C
ha
pt
er
12
77
Milan Sheth, MD, and
Harold I. Litt, MD, PhD
CT AngiogrAphy of The pulmonAry
VAsCulATure
1. What are the primary methods for imaging for pulmonary embolus (PE)?
There are three main methods of pulmonary arterial imaging. One is pulmonary arteriography, which is accomplished by
inserting a catheter under fluoroscopic guidance into the pulmonary artery and injecting contrast agent to visualize the
pulmonary arteries directly. Nuclear ventilation/perfusion (
.
V/
.
Q) examinations compare the location of radiolabeled
ventilated particles with radiolabeled injected particles to help infer the presence of PE. The third method is computed
tomography (CT) pulmonary angiography, which involves injecting contrast agent into a vein and using CT to evaluate
the pulmonary arteries.
2. What plain film findings may suggest PE?
A chest radiograph is usually the first imaging modality used for a patient with suspected PE. The results of the chest
film may be negative or have nonspecific findings, such as pleural effusions and atelectasis, but occasionally the
film can have a wedge-shaped peripheral opacity, referred to as a Hampton hump. An area of lucency resulting from
decreased perfusion that is termed Westermark sign also may be seen.
3. What are the advantages of CT angiography over other methods in the evaluation
of PE?
One important advantage over catheter pulmonary arteriography and
.
V/
.
Q nuclear medicine scans is that CT
angiography may be used to diagnose other causes of the patient’s symptoms, such as a pleural effusion or atelectasis.
In contrast to arteriography, CT angiography is noninvasive and safer. CT angiography also takes less time to perform.
CT angiography has several advantages over nuclear
.
V/
.
Q imaging. It is less dependent on patient cooperation. In
addition, nuclear
.
V/
.
Q examinations may have a 60% to 70% indeterminate rate, especially in patients with underlying
lung disease or other comorbidities, which limit specificity.
4. How do you perform a CT angiography examination for PE?
The technique for performing CT angiography optimally involves the use of a multidetector row CT scanner. Contrast
agent is injected at a high rate into a peripheral vein. Scanning is timed to obtain optimal contrast opacification of the
pulmonary arteries. Thin-section axial CT images of 1- to 2-mm thickness are obtained throughout the chest. With CT
scanners containing 16, 64, or more slices, a CT scan for PE requires only a 5- to 10-second acquisition, and provides
high-quality images, even in very dyspneic patients.
