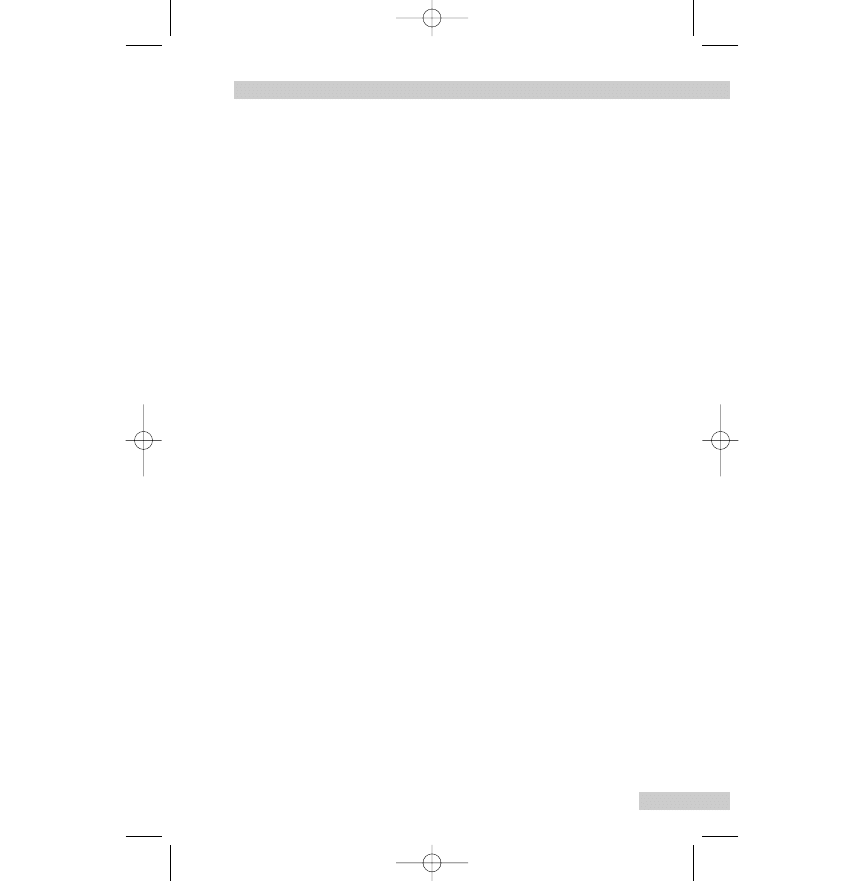
The nursing process is a systematic approach to nursing care.
It has four phases (Fig. 1.1):
— assessment
— planning
— implementation
— evaluation.
NURSING IN THE UK
7
C3996-01.qxd 25/02/2004 18:20 Page 7
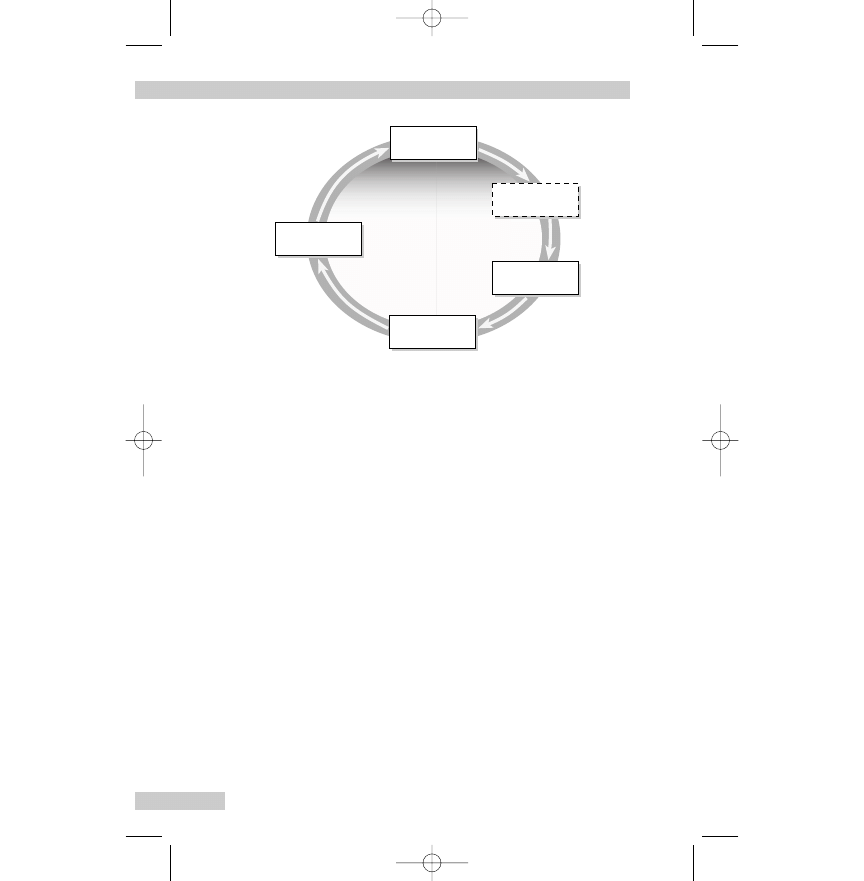
Although the four phases are described in sequence, in reality
they overlap, and occur and recur throughout the period for
which a person is receiving nursing care.
The nursing assessment refers to assessing a person (patient
or client) for physical, psychological, social or spiritual needs
and deciding on their relative nursing value. The status of the
person is assessed in order to help with planning the nursing
care plan.
The care plan is prepared with a specific person in mind; how-
ever, it is possible to have a prepared standard care plan, which
is then adapted and individualised for a particular person’s needs.
This often happens on day-case surgery units and surgical wards
where routine surgical procedures are undertaken. Such an
approach ensures that not only are routine procedures undertak-
en, but also that the care can be individualised. Care plans may
be hand written or, as is increasingly the case, stored on comput-
ers. In both instances, the information is confidential and should
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
8
Assessment
Implementation
Planning
Nursing
diagnosis
Evaluation
Fig. 1.1
The nursing process. Reproduced with permission from
Brooker & Nicol (eds), Nursing Adults: the Practice of Caring,
Mosby, 2003.
C3996-01.qxd 25/02/2004 18:20 Page 8
be held/stored in a safe place (see Ch. 4). In the UK, patients are
entitled to know their diagnosis, to be included in care planning
and to be consulted at every point of the nursing process cycle.
This is to ensure fully informed and freely given consent to the
care proposed (see Ch. 4).
The implementation of the care plan is based on the initial
assessment process and the care delivered is expected to be
evidence-based (i.e. in accordance with the latest nursing
research findings and medical knowledge). If research findings
are not available the evidence may be developed from the collec-
tion of best expert practice in the field. It is the responsibility of
individual nurses to keep themselves updated in nursing practice,
as they are individually accountable for patient care.
The final stage of the nursing process is the evaluation. At this
point the nurse evaluates the effectiveness of the care delivered
and either decides to continue with the current care plan, con-
siders making changes, or moves on to another new assessment
and care plan, as the person is now at another stage and has dif-
ferent needs. Evaluation must be undertaken against some meas-
urement or established criteria (e.g. a pressure ulcer risk scale).
This stage of the care plan is very important, as otherwise the
nurse runs the risk of continuing to give ineffective and or inap-
propriate care.
The nursing process is used effectively by all nurses in the UK,
regardless of their speciality, and as you gain clinical experience
so it becomes easier to move through the stages of the process.
As you would expect the nursing process needs a caring and
knowledgeable approach and is usually made easier by using an
established model or theory of nursing practice, such as the
Roper, Tierney & Logan (1996) model of nursing based on activ-
ities of living or Orem’s self-care model (1995). The result is that
nursing care is being delivered more appropriately, effectively
and in ways that promote holistic well-being.
Nurses should record all the relevant information at all stages
of the nursing process (see Ch. 4).
NURSING IN THE UK
9
C3996-01.qxd 25/02/2004 18:20 Page 9
AN EXCITING FUTURE – EXPANDING THE ROLE OF
NURSES
In 1999 the UK Government issued a document for nurses to con-
sider: NHS Plan for England (Department of Health 1999) in
which it set out areas that it felt needed to be expanded and to
become more mainstream, so that more nurses could be involved
working in these areas in new and more challenging nursing
roles. The areas were:
— to be capable of and responsible for ordering medical investi-
gations, such as pathology tests and X-rays
— to be capable of making direct referrals to specialist services,
such as a pain control team or the continence adviser
— to have responsibility for both admitting and discharging a
range of patients with specified conditions according to a
protocol
— for more nurses to manage their own patient caseloads, e.g. in
the care of people with diabetes
— to increase the number of nurses who would be educated to
prescribe medicines and treatments
— for nurses to be responsible for resuscitation procedures,
including the use of defibrillation
— to be trained to undertake minor surgery and outpatient
procedures
— to be responsible for the administration of outpatient clinics
— to take lead roles and executive positions in local health ser-
vices and their management.
Nurses now have the chance to expand their practice, such as
prescribing medicines, and diagnosing and treating many minor
injuries and illnesses, as well as continuing to give holistic care,
especially for those people with chronic conditions. Nurses work
in ever more sophisticated and technologically advanced settings
(e.g. in oncology units, endoscopy suites, neonatal units and
renal and dialysis units). This requires a high level of basic nurs-
ing care, continuing post-basic specialist knowledge, a system of
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
10
C3996-01.qxd 25/02/2004 18:20 Page 10
advanced nursing education to reflect the increased and variable
nursing work environments and an ethical viewpoint that is
informed and sensitive to the needs of people and their families.
The next two chapters will help you to understand the routes and
methods of achieving these specialisations and to have a basic
understanding of the UK healthcare system and the role and func-
tion of nursing within it.
REFERENCES
Department of Health (DoH) 2000 The NHS plan. DoH, London.
Nursing and Midwifery Council (NMC) 2002 Code of professional
conduct. NMC, London.
Orem DE 1995 Nursing: concepts and practice, 5th edn. Mosby,
St. Louis.
Roach S 1984 Caring: the human mode of being, implications
for nursing. Perspective in caring. Monograph 1. Faculty of
Nursing, University of Toronto, Toronto.
Roper N, Logan WW, Tierney AJ 1996 The elements of nursing,
4th edn. Churchill Livingstone, Edinburgh.
FURTHER READING
Brooker C, Nicol M (eds) 2003 Nursing adults: the practice of
caring. Mosby, Edinburgh, Ch. 1.
Oxtoby K, Crouch D 2003 Value for money. Nursing Times
99(17):21–23.
Royal College of Nursing (RCN) 2002 Labour market review.
RCN, London.
NURSING IN THE UK
11
C3996-01.qxd 25/02/2004 18:20 Page 11
C3996-01.qxd 25/02/2004 18:20 Page 12
This page intentionally left blank
Registering as a nurse in
the UK and career
development
INTRODUCTION
Of all the European countries, the UK has the largest number of
overseas trained nurses working within the healthcare system. It
is estimated that there are about 42 000 internationally recruited
nurses practising in the UK, with another 16 000 waiting for place-
ments on supervised practice courses. Every nurse who works in
the UK needs to be registered with the Nursing and Midwifery
Council (NMC). Since 1919 nurses have been regulated in the UK
(Nurse Registration Act) and the NMC is the latest statutory body
set up by Parliament to perform this regulatory role. The NMC
was established in April 2002 and replaced The UK Central
Council for Nursing, Midwifery and Health Visiting (UKCC). The
change in regulatory body coincided with a change in the way
that the nursing profession was to be organised and administered
around the country and was in keeping with major changes
occurring in the delivery of healthcare in the UK (see Ch. 3). One
of the NMC’s main functions is to protect the public by ensuring
that all those who are registered to work as Registered Nurses
(RNs) in the UK are considered to be safe and competent nurs-
ing practitioners (see Ch. 1).
This chapter will help you to understand how to obtain initial
registration with the NMC and the requirements for periodic reg-
istration. There is further information about adaptation courses,
and in addition the chapter will help you to develop your career
and be successful as a nurse in the UK.
13
2
C3996_02.qxd 25/02/2004 18:21 Page 13
NURSING PROGRAMMES AND OBTAINING
REGISTRATION
The first thing an overseas trained nurse must do to get onto the
NMC register is to write to the NMC (for the address see Ch. 10)
for an application pack. The pack gives information about pay-
ments and how to fill out the forms and what is needed to
become a nurse in the UK. Information on how to apply to the
NMC for registration can also be obtained from the NMC website
(http://www.nmc-uk.org). The first sum of money you send off
to the NMC is to cover the administration cost of processing the
application forms. Refugee nurses do not have to pay the initial
fee if they send the NMC a copy of the letter from the Home
Office confirming their refugee status.
It is the NMC who will determine whether you are a safe and
competent practitioner to work in the UK. This is done by look-
ing at all applications on an individual basis. The NMC will assess
several different things about you; for example, your nursing edu-
cation, character references (from your school of nursing and
employers), and experience and career pathway.
Nursing education models vary considerably around the world
and Registered Nurses may undertake courses that last anything
from 1 to 4 years. Some nurses have been educated at universi-
ties and colleges of higher education, others on pre-matriculation
courses (before leaving secondary school) and also in specialised
nursing further education institutes, which are often attached to
specific teaching hospitals.
In some countries nursing programmes follow a universal
healthcare career structure, where all or many of the healthcare
workers progress together through a generic health worker train-
ing programme. However, some individuals remain at particular
levels, while others will continue their education to gain more
experience and thereby change the role that they are qualified to
undertake. In other countries nurse education is completely sep-
arate from other healthcare professions. In the UK all nurse edu-
cation, wherever it is provided, follows the European Union (EU)
Directives on the nature and length of nurse education
programmes.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
14
C3996_02.qxd 25/02/2004 18:21 Page 14
The majority of overseas trained nurses will be seeking to have
their name put on the nursing part of the register (for more infor-
mation on the three-part register, see Ch. 1) and most of these
will be for adult nursing. To be placed on the register you need
to demonstrate that your nursing education programme meets the
conditions outlined in Box 2.1.
These rules and regulations were agreed by the EU and have
been agreed as valid for the whole of Europe. This was agreed in
REGISTERING AS A NURSE IN THE UK AND CAREER DEVELOPMENT
15
Box 2.1
Nurse education programmes – conditions required
for UK registration
— Duration of at least 3 years of full-time nursing studies and which
included at least 4600 hours of nursing education.This means that
unrelated subjects, such as foreign languages, sport or philosophy, do
not count towards the nursing education hours, but applied subjects
such as healthcare ethics would be relevant.
— The nursing programme does not have to be delivered at a degree
level, but it should be undertaken after completion of full secondary
education and after reaching the age of 17.
— The nursing programme needs to be equally divided between theory
and practice and the programme must cover five main areas, i.e. med-
ical, surgical, women and children, mental health and community.
— Upon completion of the nursing education programme, nursing stu-
dents should be considered to be fully qualified registerable first-level
nurses and fully capable of obtaining the nursing diploma and right to
practise.This implies that the nursing education programme is consid-
ered to be complete in itself and without additional practice periods
and/or supervision, and that until nursing students obtain the nursing
diploma they are not considered to be fully qualified first-level nurses.
Apart from these requirements, the NMC requests that nurses complete
at least 6 months of nursing work in their home country to consolidate
their educational experience. Nurses trying to obtain UK registration
without 6 months' experience in their home country might experience
problems getting onto the register.
C3996_02.qxd 25/02/2004 18:21 Page 15
an effort to standardise the level of nurse education in Europe,
and thereby enable automatic recognition of qualifications
between the countries of the EU. Thus, if a qualified nurse from,
for example, Zambia obtains nursing recognition from the NMC
as a fully qualified first-level nurse in the UK, and obtains an NMC
Professional Identification Number (PIN) and is put on the UK
nursing register, the UK registration and recognition is valid
throughout the whole of Europe. It means that Registered Nurses
can easily move around within the EU for purposes of continuing
nurse training and obtaining professional work.
The same rules ensure that the levels of nurse education are
automatically raised overall. With the introduction of this type of
nurse education the countries of Europe were asked to close their
second-level nursing programmes. The only way to become a
nurse in the EU today is by undertaking a 3-year programme of
full-time education at post-secondary school level, as already
described. The only nurses in Europe who are practising on the
second-level register are those nurses who completed their train-
ing before the new regulations came into force, either from the
UK or from other EU countries.
Will your application be accepted?
The NMC may accept your qualifications, require you to do an
adaptation course, or insist on further training:
1. The NMC may fully recognise your qualifications, and because
the education programme was conducted in English and it
covered the European nursing education requirements you
can be admitted onto the register without any additional
requirements. This is the common situation if you have com-
pleted university degrees in nursing from North America,
Australia or New Zealand and have sufficient additional prac-
tical nursing experience.
2. The vast majority of all other nurses will receive a letter from
the NMC stating that their qualifications are sufficient for them
to be put on the NMC register but that now they must com-
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
16
C3996_02.qxd 25/02/2004 18:21 Page 16
plete an adaptation programme (supervised practice) in an
approved healthcare establishment in the UK over a specified
period of time. This can range from 3 months to 1 year, but
most commonly is for a period between 3 and 6 months.
3. Some non-EU trained nurses will be asked to undertake more
pre-registration nurse education before they can be put on the
UK register. Meanwhile, some of their original nurse training
can be considered valid and academic credits can be awarded
towards the new UK pre-registration nursing education. This
process of giving credit for prior education is called
Accreditation of Prior Experience and Learning (APEL). Every
school of nursing in the UK can undertake this accreditation
process for overseas-trained nurses. APEL was put into place
to help adult mature entrants return to formal education to
obtain new skills, and now this process is being extended to
include previous achievements, even those gained overseas. It
is a long process, but well worth undertaking.
The NMC may ask you for more information before they make
a decision, or reject your application if your nursing course was
less than 3 years long or you cannot meet other requirements (see
Box 2.1).
Once you have completed all the requirements set by the NMC
and sent your initial registration payment to the NMC, you will
receive a PIN and a copy of the NMC Code of Professional
Conduct (see Ch. 1).
Adaptation programmes (supervised practice)
Unfortunately there are not enough places on adaptation pro-
grammes. Although almost all acute NHS Trusts and many
Primary Care Trusts (PCTs) do provide adaptation programmes,
there are still not enough to provide adaptation placements for
the large numbers of overseas trained nurses wishing to work in
the UK.
Adaptation programmes for overseas trained nurses are run
jointly by the NHS Trusts who provide access to the clinical areas
REGISTERING AS A NURSE IN THE UK AND CAREER DEVELOPMENT
17
C3996_02.qxd 25/02/2004 18:21 Page 17
and the necessary mentors and schools of nursing, who provide
the lecturers and teaching support. Some approved supervised
placements can also be undertaken in the independent sector,
predominantly in care homes for older people. There is a short-
age of placements for supervised practice because there are not
enough qualified nurses to undertake the training necessary to
become mentors, and the clinical areas are already completely
full of pre- and post-registration nursing students. The authorities
who commission and fund adaptation programmes are trying to
increase the number of placements. The NMC is also beginning
to look at other ways of assessing nurses’ readiness to practise in
the UK, such as by passing an examination, which may or may
not include a clinical component, but all these alternatives are still
a long way away.
It is because of these logistical problems that the NMC recom-
mends that overseas trained nurses do not arrive in the UK until
they have a guaranteed place on an approved adaptation course,
since at the time of writing there is an estimated 2- to 3-year back-
log in getting onto an adaptation programme in the UK.
Communication in English – International English Language
Testing System
Overseas trained nurses need to be able to demonstrate the use
of the English language to a level that is good enough to commu-
nicate with colleagues and patients and to function safely in the
clinical environment. The NMC currently requires that all overseas
trained nurses who completed their training in a language other
than English need to pass the International English Language
Testing System (IELTS) examination. The IELTS is a specific
English language test that is administered by the British Council
in centres worldwide. The IELTS test required for nurses is the
General Test, and this consists of several sections, such as com-
prehension and communication. All these sections need to be
completed successfully with a minimum grade of 5.5; however,
an overall grade of 6.5 must finally be achieved. Many nurses find
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
18
C3996_02.qxd 25/02/2004 18:21 Page 18
the examination difficult and not necessarily appropriate for nurs-
ing practice. The NMC is considering several other possibilities,
but one thing is sure – nurses whose first language is not English
will need to demonstrate that they have a reasonable command
of the English language. In addition to needing sufficient English
to function safely in clinical areas and with patients, overseas
trained nurses will need the equivalent of IELTS grade 6.5 in
order to undertake further nursing education at a UK university.
PERIODIC REGISTRATION AND CONTINUING
PROFESSIONAL DEVELOPMENT
Periodic registration
The nursing register is constantly being updated, and you will
need to update your right to be on the register by periodic regis-
tration. The right to practise as a nurse in the UK is not only
dependent on paying an initial fee, but you must also complete
a Notification of Practice form every 3 years and pay another fee,
and fulfil certain requirements for post-registration education and
practice (PREP) (Box 2.2).
Continuing professional development
Continuing professional development (CPD) can be gained in a
number of ways, for example:
— Reading professional articles in the nursing press, such as the
Professional Nurse, Nursing Times or Nursing Standard. Doing
literature searches relevant to your area of practice.
— Visiting other units.
— Ward teaching sessions, study days, conferences or seminars.
— Short courses, such as moving and handling, managing aggres-
sion and pain control. Longer courses, such as a degree, or
studies that lead to registration on another part of the NMC
nursing register, or the community public health nursing or
midwifery parts of the register.
REGISTERING AS A NURSE IN THE UK AND CAREER DEVELOPMENT
19
C3996_02.qxd 25/02/2004 18:21 Page 19
The important thing is that you are able to demonstrate an
approach to professional nursing that is consistent with the prin-
ciples of life-long learning. The way to do this is to keep a per-
sonal professional profile/portfolio that contains evidence of all
the CPD activities you have achieved over a 3-year period. This
is a requirement for PREP, and if you keep your profile up to date
you will always be ready for periodic registration.
It is vital to reflect on your CPD activities, so you can identify
what you have learned and its relevance to your practice.
Reflection is an important part of all nursing activity, which of
course ties into the evaluation stage of the nursing process (see
Ch. 1). Many overseas trained nurses will already have been
asked to undertake a reflective diary on their adaptation course,
so you will probably be familiar with this approach. Reflecting on
personal nursing practice is crucial to meaningful CPD.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
20
Box 2.2
Post-registration education and practice (PREP)
The requirements for periodic registration are:
— undertake a minimum of 5 days or 35 hours of learning that is rele-
vant to their practice (see Continuing Professional Development
(CPD), p. 19)
— work in some capacity by virtue of their nursing qualifications for a
minimum of 750 hours (100 days) during the last 5 years, or have
done a return to practice course
— keep a personal professional profile of their learning (see Further
Reading and Resources at the end of this chapter)
— comply with any request by the NMC to check (audit) how the
requirements have been met.
The NMC states that the CPD requirements for PREP can be achieved in
many different ways and need not cost a lot of money (see Further
Reading and Resources at the end of this chapter).
C3996_02.qxd 25/02/2004 18:21 Page 20
DEVELOPING YOUR CAREER
Some adaptation placements, nursing courses and all job vacan-
cies are published in the nursing press and sometimes in local
newspapers. It may also be a good idea to go to the local hospi-
tal or PCT headquarters and look at the job vacancies bulletin
board. The NMC also provides a website of job vacancies
(http://www.nmc4jobs.com). Whether you are applying for an
adaptation placement or for a first nursing job after completing
the supervised practice, you will need to complete a curriculum
vitae (CV) (see Further Reading and Resources at the end of this
chapter), to fill out an application form, and if short-listed you
will need to attend an interview. It is really important that the
application form is filled out correctly and that your CV is com-
plete, so that the reader (i.e. the prospective employer) knows
who you are, what you have done and why you want the job. If
you do not provide all the information you are unlikely to get
short-listed for an interview.
Many teachers of English as a Second Language (ESOL) and
IELTS classes will help you write a CV and explain how to fill out
application forms. In addition, you can ask for help from Job
Centres or your nursing mentors, whoever is more accessible and
appropriate. There are also many books about how to complete
application forms and a CV, and how to prepare for interviews.
These can be found in public and nursing libraries.
Preparing for a job interview is time well spent – you should,
for example, be familiar with the job description and any special
responsibilities of the post (see Further Reading and Resources at
the end of this chapter). If you are unable to attend on the date
given for an interview it is considered polite to inform the per-
sonnel department; as they were impressed enough to invite you
for interview they may well offer you another date. It is essential
to give yourself plenty of time to get to the interview, to be punc-
tual, to be prepared and to be positive about the experience,
however nervous you may be. If you find you are going to be late
for a reason beyond your control, it is a good idea if at all possi-
REGISTERING AS A NURSE IN THE UK AND CAREER DEVELOPMENT
21
C3996_02.qxd 25/02/2004 18:21 Page 21
ble to telephone and explain the situation. That way, they may
even offer you another time to attend the interview.
At the start of your UK nursing career (whether in the National
Health Service (NHS) or the private sector) you will be placed on
a fairly basic salary grade, most probably grade D or E (see Ch.
3). When you are ready for more responsibility and can work in
more specialised areas you will be given the opportunity to apply
for more senior posts and develop your nursing career. The NHS
pay and career structure is undergoing change, and a new system
of payment and assessing workloads and work definitions is
being piloted and will then be introduced nationwide (Agenda
for Change, Department of Health 1999).
Most employers require nurse managers, including ward sisters
and charge nurses to have at least a first degree in nursing or a
relevant subject and usually evidence of specialisation in the
work undertaken in the clinical area. Nursing degrees (first and
higher degrees) are offered by schools of nursing which are
based in universities. A degree can last from between 1 and
3 years, depending on the existing level of nursing education.
There are many opportunities for advancing your nursing career
through education, and many of these are sponsored by the NHS.
It is common nowadays for your manager to do periodic
reviews of your work with you. When you have a review meet-
ing it is important to talk about your career plans and to start
mapping out (planning and deciding) how you plan to achieve
your nursing goals. Moving around clinical areas is one way of
gaining new experience, but most UK nurses progress slowly
through a given specialty, becoming more expert in specific
aspects of nursing care (e.g. pain control, stoma care, tissue via-
bility or substance misuse).
REFERENCES
Department of Health (DoH) 1999 Agenda for change. DoH,
London.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
22
C3996_02.qxd 25/02/2004 18:21 Page 22
FURTHER READING AND RESOURCES
Banks C 2003 How to ... excel at interview. Nursing Times
99(33):58–59.
Hyde J 2002 In: Brooker C (ed). Churchill Livingstone’s
dictionary of nursing, 18th edn. Churchill Livingstone,
Edinburgh, p 512–518.
Hoban V 2003 How to ... write a CV. Nursing Times
99(27):52–53.
Registering as a nurse or midwife in the UK, see the NMC
website: http://www.nmc-uk.org
REGISTERING AS A NURSE IN THE UK AND CAREER DEVELOPMENT
23
C3996_02.qxd 25/02/2004 18:21 Page 23
C3996_02.qxd 25/02/2004 18:21 Page 24
This page intentionally left blank
The National Health
Service and Social
Services
INTRODUCTION
Since 1948 the healthcare system in the UK has been structured
around the National Health Service (NHS) and social welfare has
been delivered by local Social Service agencies. Both systems are
maintained from the contributions of UK taxpayers, but the servi-
ces are available to everyone, whether they pay taxes or not, such
as children and some older people.
Although the NHS and Social Services have changed dramati-
cally over the years, most people in the UK still want a national
healthcare and social welfare system to continue to serve the
whole population. Currently, the NHS is undergoing further struc-
tural change, which is aimed at improving the services to the pub-
lic and making NHS workers more accountable to patients and
UK taxpayers.
There are over a million people working for the NHS, as
healthcare professionals and individuals supporting the clinical
staff, such as electricians, gardeners, managers and clerical staff.
The public sector NHS provides over 75% of the healthcare deliv-
ered in the UK.
This chapter will help you understand how the NHS is organ-
ised in England (services in Wales may be different and in
Scotland services are organised differently) and explain the vari-
ous roles of people within the NHS and the close links between
the NHS and Social Services.
25
3
C3996_03.qxd 26/02/2004 13:45 Page 25
THE STRUCTURE OF THE NHS
The NHS is the responsibility of the Department of Health (DoH)
with a remit to deliver comprehensive healthcare to the public.
This ranges from primary care, including access to general prac-
titioners (GPs), screening programmes, maternity care, mental
health, secondary (surgical and medical) care in hospitals, spe-
cialist hospitals, and through to care of chronically ill people and
those needing palliative care.
New developments in medical science place extra demands on
the NHS and means that treatment provision needs to keep
changing, as do the medicines that doctors and nurses can pre-
scribe. It is one of the aims of the DoH to ensure that all treat-
ments delivered by the NHS are evaluated and evidence based.
The National Institute for Clinical Excellence (NICE) is the gov-
ernment agency set up to evaluate new treatments and drugs and
provide guidance (see Further Reading and Resources at the end
of this chapter). This is to guarantee that the best care is deliv-
ered by the most cost-effective method.
In the last few years the DoH has launched NHS Direct, an
innovative service with a completely new approach to healthcare.
NHS Direct is a telephone helpline (0845 4647), which aims to
empower individuals and prevent the inappropriate use of GPs
and emergency departments for minor conditions, by providing
information and healthcare advice. NHS Direct is operated
24 hours a day by qualified nurses and health workers. The oper-
ators recommend what the caller should do (e.g. call an emer-
gency ambulance, make an appointment to see their GP, or take
a simple self-care remedy). The service empowers people to take
responsibility for their health and the choices that they make. NHS
Direct also provides web-based information about healthcare and
the NHS (www.nhsdirect.nhs.uk).
The DoH manages the overall health and social care system,
develops policy and manages changes in the NHS, regulates and
inspects health and social care establishments and services and
intervenes when necessary to improve services.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
26
C3996_03.qxd 26/02/2004 13:45 Page 26
The work of the DoH is divided into two main areas:
— Strategic Health Authorities (SHAs), based on specific geo-
graphical regions. The SHAs ensure that NHS Trusts deliver the
healthcare that has been commissioned, and they oversee var-
ious aspects of workforce planning (e.g. monitoring and
arranging the training of healthcare workers, including nurs-
es). They work with NHS Trusts and universities to plan and
support clinical placements for overseas trained nurses (see
Ch. 2). The SHA is responsible for strategic healthcare plan-
ning and for ensuring that national priorities are integrated
into the work of the Primary Care Trusts (PCTs) and NHS
Trusts (see below). Thus the SHA is concerned with primary
healthcare and community services, which are organised by
the PCTs, and acute hospital (secondary) services provided by
NHS Trusts. Mental healthcare (delivered by mental health
nurses) may be delivered either through the services of a spe-
cial Psychiatric NHS Trust (covering inpatient and outpa-
tient/community services) or by a Community NHS Trust (i.e.
a PCT) or a General NHS Hospital Trust.
— Special health authorities, called Special Trusts. Special Trusts
are usually considered to be secondary care providers or
sometimes tertiary referral centres, such as the Hospital for
Sick Children in London. Other Special Trusts include some
inpatient units designated for forensic psychiatry.
Primary Care Trusts
PCTs work closely with Social Services (see below) and other
agencies and organisations to assess local health needs, plan,
develop and deliver community and primary healthcare services,
and commission secondary services for the local population, in
order to improve health and reduce inequalities in health. PCTs
are responsible for public health and various intermediate care
services. The SHA is responsible for the performance manage-
ment of PCTs. Over recent years there has been a huge shift in
how and where healthcare is delivered and much more care is
THE NATIONAL HEALTH SERVICE AND SOCIAL SERVICES
27
C3996_03.qxd 26/02/2004 13:45 Page 27
provided within the community (person’s home, care homes,
NHS walk-in centres, healthcare clinics, etc.) by Primary
Healthcare Teams (PHCTs) comprising nurses, midwives, doctors,
therapists, etc. In addition, pharmacists, dentists, opticians and
optometrists, and podiatrists all work within the community.
Primary Healthcare Team
GPs usually work in a group practice with several doctors who
work within a team comprising practice nurses, district nurses
(DNs), health visitors (HV), community midwives, community
mental health nurses, physiotherapists, occupational therapists,
speech and language therapists, counsellors and podiatrists, etc.
Other professionals involved include school nurses (school health
advisers), dieticians, etc. The PHCT delivers basic medical servic-
es, community care and liaises with local acute NHS Trusts for the
continued and ongoing care of their patients. Practice nurses and
GPs are usually the first point of contact for the person who is
unwell or needs healthcare advice.
The nursing and midwifery roles within the team include:
— The practice nurse is a Registered Nurse (adult) who works
alongside the GP in the GP surgery and often runs specialised
clinics (e.g. immunisation, family planning and diabetic clin-
ics). Some practice nurses are also nurse practitioners who
perform many activities that are considered to be an extension
of traditional nursing roles. Nurse practitioners are educated
(usually to degree level) to diagnose and manage many basic
conditions and to prescribe medications from the Nurse
Prescribers’ Formulary (NPF). Suitably qualified district nurses
and health visitors also prescribe from the NPF.
— District nurses (DNs), who are also called community nurses,
are responsible for the nursing care provided for people in
their homes or in care homes. DNs are Registered Nurses (usu-
ally adult branch, although some are paediatric or learning dis-
ability nurses) who have undertaken additional education at a
university to obtain a degree in community nursing. A DN
usually supervises a small nursing team of staff nurses and
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
28
C3996_03.qxd 26/02/2004 13:45 Page 28
nursing assistants. Various health and social care professionals
may ask for a DN to assess a person in their home or a patient
may make a self-referral; similarly, a hospital may request that
a DN provide nursing care for a person following discharge
from hospital.
— Health visitors (HV) are Registered Nurses who have under-
gone further university nursing education in order to work in
the community and who specialise in health promotion, health
education and health maintenance. HVs do not deliver hands-
on nursing care. They concentrate on the welfare of small chil-
dren and mothers, but some HVs also work with older people
or groups with specific needs, such as refugees. In every geo-
graphical area there will be a designated HV who is responsi-
ble for children with special needs and those children who
may be at risk of being neglected or abused physically, men-
tally or sexually by their parents or carers.
— Community midwives provide professional care during preg-
nancy and labour and look after newly delivered mothers and
their babies in the community. Most babies are born in a
District General Hospital in the UK and in many areas com-
munity midwives accompany women into hospital to conduct
the delivery and take the woman and new baby home after a
few hours if all is well. Community midwives attend home
births, especially for women who have already had a child and
are expected to have a straightforward delivery. They also pro-
vide care for women who have been discharged following a
booked hospital delivery. In an uncomplicated delivery the
woman and baby are often discharged home to the care of the
community midwife within 12 hours.
— Community mental health nurses also work in the community,
but they specialise in the care of people with mental health
problems. They work with people in their own homes,
community-based mental health units, drugs and alcohol servi-
ces and the criminal justice system. They liaise with other
members of the PHCT, psychiatrists from local NHS Mental
Health Trusts, clinical psychologists and social workers.
THE NATIONAL HEALTH SERVICE AND SOCIAL SERVICES
29
C3996_03.qxd 26/02/2004 13:45 Page 29
Other community health professionals
See Box 3.1 for an outline.
Ambulance Trusts
The Ambulance Service provides emergency care in the event of
serious illness or accident. Ambulance paramedics will stabilise
the person’s condition and then transport them to the most
appropriate emergency department (e.g. the local District
General Hospital). There is no charge for an emergency ambu-
lance, which is summoned by telephoning (999). You must ask
the operator for an ambulance, explaining as clearly as possible
the nature of the problem and the location. The Ambulance
Service itself is divided into emergency services and patient trans-
port services.
Secondary Care – NHS Acute Care Trusts
Secondary hospital care in the UK is delivered by NHS Trusts.
Acute care hospitals and some inpatient continuing care units
(e.g. for the care of older people) are part of NHS Trusts.
Hospitals are managed by a chief executive who is accountable
to the Executive Board of the Hospital Trust. Increasingly, the
management of hospitals is delegated to specific clinical direc-
torates within the Trust. Secondary care is provided in outpatient
departments, day case units and inpatient beds.
Nursing staff
Many nurses wear a uniform of some sort, which varies from hos-
pital to hospital and even within a hospital according to rank but
also according to nursing department. For example, paediatric
nurses often wear colourful tops and tabards, while those in
intensive care wear theatre tops and trousers, and mental health
nurses and senior nurses may wear their own clothes.
Within each Hospital Trust there will be a chief nurse (who
may be known as the nursing director, etc), who also sits on the
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
30
C3996_03.qxd 26/02/2004 13:45 Page 30
Trust board. The chief nurse provides professional nursing lead-
ership and is responsible for the overall implementation of nurs-
ing policies in a Trust and for the smooth running of the nursing
department.
THE NATIONAL HEALTH SERVICE AND SOCIAL SERVICES
31
Box 3.1
Other health professionals working in the community
— Community pharmacists: most work within the NHS although they
are independent practitioners. A typical pharmacist on the high
street will have a working relationship with their local GP surgeries.
Medicines and surgical/nursing supplies written out on a GP's or
nurse's prescription form will be dispensed by the pharmacist. A
standard NHS prescription charge applies to each item, but most
people are exempt and do not pay for prescriptions.These include
children and pregnant women, people aged over 60 years, people
receiving certain social security benefits and people with certain
conditions (e.g. diabetes mellitus). Community pharmacists also
offer advice to the public about minor ailments and all aspects of
medication.
— Dentists are independent practitioners and some work with NHS
patients and provide services to patients at NHS rates. However,
there are few dentists who provide care under the NHS and currently
PCTs are employing more dentists to deliver NHS dental care.There
are several NHS dental hospitals in the UK, which provide for patients
with maxillofacial and dental problems.These hospitals also train and
provide practical placements for specialist personnel such as dental
nurses and speech and language therapists and of course dentists and
postgraduate dental surgeons.
— Opticians are also independent practitioners, but most work with NHS
patients and provide services to people at NHS rates. Some
optometrists and opticians work in NHS hospitals, but the majority
practise in the community. Certain groups of people do not pay for
eye care; these include pregnant women and children. People aged
over 60 years and those with conditions such as diabetes or glaucoma
are exempt from some charges.
C3996_03.qxd 26/02/2004 13:45 Page 31
Currently the nursing posts open to qualified Registered
Nurses are graded from D to I:
— A D grade staff nurse is considered the first nursing post that
a newly qualified nurse undertakes. A D grade post is really a
‘consolidation’ post, where the new nurse graduate consoli-
dates the training and education that he or she has received
before seeking promotion after a year or two. Initially, most
overseas trained nurses will be D grade until they become
used to nursing in the UK. However, depending on a nurse’s
previous experience and learning, he or she may be upgraded
very quickly.
— An E grade is for a more experienced staff nurse.
— A staff nurse is responsible to the F or G grade nurse known
as the ward sister/charge nurse (male) or ward manager.
Some hospitals use F grade for senior staff nurses, whereas
others use it for junior ward sisters/charge nurses. Apart from
staff nurses, ward sisters/charge nurses, healthcare assistants
and nursing students there will be senior nurses, clinical nurse
specialists, research nurses, lecturer–practitioners and nurse
consultants who are also employed by some PCTs.
— Senior nurses (G, H or I grade) usually have a managerial role
as well as responsibilities for a clinical speciality. Some senior
nurses have responsibility for several wards or units and they
are responsible to a general manager for organisational issues
and to the chief nurse for professional issues. Some senior
nurses have taken on the role of the modern ‘matron’, a post
that is intended to give mid-level nursing managers more
authority over hospital matters, and especially control over
issues such as the cleanliness of the hospital. There are many
clinical nurse specialists working in hospitals (and the com-
munity), especially in specialised areas such as pain control,
palliative care, stoma care and oncology. The nurse will have
undergone further education at a university and be a role
model for colleagues, acting as mentor and educationalist. The
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
32
C3996_03.qxd 26/02/2004 13:45 Page 32
lecturer–practitioner has a commitment to a student group at a
university, teaches and undertakes nursing research, in addi-
tion to the role of specialist nurse.
There is quite a difference between the pay of the D grade
nurse who is starting a career in nursing and a G or H grade
nurse. However, this pay arrangement is in the process of change,
as the government is piloting a new system of payment and
assessing workloads and work definition (Department of Health
1999) prior to its introduction nationwide. The new pay deal will
be beneficial to junior nurses, but to progress in the nursing
career structure it is necessary to undertake further training and
education (see Ch. 2).
Medical staff
Medical staff posts in hospitals are structured, with the post of
consultant (e.g. a nephrologist) being at the top of the clinical
speciality:
— Consultant: a physician or surgeon who has completed a
lengthy postgraduate specialisation.
— Associate specialist: an experienced doctor who is nominally
under the supervision of the consultant.
— Staff grade: a doctor who provides support for consultants.
— Specialist registrar: a doctor undertaking higher specialist
training.
— Senior house officer: a doctor undertaking basic specialist
training.
— House officer (pre-registration): a newly qualified doctor in the
year following qualification.
Surgeons in the UK are addressed as Mr or Mrs/Miss/Ms.
The introduction of European Union Working Directives has
reduced junior doctors’ hours and this has meant that some nurs-
es are trained to undertake some of the work traditionally done
by junior doctors.
THE NATIONAL HEALTH SERVICE AND SOCIAL SERVICES
33
C3996_03.qxd 26/02/2004 13:45 Page 33
Professions allied to medicine and other staff
There are many other groups of professionals working in hospi-
tals (e.g. radiographers, technicians, medical scientists, physio-
therapists, speech and language therapists, play therapists, teach-
ers (in children’s hospitals) and social workers). You will also
encounter translators and healthcare advocates, who are bilingual
native speakers of various languages.
SOCIAL SERVICES
Social Services are provided by Local Authorities (local govern-
ment). For example, Norfolk County Council provides services for
the people who live in the county of Norfolk. Social Service
departments have a statutory responsibility to provide care for
groups that include:
— children and young people
— people with disabilities, including sensory impairments
— people who have problems with alcohol and drugs
— older people
— people with mental health problems.
Care and support is provided in the person’s own home or in
small community-based care units. People needing these services
will have a named social worker to co-ordinate and monitor the
care package. The care package may include help with personal
care, day centres, respite care and home modifications such as
bath rails and stair lifts.
As you advance in your UK nursing career you will have a
great deal of contact with social workers. Joint working between
health and social care professionals is vital for effective care plan-
ning and delivery. This is especially so in discharge planning, and
in the community where there is considerable overlap between
the work of health and social care professionals. In many areas,
such as mental health and children, health and Social Services
have formed a single Social Services & NHS Trust which aims to
provide high-quality care.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
34
C3996_03.qxd 26/02/2004 13:45 Page 34
REFERENCES
Department of Health (DoH) 1999 Agenda for change. DoH,
London.
FURTHER READING AND RESOURCES
Clinical guidance, see the National Institute for Clinical
Excellence (NICE) website: www.nice.org.uk
Medicines and healthcare products, see the Medicines and
Healthcare products Regulatory Agency (MHRA) website:
www.mhra.gov.uk
Public health (infection control, poisons, chemical and radiation
hazards), see the Health Protection Agency (HPA) website:
www.hpa.org.uk
THE NATIONAL HEALTH SERVICE AND SOCIAL SERVICES
35
C3996_03.qxd 26/02/2004 13:45 Page 35
C3996_03.qxd 26/02/2004 13:45 Page 36
This page intentionally left blank
Nursing documentation,
record keeping and
written communication
INTRODUCTION
Accurate record keeping and careful documentation is an essen-
tial part of nursing practice. The Nursing and Midwifery Council
(NMC 2002) state that ‘good record keeping helps to protect the
welfare of patients and clients’ – which of course is a fundamental
aim for nurses everywhere. You can look at the full Guidelines
for records and record keeping by visiting the NMC website
(www.nmc-uk.org).
It is equally important that you can also communicate by letter
and e-mail with other health and social care professionals, to
ensure that they understand exactly what you mean.
NURSING DOCUMENTATION AND RECORD KEEPING
High quality record keeping will help you give skilled and safe
care wherever you are working. Registered Nurses have a legal
and professional duty of care (see Code of Professional Conduct,
Ch. 1). According to the Nursing and Midwifery Council guide-
lines (NMC 2002) your record keeping and documentation should
demonstrate:
— a full description of your assessment and the care planned and
given
— relevant information about your patient or client at any given
time and what you did in response to their needs
— that you have understood and fulfilled your duty of care, that
you have taken all reasonable steps to care for the patient or
37
4
C3996_04.qxd 26/02/2004 13:53 Page 37
client and that any of your actions or things you failed to do
have not compromised their safety in any way
— ‘a record of any arrangement you have made for the continu-
ing care of a patient or client’.
Investigations into complaints about care will look at and use
the patient/client documents and records as evidence, so high
quality record keeping is essential. The hospital or care home, the
NMC, a court of law or the Health Service Commissioner may
investigate the complaint, so it makes sense to get the records
right. A court of law will tend to assume that if care has not been
recorded then it has not been given.
Documentation
You will see lots of different charts, forms and documentation.
