Disturbed eating attitudes, coping styles, and subjective quality of life in
adolescents with Type 1 diabetes
B
Vasileia Grylli
a
, Gudrun Wagner
a
, Andrea Hafferl-Gattermayer
a
,
Edith Schober
b
, Andreas Karwautz
a
,
T
a
Eating Disorders Unit, University Clinic of Neuropsychiatry of Childhood and Adolescence, General Hospital of Vienna,
Medical University Vienna, A-1090 Vienna, Austria
b
Diabetes Care Unit, University Clinic of Pediatrics and Adolescent Medicine, General Hospital of Vienna, Medical University Vienna, A-1090 Vienna, Austria
Received 25 September 2004; received in revised form 2 February 2005; accepted 2 February 2005
Abstract
Objectives: To evaluate coping styles and quality of life in
youth with Type 1 diabetes with and without eating disorders
and to identify relationships between these variables in each
group. Methods: Adolescents were evaluated for eating disor-
ders with a two-stage diagnostic procedure. Adolescents with
and without eating disorders then provided data on coping styles
and on subjective well-being. Results: Adolescents with Type 1
diabetes and disordered eating behavior reported more often
blaming themselves and resorting to wishful thinking and poorer
physical and psychosocial quality of life than do adolescents
with Type 1 diabetes without disordered eating behavior.
Specific coping strategies were also positively linked with
quality of life and metabolic control. Conclusions: Eating
disorders and disordered eating behavior in adolescents with
Type 1 diabetes seem to be associated with certain negative and
avoidant coping strategies and with impeded physical and bio-
psychosocial well-being.
D 2005 Elsevier Inc. All rights reserved.
Keywords: Adolescence; Coping; Eating disorders; Quality of life; Type 1 diabetes
Introduction
Coping with the demands of self-management of Type 1
diabetes in adolescence can be a formidable task. This
includes both the physical demands of management as well
as the emotional and social demands of adjustment
Staying in hospitals, metabolic instability, blood glucose
self-control, and injections, keeping a strict diet, and long-
term complications are major illness-specific stressors to be
dealt with
. Longitudinal data has shown that adolescents
with Type 1 diabetes seem to be extraordinarily burdened by
illness-specific stressors in addition to everyday stressors
. Specific aspects of Type 1 diabetes and its management
may be possibly so stressful for the adolescent with this
chronic disease that they may trigger eating disorders — or
more commonly in this age group—subclinical eating
disturbances of a bulimic nature
. It seems that girls
with Type 1 diabetes have at least a more than twofold risk
for developing an eating disorder than do their nondiabetic
peers
, however, this is still controversial because
some studies have shown no increased frequency compared
with controls
. In the context of Type 1 diabetes,
eating disorders are an alarming phenomenon because they
can have serious health complications
Specific coping styles in youths with Type 1 diabetes
have been linked with symptoms (like neglect of self-
monitoring, waiving dietary recommendations, and insulin
injections) that could be relevant for the development of an
eating disorder
. Age has an effect on these coping
styles. Children more frequently use wishful thinking and
cognitive restructuring, being followed by distraction, social
support, problem solving, and emotional regulation
0022-3999/05/$ – see front matter
D 2005 Elsevier Inc. All rights reserved.
doi:10.1016/j.jpsychores.2005.02.010
B
This study was supported by two grants of the Jubilaeumsfonds
of the National Bank of Austria (OENB Grant Numbers 9376 and 11086)
to AK.
T
Corresponding author. Tel.: +43 1 40400 3057; fax: +43 1 9147317.
E-mail address: andreas.karwautz@meduniwien.ac.at (A. Karwautz).
Journal of Psychosomatic Research 59 (2005) 65 – 72

The more efficacious strategies for children are social
support and problem solving, followed by cognitive
restructuring
. Adolescents, however, use more often
resignation, wishful thinking, and problem solving, fol-
lowed by cognitive restructuring. Social support and
problem solving are seen as the more helpful strategies
dealing with diabetes-specific stressors, followed by resig-
nation and cognitive restructuring by this age group
There is a gap in the literature concerning coping
strategies used by adolescents with Type 1 diabetes having
eating problems. It is important to identify the relative
contributions of important factors that favor the manifes-
tation of eating disorders, because eating disorders are
multifactorially influenced phenomena. Researchers have
suggested that the use of particular coping strategies in
populations without a chronic illness may contribute to the
onset and progression of eating pathology
. They
also proposed women with eating disorders being less
efficacious in their coping before the onset of their eating
disorder than do women without later eating disorders.
Furthermore, specific aspects of psychological control in
interpersonal relations and bodily functions while coping
with Type 1 diabetes in eating disordered patients seem to
predict levels of metabolic control
Diabetes care poses a constant challenge on the well-
being of the adolescent while coping with the demands of
this chronic metabolic disease. Subjective well-being serves
as very important comprehensive indicator of the health
condition of a particular person and has been consistently
found to be poorer in youths with Type 1 diabetes compared
with their healthy peers
. Linking specific coping
strategies with quality of life and subjective well-being in
a population of youth with both diabetes and eating
disturbance has not been studied so far.
As part of a larger study on several relational aspects
between Type 1 diabetes and eating disorders
, we
therefore aimed (1) to investigate coping strategies during
diabetes-related stressful situations in adolescents with Type
1 diabetes as a function of their eating disorder status, and
(2) to identify how coping strategies that differentiate
between eating-disordered and non-eating-disordered ado-
lescents with Type 1 diabetes are associated with subjective
well-being, and (3) with the quality of metabolic control.
