Iranian Journal of Clinical Infectious Disease 2006;1(3):149-155
Iranian Journal of Clinical Infectious Diseases
2006;1(3):149-155
©2006 IDTMRC, Infectious Diseases and Tropical Medicine Research Center
Epidemiology of Shigella species isolated from diarrheal children
and drawing their antibiotic resistance pattern
Rasoul Yousefi Mashouf
1
, Ali Akbar Moshtaghi
2
, Seyyed Hamid Hashemi
3
1
Department of Microbiology, Hamadan University of Medical Sciences, Hamadan, Iran.
2
Department of Pediatric, Hamadan University of Medical Sciences, Hamadan, Iran.
3
Department of Infection Diseases and Tropical Medicine, Hamadan University of Medical Sciences, Hamadan, Iran.
ABSTRACT
Background: Shigellosis accounts for majority of cases of bacterial diarrhea in infants in developing countries. The
present study was conducted to determine the distribution and pattern of antimicrobial resistance of Shigella species
among children 0-14 years of age with acute diarrhea in Hamadan.
Materials and methods: The study included all acute diarrhea patients who admitted in the pediatric department from
January 2001 to December 2004. Antibiogram test was performed by gel-diffusion method and ten commonly used
antibiotics were applied.
Results: Of 1686 stool samples, 166 (9.8%) were positive for Shigella species. Shigella flexneri was the predominant
serogroup (40.3%) followed by S. dysentriae (33.7%), S. boydii (15.1%) and S. sonnei (10.8%). Of Shigella isolates,
91% were resistant to one or more antimicrobial agent(s), and 88% were multi-drug resistant. Most strains were resistant
to chloramphenicol (90%), ampicillin (89%), co-trimoxazole (84%), tetracycline (83%) and nalidixic acid (51%).
Resistance to amoxicillin-clavulanic acid (co-amoxiclav), ceftriaxone, amikacin, nitrofurantoin and ciprofloxacin was
observed in 34.9%, 23.4%, 6.6%, 3.6% and 1.8% of the isolates, respectively. Emerging resistance against nalidixic acid
(42.3%) was observed.
Conclusion: Our experiences suggest that Shigella species could be an important etiological agent of diarrhea in this
area, while the drugs of choice for the treatment of Shigella infection should be ciprofloxacin and nitrofurantoin.
Amikacin was the third drug of choice.
Keywords: Diarrhea, Shigella, Antibiotic, Resistance, Children.
(Iranian Journal of Clinical Infectious Diseases 2006;1(3):149-155).
INTRODUCTION
1
Diarrheal diseases remain a major cause of
morbidity and mortality in all age groups,
especially in developing countries including Iran
(1,2). In our country, diarrhea is estimated for the
Received: 12 March 2006 Accepted: 18 July 2006
Reprint or Correspondence: Rasoul Yousefi, PhD.
1
Department of Microbiology, Hamadan University of Medical
Sciences, Hamadan, Iran.
E-mail: yousefimash@yahoo.com
third leading cause of overall morbidity and the
leading cause of infant mortality (3).
Shigellosis occurs both in epidemic and
endemic forms in children and remains a major
public health problem in developing countries
(4,5). In a study conducted from 1997 to 1999,
Shigella (S.) flexneri was found to be the most
frequently isolated organism from diarrheal
patients in a community setting in Jakarta (6).
ORIGINAL ARTICLE

150 Epidemiology of Shigella in Hamadan
Iranian Journal of Clinical Infectious Disease 2006;1(3):149-155
Similarly, S. flexneri was the most common
organism isolated in four low socio-economic areas
of Karachi between January 2002 and March 2003
(7). The attack rate of shigellosis in India is 1-15%
and bacillary dysentery is responsible for
approximately 10% of deaths in children (2,8,9).
In another study from Bangladesh (10), Shigella
species were the most common isolated species
from patients with acute diarrhea and S. flexneri
(54 %) was the most frequently isolated one,
followed by S. dysenteriae, S. boydii and S. sonnei.
An investigation from Bahia, Brazil was also
revealed that the shigellosis was the predominant
cause of acute diarrhea, while S. sonnei (80.1%)
was the most common isolated organism followed
by S. flexneri (19.9%) (5). Shigellosis is also an
important cause of infectious diarrhea in Iran (3),
mostly community-acquired, caused mainly by S.
flexneri and S. dysenteriae.
Over the past decades, Shigella species have
become progressively resistant to most of the
widely used and inexpensive antibiotics (11-14).