Every hospital, care home and community nursing service will
have the same basic ones, but with small variations that work best
locally. The common documents that you will use include some
of the following.
Nursing assessment sheet
The nursing assessment sheet contains the patient’s biographical
details (e.g. name and age), the reason for admission, the nursing
needs and problems identified for the care plan, medication,
allergies and medical history.
Nursing care plan
The documents of the care plan will have space for:
— Patient/client needs and problems.
— Sometimes, nursing diagnoses will be documented but these
are not used as frequently as in North America.
— Planning to set care priorities and goals. Goal-setting should
follow the SMART system, i.e. the goal will be specific, meas-
urable, achievable and realistic, and time-oriented. For exam-
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
38
C3996_04.qxd 26/02/2004 13:53 Page 38
ple, a SMART goal would be that ‘Mr Lee will be able to drink
1.5 L of fluid by 22.00 hours’. Some goals, such as reducing
anxiety, are not easily measured and it is usual to ask patients
to describe how they feel about a problem that was causing
anxiety.
— The care/nursing interventions needed to achieve the goals.
— An evaluation of progress and the review date. This might
include evaluation notes, continuation sheets and discharge
plans. In some care areas you might record progress using a
Kardex system along with the care plan.
— Reassessing patient/client needs and changing the care plan as
needed.
Vital signs
The basic chart is used to record temperature, pulse, respiration
and possibly blood pressure. Sometimes the patient’s blood pres-
sure is recorded on a separate chart. Basic charts may also have
space to record urinalysis, weight, bowel action and the 24-hour
totals for fluid intake and output. More complex charts, such as
neurological observation charts, are used for recording vital signs
plus other specific observations, which include the Glasgow
Coma Scale score for level of consciousness, pupil size and reac-
tion to light, and limb movement (Fig. 4.1).
Fluid balance chart
This is often called a ‘fluid intake and output chart’ or sometimes
just ‘fluid chart’. It is used to record all fluid intake and fluid out-
put over a 24-hour period. The amounts may be totalled and the
balance calculated at 24.00 hours (midnight), or at 06.00 or
08.00 hours. Sometimes the amounts are totalled twice in every
24 hours (i.e. every 12 hours). Fluid intake includes oral, naso-
gastric, via a gastrostomy feeding tube, and infusions given intra-
venously, subcutaneously and rectally. Fluid output from urine,
vomit, aspirate from a nasogastric tube, diarrhoea, fluid from a
stoma or wound drain are all recorded (Fig. 4.2).
NURSING DOCUMENTATION, RECORD KEEPING AND WRITTEN COMMUNICATION
39
C3996_04.qxd 26/02/2004 13:53 Page 39
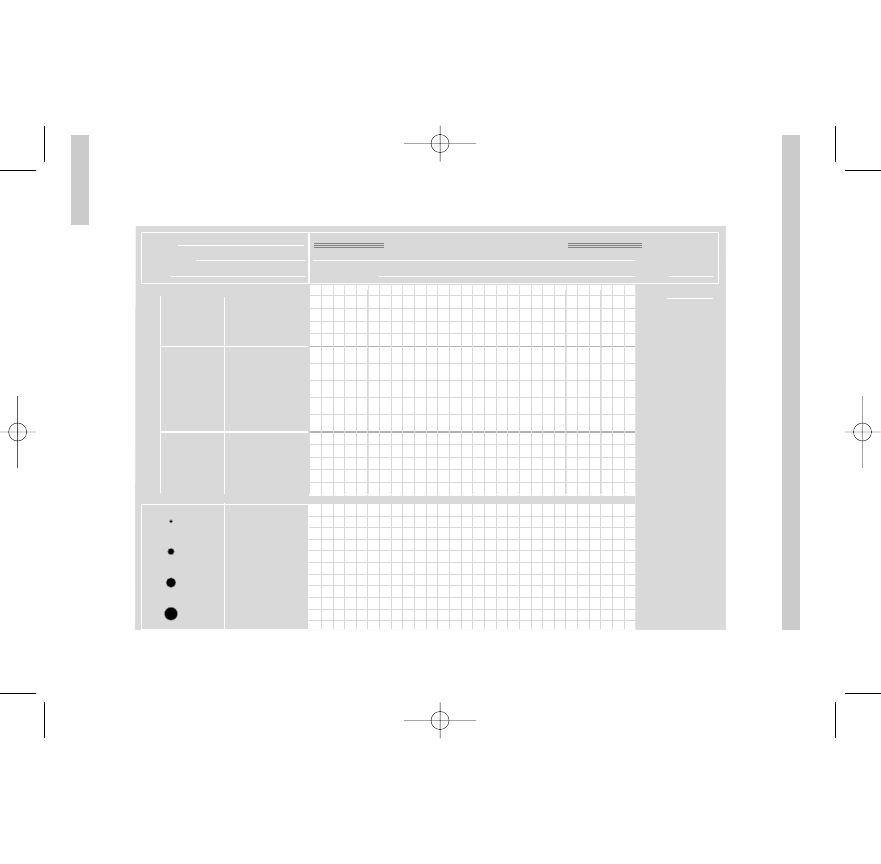
P
ARKINSON
AND
BR
OOKER:
EVER
YD
A
Y
ENGLISH FOR INTERNA
TIONAL NURSES
40
Eyes open
Best verbal
response
Best motor
response
Spontaneously
To speech
To pain
None
Orientated
Confused
Inappropriate
words
Incomprehensible
sounds
None
Obey commands
Localise pain
Flexion to pain
Extension pain
None
1
2
3
4
Blood
pressure
and pulse
rate
240
230
220
210
200
190
180
170
160
150
40
39
38
37
36
35
34
33
32
Temperature
°C
Usually record
the best arm
response
Endotracheal
tube or
tracheostomy
= T
Eyes closed
by swelling
= C
NAME:
HOSP. No.:
AGE:
DATE:
TIME:
CONSULTANT:
C3996_04.qxd 26/02/2004 13:53 Page 40
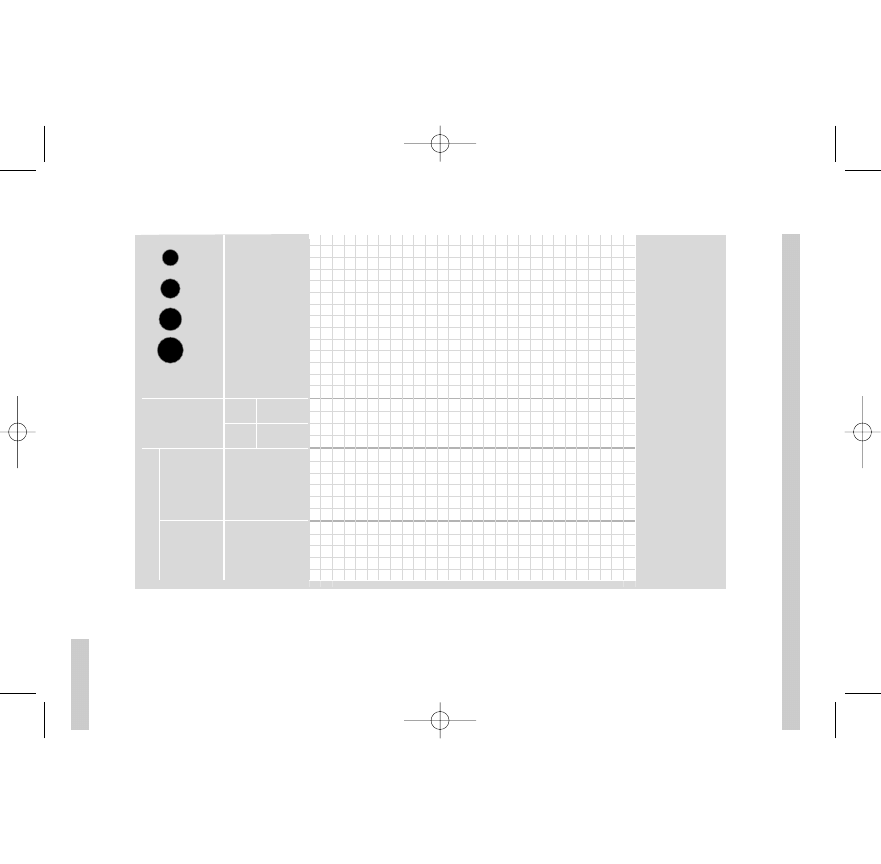
NURSING DOCUMENT
A
TION,
RECORD KEEPING
AND
WRITTEN COMMUNICA
TION
41
Pupils
!
L
I
M
B
M
O
V
E
M
E
N
T
" #
$% #&
' #&
(
)(
"
*
–
, - %
%
%
-
%
.#
# %
" #
$% #&
' #&
)(
"
Arms
Legs
!
Fig. 4.1
Neurological observation chart: the Glasgow Coma Scale. Reproduced with permission from Brooker &
Nicol (eds), Nursing Adults: the Practice of Caring, Mosby, 2003.
C3996_04.qxd 26/02/2004 13:53 Page 41
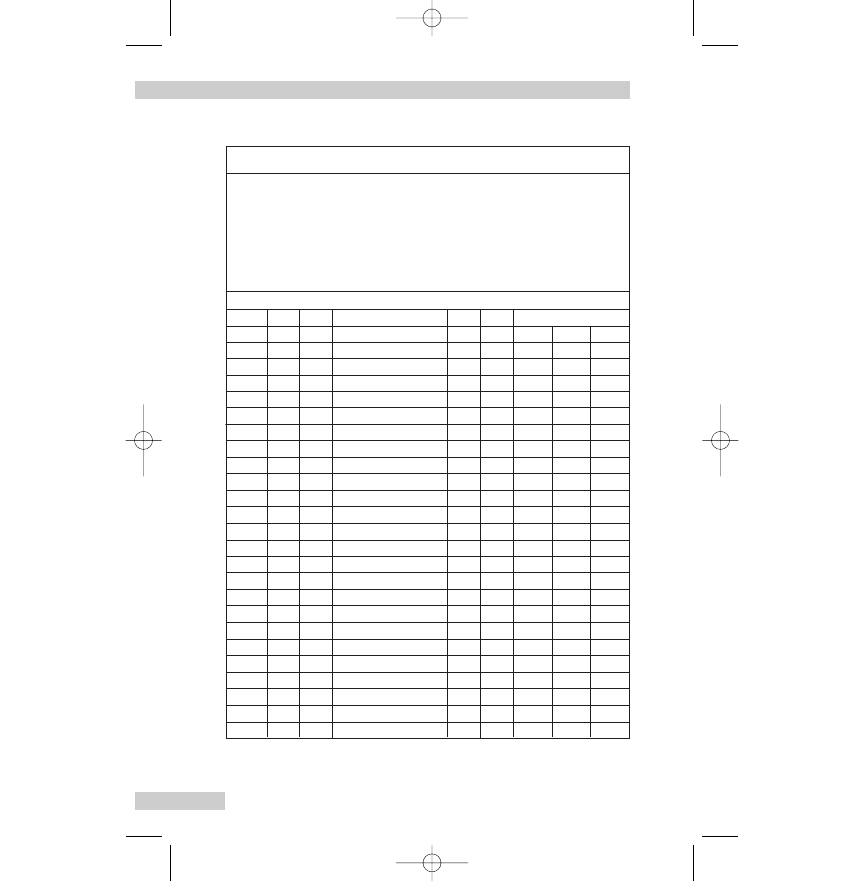
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
42
Time (hrs)
Fluid intake
Oral
IV
Other (specify route)
Fluid output
Urine Vomit
01.00
Other (specify)
TOTAL
Hospital/Ward:
Date:
Hospital number:
Surname:
Forenames:
Date of birth:
Sex:
Fluid balance chart
02.00
03.00
04.00
05.00
06.00
07.00
08.00
09.00
10.00
11.00
12.00
13.00
14.00
15.00
16.00
17.00
18.00
19.00
20.00
21.00
22.00
23.00
24.00
Fig. 4.2
Fluid balance chart. Reproduced with permission from Nicol
et al, Essential Nursing Skills, Mosby, 2000.
C3996_04.qxd 26/02/2004 13:53 Page 42
Medicine/drug chart
It is important for you to become familiar with the medicine/
drug-related documents used in your area of practice. A basic
medication record will contain the patient’s biographical infor-
mation, weight, history of allergies and previous adverse drug
reactions. There will be separate areas on the chart for different
types of drug orders. These include:
— drugs to be given once only at a specified time, such as a seda-
tive before an invasive procedure
— drugs to be given immediately as a single dose and only once,
such as adrenalin (epinephrine) in an emergency
— drugs to be given when required, such as laxatives or anal-
gesics (pain killers)
— drugs given regularly, such as a 7-day course of an antibiotic
or a drug taken for longer periods (e.g. a diuretic or a drug to
prevent seizures).
All drugs, except a very few, are ordered using the British
Approved Name, and the order (or prescription) will include the
dose, route, frequency (with times), start date and sometimes a
finish date. There is space for the signature of the nurse giving
the drug and, in some cases, the witness. It is vital to record when
you give a drug. This is done at the time so that all staff know
that it has been given, and do not repeat the dose. Likewise, if
you cannot give the drug for some reason (e.g. patient is in
another department or their physical condition contraindicates
giving the drug), make sure that this fact is recorded on the med-
icine/drug chart and the doctor is informed if necessary.
Remember that in some situations you will need to record in
the nursing notes when you give patients a drug (e.g. if you give
analgesic drugs (pain killers)).
Informed consent
Responsibility for making sure that the person or the parents of a
child have all the information needed for them to give informed
written consent rests with the health practitioner (usually a doctor
NURSING DOCUMENTATION, RECORD KEEPING AND WRITTEN COMMUNICATION
43
C3996_04.qxd 26/02/2004 13:53 Page 43
or nurse) who is undertaking the procedure or operation. This
information will include:
— information about the procedure/operation
— the benefits and likely results
— the risks of the procedure/operation
— the other treatments that could be used instead
— that the patient/parent can consult another health practitioner
— that the patient/parent can change their mind.
Young people can sign the consent form once they reach the
age of 16 years and/or have the mental capacity to understand
fully all that is involved. If the young person cannot sign the form,
the parent or legal guardian may sign it. If an adult lacks the men-
tal capacity, either temporarily or permanently, to give or deny
consent, no person has the right to give approval for a course of
action. However, treatment may be given if it is considered to be
in the person’s best interests, as long as an explicit (clear) refusal
to such action has not been made by the person in advance.
Doctors do most invasive procedures and operations, but nurs-
es in the UK are extending their practice to include many proce-
dures that were previously done by doctors. You may work with
nurses who do procedures such as endoscopic examinations, so
it is becoming more common for nurses to obtain informed con-
sent. The patient or parent and the healthcare practitioner both
sign the consent form.
When your patients are due to have any invasive procedure,
always check their level of understanding before it is scheduled
to happen. If you are not sure about answering a question, ask
the healthcare practitioner who is doing the procedure to see the
patient and explain again. It is essential that the consent form is
signed before the patient is given a sedative or other premedica-
tion drugs.
Incident/accident form
Any non-routine incident or accident involving a patient/client,
relative, visitor or member of staff must be recorded by the nurse
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
44
C3996_04.qxd 26/02/2004 13:53 Page 44
who witnesses (sees) the incident or finds the patient/client after
the incident happened. Incidents include falls, drug errors, a vis-
itor fainting or a patient attacking a member of staff in any way.
An incident/accident form should be completed as soon as
possible after the event. Careful documentation of incidents is
important for clinical governance (continuous quality improve-
ment, learning from mistakes and managing risk, etc.) and in case
of a complaint or legal action (see above).
The following points provide you with some guidance:
— be concise, accurate and objective
— record what you saw and describe the care you gave, who else
was involved and the person’s condition
— do not try to guess or explain what happened (e.g. you should
record that side rails were not in place, but you should not
write that this was the reason the patient fell out of bed)
— record the actions taken by other nurses and doctors at the time
— do not blame individuals in the report
— always record the full facts.
Guidelines for documentation and record keeping
The basic guidelines for good practice in documentation and
record keeping apply equally to written records and to computer-
held records.
The Nursing and Midwifery Council (NMC 2002) has said that
patient and client records should:
— be based on fact, correct and consistent
— be written as soon as possible after an event has happened to
provide current (up to date) information about the care and
condition of the patient or client
— ‘be written clearly and in such a way that the text cannot be
erased’ (rubbed out or obliterated)
— be written in such a way that any alterations or additions are
dated, timed and signed, so that the original entry is still clear
— ‘be accurately dated, timed and signed, with the signature
NURSING DOCUMENTATION, RECORD KEEPING AND WRITTEN COMMUNICATION
45
C3996_04.qxd 26/02/2004 13:53 Page 45
printed alongside the first entry’ (this is even more important
because your last name may not be very common in the UK)
— ‘not include abbreviations, jargon, meaningless phrases, irrele-
vant speculation and offensive subjective statements’
— ‘be readable on any photocopies’.
Note: Although the NMC guidelines clearly state that abbrevia-
tions should not be used in patient/client records, because you
will see and hear abbreviations used in medical notes and han-
dover reports, a list of commonly used ones is provided in
Chapter 9 to help you understand what people mean.
The NMC goes on to say that records should:
— ‘be written, wherever possible, with the involvement of the
patient, client or their carer’
— ‘be written in terms that the patient or client can understand’
— ‘be consecutive’ (uninterrupted)
— ‘identify problems that have arisen and the action taken to rec-
tify’ (correct or put right) them
— ‘provide clear evidence of the care planned, the decisions
made, the care delivered and the information shared’.
OTHER WRITTEN COMMUNICATION
Letter writing
Letters may be professional, business or private. The private type
is obviously easier to write, but there are, nevertheless, certain
basic rules to be remembered.
The envelope
— It is becoming increasingly common in the UK to put the
sender’s name and address on the back of the envelope, par-
ticularly when sending packages and important documents.
However, most people in the UK throw away envelopes as
soon as letters are opened, so if you want an answer you must
write your full address on the letter itself.
— It is correct to address people as Mr, Ms, Mrs or Miss with ini-
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
46
C3996_04.qxd 26/02/2004 13:53 Page 46
tials and last name (e.g. Miss J Smith or Mr O Massoud). Many
women prefer to be addressed as Ms, regardless of marital sta-
tus, and certainly Ms should be used where you are unsure. A
married woman or a widow may be addressed as Mrs unless
she has some other title or is known to prefer Ms. An unmar-
ried woman may be addressed as Miss. There is a growing ten-
dency to omit the title completely and simply use the name
(Jill Smith or Omar Massoud) on the envelope. Other titles,
such as Professor or Dr, should be used if appropriate.
— When writing a professional or business letter to a college, a
company, an hotel, a professional journal, etc., the letter must
be addressed to someone. You would, in fact, write to the
Principal of a college, to the Secretary or Manager of a com-
pany, to the Manager or Receptionist of an hotel and to the
Editor of a professional journal.
— The address follows the name, in this order:
i. the number of the house and the name of the street (on
the same line), or the name of the house (e.g. Allgoods
Cottage) with the street name on a separate line
ii. village, town or city
iii. county (and country if written from abroad)
iv. postal code.
For example:
Ms C Gower
116 Tenby Drive
Fakenham
Norfolk
PE57 1ZZ
As can be seen from the above example, usual practice is to omit
punctuation from the details of the name and address. On word-
processed or typewritten letters, indentation is no longer used.
The letter
— The sender’s address is written in full at the top right-hand side
of the paper. It is not usual to put your name there. In care
NURSING DOCUMENTATION, RECORD KEEPING AND WRITTEN COMMUNICATION
47
C3996_04.qxd 26/02/2004 13:53 Page 47
homes and hospitals and other places where official writing
paper is printed, the address, including the telephone num-
ber and e-mail address, is either on the right-hand side or in
the centre.
— In private letters the date is usually written below the sender’s
address in the order: day, month, year (e.g. 7 June 2006, or
sometimes as 7.6.2006).
— In a professional or business letter, the name and address of
the person to whom the letter is written are placed on the left-
hand side, at the top, with the date written below the address.
— When you write to an unknown person the letter begins ‘Dear
Sir’, or ‘Dear Madam’ if it is to a woman. If you are unsure,
write ‘Dear Sir/Madam’.
— When you have met the person or corresponded before, the
last name is used and the letter begins with ‘Dear Dr Sanchez’.
If you know the person well or they have signed previous let-
ters to you with their first name it is usual to address them by
their first name (e.g. ‘Dear Rao’).
— When writing to a friend, one begins ‘Dear John’, ‘Dear Farida’,
or ‘My dear Elizabeth’, to a closer friend.
— If the letter begins ‘Dear Sir or Madam’, the ending should be
‘Yours faithfully’.
— If the letter begins, ‘Dear Ms Steele’ or some other name in a
professional or business correspondence, the ending should
be ‘Yours sincerely’.
— ‘With best wishes’, ‘With kindest regards’ or ‘Yours’ are quite
usual endings for letters to friends, or colleagues who you
know well.
— Phrases such as ‘Yours respectfully’ are no longer used. Nor is
it UK practice to use very flowery, effusive (over the top) lan-
guage in a professional or business letter. Write clearly and
simply and briefly in a professional or business letter.
— Each new subject or aspect of the subject should be dealt with
in a separate paragraph. In a handwritten letter the para-
graphs are marked by starting a little distance from the left
side, or in word-processed letters by leaving space between
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
48
C3996_04.qxd 26/02/2004 13:53 Page 48
the paragraphs.
— It is important to print your name in block letters underneath
your signature, as names are often very difficult to read in
handwriting. Also, note that in the UK the numbers one and
seven are written thus: 1, 7. Figures written in the style used
in continental European countries may cause delay, and even
loss, to correspondence
— In situations where you have written asking for information
such as details of a course, the institution may write to thank
you for your interest and ask you to send an envelope with
your address and enough postage stamps (stamped addressed
envelope), so they can send you the printed material. The
request for such an envelope is usually abbreviated to ‘please
send/enclose an SAE’.
Writing electronic mail
The use of electronic mail (e-mail) is increasingly important for
both professional and private communication. The following list
provides you with some guidance:
— Remember that e-mail cannot be 100% secure or confiden-
tial – it may be read by other people. It is especially important
to make sure that e-mail containing patient/client details is
only seen by those authorised to do so. Always follow the
local protocols for keeping computer records confidential.
— It is important to be concise. People often get many e-mails
each day and you want them to read yours.
— It is good sense to think before you send any written commu-
nication – you can change your mind right up to putting a let-
ter in the postbox, but once you click on post/send for e-mail
it is too late to change your mind. Feeling upset or angry is not
an ideal time to send an e-mail.
— In common with professional or business letters, it is usual to
address people as Mr, Ms, Mrs, Miss, Dr, etc., unless you know
them well and generally use their first name.
NURSING DOCUMENTATION, RECORD KEEPING AND WRITTEN COMMUNICATION
49
C3996_04.qxd 26/02/2004 13:53 Page 49
— It is not appropriate to use e-mail abbreviations (e.g. ‘BTW’ for
‘by the way’) or nursing/medical abbreviations in professional
e-mail. Not everyone will know what the abbreviation means,
or an abbreviation may have more than one meaning.
— It is not necessary to overuse punctuation in e-mail, such as
using many exclamation marks. It is much better to let your
text emphasise the important points. Likewise, it is not usual
to use upper case (capital) letters for whole words, as this is
the e-mail equivalent to shouting.
— A reply is not always instant. It is important to remember that
although e-mail usually reaches its destination in just a few
minutes, it can take longer. Some people read and reply to
their e-mail several times a day, but others may only check
once a week.
REFERENCES
Nursing and Midwifery Council (NMC) 2002 Guidelines for
records and record keeping. NMC, London.
FURTHER READING
Hoban V 2003 How to ... handle a handover. Nursing Times
99(9):54–55.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
50
C3996_04.qxd 26/02/2004 13:53 Page 50
Communication in
nursing
INTRODUCTION
Being able to communicate is an essential skill for all health pro-
fessionals and it is particularly important for nurses who are with
people and their families for many hours a day. It is not always
easy to understand what people are saying or to get them to
understand what you are trying to tell them. Sometimes nurses
who qualified in the UK have difficulties understanding people
who have regional accents and many patients use different words
for feelings and everyday events. Some of these words are part of
this chapter, and Chapter 6 (Colloquial English) gives you lots
more examples.
Nurses need to communicate so they can find out about the
people in their care by taking a nursing history, give them infor-
mation about their care and teach them about managing their
illness.
This chapter will help you with some of the questions needed
to take a nursing history and plan care based on a commonly
used Activities of Living Model of Nursing (see Roper et al 1996)
and some other important nursing issues (e.g. confusion and anx-
iety). Short case histories that focus on a particular activity are
included to help you with some common situations. There are
extracts from dialogues (conversations) between nurses and peo-
ple/clients/relatives that give you examples of what they may say
to you in answer to your questions. These case histories will be
useful when you deal with similar situations at work, and later
reflect on the positive and negative features of a particular con-
versation you had with a patient/client and their family.
51
5
C3996_05.qxd 26/02/2004 13:56 Page 51
Note: All the people and case histories used are fictitious and
are not based on any persons we have nursed or met when
supervising students
GETTING STARTED
The first words you say to a person are very important – you need
to get it right. You need to say who you are and why you are
there. What you say will depend on the situation, but you might
start with:
‘Hello [or good morning/good evening] Mrs Jones I am Nurse [your
last name/surname/family name].’
or just use your first and last names and say that you are the
nurse who will be caring for them for the shift (or whatever is
appropriate).
Ask Mrs Jones what she likes to be called. You will hear
patients and nurses using lots of different forms of address; for
example, the titles Mr, Ms, Miss, Mrs or Dr with the last name, or
first names, or sometimes endearments such as love, dear, gran,
nan, grandpa, honey, darling, mate, pet, hen, duck, etc. As a gen-
eral rule it is not acceptable to use endearments when speaking
to patients. Do not use a person’s first name unless they ask you
to do so. It is important to follow a person’s wishes about their
preferred form of address – make sure that this is written in the
nursing notes for all nurses to read.
Once you know what the person wants to be called you can
start to get the information needed to plan nursing care, explain
the care, tests or treatment planned, and answer any questions.
Remember that if you cannot answer a person’s question it is
important to get another nurse, doctor or other healthcare pro-
fessional to do so.
Whenever possible ask simple questions that will ensure you
get the exact information needed, and avoid using jargon. For
example, saying to Mrs Jones ‘I will be back to do your vital signs
or obs’ will mean nothing to her – you will need to explain that
you will be back to record her blood pressure, temperature, pulse
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
52
C3996_05.qxd 26/02/2004 13:56 Page 52
and respiration. Always check any prepared documents that
arrive from the admissions office or the emergency department –
the person’s details may have changed or there might be a
mistake.
Biographical data
— You will need to start with the assessment sheet, finding out
details about your patient such as their full name, where they
live (address) and who with.
‘Mrs Jones can you tell me your full name [first name or forename
followed by last name which is also called the surname or family
name] and your address and telephone number.’
If you ask where they live patients might say ‘In the town’ or
‘With my husband’, so it is best to ask for the address (house
number/name, the street, the town, county and the postcode,
see Ch. 4). If you have problems spelling a name or address,
always ask the patient or their relative to spell it out letter by
letter or even copy it out for you – it must be accurate. It is
important to ask your patient’s age and date of birth, e.g.
57 years, 22/2/1946. In the UK dates are always written in the
order day, month and year.
— Always ask the name and address of the patient’s next of kin,
and get telephone numbers (daytime and for use at night) in
case it is necessary to contact family members. Obviously this
might be necessary if the patient’s condition worsens, but it
might be to say that the person can come home so please can
the family bring in outdoor clothes. If the next of kin lives
many miles away the patient may give you contact details of a
friend or neighbour (someone living close to them).
— An assessment includes asking about the patient’s religion (if
any) or spiritual needs, so you can plan care that ensures any
religious, spiritual or cultural needs are met. These needs may
include attending a religious service/ceremony, having a visit
from a religious leader, priest, minister, mullah, rabbi, etc., or
COMMUNICATION IN NURSING
53
C3996_05.qxd 26/02/2004 13:56 Page 53
having facilities for prayer, needing to fast or having special
food.
‘What religion are you Mrs Jones?’
Then you can ask appropriate questions, such as
‘Will you want to see your minister or visit the hospital chapel?’
In the UK many patients will answer with the abbreviation for
their religion, e.g. ‘C of E’ for Church of England or ‘RC’ for
Roman Catholic.
Work (employment) history
You will need to ask the patient if they work. This usually means
paid work, but many people in the UK do unpaid voluntary work
and this should also be recorded on the assessment form.
Once you know that the patient works you can get more
details. The type of work may be influencing their health (e.g.
exposure to substances such as asbestos that can cause cancer,
work in a dusty environment and chest diseases, or back pain
where heavy objects must be moved). The length of time off
work following an operation will depend on the type of work the
patient does, and in some situations patients cannot go back to
their old job (e.g. some driving jobs following a heart attack
(myocardial infarction)).
The question:
‘What do you do?’
usually means ‘What is your work?’. Patients may tell you where
they work (i.e. the company name) rather than the type of job
they do. So if they say
‘I’ve been at Clarks since I left school and that’s nearly 30 years’
you will have to ask:
‘What job do you do at Clarks?’
‘Do you work full time or part time?’
‘How many hours do you work in a week?’
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
54
C3996_05.qxd 26/02/2004 13:56 Page 54
‘Do you work shifts?’ (This relates to irregular hours, e.g. in a
hospital or factory.)
‘How long have you been doing this job?’
‘Do you have a stressful job? ‘Do you work late or have to take
work home?’
If patients are not working you need to find out why – are they
retired from work and, if so, ask what type of work they used to
do, looking after children or a relative, looking for work, study-
ing or unable to work for health reasons.
Reason for admission or contact with health services and
medical details
— The patient’s understanding of reason for admission/treat-
ment, etc. It is important to find out exactly why the patient
thinks they have visited the general practitioner/practice nurse,
or come into hospital or the care home. It might be correct to
ask a direct question such as:
‘What do you think is the matter with you?’
or
‘Tell me why you have come in today.’
This last type of comment might be used for a patient coming
in for a planned operation. The patient may say something
like
‘I’ve come in to get my cataract done [operated on].’
Sometimes you will need to use questions such as:
‘Have you been having some problems at home?’
and the patient may say:
‘I’ve been having dizzy turns [vertigo] when I keel over [fall over].’
or
‘I had a spell [a period of time] of feeling very down [depressed
mood] but that has cleared up [got better, disappeared] now.’
COMMUNICATION IN NURSING
55
C3996_05.qxd 26/02/2004 13:56 Page 55
You will also need to check that the family know why the
patient has been admitted.
— Past medical history and family history. You will need to ask
about past illnesses or operations. For example, a patient com-
ing in for a routine operation may have type 1 diabetes or they
may have severe arthritis that makes walking very difficult and
you will need to plan care accordingly. You might ask:
‘Have you ever had any serious illnesses in the past?’
‘Have you ever had an operation?’
‘Have you ever been in hospital before?’
‘Have you ever had any accidents or injuries?
‘Is there anything else you’d like to tell me?
As some illnesses, such as some types of heart disease and dia-
betes, may run in certain families (familial) you will also need
to ask about the family medical history:
‘Are there any serious illnesses in you family?’
— Allergies. Always ask about any allergies, including foods, drugs
(see below) and other substances such as washing powders:
‘Are you allergic to anything?’
‘Have you any allergies?’
It might be necessary to ask the family, for example, if the
patient is a child, has dementia or is unconscious.
— Drugs. It is necessary to ask all patients/clients if they are tak-
ing any drugs, but it is worth remembering that some patients
will associate the word ‘drugs’ with illegal substances and drug
misuse, so you can ask:
‘Are you taking any medicines (or drugs)?’
Always ask patients about all types of drugs, including those
prescribed by a doctor or nurse, drugs they buy at the chemist
(pharmacy) or supermarket (over-the-counter drugs), natural
remedies such as St. John’s Wort, and if appropriate ask about
recreational (illegal) drugs such as cannabis. It is vital to know
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
56
C3996_05.qxd 26/02/2004 13:56 Page 56
about any drug allergies (e.g. penicillin) or adverse drug reac-
tions. Always ask and make sure that this is recorded in all the
relevant nursing documentation.
Physical function and effects of current illness on daily living
or work
Many areas of physical function, such as mobility (moving about),
are covered in the dialogue section (see pp. 59–123), but you will
need to ask how the current illness affects everyday life.
For example:
‘Is there anything you need help with at home, such as getting out of
bed or making a cup of tea?’
‘How often does your neighbour come in to help you?’
‘Are you still able to work?’
Social history
— Support networks are important particularly after discharge.
You can ask questions that include:
‘Do your family live close by?’
‘Who will be at home to look after you when you are discharged?’
‘Will you be able to stay with your family until you are able to
manage back at home?’
— Type of home. Although you know the patient’s address, you
also need to know about the type of home they have. Patients
who live alone in a big house may be unable to keep it heat-
ed or clean after discharge, and a patient who lives in a flat up
several flights of stairs may need to be found a ground-floor
flat before they can go home. You will need to ask questions
that include:
‘Do you live in a house, bungalow, flat, bedsit, etc.?’
(A bedsit is a room used for both sleeping and daytime activ-
COMMUNICATION IN NURSING
57
C3996_05.qxd 26/02/2004 13:56 Page 57
ities with the use of shared kitchen and bathroom.)
‘How do you heat your home?’
(Patients may not be able to manage an open fire or may not
use expensive heating if they are living on a low wage, pen-
sion or benefits.)
‘Do you have good neighbours?’
(The patient may be relying on the neighbours to check the
house, feed pets, take in post and do things like cutting the
grass while they are in hospital.)
— Social problems due to present condition/admission. Patients
admitted as an emergency may be worried about children or
others such as older relatives at home who depend on them.
Many people in the UK have pet animals such as a cat or dog
and you should always ask if they have a pet, and if someone
is caring for them.
‘Do you have any pets at home?’
‘What’s your cat’s name?’
‘Who is feeding Harry?’
You will need to listen very carefully, as a patient with
dementia, for example, may keep repeating the name of the
pet animal rather than tell you the details. Patients can be very
anxious about the care of their pet animals while they are in
hospital or a care home.
— Hobbies and interests.
‘How do you spend your free time?’
‘How much exercise do you take?’
‘Do you play any sports?’
‘Have you any hobbies?’
‘Do you like to watch TV [television] or listen to music?’
— Contacts with and input from other health and social care
professionals. Many older patients will already be in contact
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
58
C3996_05.qxd 26/02/2004 13:56 Page 58
with a wide range of health and social care professions, such
as a district nurse, health visitor, practice nurse, general prac-
titioner (family doctor), physiotherapist, occupational thera-
pist, speech and language therapist, dietician, podiatrist or
social worker. You should ask about this and find out who
comes, how often and what they do:
‘Do you see the nurse at home?’
‘What do the nurses do?’
‘Do they come in everyday?’
Lifestyle
During the nursing assessment you will need to find out about
lifestyle or behaviour that can influence health in both good or
bad ways (e.g. the type of foods eaten, amount of exercise, alco-
hol intake, use of drugs, use of tobacco, sexual behaviour and
high-risk leisure activities). Often a person’s lifestyle or behaviour
is sensitive and they may feel embarrassed or guilty if you ask lots
of questions. Thus direct questioning does not always work well
in this situation, but often you will be able to get the information
as the patient talks about their lifestyle and view of health. For
example, a patient may tell you, without any prompting, that they
know they do not get enough exercise and you can find out more
by asking them what they mean. Sometimes, however, you will
need to ask more directly and the sort of questions that may be
needed to get information about some of these lifestyle issues are
discussed in the following section under the related activity.
BREATHING
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with breathing
are given in Box 5.1.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
COMMUNICATION IN NURSING
59
C3996_05.qxd 26/02/2004 13:56 Page 59
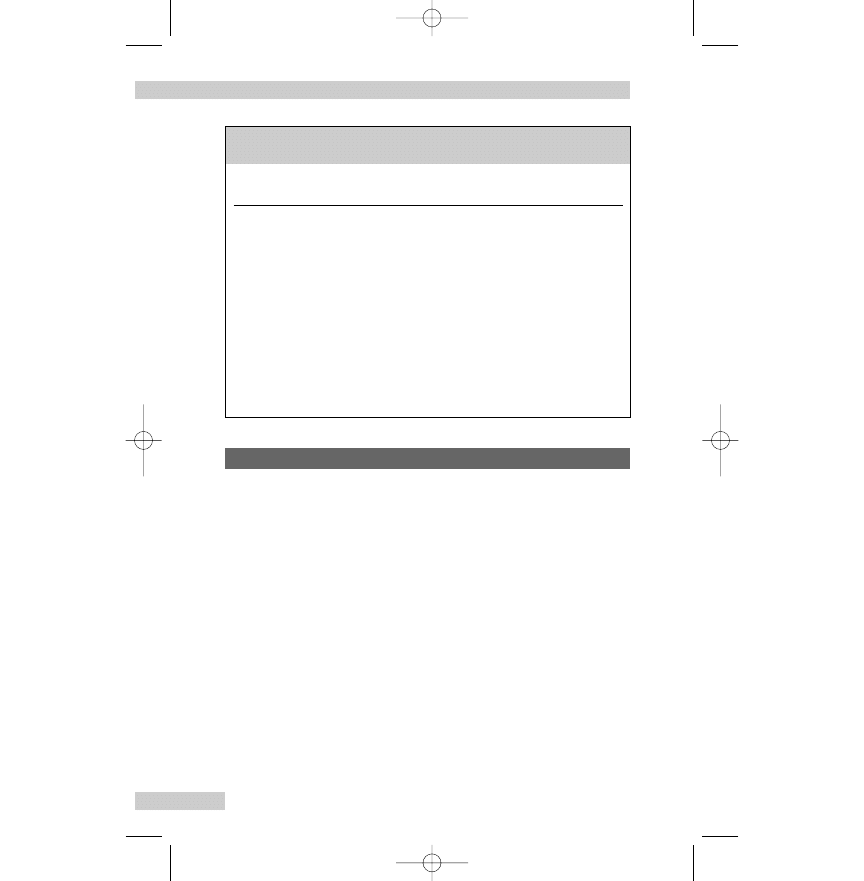
Mr Ryan has been admitted to the medical assessment unit with
a chest infection causing an exacerbation [worsening] of his
chronic obstructive pulmonary disease (COPD). He is very dis-
tressed and finding it hard to breathe. His wife tells you that ‘His
breathing has been bad for years and he can’t get about much
these days’ – meaning that his mobility is reduced. You can get
the biographical data from Mrs Ryan, and as soon as Mr Ryan’s
condition improves you can find out more about his breathing
and related problems. You might also want to ask Mrs Ryan if
her husband becomes confused or mixed up [disorientated], as
this may be a sign of reduced oxygen getting to the brain
(caused by hypoxia), or if he is more drowsy [sleepy] than nor-
mal. This may happen if there is too much carbon dioxide in the
arterial blood (hypercapnia).
Nurse:
Mrs Ryan have you noticed a change in your husband’s
mental state recently, does he get confused?
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
60
Box 5.1
Words associated with breathing (for further examples
see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Dyspnoea
Breathlessness; out of breath; puffed; short of
breath; fighting for breath (severe cases)
Expectorate
To bring up/cough up phlegm; spit
Expiration
Breathing out
Inhaler for drugs
Puffer
Inspiration
Breathing in
Respiration
Breathing
Sputum
Phlegm (pronounced flem)
Case history – Mr and Mrs Ryan
C3996_05.qxd 26/02/2004 13:56 Page 60
Mrs R.: Now you come to mention it he does seem a bit dotty
[silly] sometimes. You know, not always knowing
where he is.
Nurse:
Hello Mr Ryan tell me about the problems you have with
your breathing.
Mr R.:
I’m breathless most of the time but the infection
made it much worse – I was really frightened and felt
that I was fighting for breath until the treatment (more
bronchodilators, corticosteroids and antibiotic therapy)
started to work [became effective].
Nurse:
Before the infection how was your breathing? Were you
breathless sitting still?
Mr R.:
Oh no, only when I tried to walk about.
Nurse:
Can you normally get upstairs in one go [without
stopping]?
Mr R.:
Only if I rest on the landing [flat part of a staircase] and
get my breath back [recover].
Nurse:
How far can you walk on the level without getting
breathless?
Mr R.:
I can get as far as the back garden but I’m fair jiggered
[exhausted, breathless] after.
Nurse:
Is there anything else about your breathing? Do you
wheeze [make an audible noise when breathing]?
Mr R.:
Yes, I do wheeze and my chest often feels tight,
but Dr Singh is going to put me on something new
[prescribe a different drug], so hopefully that will do
the trick [hopes the new treatment will be effective] –
fingers crossed [hope for good luck].
Nurse:
Hope so.What medicines were you taking at home before
you came into the ward?
Mr R.:
The blue inhaler [salbutamol inhaler], and the antibiotics
from the GP for the infection.
Nurse:
Are you using oxygen at home?
Mr R.:
Yes, for up to 15 hours a day. It’s OK, we have a
machine that takes some gases out of the air and
leaves the oxygen [oxygen concentrator] for me, so the
COMMUNICATION IN NURSING
61
C3996_05.qxd 26/02/2004 13:56 Page 61
missus [wife] doesn’t need to keep changing cylinders
and I can get around in the house and out as far as the
back garden.
Nurse:
What else helps your breathing?
Mr R.:
Well – sitting up and leaning on the table helps, but
when I’m very chesty [trouble with chest, coughing] it’s
better to sleep downstairs in an armchair. At least the
wife gets some sleep even if I don’t. A while ago I
started doing relaxation exercises and that helps when
I feel panicky [frightened], but they didn’t work last
night – worse luck.
Nurse:
Do you still smoke?
Mr R.:
No, not for years.
Nurse:
When did you stop smoking?
Mr R.:
I used to smoke roll-ups [cigarettes that the patient
makes himself] and I cut myself down [reduced the
number of cigarettes] to 10 a day, and then I said
‘That’s it. No more’ and I haven’t smoked for 5 years.
It was hard but I was determined to stick to [keep to]
no smoking.
Nurse:
That’s good, but do you still cough?
Mr R.:
Yes, cough and bring up stuff [phlegm or sputum]. I
had a smokers’ cough [early morning cough] when I
was in the Army, but now I cough any time of the day
or night.
Nurse:
What colour is the sputum you cough up? Has the amount
increased?
Mr R.:
Really green because of the infection, and much more,
and my mouth tastes foul.
Nurse:
We sent a specimen to the laboratory earlier, so I’ll get you
some sputum pots and tissues and some mouthwash.The
physiotherapist is on his way up to see you, so he will help
you to cough and clear your chest. Do you have any pain
with the cough?
Mr R.:
Not at the moment.
Nurse:
What about washing and dressing – are you able to manage
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
62
C3996_05.qxd 26/02/2004 13:56 Page 62
or do you need some help?
Mr R.:
Just need some help to wash my back and feet. She
does it at home [meaning Mrs Ryan helps].
Nurse:
How is your appetite? What about eating and drinking?
Mr R.:
I’m trying to have a drink every hour like you said, but
I can’t face [manage] a big meal.
Nurse:
I will ask the dietician to visit and discuss it with you, but
for today I can give you some nourishing drinks and order
snacks or light meals for you.
Mr R.:
Thanks, that sounds spot on [exactly right].
Nurse:
Your bed is close to the bathroom and lavatory.Will you be
able to walk or will a wheelchair be easier?
Mr R.:
It’s not far – I can get there, but after washing I might
need some help back.
Nurse:
How are you sleeping?
Mr R.:
Don’t worry I’ll sleep OK tonight – after today with
having to call the ambulance and everything I’m
knackered [exhausted].
Nurse:
Is there anything you would like to ask me?
Mr R.:
No thanks. You and the doctor explained what was
going on [happening] earlier and I do understand about
COPD. An ‘expert patient’ you might say.
Nurse:
Just ring the bell if you need me. I think Mrs Ryan went to
phone your son and have a cup of tea while we did the
paperwork. I’ll bring her in to you when she gets back.
Other questions
Mr Ryan will find it difficult to talk for long if he is breathless, so
you may need to ask some other questions later. Sometimes it will
not be necessary to ask because Mr Ryan may tell you extra
things as you are attending to his care or he may tell other health
professionals, such as the physiotherapist.
Other questions may include some of the following:
‘Do you have pain or chest discomfort on breathing or coughing?’
‘Do your ankles get swollen?’
COMMUNICATION IN NURSING
63
C3996_05.qxd 26/02/2004 13:56 Page 63
‘Is there anything that makes you cough worse, such as a smoky or
dusty atmosphere, or changes in temperature like going out into the
cold? Does any position make it worse?’
‘Have you noticed any blood in your sputum?’ Is there a lot of blood
or is it streaked with blood?