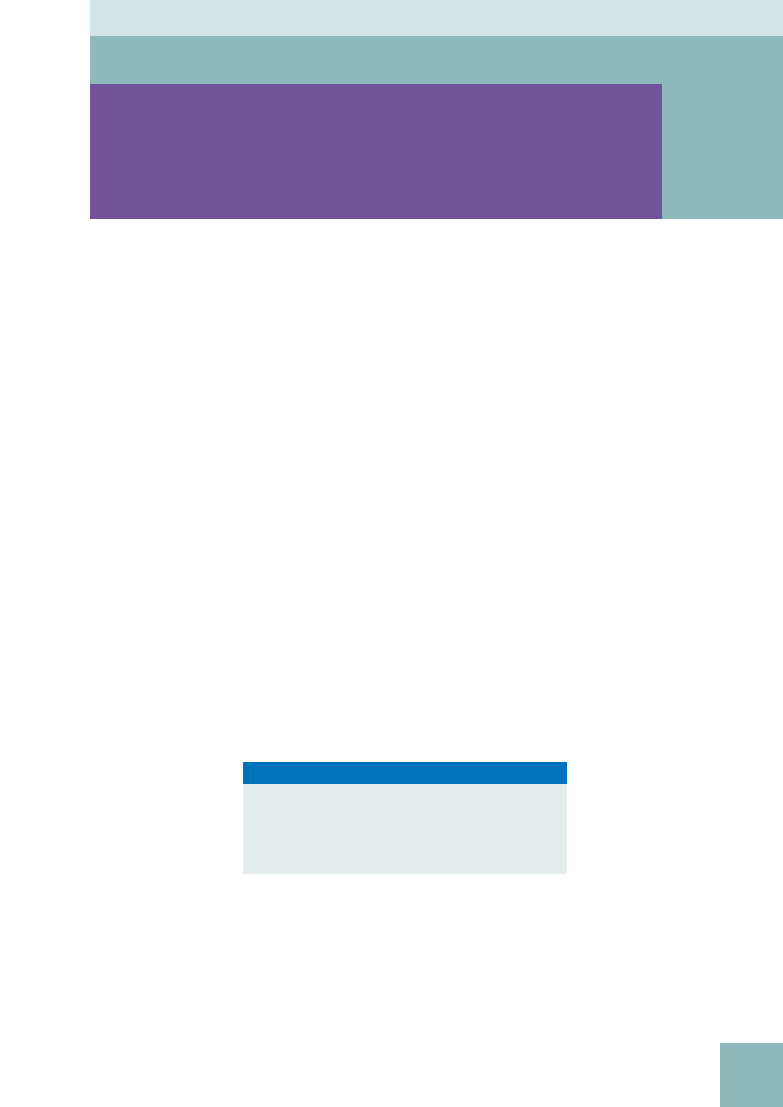
5. What are the direct CT angiography findings of PE?
The most specific finding of a PE is a partial or complete intraluminal filling defect in a pulmonary artery (
).
It should be present on at least two contiguous sections. Abrupt cutoff of the artery also indicates a PE.
6. What are the indirect findings of PE?
A pulmonary artery with an embolus may be slightly enlarged. Parenchymal findings, such as wedge-shaped opacities
denoting areas of infarction and atelectasis, sometimes can be seen as well. Areas of decreased perfusion can manifest
as wedge-shaped hyperlucency.
Key Points: CT Angiography
1. Multidetector row CT angiography has become the first-
line imaging examination for evaluation of suspected PE.
2. CT angiography has greater specificity than a
.
V/
.
Q scan.
3. CT angiography has greater availability and safety than
pulmonary angiography.
78
CT AngiogrAphy of The pulmonAry VAsCulATure
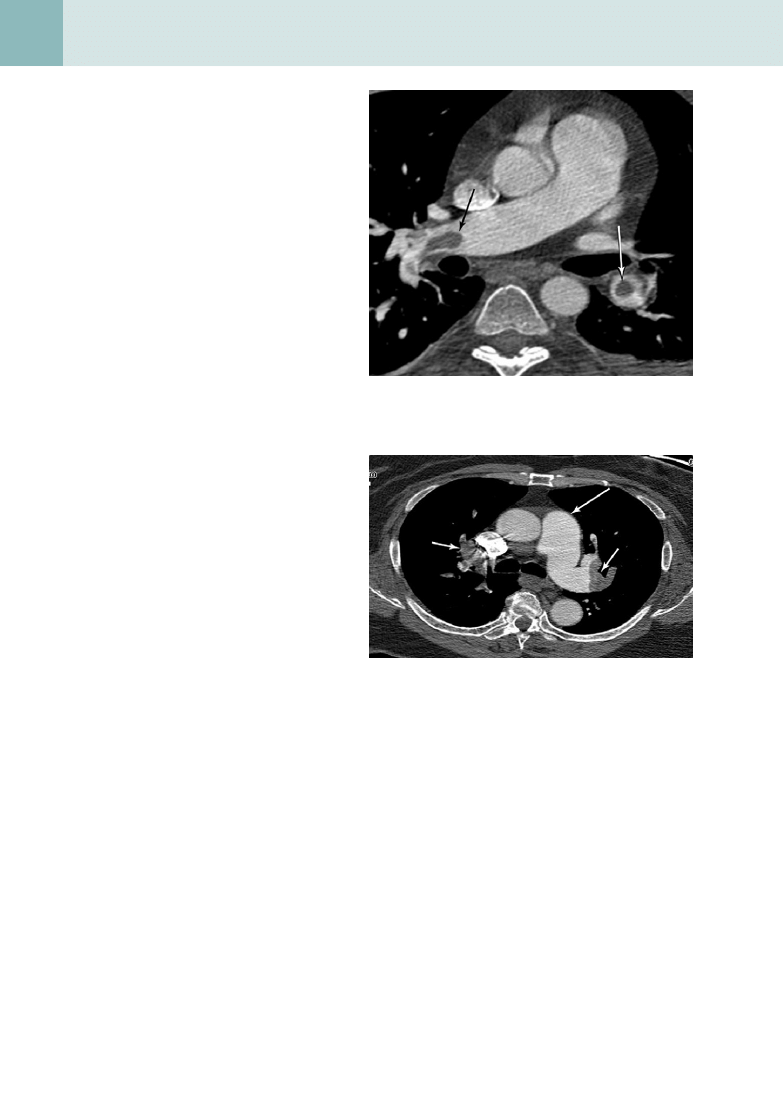
7. How can acute PE be distinguished
from chronic PE on CT
angiography?
It may be difficult to differentiate acute from
chronic PE. Chronic PE may be complicated
by superimposed acute PE. Acute PE are often
seen as central filling defects, in contrast to
chronic emboli, which are more peripheral. This
is easy to remember because the peripheral
appearance of chronic PE is due to an acute
clot in a vessel that recanalizes over time.