Resistance has emerged even to newer, more potent
antimicrobial agents. Moreover, a change in the
incidence of Shigella subgroups from time to time
makes it difficult to formulate a drug of choice for
Shigellosis (2,15,16). Prior to this study, the
antibiotic resistance pattern of Shigella isolates has
not been previously determined in this region.
Therefore, this study was carried out to identify
and to establish the antimicrobial resistance pattern
of the most important Shigella serotypes involved
in the epidemiology of acute diarrhea in children
who admitted in the pediatric department of
hospitals in Hamadan.
PATIENTS and METHODS
A prospective study was conducted on children
with acute diarrhea and dysentery between 0 and
14 years of age from January 2001 to December
2004 who were admitted in the pediatric
departments of two hospitals (Ghaem and Ekbatan)
in Hamadan. A total of 1686 stool samples were
examined for Shigella species, then isolates were
serotyped and their antibiotics susceptibilities were
determined. Only one Shigella isolate per patient
per diarrheal episode was included in the analysis.
No outbreak has been detected during the study
period.
Fecal samples were collected in Cary-Blair
transport medium and transferred immediately to
the laboratories of hospitals. Cultivation and
isolation of organisms were performed according to
the methods outlined in the Bailey & Scott’s
Diagnostic Microbiology (17).
The samples were
cultured into GN broth and plated onto Salmonella-
Shigella (SS) agar and MacConkey agar (Merck,
Germany). Plates were incubated at 37°C for
selective isolation of Shigellae and were examined
after 18-24h of incubation. Suspected colonies
were inoculated into Triple sugar iron agar
(Oxoid), Mannitol motility medium (Hi-media,
India), Urea medium (Hi-media), and peptone
water (1% Bactopepton, Difco; pH 7.2) for
biochemical identification of Shigellae.
Shigella serotypes were identified using
standard commercially available polyvalent and
monovalent antisera (Wellcome Research
Laboratories, Beckenham, UK). Single colonies of
isolates were tested serologically by slide and tube
agglutination with specific antisera against Shigella
sonnei, Shigella flexneri, Shigella boydii and
Shigella dysenteriae, according to the standard
protocols (17).
In order to draw the susceptibility patterns of
isolates, they were tested by disk
diffusion method
using guidelines established by the National
Committee for Clinical Laboratory Standards
(NCCLS) (18). A total of 10 selected antibiotic
disks (Mast Group LTD, UK) including
chloramphenicol (CHL, 30µg), co-amoxiclav
(AMC, 20µg), amikacin (AMK, 30µg), ampicillin
(AMP10µg), ceftriaxone (CRO, 30µg),
ciprofloxacin (CIP, 5µg), co-trimoxazole (TMP-
SXZ, 25µg), nitrofurantoin (NIT, 300µg), nalidixic
Yousefi MR. et al 151
Iranian Journal of Clinical Infectious Disease 2006;1(3):149-155
acid (NAL, 30µg) and tetracycline (TET, 30µg)
were applied during the test. The
organisms used
for quality control were Escherichia coli (ATCC
25922; American Type Culture Collection) and
Staphylococcus aureus
(ATCC 25923).
The initial data including patient's age and sex
as well as types of microorganisms isolated from
stool cultures and their antimicrobial resistance
patterns were recorded in a special questionnaire.
Finally, data analysis was achieved by SPSS
software package (version 13.0, SPSS Inc., USA)
and discrete variables were compared by the χ
2
test.
RESULTS
During the study period, of 1686 stool samples,
166 (9.8%) were positive for Shigella species. S.
flexneri (40.3%) was the predominant serogroup
followed by S. dysenteriae (33.7%), S. boydii
(15.1%) and S. sonnei (10.8%). A number of
serotypes were isolated in each serogroup, 7
serotypes in S. flexneri, 5 in S. dysenteriae, 4 in S.
boydii, and Phase 1 & 2 in S. sonnei. The most
common S. flexneri serotypes were 2a (31.3%), 1b
(29.8%), and 2b (10.4%). The least common S.
flexneri serotype was 1a (4.4%). The most
common S. dysenteriae serotypes were type 1
(41.1%), type 2 (21.4%), and type 4 (16.1%), while
type 7 (5.3%) was the least common. Table 1
represents the serotype distribution of shigella
species (each isolate representing a case). Most of
shigella species were isolated from patients during
the first two years of study, 2001 and 2002 (25.9%
and 30.7%), respectively.
