
C
ha
pt
er
279
40
Joseph R. Perno, MD, PhD, and
Neil Roach, MD
OsteOarthritis and inflammatOry
arthritis
1. What imaging modality is best for diagnosis and follow-up of arthritic diseases?
Plain films are the mainstay for arthritis imaging. They are easy to obtain and give high-resolution information
about cortical bone changes such as erosions, joint space narrowing, and osteophytes. The sensitivity of plain
radiographs to detect early changes of rheumatoid arthritis (RA) is limited, however. Magnetic resonance
imaging (MRI) has been shown to be sensitive to early changes, such as marrow edema, erosions, and synovial
inflammation.
2. What is the difference between an inflammatory arthritis and a degenerative
arthritis?
Inflammatory arthritides are diseases of the synovium, which subsequently produce erosive changes of the adjacent
bones. Examples of inflammatory arthritis include RA and psoriatic arthritis. Degenerative arthritis/osteoarthritis is
secondary to articular cartilage damage from repetitive microtrauma that occurs throughout life, although multiple other
factors, such as heredity, nutrition, metabolic factors, preexisting articular disease, and body habitus, may contribute to
development of the radiographic features of osteoarthritis, which include osseous proliferation, joint space narrowing,
and subchondral sclerosis.
3. Which joints are most often affected
in RA?
RA has a predilection for the carpal/
tarsal, carpometacarpal/tarsometatarsal,
metacarpophalangeal/metatarsophalangeal,
and proximal interphalangeal joints (
In adults, the distal interphalangeal joints rarely
are affected. Joint involvement tends to be
bilateral, but not always symmetric. Generally, the
metacarpophalangeal and the metatarsophalangeal
joints are affected first.
4. What portion of the spine does RA
most commonly affect?
In the cervical spine, RA commonly causes
atlantoaxial (C1 to C2) subluxation because of
laxity of the transverse ligament and pannus
formation. Other disease entities may affect this
region of the cervical spine, including gout, calcium
pyrophosphate dihydrate (CPPD) crystal deposition
disease, and hydroxyapatite deposition disease.
Some of these other disease processes may cause
erosions of the dens, atlantoaxial subluxation, and
radiopaque calcifications.
5. Can RA affect nonarticular structures?
Yes. Retrocalcaneal bursitis is common and is detected when the retrocalcaneal fat at the posterior-superior aspect of
the calcaneus is obscured by edema. It is often accompanied by bone erosion.
6. How do inflammatory arthritides affect cartilage?
Inflammatory arthritides are a chronic synovitis, eroding bone that is “unprotected” by cartilage. These changes are
noted first at the margins of joints, where cartilage is thinnest. Cartilage is also eroded by the joint inflammation, but
tends to erode in an even and uniform manner.
Figure 40-1.
Ulnar deviation of the metacarpals is noted in this patient
with RA. There is a typical marginal erosion of the metacarpal head
(arrow).

280
OsteOarthritis and inflammatOry arthritis
7. What finding, which is common in osteoarthritis, is virtually never seen
with RA?
The presence of significant osteophytes (productive bone changes) is not consistent with the diagnosis of RA. A joint that
has been destroyed by RA may then develop osteoarthritis, however, owing to cartilage loss.
8. What additional joint findings are seen with RA?
Subluxations and malalignments at the metacarpophalangeal and metatarsophalangeal joints are typical. The
subluxations tend to deviate the phalanges in the ulnar direction (see
9. Where are the swan neck and boutonnière deformities located?
The chronic inflammatory changes of RA in the joints of the fingers produce retraction of the tendons. The swan
neck deformity is caused by hyperextension of the proximal interphalangeal joint with simultaneous flexion of the
distal interphalangeal joint. If you try this manipulation on yourself, you will recognize the reason for the name. The
boutonnière (or buttonhole) deformity is caused by hyperextension of the distal interphalangeal joint with simultaneous
flexion of the proximal interphalangeal joint.
10. When can RA be confused with other arthritides?
Severe erosions of the subchondral bone may develop late in RA after the cartilage is destroyed and may give an
appearance similar to erosive osteoarthritis.
11. What joints are typically affected by osteoarthritis?
Osteoarthritis most often affects the proximal and distal interphalangeal joints of the hands and the major weight-
bearing joints—the hips and the knees. In addition, the carpal joints at the base of the thumb are commonly affected
(trapeziometacarpal and scaphotrapeziotrapezoidal joints). The most commonly affected joint in the foot is the first
metatarsophalangeal joint. Any joint damaged by trauma that results in an irregular articular surface can become
prematurely arthritic.