COMMUNICATING
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with communi-
cating are given in Box 5.2.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
64
Box 5.2
Words associated with communicating (for further
examples see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Diplopia
Double vision; seeing double
Dysarthria
Can't get the words out
Dysphasia (aphasia)
I know what to say but nothing comes out; I
can't find the right word; the sentence comes
out all wrong; I can say the word but I don't
know what it means
Hearing impairment,
Hard of hearing; deaf as a post
deafness
Tinnitus
Ringing, buzzing or roaring sound in the ears
Visual impairment,
Can't see the hand in front of me; blind as a bat
blindness
Vertigo
Dizzy; dizziness; giddy
C3996_05.qxd 26/02/2004 13:56 Page 64
Mrs Egbewole had a stroke (cerebrovascular accident) about
18 months ago, and her family, with the help of twice-daily visits
from the home carer, usually look after her at home. She has
come into the care home while her family has a short holiday.
The stroke has left Mrs Egbewole with left-sided paralysis and
poor balance. She does not have dysphasia, but because the left
side of her face is also paralysed she sometimes has slurred
speech and dribbles saliva. She also has problems with non-
verbal communication because her facial expression is affected.
Nurse:
Mrs Egbewole, do you have any problems with your speech?
Mrs E.: It is slurred sometimes, but that’s because my mouth
doesn’t work properly.
Nurse:
How does that make you feel?
Mrs E.: I feel really embarrassed, especially if I’m talking to
someone new.
Nurse:
How can we help?
Mrs E.: I’ll be all right as long as [provided] people give me
enough time to get the words out. It gets me flustered
[agitated/confused] if people are impatient’
Nurse:
I’ll make sure that is recorded in your care plan and that all
members of staff know to give you plenty of time to tell us
things. Did you see the speech and language therapist after
the stroke?’
Mrs E.: Yes, but I couldn’t handle it [cope] so soon after losing
my husband [my husband died].
Nurse:
How would you feel about trying again with speech and
language therapy?
Mrs E.: If you think it might help I’m willing to give it another
go [try again].
Nurse:
Fine – I’ll organise a referral. Is there anything else that’s
troubling you?
Mrs E.: Well yes there is, and it’s all down to [caused by] the
muscles in my face not working properly. I can’t help
dribbling [saliva flows from the mouth].
COMMUNICATION IN NURSING
65
Case history – Mrs Egbewole
C3996_05.qxd 26/02/2004 13:56 Page 65
Nurse:
You obviously know about keeping the skin round your
mouth clean and dry because there is no sign of soreness.
Mrs E.: Yes, the nurses on the stroke unit really stressed good
skin care. But another thing that worries me is the look
of my face – it’s really lopsided [asymmetrical] and
when I try to smile I must look dreadful.
Nurse:
Maybe the speech and language therapist can suggest
something to help, but you could mention it to Dr Newell.
She will be in this afternoon.
Mrs E.: That’s a good idea – I will add it to my list of questions
I have for her.
Nurse:
How is your sight? I see you have spectacles/glasses on at
the moment.
Mrs E.: Yes, I’m blind as a bat without them [usually meaning
poor vision rather than completely blind] and have
needed help for years. I used to have contact lenses,
but after my stroke I found it too difficult to take them
out, so I got some specs [short for ‘spectacles’].
Nurse:
Do you have a second pair for reading or does the one
pair do for everything?
Mrs E.: They are bifocals and I am supposed to look through a
different bit for reading. But if the print is very small,
such as on food labels, I use a magnifying glass instead.
Nurse:
Did you bring the magnifying glass in with you?
Mrs E.: Oh yes, my carer packed everything but the kitchen
sink [implies that the carer was very thorough when he
packed Mrs Egbewole’s suitcase].
Nurse:
Who normally cleans your spectacles?
Mrs E.: My lovely [meaning admirable in this case] carers do
that, I can’t with only one good hand.
Nurse:
Would you like me to give them a clean now?
Mrs E.: Thanks – they’re not very clean and it makes things
look blurred.
Nurse:
Do you have any other problems with your eyes?
Sometimes a stroke can affect vision, such as seeing
things double.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
66
C3996_05.qxd 26/02/2004 13:56 Page 66
Mrs E.: Oh no, I was lucky [that the stroke did not affect her
sight]. When I was younger I suffered terribly [very
badly affected] with migraine and then I used to see
flashing lights with a zigzag pattern before the
headache came on [started]. If I’m out in a cold wind
my eyes start running [watering; tears flow down the
cheeks], but that’s normal.
Nurse:
Definitely normal – it certainly happens to me.
Mr Sandford is 42 years old and has poor hearing, tinnitus and
problems with the build-up of earwax, which also affects his
hearing. He has Down syndrome and lives independently at the
local group housing complex where he has a bedsit. He works
full-time in a supermarket. His parents are dead, but his two older
sisters, who live close by, see him several times a week and he
has many friends from work and in the house.
Nurse:
Hello Mr Sandford, I’m Nurse MacGregor. I understand that
you have come to see us about your hearing.
Mr S.:
Hello, everyone calls me Nick. My hearing is no good,
I can’t hear them on the telly [television] or the boss
[manager] at the shop.
Nurse:
Can you hear me all right?
Mr S.:
Yes.
Nurse:
What would you like me to call you?
Mr S.:
You can call me Nick if you like.
Nurse:
OK. Has your hearing always been bad Nick?’
Mr S.:
Not as bad – it’s really bad now and I can’t hear the telly.
Nurse:
What do you like on the telly?
Mr S.:
I watch Eastenders and Coronation Street [both popular,
long-running series in the UK], they’re the best and I
like the football as well.
Nurse:
What helps you to hear?
Mr S.:
Like now when I can see you and nobody else is
talking. When I’m calm.
COMMUNICATION IN NURSING
67
Case history – Mr Sandford
C3996_05.qxd 26/02/2004 13:56 Page 67
Nurse:
Anything else?
Mr S.:
The ear wash [ear irrigation, previously known as
‘syringing’] but it feels funny [strange].
Nurse:
We can have a look inside your ears with the special light
[otoscope] to check for wax, you might need another ear
wash to help you hear.
Mr S.:
OK.
Nurse:
Have you got a hearing aid?
Mr S.:
Don’t like it.
Nurse:
What don’t you like?
Mr S.:
It’s broken.
Nurse:
Have you got it with you? Perhaps the technician can
mend it.
Mr S.:
Here it is, but it’s no good.
Nurse:
I’ll take it to the technician in a bit [in a short while]. Does
anything else happen as well as not being able to hear?
Mr S.:
Roaring [loud noise] and buzzing [like the sound made
by insects] in my ears.
Nurse:
Anything else?
Mr S.:
My ears feel stuffed up [fullness] and I get giddy
[experience vertigo] and stagger.
Nurse:
Do you fall over?
Mr S.:
I know it’s coming, so I sit down.
SAFETY AND PREVENTING ACCIDENTS
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with safety and
preventing accidents are given in Box 5.3.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
Mrs Kaur has scalded her arm while making a cup of tea. Her
neighbour brought her to the Emergency Department after they
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
68
Case history – Mrs Kaur
C3996_05.qxd 26/02/2004 13:56 Page 68
had bathed the damaged area with lots of cool water and kept it
cool on the way to hospital with a wet towel. She is upset about
being so clumsy and feels that she has been a nuisance to her
neighbour and to the hospital staff who already have enough to
do. Luckily the skin damage is superficial and should be com-
pletely healed in a few days.
Nurse:
Hello again Mrs Kaur. Have the painkillers worked [taken
away the pain]?
Mrs K.: Hello Nurse. Yes, the pain is much less. My arm just
feels sore [tender].
Nurse:
The plan is to keep the scald dry and warm and let it heal.
I’ve come to put a dressing on your arm.
Mrs K.: I don’t want anything that will stick.
Nurse:
The dressings we use don’t stick anymore, they are made
to be non-adherent.
Mrs K.: I remember the pain years ago when dressings did stick.
Nurse:
The dressing only needs to be on for a few days and the
scald will heal. It was a good thing that you knew the first
aid for scalds, cooling the skin down certainly stopped it
getting any worse.
COMMUNICATION IN NURSING
69
Box 5.3
Words associated with safety and preventing accidents
(for further examples see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Fall
Took a tumble; lost my footing; tripped up
Fracture
Broken or cracked (as in bone)
Seizure
Fit; funny turn; convulsion; an attack
Sprain
Twisted (as in ankle)
Syncope
Fainting attack; black out; collapse; pass out
Unconscious
Knocked out (KO'd); out cold; dead to the
world; out of it
C3996_05.qxd 26/02/2004 13:56 Page 69
Mrs K.: I saw a thing on the telly [television] about what to do
with burns. But what about some burn ointment? It
must need something.
Nurse:
If you leave the dressing on for 2 or 3 days the scald will
heal without any other treatment.You can take mild
painkillers such as paracetamol if your arm is sore.
Mrs K.: I don’t like the idea of taking it [the dressing] off
myself.
Nurse:
Well today is Saturday, so it should all be healed by
Monday.You can get an appointment with the practice
nurse for Tuesday and she can take off the dressing and
check your arm.
Mrs K.: Sounds sensible – I will do that. I really feel such a
fool – how could I pour boiling water over myself. I
am doing all the silly things my granny [grandmother]
did when she was 80.
Nurse:
How do you think it happened?
Mrs K.: I can’t seem to judge where the cup is. It’s the same
when I pour orange juice into a glass. And the kettle is
so heavy.
Nurse:
Have you had your eyes checked recently?
Mrs K.: My routine test must be due very soon – I will phone
on Monday.
Nurse:
Could you talk to the practice nurse about the trouble
[difficulty] you have when pouring fluids?
Mrs K.: Yes, do you think I should tell her about how things
are blurred and sometimes lines look very odd and
wavy?
Nurse:
That sounds like a good idea. But what can you do to make
the kettle easier to use?
Mrs K.: I forget it’s only me having a drink and usually fill it
too full.
Nurse:
Yes, I just fill mine without thinking. I have seen smaller
kettles. Perhaps you would find that easier.
Mrs K.: My daughter can get me one when she goes to the
big shops.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
70
C3996_05.qxd 26/02/2004 13:56 Page 70
Mr Anderson is going home with several different drugs. He has
been in hospital to have intravenous antibiotics for cellulitis and
needs to have a course of oral antibiotics (phenoxymethylpeni-
cillin, flucloxacillin and metronidazole). He also takes an
antiepileptic drug (sodium valproate) to control generalised
seizures and a diuretic (torasemide) for hypertension.
Nurse:
The antibiotics for you to take home have come up from
the pharmacy and I would like to go over [discuss] what
you need to do.There are instructions on the labels, but it
helps if we talk it through [discuss] as well.
Mr A.:
Yeah [yes], OK then. I want to get it right. It was a bit
of a fright ending up in here just for a cat bite gone
septic [infected].
Nurse:
What seems like such a minor thing can quickly get
really bad.There are three separate antibiotics to
take – here look [at the containers].There are two
penicillins: flucloxacillin and phenoxymethylpenicillin.You
need to take these every 6 hours and an hour before
food or on an empty stomach.These are the best ones
for your infection and you have already told us that you
are not allergic to penicillin.The other antibiotic is
metronidazole, which you need to take every 8 hours,
but this time with or after food.
Mr A.:
Yeah, no problems with penicillin and I’m used to
taking tablets – with the Epilim [a proprietary name
for sodium valproate] twice a day and the Torem
[proprietary name for torasemide] first thing [early
morning].
Nurse:
Will there be any problem with having to take two before
food and one with or after food?
Mr A.:
No, I already need to remember to take the Epilim
after food.
Nurse:
What about writing out a chart? That would help, especially
if you cross off doses as you take them.
COMMUNICATION IN NURSING
71
Case history – Mr Anderson
C3996_05.qxd 26/02/2004 13:56 Page 71
Mr A.:
I don’t write so well, but one of our kids [children] can
do it.
Nurse:
It is important to take the antibiotics at regular times and
to finish the 7-day course even if your hand seems better.
Mr A.:
Why can’t I stop once it looks better?
Nurse:
Finishing the course means that the treatment will kill off
all the bugs [bacteria in this case] – the infection is cured,
and it is very important the bugs don’t become immune
[develop resistance] to the antibiotics.
Mr A.:
What like that MRSA has? OK. I’ll carry on [continue] to
the end.
Nurse:
Yes, just like MRSA, but you haven’t got that.There are a few
other things I need to tell you about the metronidazole. It
is important to swallow the tablets whole with plenty of
water. And you shouldn’t drink alcohol while you are taking
them and for 2 days after you stop – it can cause a nasty
reaction with nausea and sickness [vomiting].You might
have a furred tongue and your urine can be dark.
Mr A.:
That’s a blow [disappointment]. I could really do with a
couple of pints [meaning he would enjoy some beer].
Thanks for the warning about my pee [urine]. That
would have really put the wind up me [alarm me].
Nurse:
Have you got plenty of Epilim and Torem at home?
Mr A.:
Yeah – I never run out of tablets [have none left]. I
dread having another fit [seizure] now that they have
settled down.
Nurse:
Have you any questions or bits you don’t quite understand?
Mr A.:
It’s a lot to take in [information to absorb, understand].
Can you go through it all again please?
Nurse:
You’re right it is a lot of information. Let’s start with the
three antibiotics and when to take them ...
MOBILITY
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with mobility
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
72
C3996_05.qxd 26/02/2004 13:56 Page 72
are given in Box 5.4.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
Joint stiffness and pain are causing Ms Wayne severe difficulties
with mobility. She has had rheumatoid arthritis for many years
COMMUNICATION IN NURSING
73
Box 5.4
Words associated with mobility (for further examples
see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Akinesia
Freezing or frozen; rooted to the spot; can't go
forward
Ataxia
Staggering; jerky; shaky; all over the place
Bradykinesia
Can't get started; slowed me almost to a halt;
slowed me down nearly to a complete stop
Dorsal part of a
Knuckle
phalangeal joint,
especially the meta-
carpophalangeal joints
(with fingers flexed)
Sudden tonic muscle
Cramp
contraction
Festination
Shuffling; can't stop once I get going
Swollen
Puffed up
Swollen and deformed
Knobbly
(as an arthritic finger
joint)
Tremor
The shakes
Case history – Ms Wayne
C3996_05.qxd 26/02/2004 13:56 Page 73
and now has some joint destruction and deformity with associat-
ed muscle wasting. At the moment she feels generally unwell –
very lethargic, her temperature is slightly elevated and she has
anorexia. In the past she has had surgery to her hands, which are
very badly affected.
Ms W.: Hello Nurse. Have you sorted out [organised] my
physiotherapy appointment yet?
Nurse:
Yes, the physiotherapist is coming to treat you here.What
do they usually do?
Ms W.: In the past I had heat treatment, but now they
concentrate on gentle exercise and making sure that
my hand splints are still helping and not making my
skin sore.
Nurse:
Tell me how your mobility is affected by the arthritis.
Ms W.: I have trouble [difficulties] getting in and out of bed, or
the bath, and I need help to get out of a low chair.
Nurse:
What about walking?
Ms W.: Getting about [moving about, going out] is hard. I get
around the house with the walking aid and tend to
use a wheelchair when I go out. The car has been
modified so at least I’m independent. I can go shopping
and out with my pals [friends].
Nurse:
Yes, that is important.
Ms W.: I’m not going to be an invalid [someone who is always
ill], always needing help and griping [complaining]
about the unfairness of it all.
Nurse:
How do you stay so positive?
Ms W.: After my joints, especially my hands, got really
bad [deteriorated] and I had to give up work [left
employment] I thought ‘I’m only 40 and can’t just do
nothing’. So I looked at ways I could be busy and
useful.
Nurse:
What do you do?
Ms W.: I go into the local primary school three mornings a
week and listen to the children read. It’s a great [good]
feeling when you hear them improve and become
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
74
C3996_05.qxd 26/02/2004 13:56 Page 74
more confident. Just lately I started helping on a
telephone helpline for people with disabilities – there
are special hands-free phones so I don’t need to use
my hands much.
Nurse:
We [meaning Ms Wayne and the nurse] can sort out your
care plan now and make sure that we include the help you
need.You must tell me your usual routine for the hand
splints, as you’re the expert. Can you arrange for your own
wheelchair to be brought in?
Ms W.: My brother can fetch it at lunchtime if I give him a ring
[contact by telephone].
Nurse:
What about other activities? Do you have difficulty using
your hands?
Ms W.: Yes, the pain and stiffness in my hands and wrists
really hold me back [curb or inhibit]. My hands look
so awful with the finger joints all puffed up [swollen]
and it’s so frustrating and it really riles [annoys, makes
me angry] me when I can’t do something simple like
doing up [fastening] buttons. It’s always worse in the
morning when you need to wash and dress, which is
a real pain [nuisance] when I’m due at the school.
Nurse:
Are there any other movements that you find difficult?
Ms W.: Anything where I have to grip and move my wrist like
holding the kettle and pouring.
Nurse:
Again we can plan what help you will need from us while
you’re here. Do you see the OT [occupational therapist]
for help with this?
Ms W.: Yes, she has been so helpful – lots of gadgets to help
me do things, like dressing and cooking, for myself,
and so many good ideas about how to do things
without getting tired or making the pain worse.
Nurse:
Perhaps your brother can bring in the gadgets you need in
here when he comes with the wheelchair.What do you
think?
Ms W.: OK. I hadn’t thought of that.
Nurse:
The rheumatology nurse specialist will be up later to
COMMUNICATION IN NURSING
75
C3996_05.qxd 26/02/2004 13:56 Page 75
review your drugs with Dr Wong [the rheumatologist], and
co-ordinate all the other practitioners – I expect you know
them both quite well by now.
Ms W.: Yes, I certainly do. Having Sam [Ms Wayne has known
the nurse specialist for several years and they use first
names] is a real support – he’s always there on the
phone and it’s so nice to see the same person at the
nurse-led clinics. I’m a bit disappointed about the new
drugs we tried – the benefits have definitely worn off
[become less effective].
Nurse:
Do you need anything for pain?
Ms W.: No, not at the moment thanks. I took all my morning
drugs at home and I’d rather wait to see what happens
after the drug review.
Mr Lajowski has come into the day-surgery unit to have a lipoma
removed from his back. His mobility is seriously affected by
Parkinson’s disease, which he has had for some years. He is not
particularly anxious about the surgery, as this was explained to
him at the pre-admission assessment clinic, but he is worried
about how he will cope with moving about in the new
environment.
Nurse:
Hello Mr Lajowski. I understand that you have come in
today to have a fatty lump [lipoma] removed from your
back and the plan is to send you home later this afternoon.
Mr L.:
Yes, that’s right. The lump needs to come off [be
removed] – it gets in the way of the waistband of my
trousers. I shall be glad to see the back of it [pleased
when it has gone]. Did they tell you that I have
Parkinson’s disease?
Nurse:
Yes, it’s in your notes from the assessment clinic. How does
it affect you?
Mr L.:
The walking is the worst. Its difficult to start moving
and I’m so slow [bradykinesia]. All I can do is shuffle
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
76
Case history – Mr Lajowski
C3996_05.qxd 26/02/2004 13:56 Page 76
[feet sliding, legs dragging, characteristic of Parkinson’s
disease] to start with and then my steps get shorter and
I get faster and faster [festination], can’t stop, and like
as not [likely] over I go [fall over]. I’ve really lost my
nerve [to lose confidence]. If you saw me you would
think I was the worse for drink [‘drink’ in this case
means alcoholic drink – the person is drunk, or
intoxicated, or inebriated].
Nurse:
Do you have any other movement problems?
Mr L.:
I get that freezing [akinesia] where I’m rooted to the
spot [can’t move]. It mostly comes on out of the blue
[comes unexpectedly], but I worked it out [found out,
realised] that trying to do more than one thing at once
[simultaneously] will bring it on [cause it]. The shaking
[tremor] in my hands is bad, and its hard to do some
things because my arms are so stiff [caused by rigidity].
Nurse:
What things are particularly difficult for you?
Mr L.:
It sounds daft [absurd], but it’s mainly things like
turning over in bed, reaching out for a cup, getting
up out of a chair and turning round once I’m up.
Nurse:
Are there things that help?
Mr L.:
I’ve learnt a few tricks [ways to overcome the problems],
such as having a good firm mattress and a high-backed
chair with arms. The others things are really simple,
like other people waiting until I’m ready to move and
giving me time to do things for myself. When I freeze,
the physio’ [physiotherapist] told me to try stepping
over an imaginary line, or to count ‘one–two’ out loud
with each step and that does help.
Nurse:
What about other activities, such as those needing fine
movements?
Mr L.:
Doing up [fastening] shoelaces or buttons is impossible,
so that material that sticks to itself is very handy
[helpful, useful]. What’s it called again?
Nurse:
Oh, you mean Velcro. It’s very useful, we use it a lot in the
rehab. [rehabilitation] unit.
COMMUNICATION IN NURSING
77
C3996_05.qxd 26/02/2004 13:56 Page 77
Mr L.:
I get loads [a lot] of cramp [sudden tonic muscle
contraction] attacks at night, so I’m awake half the
night [disturbed sleep]. Before the Parkinson’s I could
just pop out [get out] of bed and it would go.
Nurse:
Not so easy now.
Mr L.:
How right you are. I wish it would settle down
[become quiescent].
Nurse:
I gather [understand] that your medication has just
[recently] been changed.
Mr L.:
Yes, I said to the Doc [short for doctor] that the cramp
had gone on [continued] too long and he said that I
could try some different tablets.
Nurse:
Any luck with the new tablets [meaning are they
effective]?
Mr L.:
Early days [too soon to be sure], but I think the cramps
have eased off [become less frequent].
EATING AND DRINKING
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with eating and
drinking are given in Box 5.5.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
Miss Hyde-Whyte has come into the community hospital for
assessment. She lives alone and has been retired for over 20 years.
The district nursing team, who have been visiting Miss Hyde-
Whyte to treat her leg ulcer, have recently become concerned
about her lack of interest in meals and obvious weight loss.
Nurse:
Hello Miss Hyde-Whyte, I’m Nurse Mosquera. I would like
to ask you some questions.Will that be all right?
Miss H.: Hello – please call me Maggie. The rest is such a
mouthful [difficult to say].
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
78
Case history – Miss Hyde-Whyte
C3996_05.qxd 26/02/2004 13:56 Page 78
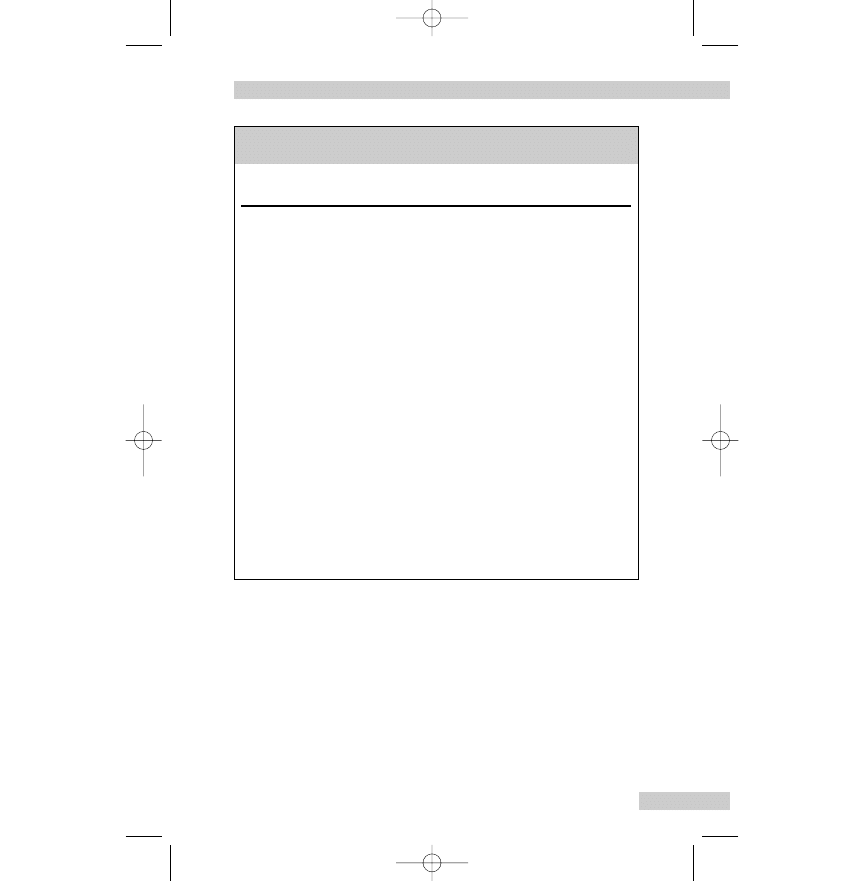
Nurse:
I will need to weigh you and measure your height, but first
a few questions.
Miss H.: I’m sure that I have lost weight – all my clothes hang
on me [are much too big].
Nurse:
How often do you eat and drink?
Miss H.: Well I used to have breakfast, a proper cooked lunch
and something on toast or a sandwich in the evening.
Nurse:
Has something changed?
Miss H.: I used to really enjoy cooking, have a G&T [gin and
tonic] and then sit at the table with a nice meal, but
COMMUNICATION IN NURSING
79
Box 5.5
Words associated with eating and drinking (for further
examples see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Abdomen
Belly; gut; stomach; tummy
Abdominal pain
Belly ache; gut rot; stomach/tummy ache
Anorexia
No appetite
Dyspepsia
Acid indigestion; heartburn
Good appetite
Always hungry; eat like a horse; ready for my
grub
Halitosis
Bad breath; mouth odour
Nausea
Biliousness; feel sick; queasiness
Oesophagus
Gullet
Poor appetite
Can't face food; don't eat enough to keep a
bird alive; been off my food; not hungry; peck
or pick at food
Stomatitis
Mouth ulcers; sore mouth
Vomit
Be sick; bring up; lose the lot; puke; retch; sick
up; spew; throw up
C3996_05.qxd 26/02/2004 13:56 Page 79
now I’ve got no appetite and I just pick at it [the food].
My dad [father] would have said you don’t eat enough
to keep a bird alive [have a poor appetite].
Nurse:
Why do you think your appetite has decreased?
Miss H.: Two reasons I think. I’ve had mouth ulcers for ages [a
long time]. Probably my false teeth [dentures] don’t fit
anymore; and I have been sick [vomited] a few times
after meals.
Nurse:
I’ll look at your mouth in a moment [in a short time] and
see if any treatment would help. It might be a good idea to
see your dentist about the poorly fitting dentures.Tell me
about the vomiting.
Miss H.: If I eat a proper meal I soon feel sick [nauseated] and
then I’m sick [vomit]. The food just comes back.
Nurse:
Are you sick at any other time?
Miss H.: No, only after food.
Nurse:
What colour is the vomit? Is there any blood or bile?
Miss H.: No blood and it’s not green or yellow like bile. The
colour varies – it depends on what I’ve eaten.
Nurse:
Sometimes blood can look like coffee grounds [describes
the appearance of partially digested blood in the
vomit] – anything like that?
Miss H.: No, nothing like that.
Nurse:
How do you feel afterwards?
Miss H.: That’s the strange thing. Once I’ve been sick I feel fine
[all right]. My stomach [abdomen] feels uncomfortable
before I’m sick, but that feeling soon goes afterwards.
Nurse:
When you were eating normally what sort of food did
you cook?
Miss H.: Proper meals – meat or fish and lots of veg. [short for
‘vegetables’] and I always had dessert or some cheese.
No point doing all that if you’re going to be sick.
Nurse:
How often do you usually shop for food?
Miss H.: Most days. It’s nice to get out and have a chat [talk]
with people.
Nurse:
What do you eat and drink now?
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
80
C3996_05.qxd 26/02/2004 13:56 Page 80
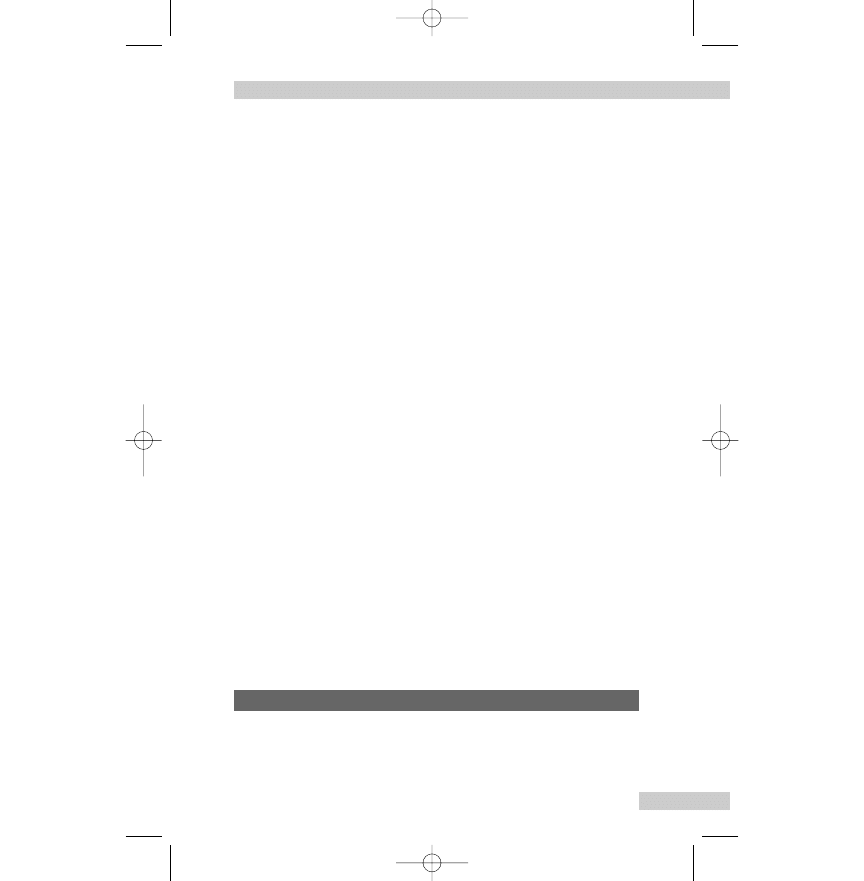
Miss H.: I know that I must eat something, so I have things
like scrambled [a cooking method] egg on toast,
soup and milky drinks. It’s not unpleasant [In English
when you have two negatives, known as a ‘double
negative’, it creates a middle way, meaning ‘not a
positive’ (‘a pleasant diet’) but not a negative (‘an
unpleasant diet’) either. So here, ‘not unpleasant’ means
a fairly acceptable diet], but I know it’s not enough.
Nurse:
Let’s see how much you weigh.What’s your normal weight?
Miss H.: Before the vomiting started I had been about 10 stone
[an Imperial Unit of weight where 1 stone = 14 pounds,
see Ch. 11] for as long as I can remember [for a long
time].
Nurse:
We use the kilogram for weight, but I can tell what it is in
stones and pounds.
Miss H.: What’s the verdict [finding] then. Have I lost much?
Nurse:
I’m afraid [The phrase ‘I’m afraid’, is used to introduce news
which is unwelcome or bad] you have lost about 11 kilo-
grams.You weigh 52 kilograms; that’s 8 stone 2 pounds, so
that’s nearly 2 stone less than usual.We will have to keep
an eye on [keep a frequent check] your weight.
Miss H.: Well, it’s no surprise my clothes are much too big.
Nurse:
I’m going to refer you to the dietician and ask her to come
and do a full nutritional assessment and see how we can
provide you with enough nutrients and fluid while we wait
for all the tests [investigations] to be done. Meanwhile, we
can order things like scrambled eggs, and give you soup and
drinks with added nutrients [fortified] if you’re sure that
won’t make you sick.
Miss H.: I’m sure that will be fine, thank you.
Mr Wakefield is a farmer. His son Tom also works on the farm
and lives with his wife and two children in the main farmhouse.
Mr Wakefield moved to a smaller house on the farm when his
COMMUNICATION IN NURSING
81
Case history – Mr Wakefield
C3996_05.qxd 26/02/2004 13:56 Page 81
wife died about 6 months ago. The last 6 months have been very
difficult for Mr Wakefield, and he has come into the health cen-
tre to see the practice nurse about feeling generally unwell.
Nurse:
Hello Mr Wakefield. How are you today?
Mr W.: Not up to much [a term used to describe feeling
generally unwell or having a low mood]. You
know – it’s hard to feel interested in anything
these days.
Nurse:
Yes, it must be about 6 months since your wife died.
Mr W.: It will be exactly 6 months on Wednesday. Her dying
like that really hit me for six [dealt a severe blow or
disappointment]. Tom does his best, but I miss her so
much. I can’t keep on like this [can’t continue in this
condition].
Nurse:
What do you mean?
Mr W.: I can’t leave Tom to run [manage] everything, but I
feel dreadful [an emotional phrase to express feeling
very unwell].
Nurse:
In what way do you feel unwell?
Mr W.: Most of it’s my own fault. I know it’s bad for me.
Nurse:
Bad for you?
Mr W.: The evenings are so long without her [his wife] and at
first I thought a couple of drinks [meaning alcoholic
drinks] would help me unwind [relax] and get through
until bedtime.
Nurse:
Did it help?
Mr W.: Not really and I ended up having more than a couple
of drinks.
Nurse:
Many more?
Mr W.: Oh yes, most evenings I manage a bottle of wine and
some whisky, and then regret it in the morning.
Nurse:
How do you feel in the morning?
Mr W.: Headache and generally lousy [unwell]. I can’t face
breakfast and I’m often sick [vomit].
Nurse:
Do you take anything for the headache?
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
82
C3996_05.qxd 26/02/2004 13:56 Page 82
Mr W.: A couple of aspirin, but they give me terrible [severe]
indigestion.
Nurse:
You have obviously been thinking about the amount of
alcohol you drink.
Mr W.: Yes, it’s worrying me. What if I can’t stop and become
an alcoholic or something?
Nurse:
How much do you think you’re having in a week?
Mr W.: I know that there are sensible limits in units, but I
don’t know what they are.
Nurse:
Most men can safely drink 3–4 units a day without a
significant risk. A unit is 10 grams of alcohol and this is
half a pint [an Imperial measure, see Ch. 11] of standard
strength beer or one glass of wine or one pub measure of
spirits. Some stronger wines have more than 1 unit.The
recommended level is 21–28 units for a man spread over
1 week. It’s best to avoid binge drinking [uncontrolled
drinking] and keep 1 or 2 days when you don’t drink.
Mr W.: My intake is well over the sensible limit. Most nights I
probably have over 10 units. I need to do something
about it.
Nurse:
You seem to have made up your mind to reduce your
intake of alcohol. Have you thought about how you might
do this?
Mr W.: I don’t want to give up [stop] drinking completely. In
the past I enjoyed a drink in moderation and that’s
what I want to aim for. Some people say that they
never touch a drop [in this case never drink alcohol],
but that’s not for me.
Nurse:
It’s good to have a realistic goal, and drinking in moderation
may have health benefits, such as reducing heart disease.
Mr W.: All this booze [slang for alcohol] has made me put on
weight [weight increased], so it will be healthier if I cut
down [reduce] on drinking and lose weight.
Nurse:
Are evenings the only time that you have a drink?
Mr W.: Yes, when I’m on my own [alone].
Nurse:
What can you do to change the pattern?
COMMUNICATION IN NURSING
83
C3996_05.qxd 26/02/2004 13:56 Page 83
Mr W.: I used to enjoy a walk round the farm of an evening
and my grandsons keep badgering [pestering] me to
take them out.
Nurse:
Do you think that’s possible?
Mr W.: Yes, and I think it would help.
Nurse:
I would like to see how you get on [check on your
progress]. Perhaps we can make another appointment,
and while you’re here we can make you an appointment
with Doctor Welch. She can arrange for support from a
counsellor, and she might think that you would benefit
from some medication.
Mr W.: Yes, I know I need some proper help and it’s such a
relief to have told someone about my drinking. I could
never tell Tom. It would cause too much bother [upset].
ELIMINATION
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with elimina-
tion are given in Box 5.6.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
Mrs Carter has been admitted to the coronary care unit for treat-
ment of unstable angina. She has had angina for about 2 years.
During a conversation about the need to use a commode by the
bed in order to reduce exertion and hence the oxygen needed by
the heart muscle [myocardium], she tells you that she has trouble
with her waterworks [urinary tract, especially the bladder].
Nurse:
What sort of problem with your waterworks?
Mrs C.: I can’t hold on and I leak urine [incontinent of urine].
It’s so embarrassing.
Nurse:
It sounds like you have two separate problems.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
84
Case history – Mrs Carter
C3996_05.qxd 26/02/2004 13:56 Page 84
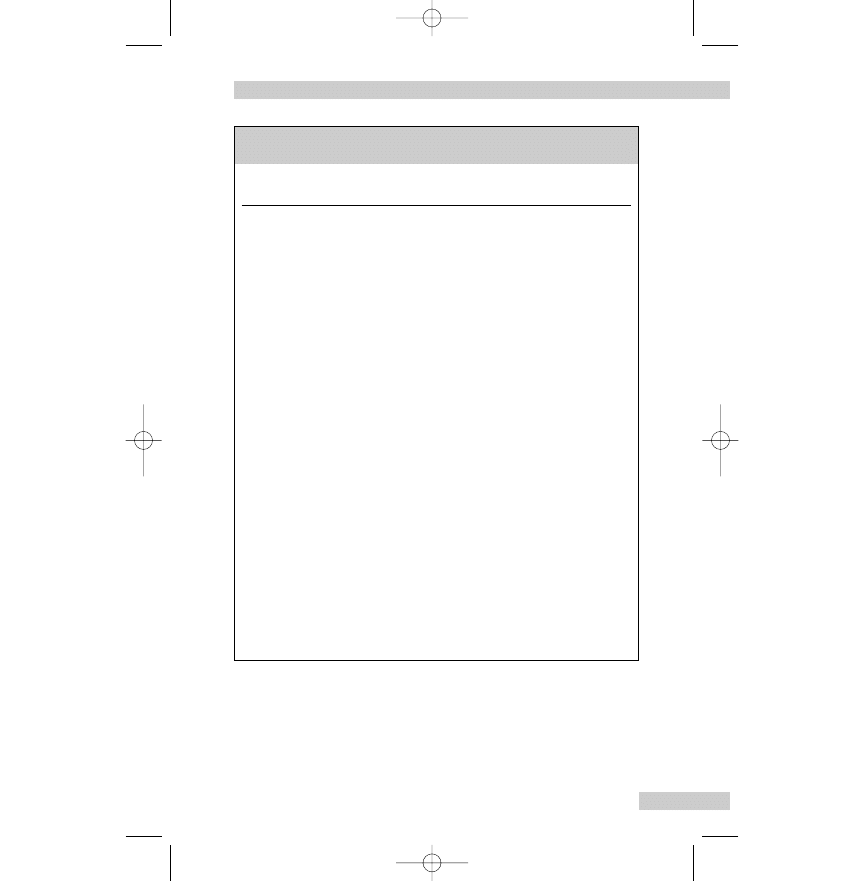
Mrs C.: I hadn’t thought of it as two problems, but it does
happen at different times. The main problem is the
need to pass water [micturate] so often and when I need
the toilet [lavatory] it is all of a rush [urgent]. Sometimes
I don’t make it in time and wet myself [incontinent of
COMMUNICATION IN NURSING
85
Box 5.6
Words associated with elimination (for further
examples see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Constipation
Bunged up; clogged up; costive; haven't been for
days; not going properly
Defaecate
Go to the toilet; have bowels open; do number
two; pass a motion or stool; to do one's
business; to have a clear out
Diarrhoea
Gippy tummy; loose motion; runs; squitters; to
be taken short; trots
Faeces; stool
Business; motion; number two; pooh
Flatulence
Belching; feel bloated; gas; wind
Incontinence
Have an accident; I leak; leaky; messed myself;
not able to hold on; wet myself
Micturition/urinate
Number one; go to the loo/toilet; pass water;
pass urine, pee; spend a penny; tiddle; wee or
wee-wee
Lavatory
Bathroom; bog; cloakroom; convenience; gents';
ladies'; latrine; lav.; little girls' room; loo; privy;
smallest room; toilet; washroom; water closet
(WC)
Urine
Pee; water
Urinary tract
Waterworks (especially the bladder)
C3996_05.qxd 26/02/2004 13:56 Page 85
urine]. The leaking happens when I cough or laugh.
Nurse:
How often do you pass water [micturate]?
Mrs C.: Every couple [two] of hours or so [approximately]
during the day.
Nurse:
What about at night, do you have to get up in the night
[to pass water]?
Mrs C.: Oh yes, I have to keep getting up [frequently get out of
bed to urinate]. Always twice a night and sometimes
more often.
Nurse:
When did you start having problems?
Mrs C.: Just after I retired. I’m 68 now, so it must be about
4 years ago.
Nurse:
Have you told your GP or the practice nurse?
Mrs C.: I felt too embarrassed and it’s something that happens
when you get older isn’t it? It really limits my social life
and it worries me that I might smell.
Nurse:
It is more common in older people, but there are different
causes and many can be successfully treated. How do you
normally cope with the problem?
Mrs C.: I try to be near a toilet, but that’s not always easy if
I’m out. There are not many public toilets and some
of them are not very clean. I wear a sanitary towel
[normally used during menstruation] in my knickers
[pants, underwear] to cope with the leaks, but I still
have plenty of washing to do [implying that this does
not always work].
Nurse:
I will add all this to your care plan and make sure that
everyone knows to bring the commode as soon as you ask.
Would you like a supply of towels and disposal bags to
keep in the locker?
Mrs C.: Yes please.
Nurse:
When your angina has settled down and you are feeling
better I will arrange for the continence nurse specialist
to come to see you. She is the expert and will be able
to do a full assessment and suggest ways of improving
the situation.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
86
C3996_05.qxd 26/02/2004 13:56 Page 86
Mrs C.: I wish I’d told someone earlier, but I thought that you
had to grin and bear it [put up with it]. I had no idea
that anything could be done.
Nurse:
While we’re waiting I’d like to have a specimen [sample] of
your water to test, and if that shows that you might have
an infection we can collect a midstream specimen of urine
for the laboratory.
Mrs C.: Is that the test where you have to pee [micturate] into
a pot?
Nurse:
Yes, that’s the one, but we only need the middle bit of the
flow, not the urine that comes out first. Have you noticed
any blood in your urine or an unusual smell?
Mrs C.: No, nothing like that.
Nurse:
What about pain when you pass urine? Does it burn or
sting?
Mrs C.: No, I had cystitis when I was younger and I know how
painful it is when you go [when she passes urine;
micturates].
Nurse:
We also need to know how often you are passing urine
and how much fluid you are having, but as we are already
recording fluid balance for you we will have that
information.
Mrs C.: You will tell the nurses about how urgent it is when I
ask for the commode?
Nurse:
Don’t worry I’m putting it on the care plan now, and I will
tell the nurse who takes over from me tonight. Do you
think you could give me that sample now?
Mrs C.: Yes.
Nurse:
Have you any questions before I go and get the commode?
Mrs C.: No, I’m looking forward to feeling better and seeing
the specialist nurse about the waterworks.
Mr Norton fractured his femur in a motorcycle accident 2 weeks
ago. The fracture is being managed with skeletal traction and
COMMUNICATION IN NURSING
87
Case history – Mr Norton
C3996_05.qxd 26/02/2004 13:56 Page 87
Mr Norton has accepted that he will be much less active than
usual and will be in hospital for some weeks. He had started to
feel better after the accident and the pain in his leg was gradual-
ly subsiding, but now he feels bloated [blown up, distended],
lethargic and has no appetite.
Mr N.:
I feel terrible [very bad], really out of sorts [unwell].
Nurse:
What’s the trouble?
Mr N.:
I haven’t been properly for days [has not defaecated
properly for days and is constipated].
Nurse:
When did you last have your bowels open [defaecate]?
Mr N.:
Saturday was OK, so that’s 4 days ago. I wish I’d said
earlier, but it seemed stupid to be worried about not
going [defaecating] when I’m laid-up [confined to bed]
with a leg that’s broke [fractured].
Nurse:
How often do you usually go?
Mr N.:
Every day without fail.
Nurse:
It’s probably happened because you’re not as active as usual
and having to use a bedpan doesn’t help.
Mr N.:
Well I can’t do much with the traction and stuff.
Nurse:
How is it making you feel?
Mr N.:
I’m all blown up and full of wind [flatulence]. Look at
my stomach [abdomen], it’s huge. I couldn’t eat nothing
and my mum [mother] had brought in a Chinese [a
takeaway meal] as a treat.
Nurse:
Yes, your abdomen is a bit distended. Have you any pain?
Mr N.:
A bit. It feels like colic [usually refers to intermittent
abdominal pain, most often from the intestine, but
sometimes from other structures].
Nurse:
What was your motion [faeces; stool] like on Saturday?
Mr N.:
Just a few hard bits and I had to strain [push hard] to
get that out.
Nurse:
What it’s like normally?
Mr N.:
Normal – soft and not having to strain. Except when
I’ve got the runs [diarrhoea] after too much beer and
a curry.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
88
C3996_05.qxd 26/02/2004 13:56 Page 88
Nurse:
Was there any pain passing the hard motion, or blood
when you cleaned yourself?
Mr N.:
No pain and I didn’t see no blood. If I had I would
have said straight away [immediately, at once].
Nurse:
Did you feel that you hadn’t passed a complete motion?