Of 166 patients, 89(53.6%) were male, and
15(9.1%) were younger than two years of age,
while 41(24.7%), 54(35.5%) and 51(30.7%) aged
3-6, 7-10, and 11-14 years, respectively. Table 2
presents the distribution frequencies of the age
groups of patients with Shigella. As shown in this
table, S. flexneri and S. dysenteriae were more
frequently observed in 7-10 and 11-14 year-old
group, respectively.
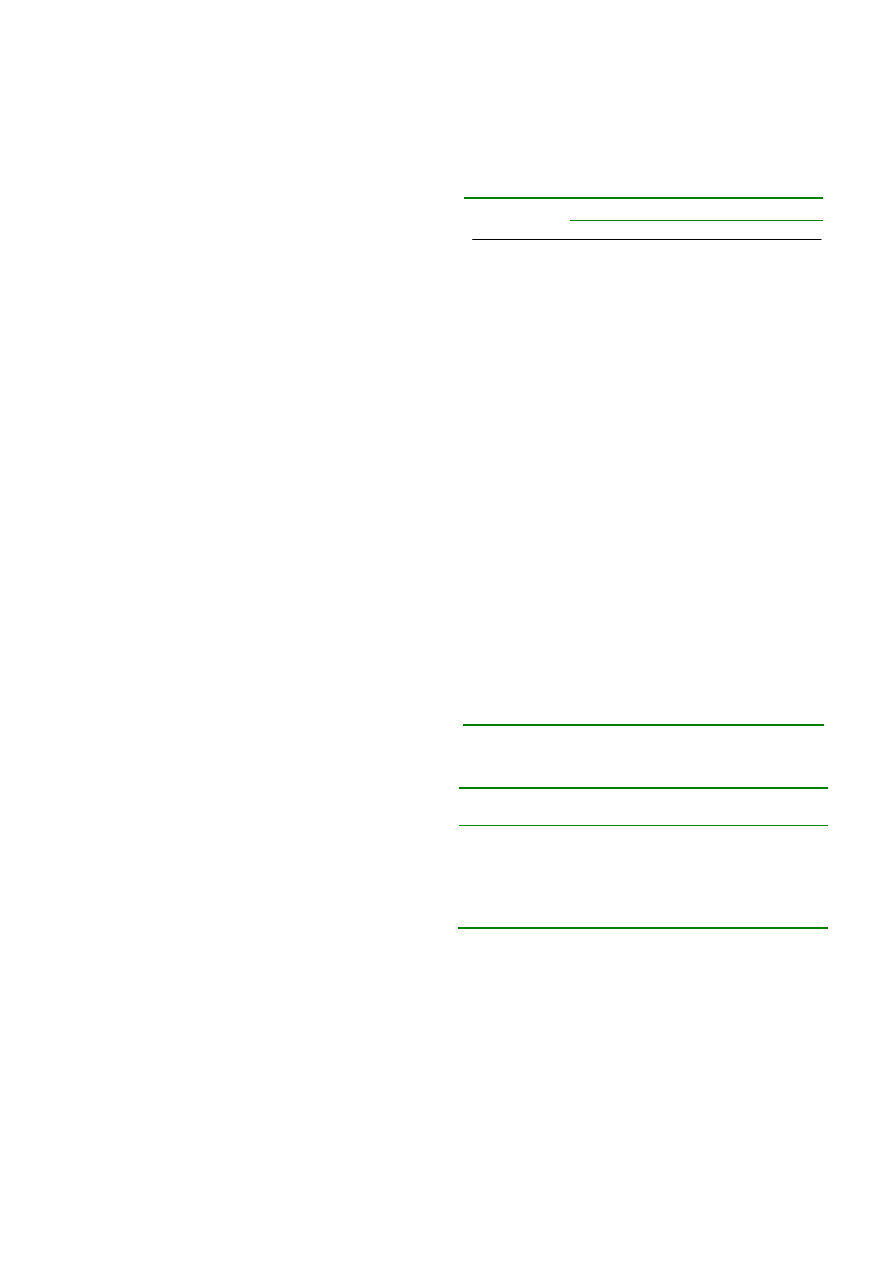
Table 1. Distribution of Shigella species and their
serotypes in Hamadan, 2001-2004
Studied years
2001 2002 2003 2004
Shigella
isolates
43(25.9) 51(30.7) 37(22.2) 35(21.1)
S. flexneri
18(26.8) 25(37.3) 13(19.4) 11(16.4)
Type 1a
0
0
2
1
Type 1b
5
8
4
3
Type 2a
9
5
3
4
Type 2b
1
4
2
0
Type 3a
0
2
0
2
Type 4a
2
4
0
1
Type 5
1
2
2
0
S.dysenteriae
15(26.7) 13(23.2) 15(26.7) 13(23.2)
Type 1
8
6
5
4
Type 2
3
2
5
2
Type 4
0
2
3
4
Type 5
2
3
0
3
Type 7
1
0
2
0
S. boydii
7(28.0) 6(24.0) 5(20.0) 7(28.0)
Type 3
3
2
1
2
Type 5
0
1
2
3
Type 9
2
0
1
2
Type 12
2
3
1
0
S. sonnei
3(16.6) 7(38.8) 4(22.2) 4(22.2)