12. Where are Heberden and Bouchard nodes located?
•
Heberden nodes are osseous outcroppings involving the distal interphalangeal joints.
•
Bouchard nodes involve the proximal interphalangeal joints.
Bouchard and Heberden nodes are physical examination signs of hand osteoarthritis.
13. Which joints are rarely involved in
primary osteoarthritis?
Involvement of the radiocarpal, pan-carpal, and
metacarpophalangeal joints is rare in osteoarthritis,
but is common in RA and psoriatic arthritis.
14. What are the hallmarks of
osteoarthritic change in a joint?
Erosive arthritides have uniform cartilage loss,
whereas degenerative osteoarthritis results in
segmental cartilage loss. In small joints, such
as joints in the fingers, the loss may seem to
be uniform. The layer of bone just beneath the
cartilage is called the subchondral bone. When
exposed to increased stress, this layer becomes
sclerotic. As this process continues, the cartilage
and the underlying bone can become eroded,
producing cystlike pockets in the bone, called
geodes. At the edge of a joint where the cartilage
is thinnest, exposed bone becomes hypertrophic,
resulting in irregular or pointed outcroppings of
bone, called osteophytes.
15. What is erosive osteoarthritis?
Erosive osteoarthritis is a form of osteoarthritis that
is sometimes called inflammatory osteoarthritis
(
). Although the joint distribution is the
Figure 40-2.
Erosive osteoarthritis involving the distal interphalangeal
joints, with a combination of productive and erosive changes. Note the
classic “gull wing” deformity of the distal interphalangeal joint (arrow).
OsteOarthritis and inflammatOry arthritis
281
musculOskeletal radiOlOgy
same as in typical osteoarthritis, the erosive changes are more severe, and there is soft tissue swelling, which may give
a similar appearance to RA or psoriatic arthritis. These changes involve the subchondral cortex in the main portion of the
joint, however, rather than the peripheral “bare areas.” Ultimately, the phalangeal joints may become fused.
16. Name the seronegative spondyloarthropathies.
Seronegativity refers to the absence of rheumatoid factor in blood tests of patients who present with inflammatory
arthritis. This group of diseases includes psoriatic arthritis, reactive arthritis (Reiter syndrome), ankylosing spondylitis (AS),
and enteropathic arthritis (associated with inflammatory bowel diseases such as Crohn disease and ulcerative colitis).
17. What mnemonic can be used to remember the triad of symptoms seen with reactive
arthritis (also known as Reiter syndrome)?
“Can’t see (uveitis), can’t pee (urethritis), can’t bend your knee (arthritis).”
18. What are the different presentations of psoriatic arthritis?
Psoriatic arthritis tends to involve the terminal interphalangeal joints of both hands; this is in contrast to RA, which more
commonly involves more proximal joints in the hands and wrists. A second presentation pattern of psoriatic arthritis
may involve multiple joints of a single hand. The third pattern involves only the joints of a single ray. The appearance is a
combination of erosive and productive bony changes. The erosive changes occur at the peripheral bare areas, similar to RA.
Psoriatic arthritis also has productive bone formation adjacent to the joint, however, typically in an exuberant and irregular
manner. Although the clinical symptoms of psoriatic arthritis develop in 30% to 40% of patients with psoriasis, psoriatic arthritis
usually does not occur concomitantly with the dermatologic diagnosis and may take 10 years or longer to manifest. It has been
estimated, however, that 10% to 15% of patients have musculoskeletal complaints as the first manifestations of psoriasis.
19. What is the “pencil-in-cup” deformity?
The advanced erosive changes seen in psoriatic arthritis can produce a pointed appearance of the proximal phalanx that
then pushes into the base of the more distal phalanx and deforms it to look like a cup.