Mr N.:
Yeah [yes], my back passage [rectum] felt full just as if
there was more to come.
Nurse:
I’ll get Dr Cox to write you up for [prescribe] some
medicine [laxative] to make you go and we can ask the
physio. [short for ‘physiotherapist’] to suggest some
exercises to help.
Mr N.:
My gran [grandmother] swears by [relies on] her bottle
of bowel medicine.
Nurse:
You might need some suppositories or a micro enema to
get things started and then a few doses of an oral laxative.
Hopefully you won’t need a whole bottle. It will also help if
you can drink more water and choose food high in fibre
from the menu.
Mr N.:
Yeah alright, but I don’t want salad every meal.
PERSONAL CARE – CLEANSING AND DRESSING,
SKIN CARE
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with personal
care are given in Box 5.7.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
Mrs McBride lives alone, and Sue her daughter-in-law [the wife of
Mrs McBride’s son] pops in [visits] most days to take her a meal
and check that she is all right. Recently, Sue has noticed that Mrs
McBride is increasingly frail and takes a long time to answer the
door or make a drink.
COMMUNICATION IN NURSING
89
Case history – Mrs McBride
C3996_05.qxd 26/02/2004 13:56 Page 89
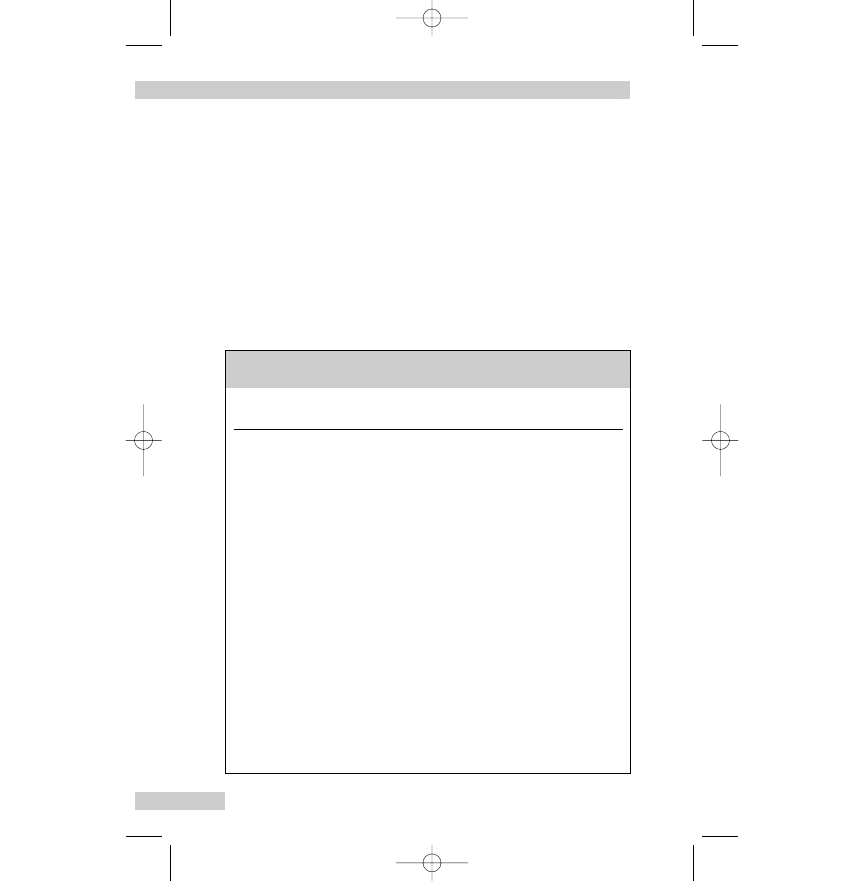
Nurse:
Hello Mrs McBride. I’m Nurse Ramos. I think you are
expecting me. I’ve come in to see how you are managing
at home.
Mrs M.: Hello dear [an endearment often used by older people]
come in. Yes, I knew you were coming. Sue mentioned
it earlier when she was in with my lunch [meal in the
middle of the day]. She’s a good girl to me.
Nurse:
I’ve got a checklist to complete, but it’s usually better if
you tell me in your own words how you think you are
managing.What about if we start with any difficulties you
might be having with washing and dressing?
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
90
Box 5.7
Words associated with personal care (for further
examples see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Bath/bathe
Have a soak; scrub down
Contusion
Bruise
Dandruff
Scurf
Emollient
Moisturiser
Erythema
Redness
Excoriation
Soreness
Halitosis
Bad breath; mouth odour
Oral hygiene
Brush/clean teeth; mouth wash
Pressure ulcer
Bedsore; pressure sore
Pruritus
Itching (intense)
Rash
Spots/spotty
Wash
Hair wash; hands and face wash; strip wash;
wash at the sink/basin
C3996_05.qxd 26/02/2004 13:56 Page 90
Mrs M.: Yes, that’s fine. I’ve always been as fit as a fiddle [in
very good health], but since the winter it’s got more
and more difficult. Well I am 83. It’s all down to [as a
result of] old age I suppose.
Nurse:
What’s more difficult?
Mrs M.: I struggle a bit with a strip wash [wash all over] at the
sink, but I get by [cope]. My feet and back don’t get
done, and it’s hard to stand up to wash down below
[genital and perianal area]. I need to hold on to the
sink and then I can’t soap the flannel.
Nurse:
Are you able to have a bath or shower?
Mrs M.: No, I’m not strong enough to get in and out of the
bath. I’m frightened of slipping, or getting in and not
getting out again.
Nurse:
How often did you have a bath when you were able to
manage?
Mrs M.: Two or three times a week. Heating the water with
the immersion heater costs too much to have a bath
every day.
Nurse:
How do you heat the water for your strip wash?
Mrs M.: Boil a kettle; I’ve got one in the bedroom for a cuppa
[usually refers to a cup of tea] in the morning. Would
you like a cup of tea now?
Nurse:
No thanks I had one [cup of tea] just before I came out to
see you.Would you like to have a bath if it was possible?
Mrs M.: Oh yes, there’s nothing like a soak in the bath for
getting clean and relaxing you.
Nurse:
I quite agree. Is there anyone who could help you?
Mrs M.: I can’t ask Sue. She has three children to get off to
school, and I don’t want to sit in my dressing gown
until she can get here.
Nurse:
Would you consider having a bath seat that lowers you into
the bath and then goes up when you’re ready to get out?
Mrs M.: I’m hopeless with machines. How easy are they to use?
Nurse:
Very easy.You have a button to push that lowers and raises
the seat. If you like we can arrange for someone from
COMMUNICATION IN NURSING
91
C3996_05.qxd 26/02/2004 13:56 Page 91
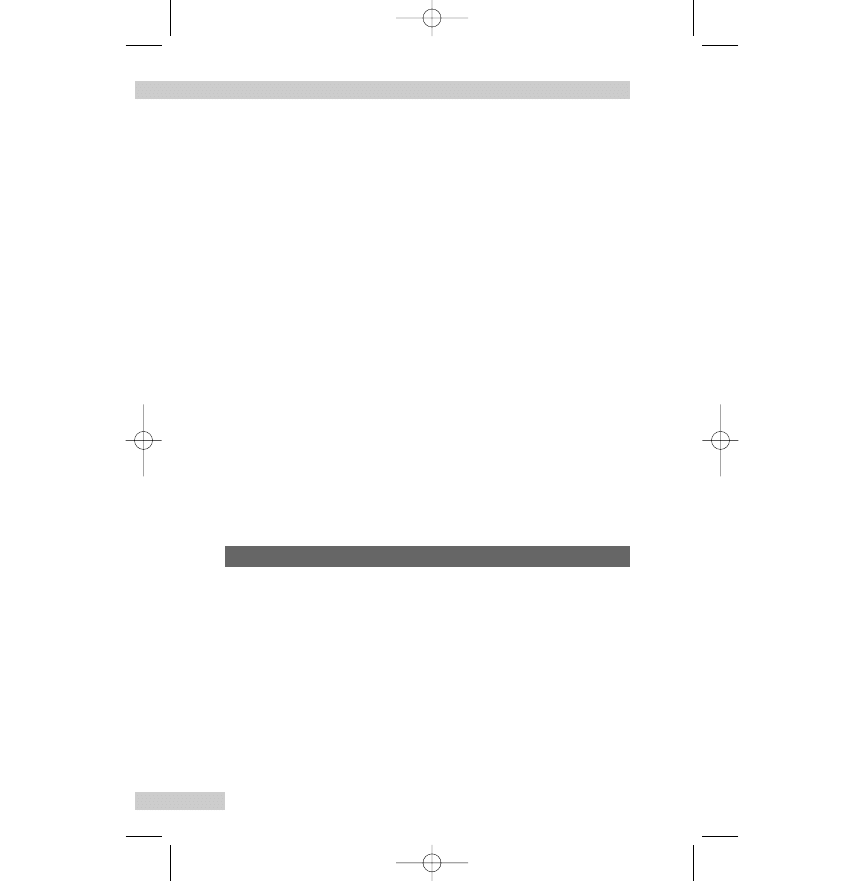
Social Services to come out and do an assessment.What
about washing your hair?
Mrs M.: That’s no problem. I can do it at the sink. My
neighbour used to be a hairdresser and she comes
in every few weeks and gives it a cut and set.
Nurse:
That’s handy [convenient].
Mrs M.: It certainly is. I can’t get down the town these days
unless Sue takes me. I haven’t been shopping on my
own for ages [for a long time].
Nurse:
Do you have any problems getting dressed and undressed?
Mrs M.: Some things take for ever [a long time], like putting on
tights or trousers.
Nurse:
What about doing things up – buttons and zips, etc.?
Mrs M.: I make sure that clothes do up at the front – no good
struggling with a zip at the back of a dress.
Nurse:
The occupational therapist can suggest some simple
gadgets [appliances, devices] to help with dressing and
show you about easier ways of doing things.Would you
like me to arrange for her to come?
Mrs M.: Yes please. Another neighbour, Mrs Smith at number 80
[the house number], had a visit from one of them and
she got on very well.
Mr Dafnis is going to have planned [elective] surgery. He has a
long history of eczema, with dry, itchy skin. When he attends the
pre-admission assessment clinic he expresses some concern
about the care of his skin condition while he is in the ward after
the major surgical operation.
Mr D.:
I’m worried about my eczema when I come into
hospital. It’s important to follow my usual routine or
it will flare up [get worse] again.
Nurse:
How long have you had eczema?
Mr D.:
For years, it’s chronic now but some things make it
worse.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
92
Case history – Mr Dafnis
C3996_05.qxd 26/02/2004 13:56 Page 92
Nurse:
What sort of things?
Mr D.:
In my case it’s things like getting too hot, such as from
the sun shining through a window.
Nurse:
We can arrange for you to have a bed well away from any
windows. Is there anything else?
Mr D.:
Alcohol starts up the itching [pruritus], but I never
touch it [does not drink alcohol] nowadays.
Nurse:
What’s your skin like now?
Mr D.:
Not very good. It’s very red [erythema] and the itching
and scratching is much worse. I put it down to [caused
by] the stress of having to have the op. [short for
‘operation’].
Nurse:
Which areas are worse affected?
Mr D.:
Mainly my face, as you can see, and my back is
very itchy.
Nurse:
Have you any sore areas [excoriation] or weeping
[producing exudate] areas?
Mr D.:
No, my skin is just dry and very itchy. Any vesicles
and broken areas would mean I was open to infection.
Is that why you’re asking?
Nurse:
Yes, exactly. But to be on the safe side I’ll get the doctor to
have a look now.What measures are you taking to reduce
the flare up?
Mr D.:
I never use soap because it takes out my natural skin
oils, so I use soap substitute, and at the moment I’m
using an oily moisturiser [emollient] nearly every hour,
but touch wood [a reference to the habit of touching
something wooden to avert bad luck] it won’t be so
bad by the time I come into the ward.
Nurse:
Are you using anything other than the emollient on your skin?
Mr D.:
No.
Nurse:
Have you used steroid ointments lately?
Mr D.:
No, not for months. I only have them as a last resort.
Nurse:
What about other medicines?
Mr D.:
I’m taking an antihistamine so the scratching is reduced
and I can get some sleep.
COMMUNICATION IN NURSING
93
C3996_05.qxd 26/02/2004 13:56 Page 93
Nurse:
I’ll make sure that your skin management is written in the
care plan. Have you any questions?
Mr D.:
What if my eczema gets really bad before I’m due to
come in?
Nurse:
If it gets any worse please let us know. I’ll be giving you
some printed information with the unit telephone number
in any case.
Mr D.:
OK, thanks.
SLEEPING
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with sleeping
are given in Box 5.8.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
Mrs Bell moved into the care home from sheltered housing [hous-
ing with communal areas and a warden] 5 days ago. She had
enjoyed her time there, but after the fall and the fractured hip she
felt that she needed more care. Although there was a button to
press to get help, she was frightened of falling again and having
to wait for help to come. Both her sons were concerned about
her and going into the home seemed the most sensible thing to
do. She hadn’t expected to feel at home straight away, but she is
missing her friends and is not sleeping well.
Nurse:
Good morning Mrs Bell how are you settling in?
Mrs B.: Not too bad I suppose, but it feels a bit strange still.
Nurse:
I thought it would be helpful for us to have a chat now
that you have been here for a few days.You said that it
feels strange.
Mrs B.: I’m not complaining and everyone is so kind, but I
miss the ladies from the sheltered housing.
Nurse:
Have any of them visited you yet?
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
94
Case history – Mrs Bell
C3996_05.qxd 26/02/2004 13:56 Page 94
Mrs B.: The warden came yesterday and it was nice to hear all
the gossip. My special friends are away on their hols
[holiday] until next week, so I expect they will be
round then.
Nurse:
That’s good.What about your sons?
Mrs B.: John brought me in, and he came yesterday on his way
home from work. Nigel works away during the week,
but he will be in on Saturday.
Nurse:
Have you got to know the other residents yet?
Mrs B.: I had tea [a light meal in the afternoon or evening]
with Mrs Forbes and she was very friendly.
Nurse:
How are you sleeping?
Mrs B.: Not very well, I’m awake half the night.
COMMUNICATION IN NURSING
95
Box 5.8
Words associated with sleeping (for further examples
see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Bruxism
Grind my teeth during sleep
Go to bed/sleep
Hit the hay/sack; retire for the night;
say goodnight; turn in
Insomnia
Awake half the night; can't get off (to sleep);
sleeplessness; wakefulness; wide awake
Narcolepsy
Drop off without warning
Sleep
Catnap; doze/dozing off; drop off; forty winks;
kip; lose myself; nap; siesta; shut eye; snooze
Sleep hygiene
Bed time or pre-sleep routine/rituals
Somnambulance
Sleep walking
Somnolent
Dozy; drowsy; heavy-eyed; nodding off; sleepy
Weary
Dead beat; dog-tired; done in; ready to drop;
whacked
C3996_05.qxd 26/02/2004 13:56 Page 95
Nurse:
Is that usual for you?
Mrs B.: Not really. I used to have the odd [in this context
means ‘infrequent’ or ‘unusual’] night when I would
wake up, but most nights I would sleep right through
until about half past six [6.30 a.m.].
Nurse:
Do you have trouble falling asleep [going to sleep] or do
you wake up in the night?
Mrs B.: I’m really tired, but as soon as I put the light out I’m
wide awake again.
Nurse:
Do you get to sleep eventually?
Mrs B.: Yes, but then I wake up feeling whacked [weary] and
groggy [unwell]. I don’t feel rested.
Nurse:
Do you wake up earlier than usual?
Mrs B.: I did this morning. There was a lot of coming and
going [activity] because the lady in the next room was
poorly [unwell].
Nurse:
Yes, she had to go into hospital.
Mrs B.: And I’m so tired in the day I keep dozing off [going to
sleep] in the chair.
Nurse:
Did you usually have a short nap [sleep] during the day
before you came to us?
Mrs B.: Well, if I’m honest, I did sometimes put my feet up
[relax] after the lunchtime Archers [a long-running
radio programme] and lose myself for a bit [have a
short sleep].
Nurse:
What time have you been falling asleep in the chair?
Mrs B.: After supper [last meal of the day], so when I come to
[wake up] it’s time to start thinking about going to bed.
That’s a bit late for a nap I know.
Nurse:
Do you have a bedtime routine – things that help you get
to sleep?
Mrs B.: I used to have a bath last thing [just before going to
bed] and take a milky drink to bed. Then read until I
felt drowsy [somnolent].
Nurse:
What sort of time [approximate timing] would you usually
have the bath?
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
96
C3996_05.qxd 26/02/2004 13:56 Page 96
Mrs B.: After the news at ten [10 p.m.] and be in bed by 11
[11 p.m.]. I’m not sure if it’s all right to have a bath that
late here. I expect the girls [night staff] are too busy to
help with baths.
Nurse:
I will have a word [discuss it] with the nurse in charge
tonight about making sure you can have a bath if you want,
and get a milky drink. It is so important to get a good
night’s sleep.
Mrs B.: You can say that again [emphasises the importance of
the nurse’s last statement]. I would be very grateful if
they could help me with a bath.
Nurse:
Is there anything else that can be done to help you sleep
properly?
Mrs B.: It is quite warm in my room. I’m not used to having
the radiator so hot in the bedroom.
Nurse:
We can turn the thermostat down, so it just takes the chill
off the room [make sure that the room is not cold].
Mrs B.: They tried last night, but it was too stiff to turn.
Nurse:
I’ll get on to [contact] the maintenance staff right away
[at once].
Mrs B.: It was so hot I pushed the duvet off me. I haven’t done
that since the change [climacteric/menopause] when I
used to have night sweats.
Nurse:
What about when you get up in the morning, will you be
warm enough?
Mrs B.: Oh yes, my boys [her sons] treated me to [paid for]
some new clothes to come in here and that included
a fleecy dressing gown. Look it’s on the chair. Do you
think it’s too bright?
Nurse:
I like that dark pink. It’s such a warm colour.
Mrs B.: Yes, I like it. I did wonder about pink at my age, but
then I thought ‘Why not?’.
Nurse:
Is there anything else that stops you sleeping?
Mrs B.: I still need to get used to [become accustomed to] the
light coming in from the corridor.
Nurse:
Were you used to sleeping in complete darkness?
COMMUNICATION IN NURSING
97
C3996_05.qxd 26/02/2004 13:56 Page 97
Mrs B.: Yes, the sheltered housing is on the edge of the village,
right out in the sticks [rural location, in the
countryside].
Nurse:
We need to keep the light on in the corridor, so that
everyone can move about safely.
Mrs B.: Yes, I know. I don’t suppose it will bother [trouble] me
for long.
WORKING AND PLAYING
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with working
and playing are given in Box 5.9.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
Mr Khan is about to be discharged home after having a myocar-
dial infarction a week ago. He normally helps to run the family
business and needs to drive all over the UK to see customers. He
is anxious about how a recent myocardial infarction will affect his
driving, the business and his leisure activities.
Mr K.:
Nurse Brown, have you got a minute [the time] to talk?
Nurse:
I need to give a painkiller to another patient. I’ll be back in
5 minutes.
Mr K.:
OK.
Nurse:
Right, Mr Khan I’m back.What would you like to talk about?
Mr K.:
I’m really worried about how I’ll manage to run my
part of the business after the heart attack [myocardial
infarction].
Nurse:
Did you speak to the cardiac nurse specialist?
Mr K.:
Yes, on Tuesday. She explained everything and I asked
lots of questions. It all seemed quite straightforward
[easy, simple], but now that I’m dressed and ready to
go home I’m not so sure.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
98
Case history – Mr Khan
C3996_05.qxd 26/02/2004 13:56 Page 98

Nurse:
Did she leave the printed information?
Mr K.:
Yes.
Nurse:
What bits are worrying you?
Mr K.:
Well, mainly the driving and getting back to work. I
drive about 20 000 miles a year on business. There is
something in the leaflet about driving, but I’m worried
that Swansea [the location of the Driver and Vehicle
COMMUNICATION IN NURSING
99
Box 5.9
Words associated with working and playing (for fur-
ther examples see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Dismissed
Fired; given my cards; given the boot; given my
notice; given the push; got the sack; laid off; let
go; marching orders; sacked; sent packing
Employed
Hired; in a job; in work; paid work; working
Employee
Bread-winner; wage-earner; worker
Employer
Boss; gaffer; governor
Leisure/leisure activities
Amusement; breathing space; free time; fun;
hobby; pastime; play; pleasure; recreation; R&R;
spare time; time off
Occupation; profession
Business; career; calling (outdated); craft; job;
line of work; livelihood; position; trade; walk of
life; work
Relaxation
Chill out; laze about; let one's hair down;
loosen up; put one's feet up; take it easy; unwind
Retired
Given up work; pensioner; pensioned off;
put out to grass
Self-employed
Freelance; my own boss; work for myself
Unemployed
Jobless; looking for a job/work; not working; on
the dole/social; out of work
C3996_05.qxd 26/02/2004 13:56 Page 99
Licensing Agency (DVLA); the word ‘Swansea’ may be
used to describe it in conversation] will take my
licence away.
Nurse:
Is yours an ordinary licence?
Mr K.:
I should think so.
Nurse:
You don’t drive a bus or a lorry do you?
Mr K.:
No, just the car and sometimes the minibus for the
Community Centre.
Nurse:
You will need to stop driving for at least 4 weeks and you
don’t have to notify DVLA.You have an appointment to see
Dr Bradley [the cardiologist] next month. He will advise
you about when you can start driving again.
Mr K.:
I hope it’s not much longer than 4 weeks. My dad
[father] and brother can visit the customers for a few
weeks, but not for ever.
Nurse:
So far your recovery has gone well.There’s no reason to
think you won’t be fit [well enough] to drive in a month. It
might be a good idea to tell your insurance company about
the heart attack.
Mr K.:
Yes, that’s sensible. I don’t want to drive without
insurance. That means a fine and six points on your
licence.
Nurse:
You mentioned getting back to work.
Mr K.:
We run a small family business, so one person off sick
puts a real strain on everyone else.
Nurse:
Yes, I can see that. Do you do most of the customer
visiting?
Mr K.:
Yes, my dad doesn’t really like driving long distances
and my brother is better at the day-to-day business.
Nurse:
Again Dr Bradley will advise you about going back to work,
but most people gradually increase their activity and are
back at work in 4–6 weeks. It would be longer if you had a
job with a lot of physical activity.
Mr K.:
No, if I’m in the office it’s mainly computer work and
telephoning customers. My job isn’t very active, but I’m
keen on sport.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
100
C3996_05.qxd 26/02/2004 13:56 Page 100
Nurse:
What sport do you do?
Mr K.:
I play some cricket and coach some lads [boys,
youngsters] in a local football team.
Nurse:
How active is the coaching?
Mr K.:
Well I work-out [train] with the boys. I’m keen to keep
on [continue] with both the cricket and the coaching.
Nurse:
The staff running [organising] the formal sessions of the
cardiac rehabilitation programme will be able to give you
information about safe levels of exercise and playing sport.
When do you start?
Mr K.:
The specialist nurse said that she will give me a ring
[telephone] next week to see how we’re getting on
[coping] at home and by then she will know the dates
for the exercise sessions.
Nurse:
Don’t forget the cardiac nurses have a telephone helpline if
you have any worries once you get home, and you can also
use their e-mail.
Mr K.:
Yes, it’s very reassuring to know that there is some
back-up [support].
Nurse:
Have you any questions about your drugs and the dietary
changes, or anything else?
Mr K.:
No, that’s all the worries for now. I just needed to get
those things straight [sorted] in my mind.
Mrs Hamilton has had diabetes for many years and her vision is
deteriorating due to diabetic retinopathy. She and her husband
are both retired and enjoy walking and gardening.
Nurse:
Hello Mrs Hamilton. It doesn’t seem like a year since we
last saw you.
Mrs H.: Yes, time for the annual eye check again.
Nurse:
Not everyone is so reliable about attending as you.
Mrs H.: I’d be daft [foolish, unwise] not to. Finding problems
early is so important. My sight is already bad, I don’t
want it to get any worse.
COMMUNICATION IN NURSING
101
Case history – Mrs Hamilton
C3996_05.qxd 26/02/2004 13:56 Page 101
Nurse:
I will be putting the eye drops in to dilate your pupil, so we
can examine the back of your eye [retina]. How has your
sight been since last year’s check?
Mrs H.: I’m finding it more difficult to read small print and
I’ve got patchy [uneven] blurring of vision. It does
make life difficult.
Nurse:
How does it affect you on a day-to-day basis?
Mrs H.: Now Jim [her husband] and I have given up working
[retired] we have time to do our garden. I have always
had green fingers [keen gardener] and we like walking
in the countryside, but it’s not much fun with my poor
vision. I have to rely on Jim to read the labels on weed
killer for the garden and the plant labels at the garden
centre. He doesn’t mind, but I mind very much. I feel
so helpless and frustrated about losing my
independence.
Nurse:
Yes, it must be frustrating.
Mrs H.: I’m really cheesed off [fed up]. It’s reading books as
well. I like to relax with a book after supper [last meal
of the day] while Jim has a pint [in this context it
means beer] at our local [nearest public house]. But
now I can only see if the print is very large and every
light in the room is on. It’s not very relaxing.
Nurse:
No, it doesn’t sound very relaxing. Have you got any low
vision aids?
Mrs H.: I’ve got my glasses [spectacles] and a magnifier and I
make sure that the lighting is right for what I’m doing.
Nurse:
How is your diabetic control?
Mrs H.: OK. I’m doing quite well with the sugar control and the
insulin injections are no problem now I use a preloaded
insulin pen [device for injecting insulin].
Nurse:
I’m sure you know how important this is to help stop the
retinopathy from getting worse.
Mrs H.: Oh yes, the diabetic nurse specialists are always harping
on about [emphasising] the importance of managing the
diabetes properly.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
102
C3996_05.qxd 26/02/2004 13:56 Page 102
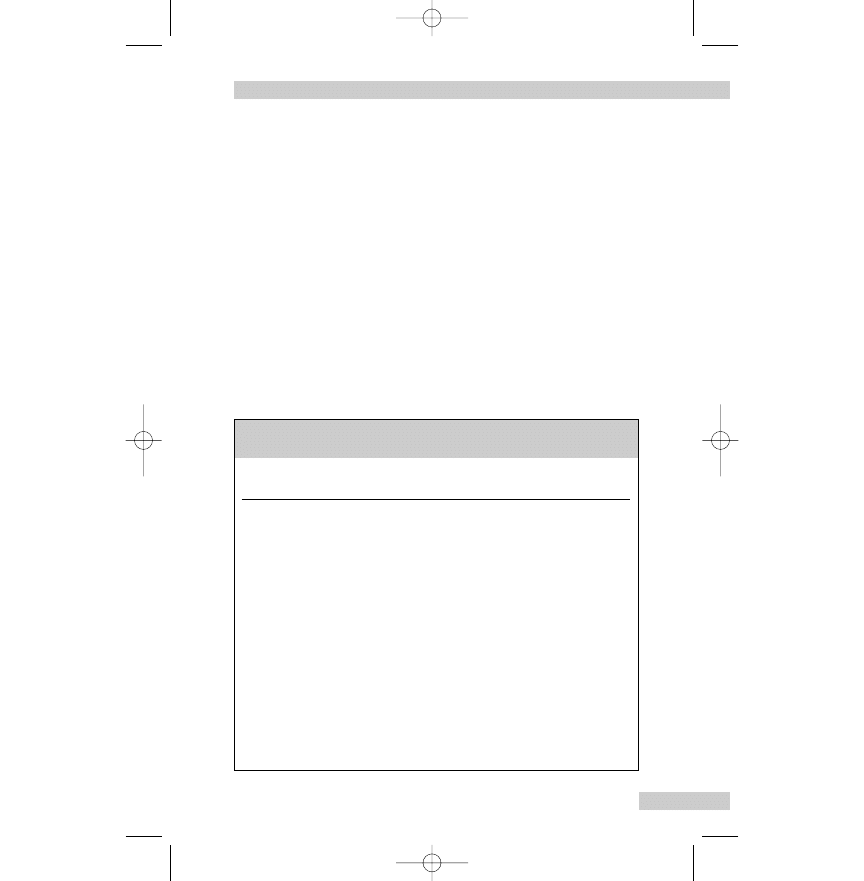
Nurse:
We all nag [keep on at] you, don’t we?
Mrs H.: I don’t mind. But just think, if I hadn’t gone after
[applied for] the area manager post [job] and had to
have a medical [routine health check] it might have
been ages [long time] before they found the diabetes
and I started the insulin and a proper diet.
SEXUALITY
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with sexuality
are given in Box 5.10.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
COMMUNICATION IN NURSING
103
Box 5.10
Words associated with sexuality (for further exam-
ples see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Cervix
Neck of womb
Dysmenorrhoea
Painful periods
Erectile dysfunction
Impotent
Genitalia
Bits; down below; down there, naughty bits;
private parts; privates
Menorrhagia
Flooding; heavy periods
Menstruation
Being unwell; having the curse, period(s)
Sexual intercourse
Go to bed with; intimacy; lovemaking;
make love; sex; sexual relations; sleep with;
to do/have it
Uterus
Womb
C3996_05.qxd 26/02/2004 13:56 Page 103
Mr Johns has been a widower [a man whose wife has died and
has not remarried] for many years. He is generally fit [in good
health], apart from hypertension which is treated with enalapril
maleate.
Mr J.:
I’ve been under the doctor [in the doctor’s care, being
treated] for my blood pressure. She said to make an
appointment for you to check me over and do the
blood pressure.
Nurse:
What has the doctor prescribed?
Mr J.:
Innovace [proprietary name for enalapril maleate].
Nurse:
How have you been?
Mr J.:
Not bad [In English, when you have two negatives,
known as a ‘double negative’, it creates a middle way,
meaning not a positive (‘very good’), but not a negative
(‘very bad’) either].
Nurse:
What, not feeling really well?
Mr J.:
A bit seedy [unwell], but nothing specific.
Nurse:
Is there anything worrying you?
Mr J.:
I’ve met a nice lady, we really hit it off [get on well].
She likes all the same things as me, music, food and
everything.
Nurse:
Had you been on your own for long?
Mr J.:
A long time. Jenny [his wife] died of cancer 10 years
ago. I didn’t want anyone else at first, but when the
kids [children] married and moved away I felt a bit
lonely and that.
Nurse:
Yes.
Mr J.:
I met someone at work, but that soon fizzled out [came
to nothing].
Nurse:
Some men can have difficulty with erections when
taking the medicine you are on. Have you had any
trouble?
Mr J.:
It’s difficult to talk about it, but I was impotent [had
erectile dysfunction] and couldn’t do it [have sexual
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
104
Case history – Mr Johns
C3996_05.qxd 26/02/2004 13:56 Page 104
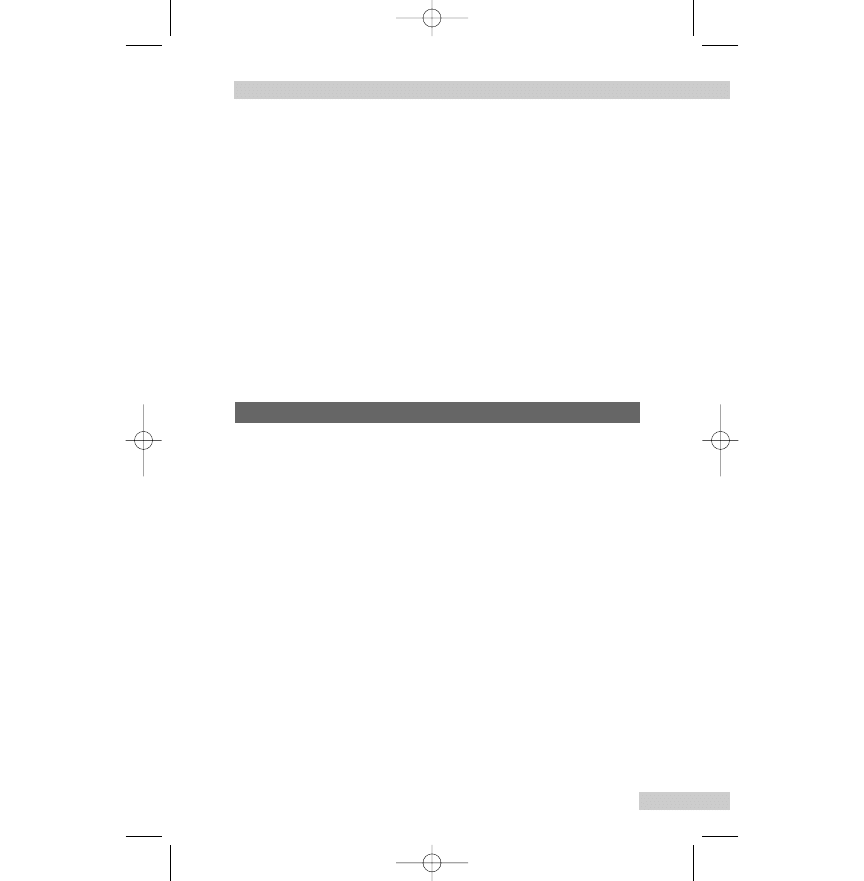
intercourse]. I told myself it was just nerves being with
someone new and tiredness.
Nurse:
Yes, it’s difficult to talk about intimate things.
Mr J.:
I’m worried about my new relationship. I don’t want
anything to go wrong like last time.
Nurse:
We’re lucky in this area to have a nurse who specialises in
the management of erectile dysfunction, that’s the medical
term for problems with erections.Would you like me to
arrange an assessment appointment with him?
Mr J.:
Yes please, I need to talk to someone. When the
doctor gave me the script [short for prescription] she
said one of the side-effects was trouble with erections,
but how could I ask her any questions? It was so
embarrassing.
Problems with menstruation have been part of Mrs Hall’s life for
as long as she can remember. First it was dysmenorrhoea as a
teenager and into her 20s, and now 20 years later she has men-
orrhagia and the dysmenorrhoea is back. She has seen the con-
sultant and the plan is for her to come in as a day case for a hys-
teroscopy and endometrial biopsy.
Nurse:
Hello again Mrs Hall. I’ve come to answer any questions
you might have about having the examination as a day case.
Mrs H.: You and the consultant explained that he would look
inside the womb [uterus] with a special instrument and
then do a scrape [dilatation and curettage] to get a sam-
ple for testing, so I’m fairly clear about what will
happen.
Nurse:
Have you any questions about the possible complications of
the procedure?
Mrs H.: No, I’m fully aware that there is a risk of the womb
being perforated.
Nurse:
You signed your consent form and consented to a general
anaesthetic.
COMMUNICATION IN NURSING
105
Case history – Mrs Hall
C3996_05.qxd 26/02/2004 13:56 Page 105
Mrs H.: I didn’t fancy [like the idea of] having it done in
outpatients, I’d rather be put to sleep [anaesthetised]
first.
Nurse:
It will only be a short anaesthetic.You should be able to go
home later that afternoon/evening.Will your partner be
collecting you?
Mrs H.: Yes, he’ll come straight from work. His shift finishes at
3 o’clock, so it will be about 4 [4.00 p.m.]. Is that OK?
Nurse:
No problem, but he should ring [telephone] first just to see
if you are recovered enough to go home.You might still be
a bit sleepy.
Mrs H.: Mr Bainbridge said you could give me a date for the
examination.
Nurse:
Yes, I’ll get the dates up on the computer, but first I need to
check a few things with you.
Mrs H.: OK.
Nurse:
We do the examinations on a Wednesday morning. Are
there any dates that we need to avoid?
Mrs H.: No, we’re not going away [in this context means
away on holiday] until the problems with my periods
[menstruation] have been sorted out.
Nurse:
We will need to avoid dates when you have your period, as
it makes it difficult to get a good view of the inside of the
womb. Are your periods regular?
Mrs H.: Fairly. It usually comes every 30 days or so. The real
problem is that it lasts much longer.
Nurse:
How long?
Mrs H.: The last 3 months have been dreadful, with the heavy
bleeding going on for 7 or 8 days.
Nurse:
Does that make things difficult for you?
Mrs H.: Yes, very difficult, because I keep flooding [excessive
bleeding from the uterus]. Sometimes the blood
comes through the pad and my clothes, so I’m
scared [frightened] to go out. Plus I’m forever
washing clothes and the bedding.
Nurse:
It sounds as if your daily activities are seriously affected.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
106
C3996_05.qxd 26/02/2004 13:56 Page 106
Mrs H.: Yes, they are. I can’t plan to do anything for a whole
week every month.
Nurse:
Do you have any spotting [intermenstrual bleeding], such as
after having sexual intercourse?
Mrs H.: No, only the heavy bleeding [menorrhagia] and flooding
during my period. But it’s affecting our sex life; either
I’m bleeding or too tired.
Nurse:
The blood test we took will show if you are anaemic.
Heavy periods often cause anaemia and that would make
you tired.
Mrs H.: I really want the bleeding sorted. It’s really dragging
me down [making me ill, emotionally and physically].
Nurse:
The examination will help to find a physical cause, but
as you know Mr Bainbridge thinks that you may have
dysfunctional uterine bleeding and he might not find a
physical cause.
Mrs H.: I’m in agony [in extreme pain] with period pains
[dysmenorrhoea] as well. I used to have pain with
my periods when I was young, but this pain is
much worse.
Nurse:
What do you take for it?
Mrs H.: Just paracetamol, but they don’t do much good [not
very effective]. I know I said that I want it sorted, but
I’m worried in case he says I need a hysterectomy.
Nurse:
There are several different treatments for heavy bleeding,
such as tablets, hormones and a fairly new technique called
ablation, where the lining of the womb is removed.There is
lots to try before hysterectomy needs to be considered.
Mrs H.: I do hope so. You hear about women having a hys-
terectomy and never really getting over it [recovering],
plus all those things that happen to you.
Nurse:
What sort of things?
Mrs H.: Well you put on weight.
Nurse:
There is no reason for anyone to put on weight after a
hysterectomy other than the usual reasons of eating too
much and not getting enough exercise.
COMMUNICATION IN NURSING
107
C3996_05.qxd 26/02/2004 13:56 Page 107
Mrs H.: It wouldn’t feel right somehow.
Nurse:
In what way?
Mrs H.: You know – not feeling like a proper woman.
Nurse:
If Mr Bainbridge advised a hysterectomy and you were
considering it, the usual thing would be for you to see one
of us specialist nurses again to have a proper discussion
about the operation before it went ahead. But we could
talk it through [discuss fully] now if you would like to.
Mrs H.: Yes please, if you’ve got time now.
ANXIETY, STRESS AND DEPRESSION
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with anxiety,
stress and depression are given in Box 5.11.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
108
Box 5.11
Words associated with anxiety, stress and depression
(for further examples see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Anxious
Jumpy; nervy; wired (often used in connection
with substance misuse)
Depressed
Down in the dumps/mouth; feeling down; got
the hump; hacked or naffed off (also means
annoyed); low (Note: Many of these expressions
describe mild mood change rather than a
depressive illness)
Mental health problem
Barmy; batty; bonkers; cracked/crackers; crazy;
cuckoo; loony; loopy; mad; mental; nuts/nutty;
off one's chump/head/rocker/trolley; out of
one's mind; round the bend; screw loose;
screwy
Stressed
Strung out; up tight
C3996_05.qxd 26/02/2004 13:56 Page 108
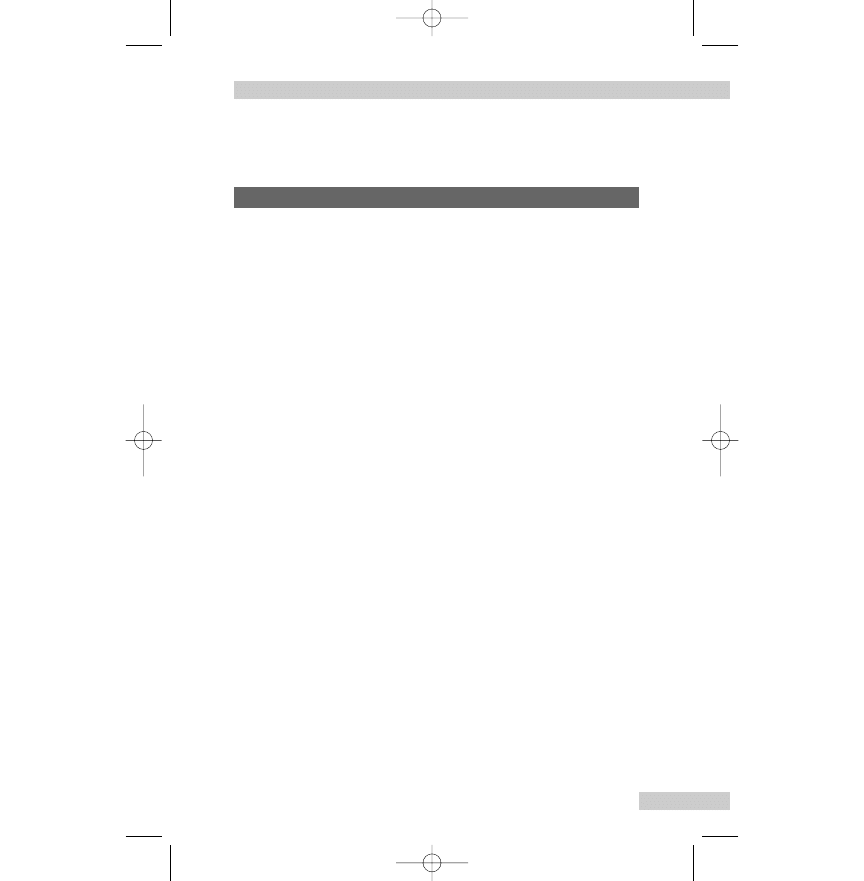
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
Mr Reeves has always worried about things at work and often
becomes anxious if he can’t clear his desk each day. Recently, he
doesn’t seem to be able to concentrate properly and has been
staying late at work to get the day’s jobs finished. He has started
to feel anxious about returning to work after the weekend, and
on two occasions he has had a panic attack during the bus ride
to work on a Monday morning.
Nurse:
Hello Mr Reeves. I’m Nurse Owen. Is it all right if I ask you
some questions?
Mr R.:
Yes.
Nurse:
I understand that you have had some panic attacks.
Mr R.:
Yes, when I had to go back to work after the weekend.
Nurse:
Tell me what happened.
Mr R.:
It came out of the blue [suddenly, without warning].
I felt uneasy and came over [felt] all sweaty, my heart
was pounding [palpitations] and my chest felt like it
would burst. I thought I was about to snuff it [die].
Nurse:
What did you do?
Mr R.:
I tried to calm down and take some big breaths, but it
didn’t work [not effective] and I had to get off the bus
in a hurry and pushed my way off. People must have
thought I was round the bend [have a mental health
problem].
Nurse:
Did you get to work in the end?
Mr R.:
No, I needed to get home.
Nurse:
Were things any better once you got home?
Mr R.:
The panic had gone, but I felt edgy [nervous, irritable].
Nurse:
How do you mean?
Mr R.:
I couldn’t settle to anything [moved from task to task]
and was fidgety [nervously touching or playing with
things] all day.
COMMUNICATION IN NURSING
109
Case history – Mr Reeves
C3996_05.qxd 26/02/2004 13:56 Page 109
Nurse:
Tell me about your job.
Mr R.:
I work for an insurance company in the claims
department.
Nurse:
What does that involve?
Mr R.:
I deal with claims from clients. It’s mainly people
damaging things at home or perhaps they have had a
break-in [burglary]. It must be dreadful and I worry
about getting the claims agreed quickly if someone has
had a break-in.
Nurse:
Do your managers put pressure on you to complete claims
within a set time?
Mr R.:
Yes, it’s all about targets and outcomes, but you must
know. It’s like that in the NHS these days.
Nurse:
Yes, most people seem to have pressures at work.
Mr R.:
It started when I wanted be the quickest to get claims
sorted out.
Nurse:
What happened?
Mr R.:
I was working against the clock [pushed for time] and
I managed for a while, but then I felt that I must
complete everything the same day.
Nurse:
Was that realistic?
Mr R.:
No, but I couldn’t see that. I stayed most evenings, but
seemed to get less and less done.
Nurse:
Why do you think that happened?
Mr R.:
I couldn’t concentrate and went from job to job without
finishing it. I couldn’t deal with claims that were any-
thing out of the ordinary [unusual].
Nurse:
How did you cope?
Mr R.:
Well I didn’t cope. I just put them to the bottom of my
pile of work.
Nurse:
How has the work situation affected your daily life?
Mr R.:
I’m finding it hard to get out of the house [leave] for
work in the mornings.
Nurse:
Anything else?
Mr R.:
Same sort of problems as the ones at work. I can’t
concentrate on one thing and keep starting things and
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
110
C3996_05.qxd 26/02/2004 13:56 Page 110
then leaving it to start something else. Doing the
shopping is a nightmare [in this context means ‘an
ordeal’]. I just wander from aisle to aisle picking items
up and putting them down. It takes me over an hour
and then I forget lots of items.
Nurse:
Do you feel under stress?
Mr R.:
Most of the time.