Phase 1
3
5
3
4
Phase 2
0
2
1
0
Table 2. Distribution frequencies of the age groups of
patients according to Shigella species
Age group
(yrs)
S.flexneri S. dysenteria S. boydii S. sonnei
Total
0-2 6(3.6)
0
8(4.8)
1(0.06) 15(9.1)
3-6 19(11.4)
15(9.0)
4(2.4)
3(1.8)
41(24.7)
7-10 26(15.6)
18(10.8)
7(4.2)
8(4.8)
59(35.5)
11-14 16(9.6)
23(13.8)
6(3.6)
6(3.6)
51(30.7)
Total 67(40.3)
56(33.7)
25(15.1)
18(10.8) 166(100)
Of the Shigella isolates, 82.5% were resistant to
one or more of all tested antibiotics in this study (S.
dysenteriae 100%, S. flexneri 90%, S. sonnei 80%
and S. boydii 60%). Most strains were resistant to
chloramphenicol (90%), ampicillin (89%), co-
trimoxazole (84%), tetracycline (83%) and
nalidixic acid (51%). Resistance to co-amoxiclav,
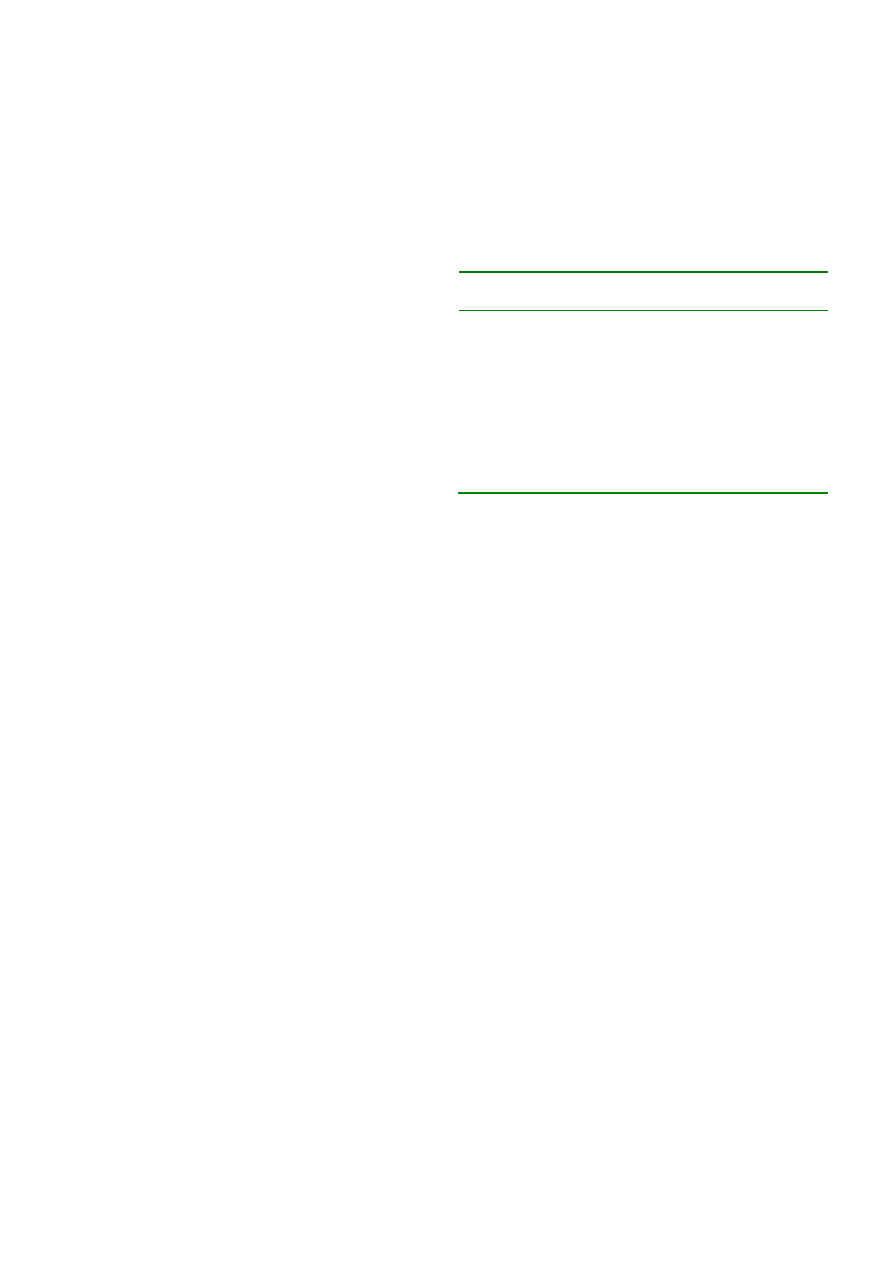
152 Epidemiology of Shigella in Hamadan
Iranian Journal of Clinical Infectious Disease 2006;1(3):149-155
ceftriaxone, amikacin, nitrofurantoin and
ciprofloxacin was observed in 34.9%, 23.4%,
6.6%, 3.6% and 1.8% of the isolates, respectively.