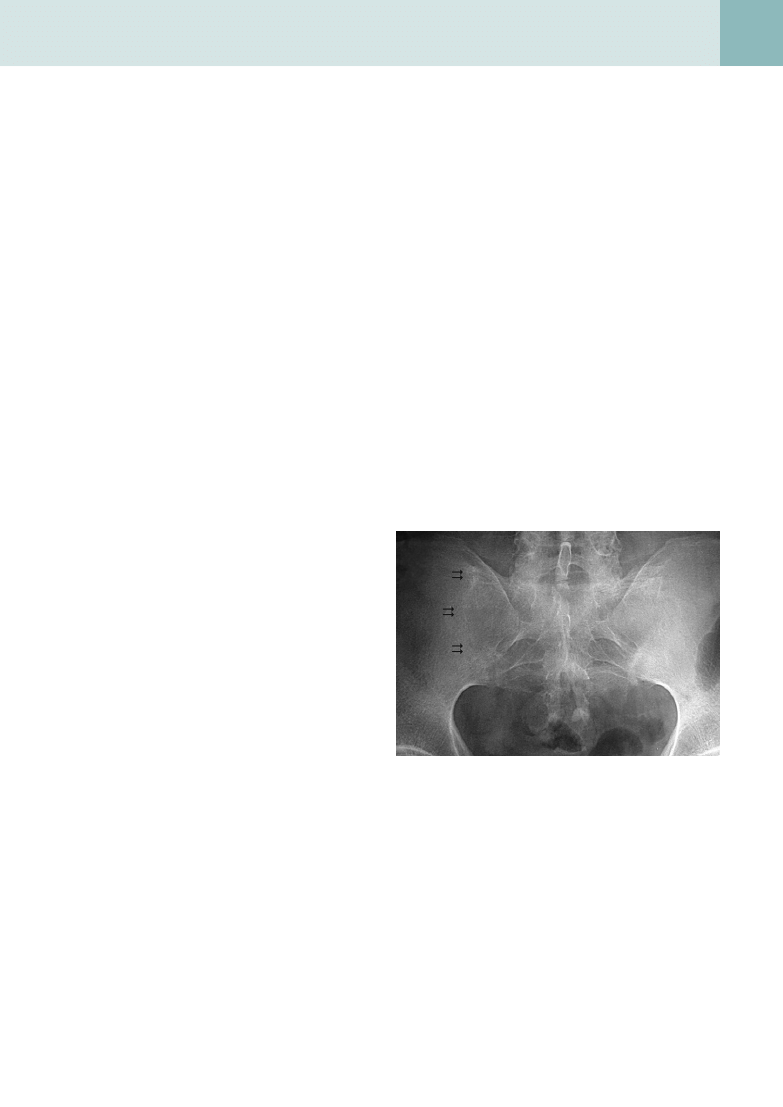
20. Does AS have a specific pattern of
joint involvement?
AS preferentially involves the sacroiliac joints and
lumbar spine, and then may advance craniad to
involve the thoracic and cervical spine. Ankylosis
refers to the bony fusion of the opposing surfaces,
which results in sclerosis and loss of the normal
sacroiliac joint cartilage space (
). Focal
cortical irregularities at the anterior margin of the
superior and inferior discovertebral junctions are
considered early and significant features of AS
seen on conventional radiographs and have been
termed Romanus lesion. The MRI correlate has
been described and is termed the “MRI corner”
sign. Healing of the Romanus lesion leads to
sclerosis at the end-plate corners and has been
termed the “shiny corner” sign.
21. What does the term bamboo spine
describe?
AS produces syndesmophytes, which are osseous bridges of the intervertebral disc spaces along Sharpey fibers in
the anulus fibrosus. Combined with fusion of the facet joints and ossification of the longitudinal spinal ligaments, the
appearance is similar to that of a stick of bamboo.
22. What is the radiologic appearance of gout?
Gout classically involves the first metatarsophalangeal joint. Other joints of the hand and foot can also be affected,
however. Although more than one joint may be involved, it does not tend to be symmetric as other inflammatory
arthritides can be. The classic appearance of a gout erosion is termed the overhanging margin, with a rim of eroded
cortex hanging over a soft tissue density called a tophus. Tophi are soft tissue deposits of monosodium urate crystals
that may occur anywhere, particularly in the dorsal aspect of the foot and the extensor aspect of the elbow.
23. What is pseudogout?
Pseudogout is not a radiographic diagnosis; it refers to a goutlike clinical syndrome with acute attacks of intermittent pain.
Figure 40-3.
AS causes fusion of the sacroiliac joint. When this joint
fuses, the normally dark-appearing cartilage becomes replaced by bone
matrix (double arrows).
282
OsteOarthritis and inflammatOry arthritis
24. What are the differences between
pyrophosphate arthropathy and
CPPD crystal deposition disease?
CPPD crystal deposition disease is a specific
term for a disorder characterized by the exclusive
presence of CPPD crystals in and around joints.