Methods
Participants
Recruitment for this study was part of a larger project
involving adolescent girls and boys with Type 1 diabetes
and their families, assessing psychological, familial, and
biological factors affecting their eating behavior
The study protocol was approved by the Ethics Committee
of the University Hospital Vienna. Eligible adolescents were
identified from current outpatients at our diabetes care unit
and other general province hospitals. Potential participants
were contacted directly during their clinical visits or
during their stay at a diabetes camp. Informed written
consent was obtained from each participant (and also from
a parent, for those less than 16 years of age). In a first step,
251 adolescents were approached for screening purposes,
and 199 of them (96 girls and 103 boys) returned complete
self-report measures. Thirty-five (17.6%) of these scored
above the predetermined cut-off scores and were subse-
quently interviewed in person with a semistructured inter-
view. Their body mass index (BMI) was 20.4 (S.D.=3.3), on
average, and the duration of diabetes since first diagnosis
was 5.6 years (S.D.=3.4), on average. They had been visiting
their consultant paediatrician 5.6 (S.D.=3.7) times in the
preceding year and had a mean glycosylated haemoglobin
(HbA1c) blood levels of 8.4% (S.D.=1.8%). All participants
came from middle socioeconomic backgrounds according to
Kleining and Moore
. Seventy-six percent of their
parents were married, and 9% lived separated, were
divorced, raised a child alone, or lived in a partnership,
without being married. Mothers were professionals (9.6%),
employees (60.4%), housewives or unemployed (25.2%), or
retired (0.8%). Fathers were professionals (16.4%), employ-
ees (68.8%), unemployed (0.8%), retired (2.4%), and
students (0.4%).
Classification of eating disorder status
Eating disorders were diagnosed according to Diagnostic
and Statistical Manual of Mental Disorders (DSM-IV;
). Subthreshold eating and weight loss behaviors and
shape concerns were diagnosed according to criteria based
largely on the study conducted by Jones et al.
. On the
basis of the adolescents’ responses, the patients were
categorized into one of two beating status groupsQ
[1]
Clinical eating disorders and mild eating and shape
problems (subthreshold): This category included
patients who met DSM-IV criteria for anorexia
nervosa (AN), bulimia nervosa (BN), or eating
disorders not otherwise specified (ED-NOS) and also
girls and boys who met one of the following criteria:
occasional binge eating (a minimum of three epi-
sodes); subsyndromal binge eating disorder (almost all
of the proposed research criteria of binge-eating
disorder have been met except for one); purging over
the past 3 months; repeated chewing and spitting out of
food to prevent weight gain (at least once a week over
the preceding 3 months or twice a week over the past
4 weeks); regular extreme dietary restraint [b2.1 MJ
(501.9 kcal)/day]; excessive exercising (more than
120 min, five times a week) for purpose of weight loss
over the past 4 weeks in the absence of binge eating;
problems in body image or eating attitudes, as
indicated by a mean score of z2 on the bweight
concernQ or a mean score of z2 on the bshape concernQ
V. Grylli et al. / Journal of Psychosomatic Research 59 (2005) 65 –72
66

subscales of the Eating Disorders Examination (EDE;
see below).
[2]
No eating problems: This category included patients
who reported no problems in eating attitudes and
behaviors, as reflected by the absence of a clinical
eating disorder and of a subthreshold eating and shape
problems (that is, this category included those who
screened positive but were subsequently found not to
have full-blown pathology).
Measures
The Eating Attitudes Test-26 (EAT-26;
) is probably
the most widely used standardized self-report measure of
symptoms and concerns characteristic of an eating disorder,
which has been extensively used as screening measure
and also in studies including populations with diabetes
. The EAT-26 alone does not yield a specific
diagnosis of an eating disorder. However, studies have
shown that it can be an efficacious screening instrument (in
particular, for anorexic behavior) as a part of a two-stage
screening process in which those who score at or above a
cut-off score are interviewed in person
. A total
score of z20 was used as a cut-off score.
The Eating Disorders Inventory-2 (EDI-2;
) is a self-
report measure designed for the assessment of attitudinal
and behavioral dimensions relevant to anorexia and bulimia
nervosa, with satisfactory reliability and validity data
Three important subscales bdrive for thinnessQ (z9), bbody
dissatisfactionQ (z15), and bbulimia symptomsQ (z5) serve
as cut-off measures.
The EDE/Version 12.0 D (EDE;
) is a semistructured
diagnostic interview that quantifies the symptoms, behavior,
and psychopathology of eating disorders and allows eating
disorders to be diagnosed according to the DSM-IV. This
interview is the bgold standardQ for the assessment of eating
disorders and has good reliability and validity. The
interviewers (VG, A H-G) were trained in the correct use
of this interview by Dr. Hilbert (Marburg). The current
version includes items that have been specifically developed
for people suffering from diabetes.
The KIDCOPE
is a self-report measure of coping
strategies with disease-related and everyday problems in
chronically ill children and adolescents based on the
Lazarus and Folkman theory of stress and coping and
assesses both the frequency and the efficacy of cognitive
and behavioral specific coping strategies. Ten coping
strategies are being considered: bdistractionQ, bsocial with-
drawalQ, bwishful thinkingQ, bresignationQ (avoidant coping),
bcognitive restructuring Q, bproblem-solving Q, bemotional
regulationQ, bsocial support Q (active coping), and bself-
blameQ and bblaming othersQ (negative coping). There are
two versions of the test: the children-version (KID-COPE-C),
designed for children aged 7–12.9 years, and the adolescents-
version (KID-COPE-A) for youths aged 13–18.9 years. The
internal consistency for both versions is judged to be
sufficient for illness-related problems. The ratings for
frequency of each coping strategy of the KID-COPE-C are
dichotomized. The ratings for efficacy of the KID-COPE-C
are given on a three-point Likert scale.