Emerging resistance against nalidixic acid (42.3%)
was observed. The antibiotics resistance
distribution of Shigella isolates is shown in table 3.
Shigella flexneri, S. dysenteriae and S. sonnei
shared
very similar susceptibility profile for most
of the tested antibiotics. The most frequent patterns
of resistance were
exhibited towards
chloramphenicol, ampicillin, co-trimoxazole,
tetracycline and co-amoxiclav (Table 3). S. boydii
showed slightly different susceptibility profile.
Resistance to nalidixic acid and ceftriaxone were
appeared to be different in four types of Shigella
isolates. S. dysenteriae isolates were more resistant
than isolates of S. flexneri, S. sonnei and S. boydii
to nalidixic acid (85.5% versus 44.7%, 38.8% and
0.0%, respectively, p<0.001). S. dysenteriae
isolates also were more resistant than other three
types of Shigella isolates to ceftriaxone (41.1%
versus 14.9%, 0.0% and 12.0%, p<0.001).
Seventy eight percent of the Shigella isolates
were multi-antibiotics resistant (resistance to at
least two antibiotics). Different resistance patterns
were defined in the four categories
of the Shigella
isolates. S. dysenteriae showed the highest multi-
antibiotics resistant, while S. boydii showed the
lowest. Twelve resistance patterns were observed
in S. dysenteriae, while 10 R-patterns in S. flexneri,
9 in S. sonnei and 7 in S. boydii. The most
prevalent multi-antibiotic resistance
pattern was
CHL
r
, AMP
r
, TMP-SXT
r
, TET
r
in all types of
Shigella isolates, namely,
37.6%, 32.6%, 28.2%
and 19.4% for S. dysenteriae, S. flexneri, S. sonnei
and S. boydii, respectively.
The CHL
r
, AMP
r
,
TMP-SXT
r
, TET
r
, NAL
r
, AMC
r
pattern in S.
flexneri strains and the CHL
r
, AMP
r
, TMP-SXT
r
,
TET
r
, NAL
r
, CRO
r
pattern
in S. dysenteriae strains
were the second most prevalent multi-antibiotic
resistance
patterns with a prevalence of 18.4 and
16.2% in each category,
respectively. Three S.
dysenteriae strains were resistant to all tested
antibiotics, however, 2 S. boydii strains were
susceptible to all tested antibiotics.
Table 3. Distribution frequencies of the antibiotic
resistance of 166 isolated Shigella species
Antibiotics
S.
flexneri
S.
dysenteria
S.
boydii
S.
sonnei
Total
Chloramphenicol(30)
61(91.1)
52(92.8) 21(84.0)
17(94.4) 151(90.9)
Ampicillin (10)
*
63(94.0)
54(96.4) 17(68.0)
15(83.3) 149(89.7)
Co-trimoxazole (25)
59(88.1)
52(92.8) 15(60.0)
14(77.7) 140(84.3)
Tetracycline (30)
61(91.1)
50(89.2) 13(52.0)
15(83.3) 139(83.7)
Nalidixic acid (30)
3(44.7) 48(85.7) 0 7(38.8) 85(51.2)
Co-amoxiclav (20)
20(29.8)
21(37.5) 10(40.0)
7(38.8) 85(51.2)
Ceftriaxone (30)
10(14.9)
23(41.1) 3(12.0) 0 36(21.6)
Amikacin (30)
5(7.4) 4(7.1) 0 2(11.1)
11(6.6)
Nitrofurantion (300)
2(2.9) 4(7.1) 0 0 6(3.6)
Ciprofloxacin (5)
0 3(5.3) 0 0
3(1.8)
*
µg/disk
DISCUSSION
In present study, S. flexneri was the
predominant isolated shigella species, followed by
S.
