Improving primary care treatment of depression among patients with
diabetes mellitus: the design of the Pathways Study
Wayne Katon, M.D.
a,
*, Michael Von Korff, ScD.
b
, Elizabeth Lin, M.D., M.P.H.
b
,
Greg Simon, M.D., M.P.H.
b
, Evette Ludman, Ph.D.
b
, Terry Bush, Ph.D.
b
, Ed Walker, M.D.
a
,
Paul Ciechanowski, M.D., M.P.H.
a
, Carolyn Rutter, Ph.D.
b
a
Department of Psychiatry and Behavioral Sciences, University of Washington School of Medicine, Seattle, WA 98195– 6580, USA
b
Center for Health Studies, Group Health Cooperative, Psychiatry Service, University Hospital, Seattle, WA 98195– 6580, USA
Abstract
This paper describes the methodology of a population based study of primary care patients with diabetes mellitus enrolled in a health
maintenance organization. The first goal was to determine the prevalence and impact of depression in patients with diabetes. The second
goal was to randomize approximately 300 patients with diabetes and major depression and/or dysthymia in a trial to test the effectiveness
of a collaborative care intervention in improving quality of care and health outcomes among patients with diabetes and depression. © 2003
Elsevier Inc. All rights reserved.
1. Introduction
Diabetes is a common and costly condition that affects 16
million Americans [1]. Patients with diabetes are at increased
risk of kidney disease, peripheral vascular disease, heart dis-
ease, lower extremity ulcers and amputations, retinal disease,
neuropathy, infections, digestive disease and periodontal dis-
ease [2]. The prevalence is as high as 20% in patients who are
65 years and over with significantly higher rates in minority
group members (African Americans, Hispanics and Native
Americans) [3]. The total direct medical costs and indirect
costs in the United States due to diabetes have been estimated
at $102 billion per year [4]. Patients with diabetes appear to
have increased risk of major depression. Depression may ad-
versely affect self-care regimens as well as increase risk of
complications such as diabetic retinopathy [5–7].
Anderson and colleagues’ recent meta-analysis of the
prevalence of major depression or depressive symptoms in
patients with diabetes found a two-fold higher prevalence
rate of depression in diabetics compared to controls in 20
controlled studies [5]. Current major depression was ob-
served in 10 to 15% of diabetics with similar prevalence
rates in Type 1 and Type 2 cases [5].
Both major depression and depressive symptoms have been
shown in most studies to be associated with glucose dysregu-
lation [6 – 8]. This may either be due to the adverse impact of
depression on diabetes self-care (i.e., diet, exercise, checking
blood glucose, and taking medications), [6 – 8] direct adverse
physiologic effects on glucose metabolism, [9] or a combina-
tion of these two mechanisms. Several studies have shown that
depression is associated with poor adherence to self-care reg-
imens such as checking blood glucose, following a special diet
and medication compliance, as well as less sensitivity to insu-
lin effects on lowering blood glucose [6,10].
Two small randomized trials have shown that nortripty-
line [11] and fluoxetine [12] were more efficacious in con-
trolling depressive symptoms than placebo in patients with
major depression and diabetes. One cognitive behavioral
trial also demonstrated enhanced efficacy compared to an
educational diabetes group [13]. One of these 3 trials found
that improved depression outcomes was associated with
improved HbA
1
C levels [13]. These three trials enrolled a
combined total of less than 180 patients and lacked power to
study key outcomes such as the effect of enhanced treatment
of depression on self-care regimens (diet, exercise, refilling
medication), disability, quality of life, and medical costs.
Whether enhanced treatment of depression improves glyce-
mic control is also an unanswered question.
The study that we describe has two arms: 1) a popula-
tion-based epidemiologic investigation of the prevalence
* Corresponding author. Tel.:
⫹1-206-543-7177; fax: ⫹1-206-221-
5414.
E-mail address: wkaton@u.washington.edu (W.J. Katon).