The ratings for frequency of each coping strategy for the
KID-COPE-A (ages 13 –18.9) were made on a four-point
Likert-scale but were dichotomized — as either occurring or
not occurring
. The ratings on the efficacy scales of the
KID-COPE-A again were made on a five-point Likert scale,
but they were categorized as not, lowly, or highly effica-
cious. In this way the older, and younger, adolescent
versions of the KIDCOPE were made comparable.
The Berner Subjective Well-being Inventory (BFW,
is a 39-item self-report measure that assesses two separate
aspects of subjective well-being: bsatisfactionQ and bill-
being Q. The components of satisfaction are bpositive attitude
towards lifeQ, bself-valueQ, bdepressive moodQ, and bjoy in
livingQ. Ill-being comprises bproblem-awarenessQ and
bsomatic complaints and reactionsQ. The BFW meets
accepted psychometric criteria with respect to reliability,
stability, and validity
Glycosylated Haemoglobin (HbA1c) was measured by
high-performance liquid chromatography (Fa. Minarini).
The nondiabetic range is 4.5 – 6.3%.
BMI was calculated as the weight in kilograms (kg)
divided by the squared height (h
2
) in meters. A BMI V5th
percentile or a BMI z91st percentile was used as a cut-off
measure.
Data analysis
Data on coping strategies as a function of the eating
disorder status in adolescents with Type 1 diabetes were
analyzed using the chi-square test for proportions. Bio-
medical data and data on the subjective quality of life of
adolescents with Type 1 diabetes as a function of their
eating disorder status were analyzed using t tests for
independent samples (normal distribution assumptions were
met). Bivariate correlations between coping strategies, well-
being, and HbA1c were calculated with Sperman rho tests
(skewed distribution). All calculations were computed with
SPSS, Version 11.5
. The results of the statistical tests
were considered significant when Pb.05.
Results
Sociodemographics across the two diagnostic groups
From the 35 adolescents who reached the cut-off score
(30 girls and 5 boys), 9 did not meet the criteria for a DSM-
IV-classified eating disorder or for subthreshold eating
problems. Among girls above the cut-off criteria, none had
AN (307.1), two had BN (307.51), and nine had ED-NOS
(307.50). In addition, 12 girls and 1 boy had subthreshold
disorders (details given in
). For further analyses, patients
V. Grylli et al. / Journal of Psychosomatic Research 59 (2005) 65–72
67
with DSM-IV diagnoses and with subthreshold eating
problems were pooled together. The two diagnostic groups
[Type 1 diabetes with (n=24, i.e., 23 girls and 1 boy) and
without (n=175, i.e., 73 girls and 102 boys) an eating
disorder/problem] did not differ in age (14.1F2.1 vs.
14.1F2.6; df =197, P =.39), duration of illness (6.3F3.3
vs. 5.5F3.5; df =196, P =.27), number of consultations
per year (6.0F2.5 vs. 5.6F3.8; df =183, P =.68), and
metabolic control (8.8F2.0 vs. 8.3F1.8; df =184, P =.24).
However, the patients with disordered eating were pre-
dominantly female and had a significantly higher BMI
than did the diabetic adolescents without eating problems
(22.3F3.6 vs. 20.2F3.2; t =2.86; df =193; P =.005).
Frequency and efficacy in the group with eating disorders
and problems
Adolescents with disordered eating more frequently used
wishful thinking and emotional regulation and less fre-
quently blaming others as their strategies of coping.
Cognitive restructuring and emotional regulation were
experienced as the more, blaming others as the less
efficacious strategies.
Frequency and efficacy in the diabetes group without eating
disorders and problems
Adolescents without disordered eating more frequently
used cognitive restructuring and wishful thinking and less