dysenteriae, S. boydii and S. sonnei. This is
consistent with other reports from other part of Iran
(3). However, temporal and spatial variations in the
isolation of Shigella species have been reported in
various parts of world from time to time. Before
1984, S. flexneri was the predominant species
isolated sporadically from 3% of diarrhea cases in
Calcutta, India (19). During 1990-1992 S.
dysenteriae type 1 was isolated more from this area
(20), again during 2001 to 2004 S. flexneri was the
most prevalent serogroup (8). In an
epidemiological study of acute bacterial diarrhea in
children during 2002-2003 in Bahia, Brazil, S.
sonnei was the most frequent pathogen (5). From
1999 to 2000 S. flexneri and S. dysenteriae were
the most common shigella isolates in Lagos,
Nigeria (21). From 1987 to 2002 S. sonnei was
predominant species in central Turkey (22). In our
study, S. sonnei was the least frequent isolates
among other Shigella species that was in agreement
with findings of Lee et al from Malaysia (23).

Yousefi MR. et al 153
Iranian Journal of Clinical Infectious Disease 2006;1(3):149-155
In our study, S. flexneri types 1b, 2a and 2b
were the most common serotypes isolated from
children with bacillary dysentery, respectively
(Table 1). These findings are differed from other
reports. In China (14) the most common serotypes
of S. flexneri were 1a, X, and 2a and in Thialand
(24)
the three most frequently encountered
serotypes were 2a, 1b and 3b, respectively. Among
S. dysenteriae isolates that were serotyped in
current study, types 1 and 2 were more prevalent.
This finding was supported with some other studies
(2,25,26). In the present study, S. flexneri and S.
sonnei were mostly found in children aged 7-10
years, while S. boydii was found in children <2
years old, this was not supported with other reports
(2,5). However, S.
dysenteriae was mostly isolated
in children aged 11-14 years old.
Our study also documents the trend of multi-
resistant Shigella species associated
with bacillary
dysentery in Hamadan over a four-year period.
Multiple antibiotic resistances were observed
among the strains of Shigella isolates and more
than four commonly used antibiotics were
ineffective against Shigellae isolates in this study.
S. flexneri showed
a high degree of resistance to
most of the commonly used antibiotics,
such as
chloramphenicol, ampicillin, co-trimoxazole, and
tetracycline (table 3). This finding is in agreement
with other reports from
developing countries such
as India (8,9), Bangladesh (10),Brazil (5),
Chile
(13), China (14), Nigeria (21) and Thailand (24).
However, in our experience S. flexneri also showed
resistance to nalidixic acid (44.7%) and co-
amoxiclav (29.8%). These results are slightly
differed from other reports (3,13,27). In developing
countries and low socio-economic conditions
including Iran, S. flexneri is still the predominant
serotype (3,10,21,25).
Evaluating the trends in the resistance patterns
of Shigella species demonstrated that S.
dysenteriae
is currently significantly more resistant than the
other Shigella species in Hamadan, especially to
the commonly used antimicrobial agents. This
finding is of utmost importance since S.
dysenteriae
is, at present, the second predominant species in
this region. In our survey, S.
dysenteriae showed
the highest rate of resistance to most of the tested
antibiotics including ampicillin, co-trimoxazole,
chloramphenicol, tetracycline, nalidixic acid, co-
amoxiclav and ceftriaxone (table 3). Resistance
was emerged even to more potent antimicrobial
agents such as ciprofloxacin, nalidixic acid, co-
amoxiclav and nitrofurantoin.
Resistance to nalidixic acid (85.7%),
ceftriaxone (41.1%) and co-amoxiclav (37.5%) was
not compatible with studies of some other countries
such as Ethiopia (27), Israel (28),
Thailand (24),
Turkey (22), and Chile (13).
S. boydii and S. sonnei also showed
a high level
of resistance to chloramphenicol, ampicillin, co-
trimoxazole, and tetracycline, but most of them
were susceptible to co-amoxiclav and ceftriaxone.