Pyrophosphate arthropathy describes a pattern
of joint damage that is secondary to CPPD crystal
deposition disease. Although the radiographic
changes of pyrophosphate arthropathy may
be similar to osteoarthritis (osteophytosis,
subchondral sclerosis, and joint space narrowing),
there is a tendency to develop prominent
subchondral cystic changes and decreased
osteophytosis (as seen in osteoarthritis), and
it tends to involve non–weight-bearing joint
spaces, such as the shoulder, patellofemoral, and
radiocarpal joints. It also tends to be symmetric.
In the hand, CPDD crystal deposition disease
tends to involve the metacarpophalangeal joints,
particularly the second and third, but spares
the interphalangeal joints. The subchondral
bone becomes involved by multiple cystlike
lucencies that can eventually lead to collapse
of the articular surface (scapholunate advanced
collapse wrist).
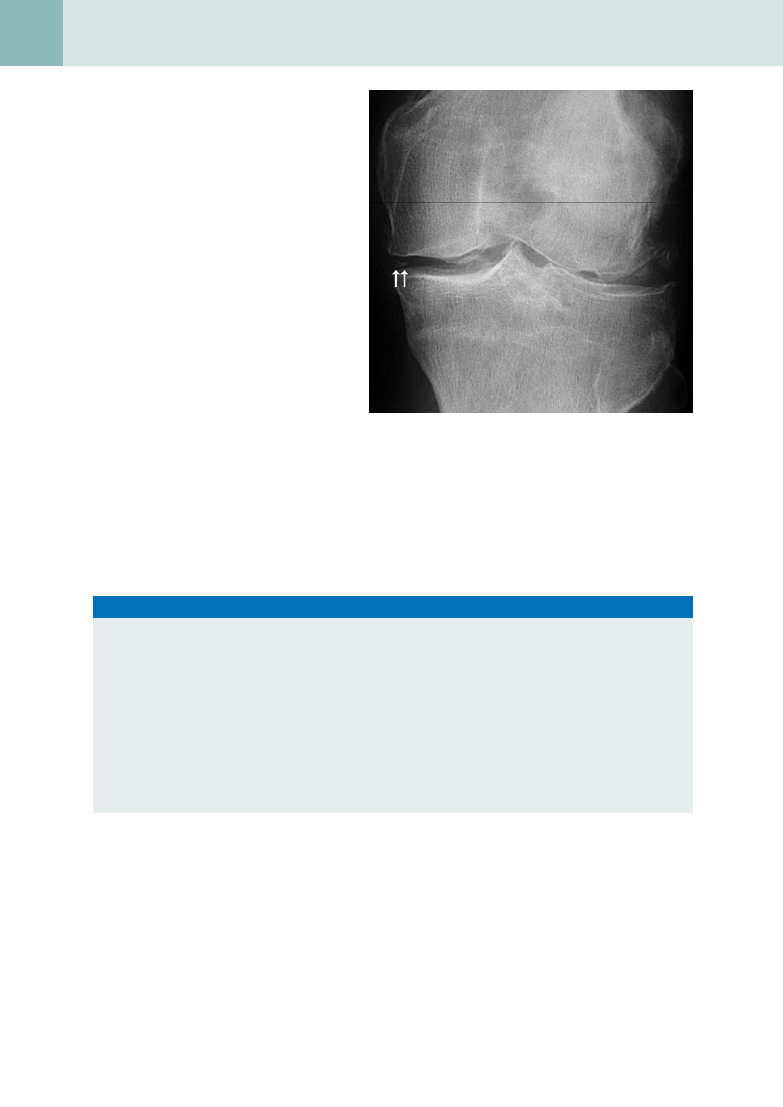
Calcium pyrophosphate crystals tend to deposit within fibrocartilage. The menisci of the knee, triangular fibrocartilage
of the wrist, labra of the acetabulum and glenoid, symphysis pubis, and anulus fibrosus of the intervertebral disc are
common sites. These cartilage calcifications are termed chondrocalcinosis (
). These deposits may also affect
the hyaline cartilage, which becomes a more specific radiologic marker for the disease. Soft tissue calcification is also
common in tendons, bursae, and synovium.
B
iBliography
[1] A. Brower, Arthritis in Black and White, Saunders, Philadelphia, 1988.
[2] J.M. Farrant, P.J. O’Connor, A.J. Grainger, Advanced imaging in rheumatoid arthritis, part 1: synovitis, Skeletal Radiol. 36 (2007) 269–279.
[3] A. Feydy, F. Lioté, R. Carlier, et al., Cervical spine and crystal-associated diseases: imaging findings, Eur. Radiol. 16 (2006) 459–468.