Nurse:
What sort of things make you feel stressed?
Mr R.:
Work obviously, but things at home can hassle me [in
this context means ‘worry’] as well.
Nurse:
At home [in this context reflecting what Mr Reeves has
said]?
Mr R.:
Yes, paying bills on time and the state of the garden,
it’s like a jungle [very untidy]. When I feel uptight
[stressed] I get really fussy about piddling [petty,
unimportant] things that don’t matter.
Nurse:
What do you normally do to relieve the stress?
Mr R.:
Listening to music helps and I’ve started doing yoga
again.
Nurse:
Your GP [general practitioner] thought that our team
might be able to offer you some help.
Mr R.:
Yes, we discussed some of the options, but I need
more details.
Mel, aged 16 years, has just started at a new school. She had to
change schools when her parents split up [divorced]. It has been
difficult to make new friends and she is worried about the exams
in the summer.
Nurse:
Hello, I’m Nurse Sanchez. May I call you Mel?
Mel:
If you like.
Nurse:
What would you like to talk to me about?
Mel:
You know, I moved here last term when my mum
[mother] and dad [father] split up [divorced].
Nurse:
Yes, you came from St. Mary’s didn’t you?
COMMUNICATION IN NURSING
111
Case history – Mel
C3996_05.qxd 26/02/2004 13:56 Page 111
Mel:
Yeah [yes], it was cool [OK, excellent] there.
Nurse:
How are you settling in here?
Mel:
Don’t know really.
Nurse:
What about the people in your class? Have you made
any friends?
Mel:
They’ve all known each other since year 7 [the first
year in high school]. They don’t want me – they think
I’m stupid.
Nurse:
Is that what you think?
Mel:
Yeah, ‘cos [because] of the row [quarrel] I had with that
girl who’s always talking.
Nurse:
How do you feel about the quarrel?
Mel:
It’s getting me down [depressing me].
Nurse:
Have you felt like crying at all?
Mel:
I’m usually OK, as long as [provided] they don’t keep
picking on [bully, tease] me. During PE [physical edu-
cation] I burst into tears when they made a thing about
not picking me [choosing me] for their team. They said
I was naff [in this context means ‘useless’] at sport.
Nurse:
Do feel like breaking down [bursting into tears] at other
times?
Mel:
Yeah, sometimes at home for no reason, but my mum
[mother] says I should try not to take things to heart
[try not to be too hurt by people’s remarks].
Nurse:
Did you tell your mum that you just felt like crying?
Mel:
I don’t want to worry her. She’s having a bad time.
Nurse:
Because of the divorce?
Mel:
Yeah, she was gutted [very upset].
Nurse:
How have you been feeling generally?
Mel:
Sort of sad and fed up [bored, discontented].
Nurse:
Are you able to enjoy the things you used to do?
Mel:
I can’t be bothered to get dolled up [get dressed up].
You can’t go out on your own.
Nurse:
What about hobbies?
Mel:
I used to help out at the local riding stables.
Nurse:
Yes?
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
112
C3996_05.qxd 26/02/2004 13:56 Page 112
Mel:
I gave it up [stopped] when we moved to this place. I
can’t get interested in anything now.
Nurse:
Apart from what you have told me is there anything else
you are particularly worried about?
Mel:
Yeah, I’m frantic [very worried] about my exams.
Nurse:
What are you planning to do [career plans, etc.]?
Mel:
Yeah, I really want to go to uni’ [university] to do law,
so I need good grades.
Nurse:
It’s difficult changing schools just before exams.
Mel:
Tell me about it [in this context, emphasises that Mel
knows this already].
Nurse:
How is your studying going?
Mel:
I should do a plan, but I keep putting it off [delaying].
It’s easier to watch TV [television].
Nurse:
How are you sleeping?
Mel:
It’s difficult to drop off [get to sleep] worrying about
my revision.
Nurse:
What about your appetite?
Mel:
OK, if you count junk food. If my mum is out I just
have chips.
Nurse:
When you feel sad do you ever feel like harming yourself?
Mel:
No, not really. I know my mum needs me and I’m set
on [determined] being a lawyer.
Nurse:
Do you think you could talk to your mum about how
you’re feeling?
Mel:
I suppose it would be best.
Nurse:
The doctor might be able to help as well.
Mel:
Yeah, thanks.
DEMENTIA AND CONFUSION
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with dementia
and confusion are given in Box 5.12.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
COMMUNICATION IN NURSING
113
C3996_05.qxd 26/02/2004 13:56 Page 113
Mrs Georges has cared for her husband for over a year. His con-
dition has deteriorated rapidly and he has now been admitted to
a nursing home. He has severe dementia due to Alzheimer’s dis-
ease, and it is impossible for his wife to manage with him at
home.
Mrs G.: Hello Nurse. My husband seems quite settled now.
Would you like me to answer those questions?
Nurse:
Hello.Yes, now’s a good time.Tea will be here in half an
hour [30 minutes] or so.Will you be staying to have tea
with Mr Georges?
Mrs G.: Yes, that would be nice. It’s a real treat [pleasure] to
sit down and have a meal that someone else has
got ready.
Nurse:
Being the only carer is such hard work.
Mrs G.: At home he [her husband] wouldn’t let me out of his
sight for a minute. You can imagine how hard it is to
get a meal.
Nurse:
Yes, how are you feeling now that Mr Georges is here
with us?
Mrs G.: I know it was the right decision and had it all out
[discussed it fully] with the people from the Social
[social workers], but I’ll miss him not being at home.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
114
Box 5.12
Words associated with dementia and confusion
(for further examples see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Confused
At a loss; at sea; at sixes and sevens; befuddled;
bewildered; mixed up; muddled; muzzy;
not with it
Demented
Crack brained; crazed; crazy; daft; dotty;
non-compos mentis
Case history – Mrs Georges
C3996_05.qxd 26/02/2004 13:56 Page 114
It had to happen. I’m completely done in [exhausted
or worn-out].
Nurse:
Tell me about Mr Georges.
Mrs G.: I wish you could have seen him before all this
happened. He was so on the ball [alert] and always
helping people. He was in the merchant navy and
spent months away, so I was used to being on my
own before he retired.
Nurse:
Have you got family nearby?
Mrs G.: I won’t be lonely. Our lad [son] lives just around the
corner. I really lost my Bob [Mr Georges] when his
mind started to go.
Nurse:
When did you first notice?
Mrs G.: Hard to say [difficult], I suppose you expect your
memory to get worse, so you put the little lapses
down to [caused by] him getting older.
Nurse:
Well we all lose our glasses and forget names.
Mrs G.: Yes, but it was more than that. He seemed muddled
[confused] by everyday things like making a pot of tea.
He would put the teabags in the kettle or make the tea
with cold water.
Nurse:
How was he in himself?
Mrs G.: At first he knew something was wrong. He was
frustrated and would fly off the handle [be irritable]
with me and I would snap back. I didn’t realise he
couldn’t help it [not his fault].
Nurse:
How do you feel about it now?
Mrs G.: Real bad. I feel weepy [tearful] just talking about it.
Silly isn’t it?
Nurse:
No it’s not silly, not at all.
Mrs G.: After 40 years married we knew what the other was
thinking most of the time and now we’re not even on
the same wavelength [don’t understand one another].
Nurse:
What other things have been happening?
Mrs G.: He would witter on and on [go on] about the same
thing and asking me the same question. I’d say to him
COMMUNICATION IN NURSING
115
C3996_05.qxd 26/02/2004 13:56 Page 115
‘Bob you’re driving me up the wall [irritating me]’, he’d
smile and next minute do it again. But he hardly says a
word now [does not speak very much].
Nurse:
What about washing and dressing?
Mrs G.: Gets in a right pickle [difficulty] with dressing. I have to
help him. It’s as if he can’t remember what to do.
Getting him to shave is a right carry-on [performance],
he just won’t do it and pushes me away if I try to help.
I hate to see him so scruffy [untidy]. He was always so
particular with his turn out [clothes and appearance]. I
don’t know whether you’ll have better luck with him.
Nurse:
The care assistants have special training sessions and
they’re all used to looking after people who have problems
like Mr Georges’.
Mrs G.: But they won’t know how to stop him getting in a
lather [agitated].
Nurse:
Would you like to meet the team who will be caring for
Mr Georges, so you can tell them about the best way to do
things? Most relatives say it’s reassuring.
Mrs G.: That would put my mind at rest [feel reassured] about
leaving him here. I will just say that he seems to like
sitting in front of the box [television]. He can’t know
what’s on but he does seem calmer. Before he got this
bad he was forever changing channels and I never got
to see the end of anything.
Nurse:
How frustrating for you. Does Mr Georges wander about?
Mrs G.: In the last few months it started. He kept wandering off
during the day. He was off like a shot [moved quickly]
and he’d be in the road before I got out the house. I
was sure he’d be under a car at any moment [have a
road accident]. And then he stopped knowing day and
night and would get up [out of bed] at all hours of the
night. That really scared me. What if he’d turned on
the gas [the gas cooker/oven]? He was always fiddling
[touching] with it during the day.
Nurse:
That must have been a real worry.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
116
C3996_05.qxd 26/02/2004 13:56 Page 116
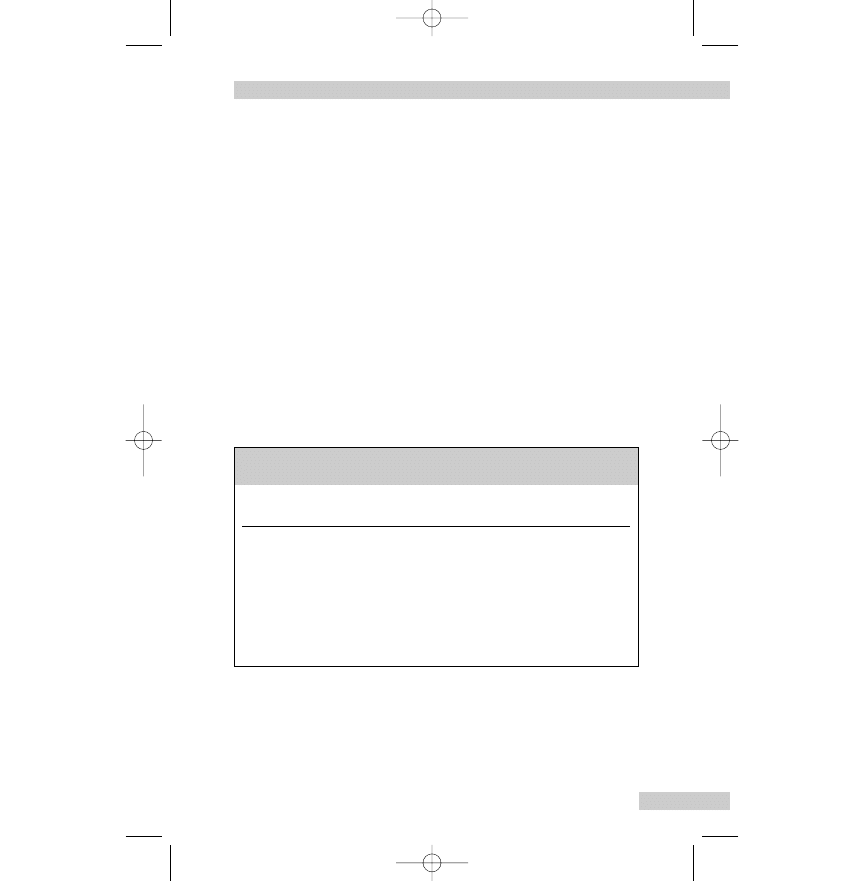
Mrs G.: I’d lay there in the dark listening for him getting up,
and when I dropped off [got to sleep] any little noise
would wake me. That’s what really decided me about
him coming here.
Nurse:
I just heard the tea trolley go by.We can finish this later if
you like.
Mrs G.: I could do with a cuppa [usually refers to a cup of tea]
I’m parched [thirsty].
PAIN
Some nursing/medical or Standard English words and correspon-
ding colloquial words and expressions associated with pain are
given in Box 5.13.
Note: Colloquial expressions used in the case histories and
example conversations are explained in brackets […].
COMMUNICATION IN NURSING
117
Box 5.13
Words associated with pain (for further examples
see Ch. 6)
Nursing/medical or
Colloquial (everyday) or slang (very informal)
Standard English words
words and expressions used by patients
Analgesic
Painkiller
Grimaces
Pull a face
Pain
Ache; agony; cramp; discomfort; hurt; irritation;
smarting; soreness; spasm; tenderness; throb;
twinge (see text for more words used to
describe pain)
‘Pain’ and ‘ache’ mean the same thing and we speak of ‘aches
and pains’ generally. Both these words are nouns, but the word
‘ache’ can be used with the following to form a compound noun:
backache, earache, headache, stomach-ache (usually means an
C3996_05.qxd 26/02/2004 13:56 Page 117
ache in the abdomen), toothache. For the other parts of the body,
we say:
‘I have a pain in my shoulder, chest, etc.’
It is possible to have a pain in the back, head and stomach
(usually means the abdomen), but this generally refers to a more
serious condition than backache, headache and stomach-ache.
The word ‘ache’ can also be used as a verb:
‘My leg aches after walking 10 miles.’
‘My back aches after gardening.’
The word ‘hurt’ is another verb used to express injury and
pain:
‘My chest hurts when I cough.’
‘My neck hurts when I turn my head.’
How patients describe pain: commonly used words
— aching
— beating
— biting
— boring
— burning (as in cystitis, oesophagitis)
— bursting
— colicky (often used to describe the pain that results from
periodic spasm in an abdominal organ (biliary, intestinal),
but also used to describe renal colic and dysmenorrhoea)
— crampy
— crushing (as in angina pectoris or myocardial infarction)
— cutting (rectal disease)
— discomfort (may describe mild pain sensation)
— dragging (as in uterine prolapse)
— drawing
— dull (headache, tumour)
— gnawing (tumour) (pronounced nawing)
— grinding
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
118
C3996_05.qxd 26/02/2004 13:56 Page 118
— griping
— gripping (as in angina pectoris)
— heavy (as pre-menstrual)
— knife-like
— numb (lack of sensation)
— piercing (angina pectoris)
— pinching
— pounding (headache – ‘My head is pounding’)
— pressing
— prickling (as in conjunctivitis)
— scalding (cystitis)
— severe pain (gip – ‘It gives me the gip’)
— sharp
— shooting (sciatica, toothache)
— sickening
— smarting (burns)
— sore
— spiky
— splinter-like
— stabbing (indigestion)
— stinging (cuts, stings)
— stitch (sudden sharp pain usually due to spasm of the
diaphragm)
— straining
— tearing
— tender
— throbbing (headache, an infected area)
— tingling (return of circulation to extremities)
— twinge (sudden, sharp)
— twisting.
Pain may also be described as being: acute, agonising, chron-
ic, constant, constricting, convulsive, darting, deep-seated, diffi-
cult to move, diffuse, excruciating, fleeting, intense, intermittent,
localised, mild, obstinate, persistent, radiating, severe, spasmod-
ic, spreading, stubborn, superficial, very severe, violent.
COMMUNICATION IN NURSING
119
C3996_05.qxd 26/02/2004 13:56 Page 119
Miss Carter has had migraine attacks for many years, but recently
they are coming more often and her usual tablets are not as effec-
tive. This has led to her having several days off sick from work.
Miss C.: My heads [in this context meaning the ‘migraine
attacks’] are getting worse. I wish I knew what brings
it on [causes it].
Nurse:
When did you start having migraine?
Miss C.: Oh, years ago when I was still at school, but now
they’re coming every couple of weeks.
Nurse:
How does that differ from before?
Miss C.: I only had them once in a blue moon [very
infrequently], but always when I was planning
to do something special.
Nurse:
Can you think of any reasons why they’re coming more often?
Miss C.: Well, I’ve got a new job and it’s more stressful.
Nurse:
Can you do anything about that?
Miss C.: No chance at the moment.
Nurse:
What about things like certain foods, or drinks [in this
context alcoholic drinks]. Have you noticed any link?
Miss C.: I know to lay off [give up] chocolate. But now it’s really
spooky [weird, strange]. Sometimes I have a sip of
wine and my head feels tight and I just know that a
migraine is on its way [going to occur], and other times
I have two or three glasses and get away with it
[escape having a migraine attack].
Nurse:
Is it a particular type of wine?
Miss C.: No, sometimes red and sometimes white wine.
Nurse:
Does anything special make it worse once you’ve got the
pain?
Miss C.: Yes, any bright light. You know like sunlight on water.
It’s no problem ‘cos [because] I always have my dark
glasses with me until I can get into bed.
Nurse:
What about the migraine attacks? Have they changed?
Miss C.: The throbbing is much worse. It’s so bad I have to lie
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
120
Case history – Miss Carter
C3996_05.qxd 26/02/2004 13:56 Page 120
on the bed and try to sleep.
Nurse:
Do you take anything for the pain?
Miss C.: I always used to take a painkiller [analgesic] and the
pain would soon go off [stop], but no joy [failure] now.
Nothing seems to shift the pain [relieve the pain].
Nurse:
Which painkillers?
Miss C.: Mostly Panadol [a proprietary name for paracetamol],
but sometimes ibuprofen. It depends on what I have
with me.
Nurse:
Over the last few years much better drugs have become
available for migraine.
Miss C.: Yes, I knew that, but it didn’t matter while the Panadol
still worked OK.
THINKING ABOUT (REFLECTION) PRACTICE:
EXERCISE
Think about a recent time at work when you needed to get infor-
mation, or help patients/clients/relatives to understand something
to do with their care.
— Who was the person?
— What did you need to find out or tell them?
— How did you start the conversation?
— Did you get the information you needed, or were you suc-
cessful in helping the person understand something?
— Did you have any difficulty understanding everything the
patient/client/relative said to you?
— Do you think that they understood everything you said?
— Which parts of the communication were good and what
helped to make it so?
— Which parts were less successful and what stopped them
working so well?
Consider the answers you have given and pick out what you
have learned from this situation. What, if anything, would you do
differently if the same sort of situation happened again?
COMMUNICATION IN NURSING
121
C3996_05.qxd 26/02/2004 13:56 Page 121
FURTHER READING
Holland K, Jenkins J, Solomon J, Whittam S 2003 Applying the
Roper–Logan–Tierney model in practice. Churchill
Livingstone, Edinburgh.
Roper N, Logan WW, Tierney AJ 1996 The elements of nursing,
4th edn. Churchill Livingstone, Edinburgh.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
122
C3996_05.qxd 26/02/2004 13:56 Page 122
Colloquial English
LANGUAGE USED BY PEOPLE TO DISCUSS PROBLEMS
OR SIGNS AND SYMPTOMS
Many people, especially older people, find extreme difficulty in
discussing their bodily functions and signs and symptoms of a
disorder with a health worker. This may be from not knowing the
correct words, or shyness. Obviously, the more intimate the part
of the body, the greater the embarrassment, and so a wide vocab-
ulary of euphemisms and slang expressions has sprung up in the
English language.
Quite often the person is so inarticulate that you will have to
suggest various problems or symptoms and the person merely
says ‘yes’ or ‘no’. In some situations, the nurse or doctor may
have to use colloquial expressions. However, there is consider-
able risk of misunderstanding and it is safer to use the correct
terms and check that the person has understood.
Colloquial expressions show considerable regional differences.
A few are included in this chapter, but it is important that you
become familiar with those used locally. The expressions that
people use are also influenced by their age and culture, and again
you should note the expressions used locally. Those phrases
which are most commonly used have been printed in italics (e.g.
back passage). Many colloquial expressions you will hear are con-
sidered to be vulgar, offensive or discriminatory in some way.
You should not use them, and those that are not commonly used
in polite society, have been marked with an asterisk (*).
PARTS OF THE BODY
Anus – arse*, arsehole*, back passage, butt*, butthole*, hole*.
To break wind: to fart*, to poop*, to trump*.
123
6
C3996_06.qxd 25/02/2004 18:31 Page 123
Bladder – waterworks, e.g. Nurse to patient: ‘How are the water-
works?’ or
How is your bladder working?
Bowels – gut, e.g. a pain in one’s gut, to have belly ache (often
used to mean bowels), to have gut ache.
Brain – head-piece, noodle, nut (e.g. use your nut).
Breast – boobs*, bosom, buffers*, charleys*, chest, chestnut*,
globe*, knockers*, nipples, paps*, tits*, titties*, top part.
Imitation breasts: falsies. Small breasts: ‘I haven’t got much’.
Buttocks – arse*, backside, behind, bottom, botty (childish),
bum*, buns* (male), cheeks, hind quarters, posterior, rear,
rump*, seat, sit-upon, stern, tail, toby.
To have large buttocks: to be broad in the beam.
Cervix – neck of womb.
Chest – to have a flat, barrel, hollow, pigeon chest.
The following are only used for females:
bosom, breast, buffers*, bust.
To have a bad cough: to bark.
Coughing: to be chesty, a bit chesty.
To have one’s chest finger-tapped: to have a thump.
Clitoris – clit*.
Crotch – often used to mean groin or skin covering genitalia.
Ear – bat ears (prominent), a cauliflower ear (from boxing), flap-
pers, lug* (e.g. to have lugache*).
Rather deaf: to be hard of hearing.
Elbow – funny bone, e.g. to hit one’s funny bone (so called
because of the strange tingling one experiences when it is
struck).
Enlargement of abdomen in older people – middle-age
spread.
Eyes – glimmers*, ogles*, optics, peepers.
To have a squint: to be boss-eyed, to be cock-eyed, to be
wall-eyed.
To have low visual acuity in one eye: to have a lazy eye.
Face – clock*, dial*, mug*, physog*.
Genitals – male and female: bits, package, down below, private
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
124
C3996_06.qxd 25/02/2004 18:31 Page 124
parts, thing, pencil and tassle* (male child’s penis and scrotum).
Hand – mitt, paw.
Head – bonce; brain-box, brain-pan, napper, nob, noddle, nous-
box (nous means intelligence, common sense), nut, skull.
Heart – engine, e.g. ‘my engine’s not working properly’, jam tart*
(Cockney), ticker.
Something wrong with one’s heart: to have a dicky heart.
To have a weak heart: to have a heart.
Hymen – cherry, maidenhead, maid’s ring (Cockney).
Intestines – bowels, guts, innards, inside.
Legs – bandy legged (bow), drumsticks (very thin), K-legged
(with knees knocking together), knock-kneed (knees bent
inwards to face each other), peg leg (an artificial leg), pins,
spindles.
A lame leg: to have a gammy leg.
Short legs: to have duck’s disease.
Walk badly: to be bad on one’s pins.
Walking with the feet turned in: hen-toed.
Lungs – bellows, tubes.
To be bad in one’s breathing: to be short-winded.
Mouth – chops*, gob* trap*.
Navel – belly button.
Neck – Adam’s apple (projection of thyroid cartilage of larynx),
salt cellars (very deep hollows above collar-bone in female
neck), scruff of neck (nape).
Nose – beacon* (red and large), beak*, conk*, hooter*, sniffer*,
snitch*.
Nasal congestion: to be blocked up, bunged up, stuffy.
Nasal discharge: snot*.
Noisy breathing in children due to nasal congestion: snuffles.
Running nose: a snotty nose*.
Penis – almond*, almond rock* (Cockney), bean*, button* (baby),
club*, cock*, dick*, equipment*, gear*, it*, John Thomas*, knob*,
little man*, little tail* (small boys), meat*, old man*, Peter*, pin-
kle*, prick*, private parts, privates, rod*, shaft*, she*, stick*,
tadger* (Northern England), tassel*, thing*, tool*, Will*, Willie*.
COLLOQUIAL ENGLISH
125
C3996_06.qxd 25/02/2004 18:31 Page 125
Scrotum – bag*, sac.
Skull – brain pan.
Spine – backbone.
Stomach – abdomen, belly, bread-basket*, corporation (when
large), croop, guts (stomach and intestines), innards, inner
man, peenie, pinafore, tummy.
To belch: to burp.
The noise the stomach makes when one is hungry: to have
stomach rumbles.
Something wrong with it: to have a gastric stomach.
Stomach ache: to have a pain in one’s guts.
Teeth – buck teeth (protruding); peggy, peggies (childish).
Testes/testicles – ballocks*, balls*, bollocks*, charleys*, cobblers*,
cods*, nuts*, pills*, pillocks*, stones*. See Genitals.
Throat – clack*, gullet, organ-pipe (windpipe).
A very severe cough: a churchyard cough.
Sputum: phlegm.
To be hoarse: to have a frog in the throat.
To have a sore throat: to have a throat.
Tongue – clack*, clapper*.
The tongue can be described as: coated, dirty, furred, furry,
thick.
Talkative person: a chatterbox.
Trachea – windpipe.
Umbilicus – belly button (childish), navel.
Urethra – pipe, waterpipe.
Uterus – box, womb.
Vagina (or vulva) – birth canal, box*, brush*, crack*, cunt*,
down below, fanny*, front passage, hair pie*, it, private (e.g.
‘my private is sore’), private part, pussy*, slit*, thing*, there,
twat*, up inside.
BODY FUNCTIONS
Constipation, to have – to be bunged up, to be costive, I haven’t
been for 4 days. I haven’t had a road through me for a week*.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
126
C3996_06.qxd 25/02/2004 18:31 Page 126
Defaecate, to – to crap*, to do a big job, to do a job, to do a
pooh (childish), to do a rear*, to do number two, to do one’s
business, to go to the toilet (and use paper), to have a clear
out, to have the bowels opened, to job*, to pass one’s motions,
to shit*, to use a bedpan (hospital).
Diarrhoea, to have – the trots, collywobbles, Gippy tummy,
run’ems, runs, scours, squitters.
To have a sudden attack of diarrhoea: to be taken short.
Die, to – to be a goner, to be all over, to be slipping (to be
dying), to burn oneself out (die early through overwork), to
conk out, to go (go away), to go home, to go to the next
world, to hang up one’s hat, to have had it, to have one’s num-
ber up, to have had one’s chips, to have one foot in the grave
(to be dying), to kick the bucket, to pass away, to peg out, to
pip out, to pop off (usually die suddenly), to push up daisies,
to snuff it or out, to turn it in, to turn one’s toes up, to have
had a long (or good) innings (to die at an old age), to lay out
(prepare for burial or cremation).
Note: To commit suicide: to kill oneself.
Faint, to – to black out, to have a black-out, to go off hooks, to
pass out.
Faeces, stools – baby’s yellow (infantile excrement), business,
cack*, job*, mess*, motions, number two, shit*.
Nurse to patient: ‘Are your motions well formed?’.
Mothers often say of a child: ‘His toilet is green’ (meaning his
stools are green).
Note that ‘a dose of salts’ means Epsom salts.
Tenesmus: straining.
Impotent, to become – to be no good to one’s wife, to lose
one’s nature.
A man’s impotence will be expressed by his wife/partner in
the following ways: he can’t sustain an erection, he can’t
manage, his cock’s soft or droopy*. Doctor to man: ‘Can
you get a hard on?’.
Menstruate, to – to be unwell, one’s period, the curse, the days,
the monthlies, the other, the thing, the time of the month, the
usual.
COLLOQUIAL ENGLISH
127
C3996_06.qxd 25/02/2004 18:31 Page 127
‘Have you seen anything?’ (feminine euphemism).
‘I haven’t seen for 6 weeks’ (no menstruation, possibly preg-
nant).
Nurse to patient: ‘When was your last period?’
Naked, to be – to be in one’s birthday suit, to be in the altogeth-
er, to be starkers.
Pregnant, to be – away the trip* (Scottish working class), to be
caught*, to be expecting, to be having a baby, to be in a deli-
cate condition, to be in an interesting condition, to be in Kittle
(Scottish), to be in pig*, to be in pod*, to be in the club*, to be
in the family way, to be in the pudding club*, to be one in
line*, to be preggers*, to be up the duff*, to be up the pole*,
to be up the stick*, to catch on, to catch the virus*, to click*,
to cop it*, to fall for a baby (to have an unwanted pregnancy),
to have a bun in the oven*, to have a touch of the sun*.
She’s 6 months pregnant: she’s 6 months gone.
Sleep, to – to close one’s eyes, to doze (short sleep), to go off (to
fall asleep), to go to the land of nod, to have a catnap (short
sleep), to have a doze, to have a snooze (short sleep), to have
forty winks (short sleep), to have some shut-eye, to nod off
(short sleep), ziz.
Urinate, to (micturate) – to do number one, to go to the loo, to
have a run-out, to pass water, to pee, to pee-wee (childish), to
piddle*, to piss*, to spend a penny (women only), to tiddle
(childish), to tinkle (women only), to wee-wee (childish).
Nocturia: to get up in the night to pass urine.
Hostess to guests: ‘Do you want to wash your hands?’ (Do
you want to go to the toilet?).
The lavatory can be described as: bathroom, bog*,
cloakroom, convenience, Gents’, heads*, Ladies’, lav,
lavvy, little girls’ room, loo, place, powder room (Ladies’
in a hotel), privies, rears*, toilet, WC.
A chamber pot: banjo*, gerry*, po, pot, potty (childish).
To hold a baby over a chamber pot: to hold out a baby.
To put a baby on a chamber pot: to pot.
Vomit, to – to be ill, to be sick, to bring up, to lose the lot, to
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
128
C3996_06.qxd 25/02/2004 18:31 Page 128
puke*, to pump your heart up, to sick up, to spew*, to throw
up*.
Nausea: the sicks.
To have nausea: to feel queasy, to feel sick.
‘Have you vomited?’ ‘Have you been sick?’
To try to vomit but nothing comes up: to retch.
To vomit very much: to be as sick as a dog (or cat).
To have a headache and vomiting: to have a sick headache.
Weep, to – to blub, to blubber, to break down, to cry, to turn on
the waterworks, to turn the tap on.
MENTAL AND PHYSICAL STATES
Angry, to be – to be cross, to be crusty, to be heated, to be hot
under the collar, to be liverish, to be livid, to be shirty, to be
steamed up, to flip, to fly off the handle, to go off the deep
end, to have a paddy, to have a tantrum, to jump down some-
one’s throat, to let off steam, to lose one’s hair, to lose one’s
shirt, to play the devil, to see red.
Confused, to be – to be all at sea, befuddled, bewildered, disori-
entated, flummoxed, forgetful, muddled, muzzy, unsure.
Depressed, to be – to be blue, to be browned-off, to be down in
the dumps, to be down in the hips, to be down in the mouth,
to be fed up, to be low, to be off the hinges, to have a button
on, to have a chopper, to have a face as long as a fiddle, to
have the droops, to have the hump, to have the hyp, to have
the mopes, to have the pip.
Drunk, to be – to be a dipso (dipsomaniac), to be boozed
(boozy), to be fou*, to be fresh (slightly drunk), to be fuddled
(confused with drink), to be high on surge (to be drunk on
surgical spirit), to be lush (slightly drunk), to be merry (happy
with drink), to be muzzed, to be on the bottle (habitual
drinker), to be paralytic (very drunk), to be pie-eyed, to be
plastered, to be slewed, to be sloshed, to be soaked (very
drunk), to be sozzled (very drunk), to be squiffy (slightly
drunk), to be tiddly (slightly drunk), to be tight, to be tipsy
COLLOQUIAL ENGLISH
129
C3996_06.qxd 25/02/2004 18:31 Page 129
(slightly drunk), to be under the influence (of liquor), to be
well-oiled, to be woozy (confused with drink), to have a skin-
ful (very drunk), to have Dutch courage (extra courage
induced by alcohol), to have more than one can carry, to have
one over the eight, to see pink elephants (or spiders) (to suf-
fer from DTs), to have a hangover (to feel ill as a result of alco-
hol), to have a morning-after-the-night-before (to feel ill as a
result of alcohol), to hit the bottle (to drink excessively).
Dull, to be – to be a dream, a drip, a moron, a muggins, a noo-
dle, a pie-can, a sap*, a wet, dead alive, dopey, dumb, foolish,
goofy, half-baked, half-witted, lethargic, mutton-headed, silly,
simple, slack, slow, soft, stupid, thick, thick-skulled.
Exhausted, to be – to be all in, to be clapped out*, to be dead,
to be done for, done in, done up, to be fagged out, to be fin-
ished, to be flaked out, to be jiggered, to be knackered*, to be
knocked up, to be ready to drop, to be shagged*, to be shat-
tered, to be tired out, to be used up (utterly exhausted), to be
weary, to be whacked, to feel like death, to go all to pieces
(collapse from exhaustion).
To knock it out of one, ‘walking uphill knocks it out of me’
(walking uphill exhausts me).
Healthy, to be – to be A1, to be as fit as a box of birds, to be as
fit as a fiddle, to be fighting fit, to be first rate, to be full of
beans, to be in fine fettle, to be in the pink, to be on good
form, to have plenty of pep (pep = energy), to have plenty of
vim (energy, vigour), to perk up (recover good health).
To begin to recover after an illness: to be on the mend, to
turn the corner.
Madness – (in varying degrees): to be a bit touched, to be a
case, to be a character (to be eccentric, odd), a scatterbrain
(very forgetful, vague), to be as mad as a hatter, balmy,
(barmy), bats, batty, bonkers, to be clean gone, cracked,
crackers, crack-pot, crank, crazy, to be dippy, dotty, gaga
(senile), goofy, half-baked, kinky, loony, loopy, mad, to be
mental, non compos mentis, not all there, to be not right in
one’s head, nuts, off one’s block, off one’s chump, off one’s
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
130
C3996_06.qxd 25/02/2004 18:31 Page 130
head, off one’s nut, off one’s rocker, to be off the rails, out of
one’s mind, to be peculiar, potty, round the bend, scatty, a
screwball, screwy, silly, simple, soft, stupid, up the creek,
weak in the upper storey, to go doolally, to go hay-wire, to
have bats in the belfry, with a tile (or screw) missing (or
loose).
Psychiatric (mental) hospital: bin, funny farm, loony bin,
nuthouse.
Nervous, to feel – to be a fuss-pot, to be a jitter-bug, to be all
hot and bothered, to be all of a dither, to be chewed up, to be
edgy, on edge, to be fidgety, to be in a blue funk, to be in a
flap, to be in a stew, to be in a tizzy, to be jittery, to be
screwed up, to be shook-up (nerve-racked), to get all het-up,
to get in a state, to get uptight, to go all hot and cold, to go
into a flat spin, to go to pieces (collapse through nerves), to
go up the wall, to have ants in one’s pants*, to have butterflies
in one’s stomach, to have forty fits, to have kittens, to have the
creeps, to have the heebie-jeebies, to have the shakes, to have
the shivers, to have the twitters, to have the willies, to have
the wind up, to have the worrits, to lose one’s cool, to worrit
(be anxious).
Unwell, to be – to be anyhow, to be below par, to be groggy,
to be not oneself, to be not quite right, to be off colour, to be
out of sorts, to be peaky, to be pingley, to be poorly, to be
run down, to be taken bad, to be tenpence to the bob, to be
under the weather, to be washed-out, to be weedy (anaemic,
sickly), to be wobbly (weak after an illness), to be wonky
(weak), to come all over queer, faint, ill (suddenly feel
unwell), to crack up, to feel a bit off it, to feel a bit rough, to
feel funny, to feel half-baked, to feel like death warmed up
(very unwell), to feel like nothing on earth, to feel lousy, to
feel queer, to feel ragged, to feel seedy, to go funny, to have
a bad turn.
Vertigo – to be dizzy, to be giddy, to be muzzy, to feel the room
spin, to feel queer, to have a mazy bout, to have a swimming
head.
COLLOQUIAL ENGLISH
131
C3996_06.qxd 25/02/2004 18:31 Page 131
GENERAL EXPRESSIONS
(In this section the text in bold type is the colloquial expression.)
Dope, physic – any kind of medicine.
Medicine – anything taken to relieve pain or symptoms of illness.
Usually the word refers to liquid or drugs taken by mouth.
Pills, tablets – drugs in tablet form. Note: to be on the pill: to be
taking the contraceptive pill.
A tonic – medicine to invigorate one after an illness.
To be at death’s door, to be critical, to be nearly a goner – to
be dangerously ill.
To be laid up – to be confined to bed, e.g. ‘I was laid up for
3 months’.
To be looking up – to improve.
To be off sick, to be on the sick-list, having a sicky – to be
absent from work due to illness.
To be on the mend – to improve.
To be nesh, to be soft – to be prone to illness.
To be under a doctor – to be in a doctor’s care.
To find one’s legs – to begin to walk after an illness.
To get a chit from the doctor – to get a medical certificate.
To go under – to have a general anaesthetic.
To have a bad turn – to become ill suddenly.
To have a bug, a germ – to have an infection.
To have a check-up – to be medically examined, or have a
screening test.
To have a jab – to have an injection.
To have a set-back – to have a relapse.
To have a temperature – to be pyrexial or feverish, to have a
high temperature, e.g. ‘I’ve had a temperature all day’.
To have gas – to have a general anaesthetic.
To have painkillers – to have analgesics.
To have sleeping pills – to have sedatives.
To have time off – to have sick leave.
To stitch – to suture.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
132
C3996_06.qxd 25/02/2004 18:31 Page 132
To suck lozenges – to suck small tablets, usually for coughs and
sore throat.
To take a turn for the better – to improve.
To take medicine for the bowels – to take a laxative.
To take stitches out – to remove sutures.
To turn the corner – to improve.
REPRODUCTIVE AND SEXUAL HEALTH PROBLEMS
The vocabulary to express menstruation and pregnancy is listed
separately under body functions (see p. 126–129).
Women’s health expressions
Abortion (Note: In practice it is usual to refer to an abortion as
a ‘miscarriage’ to avoid causing distress, as some women will
associate the term abortion with a deliberate termination of
pregnancy) – spontaneous miscarriage, a miscarriage, a miss*.
‘It came away.’ ‘I lost my baby’ or ‘We lost our baby.’
Candidiasis – vaginal thrush.
Confinement – childbirth, delivery. ‘Did you have an easy con-
finement?’
Dilatation and curettage – D&C, a scrape, e.g. ‘I’ve had two
D&Cs’ (two scrapes).
Dysmenorrhoea – period pains, to be unwell.
Efforts to terminate a pregnancy – to bring on a period, to
lose it (a baby), to get rid of a baby. ‘They took the baby
away.’
Episiotomy – to make a perineal cut. ‘I’m going to cut you now.’
Flooding – excessive bleeding from the uterus during
menstruation.
Hot flushes and night sweats, to have – to have a feeling of
being hot, looking hot and red, and sometimes sweaty.
Associated with the menopause.
Hysterectomy – to have an internal operation, to have a major
operation, to have all taken away (uterus and ovaries).
COLLOQUIAL ENGLISH
133
C3996_06.qxd 25/02/2004 18:31 Page 133
Menarche – the beginning of menstrual periods, e.g. ‘When did
your periods start?’.
Menopause – the end of periods, e.g. ‘When did your periods
end?’, the change, that certain age, the time of life.
I haven’t seen anything for 6 months.
It’s your age. It’s the time of life.
Menorrhagia – heavy periods.
Parturition – labour, to be in labour. ‘How often are you having
contractions?’
Placenta – the afterbirth.
Repair of the prolapse – ‘I was stitched up below’, to be
hitched up.
Rupture the membranes, to – to break my waters.
Sanitary towels – pads, STs, Tampax (a brand of tampons worn
internally), towels, wings.
Still-born baby – baby born dead.
Suture – to be stitched up.
Termination of pregnancy – an abortion. ‘I don’t want this
baby. Can I have an abortion?’ ‘I did away with it.’* ‘I decided
not to go ahead with the pregnancy.’
Vaginal discharge – to have whites, to lose down there.
‘Something comes away from me ...’
Version – turning (of fetus).
Men’s health expressions
Coitus interruptus – to be careful, to withdraw. ‘My husband’s
very careful.’
Ejaculate, to – to come, to get your rocks off*, to shoot.
Erection, to have an – to have a hard on, to have a stand*, to
have a stiff*, to have the horn*.
Impotent (now known as erectile dysfunction), to be – to
have a half-stand*. ‘I can’t keep it up.’ ‘My husband has trouble.’
Impotent, to become – to lose one’s nature.
Semen – come, cum, jizz.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
134
C3996_06.qxd 25/02/2004 18:31 Page 134
Sexual health expressions
Anal intercourse – buggery, bumming*. ‘He wants to come at
me from behind.’* To rim*.
Bisexual – AC–DC*, to be double-jointed*.
Dyspareunia – love pain.
Female homosexual/lesbian – to be gay, kinky*, to be butch (a
lesbian with male characteristics), a dyke*, a lessie*.
French kiss – kiss with mouth open and insert tongue in part-
ner’s mouth.
Heterosexual – straight.
Homosexual expressions – to be the active/passive partner,
eating ass*, reaming*, tonguing (using the mouth on anus),
finger fucking*, fisting* (using finger/fist in anal canal).
Illegitimate, to be – to be a bastard, to be born on the wrong
side of the blanket, to get into trouble (unmarried pregnancy),
to have a natural child.
Male homosexual – bent*, a fag*, a faggot*, a fairy*, a nancy-boy*,
a pansy*, a pouf*, a poufter*, a queen*, a queer*, gay, kinky*.
Oral sex – blow job*, give head*, to go down on someone, rim-
ming*, sixty-nine* (mutual oral sex), to suck off.
Orgasm – climax.
To experience an orgasm: to come, to have a thrill. ‘When I
come.’ ‘When he’s finished.’
Sexual intercourse – intimacy, to do it, to fuck*, to get it with,
to get layed, to go with someone, to go to bed with someone,
to have it, to have sex, to knock up*, to make love, to perform,
to shag*, to roger, to screw*, to sleep with.
To have a regular sexual partner – to go steady. ‘We’re an item.’
To masturbate – to beat off*, to bring oneself off*, to fiddle*, to
jack off*, to jerk off*, to rub up*, to shag*, to shake*, to toss*,
to wank* (wanker: masturbator).
To neck – hug and kiss intimately.
To pet – kiss and caress extensively.
Sexual intercourse is often referred to as a normal married life
by older people. Note the negative use, such as ‘We can’t have a
COLLOQUIAL ENGLISH
135
C3996_06.qxd 25/02/2004 18:31 Page 135
normal married life’. Also, ‘He doesn’t trouble me’, meaning the
husband/partner does not demand sexual intercourse if the
woman does not want it. ‘He doesn’t bother about that sort of
thing’ implies a not very demanding partner. ‘He wants it too
often’ means a demanding one.
Phrases such as, ‘When I go with my husband’, When we have
it’, ‘When we have sex’, ‘When he does it’ are most commonly
used.
Family planning, contraception
Condom – briefs (short condoms), Durex (trade name often used
as a synonym), envelope, French letter, Johnny*, jolly bag*,
rubber*, sheath, skin.
Diaphragm – Dutch cap, cap.
Emergency contraception – morning after pill.
Female condom.
Intrauterine contraceptive devices (IUCDs) – the coil.
Oral contraceptive – the pill.
Assisted conception, fertility clinic
Frequency of sexual intercourse – ‘How often do you try for a
baby?’, ‘When and how often do you have intercourse?’
In vitro fertilisation (IVF) – test tube baby.
Tubal insufflation – I had my tubes blown.
Sexually transmitted (acquired) infections (STIs, SAIs)
Gonorrhoea – clap, gleet, morning drop, strain, tear, a dose, the
whites, to catch a cold.
Primary syphilis – bumps (African Caribbean).
Pubic lice – crabs, to be chatty*.
Seminal fluid – your husband’s fluid.
Sexual health centre/clinic – GUM clinic, special clinic, VD
clinic
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
136
C3996_06.qxd 25/02/2004 18:31 Page 136
Syphilis – bad blood, lues, pox, siff.
Expressions:
To have a double event (syphilis and gonorrhoea).
To piss pins and needles*.
Scalded (infected with gonorrhoea).
Expressions used by patients:
I’ve been to the GUM clinic.
I’ve picked up something.
I’m afraid I’ve got it.
I’ve caught (or got) something.
I’ve got a dose (gonorrhoea).
I’ve got a full house* (syphilis and gonorrhoea).
I’ve got genital warts.
I’ve got trouble down below.
I’ve noticed something odd.
I’ve got trouble with my meat*.
I’ve been after the girls (or men).
Note: ‘The whites’ may be used by women to mean any white
vaginal discharge.
African Caribbean individuals may use ‘scratch’ for irritate or
itch, e.g. ‘It scratches me’ means ‘It irritates and I want to scratch’.
Prostitutes (sex workers) may say, ‘I’m a business/working
girl’, ‘I’m on the game’.
The health professional in the sexual health clinic will ask:
‘Have you any discharge?’, ‘Does it irritate?’, ‘Do you have pain
when you pass water?’, ‘Have you any swelling?’, ‘Have you a
sore place?’, ‘Have you a rash?’.