In children with severe shigellosis, especially in
those who are hospitalized, parenteral ceftriaxone
is effective and usually recommended. In our
study, all shigella isolates, except S.
dysenteriae,
were sensitive to ceftriaxone. All isolates of S.
boydii were susceptible to amikacin, ciprofloxacin,
nitrofurantoin and nalidixic acid. Increasing
resistance of Shigella strains to nalidixic acid has
been emerged over the past few decades in some
part of the worlds, especially in developing country
(14,21,25,26). This may be
due to inappropriate use
of this drug.
In our study, all shigella isolates, except S.
boydii, were resistant to nalidixic acid. In spite of
the worldwide spread of resistant strains, the use of
nalidixic acid is still recommended by the World
Health Organization guidelines for the
management of acute bloody diarrhea in children
(2).
Although resistance to ciprofloxacin has been
rarely reported, nearly all Shigella isolates (except
a few strains of S.
dysenteriae) remained
susceptible to this agent. Ciprofloxacin is often
recommended as empirical therapy in areas with
154 Epidemiology of Shigella in Hamadan
Iranian Journal of Clinical Infectious Disease 2006;1(3):149-155
high resistance to Shigella. It is, however, not
approved for children because of the potential risk
of damage to growing cartilage (29).
In conclusion, our results revealed that multi-
resistant strains of Shigella (in particular S.
dysenteriae and S.
flexneri) are present in Hamadan
and emphasize the importance of maintaining
surveillance of these strains in order to assess local
susceptibility patterns and empiric therapy. Most
strains of Shigella species in this study were found
to be resistant to chloramphenicol, ampicillin, co-
trimoxazole, nalidixic acid and tetracycline, and
sensitive to ciprofloxacin, amikacin and
nitrofurantoin.
REFERENCES
1. Cleary TG. Shigella: In: Feigin RD, Chery JD,
Demmier GJ, Kapian SL, editors, Textbook of pediatric
infectious diseases. 5
th
edition. Philadelphia: Saunders,
2004; p:541-53.
2. Clemens J, Kotloff KL, Kay B. Generic protocol to
estimate the burden of Shigella diarrhea and dysenteric
mortality. Geneva: World Health Organization; 1999.
WHO document WHO/V&B/99.26:1-11.
3. MoezArdalan K, Zali MR, Dallal MM, et al.
Prevalence and pattern of antimicrobial resistance of
Shigella species among patients with acute diarrhoea in
Karaj, Tehran, Iran. J Health Popul Nutr 2003;21(2):96-
102.
4. World Health Organization. Diarrheal disease due
to Shigella disease. In: Vaccines, immunization and
biologicals. Geneva: World Health Organization,
1998:1-5.
5. Diniz-Santos DR, Santana JS, Barretto JR, et al.
Epidemiological and microbiological aspects of acute
bacterial diarrhea in children from Salvador, Bahia,
Brazil. Braz J Infect Dis 2005;9(1):77-83.
6. Oyofo BA, Subekti D, Tjaniadi P, et al.
Enteropathogens associated with acute diarrhea in
community and hospital patients in Jakarta, Indonesia.
FEMS Immunol Med Microbiol 2002;34:139-46.
7. Zafar A, Sabir N, Bhutta ZA. Frequency of
isolation of shigella serogroups/serotypes and their
antimicrobial susceptibility pattern in children from
slum areas in Karachi. J Pak Med Assoc
2005;55(5):184-8.
8. Niyogi SK, Mitra U, Dutta P. Changing patterns of
serotypes and antimicrobial susceptibilities of Shigella
species isolated from children in Calcutta, India. Jpn J
Infect Dis 2001;54:121-22.
9. Niyogi SK, Pazhani GP. Multiresistant Shigella
species isolated from childhood diarrhea cases in
Kolkata, India. Jpn J Infect Dis 2003;56:33-34.
10. Khan AI, Huq S, Malek MA, et al. Shigella
serotypes among hospitalized patients in urban
Bangladesh and their antimicrobial resistance.
Epidemiol Infect 2004;132(4):773-7.
11. Battacharya SK, Sarkar K, Nair GB, et al. Multi-
drug resistant Shigella dysenteriae type 1 in South Asia.
Lancet Infect Dis 2003;3(12):755.
12. Tjaniadi P, Lesmana M, Subekti D, et al.
Antimicrobial resistance of bacterial pathogens
associated with diarrheal patients in Indonesia. Am J
Trop Med Hyg 2003;68:666-70
13. Fulla N, Prado V, Duran C, et al. Surveillance for
antimicrobial resistance profiles among Shigella species
isolated from a semirural community in the northern
administrative area of Santiago, Chile. Am J Trop Med
Hyg 2005;72(6):851-4.