[4] C.A. Helms, Fundamentals of Skeletal Radiology, second ed., Saunders, Philadelphia, 1995.
[5] N.R. Kim, J.Y. Choi, S.H. Hong, et al., “MR corner sign”: value for predicting presence of ankylosing spondylitis, AJR Am. J. Roentgenol.
191 (2008) 124–128.
[6] J.A. Jacobson, G. Girish, Y. Jiang, B.J. Sabb, Radiographic evaluation of arthritis: degenerative joint disease and variations, Radiology 248
(2008) 737–747.
[7] C.C. Peterson, M.L. Silbiger, Reiter’s syndrome and psoriatic arthritis: their roentgen spectra and some interesting similarities, AJR Am. J.
Roentgenol. 100 (1967) 860–871.
[8] L.S. Steinbach, D. Resnick, Calcium pyrophosphate dihydrate crystal deposition disease revisited, Radiology 200 (1996) 1–9.
[9] J.M. Taveras, J.T. Ferrucci, Radiology: Diagnosis, Imaging, Intervention, 2002 ed. on CD-ROM, Lippincott Williams & Wilkins, Philadelphia,
2002.
Key Points: Differentiating Arthritis on Hand Radiograph
1. Symmetric erosive change of the metacarpophalangeal and proximal interphalangeal joints of both hands,
periarticular osteopenia, and symmetric joint space loss suggest RA.
2. Extensive productive osteophyte changes of the distal interphalangeal joints, with less severe changes of the
proximal interphalangeal and metacarpophalangeal joints, or a thickened “sausage-digit,” suggests psoriatic
arthritis.
3. Osteophyte production and joint space narrowing without marginal erosions of the distal interphalangeal and
proximal interphalangeal joints, with little or no involvement of the metacarpophalangeal joints, suggests
degenerative joint disease.
4. A soft tissue mass with an overhanging rim of bone, adjacent to a joint space, suggests gout. Gout also tends
to preserve the joint space and the mineralization of the bone.
5. Calcifications within the soft tissues of the fingertips, resorption of the cortex of the finger tufts, or both suggest
scleroderma or polymyositis.
Figure 40-4.
CPDD with calcium crystal deposition in the meniscus
(double arrows). This is called chondrocalcinosis.
Document Outline
- Osteoarthritis and Inflammatory Arthritis
- What imaging modality is best for diagnosis and follow-up of arthritic diseases?
- What is the difference between an inflammatory arthritis and a degenerative arthritis?
- Which joints are most often affected in RA?
- What portion of the spine does RA most commonly affect?
- Can RA affect nonarticular structures?
- How do inflammatory arthritides affect cartilage?
- What finding, which is common in osteoarthritis, is virtually never seen with RA?
- What additional joint findings are seen with RA?
- Where are the swan neck and boutonnière deformities located?
- When can RA be confused with other arthritides?
- What joints are typically affected by osteoarthritis?
- Where are Heberden and Bouchard nodes located?
- Which joints are rarely involved in primary osteoarthritis?
- What are the hallmarks of osteoarthritic change in a joint?
- What is erosive osteoarthritis?
- Name the seronegative spondyloarthropathies.
- What mnemonic can be used to remember the triad of symptoms seen with reactive arthritis (also known as Reiter syndro ...
- What are the different presentations of psoriatic arthritis?
- What is the “pencil-in-cup” deformity?
- Does AS have a specific pattern of joint involvement?
- What does the term bamboo spine describe?
- What is the radiologic appearance of gout?
- What is pseudogout?
- What are the differences between pyrophosphate arthropathy and CPPD crystal deposition disease?
- Bibliography
Wyszukiwarka
Podobne podstrony:
C20090551288 B9780323067942000420 main
C20090551288 B9780323067942000055 main
C20090551288 B9780323067942000225 main
C20090551288 B9780323067942000432 main
C20090551288 B9780323067942000547 main
C20090551288 B9780323067942000298 main
C20090551288 B9780323067942000602 main
C20090551288 B978032306794200047X main
C20090551288 B9780323067942000250 main
C20090551288 B9780323067942000638 main
C20090551288 B9780323067942000316 main
C20090551288 B9780323067942000286 main
C20090551288 B9780323067942000560 main
C20090551288 B9780323067942000341 main
C20090551288 B9780323067942000390 main
C20090551288 B9780323067942000766 main
C20090551288 B9780323067942000754 main
C20090551288 B9780323067942000122 main
C20090551288 B9780323067942000626 main
więcej podobnych podstron