frequently blaming others and self-blame as their strategies
of coping. Social support and cognitive restructuring were
experienced as the more, self-blame and blaming others as
the less efficacious strategies.
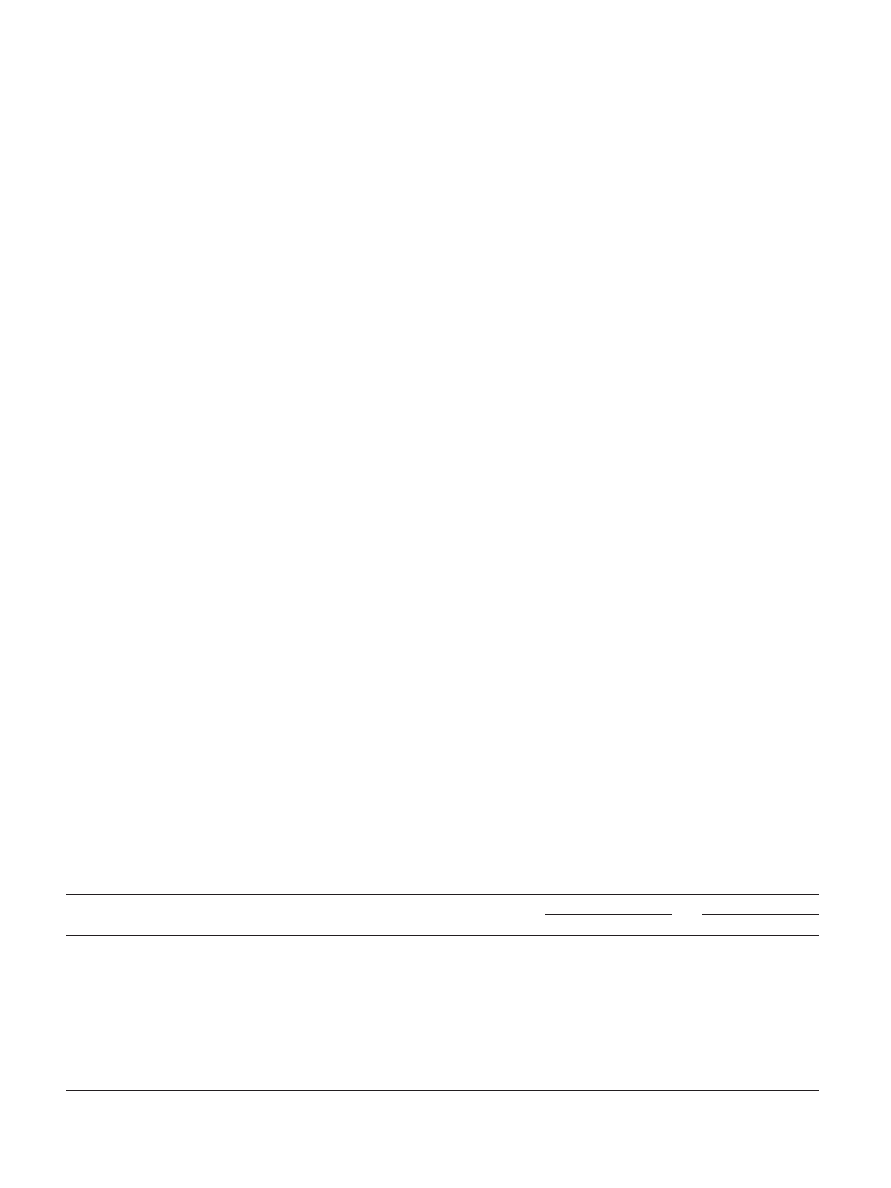
Frequency and efficacy of coping strategies across the
eating status groups
The frequencies of coping strategies selected during a
stressful diabetes-related situation, like measuring blood
sugar, dieting, and injecting insulin, are given in
Adolescents with disordered eating behavior signifi-
cantly more often used self-blaming and wishful thinking,
and significantly less often blaming others than did the
group of adolescents with Type 1 diabetes without eating
problems and body image concerns.
Adolescents with disordered eating behavior rated dis-
traction (v
2
= 6.15, P = .04), social withdrawal (v
2
= 6.94,
x = 0.03), and wishful thinking (v
2
= 5.53, P = .05) as signifi-
cantly more efficacious strategies and problem solving
(v
2
= 13.56, P = .001) as significantly less efficacious than
did the group of adolescents with Type 1 diabetes without
eating problems and body image concerns (
Quality of life across the eating status groups
Adolescents with disordered eating behavior had less
positive attitudes toward life [t(25.3) = 3.65, P =.001], more
problems [t(193) = 2.55, P =.01], more somatic complaints
and reactions [t(193) =3.46, P =.001], lower self-esteem
[t(24.4)=4.14, Pb.000], higher depressive mood [t(190) =
3.62, Pb.000], and lower joy in life [t(190)=4.79, Pb.000]
than did the adolescents without eating problems and body
image concerns.
Correlations between coping strategies, quality of life, and
HbA1c
Bivariate correlations were calculated between frequent
coping strategies used by adolescents with Type 1 diabetes
as a function of their eating disorder status, the quality of
life variables, and HbA1c. bSelf-criticismQ correlated
positively with problems (r =.22, Pb.003), somatic com-
plaints, and reactions (r =.17, P =.02) and negatively with
self-esteem (r =.19, P =.01) and HbA1c (r =.21, P =.005).
The coping strategy bblaming othersQ correlated positively
with problems (r =.14, P =.05) and joy in life (r =.16,
P =.03). Finally, the coping strategy bwishful thinkingQ
correlated positively with problems (r =.30, Pb.000),
depressive mood (r =.20, P =.001), and HbA1c (r =.18,
P =.01) and negatively with positive attitude towards life
Table 1
Coping strategies used by adolescents with Type 1 diabetes with and without an eating problem — frequency and efficacy
Coping strategy
Frequency
in ED (%)
Frequency
in NED (%)
Efficacy
in ED (%)
Efficacy
in NED (%)
Frequency ED vs. NED
Efficacy ED vs. NED
v
2
value
P value
v
2
value
P value
Distraction
56.5
58.6
46.2
20.4
0.03
Ns
6.15
.04
Social withdrawal
60.9
44.0
21.4
19.2
2.40
Ns
6.94
.03
Cognitive restructuring
73.9
85.7
52.9
52.4
2.52
Ns
0.93
Ns
Self-blame
52.2
29.8
16.7
10.0
4.64
.05
0.57
Ns
Blaming others
4.3
21.9
0
13.5
3.93
.05
3.94
Ns
Problem solving
78.3
76.9
38.9
46.5
0.15
Ns
13.56
.001
Emotional regulation
82.6
69.0
52.6
42.5
1.80
Ns
3.60
Ns
Wishful thinking
100
81.7
39.1
23.9
5.03
.03
5.53
.05
Social support
73.9
78.6
47.1
60.3
0.45
Ns
3.35
Ns
Resignation
78.3
69.6
27.8
48.3
0.73
Ns
4.24
Ns
NS = not significant; ED = Type 1 diabetes with eating disorder/problem; and NED = Type 1 diabetes without eating disorder/problem.
V. Grylli et al. / Journal of Psychosomatic Research 59 (2005) 65 –72
68

(r =.20, Pb.01) and self-esteem (r =.16, P b.03). The low
correlations with high statistical significance in the present
calculations could be due to the high homogeneity of the
sample with respect to eating disorder status.