Chronic emboli can also calcify, whereas acute
emboli do not. Long-standing PE are more
likely than acute emboli to cause pulmonary
hypertension, leading to right heart enlargement
and enlargement of the main and central
pulmonary arteries (
). Lastly, increased
mediastinal collateral vessels can be seen in
some cases of chronic PE.
8. What are other uses for CT in PE?
CT also can be used to evaluate the lower
extremity venous system for thrombosis, using
the same contrast bolus, by imaging several
minutes after the PE study. Lower extremity
ultrasound (US) is generally used to evaluate
lower extremity veins, but CT has several
advantages. One is that it is not operator
dependent, in contrast to US. CT can be used to
evaluate for clot in areas that are inaccessible to
US or difficult to evaluate. This includes the deep
pelvic veins (a common source of thrombus
that may embolize to the lungs) and the region
around the adductor canal. US can be of limited
value in patients who are obese or have had
recent surgery. Within certain limitations,
CT may be a better choice than US in these
situations.
9. What is a pulmonary arteriovenous
malformation (AVM), and what
symptoms can it cause?
A pulmonary AVM is an abnormal communication
between the pulmonary artery and a draining vein, causing blood to bypass the pulmonary capillary bed before
returning to the left heart. AVMs may be asymptomatic, but they can manifest with a wide range of clinical symptoms.
Symptoms result from the loss of two essential physiologic functions of the lungs. Hypoxia may occur because of
shunting, and paradoxic emboli, stroke, or brain abscess may occur because of the loss of the “filter” effect of the
lung. Pulmonary AVMs may cause vague symptoms, such as chest pain and dyspnea on exertion, because of shunting
of deoxygenated blood. With severe shunting, high-output cardiac failure can result from right-to-left shunting.
10. What is orthodeoxia?
The term orthodeoxia is used to describe position-dependent oxygen desaturation. Most pulmonary AVMs occur in
the lower lobes. Shunting of blood and desaturation are maximum when blood flow to the lung bases is greatest.
Patients with large pulmonary AVMs in the lower lobes have larger shunts and lower oxygen saturation when
standing. When lying down, blood is redirected toward the lung apices, and the shunt fraction and desaturation may
decrease.
Figure 12-1.
Axial image from pulmonary CT angiography
examination shows bilateral PE, which are visualized as intraluminal
filling defects in the pulmonary arterial system (arrows).
Figure 12-2.
Axial CT angiography image shows bilateral chronic
PE (short arrows). Although these emboli have not calcified, the main
pulmonary artery (long arrow) is enlarged, indicating pulmonary
hypertension.
CT AngiogrAphy of The pulmonAry VAsCulATure
79
CArDiAC AnD noninVAsiVe VAsCulAr imAging
11. What pulmonary AVMs are associated with what hereditary disorder?
Although pulmonary AVMs are often isolated, they can be associated with hereditary hemorrhagic telangiectasia, also
known as Osler-Weber-Rendu disease. Hereditary hemorrhagic telangiectasia is a genetic disorder that causes vascular
malformations that can lead to multiple pulmonary AVMs. It is characterized by telangiectasias of the skin and mucosal
linings, epistaxis, and AVMs in various internal organs such as the brain and liver. It is wise to screen family members of
patients who present with pulmonary AVMs so that they can receive treatment.
12. You are asked to start a peripheral intravenous line in a patient with a known
pulmonary AVM. What special precautions should you take?
Patients with pulmonary AVMs lack the “filter” function performed by the pulmonary capillary bed. This situation
predisposes patients to paradoxic emboli from endogenous and exogenous sources. Air or other material accidentally
introduced into the venous system could pass through the shunt and cause a stroke. Care must be taken that all venous
lines are free of air, and that filters are used to prevent paradoxic emboli.