GLOSSARY OF MEDICAL AND COLLOQUIAL NAMES
Medical name
Colloquial name
Alopecia
baldness
Arteriosclerosis
hardening of the arteries
Blepharitis
sore eyelids
COLLOQUIAL ENGLISH
137
C3996_06.qxd 25/02/2004 18:31 Page 137
Bursitis
housemaid’s knee, tennis elbow
(see epicondylitis)
Cancer
a growth, the big C, the worst,
tumour
Candidiasis; monilia
thrush
Cerebral palsy
to be spastic
Cerebrovascular accident stroke
Colic
gripes
Concussion
KO’d, to be concussed, to be
knocked out
Conjunctivitis
pink eye
Contusion
bruise
Convulsions
fits
Coronary thrombosis;
a coronary, heart attack
myocardial infarction
Coryza
cold
Dandruff
scurf
Delirium tremens
DTs, the jerks, the shakes
Diabetes mellitus
sugar diabetes
Dysmenorrhoea
painful periods
Dysphagia
difficulty swallowing
Dyspnoea
breathless, out of breath, panting,
puffed, short of breath
Dyspepsia
indigestion
Encephalitis
brain fever
Enuresis
bed-wetting
Epicondylitis
golfer’s elbow (medial side),
tennis elbow (lateral side)
Epistaxis
nosebleeds
Eructation
belching
Erythema pernio
chilblains
Flatulence, flatus
wind. Note: To belch (to send out
wind from stomach noisily),
to fart* (to send out wind from
anus)
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
138
C3996_06.qxd 25/02/2004 18:31 Page 138
Frequency
I keep wanting to go (to pass
urine)
Furuncle
boil
Gonorrhoea
clap
Haemorrhoids
piles
Halitosis
bad breath
Hernia
rupture
Herpes simplex
cold blister or sore
Herpes zoster
shingles
Hordeolum
stye
Hydrophobia
rabies
Hypertension
high blood pressure
Incontinence
leaky, not to be able to hold
one’s water or motions, to
have an accident
Infectious mononucleosis glandular fever
Influenza
flu
Leucorrhoea
whites
Menopause
the change (of life), the turn (of
life)
Menstruation
period(s)
Myopia
short-sight
Neuralgia
face ache
Nocturia
to get up at night (to pass water)
Oedema
dropsy, swelling
Osteoporosis
brittle bone disease
Parotitis (infectious)
mumps
Pediculosis capitis;
nits
head lice
Peritonsillar abscess
quinsy
Pertussis
whooping cough
Poliomyelitis
infantile paralysis, polio
Pruritus
itching
Pyrexia
fever, a high temperature
Pyrosis
heartburn, water-brash
COLLOQUIAL ENGLISH
139
C3996_06.qxd 25/02/2004 18:31 Page 139
Rheumatic disease
screws, springes, rheumatics
Rubella
German measles
Rubeola; morbilli
measles
Scarlatina
scarlet fever
Seizure
convulsion, fit
Strabismus
a squint
Syncope
fainting
Tachycardia
palpitations
Tendonitis
golfer’s elbow, tennis elbow
Tetanus
lockjaw
Tinea circinata
ringworm
Tinnitus
ringing in the ears
Tuberculosis
TB
Urticaria
heat spots, hives, nettle rash
Varicella
chickenpox
Verrucae
warts
Vesicle
blister
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
140
C3996_06.qxd 25/02/2004 18:31 Page 140
Idioms: parts of the
body
INTRODUCTION
The English language has thousands of idioms. By an ‘idiom’ we
mean a number of words which, when taken together, have a dif-
ferent meaning from that of each separate word.
The reason for including these idioms of parts of the body is
that, although you may never need to use them yourself, you
should be able to recognise them. You may be told by a person
that by the end of the day he is ‘on his knees’ and you must
realise that he is using the word ‘knee’ idiomatically. What he
means is that he is extremely tired after work and feels like
collapsing.
A woman may tell you of her worries and say she has just
managed to ‘keep her head above water’. If you are not familiar
with the idiom, you may think she has tried to save herself from
drowning but, in fact, she means that she is terribly short of
money and is having a struggle to keep out of debt.
Words and phrases connected with parts of the body have also
been included, such as ‘chesty’, ‘throaty’ and ‘to speak through
one’s nose’. It is essential that you understand these.
IDIOMS: PARTS OF THE BODY
Figures 7.1 to 7.3 are provided so you can familiarise yourself
with the words usually used in everyday conversation to describe
parts of the body.
Arm
A shot in the arm: something that does a person good.
141
7
C3996_07.qxd 25/02/2004 18:32 Page 141
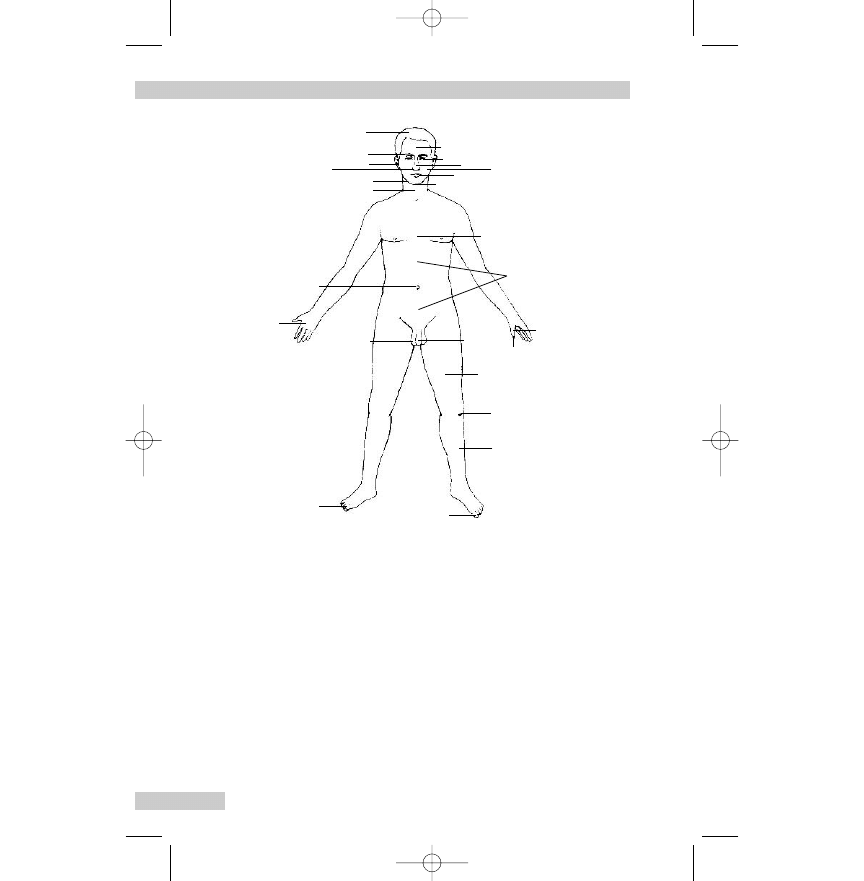
To give one’s right arm (usually with would): to be willing to
make a sacrifice to get something.
To keep someone at arm’s length: to avoid being friendly.
To stand by with folded arms: to do nothing when action seems
necessary.
To welcome someone with open arms: to greet warmly.
Back
To back a horse: to place money on a horse in a race, to bet.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
142
Jaw
Throat
Navel
Palm
Big toe
Toenail
Penis
Chest
Chin
Cheek
Nose
Eye
Forehead
Mouth
Thumb
*
*
Stomach
(meaning abdomen)
Scrotum
Knee
Thigh
Nail
Shin
Nostril
Ear
Eyebrow
Hair
(containing testes)
Fig. 7.1
Parts of the body (male front view). Reproduced with per-
mission from Parkinson, Manual of English for the Overseas Doctor,
5th edn. Churchill Livingstone, 1999.
C3996_07.qxd 25/02/2004 18:32 Page 142
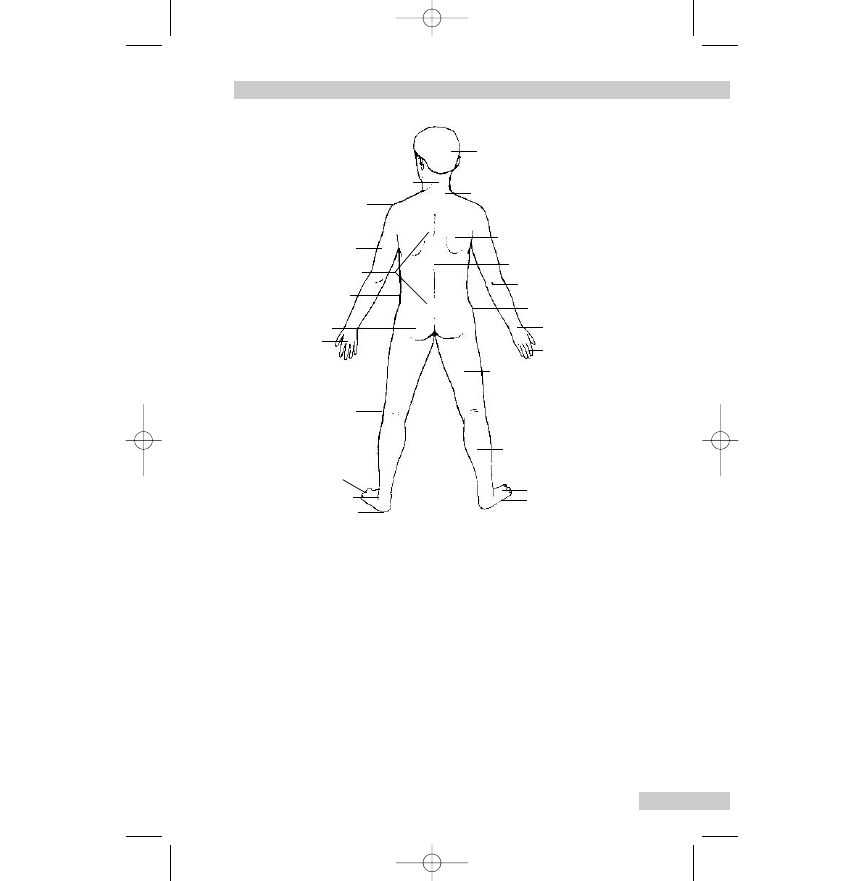
To back down: to be less demanding than before; to withdraw
one’s claim.
To back out: to withdraw from.
To back someone or something: to give one’s support.
To be on one’s back: to be ill in bed.
To break one’s back: to overwork.
To do something behind someone’s back: to act deceitfully.
To have one’s back to the wall: to be struggling against great
difficulties.
IDIOMS: PARTS OF THE BODY
143
Head
Neck
Nape
Shoulder
Arm
Back
Waist
Buttocks
Hand
Knee
Toes
Ankle
Heel
Shoulder blade
Spine
Elbow
Hip
Wrist
Fingers
Thigh
Calf
Instep
Foot
Fig. 7.2
Parts of the body (back view). Reproduced with permis-
sion from Parkinson, Manual of English for the Overseas Doctor, 5th
edn. Churchill Livingstone, 1999.
C3996_07.qxd 25/02/2004 18:32 Page 143
To put (get, set) someone’s back up: to make someone angry.
To see the back of someone/something: to get rid of someone/
something that is annoying, unpleasant.
To turn one’s back on: to abandon, to refuse to help.
Blood
A young blood: dashing young man.
Bad blood: ill feeling (between people, nations).
Blood is thicker than water: one’s own relations come before all
other people.
His blood is up: he is in a fighting mood.
His blood ran cold in his veins: he was filled with terror.
It is more than flesh and blood can stand: too much for human
beings to endure.
One’s own flesh and blood: one’s own family.
To do something in cold blood: deliberately; when one is not
angry.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
144
Groin
Armpit
Nipple
Vagina
(used to describe the
vulva or external genitals)
Breasts
Fig. 7.3
Parts of the body (female front view). Reproduced with
permission from Parkinson, Manual of English for the Overseas
Doctor, 5th edn. Churchill Livingstone, 1999.
C3996_07.qxd 25/02/2004 18:32 Page 144
To get blood out of a stone: to get pity from someone hard; to
achieve the impossible.
To get someone’s blood up: to provoke someone very much.
To have fresh, new blood: to have new members in a business,
family or society.
To make one’s blood boil: to make one very angry.
To run in the blood: to have an inherited quality.
Bone
A bone of contention: the subject of constant disagreement.
He will never make old bones: will not live to an old age.
To be all skin and bones: very thin.
To be bone dry: completely dry.
To be bone-idle: completely idle, lazy.
To bone up on: to study intensively.
To feel something in one’s bones: to feel quite sure about some-
thing intuitively.
To have a bone to pick with someone: to wish to complain about
something.
To make no bones about doing something: to have no hesitation
in doing something (usually unpleasant).
To work one’s fingers to the bone: to work very hard without
appreciation.
Brain
A brain-child: original idea of a person or group.
A brain drain: movement of trained and qualified workers to
other countries (usually for better conditions).
A brainstorm: cerebral disturbance; a mental aberration.
A brainstorming session: a method of solving problems in which
many people suggest ideas which are then discussed.
A brain-teaser: problem, puzzle.
A brainwave: a sudden inspiration or clever idea.
A scatter-brained person: a careless, forgetful person.
IDIOMS: PARTS OF THE BODY
145
C3996_07.qxd 25/02/2004 18:32 Page 145
Brain-fag: mental exhaustion.
Brain fever: encephalitis.
Brainwashing: forcing someone to change his beliefs by use of
extreme mental pressure.
Brainless: foolish, stupid.
Brainy: clever.
To blow one’s brain out: to shoot oneself in the head.
To have something on the brain: to be obsessive about something.
To pick someone’s brains: to find out someone’s good ideas and
use them.
To rack one’s brains: to think very hard; to solve a problem or
remember something.
Breast
To make a clean breast of something: to confess everything.
Brow (forehead), Brows (arch of hair above eyes)
A high-brow: someone interested in intellectual matters and
culture.
A low-brow: someone showing little interest in intellectual matters
and culture.
To browbeat someone into doing something: to intimidate some-
one with severe looks and words, to bully.
To knit one’s brows: to frown.
Cheek
Cheek: disrespectful speech, impudence.
Cheeks: buttocks.
To be cheeky: to be disrespectful, impudent.
To cheek someone: to speak impudently to someone.
To have the cheek to do something: to be bold, rude enough to do
something.
To turn the other cheek: to refuse to retaliate.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
146
C3996_07.qxd 25/02/2004 18:32 Page 146
Chest
To be chesty: to have trouble with one’s lungs.
To cock one’s chest: to boast about oneself.
To get something off one’s chest: to free one’s mind by speaking
about something that was troubling one.
Get that across your chest!: Eat that! (usually a large, nourishing
meal). Slang.
To puff one’s chest out: to be proud of oneself.
Chin
A chin: a talk.
Chin up: be brave.
To be up to the chin in work, etc.: to have too much work to do.
To chin: to talk, to gossip.
To have a chin-wag: to talk with friends about unimportant mat-
ters, to chatter.
To keep one’s chin up: to be brave, to be cheerful in the face of
difficulties.
To take something on the chin: to suffer severe difficulties with
courage.
Ears
In at one ear and out at the other: ignored or quickly forgotten
advice.
To be all ears: to listen very carefully.
To be up to one’s ears in: deeply involved or occupied in.
To box someone’s ears: to smack someone on the ears.
To come to one’s ears: to hear a rumour.
To earmark: to put someone/something aside for a special
purpose.
To fall on deaf ears: to pass unnoticed.
To give one’s ears for something: to be prepared to do anything to
get what one desires.
IDIOMS: PARTS OF THE BODY
147
C3996_07.qxd 25/02/2004 18:32 Page 147
To have a person’s ear: to have the favourable attention of
someone.
To have a word in someone’s ear: to speak in private.
To keep one’s ear to the ground: to listen carefully.
To play it by ear: to do what seems best at the time.
To prick up one’s ears: to have one’s attention suddenly aroused.
To send someone away with a flea in his ear: to criticise someone
severely so that he goes away unhappily.
To set people by the ears: to cause them to quarrel.
To turn a deaf ear: to ignore, pretend not to hear.
Elbow
Elbow-grease: vigorous polishing; hard physical work.
Elbow-room: plenty of room to move freely.
Out-at-elbows: of a coat, worn out; of a person, poor.
To elbow one’s way through a crowd: to push with one’s elbows.
To raise the elbow: to drink too much.
Eye
A blue-eyed boy: a pet, a favourite.
A sight for sore eyes: someone or something very welcome,
pleasant.
An eye for an eye: to punish those who hurt us.
An eye-opener: an event or piece of news which causes surprise.
An eyesore: a very unpleasant thing to look at.
Eyeball to eyeball: face to face with someone.
Eye contact: looking directly into another person’s eyes.
Eye-opener: an enlightening experience.
Eye-wash: lotion for bathing eyes; words or actions intended to
mislead.
Green-eyed: jealous.
In the eyes of: in the opinion of.
In the mind’s eye: imagining in the mind.
In the public eye: to be watched by the public constantly.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
148
C3996_07.qxd 25/02/2004 18:32 Page 148
The apple of one’s eye: someone or something very precious.
To be up to the eyes in work: to have far too much work to do.
To catch someone’s eye: to attract someone’s attention.
To cry one’s eyes out: to weep very much.
To do something with one’s eyes open: to act knowing the results
of the action.
To eye someone: to look at carefully, admiringly, jealously, etc.
To get (or give) a black eye: to receive (or give) a blow on the eye
so that the skin around it goes black.
To give someone the glad eye: to encourage someone to be
amorous.
To have an eye for: to have a liking or ability to do something; to
have good judgement on something.
To have an eye on/to the main chance: to think and work with
one’s own advantage always in view.
To have half an eye on: not to give something one’s full attention.
To have one’s eyes opened: to be forced to see reality.
To keep an eye on someone/something: to watch carefully.
To keep one’s eye open for: to watch carefully.
To keep one’s eyes skinned: to be very watchful.
To make eyes at someone: to look at someone (usually of the
opposite sex) with open admiration and invitation.
To pull the wool over someone’s eyes: to try to hide the truth from
someone.
To run one’s eye over: to look quickly at, to glance at.
To see eye to eye with someone: to agree; to have the same ideas.
To turn a blind eye: to ignore deliberately, pretend not to see.
Face
Face-ache: neuralgia.
Let’s face it: let’s be honest with each other.
To be a slap in the face: a sudden disappointment, rejection.
To face the music: to face criticism/punishment as a result of one’s
own actions.
To face up to something: to meet courageously (usually difficulties).
IDIOMS: PARTS OF THE BODY
149
C3996_07.qxd 25/02/2004 18:32 Page 149
To fly in the face of convention, rules, etc.: to defy, disobey
openly.
To have a face as long as a fiddle: to look depressed.
To keep a straight face: not laugh. (Often used negatively, e.g. ‘I
couldn’t keep a straight face’.)
To look someone in the face: to look directly at someone.
To lose face: to be humiliated, to be put to shame.
To make/pull a face: to grimace.
To pull a long face: to look depressed, disappointed, displeased.
To put a brave/good face on it: to behave as if circumstances are
better than they really are.
To put one’s face on: to apply cosmetics to one’s face.
To save one’s face: to try to avoid shaming oneself openly.
To set one’s face against: to oppose.
To show one’s face: to appear, be seen.
To stare one in the face: something that is obvious, clear to see.
Feet – see Foot
Fingers
Not to raise (lift, stir) a finger to help someone: to refuse to be of
any help.
One’s fingers itch to do something: one wishes very much to do
something.
To be all fingers and thumbs: to be clumsy with one’s hands often
due to nervousness.
To be light-fingered: to steal easily.
To burn one’s fingers: to get into trouble by interfering in other
people’s affairs.
To finger: to touch.
To get/pull one’s finger out: to stop being lazy, work harder
(slang).
To have a finger in every pie: to be involved in many activities.
To have butter fingers: to let things slip out of the hands.
To have something at one’s fingertips: to know perfectly.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
150
C3996_07.qxd 25/02/2004 18:32 Page 150
To keep one’s fingers crossed (for someone): hope for luck with a
problem or difficulty.
To lay/put one’s finger on something: to realise the most important
aspect of a matter.
To let something slip through one’s fingers: to lose hold of, allow
to escape (usually of opportunities).
To twist a person round one’s finger: to have someone in one’s
power so that they do all one wishes.
Flesh
Flesh wound: one not reaching bone or a vital organ.
One’s own flesh and blood: one’s own family.
Proud flesh: new flesh coming from a wound.
Sins of the flesh: sexual sins.
To be neither fish nor flesh: to be of indefinite character.
To have one’s pound of flesh: to insist cruelly on repayment.
To lose flesh: to get thinner.
To make one’s flesh creep: to be terrified so that one’s skin seems
to move.
To put on flesh: to get fatter.
To see someone in the flesh: actually to see someone.
Foot, feet
My foot!: Nonsense! Rubbish!
Not to let the grass grow under one’s feet: to act quickly when one
has made a decision.
To be on one’s feet: to be in reasonable health; to be standing.
To be run off one’s feet: to be so busy one cannot sit down.
To dog one’s footsteps: to follow one constantly and so cause
irritation.
To drag one’s feet: to be slow to take action.
To fall on one’s feet: to be lucky.
To fall over one’s feet to be kind, helpful, etc.: to make a great
effort to be kind, helpful, etc.
IDIOMS: PARTS OF THE BODY
151
C3996_07.qxd 25/02/2004 18:32 Page 151
To find one’s feet: to be comfortably settled in a new job, situa-
tion, etc.
To foot the bill: to pay.
To get cold feet: to be afraid, discouraged.
To go on foot: to walk.
To have one foot in the grave: to be very ill, close to death.
To have one’s feet on the ground: to be practical, sensible.
To have the world at one’s feet: to be very successful.
To put one’s best foot forward: to walk quickly, to work quickly.
To put one’s feet up: to relax, to rest.
To put one’s foot down: to be firm, to protest.
To put one’s foot in it: to do or say something that causes anger,
trouble.
To set someone on his feet: to help, usually with money, to start a
business, etc.
To stand on one’s own feet: to be independent.
To step off on the wrong foot: to start something in the wrong way.
Hair
A hair’s breadth: a very small distance.
Hair-raising (stories): terrifying.
Not turn a hair: to show no sign of fear or emotional upset.
To a hair: exactly (usually of weight).
To get in a person’s hair: to annoy, irritate someone.
To have one’s hair standing on end: to be terrified.
To have someone by the short hairs: to have control over them.
To keep one’s hair on: not to grow angry.
To let down one’s hair: to act freely, to be uninhibited.
To split hairs: to argue about very small, unimportant differences.
Hand
A right-hand man: someone who can be relied on for help and
advice.
At first hand: directly.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
152
C3996_07.qxd 25/02/2004 18:32 Page 152
Hands off!: Do not touch.
Hands-on experience: involving active participation.
Never to do a hand’s turn: never make the slightest effort.
To be a handful: to be difficult to control.
To be an old hand at something: to be experienced.
To be hand-in-glove with someone: to be extremely friendly (usu-
ally planning something together).
To be high-handed: to be arrogant.
To be offhand: to be abrupt in manner, casual.
To be off one’s hands: to no longer be responsible for someone
or something.
To be open-handed: to be generous with money.
To be out of hand (of children, a situation, etc.): to be out of
control.
To be underhand: to be deceitful, dishonest, not open.
To eat out of someone’s hand: to do whatever one wishes.
To force someone’s hand: to make someone do something.
To get one’s hand in: to get to know how to do something.
To give/lend someone a hand: to help someone physically.
To give someone a free hand: to allow someone to do as he
wishes.
To hand: to give, to offer.
To have a hand in something: to share in the activity.
To have one’s hands full: to be extremely busy.
To have one’s hands tied: to be unable to act in the way one
wishes.
To have the upper hand over someone: to dominate.
To have time on one’s hands: to have plenty of free time.
To keep one’s hand in: to be in practice.
To lay hands on: to seize, touch (often used negatively).
To live from hand to mouth: to live from day to day; without reg-
ular money.
To play into someone’s hands: to do something which helps one’s
opponent.
To rule with a heavy hand: to rule severely.
To say offhand: to give an answer immediately from memory.
IDIOMS: PARTS OF THE BODY
153
C3996_07.qxd 25/02/2004 18:32 Page 153
To take one’s courage in both hands: to force oneself to do some-
thing difficult, unpleasant.
To take someone in hand: to try to improve someone’s
behaviour.
To try one’s hand at something: to make an attempt to do some-
thing new.
To wait on someone hand and foot: to attend to someone’s needs
with great care.
To wash one’s hands of someone/something: to have nothing more
to do with.
Head
A headache: a pain in the head; a difficult problem; a trouble-
some person.
From head to foot/toe: completely; all over the person.
It is on his head: he is responsible for it.
Not to know whether one is standing on one’s head or one’s heels:
to be in a state of extreme confusion.
To be above/over one’s head: too difficult to understand.
To be big-headed: to be conceited.
To be block-headed: to be dull, stupid.
To be fat-headed: to be stupid.
To be hard-headed: to be practical, unsentimental.
To be head and shoulders above others: to be much taller; to be
far better.
To be head over heels in love: completely, very much in love.
To be hot-headed: to be hasty, impulsive.
To be pig-headed: to be obstinate.
To be soft-headed: to be simple-minded.
To be touched in the head: to be slightly mad.
To bite a person’s head off: to speak sharply, angrily to someone.
To bury one’s head in the sand: to avoid facing facts by pretend-
ing not to see them.
To come to a head: to reach a crisis.
To eat one’s head off: to eat an excessive amount.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
154
C3996_07.qxd 25/02/2004 18:32 Page 154
To get one’s head down: to go to bed.
To get something into one’s head: be convinced that something
is true.
To go off one’s head: to become crazy, mad.
To go to one’s head: to make one excited, to intoxicate one.
To have a good head for business: to have a natural aptitude for it.
To have a good head-piece: to have plenty of brains.
To have a head: to have a headache, often from drinking too
much.
To have a head like a sieve: to be very forgetful.
To have an old head on young shoulders: to be wise beyond
one’s years.
To have one’s head screwed on the right way: to be intelligent, full
of common sense, especially in practical matters.
To have something hanging over one’s head: to have some danger,
something unpleasant going to happen soon.
To head off: to divert a person from someone or something.
To heap coals of fire on a person’s head: to treat a person well
who has treated oneself badly.
To hit the nail on the head: to guess right, to reach the correct
conclusion.
To keep one’s head: to stay calm in a difficult situation.
To keep one’s head above water: to keep out of debt.
To knock on the head: to destroy, disrupt an idea, plan, etc.
To knock/run one’s head against a stone wall: to do something
that will fail, because of opposition.
To let someone have his head: to let him do as he wishes.
To lose one’s head: to lose one’s self-control in a difficult situation.
To make head, headway: to make progress.
To make head or tail of something: to understand it. (Usually used
negatively, e.g. ‘I couldn’t make head or tail of the letter he
sent me’.)
To put something out of one’s head: to forget it deliberately, to
stop thinking about it.
To put things into someone’s head: to suggest things to him.
To take it into one’s head: to make a sudden decision.
IDIOMS: PARTS OF THE BODY
155
C3996_07.qxd 25/02/2004 18:32 Page 155
To talk someone’s head off: to talk so much that the other person
is weary.
Two heads are better than one: two people know more together
than one person alone.
Heart
After one’s own heart: a person sharing one’s own interests,
opinions.
At heart: basically, deep down.
Have a heart!: Be reasonable; don’t be unkind!
Heartache: deep sorrow, grief.
Heartburn: pain in chest as a result of indigestion, pyrosis.
Heart-felt sympathy: deepest sympathy.
Heart-searching: doubts, uncertainties.
In one’s heart of hearts: deep down in oneself.
Not to have the heart to do something: not to have the courage to
do something.
The heart of the matter: the essence, the vital part.
To be downhearted: to be depressed.
To be good at heart: to be good basically.
To be half-hearted about something: not to be very enthusiastic.
To be hard-hearted: to be hard, unkind.
To be heartless: to be unkind, unsympathetic.
To be hearty: to be cheerful.
To be in good heart: to be cheerful, confident.
To be lion-hearted: to be very brave.
To be soft-hearted: to be kind, sympathetic.
To be stout-hearted: to be very brave.
To break one’s heart: to be overwhelmed with sorrow.
To cause heartache: to cause suffering.
To cry one’s heart out: to cry excessively.
To eat one’s heart out: to fret, worry excessively.
To have a big heart: to be warm, generous.
To have a heart: to have trouble with one’s heart.
To have a heart-to-heart talk with someone: to speak openly, hid-
ing nothing.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
156
C3996_07.qxd 25/02/2004 18:32 Page 156
To have a hearty appetite: to have a very good appetite.
To have no heart: to be hard, insensitive.
To have no heart for something: to have no enthusiasm for
something.
To have one’s heart in one’s boots: to be depressed, to feel
hopeless.
To have one’s heart in one’s mouth: to be very afraid.
To know/learn/ say by heart: to know/learn/say something word
for word by memory.
To lose heart: to have no hope, to become discouraged. (Often
used negatively, e.g. ‘Don’t lose heart: keep on hoping’.)
To lose one’s heart: to fall in love.
To put one’s heart into something: to do something with
enthusiasm.
To set one’s heart on something: to want something very much.
To take heart: to become more hopeful.
To take someone to one’s heart: to feel deep affection for someone.
To take something to heart: to be upset; to worry too much about
things.
To tear one’s heartstrings: to hurt one very deeply.
Whole-hearted: complete, without doubts.
Heel(s)
A heel: a completely unreliable person.
An/one’s Achilles heel: weak or vulnerable point, especially of
character.
Not to know whether one is standing on one’s head or one’s heels:
to be in a state of extreme confusion.
To be down at heel: poorly dressed and in a state of poverty.
To be head over heels in love: completely, very much.
To bring someone to heel: to put them under control.
To carry with the heels first: as a dead body.
To come on the heels of: to follow immediately.
To kick one’s heels: to stand waiting idly, impatiently.
To leave to cool his heels: to make someone wait deliberately.
IDIOMS: PARTS OF THE BODY
157
C3996_07.qxd 25/02/2004 18:32 Page 157
To show a clean pair of heels: to run away.
To take to one’s heels: to run away.
Knee
To be knee-deep in something: deeply involved in.
To be on one’s knees: to kneel, especially when praying; to be
completely exhausted.
To bring someone to his knees: to make him submit, stop fighting.
To go down on one’s knees to someone: to beg for something.
To have a knees-up: a very lively party.
Knuckles
To knuckle down to a job: to work as hard as one can.
To knuckle under: to accept defeat.
To rap someone’s knuckles: to reprimand.
Lap (waist to knees of one sitting)
In the lap of the gods: uncertain future.
In the lap of luxury: in great comfort and luxury.
Leg
A blackleg: a person who continues working when others are on
strike.
Not to have a leg to stand on: have no good reason to support
one’s argument.
The boot is on the other leg: the truth is the opposite of what one
believes.
To be on one’s last legs: to be close to death; utterly weary.
To find one’s legs: to be able to stand and walk (usually after an
illness).
To get one’s sea legs: to become used to the movement of a ship.
To give someone a leg up: to help someone.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
158
C3996_07.qxd 25/02/2004 18:32 Page 158
To pull someone’s leg: to tease someone.
To show a leg: to get out of bed.
To stretch one’s legs: to go for a walk.
To walk someone off his legs: to tire him out with walking.
Lip
Lip: impudence, saucy talk.
None of your lip!: ‘Don’t speak to me like that!’
Lip-language, -reading, -speaking: use of the movement of the
lips to and by the deaf and dumb.
A word escapes one’s lips: something is said without thought.
To bite one’s lip: to hide emotion, to stop oneself from saying
something.
To curl one’s lip: to show scorn.
To hang on someone’s lip: to listen with great care.
To have sealed lips: to be silent about something.
To keep a stiff upper lip: to bear troubles without showing
emotion.
To lick one’s lips: to show appreciation of food (or sometimes
other things).
To pay lip service to principles, etc.: to say one believes in some-
thing but not to act accordingly.
Mind
Mind: memory, remembrance.
Mind-blowing: (of drugs, etc.) causing ecstasy, excitement; (of
news) confusing, shattering.
Mind-boggling: astonishing, extraordinary; overwhelming.
Never mind: ‘It doesn’t matter; don’t worry’.
To be not in one’s right mind: to be mad.
To be out of one’s mind: to be mad.
To bear something in mind: to remember.
To bend someone’s mind: to influence the mind so that it is per-
manently affected.
IDIOMS: PARTS OF THE BODY
159
C3996_07.qxd 25/02/2004 18:32 Page 159
To give someone a piece of one’s mind: to speak openly and
critically.
To go out of one’s mind: to go mad, e.g. ‘He went out of his mind
in the end’; to be forgotten, e.g. ‘I’m so sorry. It went out of
my mind’.
To have a lot on one’s mind: to be worried about many things.
To have presence of mind: to act and think quickly in
emergencies.
To know one’s own mind: to be definite about what one wants.
To make up one’s mind: to decide.
To mind: (a) To be careful (used very often in orders): ‘Mind the
step’ – be careful of the step; ‘Mind the car’ – get out of the
way of the car. (b) To care (often used negatively): ‘I don’t
mind what she does or says’. (c) To object (used mainly inter-
rogatively and negatively): ‘I don’t mind going to hospital to
have my baby’. Note the polite request: ‘Would you mind’ +
-ing form of the verb: ‘Would you mind lying on the bed?’. (d)
To take care of: ‘She had no one to mind the baby when she
went to work’. Noun: a baby-minder.
To mind one’s own business: not to interfere in the affairs of
other people.
To mind one’s p’s and q’s: to be careful what one says and does.
To mind out for: avoid.
To take a load/weight off someone’s mind: give great relief.
Mouth
Mouth: impudent talk, rudeness.
To be down in the mouth: to be depressed.
To look as if butter would not melt in one’s mouth: to look inno-
cent, incapable of badness.
To make one’s mouth water: to cause saliva to flow at the sight
of food.
To put words into someone’s mouth: to tell someone what to say.
To take the words out of someone’s mouth: to say what someone
was about to say.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
160
C3996_07.qxd 25/02/2004 18:32 Page 160
Nail(s)
(Note: Several idioms are listed which refer to other meanings of
the word ‘nail’ than the nail of the body. They have been included
because they are all commonly used and you should be familiar
with them.)
Nail-biting: causing anxiety or tension.
To be as hard as nails: to be very tough; merciless.
To be as right as nails: to be perfectly fit.
To fight tooth and nail: to fight fiercely, vigorously.
To hit the nail on the head: to say the right thing, to guess right.
To nail someone down: to make someone give a definite state-
ment; details.
To pay on the nail: to pay at once.
To put a nail in one’s coffin: to do something that will shorten
one’s life.
Neck
Neck: boldness, disrespect, impertinence.
Neck or nothing: desperately risking everything for success.
Stiff-necked: obstinate, proud, stubborn.
To be a pain in the neck: to be a nuisance and pest to someone.
To be up to the neck in debt, work: to be completely immersed in
debt, work.
To break one’s neck to do something: work extremely hard to do
something.
To get it in the neck: to be severely punished.
To have the neck to do something: to be rude enough to do
something.
To neck: to hug and kiss someone intimately.
To run neck and neck: to be level with someone in a competition.
To save one’s neck: to save oneself from punishment.
To stick one’s neck out: to act or speak in a way which exposes
one to harm or criticism.
To talk out of the back of one’s neck: to talk nonsense.
IDIOMS: PARTS OF THE BODY
161
C3996_07.qxd 25/02/2004 18:32 Page 161
To throw someone out neck and crop: to throw someone out head
first, bodily.
Nerve(s)
Nerve-racking: frightening, stressful.
Not to know what nerves are: to have a calm temperament.
To be a bundle of nerves: in a very nervous state.
To get on one’s nerves: to annoy or irritate very much.
To have a fit of nerves: to be in a nervous state.
To have iron/steel nerves: not to be easily upset or frightened.
To have the nerve to do something: to be brave, to be impudent
enough.
To lose one’s nerve: to become frightened and unsure of oneself.
To nerve oneself to do something: to use all one’s strength, mental
and physical.
To strain every nerve: to make a great effort.
What a nerve!: What impudence!
Nose
To cut off one’s nose to spite one’s face: to do something in anger
to hurt someone else which also hurts oneself.
To follow one’s nose: to go straight on, to act on instinct.
To get up a person’s nose: to annoy someone.
To have a good nose: to have a good sense of smell.
To keep one’s nose to the grindstone: to work hard over a long
period.
To lead someone by the nose: to make someone do anything one
wishes.
To look down one’s nose at someone: to regard someone as
inferior.
To nose about: to look enquiringly everywhere.
To pay through the nose: to pay an excessive price.
To poke one’s nose into something: to try to find out about people
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
162
C3996_07.qxd 25/02/2004 18:32 Page 162
and things which do not concern one.
To put someone’s nose out of joint: to do something to irritate or
upset someone.
To see no further than one’s nose: not to be able to imagine the
future or any situation other than the current one.
To speak through one’s nose: to speak with a nasal sound (often
as a result of adenoids).
To turn up one’s nose: to show dislike or disapproval.
Palm
To grease someone’s palm: to bribe him, offer money for informa-
tion, etc.
To palm something off on someone: to sell something that is
worthless or damaged.
Shoulder
A shoulder to cry on: someone who listens to one’s problems
with sympathy.
Shoulder to shoulder: with united effort.
Straight from the shoulder: a strong blow or strong criticism of
someone.
To cold-shoulder someone: to ignore someone deliberately; treat
coldly.
To have a chip on one’s shoulder: to go around with a sense of
grievance.
To have an old head on young shoulders: a young person who is
wise beyond his age.
To have broad shoulders: to be strong; to be able to bear
responsibility.
To put one’s shoulder to the wheel: to make a great effort to do
something.
To rub shoulders with: to mix with people.
To shoulder (a burden or the blame): to carry.
IDIOMS: PARTS OF THE BODY
163
C3996_07.qxd 25/02/2004 18:32 Page 163
Skin
A skinflint: a mean, miserly person.
A skinhead: a member of a group of young people who have
closely cut hair, strange clothes and are often violent.
Skin-deep (of beauty, emotion, wound): no deeper than the skin,
not lasting, on the surface.
To be skin and bone: very thin.
To be thick-skinned: not to care what others say about one,
insensitive.
To be thin-skinned: to be too sensitive to what others say.
To escape by the skin of one’s teeth: to have a narrow escape.
To get under one’s skin: to annoy intensely, to hold one’s interest
very much.
To jump out of one’s skin: to be startled, frightened suddenly.
To keep one’s eyes skinned: to be watchful.
To save one’s skin: to avoid or escape from danger.
To skin: for a wound to be covered with new skin; to remove skin
from something.
Skull
Thick-skulled: dull, stupid person.
To get something into one’s skull: to understand and remember it.
Stomach
To have a strong stomach: ability not to feel nausea; can eat
anything.
To have butterflies in the stomach: to have fluttery feelings in the
stomach due to nervousness.
To stomach something: accept. (Usually in negative form, e.g. ‘He
cannot stomach her ways’, meaning he cannot bear them.)
To turn one’s stomach: cause nausea; cause someone to be
disgusted.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
164
C3996_07.qxd 25/02/2004 18:32 Page 164
Teeth – see Tooth
Throat
Cut-throat competition: fierce, intense struggle in business.
Throaty: guttural, spoken in the throat.
To cut one’s own throat: to act in a way that harms oneself; to kill
oneself.
To have a frog in one’s throat: hoarseness or loss of voice.
To have a lump in one’s throat: to feel choked with emotion so
that one can hardly speak.
To have a throat: to have a sore throat.
To have words stick in one’s throat: to be too embarrassed by
something to be able to speak of it.
To jump down someone’s throat: to speak angrily to someone.
To thrust something down someone’s throat: to try to make some-
one accept one’s own beliefs, views, etc.
Thumb
Thumbs up!: mark of victory, satisfaction.
To be under someone’s thumb: to be dominated by someone.
To thumb a lift: to sign with the thumb to ask a motorist for a
free lift.
To twiddle one’s thumbs: to have to sit still and do nothing.
Toe(s)
From top to toe: from head to foot, completely.
To be on one’s toes: to be ready for action, alert.
To step/tread on someone’s toes: to annoy someone unwittingly
(often by doing what they want to do).
To tiptoe: to walk on the tips of one’s toes; to walk quietly.
To toe the line: to obey the rules, of a party, society, etc.
To turn up one’s toes: to die.
IDIOMS: PARTS OF THE BODY
165
C3996_07.qxd 25/02/2004 18:32 Page 165
Tongue
A slip of the tongue: a mistake made when speaking.
Tongue: language (e.g. one’s mother tongue, meaning one’s
native language).
To be tongue-tied: to be too shy, too nervous to speak.
To have a dangerous tongue: to speak maliciously.
To have a long tongue: to be talkative.
To have a ready tongue: to speak easily, fluently.
To have something on the tip of one’s tongue: to be about to say
something and then forget it.
To hold one’s tongue: to be silent.
To lose one’s tongue: to be too shy to speak.
To put out one’s tongue: grimace to mark displeasure; for doctor’s
inspection.
To speak with one’s tongue in one’s cheek: to say something that
is not true in order to joke with someone.
To wag one’s tongue: to talk indiscreetly, to gossip.
Tooth, teeth
In the teeth of evidence, opposition, wind, etc.: against it.
Teething troubles: difficulties in the first stages of something.
To be armed to the teeth: to be fully armed with many weapons.
To be fed up to the back teeth with something: to be bored by,
tired of.
To be long in the tooth: to be old.
To cast something in someone’s teeth: to blame him for it.
To cut a tooth: a new tooth begins to show above the gum (of
babies and children).
To cut one’s eye-teeth: to gain worldly wisdom, maturity.
To cut one’s wisdom teeth: (as to cut one’s eye-teeth).
To escape by the skin of one’s teeth: to have a narrow escape.
To fight tooth and nail: to fight with all one’s strength.
To get one’s teeth into something: to make an enthusiastic start on
a job, etc.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
166
C3996_07.qxd 25/02/2004 18:32 Page 166
To have a sweet tooth: to enjoy eating sweet things.
To set one’s teeth on edge: to cause an unpleasant feeling in the
teeth; to cause disgust.
To show one’s teeth: to become aggressive.
To take the bit between one’s teeth: to reject the advice and con-
trol of others.
IDIOMS: PARTS OF THE BODY
167
C3996_07.qxd 25/02/2004 18:32 Page 167
C3996_07.qxd 25/02/2004 18:32 Page 168
This page intentionally left blank
Phrasal verbs
INTRODUCTION
‘Phrasal verb’ is a name given to those combinations of verb plus
preposition or adverbial particle from which we have now hun-
dreds of phrases to describe everyday events and activities.
The most commonly used phrasal verbs are formed from the
shortest and simplest verbs in the English language such as come,
do, get, go, make, put, take, followed by words such as down,
from, in, out, up, to. A phrasal verb consists of two (sometimes
three) parts and it is essential to consider the parts together, for
the combination often makes a different meaning. Some phrasal
verbs have several meanings.
Those who study the English language as a second language
have great difficulty in understanding and using phrasal verbs
correctly. For this reason a whole chapter is given to them. It is
quite impossible to follow everyday speech without a knowl-
edge of phrasal verbs, because we use them in preference to
more formal words. To take some examples: we talk about ‘get-
ting up’ in the morning and ‘putting on our clothes’ rather than
‘rising’ and ‘dressing’.
Nurses, doctors and other health workers must use language
understood easily by their patients, so they ask, for example,
‘When did the pain first come on?’ meaning the onset of pain, or
say ‘I want you to cut down on fatty foods’, meaning to reduce
intake. The examples given here are mostly taken from healthcare
situations and so will be invaluable to you.
169
8
C3996_08.qxd 25/02/2004 18:34 Page 169
BREAK
— Break down:
i. collapse mentally or physically, often due to stress. Nurse
Foster worked too many double shifts and eventually her
health broke down.
ii. cry with grief, shock, etc. If I talk about losing my baby, I
break down.
iii. fail to work because of electrical, mechanical, etc., fault.
The cardiac imaging system has broken down.
iv. fail, discontinue. Negotiations over the ambulance work-
ers’ pay dispute have broken down.
— Break in: enter somewhere by force. I could never sleep alone
in the house after burglars broke in.
— Break out: sudden start of disease, fire, violence, war. Food
poisoning broke out in the care home.
— Break out in something: suddenly become covered in. (a)
Whenever I eat strawberries I break out in a rash. (b) I keep
waking up and breaking out in a cold sweat.
— Break through: make a major discovery or advance. The
pharmaceutical company hopes to break through with a new
treatment for Alzheimer’s disease.
— Break up: deteriorate (of health). He’s breaking up under the
strain of nursing his wife.
— Break something up: come to end (of relationships). I’ve
been ill ever since my marriage broke up.
— Break with: end relations with someone. My son has broken
with us since he mixed with this group.
BRING
— Bring something about: cause something to happen. Drug
misuse brought about his death.
— Bring something back: call to mind. Talking to you brings
back memories of my childhood.
— Bring someone back to something: restore. A complete
change will bring you back to health.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
170
C3996_08.qxd 25/02/2004 18:34 Page 170
— Bring someone down: defeat, degrade. Heavy drinking
brought him down.
— Bring something down: lower, reduce. Reducing your
weight will help to bring down the cholesterol levels in your
blood.