Discussion
We investigated coping strategies during diabetes-related
stressful situations in adolescents with Type 1 diabetes as a
function of their eating disorder status and identified how
coping strategies that differentiate between eating disor-
dered and non-eating-disordered adolescents with Type 1
diabetes were associated with subjective well-being and also
with the quality of metabolic control.
We found, first, that adolescents with Type 1 diabetes and
eating problems–predominantly female–when confronted
with disease-related stressors, tend to blame themselves
about the situation and to resort to wishful thinking. These
findings parallel findings from other studies in adolescents
with Type 1 diabetes but without eating problems
which have suggested that adolescents with poor adherence
to diabetes management tend to use more often avoidant and
negative coping strategies. In addition, findings within the
eating disorders research literature have demonstrated that,
when under stressful situations, young women with bulimia
nervosa were more likely to blame themselves and were less
likely to receive crisis support from either a partner or
another very close person
. Women with eating disorders
were more likely to use cognitive avoidance or cognitive
rumination and were less likely to downplay their problems
. Similar findings have been also reported in other
studies of young women with eating disorders, where
bulimic patients were more likely to use emotional reactions,
like self-blaming and escape avoidance, to reduce stress and
were less likely to seek emotional support
Adolescents with Type 1 diabetes and with eating
problems judge as more efficacious the coping strategies
distraction, social withdrawal, and wishful thinking com-
pared with adolescents with Type 1 diabetes without eating
problems. Such reactions could be better understood in the
light of the attempts of the adolescent to achieve more
independence and autonomy. In the case of Type 1 diabetes,
the family must keep a watchful eye over the behavior of the
adolescent to fulfil the requirements of the treatment
regimen on the one hand, but on the other hand, the
situation may become irritable when the adolescent requires
more distance and independence
. Developing problem-
atic eating behavior may represent an answer to this conflict
in the absence of a more functional coping repertoire.
In a study including girls with Type 1 diabetes and eating
disturbances
, impairments in the mother–daughter
relationship seemed to lead to poor self-esteem and low
autonomy, resulting in social withdrawal, avoidance facing
the problematic situation, and general inefficacious coping.
Irrespective of the presence of an eating disorder, diabetes-
specific family conflict has been found to impact quality of
life in youths with Type 1 diabetes
. Internalizing
stress, blaming oneself, and engaging in disordered eating
seem, therefore, to supply these young women with ways of
reducing the tension. Body dissatisfaction, resulting from a
higher BMI in the group of adolescent girls with Type 1
diabetes and with an eating disorder, can possibly not be
dealt within the context of an important family bound, like
the mother–daughter relationship constitutes
We also found that adolescents with Type 1 diabetes and
disordered eating presented significant impairments in all
aspects of well-being compared with their nondisordered
peers: Their attitude towards life seem to be essentially more
negative, they perceived themselves as having more
problems not only regarding their relationships with
significant others (parents, school teachers, and peers) but
also concerning health-related problems, problems about
entering into adulthood, and financial problems. Further-
more, they complained significantly more often about
disturbing physical symptoms like headache, stomach ache,
nausea, sleeping disorders, lack of appetite, and circulatory
disturbances. Such symptoms may act as barriers from
accomplishing tasks like going to school or to work.
Additionally, a significant lower self-esteem was also
marked, characterised by feelings of personal ineffective-
ness and worthlessness. Central was also a significantly
more depressive mood colouring their everyday activities.
Finally, joyful life events were perceived as very rare
incidents in their everyday life.
Although generic quality of life in eating disordered
patients is a topic not completely understood, the present
findings are in keeping with the findings of a recent study on
the health-related quality of life in eating disordered adults
aged 18 –34 years (98% women), which demonstrated that
patients with eating disorders were more dysfunctional in all
areas of the measured health-related quality of life, i.e.,
physical functioning, physical role, bodily pain, general
health, vitality, social functioning, emotional role, and mental
health, than were women in the general population
Linking coping strategies and quality of life and HbA1c
in our data, it was demonstrated that the amount of
practicing self-criticism was positively associated with the
amount of perceived problems and the amount of somatic
complaints and reactions. It also demonstrated a positive
association with metabolic control. Moreover, the more
intensive the self-criticism, the poorer the self-esteem. On
the contrary, blaming others, a coping strategy significantly
more often used by adolescents without disordered eating,
was also positively associated not only with the amount of
problems but also with more joy in life. Shifting diabetes-
related problems to others may enhance the perception of a
more joyful life. Adolescents may, in this way, decentre
themselves from the problems that they face, and then,
released from responsibilities, could, at least transitorily,
enjoy life more. Finally, wishful thinking as an avoidant
coping strategy was also positively linked with the amount
V. Grylli et al. / Journal of Psychosomatic Research 59 (2005) 65–72
69

of perceived problems and depressive mood and negatively
linked with self-esteem. This coping strategy seems also to
have a negative influence on the quality of metabolic control.
In conclusion, the coping strategies utilized from adolescents
with eating disorders are negative, point to low self-perceived
personal control and self-efficacy, and are associated with
impeded quality of life and poor metabolic control.