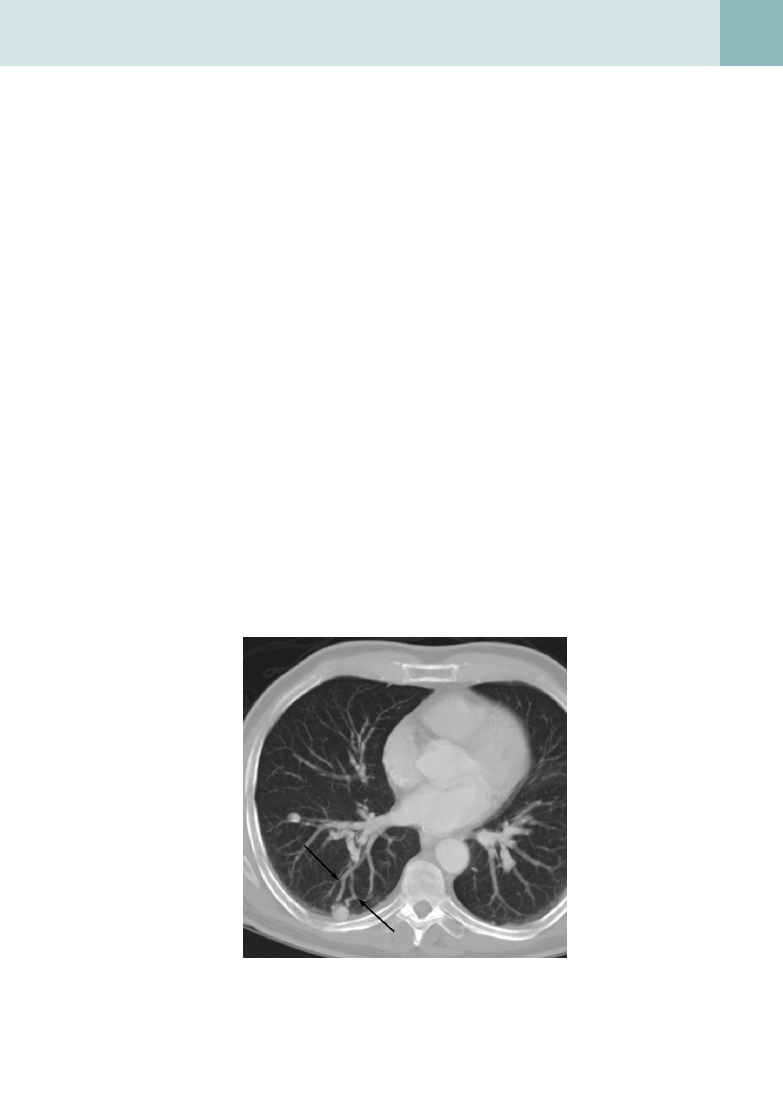
13. What are the imaging characteristics of a pulmonary AVM on plain film and CT?
On plain film, pulmonary AVMs appear as serpiginous or nodular densities that can connect to the hilum. On CT, they
appear as a homogeneous noncalcified nodule that has a vascular connection with an enlarged feeding artery and
draining vein (
). On dynamic images, the malformation enhances in a sequential manner from the feeding
artery to the malformation to the vein.
14. What is partial anomalous pulmonary venous return (PAPVR)?
PAPVR occurs when part of the pulmonary venous system drains directly into the systemic circulation. It can occur in
isolation or be associated with either atrial septal defect or a hypogenetic lung. When PAPVR is associated with atrial
septal defect (usually a sinus venosus defect), the right upper lobe drains into the superior vena cava. When PAPVR
occurs with a hypogenetic lung, it is a component of congenital pulmonary venolobar syndrome, also known as scimitar
syndrome.