— Bring something on: cause. It would help me to know what
brings on your chest pain.
— Bring someone round: restore to consciousness. The patient
was brought round by mouth-to-mouth ventilation.
— Bring someone through: save someone’s life. Her husband
was critically ill but the doctors and nurses struggled all night
to bring him through and he survived.
— Bring someone to: restore to consciousness.
— Bring someone up: rear, teach a child social habits (often
used in the passive). His mother died when he was two so he
was brought up by his grandmother. (Note: To be well brought
up. To be badly brought up.)
— Bring something up:
i. vomit. She’s not well. She brought up her lunch today.
ii. eructation. Do you bring any wind up?
COME
— Come about: happen. How did the accident come about? He
slipped on a wet floor.
— Come across: make an impression of a particular kind. She
comes across as a very nervous woman.
— Come across someone/something: find, meet or see unex-
pectedly. I’ve never come across such a bad case of shingles
before.
— Come along: make progress. You’re coming along nicely. We
shall have you walking without crutches next week.
— Come back: return. (a) Make an appointment to come back
in a month. (b) The stress symptoms have come back since I
went back to work.
— Come back to someone: return to memory. Yes, what hap-
PHRASAL VERBS
171
C3996_08.qxd 25/02/2004 18:34 Page 171
pened is all coming back to me now. I remember falling down
the steps.
— Come by something: get, obtain. How did you come by that
scar on your cheek? I was in a fight and someone threw a bot-
tle at me.
— Come down (of prices, temperature, etc.): be lowered, fall.
Your blood pressure has come down since we started you on
the tablets.
— Come down on someone: criticise someone, punish. The
police come down heavily on people found with class A
drugs.
— Come down with something: become ill with something. She
came down with flu and was unable to keep her appointment.
— Come forward: present oneself, with help, information, etc.
Will anyone who saw the accident please come forward?
— Come from: have as one’s birthplace (not used in the contin-
uous tenses). Where do you come from? I come from India.
— Come in:
i. be admitted to hospital. We’d like your mother to come in
so we can do one or two tests.
ii. be introduced, begin to be used. More people were treated
quicker and better when day surgery and keyhole surgery
came in.
— Come off something: fall from a bicycle, horse, etc. My son
came off his motor bike and broke his left leg.
— Come on:
i. encourage someone to hurry, make an effort, try harder
(used in imperative only). Come on Mr Hopkins. Let’s see
you walk across the room now.
ii. grow, make progress. Good. Your baby’s coming on very
well.
iii. start (of symptoms, etc.) Tell me exactly when these panic
attacks first came on.
— Come out:
i. be published. When’s your new book coming out?
ii. become known. It’s just come out that they are closing
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
172
C3996_08.qxd 25/02/2004 18:34 Page 172
down the factory and I shall lose my job.
iii. publicly acknowledge one’s homosexuality. John and
Simon have come out.
iv. stop work, strike. Do you think health professionals should
come out for better working conditions?
— Come out in something: be partially covered in rash, spots,
etc. Her hands came out in a rash after she used a new
detergent.
— Come over: begin to feel dizzy, faint, etc. It’s happened twice
now travelling home from work. I came over faint.
— Come round: regain consciousness. Your son hasn’t come
round yet from the anaesthetic.
— Come through something: recover from a serious illness,
accident, survive. You’re lucky to have come through such a
terrible accident.
— Come to: regain consciousness. When I came to, I was on the
bathroom floor.
— Come under something: be classified as. Diamorphine and
cocaine come under Class A of the Misuse of Drugs Act.
— Come up:
i. arise (of a subject). The question of the rights of patients
is always coming up these days.
ii. happen, occur. I’m afraid I shall be late for my clinic.
Something urgent has come up.
CUT
— Cut back (on) something: reduce expenditure. Because of
financial restrictions, all departments have had to cut back
drastically.
— Cut something down; cut down (on something): reduce
amount or quantity. (a) I’ve already cut my cigarettes down to
10 a day. (b) You should cut down on the fats you eat.
— Cut someone off: break the connection on the telephone
(often used in passive). How annoying. I’ve just been cut off
in the middle of a conversation.
PHRASAL VERBS
173
C3996_08.qxd 25/02/2004 18:34 Page 173
— Cut something off:
i. amputate, remove. Following the explosion, the man had
to have his left leg cut off.
ii. stop the supply of something (often used in passive). The
electricity has been cut off.
— Cut off: isolated. She feels very cut off since she got cancer.
— Cut out something:
i. excise. I had a lump on my neck cut out.
ii. stop eating, using. I’ve cut out alcohol completely.
— Cut someone up: upset emotionally (usually in the passive).
He was terribly cut up by his wife’s death.
DO
— Do away with oneself: to commit suicide, kill oneself. I feel
so depressed, Nurse. I could do away with myself.
— Do someone in:
i. exhaust (usually in passive). At the end of the week I’m
absolutely done in.
ii. kill (usually in passive). The old man was done in (slang).
— Do something in: injure a part of the body. He did his back
in moving furniture.
— Do something to something: cause something to happen
(questions often start with what). What have you done to your
leg? It’s bleeding.
— Do something up:
i. fasten with buttons or zip, etc. Well, Mr Cox, let’s see if
you can do up your clothes.
ii. modernise, redecorate, restore. These wards are depress-
ing. They need doing up.
— Do with something:
i. be concerned with, connected with (use with have to). His
job has something to do with nursing research.
ii. need, wish for (used with can and could). You could do
with some new glasses. Go and have your eyes tested.
— Do without someone/something: manage without. We’ve
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
174
C3996_08.qxd 25/02/2004 18:34 Page 174
had to do without a speech and language therapist since the
last one left.
FIND
— Find something out: discover the truth, learn some informa-
tion. When did you find out your son was on drugs?
FIT
— Fit someone/something in: manage to find time to see some-
one or do something. The nurse is booked up all morning, but
as it’s urgent I’ll try and fit you in.
— Fit in with someone/something: suit, harmonise with some-
one/something. Do you think she will fit in with the rest of the
team?
— Fit someone/something out/up with: equip. After the oper-
ation, we’ll fit you up with a seat to get you into the bath.
GET
— Get about:
i. move from place to place. I can’t get about much now that
I’ve got arthritis.
ii. spread (of news, rumour). It got about that the
Community Hospital might close.
— Get something across: communicate something to someone.
It’s quite difficult to get across to my mother that she can’t go
on living alone.
— Get along: make progress. Fine. You’re getting along very
well.
— Get along with someone: have a good relationship with
somebody. Do you get along with your family?
— Get around: — as for Get about.
— Get at someone: criticise someone repeatedly (usually in con-
tinuous tenses). The other children are always getting at him
PHRASAL VERBS
175
C3996_08.qxd 25/02/2004 18:34 Page 175
and he’s afraid of going to school now.
— Get at someone/something:
i. reach. Make sure you put these tablets somewhere where
the children can’t get at them.
ii. mean, try to say. I’m not sure what you’re getting at.
— Get away: have a holiday. You should try to get away for a
few days after the operation.
— Get back: arrive, return home. He says he can get back under
his own steam (without help).
— Get back to someone: contact someone again later. I don’t
have the information you need just now, but I’ll get back to you.
— Get something back: recover something that was lost. He’s
now got back the use of his arm which was paralysed by the
stroke.
— Get by: manage, cope with life. Lone-parent families often
have a struggle to get by.
— Get someone down: depress. All this quarrelling in the family
gets me down.
— Get something down: swallow (with difficulty). The tablets
you gave me last time were so big I could hardly get them
down.
— Get into: start bad habits. How did she get into drugs?
— Get (someone) off: fall asleep, help someone to fall asleep. It
takes me ages to get the baby off at night.
— Get off something: leave work with permission. He got a
week off when his wife had a baby.
— Get on:
i. perform (often used in questions with how). (a) How did
you get on in the exam? (b) I got on fine with my first
assignment but failed my second.
ii. progress. Take these tablets for a month and we’ll see
how you get on.
— Get on with someone: have a good relationship with. I get on
fine with my children, but I don’t get on with my wife.
— Get out: leave the house. You must try to get out more. No
wonder you are depressed, sitting here alone all day.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
176
C3996_08.qxd 25/02/2004 18:34 Page 176
— Get out of something:
i. escape the necessity or duty to do something. He managed
to get out of working nights for a month.
ii. give up a habit. I wish I could get out of the habit of
smoking after every meal.
— Get over something:
i. overcome. No need to worry. I’m sure we can get over
that problem.
ii. recover from disappointment, illness, shock. He’s getting
over the shock of losing his wife extremely well.
— Get something over: complete something difficult or unpleas-
ant. Thank goodness I’ve got the hysterectomy over.
— Get something over to someone: make someone under-
stand. You must get over to your husband the importance of
remaining active as far as possible.
— Get through something:
i. consume, use a certain amount. He gets through a bottle
of spirits a day.
ii. pass an exam, test. Marvellous. I’ve got through my driv-
ing test.
— Get through to someone:
i. make contact, communicate. We are in despair. We just
can’t get through to our son at all.
ii. reach, especially by telephone. I’ve tried six times to speak
to the stoma care nurse, but I can’t get through.
— Get together: assemble, meet. The management and the union
should get together to settle this problem.
— Get up: rise from bed. Do you have to get up in the night to
pass water?
— Get up to something: do something surprising or unaccept-
able. My parents have no idea what I get up to.
GIVE
— Give something back to someone: restore, return. The
operation should give you back the use of your legs.
PHRASAL VERBS
177
C3996_08.qxd 25/02/2004 18:34 Page 177
— Give in (to someone/something): stop arguing, fighting,
trying, etc. Mrs Spearey was marvellous. She had so much ill-
ness but she would not give in.
— Give out:
i. come to an end (of food supplies, strength, etc.). I can’t
go on any longer. My strength has given out.
ii. fail, stop working. At the end of the 6-hour operation, the
patient’s heart gave out and he died.
— Give something out: distribute. Those leaflets must be given
out to all staff explaining the new safety regulations.
— Give someone up:
i. renounce hope. The doctors had given her up months
ago, but she made a marvellous recovery.
ii. stop having a relationship with someone. Why don’t you
give him up if he treats you so badly?
— Give something up: stop doing something. (a) How can I give
up smoking? (b) I used to be a teacher, but I gave it up last
year.
GO
— Go against something: conflict with something. Private med-
icine goes against the principles of the NHS set up in 1948.
— Go ahead with something: proceed with something. I’ve
decided I want to go ahead with the job application.
— Go along with someone/something:
i. accompany. Nurse, go along with Mrs Hooper to the
X-Ray Department, will you?
ii. agree. I can’t go along with your idea of a further
operation.
— Go at someone: attack physically or verbally. I was walking
down the street and a young man went at me, knocked me to
the ground and took my bag.
— Go back: return. I want you to go back to your GP with this
letter.
— Go by: pass (of time). As time goes by, you’ll get more used
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
178
C3996_08.qxd 25/02/2004 18:34 Page 178
to wearing the artificial limb.
— Go by something: form an opinion. I know I look well, but
that’s nothing to go by. I feel terrible.
— Go down:
i. be swallowed (of food and drink). My food won’t go
down (i.e. I have difficulty swallowing food).
ii. be reduced in size, level, etc. How’s your ankle? Well, the
swelling has gone down, but it’s still very painful.
iii. become lower, fall (of prices, temperature, weight, etc.) (a)
His temperature has gone down. (b) I used to be 9 stone
7 pounds, but then I lost my appetite and went down to
8½ stones.
iv. decrease in quality, deteriorate. Standards of behaviour
have gone down in recent years.
— Go down with something: become ill with something. All the
children have gone down with measles.
— Go for someone: attack physically or verbally. He went for
her with a knife.
— Go for someone/something: Fetch. Go for Sister, quickly.
— Go in for:
i. enter for an examination. Thousands of nurses go in for
higher degrees every year.
ii. study for a particular profession. Are you going in for
medicine like your mother?
— Go into something: investigate. The Neonatal Intensive Care
Unit has been closed while the authorities go into the sudden
deaths of ten babies.
— Go off:
i. deteriorate, get worse. Her work has gone off since the
accident.
ii. explode. She had to have plastic surgery after an oil heater
went off in her face.
iii. faint, fall asleep, lose consciousness. (a) If he sees blood,
he goes off. (b) It takes me ages to go off. Sometimes I
take a sleeping pill.
iv. go bad (of food or drink), become unfit to eat or drink.
PHRASAL VERBS
179
C3996_08.qxd 25/02/2004 18:34 Page 179
The food poisoning was caused by eating some meat that
had gone off.
v. stop (of pain). I’ve had this abdominal pain for a month.
When I take the tablets it goes off, but it comes back.
— Go off someone/something: to lose one’s liking or taste for
someone/something. (a) My wife’s gone off me. (Usually means
does not wish to continue sexual relationship.) (b) I’ve gone off
drink since my operation. (c) I’ve gone off my food completely.
— Go on:
i. continue. (a) This trouble with your bowels has been
going on for years, hasn’t it? (When followed by a verb,
the verb is in the -ing form.) (b) Go on taking the tablets.
(c) Should I go on working while I’m pregnant, Sister? It
is often used negatively: (d) I can’t go on any longer like
this. Can you give me something to help me, Nurse?
ii. happen, take place. What’s going on?
— Go on something:
i. begin to receive payments from the State because of unem-
ployment. We’ve had to go on Social Security as we’ve no
other money coming in.
ii. go on the pill; begin to take the contraceptive pill. When
did you first go on the pill?
— Go on at someone: to complain of someone’s behaviour,
work, etc. He never stops going on at me.
— Go out:
i. be extinguished (of fire, light, etc.). All the lights have
gone out.
ii. leave the house. (a) I’m longing to go out again. (b) You
should be able to go out in a couple of days.
— Go over something: check, inspect details, repeat. Well, I’ve
told you what the treatment involves and I’m going to go over
it again to make sure you understand.
— Go round: spread from person to person (of illness). There’s a
nasty virus going round at the moment.
— Go round to: pay a visit locally. I went round to see the prac-
tice nurse last week and he sent me here.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
180
C3996_08.qxd 25/02/2004 18:34 Page 180
— Go through: endure, experience, suffer. (a) When did he go
through the phase of passing loose stools? (b) She’s gone
through a very bad patch recently (an unhappy or difficult
time). (c) I can’t tell you what I’ve gone through since my hus-
band died.
— Go under:
i. have an anaesthetic. The patient went under at 12 and
came round at 4 o’clock.
ii. die (slang). Do you think he’s going to go under?
— Go up: rise (of blood pressure, temperature, etc.). Your blood
pressure has gone up again.
— Go with someone: accompany. Have you anyone who can
go with you to hospital?
— Go without something: manage without something. (a) I
have to go without food before I have the barium enema. (b)
They went without sleep for several days.
KEEP
— Keep away from someone/something: avoid being near to.
Keep away from anyone with German measles if you think
you are pregnant.
— Keep someone/something back: hold back. (a) My disabil-
ity will never keep me back. (b) She couldn’t keep back her
tears.
— Keep someone down: dominate, oppress. They had a difficult
childhood. Their father kept them down.
— Keep something down:
i. keep something in the stomach (often used negatively
meaning to vomit). She’s so thin because she can’t keep
anything down.
ii. not increase something (e.g. wages, prices, weight, etc.).
(a) Keep your weight down. (b) Restricting salt in the diet
may help keep blood pressure down.
— Keep someone from doing something: prevent. All this
coughing keeps me from sleeping.
PHRASAL VERBS
181
C3996_08.qxd 25/02/2004 18:34 Page 181
— Keep off something: not drink, eat, smoke, etc. (a) Keep off
fatty foods. (b) You should keep off alcohol while you’re tak-
ing these tablets.
— Keep on doing something: continue doing something, do
something repeatedly. The majority of women in the UK keep
on working nowadays. (Note: ‘keep doing something’ has the
same meaning as ‘keep on doing something’.) Michael keeps
getting stomach cramps.
— Keep to something: adhere to an agreement, a course, a diet,
etc. Keep to the diet for another 2 months and then we’ll see
how you are.
— Keep someone up: prevent someone from going to bed. The
baby kept us up all night with his crying.
— Keep one’s spirits, strength up: not allow to fall. (a) She is
a very brave woman and always keeps her spirits up. (Remains
cheerful.) (b) You must eat to keep your strength up.
— Keep up with someone/something: move, progress at the
same rate. Older people find it difficult to keep up with all the
changes of modern life.
LET
— Let someone down: disappoint, fail to help. I can’t leave the
course. I can’t let my parents down.
— Let up:
i. become less intense, severe. If only this pain would let up
for a while.
ii. relax one’s efforts. After the train crash, the team at the
hospital worked night and day to treat the injured. Finally,
they were able to let up a little.
LOOK
— Look after oneself/someone: take care of. (a) She is old and
frail and needs to be properly looked after. (b) Who will look
after your children when you come into hospital?
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
182
C3996_08.qxd 25/02/2004 18:34 Page 182
— Look after something: be responsible for. The technicians
look after the equipment and keep it in good order.
— Look at something: examine carefully. I want to look at your
ear to see what’s causing the trouble.
— Look down on someone/something: feel superior. Her hus-
band looks down on her because she hasn’t been to university.
— Look forward to doing something: think of something in the
future with pleasure. I’m looking forward to having this plas-
ter cast off.
— Look in: make a short visit to someone’s house. The social
worker will look in again next week.
— Look into something: investigate. We must look into this
complaint. It says someone was left lying on a trolley in the
corridor for several hours without being attended to.
— Look on: watch something without taking part. Whilst the sur-
geon performed the delicate operation, doctors from many
countries looked on.
— Look on someone/something: consider. He’s looked on as
one of the leading nurses in this field.
— Look out: be careful, watch out. Look out! You’ll burn your-
self on that stove.
— Look out for someone/something: watch carefully for
someone/something. When assessing people, nurses look out
for signs that indicate a problem.
— Look over: inspect buildings, papers, etc. Can you look over
this report before I submit it to the Working Party?
— Look through something: examine papers quickly. I’ll just
look through the notes before seeing Ms Turner.
— Look to someone/something: take care of. The child-minder
looks to the children while I’m at work.
— Look up:
i. improve. How’s Mrs Cox? Oh, she’s looking up.
ii. raise eyes. Open your eyes now and look up. I’m going to
put some drops in your eyes.
— Look someone up: visit someone, especially after a long time
apart. Do look me up when you next come to Birmingham.
PHRASAL VERBS
183
C3996_08.qxd 25/02/2004 18:34 Page 183
— Look something up: search for a word, fact in a reference
book. If you don’t understand the colloquial English your
patient uses, look it up in the Manual.
— Look up to someone: admire, respect. Young boys like to
look up to pop stars and footballers.
MAKE
— Make something of someone/something: understand the
nature or meaning of someone/something. (a) We don’t know
what to make of this change in her behaviour. (b) What do
you make of it all?
— Make off with something: to steal something and run away
with it. The youth made off with the CDs he’d found.
— Make someone out: understand someone’s behaviour. We
just can’t make Mary out at all. She’s changed so much since
she left home.
— Make something out:
i. manage to read. Can you make out what this letter says?
ii. manage to understand. We’ll have to get an interpreter.
We just can’t make out what this person says.
iii. write a cheque, a prescription, etc. The nurse specialist
made out a prescription for my asthma.
— Make up: apply cosmetics. Whenever I make up, I come out
in a rash all over my face.
— Make something up:
i. invent a story, especially to deceive someone. Stop making
things up. What really happened?
ii. prepare a bed. Keep Mr Derby here. The bed hasn’t been
made up yet.
iii. prepare medicine. Take this prescription to the pharmacist
and he’ll make it up for you.
iv. supply deficiency. It’s not harmful to be a blood donor. The
loss of blood is made up quite quickly in a healthy person.
— Make up for something: compensate. No amount of money
can make up for the loss of her husband.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
184
C3996_08.qxd 25/02/2004 18:34 Page 184
PUT
— Put something aside: save money, etc., for future use.
Everything costs so much these days. I can’t put anything aside
for my old age.
— Put someone away: to confine someone to prison or psychi-
atric unit (often used in passive). (a) The old man began to
wander in the street at night so his family put him away. (b)
He was put away for life for murder.
— Put something away: save money for future use.
— Put something back:
i. drink large amount of alcohol (slang). He must have put
back a lot of beer to be in this state.
ii. impede. The accident has put back his hopes of running
in the Olympics.
— Put something by: save money for future use. Have you any-
thing put by?
— Put something down:
i. kill animal because it is suffering or sick. I had to have my
dog put down last week.
ii. place a baby in bed. I put him down at 9 and he starts
crying at 11.
iii. write down. I’d better put down when to take the tablets
or I shall forget.
— Put something down to: consider something is caused by.
What do you put this rash down to, Nurse? I put it down to an
allergy.
— Put something forward: propose, suggest. At the meeting it
was put forward that more operations should be dealt with in
the Day Surgery Unit.
— Put something in:
i. install. We aim to put strategies in that will reduce deaths
from cancers by at least a fifth in people under 75 years
by 2010.
ii. spend time on work. Health professionals often put in
many extra hours at work.
— Put in for something: apply for a job. He’s put in for over 20
PHRASAL VERBS
185
C3996_08.qxd 25/02/2004 18:34 Page 185
G-grade jobs without any success.
— Put someone off (something): disturb, upset. (a) She could
never be a nurse. She’s easily put off by the sight of blood.
(b) Food just puts me off at the moment.
— Put someone off doing something: dissuade someone from
doing something. My parents tried to put me off living with
Tom, but I took no notice.
— Put something off: delay, postpone. The operation had to be
put off because there was no bed available in the ICU.
— Put something on:
i. get dressed. You can put your clothes on now, Mrs Turner.
ii. increase weight. Good. You’ve put on 6 pounds since we
last saw you.
Put someone out:
i. anaesthetise. They put me out and I came round 3 hours
later (slang).
ii. annoy, upset. She was put out because her doctor didn’t
explain what the procedure involved.
— Put something out:
i. dislocate. I think you’ve put your shoulder out and we
must X-ray it to be sure.
ii. extinguish fire, light. Fire crews soon put the fire out.
— Put someone through: connect on telephone. Put me through
to A&E will you please?
— Put someone up: provide a bed and food. I lost my job and
my home. A friend put me up for a few weeks, but I’m home-
less again.
— Put something up:
i. increase price. My landlord has put the rent up by £20 a
week so I’ll have to go.
ii. raise. The pain’s so bad I can’t put my arms up to do my
hair.
— Put up with someone/something: bear, tolerate. (a) I’m
afraid there’s not much they can do about this condition. I’ll
have to put up with it. (b) How did she put up with that vio-
lent husband for so long?
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
186
C3996_08.qxd 25/02/2004 18:34 Page 186
RUN
— Run across someone/something: to meet someone or find
something by chance. I’ve never run across this before. I think
it’s a case of botulism.
— Run away from someone/something: suddenly leave,
escape. He’s always been a difficult child. He ran away from
home at the age of 10.
— Run someone/something down:
i. hit and knock to the ground. The cyclist was run down by
a lorry.
ii. speak badly about someone. He’s always running down his
girlfriend in public.
— Run someone in: arrest and take to police station. He was
run in for shoplifting (slang).
— Run into something:
i. collide or crash into. A man has just been brought into
A&E. He ran his car into a wall in the fog.
ii. get into danger, debt, trouble, etc. We’ve run into debt and
my partner’s drinking heavily.
— Run something off: make copies on a machine. Could you
run off 20 copies of this hand-out, please?
— Run out of something: come to an end (of permits, supplies,
time, etc.). (a) Make sure we’ve enough clean sheets this
weekend. We mustn’t run out. (b) I’m nearly 85 you know. I’m
running out of time. (c) My energy is running out.
— Run over someone: (of a vehicle) knock someone down and
pass over body. He’s been run over and has multiple injuries.
— Run over something: read quickly, repeat. Will you just run
over the facts again?
— Run through something:
i. discuss, examine, read quickly. I’ve run through the
names of people admitted this week, but your son’s is not
there.
ii. spend carelessly, wastefully They have run through thou-
sands of pounds on advertising.
PHRASAL VERBS
187
C3996_08.qxd 25/02/2004 18:34 Page 187
iii. use up. We run through a lot of disposable gloves in the
sexual health clinic.
— Run up something: accumulate bills. Why did you run up
such large bills?
SEND
— Send for someone: tell someone to come. He’s failing. Send
for the ambulance.
— Send for something: order something to be delivered. Send
for the latest information, will you please?
— Send off something: post. Don’t forget to send off those let-
ters today.
SET
— Set aside something:
i. save money for particular purpose. She sets aside a bit of
money every month to pay her fuel bills.
ii. keep time for a particular purpose. You must set aside half
an hour a day to practise the relaxation exercises.
— Set back someone/something: delay progress of someone/
something. (a) Mr Deakin was making a good recovery after
his operation, but unfortunately a wound infection has set him
back. (b) Work on the new theatre has been set back 3 months.
— Set in: begin and seem likely to continue (of infection, rain,
winter, etc.). (a) When cold weather sets in, older people must
take precautions to care for themselves. (b) You can see gan-
grene has set in to your left leg and, as it has not responded
to treatment, we have no alternative but to remove it.
— Set on someone: attack. I got this bite when a dog set on me.
— Set someone up: make better, healthier. A week by the sea
will set you up after the bowel surgery.
TAKE
— Take after someone: resemble in appearance or character.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
188
C3996_08.qxd 25/02/2004 18:34 Page 188
I’m worried about Jane. She’s so different from me. She takes
after her father.
— Take something away:
i. cause a feeling, etc., to disappear. (a) I’ll give you some
tablets to take the pain away. (b) All this worry has taken
my appetite away.
ii. remove. They’ve taken her womb away.
— Take someone away from someone/something: remove.
When sexual abuse was suspected, the children were taken
away from their parents on the recommendation of social
workers.
— Take something down: record, write something. Can you
take down the details?
— Take something in: absorb, understand by listening or read-
ing. He was so confused he could not take in what the nurse
was saying.
— Take something off:
i. amputate part of body. His left arm had to be taken off
below the elbow.
ii. have time away from work for special purpose. I’m taking
next week off to be at home when my wife comes out of
hospital.
iii. lose weight by dieting. I’m overweight. I want to take off a
stone.
iv. remove part of clothing. You needn’t take off all your
clothes. Just your shirt.
— Take on something: agree to do work, have responsibility.
Don’t take on too much for the next 6 weeks.
— Take something out: remove or extract. (a) I must have this
tooth taken out. It’s giving me a lot of pain. (b) She’s going
into hospital to have her appendix taken out. (c) We’re going
to take the stitches out tomorrow.
— Take something over from someone: take control, respon-
sibility from someone else. Can you take over my bleep for
10 minutes while I see Mrs Briggs?
— Take to someone: develop a liking for someone. I never took
PHRASAL VERBS
189
C3996_08.qxd 25/02/2004 18:34 Page 189
to my daughter-in-law. She’s caused so much trouble in the
family.
— Take to something/doing something: begin to do something
as a habit. (a) We need help. Our only daughter has taken to
drugs. (b) He’s taken to going for long walks late at night.
— Take up something:
i. absorb, occupy time. Nursing takes up all his time and
energy.
ii. start a job. We expect you to take up your duties on 1st
January.
iii. start a profession, hobby, etc. He’s thinking of taking up
mental health nursing as a career.
TURN
— Turn against someone: become hostile to. After our divorce,
my wife tried to turn the children against me.
— Turn someone away: refuse to give help. Health professionals
cannot turn sick people away.
— Turn someone/something down:
i. reject an idea, person, proposal. They turned me down as
a pilot because of my eyesight.
ii. reduce volume of gas, sound, etc. When they turn down
the television I can’t hear a thing.
— Turn in:
i. go to bed (slang). It’s usually 2 o’clock before I turn in.
ii. be pigeon-toed. He walks with his toes turned in.
— Turn something in: stop doing something (slang). The job
was ruining my health so, although I loved it, I had to turn it
in.
— Turn someone off: cause someone to be disgusted by some-
thing or not sexually attracted to someone. His drinking and
bad breath turned me off.
— Turn something off:
i. stop the flow of electricity, gas, etc. Don’t forget to turn off
the machine before you leave the building.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
190
C3996_08.qxd 25/02/2004 18:34 Page 190
ii. stop radio, TV. The TV is going all day. He never turns
it off.
— Turn on someone: attack. As I left the building, the guard
dog turned on me and bit my leg.
— Turn someone on: give great pleasure, excite sexually.
Certain illicit drugs turn you on very quickly.
— Turn something on: allow gas, electricity, water to flow.
Make sure the computer is turned on first thing.
— Turn someone out: force someone to leave a place. I’ve
nowhere to sleep. My partner has turned me out.
— Turn something out: extinguish light or fire. Please turn out
the lights before going home.
— Turn out: prove to be. I never thought it would turn out to be
fatal.
— Turn over: change position of body by rolling. Turn over onto
your left side and draw your knees to your chest.
— Turn someone/something round: face in different direc-
tion. Turn round and let me look at your back.
— Turn to someone/something: go for advice, help. (a) The
practice nurse is a good person to turn to when you need
health advice. (b) Sadly, when his wife left him he turned to
drink for solace.
— Turn up:
i. appear, arrive. Mr Fox hasn’t turned up yet for his
appointment.
ii. be found, by chance, after being lost. Thank goodness
those keys have turned up. We thought they’d been
stolen.
— Turn something up: increase volume of radio, TV, etc. I have
to turn up my hearing aid to listen to the news.
PHRASAL VERBS
191
C3996_08.qxd 25/02/2004 18:34 Page 191
C3996_08.qxd 25/02/2004 18:34 Page 192
This page intentionally left blank
Abbreviations used in
nursing
INTRODUCTION
The rapid developments in nursing, healthcare and the related
sciences in recent years have brought a vast increase in the asso-
ciated vocabulary. At the same time, the increased speed of life
has driven people to use abbreviations more and more, and this
tendency is well illustrated in the nursing and healthcare field.
The use of abbreviations is discouraged because they are vari-
able and misleading. The same initials may have different mean-
ings in different areas of nursing practice. For example, PID may
mean pelvic inflammatory disease or prolapsed intervertebral disc.
The Nursing and Midwifery Council is clear about the need to
avoid the use of abbreviations in record keeping and documen-
tation (NMC 2002) (see Ch. 4).
Nevertheless, you will see and hear abbreviations being used
every day in medical reports and notes and in discussions about
patients and during handover reports, and a knowledge of them
is, therefore, absolutely essential. You should always ask if you
are not sure what an abbreviation means.
A selection of abbreviations commonly used by nurses and
other health professionals is provided to help you understand
what people mean.
193
9
AA – Alcoholics Anonymous
AAA – abdominal aortic
aneurysm
ABG – arterial blood gas
a.c. – ante cibum (Latin –
sometimes used in pre-
scriptions), before food
ACE – angiotensin-converting
enzyme
ACTH – adrenocorticotrophic
hormone
A
C3996_09.qxd 25/02/2004 18:35 Page 193
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
194
ADH – antidiuretic hormone
ADHD – attention-deficit
hyperactivity disorder
ad lib – ad libitum (Latin), to
the desired amount
ADLs – Activities of Daily
Living
ADRs – adverse drug
reactions
A&E – Accident and
Emergency Department
AF – atrial fibrillation
AFB – acid-fast bacilli
AFP – a-fetoprotein
AI – artificial insemination
AIDS – acquired immune
deficiency syndrome
ALL – acute lymphoblastic
leukaemia
ALs – Activities of Living
ALS – advanced life support
ALT – alanine
aminotransferase
AMI – acute myocardial
infarction
AML – acute myeloid
leukaemia
ANC – antenatal care
ANS – autonomic nervous
system
AP – anteroposterior
APEL – accreditation of
prior experience and
learning.
APH – antepartum haemor-
rhage
APKD – adult polycystic
kidney disease
ARC – AIDS-related complex
ARDS – adult respiratory
distress syndrome
ARF – (1) acute renal failure;
(2) acute respiratory
failure
ASD – atrial septal defect
AST – aspartate
aminotransferase
ATN – acute tubular necrosis
ATD – Alzheimer’s-type
dementia
A-V – atrioventricular: (1)
node; (2) bundle
BAI – Beck Anxiety
Inventory
BAN – British Approved
Name (of drugs)
BBA – born before arrival
BBB – (1) blood–brain barrier;
(2) bundle branch block
BBVs – blood-borne viruses
BCG – bacille Calmette
Guérin
b.d. – bis die (Latin – some-
times used in prescrip-
tions), twice daily
BDI – Beck Depression
Inventory
BHS – Beck Hopelessness
Scale
B
C3996_09.qxd 25/02/2004 18:35 Page 194
ABBREVIATIONS USED IN NURSING
195
b.i.d. – bis in die (Latin),
twice a day
BID – brought in dead
BLS – basic life support
BMI – body mass index
BMR – basal metabolic rate
BMT – bone marrow
transplant
BN – Bachelor of Nursing
BNF – British National
Formulary
BNO – bowels not opened
BO – bowels opened
BP – (1) blood pressure; (2)
British Pharmacopoeia
BPH – benign prostatic
hyperplasia
BPRS – Brief Psychiatric
Rating Scale
BSA – body surface area
BSc – Bachelor of Science
BSc (Soc Sc-Nurs) –
Bachelor of Science
(Nursing)
BSE – (1) bovine spongiform
encephalopathy; (2) breast
self-examination
BSS – Beck Scale for Suicide
Ideation
B Wt – birth weight
C – (1) carbon; (2) centigrade
(temperature scale)
Ca – carcinoma
CABG – coronary artery
bypass grafting
CAN – Camberwell
Assessment of Need
CAPD – continuous ambula-
tory peritoneal dialysis
CAPE – Clifton Assessment
Procedures for the Elderly
CATS – credit accumulation
transfer scheme
cc – cubic centimetre
CCF – congestive cardiac
failure
CCU – Coronary Care Unit
CD – controlled drug
CDC – Centers for Disease
Control and Prevention
CDS – Calgary Depression
Scale
CEA – carcinoembryonic
antigen
CF – (1) cardiac failure;
(2) cystic fibrosis
CHAI – Commission for
Healthcare Audit and
Inspection
CHD – (1) congenital heart
disease; (2) coronary heart
disease
CHF – congestive heart
failure
CIN – cervical intraepithelial
neoplasia
CINAHL – Cumulative Index
to Nursing and Allied
Health Literature
C
C3996_09.qxd 25/02/2004 18:35 Page 195
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
196
CJD – Creutzfeldt–Jakob
disease
CK – creatine kinase
CLL – chronic lymphatic
leukaemia
cm – centimetre
CML – chronic myeloid
leukaemia
CMV – cytomegalovirus
CNS – (1) central nervous
system; (2) clinical nurse
specialist
C/O – complains of
COPD – chronic obstructive
pulmonary disease
COSHH – Control of
Substances Hazardous
to Health
CPA – care programme
approach
CPAP – continuous positive
airways pressure
CPD – continuing professional
development
CPN – community psychiatric
nurse
CPR – cardiopulmonary
resuscitation
CRF – chronic renal failure
CSCI – Commission for
Social Care Inspection
CSF – (1) cerebrospinal fluid;
(2) colony stimulating
factor
CSI – Caregiver Strain
Index
CSSD – Central Sterile Supply
Department
CSU – catheter specimen of
urine
CT – (1) computed tomogra-
phy; (2) coronary
thrombosis
CTG – cardiotocograph
CV – (1) cardiovascular;
(2) curriculum vitae
CVA – cerebrovascular
accident
CVP – central venous
pressure
CVS – (1) cardiovascular
system; (2) chorionic
villus sampling
CVVH – continuous venous–
venous haemofiltration
CVVHD – continuous
venous–venous
haemodialfiltration
Cx – cervix
CXR – chest X-ray
DADL – Domestic Activities
of Daily Living
D&C – dilatation and
curettage
DC – direct current
DDH – developmental
dysplasia of the hip
DIC – disseminated intravas-
cular coagulation
D
C3996_09.qxd 25/02/2004 18:35 Page 196
ABBREVIATIONS USED IN NURSING
197
DipEd – Diploma in
Education
DipHE – Diploma in Higher
Education
DipN – Diploma in Nursing
DipNEd – Diploma in
Nursing Education
DKA – diabetic ketoacidosis
DM – diabetes mellitus
DN – district nurse
DNA – (1) deoxyribonucleic
acid; (2) did not attend
DOA – dead on arrival
DOB – date of birth
DoH – Department of Health
DPhil – Doctor of Philosophy
DRS – Delusions Rating Scale
DRV – dietary reference value
DSH – deliberate self-harm
DT – delirium tremens
DTPer – diphtheria, tetanus
and pertussis vaccine
DU – duodenal ulcer
DVT – deep venous
thrombosis
D&V – diarrhoea and
vomiting
DXR – deep X-ray radiation
DXT – deep X-ray therapy
EAR – estimated average
requirement
EBM – expressed breast milk
EBP – evidence-based practice
EBS – emergency bed service
EBV – Epstein–Barr virus
ECF – extracellular fluid
ECG – electrocardiogram
ECI – Experience of
Caregiving Inventory
ECMO – extracorporeal
membrane oxygenator
ECT – electroconvulsive
therapy
EDC – expected date of
confinement
EDD – expected date of
delivery
EEG – electroencephalogram
EFAs – essential fatty acids
ELISA – enzyme-linked
immunosorbent assay
EMD – electromechanical
dissociation
EMG – electromyography
EMLA – eutectic mixture of
local anaesthetics
EMU – early morning speci-
men of urine
ENT – ears, nose and throat
EOG – electro-oculogram
ERCP – endoscopic retro-
grade cholangiopancreato-
graphy
ERG – electroretinogram
ERPC – evacuation of
retained products of
conception
ERV – expiratory reserve
volume
E
C3996_09.qxd 25/02/2004 18:35 Page 197
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
198
ESR – erythrocyte sedimenta-
tion rate
ESRD – end-stage renal
disease
ESS – Early Signs Scale
ESWL – extracorporeal shock
wave lithotripsy
ET – (1) embryo transfer; (2)
endotracheal
EUA – examination under
anaesthesia
F – (1) Fahrenheit (tempera-
ture scale); (2) female
FAS – fetal alcohol syndrome
FB – foreign body
FBC – full blood count
FBS – fasting blood sugar
FETC – Further Education
Teaching Certificate
FEV – forced expiratory
volume
FFP – fresh frozen plasma
FH – (1) family history; (2)
fetal heart
FHH – fetal heart heard
FHNH – fetal heart not
heard
FMF – fetal movement felt
FPC – Family Planning Clinic
FPCert – Family Planning
Certificate
FRC – functional residual
capacity
FRCN – Fellow of the Royal
College of Nursing
FSH – follicle stimulating
hormone
FTND – full-term normal
delivery
FVC – forced vital capacity
g – gram
GA – general anaesthetic
GC – gonococcus
GCS – Glasgow Coma Scale
GFR – glomerular filtration
rate
GGT – g-glutamyl transferase
GH – growth hormone
GHQ – General Health
Questionnaire
GI – gastrointestinal
GIFT – gamete intrafallopian
transfer
GIT – gastrointestinal tract
GOR – gastro-oesophageal
reflux
GP – general practitioner
GSL – General Sales List
(medicines)
GTN – glyceryl trinitrate
GTT – glucose tolerance test
GU – (1) gastric ulcer;
(2) genitourinary
GUM – genitourinary
medicine
GUS – genitourinary system
F
G
C3996_09.qxd 25/02/2004 18:35 Page 198
ABBREVIATIONS USED IN NURSING
199
GVHD – graft versus host
disease
Gyn – gynaecology
HAI – hospital-acquired
infection
HAV – hepatitis A virus
HAVS – hand–arm vibration
syndrome
Hb – haemoglobin
HBIG – hepatitis B
immunoglobulin
HBV – hepatitis B virus
HC – head circumference
HCA – healthcare assistant
HCG (hCG) – human chori-
onic gonadotrophin
HCV – hepatitis C virus
HDL – high-density
lipoprotein
HDSU – Hospital Disinfection
and Sterilisation Unit
HDU – High Dependency Unit
HDV – hepatitis D virus
HEV – hepatitis E virus
HFEA – Human Fertilisation
and Embryology Authority
HHNK – hyperglycaemic
hyperosmolar non-ketotic
HI – head injury
Hib vaccine – Haemophilus
influenzae type B vaccine
HImP – Health Improvement
Programme
HIV – human immunodefi-
ciency virus
HNPU – has not passed
urine
HoNOS – Health of the
Nation Outcome Scale
HPA – Health Protection
Agency
HPV – human papilloma virus
HR – heart rate
HRS – Hallucinations Rating
Scale
HRT – hormone-replacement
therapy
HSV – herpes simplex virus
Ht – height
HUS – haemolytic uraemic
syndrome
HV – Health Visitor
HVCert – Health Visitor’s
Certificate
HVT – Health Visitor Teacher
IABP – intra-aortic balloon
pump
IADL – Instrumental Activities
of Daily Living
IBD – inflammatory bowel
disease
IBS – irritable bowel
syndrome
IC – inspiratory capacity
ICD – International
Classification of Disease
I
H
C3996_09.qxd 25/02/2004 18:35 Page 199
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
200
ICE – ice, compress and
elevate
ICF – intracellular fluid
ICN – (1) Infection Control
Nurse; (2) International
Council of Nurses
ICP – intracranial pressure
ICSH – interstitial cell stimu-
lating hormone
ICU – Intensive Care Unit
ID – infectious disease
IDDM – insulin-dependent
diabetes mellitus
IE – infective endocarditis
IGT – impaired glucose
tolerance
IHD – ischaemic heart
disease
IM – (1) infectious mononu-
cleosis; (2) intramuscular
IMV – intermittent mandatory
ventilation
INR – (1) Index of Nursing
Research; (2) international
normalised ratio
IOL – intraocular lens
IOP – intraocular pressure
IPD – intermittent peritoneal
dialysis
IPP – intermittent positive
pressure
IPPV – intermittent positive
pressure ventilation
IQ – intelligence quotient
IRV – inspiratory reserve
volume
IS – Insight Scale
IT – information technology
ITU – Intensive Therapy Unit
IU – international unit
IUD – intrauterine (contracep-
tive) device
IUI – intrauterine
insemination
IV – intravenous
IVC – inferior vena cava
IVF – in vitro fertilisation
IVI – intravenous infusion
IVU – intravenous urogram
JCA – juvenile chronic
arthritis
JVP – jugular venous pressure
KASI – Knowledge about
Schizophrenia Interview
KS – Kaposi’s sarcoma
KUB – kidney, ureter and
bladder
L, l – litre
LA – (1) left atrium; (2) local
anaesthetic; (3) local
authority
lb – pound (of weight)
LBP – low back pain
J
K
L
C3996_09.qxd 25/02/2004 18:35 Page 200
ABBREVIATIONS USED IN NURSING
201
LDH – lactate dehydrogenase
LDL – low-density lipoprotein
LDQ – Leeds Dependence
Questionnaire
LFTs – liver function tests
LH – luteinising hormone
LIF – left iliac fossa
LMN – lower motor neuron
LMP – last menstrual period
LOC – level of consciousness
LP – lumbar puncture
LRNI – lower reference nutri-
ent intake
LRTI – lower respiratory tract
infection
LSCS – lower segment
Caesarean section
LTM – long-term memory
LUNSERS – Liverpool
University Neuroleptic
Side Effect Rating Scale
LV – left ventricle
LVAD – left ventricular assist
device
LVF – left ventricular failure
LVH – left ventricular
hypertrophy
M – male
MA – Master of Arts
MAC – mid-arm
circumference
mane – in the morning (of
drugs); tomorrow
MAO – monoamine oxidase
inhibitor
MBC – maximal breathing
capacity
MCA – Medicines Control
Agency (now merged with
Medical Devices Agency)
MCH – mean cell
haemoglobin
MCHC – mean cell haemo-
globin concentration
MCL – mid-clavicular line
MCV – mean cell volume
MDA – Medical Devices
Agency (now merged
with Medicines Control
Agency)
MDR-TB – multidrug resistant
tuberculosis
ME – myalgic
encephalomyelitis
MEd – Master of Education
M/F; M/W/S/D – male/
female; married/widowed/
single/divorced
MHRA – Medicines and
Healthcare products
Regulatory Agency
(formed from the MCA
and MDA)
MI – (1) mitral incompetence
or insufficiency; (2)
myocardial infarction
mmHg – millimetres of
mercury
mmol – millimole
M
C3996_09.qxd 25/02/2004 18:35 Page 201
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
202
MMR – measles mumps and
rubella (as in vaccine)
MMV – mandatory minute
volume
MODS – multiple organ
dysfunction syndrome
MODY – maturity onset
diabetes of the young
MPhil – Master of Philosophy
MRI – magnetic resonance
imaging
MRSA – methicillin-resistant
Staphylococcus aureus
MS – (1) mitral stenosis;
(2) multiple sclerosis;
(3) musculoskeletal
MSc – Master of Science
MSH – melanocyte-
stimulating hormone
MSP – Munchausen syndrome
by proxy
MSU – mid-stream urine
MSW – medical social worker
MT – midwifery teacher
MTD – Midwife Teachers’
Diploma
MWO – mental welfare
officer
NAD – no abnormality
detected
NAI – non-accidental injury
NAS – no added salt
NBI – no bone injury
NBM – nil (nothing) by
mouth
NCVQ – National Council for
Vocational Qualifications
ND – normal delivery
NFA – (1) no fixed abode;
(2) no further action
NG – nasogastric
NHL – non-Hodgkin’s
lymphoma
NHS – National Health
Service
NICE – National Institute for
Clinical Excellence
NICU – Neonatal Intensive
Care Unit
NIDDM – non-insulin-
dependent diabetes
mellitus
NIPPV – non-invasive positive
pressure ventilation
NMC – Nursing and
Midwifery Council
NMR – nuclear magnetic
resonance
nocte – in the evening (of
drugs)
NPF – Nurse Prescribers’
Formulary
NPU – not passed urine
NRDS – neonatal respiratory
distress syndrome
NREM – non-rapid eye
movement (sleep)
NSAIDs – non-steroidal anti-
inflammatory drugs
N
C3996_09.qxd 25/02/2004 18:35 Page 202
ABBREVIATIONS USED IN NURSING
203
NSFs – National Service
Frameworks
NSP – non-starch
polysaccharides
NSU – non-specific urethritis
NT – nurse teacher
N&V – nausea and vomiting
NVQ – National Vocational
Qualification
OA – osteoarthritis
OBS – organic brain syndrome
OCD – obsessive–compulsive
disorder
o.d. – omni die (Latin –
sometimes used in
prescriptions), daily
OD – overdose
ODP – operating department
practitioner
O/E, OE – on examination
OGD – oesophagogastroduo-
denoscopy
OHNC – Occupational Health
Nursing Certificate
o.m. – omni mane
(Latin – sometimes used
in prescriptions), in the
morning
o.n. – omni nocte (Latin –
sometimes used in
prescriptions), at night
ONC – Orthopaedic Nurses’
Certificate
OND – Ophthalmic Nursing
Diploma
OPCS – Office of Population
Censuses and Surveys
OPD – Outpatients
Department
ORT – oral rehydration
therapy
OT – occupational therapist
(therapy)
OTC – over the counter
(drugs bought without a
prescription)
OU – Open University
P – pulse
PAC – premature atrial
contraction
PADL – Personal Activities of
Daily Living
PAFC – pulmonary artery
flotation catheter
PALS – paediatric advanced
life support
PANSS – Positive and
Negative Syndrome Scale
Pap – Papanicolaou smear
test
PAT – paroxysmal atrial
tachycardia
PAWP – pulmonary artery
wedge pressure
PBD – peak bone density
PBM – peak bone mass
O
P
C3996_09.qxd 25/02/2004 18:35 Page 203
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
204
p.c. – post cibum (Latin –
sometimes used in
prescriptions), after
food
PCAG – primary closed-angle
glaucoma
PCA(S) – patient-controlled
analgesia (system)
PCEA – patient-controlled
epidural analgesia
PCM – protein–calorie
malnutrition
PCP – Pneumocystis carinii
pneumonia
PCT – Primary Care Trust
PCV – packed cell volume
PCWP – pulmonary capillary
wedge pressure
PD – peritoneal dialysis
PDA – patent ductus
arteriosus
PDP – personal development
plan
PE – pulmonary embolus
PEEP – positive end-
expiratory pressure
PEFR – peak expiratory flow
rate
PEG – percutaneous endo-
scopic gastrostomy
PEM – protein–energy
malnutrition
PET – (1) positron emission
tomography; (2) pre-
eclamptic toxaemia
PFI – private finance initiative
PFR – peak flow rate
PGL – persistent generalised
lymphadenopathy
pH – hydrogen ion
concentration
PHCT – Primary Health Care
Team
PhD – Doctor of Philosophy
PHLS – Public Health
Laboratory Service
PICC – peripherally inserted
central catheter
PICU – Paediatric Intensive
Care Unit
PID – (1) pelvic inflammatory
disease; (2) prolapsed
intervertebral disc
PKU – phenylketonuria
PL – perception of light
PM – postmortem
PMB – postmenopausal
bleeding
PMH – past medical history
PMS – premenstrual
syndrome
PMT – premenstrual tension
PN – postnatal
PND – paroxysmal nocturnal
dyspnoea
POAG – primary open-angle
glaucoma
POM – prescription only
medicine
PONV – postoperative nausea
and vomiting
POP – plaster of Paris
C3996_09.qxd 25/02/2004 18:35 Page 204
ABBREVIATIONS USED IN NURSING
205
PPD – (1) progressive
perceptive deafness; (2)
purified protein derivative
PPH – post-partum
haemorrhage
PPS – plasma protein solution
PPV – positive pressure
ventilation
PR – per rectum
PREP – post-registration
education and practice
PRL – prolactin
p.r.n. – pro re nata (Latin –
sometimes used in pre-
scriptions), when required
PSA – prostate-specific
antigen
PSCT – Pain and Symptom
Control Team
PSV – pressure support
ventilation
PT – (1) physiotherapist;
(2) prothrombin
PTA – prior to admission
PTC – percutaneous transhep-
atic cholangiography
PTCA – percutaneous translu-
minal coronary angioplasty
PTH – parathyroid hormone
PTSD – post-traumatic stress
disorder
PTT – partial thromboplastin
time
PU – passed urine
PUFA – polyunsaturated fatty
acid
PUO – pyrexia of unknown
origin
PV – per vagina
PVD – peripheral vascular
disease
PVS – persistent vegetative
state
PVT – paroxysmal ventricular
tachycardia
QALY – quality-adjusted life-
year
q.d.s. – quater die sumendus
(Latin – sometimes used
in prescriptions), four
times a day
q.i.d. – quater in die (Latin),
four times a day
QIDN – Queen’s Institute of
District Nursing
q.q.h. – quarta quaque hora
(Latin), every 4 hours
R – respiration
RA – (1) rheumatoid arthritis;
(2) right atrium
RAI – Relatives’ Assessment
Interview
RAISSE – Relatives’
Assessment Interview for
Schizophrenia in a Secure
Environment
Q
R
C3996_09.qxd 25/02/2004 18:35 Page 205
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
206
RBC – (1) red blood cell; (2)
red blood cell count
RBS – random blood sugar
RCC – red cell concentrate
RCM – Royal College of
Midwives
RCN – Royal College of Nurs-
ing and National Council
of Nurses of the UK
RCNT – Registered Clinical
Nurse Teacher
RCT – randomised controlled
trial
RDA – recommended daily
allowance
REM – rapid eye movement
(sleep)
RG – remedial gymnast
RGN – Registered General
Nurse
Rh – rhesus factor
RHD – rheumatic heart
disease
RHV – Registered Health
Visitor
RICE – rest, ice, compress,
elevation
RIF – right iliac fossa
rINN – recommended inter-
national non-proprietary
name
RIP – raised intracranial
pressure
RM – Registered Midwife
RMN – Registered Mental
Nurse
RN – Registered Nurse
RNA – ribonucleic acid
RNI – reference nutrient
intake
RNIB – Royal National
Institute for the Blind
RNID – Royal National
Institute for the Deaf
RNMH – Registered Nurse for
the Mentally Handicapped
RNT – Registered Nurse Tutor
RO – reality orientation
ROM – range of movement
(exercises)
ROS – removal of sutures
RS – respiratory system
RSCN – Registered Sick
Children’s Nurse
RSI – repetitive strain injury
RSV – respiratory syncytial
virus
RTA – (1) renal tubular acido-
sis; (2) road traffic
accident
RTI – respiratory tract
infection
RV – (1) residual volume;
(2) right ventricle
RVF – right ventricular failure
SAD – seasonal affective
disorder
SAH – subarachnoidal
haemorrhage
S
C3996_09.qxd 25/02/2004 18:35 Page 206
ABBREVIATIONS USED IN NURSING
207
SAI – sexually acquired
infection
SANS – Schedule for
Assessment of Negative
Symptoms
SARS – severe acute respira-
tory syndrome
SC – subcutaneous
SCBU – Special Care Baby Unit
SCC – (1) spinal cord com-
pression; (2) squamous
cell carcinoma
SCD – sequential pneumatic
compression device
SCM – State Certified Midwife
SDAT – senile dementia
Alzheimer type
SDH – subdural haematoma
SERMs – selective (o)estro-
gen receptor modulators
SFS – Social Functioning Scale
SG – specific gravity
SGA – small for gestational
age
SHHD – Scottish Home and
Health Department
SHO – senior house officer
SI Units – Système
International d’Unités
SIB – self-injurious behaviour
SIDS – sudden infant death
syndrome
SIMV – synchronised intermit-
tent mandatory ventilation
SLE – systemic lupus
erythematosus
SLS – social and life skills
SLT – speech and language
therapist (therapy)
SMR – (1) standardised mor-
tality rate; (2) submucous
resection
SNAP – Schizophrenia
Nursing Assessment
Protocol
SOB – short of breath
SPECT – single photon
emission computed
tomography
SPF – sun protection factor
SRN – State Registered Nurse
SSRIs – selective serotonin
re-uptake inhibitors
stat. – statim (Latin – some-
times used in prescrip-
tions), immediately
STD – sexually transmitted
disease
STI – sexually transmitted
infection
STM – short-term memory
STs – sanitary towels
SVC – superior vena cava
SVQs – Scottish Vocational
Qualifications
SVT – supraventricular
tachycardia
SWD – short-wave diathermy
T – temperature
T
C3996_09.qxd 25/02/2004 18:35 Page 207
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
208
T&A – tonsils and adenoids
TB – tuberculosis
TCA – tricyclic antidepressants
TCI – to come in
t.d.s. – ter die sumendus
(Latin – sometimes used in
prescriptions), three times
a day
TEDs – thromboembolic
deterrent (stockings)
TEN – toxic epidermal
necrolysis
TENS – transcutaneous elec-
trical nerve stimulation
TIA – transient ischaemic
attack
t.i.d. – ter in die (Latin), three
times a day
TIPSS – transjugular intrahep-
atic portasystemic stent
shunting
TLC – total lung capacity
TLS – tumour lysis syndrome
TNF – tumour necrosis factor
TNM – tumour, node,
metastasis
TOP – termination of
pregnancy
TPN – total parenteral
nutrition
TPR – temperature, pulse,
respiration
TRIC – trachoma inclusion
conjunctivitis
TSF – triceps skin-fold
thickness
TSH – thyroid-stimulating
hormone
TSS – toxic shock syndrome
TT – (1) tetanus toxoid;
(2) thrombin clotting time;
(3) tuberculin tested
TTA(O) – to take away (out)
TUR – transurethral resection
TURP – transurethral
resection of the prostate
gland
TURT – transurethral
resection of tumour
TV – (1) tidal volume; (2)
Trichomonas vaginalis
U – unit
U&E – urea and electrolytes
UG – urogenital
UGS – urogenital system
UGT – urogenital tract
UKCC – UK Central Council
for Nursing, Midwifery and
Health Visiting (replaced
by Nursing and Midwifery
Council)
UMN – upper motor neuron
URTI – upper respiratory tract
infection
USS – ultrasound scan
UTI – urinary tract infection
UVA – ultraviolet A
UVB – ultraviolet B
UVL – ultraviolet light
U
C3996_09.qxd 25/02/2004 18:35 Page 208
ABBREVIATIONS USED IN NURSING
209
VA – visual acuity
VAS – visual analogue
scale
VBI – vertebrobasilar
insufficiency
VC – vital capacity
VD – venereal disease (out-
dated term)
VE – vaginal examination
VF – ventricular fibrillation
VFM – value for money
VLDL – very-low-density
lipoprotein
VRE – vancomycin-resistant
enterococci
VRS – Verbal Rating Scale
VSD – ventricular septal
defect
VT – ventricular tachycardia
VUR – vesicoureteric reflux
VV – varicose vein(s)
VZIG – varicella-zoster
immunoglobulin
VZV – varicella-zoster virus
WBC – (1) white blood cell;
(2) white blood cell count
WC – water closet (lavatory)
WHO – World Health
Organisation
WPW – Wolff–Parkinson–
White syndrome
Wt – weight
ZIFT – zygote intrafallopian
transfer
ZN – Ziehl–Neelsen (stain)
V
W
Z
C3996_09.qxd 25/02/2004 18:35 Page 209
C3996_09.qxd 25/02/2004 18:35 Page 210
This page intentionally left blank
Useful addresses and
web sources
Some useful addresses and web sources are provided in this
chapter. They will help you to get up-to-date information about
the sort of issues that are important for a satisfying and success-
ful nursing career in the UK. These include: immigration, registra-
tion as a nurse in the UK, welfare and employment, and educa-
tion opportunities. Also included are some sources of information
for your patients and their families.