The degree of perceived quality of life seems to be an
important indicator of overall health, because positive
changes in eating behavior correlate with higher quality of
life
. Such findings are encouraging in suggesting and
planning treatment concepts that enhance quality of life in
patients with eating disorders. Nevertheless, there is
evidence that, despite improvements in quality of life in
adult women with eating disturbances, they still remain
more dysfunctional even after 2 years of treatment,
compared with women in the general population. The
severity of eating disorders and the presence of anxiety
and depression at baseline significantly impede improve-
ment in well-being
. This finding is also in line with
observations from the tradition of psychodynamic psycho-
therapy, according to which persistence in individual
vulnerabilities, even after the disordered eating behavior
subsides, has been noted
Interventions like coping skills training
or
integrated inpatient therapy
could have a positive
impact on quality of life in adolescents with Type 1 diabetes
suffering from an eating disorder. In a 12-month longitudi-
nal study, adolescents with Type 1 diabetes, who were on
intensive insulin therapy, received a behavioral intervention
with the goal to increase their constructive coping styles
and, thus, to be more efficacious in achieving therapeutic
goals
. The findings demonstrated that adolescents with
Type 1 diabetes who received the training increased their
self-efficacy after 12 months, not only in diabetes-related
situations but also in other medical situations, than did these
adolescents who did not receive the training. They also
reported a less negative impact of diabetes on aspects of
biopsychosocial well-being. These findings were not so
robust in the shorter follow-up period
, mainly because
effects on self-efficacy may take longer periods to get
incorporated in the behavioral repertoire of the trainees
In other words, enhanced self-efficacy might impact the
personal models concerning the representation of an illness
and its management, which, in turn, influences the quality of
life in this population
The present findings represent just one part of the
important topic of relations between eating disorders and
Type 1 diabetes in youths. There are many more aspects of
adolescents’ lives that impact and are impacted by their
eating behaviors, including family, peers, genetics, tempera-
ment, and others
. Consequently, examining eating
problems in adolescents with Type 1 diabetes in a more
comprehensive manner would most likely provide a much
clearer and definitive understanding of the relationship
between eating problems and Type 1 diabetes.
The present study has several limitations. The cross-
sectional design does not permit conclusions about the
direction of the relationships between disordered eating,
coping strategies, and quality of life. Second, the two
screening measures for eating disorders (EAT and EDI),
although widespread, have not been developed for use or
been normed on a sample of youth with diabetes. Third, no
sensitivity and specificity data of the screening procedure
are reported. Forth, correlations between coping strategies
and the aspects of quality of life and HbA1c levels are low,
thus limiting their robustness. Longitudinal research in this
area to establish the specific course of events between
disordered eating, coping strategies, and quality of life
should be a major priority. Six, higher BMI and female
preponderance in the subgroup with eating problems could
be able to explain, in part, the differences between the
groups in the investigated psychosocial areas.
Conclusions
In conclusion, eating disorders and disordered eating
behaviors in adolescents with Type 1 diabetes seem to be
associated with certain negative and avoidant coping
strategies and an overall impeded quality of life. Coping
strategies utilized by adolescents with eating disorders are,
in turn, negatively associated with certain aspects of quality
of life, including the quality of metabolic control. Because
these factors could be important for the onset and
progression of eating disorders in adolescents with Type 1
diabetes, it is essential that they are addressed in the process
of a multidisciplinary diagnostic and treatment procedure
involving adolescents who are at risk for developing eating
problems. Such psychological monitoring has been found
to have favorable effects on the quality of life of adults
with diabetes
and could facilitate better metabolic
control in youths with Type 1-diabetes
through self-
care empowerment
Acknowledgments
This study was supported by two grants of the
Jubilaeumsfonds of the National Bank of Austria (OENB-
Grant Numbers 9376 and 11086) to AK. Presented in part at
the International congress on eating disorders in Alpbach,
October 2003.
References
[1] Hanson CL, Cigrang JA, Harris MA, Carle DL, Relyea G, Burghen
GA. Coping styles in youths with insulin-dependent diabetes mellitus.
J Consult Clin Psychol 1989;57:651 – 64.
[2] Coffey JT, Brandle M, Zhou H, Marriott D, Burke R, Tabael BP,
Engelgau MM, Kaplan RM, Herman WH. Valuing health-related
quality of life in diabetes. Diabetes Care 2002;25:2238 – 43.
V. Grylli et al. / Journal of Psychosomatic Research 59 (2005) 65 –72
70

[3] Seiffge-Krenke I. Adolescent, parental, and family coping with
stressors. In: Seiffge-Krenke I, editor. Diabetic adolescents and their
families: stress, coping, and adaptation. UK7 Cambridge Univ Press,
2001. pp. 85 – 117.
[4] Nielsen S. Eating disorders in females with type 1 diabetes: an update
of a meta-analysis. Eur Eat Disord Rev 2002;10:241 – 54.
[5] Rodin G, Olmsted MP, Rydall AC, Maharaj SI, Colton PA, Jones JM,
Biancucci LA, Daneman D. Eating disorders in young women with
type 1 diabetes. J Psychosom Res 2002;53:943 – 9.
[6] Herpertz S, Wagener R, Albus C, Kocnar M, Wagner R, Best F,
Schleppinghoff BS, Filz HP, Forster K, Thomas W, Mann K,
Kohle K, Senf W. Diabetes mellitus and eating disorders: a multi-
center study on the comorbidity of the two diseases. J Psychosom
Res 1998;44:503 – 15.
[7] Jones JM, Lawson ML, Daneman D, Olmsted MP, Rodin G. Eating
disorders in adolescent females with and without type 1 diabetes:
cross sectional study. BMJ 2000;320:1563 – 6.
[8] Grylli V, Hafferl-Gattermayer A, Karwautz A, Schober E. Prevalence
and clinical manifestations of eating disorders in Austrian adolescents
with type 1 diabetes. Wien Klin Wochenschr 2004;116/7-8:230 – 4.
[9] Colton P, Olmsted M, Daneman D, Rydall A, Rodin G. Disturbed
eating behavior and eating disorders in preteen and early teenage girls
with type 1 diabetes: a case-controlled study. Diabetes Care 2004;
27:1654 – 9.
[10] Peveler RC, Fairburn CG, Boller I, Dunger D. Eating disorders in
adolescents with IDDM: a controlled study. Diabetes Care 1992;15:
1356 – 60.