14. Wang XY, Du L, Von Seidlein L, et al. Occurrence
of shigellosis in the young and elderly in rural China:
results of a 12-month population-based surveillance
study. 1: Am J Trop Med Hyg 2005;73(2):416-22.
15. Novokshonova IV, Zelenskaia OI, Gol'dberg IE, et
al. Significance of determination of Shigella antibiotic
resistance in bacteriological diagnosis of dysentery.
Antibiot Khimioter 2005;50(2-3):30-2.
16. Chompook P, Samosornsuk S, von Seidlein L, et al.
Estimating the burden of shigellosis in Thailand: 36-
month population-based surveillance study. Bull World
Health Organ 2005;83(10):739-46.
17. Forbes BA, Sahm DF, Weissfeld AS, editors.
Bailey & Scott’s diagnostic microbiology. 11
th
edition.
Philadelphia: Mosby Co, 2002;p:368-75 and 204-13.
18. National Committee for Clinical Laboratory
Standards (2000): Performance standard for
antimicrobial disk susceptibility tests: approved
standards. M2-A7. NCCL, Villanova, PA, USA.
19. Sen D, Saha MR, Nair GB, et al. Etiological
spectrum of acute diarrhea in hospitalized patients.
Indian J Med Res 1985;82:286-91.
20. Bhattachrya MK, Bhattacharya SK, Paul M, et al.
Shigellosis in Calcutta during 1990-92 antibiotic
susceptibility pattern and clinical features. J Diarr Dis
Res 1994;12:121-24.

Yousefi MR. et al 155
Iranian Journal of Clinical Infectious Disease 2006;1(3):149-155
21. Iwalokun BA, Gbenle GO, Smith SI, et al.
Epidemiology of shigellosis in Lagos, Nigeria: trends in
antimicrobial resistance. J Health Popul Nutr
2001;19(3):183-90.
22. Ozmert EN, Gokturk B, Yurdakok K, et al. Shigella
antibiotic resistance in central Turkey: comparison of
the years 1987-1994 and 1995-2002. J Pediatr
Gastroenterol Nutr 2005;40(3):359-62.
23. Lee WS, Puthucheary SD. Species distribution and
antibiotic resistance of shigella isolates in an urban
community in Malaysia. Med J Malaysia
2003;58(2):262-7.
24. Chompook P, Samosornsuk S, von Seidlein L, et al.
Estimating the burden of shigellosis in Thailand: 36-
month population-based surveillance study. Bull World
Health Organ 2005;83(10):739-46.
25. Pazhani GP, Ramamurthy T, Mitra U, et al. Species
diversity and antimicrobial resistance of Shigella spp.
isolated between 2001 and 2004 from hospitalized
children with diarrhea in Kolkata (Calcutta), India.
Epidemiol Infect 2005;133(6):1089-95.
26. Ahmed K, Shakoori FR, Shakoori AR. Etiology of
shigellosis in northern Pakistan. J Health Popul Nutr
2003;21(1):32-9.
27. Mache A. Antibiotic resistance and sero-groups of
shigella among pediatric out-patients in southwest
Ethiopia. East Afr Med J 2001;78(6):296-9.
28. Ashkenazi1 S, Levy I, Kazaronovski V, Samra Z.
Growing antimicrobial resistance of Shigella isolates. J
Antimicrobial Chemother 2003;51:427–29.
29. Bennish ML, Salam MA. Rethinking options for
the treatment of shigellosis. J Antimicrobial Chemother
1992;30:243–7.
Wyszukiwarka
Podobne podstrony:
Shigellosis disease, burden, epidemiology and case management
04 22 PAROTITE EPIDEMICA
006 Epidemiologia AIDS wykład UNOFFICIAL
epidemiologia metody,A Kusińska,K Mitręga,M Pałka,K Orszulik 3B
epidemiologia, czynniki ryzyka rola pielegniarki rak piersi szkola, nauczyciel
Epidemiologia jako nauka podstawowe założenia
SWW epidemiologia 6
SWW epidem AIDS 2005
Epidemiologia prezentacja 13
Miejsce i rola epidemiologii w medycynie
Epidemiologia prezentacja 7
Epidemiologia
1 Epidemiologia i podstawowe informacje o NSid 8500 ppt
1 Epidemiologiade
więcej podobnych podstron