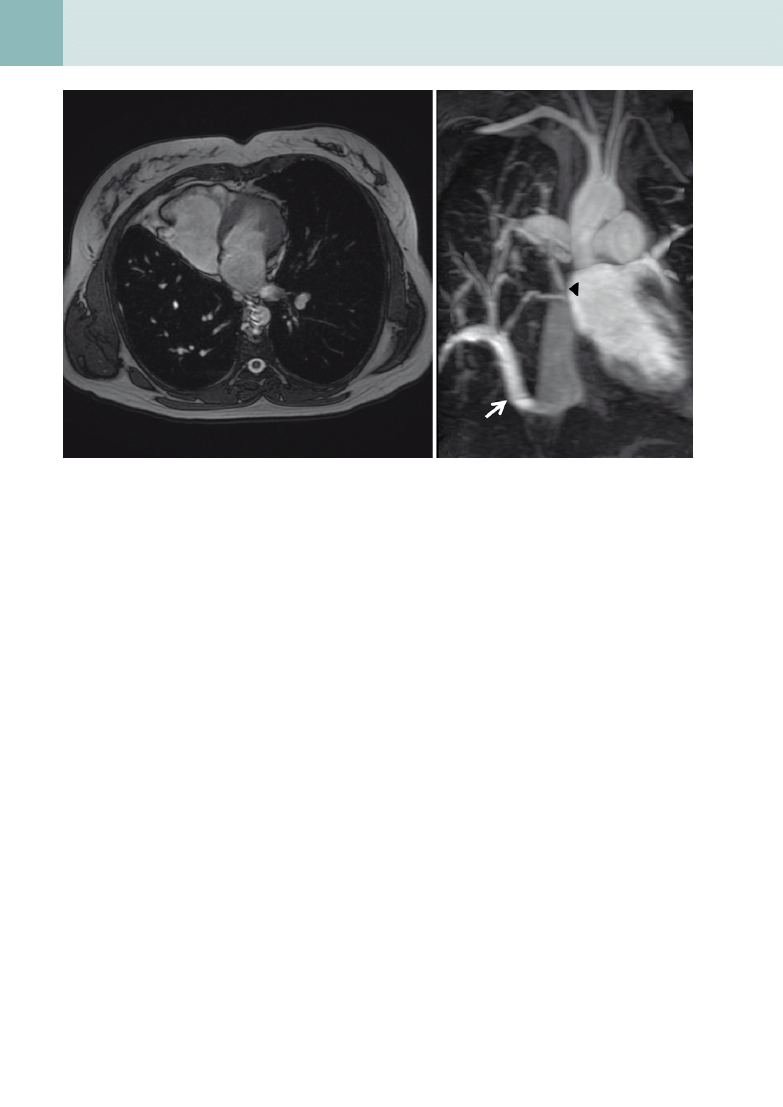
15. What is scimitar syndrome, and what are its associated imaging findings?
Scimitar syndrome is a hypogenetic lung (almost exclusively on the right) that is drained by an anomalous vein.
This anomalous vein can drain into many structures, including the infradiaphragmatic inferior vena cava (IVC),
suprahepatic IVC, portal vein, or right atrium. The chest x-ray shows a small right lung with a tubular opacity paralleling
the right heart border (called the scimitar). Magnetic resonance imaging (MRI) and CT show the course and nature of the
abnormal vascular anatomy better (
).
Figure 12-3.
Axial CT angiography image shows a pulmonary AVM,
with feeding artery and draining vein (arrows) associated with the lesion.
80
CT AngiogrAphy of The pulmonAry VAsCulATure
A
B
Figure 12-4.
Findings of scimitar syndrome.
A, Axial MR image shows small right lung and shift of the mediastinum to the right. B, Oblique
maximum intensity projection of magnetic resonance angiography (MRA) of the chest showing anomalous pulmonary venous drainage of the
right lower lobe to the IVC (arrow), the so-called scimitar vein. The upper lobe drains into the left atrium (arrowhead ).
16. What is the most common primary tumor of the pulmonary artery?
Tumors associated with the pulmonary vascular system are exceedingly rare. Angiosarcomas are most common.
These are rare tumors and sometimes can be difficult to distinguish from occlusive PE because both fill the lumen of the
pulmonary artery.
Document Outline
- CT Angiography of the Pulmonary Vasculature
- What are the primary methods for imaging for pulmonary embolus (PE)?
- What plain film findings may suggest PE?
- What are the advantages of CT angiography over other methods in the evaluation of PE?
- How do you perform a CT angiography examination for PE?
- What are the direct CT angiography findings of PE?
- What are the indirect findings of PE?
- How can acute PE be distinguished from chronic PE on CT angiography?
- What are other uses for CT in PE?
- What is a pulmonary arteriovenous malformation (AVM), and what symptoms can it cause?
- What is orthodeoxia?
- What pulmonary AVMs are associated with what hereditary disorder?
- You are asked to start a peripheral intravenous line in a patient with a known pulmonary AVM. What special precautions should you take?
- What are the imaging characteristics of a pulmonary AVM on plain film and CT?
- What is partial anomalous pulmonary venous return (PAPVR)?
- What is scimitar syndrome, and what are its associated imaging findings?
- What is the most common primary tumor of the pulmonary artery?
Wyszukiwarka
Podobne podstrony:
C20090551288 B9780323067942000420 main
C20090551288 B9780323067942000055 main
C20090551288 B9780323067942000407 main
C20090551288 B9780323067942000225 main
C20090551288 B9780323067942000432 main
C20090551288 B9780323067942000547 main
C20090551288 B9780323067942000298 main
C20090551288 B9780323067942000602 main
C20090551288 B978032306794200047X main
C20090551288 B9780323067942000250 main
C20090551288 B9780323067942000638 main
C20090551288 B9780323067942000316 main
C20090551288 B9780323067942000286 main
C20090551288 B9780323067942000560 main
C20090551288 B9780323067942000341 main
C20090551288 B9780323067942000390 main
C20090551288 B9780323067942000766 main
C20090551288 B9780323067942000754 main
C20090551288 B9780323067942000626 main
więcej podobnych podstron