[11] Striegel-Moore RH, Nicholson TJ, Tamborlane WV. Prevalence of
eating disorder symptoms in preadolescent and adolescent girls with
IDDM. Diabetes Care 1992;15:1361 – 8.
[12] Robertson P, Rosenvinge JH. Insulin-dependent diabetes mellitus: a
risk factor in anorexia nervosa or bulimia nervosa? An empirical study
of 116 women. J Psychosom Res 1990;34:535 – 41.
[13] Rydall AC, Rodin GM, Olmsted MP, Devenyi RG, Daneman D.
Disordered eating behavior and microvascular complications in young
women with insulin-dependent diabetes mellitus. N Engl J Med
1997;336:1849 – 54.
[14] Herpertz S, Albus C, Kielmann R, Hagemann-Patt H, Lichtblau K,
Kohle K, Mann K, Senf W. Comorbidity of diabetes mellitus and
eating disorders: a follow-up study. J Psychosom Res 2001;51:673 – 8.
[15] Takii M, Komaki G, Uchigata Y, Maeda M, Omori Y, Kubo C.
Differences between bulimia nervosa and binge-eating disorder in
females with type 1 diabetes: the important role of insulin omission.
J Psychosom Res 1999;47:221 – 31.
[16] Cantwell R, Steel JM. Screening for eating disorders in diabetes
mellitus. J Psychosom Res 1996;40:15 – 20.
[17] Delamater AM, Kurtz SM, Bubb J, White NH, Santiago JV. Stress and
coping in relation to metabolic control in adolescents with type 1
diabetes. Dev Behav Pediatr 1987;8:136 – 40.
[18] Graue M, Wentzel-Larsen T, Bru E, Hanestad BR, Sovik O. The
coping styles of adolescents with type 1 diabetes are associated with
degree of metabolic control. Diabetes Care 2004;27:1313 – 7.
[19] Rathner G, Zangerle M. Copingstrategien bei Kindern und Jugend-
lichen mit Diabetes mellitus Die deutschsprachige Version des
KIDCOPE. Z Klin Psychol Psychiatr Psychother 1996;44:49 – 74.
[20] Ghaderi A, Scott B. Coping in dieting and eating disorders: a
population-based study. J Nerv Ment Dis 2000;188:273 – 9.
[21] Troop NA, Holbrey A, Treasure JL. Stress, coping, and crisis support
in eating disorders. Int J Eat Disord 1998;24:157 – 66.
[22] Surgenor LJ, Horn J, Hudson SM, Lunt H, Tennent J. Metabolic
control and psychological sense of control in women with diabetes
mellitus Alternative considerations of the relationship. J Psychosom
Res 2000;49:267 – 73.
[23] Surgenor LJ, Horn J, Hudson SM. Links between psychological sense
of control and disturbed eating behavior in women with diabetes
mellitus Implications for predictors of metabolic control. J Psychosom
Res 2002;52:121 – 8.
[24] Hesketh KD, Wake MA, Cameron FJ. Health-related quality of life
and metabolic control in children with type 1 diabetes. Diabetes Care
2004;27:415 – 20.
[25] Grylli V, Karwautz A, Hafferl-Gattermayer A, Schober E. Eating
disorders and type 1-diabetes mellitus in adolescence. Eat Weight
Disord 2003;8:88 – 94.
[26] Grylli V, Hafferl-Gattermayer A, Wagner G, Schober E, Karwautz A.
Eating disorders and eating problems among adolescents with type 1
diabetes: exploring relationships with temperament and character.
J Pediatr Psychol 2005;30:197 – 206.
[27] Kleining G, Moore H. Self-rating of social position (SSE). A
measurement of social class [Soziale Selbsteinstufung (SSE). Ein
Instrument zur Messung sozialer Schichten]. Kfln Z Soziol Sozialan-
thropol 1968;20:502 – 52.
[28] American Psychiatric Association. Diagnostic and statistical manual
of mental disorders, 4th edn (DSM-IV). Washington (DC)7 American
Psychiatric Association, 1994.
[29] Garfinkel PE, Newman A. The Eating Attitudes Test: twenty-five
years later. Eat Weight Dis 2001;6:1 – 24.
[30] Garner DM. The eating disorder inventory 2. Odessa (Fla)7
Psychological Assessment Resources Inc, 1991.
[31] Rathner G, Waldherr K. Eating Disorders Inventory-2. A German
language validation with norms for female and male adolescents.
Z Klin Psychol Psychiatr Psychother 1997;45:157 – 82.
[32] Fairburn CG, Cooper Z. The eating disorder examination. In: Fairburn
CB, Wilson GT, editors. Binge eating: nature, assessment and
treatment, 12th ed. New York7 Guilford, 1993. pp. 317 – 60.
[33] Spirito A, Stark LJ, Gil KM, Tyc VL. Coping with everyday and
disease-related stressors by chronically ill children and adolescents.
J Am Acad Child Adolesc Psychiatr 1995;34:283 – 90.
[34] Grob A, Lqthi R, Kaiser FG, Flammer A, Mackinnon A, Wearing AJ.
Berner Fragebogen zum Wohlbefinden Jugendlicher (BFW). Diag-
nostica 1991;37:66 – 75.
[35] SPSS 11.5 for Windows. Chicago, SPSS.
[36] Ball K, Lee C. Psychological stress, coping, and symptoms of
disordered eating in a community sample of young Australian women.
Int J Eat Disord 2002;31:71 – 81.
[37] Nagata T, Matsuyama M, Kiriike N, Iketani T, Oshima J. Stress
coping strategy in Japanese patients with eating disorders: relationship
with bulimic and impulsive behaviors. J Nerv Ment Dis 2000;188:
280 – 6.