INFORMATION FOR NURSES
Addresses and websites
Commission for Racial Equality
Elliot House
10–12 Allington Street
London SW1E 5EH
http://www.cre.gov.uk
Commonwealth Nurses Federation
c/o International Department
Royal College of Nursing
20 Cavendish Square
London W1M 0AB
Community and District Nursing Association (CDNA)
Westel House
32–38 Uxbridge Road
Ealing
London W5 2BS
http://www.cdna.tvu.ac.uk
211
10
C3996_10.qxd 25/02/2004 18:37 Page 211
Community Practitioners’ and Health Visitors’ Association
(CPHVA)
40 Bermondsey Street
London SE1 3UD
http://www.amicus-cphva.org
(Affiliated to Amicus)
Department of Health
Richmond House
79 Whitehall
London SW1A 2NS
http://www.dh.gov.uk
Equal Opportunities Commission
Arndale House
Arndale Centre
Manchester M4 5EQ
http://www.eoc.org.uk
GMB
22/24 Worple Road
London SW19 4DD
http://www.gmb.org.uk
Health & Safety Executive
Rose Court
2 Southwark Bridge
London SE1 9HS
http://www.hse.gov.uk
Health Service Commissioner
13th Floor Millbank
Millbank Tower
London SW1P 4QP
http://www.health.ombudsman.org.uk
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
212
C3996_10.qxd 25/02/2004 18:37 Page 212
HM Customs and Excise
Dorset House
Stamford Street
London SE1 9PY
http://www.hmce.gov.uk
(Advice on bringing personal effects and goods into the UK)
Home Office
Immigration and Nationality Enquiry Bureau
Block C
Whitgift Centre
Wellesley Road
Croydon CR9 1AT
http://www.homeoffice.gov.uk
(Immigration and Nationality – information on entry visas
and work permits)
Immigration Advisory Service (IAS)
County House
190 Great Dover Street
London SE1 4YB
http://www.iasuk.org
(Independent charity that gives free confidential advice and
help with applying for entry clearance to the UK)
International Confederation of Midwives
10 Barley Mow Passage
London W4 4PH
International Council of Nurses (ICN)
3 Place Jean Marteau
1201 Geneva
Switzerland
http://www.icn.ch
USEFUL ADDRESSES AND WEB SOURCES
213
C3996_10.qxd 25/02/2004 18:37 Page 213
Mental Health Nurses’ Association (formerly CPNA)
Cals Meyn
Grove Lane
Hinton
Nr Chippenham
Wilts SN14 8HF
(Affiliated to Amicus)
Nurses Welfare Service
Victoria Chambers
16/18 Strutton Ground
London SW1P 2HP
Nursing and Midwifery Council (NMC)
Overseas Registration
23 Portland Place
London W1N 3PZ
http://www.nmc-uk.org
(Provides information about registering as a nurse or midwife
in the UK)
Royal College of Midwives
15 Mansfield Street
London W1G 9NH
http://www.rcm.org.uk
Royal College of Nursing of the United Kingdom
20 Cavendish Square
London W1M 0AB
http://www.rcn.org.uk/whyjoin/howtojoin
(Provides general information on how to become registered as
a nurse in the UK)
Royal Commonwealth Society
18 Northumberland Avenue
London WC2N 5BJ
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
214
C3996_10.qxd 25/02/2004 18:37 Page 214
Scottish Health Department
St. Andrew’s House
Regent Road
Edinburgh EH1 3DE
http://www.scotland.gov.uk
Unison (Head Office)
1 Mabledon Place
London WC1H 9HA
http://www.unison.org.uk
World Health Organisation
Avenue Appia
1211 Geneva 27
Switzerland
http://www.who.org
Web resources
Citizens Advice Bureaux (CAB) – give free advice on many
issues. Branches can be found in most large towns and cities:
http://www.adviceguide.org.uk
Foreign and Commonwealth Office – gives details about visa
requirements for visitors wishing to enter the UK:
http://www.fco.gov.uk
International English Language Testing System – useful informa-
tion about the IELTS test and the centres which run the test,
etc.: http://www.ielts.org
Nursing courses – full guide to nursing courses in the UK:
http://www.nursingcourses.co.uk
Nursing in the UK – information about immigration procedures:
http://www.nursingintheuk.co.uk
NursingNetUK – information about nursing in the UK, job vacan-
cies and courses: http://www.nursingnetuk.com
Nursing Times – information about the weekly journal, nursing
issues, and job vacancies on NT Job Alert:
http://www.nursingtimes.net
USEFUL ADDRESSES AND WEB SOURCES
215
C3996_10.qxd 25/02/2004 18:37 Page 215
Office of the Immigration Services Commissioner – UK govern-
ment regulator for immigration services. Information and
complaints: http://www.oisc.gov.uk
University of Sheffield School of Nursing and Midwifery –
supports international students in a wide variety of academic
programmes:
http://www.snm.shef.ac.uk/snm/internat/internat.htm
INFORMATION FOR PATIENTS AND FAMILIES
Addresses and websites
Action for Sick Children
300 Kingston Road
London SW20 8LX
http://www.actionforsickchildren.org
Age Concern (England)
1268 London Road
London SW16 4ER
http://www.ace.org.uk
Alcoholics Anonymous
PO Box 1
Stonebow House
Stonebow
York YO1 2NJ
http://www.alcoholics-anonymous.org.uk
Alzheimer’s Society
Gordon House
10 Greencoat Place
London SW1P 1PH
http://www.alzheimers.org.uk
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
216
C3996_10.qxd 25/02/2004 18:37 Page 216
Arthritis Care
18 Stephenson Way
London NW1 2HD
http://www.arthritiscare.org.uk
Association of Carers
20–25 Glasshouse Yard
London EC1A 4JS
Breast Cancer Care
Kiln House
210 New King’s Road
London SW6 4NZ
http://www.breastcancercare.org.uk
British Association for Cancer United Patients BACUP
3 Bath Place
Rivington Street
London EC2 3JR
http://www.cancerbacup.org.uk
British Colostomy Association
15 Station Road
Reading RG1 1LG
http://www.bcass.org.uk
British Deaf Association
1–3 Worship Street
London EC2A 2AB
http://www.bda.org.uk
British Epilepsy Association
New Anstey House
Gate Way Drive
Leeds LS3 1BE
http://www.epilepsy.org.uk
USEFUL ADDRESSES AND WEB SOURCES
217
C3996_10.qxd 25/02/2004 18:37 Page 217
British Heart Foundation
14 Fitzhardinge Street
London W1H 4DH
http://www.bhf.org.uk
British Pregnancy Advisory Service
Austy Manor
Wootton Wawen
Solihull
West Midlands B95 6BX
http://www.bpas.org.uk
British Red Cross
9 Grosvenor Crescent
London SW1X 7EJ
http://www.redcross.org.uk
Capability (formerly Spastics Society)
12 Park Crescent
London W1N 4EQ
Diabetes UK
10 Queen Anne Street
London W1M 0BD
http://www.diabetes.org.uk
Disabled Living Foundation
380–384 Harrow Road
London W9 2HU
http://www.dlf.org.uk
Ileostomy & Internal Pouch Support Group
Amblehurst House
PO Box 23
Mansfield NG18 4TT
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
218
C3996_10.qxd 25/02/2004 18:37 Page 218
Leukaemia Society
14 Kingfisher Court
Venny Bridge
Pinhoe
Exeter EX4 8JN
Macmillan Cancer Relief
89 Albert Embankment
London SE1 7UQ
http://www.macmillan.org.uk
MIND – National Association for Mental Health
Granta House
15–19 Broadway
London E15 4BQ
http://www.mind.org.uk
Multiple Sclerosis Society
National Centre
372 Edgware Road
London NW2 6ND
http://www.mssociety.org.uk
National Aids Trust
New City Cloisters
196 Old Street
London EC1V 9FR
http://www.nat.org.uk
National Asthma Campaign
Providence House
Providence Place
London N1 0NT
http://www.asthma.org.uk
USEFUL ADDRESSES AND WEB SOURCES
219
C3996_10.qxd 25/02/2004 18:37 Page 219
National Society for the Prevention of Cruelty to Children
(NSPCC)
42 Curtain Road
London EC2A 3NH
http://www.nspcc.org.uk
Royal National Institute of the Blind (RNIB)
105 Judd Street
London WC1H 9NE
http://www.rnib.org.uk
Royal National Institute for the Deaf (RNID)
19–23 Featherstone Street
London EC1Y 8SL
http://www.rnid.org.uk
St. Andrews Ambulance Association
St. Andrew’s House
48 Milton Street
Glasgow G4 0HR
http://www.firstaid.org.uk
St. John Ambulance Association & Brigade
1 Grosvenor Crescent
London SW1X 7EF
http://www.sja.org.uk
Sickle Cell Society
54 Station Road
Harlesden
London NW10 4UA
http://www.sicklecellsociety.org
Stillbirth & Neonatal Death Society (SANDS)
28 Portland Place
London W1N 4DE
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
220
C3996_10.qxd 25/02/2004 18:37 Page 220
Stroke Association
123–127 Whitecross Street
London EC1Y 8JJ
http://www.stroke.org.uk
Terrence Higgins Trust
52–54 Grays Inn Road
London WC1X 8JU
http://www.tht.org.uk
USEFUL ADDRESSES AND WEB SOURCES
221
C3996_10.qxd 25/02/2004 18:37 Page 221
C3996_10.qxd 25/02/2004 18:37 Page 222
This page intentionally left blank
Units of measurement
UNITS OF MEASUREMENT: INTERNATIONAL SYSTEM
OF UNITS (SI),THE METRIC SYSTEM AND
CONVERSIONS
In the UK we use the International System of Units (SI) or
Système International d’Unités measurement system for scientific,
medical and technical purposes. The SI units have replaced those
of the Imperial System. For example, the kilogram is used for
weight (or mass) instead of the pound, and the metre for length
instead of yards, feet and inches. However, in everyday life you
will still see a mix of units used in shops and hear people talk
about pounds, and feet and inches. For example, they will ask for
a pound of apples and describe someone being 5 foot 3 inches in
height and 10 stone in weight.
The SI comprises seven base units, with several derived units.
Each unit has its own symbol and is expressed as a decimal mul-
tiple or submultiple of the base unit by using the appropriate pre-
fix (e.g. a millimetre is one-thousandth of a metre).
Base units
223
1
11
Quantity
Base unit and symbol
Length
metre (m)
Mass
kilogram (kg)
Time
second (s)
Amount of substance
mole (mol)
Electric current
ampere (A)
Thermodynamic temperature
kelvin (°K)
Luminous intensity
candela (cd)
C3996_11.qxd 25/02/2004 18:46 Page 223
Derived units
Derived units for measuring different quantities are reached by
multiplying or dividing two or more of the seven base units.
Factor, decimal multiples and submultiples of SI units
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
224
Quantity
Derived unit and symbol
Work, energy, quantity of heat
joule (J)
Pressure
pascal (Pa)
Force
newton (N)
Frequency
hertz (Hz)
Power
watt (W)
Electrical potential, electromotive force,
volt (v)
potential difference
Absorbed dose of radiation
gray (Gy)
Radioactivity
becquerel (Bq)
Dose equivalent
sievert (Sv)
Multiplication factor
Prefix
Symbol
10
12
tera
T
10
9
giga
G
10
6
mega
M
10
3
kilo
k
10
2
hecto
h
10
1
deca
da
10
–1
deci
d
10
–2
centi
c
10
–3
milli
m
10
–6
micro
m
10
–9
nano
n
10
–12
pico
p
10
–15
femto
f
10
–18
atto
A
C3996_11.qxd 25/02/2004 18:46 Page 224
Rules for using units and writing large numbers and
decimals
— The symbol for a unit is unaltered in the plural and should not
be followed by a full stop/point except at the end of a sen-
tence: i.e. 2 cm, not 2 cm. or 2 cms.
— Large numbers are written in three-digit groups (working from
right to left) with spaces not commas (in some countries the
comma is used to indicate a decimal point): e.g. forty thousand
is written as 40 000, four-hundred thousand is written as
400 000.
— Numbers with four numbers are written without the space: e.g.
six thousand is written as 6000.
— The decimal sign between numbers is indicated by a full
stop/point placed near the line: e.g. 40.75. If the numerical
value of the decimal is less than 1, a zero should appear before
the decimal sign: i.e. 0.125, not .125.
— Decimals with more than four numbers are also written in
three-digit groups, but this time working from left to right: e.g.
0.000 25.
— ‘Squared’ and ‘cubed’ are expressed as numerical powers and
not by abbreviation: e.g. square centimetre is cm
2
, not sq. cm.
Commonly used measurements requiring further
explanation
— Volume: volume is calculated by multiplying length, width and
depth. Using the SI unit for length, the metre (m), means end-
ing up with a cubic metre (m
3
), which is a huge volume and
it is not appropriate for most uses. In clinical practice the litre
(L or l) is used. A litre is based on the volume of a cube meas-
uring 10 cm × 10 cm × 10 cm. Smaller units still, e.g. millilitre
(mL) or one-thousandth of a litre, are commonly used in clin-
ical practice.
— Pressure: the SI unit of pressure is the pascal (Pa), and the
kilopascal (kPa) replaces the old non-SI unit of millimetres of
UNITS OF MEASUREMENT
225
C3996_11.qxd 25/02/2004 18:46 Page 225
mercury pressure (mmHg) for blood pressure and blood gases.
However, mmHg are still widely used for measuring blood
pressure. Other anomalies include: cerebrospinal fluid, which
is measured in millimetres of water (mmH
2
O); and central
venous pressure, which is measured in centimetres of water
(cmH
2
O).
— Temperature: although the SI base unit for temperature is the
kelvin, by international convention temperature is measured in
degrees Celsius (°C).
— Energy: the energy of food or individual requirements for
energy are measured in kilojoules (kJ); the SI unit is the joule
(J). In practice, many people still use the kilocalorie (kcal), a
non-SI unit, for these uses. 1 calorie = 4.2 J; 1 kilocalorie (large
Calorie) = 4.2 kJ.
— Time: the SI base unit for time is the second (s), but it is
acceptable to use minute (min), hour (h) or day (d). In clini-
cal practice it is preferable to use ‘per 24 hours’ for the excre-
tion of substances in urine and faeces: i.e. g/24 h.
— Amount of substance: the SI base unit for amount of substance
is the mole (mol). The concentration of many substances is
expressed in moles per litre (mol/L) or millimoles per litre
(mmol/L), which replaces milliequivalents per litre (mEq/L).
Some exceptions exist and include: haemoglobin and plasma
proteins, which are given in grams per litre (g/L); and enzyme
activity, which is given in International Units (IU, U or iu).
MEASUREMENTS, EQUIVALENTS AND CONVERSIONS
(SI OR METRIC AND IMPERIAL)
Volume
1 litre (L) = 1000 millilitres (mL)
1 millilitre (mL) = 1000 microlitres (mL)
Note: The millilitre (mL) and the cubic centimetre (cm
3
) are usu-
ally treated as being equivalent.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
226
C3996_11.qxd 25/02/2004 18:46 Page 226
Conversions
1 litre (L) = 1.76 pints (pt)
568.25 millilitres (mL) = 1 pint (pt)
28.4 millilitres (mL) = 1 fluid ounce (fl oz)
Length
1 kilometre (km) = 1000 metres (m)
1 metre (m) = 100 centimetres (cm) or 1000 millimetres (mm)
1 centimetre (cm) = 10 millimetres (mm)
1 millimetre (mm) = 1000 micrometres (mm)
1 micrometre (mm) = 1000 nanometres (nm)
Conversions
1 metre (m) = 39.370 inches (in)
1 centimetre (cm) = 0.3937 inches (in)
30.48 centimetres (cm) = 1 foot (ft)
2.54 centimetres (cm) = 1 inch (in)
Weight or mass
1 kilogram (kg) = 1000 grams (g)
1 gram (g) = 1000 milligrams (mg)
1 milligram (mg) = 1000 micrograms (mg)
1 microgram (mg) = 1000 nanograms (ng)
Note: To avoid any confusion with milligram (mg) the word
microgram (mg) should be written in full on prescriptions.
UNITS OF MEASUREMENT
227
C3996_11.qxd 25/02/2004 18:46 Page 227
Conversions
1 kilogram (kg) = 2.204 pounds (lb)
1 gram (g) = 0.0353 ounce (oz)
453.59 grams (g) = 1 pound (lb)
28.34 grams (g) = 1 ounce (oz)
Temperature conversions
To convert Celsius to Fahrenheit, multiply by 9, divide by 5, and
add 32 to the result. For example, to convert 36°C to Fahrenheit:
36 × 9 = 324 ∏ 5 = 64.8 + 32 = 96.8ºF
therefore 36ºC = 96.8ºF.
To convert Fahrenheit to Celsius, subtract 32, multiply by 5,
and divide by 9. For example, to convert 104ºF to Celsius:
104 – 32 = 72 × 5 = 360 ∏ 9 = 40ºC
therefore 104ºF = 40ºC.
Temperature comparison
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
228
°Celsius
°Fahrenheit
100
212
95
203
90
194
85
185
80
176
75
167
70
158
65
149
60
140
55
131
50
122
45
113
C3996_11.qxd 25/02/2004 18:46 Page 228
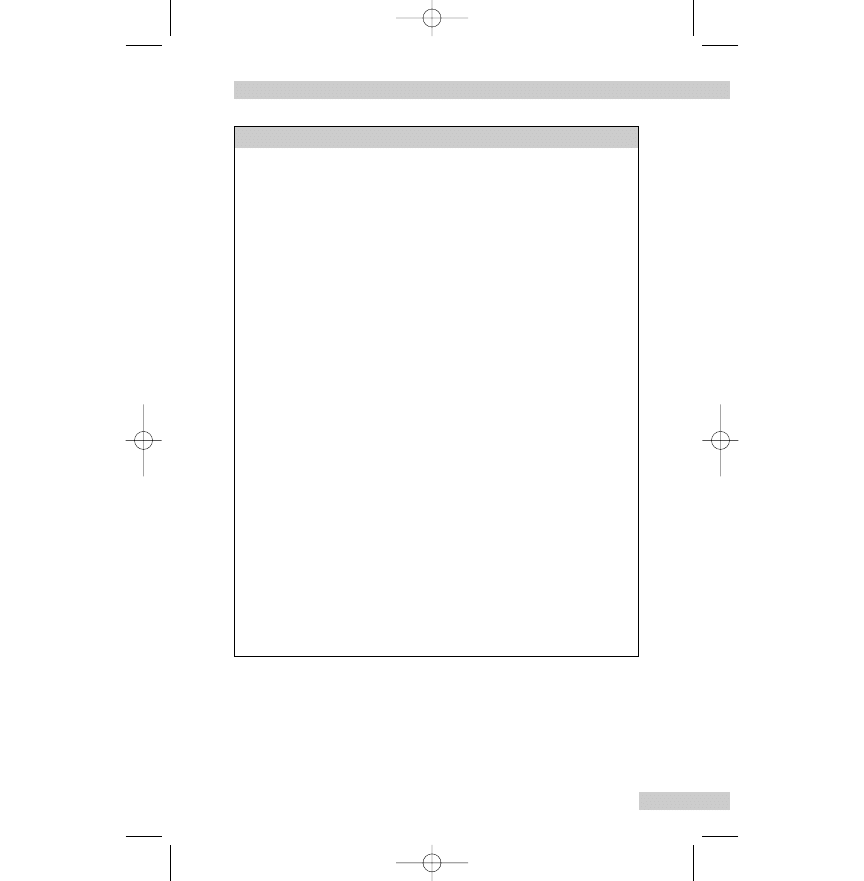
Note:
Boiling point = 100ºC = 212ºF
Freezing point = 0ºC = 32ºF
UNITS OF MEASUREMENT
229
°Celsius
°Fahrenheit
44
112.2
43
109.4
42
107.6
41
105.8
40
104
39.5
103.1
39
102.2
38.5
101.3
38
100.4
37.5
99.5
37
98.6
36.5
97.7
36
96.8
35.5
95.9
35
95
34
93.2
33
91.4
32
89.6
31
87.8
30
86
25
77
20
68
15
59
10
50
5
41
0
32
–5
23
–10
14
C3996_11.qxd 25/02/2004 18:46 Page 229
FURTHER READING
Gatford JD, Phillips N 2002 Nursing calculations, 6th edn.
Churchill Livingstone, Edinburgh.
PARKINSON AND BROOKER: EVERYDAY ENGLISH FOR INTERNATIONAL NURSES
230
C3996_11.qxd 25/02/2004 18:46 Page 230
General further reading
suggestions
Brooker C (ed) 2002 Churchill Livingstone’s dictionary of nurs-
ing, 18th edn. Churchill Livingstone, Edinburgh.
Brooker C, Nicol M (eds) 2003 Nursing adults: the practice of
caring. Mosby, Edinburgh.
Ellis RB, Gates B, Kenworthy N 2003 Interpersonal communica-
tion in nursing. Churchill Livingstone, Edinburgh.
Gunn C 2001 Using maths in health sciences. Churchill
Livingstone, Edinburgh.
Hoban V 2003 How to ... communicate better with your col-
leagues. Nursing Times 99:64–65.
Hutton A 2002 An introduction to medical terminology for
health care. A self-teaching package, 3rd edn. Churchill
Livingstone, Edinburgh.
MacConnachie AM, Hay J, Harris J, Nimmo S 2002 Drugs in
nursing practice. An A–Z guide, 6th edn. Churchill
Livingstone, Edinburgh.
Nicol M, Bavin C, Bedford-Turner S, et al 2004 Essential nursing
skills, 2nd edn. Mosby, Edinburgh.
Richards A, Edwards S 2003 A nurse’s survival guide to the
ward. Churchill Livingstone, Edinburgh.
Royal College of Nursing (RCN) 2003 Here to stay. International
nurses in the UK. Available:
www.rcn.org.uk/professional/publications/heretostay-irns.pdf
Wallace M 2002 Churchill Livingstone’s A–Z guide to profession-
al healthcare. Churchill Livingstone, Edinburgh.
231
C3996_12.qxd 25/02/2004 18:47 Page 231
C3996_12.qxd 25/02/2004 18:47 Page 232
This page intentionally left blank
Index
233
abbreviations 193–209
accident prevention 68–72
Accreditation of Prior Experience
and Learning (APEL) 17
Activities of Living Model of
Nursing 9, 51
Acute Care Trusts, NHS 17, 27, 30–4
medical staff 33
nursing staff 30–3
professions allied to medicine
and other staff 34
adaptation programmes (supervised
practice) 17–18, 20
allergies 56
Ambulance Service 30
ambulance trusts 30
anxiety 108
case histories 108–13
words associated with 108
arm, idioms for 141–2
assisted conception, colloquial
terms for 136
back, idioms for 142–4
biographical data 53–4
blood, idioms for 144–5
body function, colloquial terms for
126–9
body parts 142, 143, 144
colloquial terms for 123–6
idioms 141–67
bone, idioms for 145
brain, idioms for 145–6
break, phrasal verbs for 170
breast, idioms for 146
breathing 59–60
case history 60–4
words associated with 61
bring, phrasal verbs for 170–1
British Council 18
brow(s), idioms for 146
career development 21–2
cheek, idioms for 146
chest, idioms for 147
chin, idioms for 147
cleansing and dressing 89–92
clinical nurse specialist (CNS) 32
Code of Professional Conduct 3–4,
37
come, phrasal verbs for 171–3
communicating
case histories 65–8
words associated with 64
communication
anxiety, stress and depression
108–13
breathing 59–60
dementia and confusion 113–17
eating and drinking 78–84
elimination 84–9
mobility 72–8
pain 117–21
personal care 89–94
safety and accident prevention
68–72
sexuality 103–8
sleeping 94–8
starting 52–9
words associated with 64–8
C3996_13.qxd 26/02/2004 13:59 Page 233
INDEX
234
working and playing 98–103
communication in English, tests for
18–19
community mental health nurses 29
community midwives 29
Community NHS Trust 27
community nurses 5–6
community pharmacists 31
conception, assisted, colloquial
terms for 136
confusion 113
case histories 113–17
words associated with 114
contact with health/social care
professionals 58–9
continuing professional develop-
ment (CPD) 4, 19–20
curriculum vitae (CV) 21
cut, phrasal verbs for 173–4
dementia 113
case histories 113–17
words associated with 114
dental nurses 31
dentists 31
Department of Health (DoH) 26–7
depression 108
case histories 108–13
words associated with 108
dieticians 28, 59
district nurses (DNs) 28–9
do, phrasal verbs for 174–5
documentation 37–46
NMC guidelines for 45–6
dressing 89–92
drinking 78–84
drug chart 43
drugs 56–7
ears, idioms for 147–8
eating and drinking 78
case histories 78–84
words associated with 79
elbow, idioms for 148
electronic mail (e-mail) 49–50
elimination 84
case histories 84–9
words associated with 85
e-mail 49–50
employment history 54–5
endearments 52
English as a Second Language
(ESOL) 21
evidence-based care 1, 9
eye, idioms for 148–9
face, idioms for 149–50
family history 56
family planning, colloquial terms
for 136
feet, idioms for 151–2
fertility clinic, colloquial terms for
136
find, phrasal verbs for 175
fingers, idioms for 150–1
fit, phrasal verbs for 175
Five ‘C’s of good nursing practice 7
flesh, idioms for 151
fluid balance chart 39, 42
foot (feet), idioms for 151–2
forehead, idioms for 146
forms of address 52
general expressions 132–3
General NHS Hospital Trust 27
general practitioner (GP) 5, 26, 28,
31, 55, 59
General Test (IELTS) 18
get, phrasal verbs for 175–7
give, phrasal verbs for 177–8
go, phrasal verbs for 178–81
grades, nursing 32–3
hair, idioms for 152
hand, idioms for 152–4
head, idioms for 154–6
C3996_13.qxd 26/02/2004 13:59 Page 234
INDEX
235
health behaviour see lifestyle
health visitors (HV) 29
healthcare assistants (HCAs) 5
heart, idioms for 156–7
heel(s), idioms for 157–8
hobbies and interests 58
holistic care 1
home, type of 57–8
Hospital for Sick Children in
London 27
idioms – parts of the body 141–67
incident/accident form 44–5
informed consent 43–4
integrated care 1
International Council of Nurses
(ICN) 5
International English Language
Testing System (IELTS) 18–19,
21
job interview, preparing for 21–2
job vacancies 21
keep, phrasal verbs for 181–2
knee, idioms for 158
knuckles, idioms for 158
lap, idioms for 158
lecturer–practitioner 32, 33
leg, idioms for 158–9
leisure see working and playing
let, phrasal verbs for 182
letter writing 46–9
envelope 46–7
letter 47–9
lifestyle 59
lip, idioms for 159
look, phrasal verbs for 182–4
make, phrasal verbs for 184
medical history 56
medical names, colloquial terms
for 137–40
medicine/drug chart 43
men’s health expressions 134
mental states, colloquial terms for
129–31
mind, idioms for 159–60
mobility 72–3
case histories 73–8
words associated with 73
modern matron 32
mouth, idioms for 160
nail(s), idioms for 161
National Health Service (NHS) 5–7
structure 26–34
National Institute for Clinical
Excellence (NICE) 26
National Nursing Association
(NNA) 5
neck, idioms for 161–2
nerve(s), idioms for 162
neurological observation chart –
Glasgow Coma Scale (GCS) 39,
40–1
next of kin 53
NHS see National Health Service
NHS Direct 26
NHS Plan for England 10
NHS Trusts see Acute Care Trusts,
NHS
nose, idioms for 162–3
Notification of Practice form 19
nurse consultant 32
nurse education programmes 5, 15
nurse practitioners 28
Nurse Prescribers’ Formulary 28
Nurse Registration Act (1919) 13
Nursing and Midwifery Council
(NMC) 13, 14
Code of Professional Conduct
3–4
C3996_13.qxd 26/02/2004 13:59 Page 235
Professional Identification
Number (PIN) 16, 17
role of 2
website 21
nursing assessment 8
nursing assessment sheet 38
nursing care plan 8–9, 38–9, 51, 52
nursing degrees 22
nursing process 7–9
nursing programmes 14–19
occupational health nurses 6
occupational therapists (OTs) 28, 59
opticians 31
optometrists 31
outpatient departments 6
pain 117–21
case history 120–1
commonly used words 118–19
words associated with 117
palm, idioms for 163
periodic registration 2–4, 19–20
personal care 89
case histories 89–94
words associated with 90
phrasal verbs 169–91
physical function 57
physical states, colloquial terms for
129–31
physiotherapists 28, 34, 59
podiatrists 28, 59
postgraduate dental surgeons 31
post-registration education and
practice (PREP) 19–20
practice nurse 28, 55, 59
Primary Care Trusts (PCTs) 17, 27–9
Primary Healthcare Teams (PHCTs)
28–9
private sector 5–7
Professional Identification Number
(PIN) 16, 17
professional organisations 4–5
INDEX
236
professions allied to medicine 34
Project 2000 (PK2) 5
Psychiatric NHS Trust 27
put, phrasal verbs for 185–6
qualifications 22
for registration 16–17
reason for admission/treatment 55–7
record keeping 37–46
reflection 121
reflective diary 20
Registered Nurses 13, 16, 28, 32–3
registration
adaptation programmes (super-
vised practice) 17–18
communication in English
18–19
continuing professional devel-
opment (CPD) 4, 19–20
obtaining 14–19
periodic registration 19
qualifications 16–17
requirements 13
regulation in the UK 2–4
religion 53–4
reproductive health problems,
colloquial terms for 133–7
reviews 22
role of nurses, expanding 10–11
Royal College of Midwives (RCM) 5
Royal College of Nursing (RCN) 4, 5
run, phrasal verbs for 187–8
safety and accident prevention 68
case histories 68–72
words associated with 69
salary grade 22
secondary hospital care 30–4
self-care model 9
send, phrasal verbs for 188
set, phrasal verbs for 188
sexual health expressions 135–6
C3996_13.qxd 26/02/2004 13:59 Page 236
sexuality 103
case histories 103–8
words associated with 103
sexually transmitted (acquired)
infections, colloquial terms for
136–7
shoulder, idioms for 163
skin
care 92–4
idioms for 164
skull, idioms for 164
sleeping 94
case history 94–8
words associated with 95
SMART system 38, 39
social history 57–9
social problems due to present
condition/admission 58
Social Services 34
Special Trusts 27
speech and language therapists
(SLTs) 31
Standing Committee of Nurses in
Europe 5
stomach, idioms for 164
Strategic Health Authorities (SHAs)
27
stress 108
case histories 108–13
words associated with 108
support networks 57
INDEX
237
take, phrasal verbs for 188–90
task-based care 1
teeth, idioms for 166–7
throat, idioms for 165
thumb, idioms for 165
titles 52
toe(s), idioms for 165
tongue, idioms for 166
tooth, idioms for 166–7
trade unions 4–5
turn, phrasal verbs for 190–1
UK Central Council for Nursing,
Midwifery and Health Visiting
(UKCC) 13
Unison 4
units of measurement 223–9
useful addresses 211–21
vital signs chart 39
websites 211–221
web resources 215–16
women’s health expressions 133–4
work history 54–5
working and playing 98
case histories 98–103
words associated with 99
C3996_13.qxd 26/02/2004 13:59 Page 237
Document Outline
- Contents
- 1. Nursing in the UK
- 2. Registering as a nurse in the UK and career development
- 3. The National Health Service and Social Services
- 4. Nursing documentation, record keeping and written communication
- 5. Communication in nursing
- 6. Colloquial English
- 7. Idioms: parts of the body
- 8. Phrasal verbs
- 9. Abbreviations used in nursing
- 10. Useful addresses and web sources
- 11. Units of measurement
- General further reading suggestions
- Index
Wyszukiwarka
Podobne podstrony:
English for International Tourism Pre Intermediate WB
English for International Tourism Pre Intermediate WB
English for Presentations and International Conferences
English for CE materials id 161873
Flash on English for Mechanics, Electronics and Technical Assistance
English for Mathematics
English for Medical S&D Practic Nieznany (3)
English for Medical S&D Practic Nieznany (2)
Bank for International Settlements
English for Medical S&D Practic Nieznany
English for CE EE and water id Nieznany
Flash on English for Cooking, Catering and Reception keys
English for advanced
English For Law Vocabulary
norsk grammatik for internasjonale studenter
English for Geometry
From Stabilisation to State Building, (DEPARTMENT FOR INTERNATIONAL?VELOPMENT)
English?stract 1 for passive(1)
English for CE materials id 161873
więcej podobnych podstron