[38] Koff E, Sangani P. Effects of coping style and negative body image on
eating disturbance. Int J Eat Disord 1997;22:51 – 6.
[39] Maharaj SI, Rodin GM, Olmsted MP, Connolly JA, Daneman D.
Eating disturbances in girls with diabetes: the contribution of
adolescent self-concept, maternal weight and shape concerns and
mother – daughter relationships. Psychol Med 2003;33:525 – 39.
[40] Laffel LMB, Connell A, Vangsness L, Goebel-Fabbri A, Mansfield A,
Anderson BJ. General quality of life in youth with type 1 diabetes
Relationship to patient management and diabetes-specific family
conflict. Diabetes Care 2003;26:3067 – 73.
[41] Maharaj SI, Rodin G, Olmsted MP, Daneman D. Eating disturbances,
diabetes and the family: an empirical study. J Psychosom Res
1998;44:479 – 90.
[42] Padierna A, Quintana JM, Arostegui I, Gonzalez N, Horcajo MJ. The
health-related quality of life in eating disorders. Qual Life Res
2000;9:667 – 74.
[43] Danzl C, Kemmler G, Gottwald E, Mangweth B, Kinzl J, Biebl W.
Quality of life in patients with eating disorders: results of a pilot study.
Psychiatr Prax 2001;28:18 – 23.
[44] DeGroot J, Rodin G. Eating disorders, female psychology and the self.
J Am Acad Psychoanal 1994;22:299 – 317.
[45] Grey M, Boland EA, Davidson M, Yu C, Tamborlane WV. Coping
skills training for youth with diabetes mellitus has long-lasting effects
on metabolic control and quality of life. J Pediatr 2000;137:107 – 13.
[46] Takii M, Ushigata Y, Komaki G, Nozaki T, Kawai H, Iwamoto Y,
Kubo C. An integrated therapy for type 1 diabetic females with
V. Grylli et al. / Journal of Psychosomatic Research 59 (2005) 65–72
71

bulimia nervosa: a 3-year follow-up study. J Psychosom Res
2003;55:349 – 56.
[47] Grey M, Boland EA, Davidson M, Yu C, Sullivan-Bolyai S,
Tamborlane WV. Short-term effects of coping skills training as adjunct
to intensive therapy in adolescents. Diabetes Care 1998;21:902 – 8.
[48] Skinner TC, Hampson SE. Personal models of diabetes in relation to
self-care, well-being, and glycaemic control. A prospective study in
adolescence. Diabetes Care 2001;24:828 – 33.
[49] Pouwer F, Snoek FJ, Van der Ploeg HM, Ader HJ, Heine RJ.
Monitoring of psychological well-being in outpatients with diabetes.
Diabetes Care 2001;24:1929 – 35.
[50] Hoey H, Aanstoot HJ, Chiarelli F, Daneman D, Danne T, Dorchy H,
Fitzerald M, Garandeau P, Greene P, Holl R, Hougaard P, Kaprio F,
Kocova M, Lynggaard H, Martul P, Matsuura N, McGee HM,
Mortensen HB, Robertson K, Schoenle E, Sovik O, Swift P, Tsou RM,
Vanelli M, Aman J. Good metabolic control is associated with better
quality of life in 2,101 adolescents with type 1 diabetes. Diabetes Care
2001;24:1923 – 8.
[51] Anderson R, Funnell M, Carlson A, Saleh-Statin N, Cradock S,
Skinner TC. Facilitating self-care through empowerment. In:
Frank FJ, Chas Skinner T, editors. Psychology in diabetes care.
West Sussex, UK: John Wiley & Sons, 2000. pp. 69 – 97.
V. Grylli et al. / Journal of Psychosomatic Research 59 (2005) 65 –72
72
Document Outline
- Disturbed eating attitudes, coping styles, and subjective quality of life in adolescents with Type 1 diabetes
- Introduction
- Methods
- Results
- Sociodemographics across the two diagnostic groups
- Frequency and efficacy in the group with eating disorders and problems
- Frequency and efficacy in the diabetes group without eating disorders and problems
- Frequency and efficacy of coping strategies across the eating status groups
- Quality of life across the eating status groups
- Correlations between coping strategies, quality of life, and HbA1c
- Discussion
- Conclusions
- Acknowledgments
- References
Wyszukiwarka
Podobne podstrony:
KWESTIONARIUSZ STRATEGII RADZENIA SOBIE Z BÓLEM (CSQ) - opis, KWESTIONARIUSZ STRATEGII RADZENIA SOBI
KWESTIONARIUSZ STRATEGII RADZENIA SOBIE Z BÓLEM (CSQ) - test
Stres zawodowy a obciążenia w pracy oraz strategie radzenia sobie
2 Medycyna Stoma 2013 14 Rolińska Oddychanie przeponowe i relaksacja jako szybkie techniki radzenia
Radzenie sobie z myślami mogącymi przyczynić się do nawrotu
Zachowania asertywne jako jeden ze sposobów radzenia sobie z agresją(1), PRZEDSZKOLE
Religia jako sposob radzenia sobie
Psychologia wykład 1 Stres i radzenie sobie z nim zjazd B
stres radzenie sobie do wysl 9
Sposoby radzenia sobie ze stresem, Filologia polska, Koncepcje i praktyki nauczania i wychowania
Stres i radzenie sobie, Emocje i motywacja
Trzy metody radzenia sobie z konfliktami, Koncepcje i Praktyki Wychowania
Stres i radzenie sobie
Sposoby radzenia sobie z trudnymi sytuacjami(2)
Uzależnienie od miłości wśród kobiet a radzenie sobie w życiu
więcej podobnych podstron