General Hospital Psychiatry 25 (2003) 158 –168
0163-8343/03/$ – see front matter © 2003 Elsevier Inc. All rights reserved.
doi:10.1016/S0163-8343(02)00013-6

and impact of depression in patients with diabetes enrolled
in a health maintenance organization; and 2) a randomized
controlled trial to test the effectiveness of collaborative care
interventions in improving the quality of care and outcomes
of depression among patients with diabetes in primary care.
This paper describes the design of these research studies and
the rationale for key methodologic decisions. The first part
of the Methods section will describe the recruitment for the
epidemiologic phase of the study, and the second part the
design of the randomized controlled trial.
2. Methods
The Pathways Study was developed by a multidisci-
plinary team in the Department of Psychiatry at the Univer-
sity of Washington and the Center for Health Studies at
Group Health Cooperative. Group Health is a nonprofit
health maintenance organization with 30 primary care clin-
ics in Western Washington State.
The study was funded by the National Institute of Mental
Health Services (NIMH) Division of Intervention and Ser-
vices Research. The randomized controlled trial proposed to
test the effectiveness of a collaborative care intervention
versus usual care. Collaborative care is a multimodal inter-
vention that includes integration of a “care manager” (often
a nurse or mental health specialist) into primary care. The
“care manager” works with both the patient and primary
care physician and helps with developing a shared definition
of the problem, providing patient education and support,
developing a shared focus on specific problems, targeting
goals and a specific action plan, offering support and prob-
lem-solving to optimize self-management, achieving closer
monitoring of adherence and outcomes, and facilitating ap-
pointments to the primary care physician or specialist for
patients with adverse outcomes or side-effects [14]. The
study protocol was reviewed and approved by institutional
review boards at the University of Washington and Group
Health Cooperative.
2.1. Study setting
Nine Group Health Cooperative primary care clinics in
western Washington were selected for the study. We se-
lected clinics based on 3 criteria: 1) clinics with the largest
number of diabetic patients (to save screening and interven-
tion costs; 2) clinics within a 40-mile geographic radius of
Seattle in order to decrease travel time for nurse “care
managers”; and 3) clinics with the highest percentage of
minority patients. Because minorities have higher rates of
diabetes, we were able to enroll substantial numbers of
minority patients even though the general population was
predominantly Caucasian.
2.2. Sample recruitment
A major methodologic issue was how to best screen and
enroll a representative sample of diabetic patients with ma-
jor depression and dysthymia. The screening was facilitated
by Group Health’s prior development of a population-based
diabetes registry. Patients are added to the diabetes registry
based on: 1) currently taking any diabetic agent; or 2) a
fasting glucose
ⱖ126 confirmed by a second out-of-range
test within one year; or 3) a random plasma glucose
ⱖ200
also confirmed by a second test within one year; or 4) a
hospital discharge diagnosis of diabetes at any time during
GHC enrollment or two outpatient diagnoses of diabetes
[15]. The goal of the epidemiologic survey was to success-
fully screen at least 4,500 primary care patients with diabe-
tes with approximately 630 expected to meet criteria for
major depression and/or dysthymia. The goal of the ran-
domized trial was to enroll approximately 300 depressed
patients in the randomized controlled trial. After consider-
ing mail versus telephone screening for depression, we
decided on mail screening as the most cost effective mech-
anism based on prior studies by members of our study group
that were able to attain 60 to 65% recruitment rates with
mail screening [7,16]. To potentially increase patient re-
sponse rates, we presented the study to each of the 9 clinics
and requested written permission from all primary care
physicians to use a stamp of their signature in the approach
letter describing the study. Among the 113 doctors, 101
(90%) agreed to allow us to use their signature stamp. For
physicians refusing to let us use their signature, we used the
name of the GHC Chief of endocrinology, Dr. David Mc-
Culloch.
Patients were screened by mail in sequential waves with
approximately 700 questionnaires sent per month. A $3 gift
certificate for a local store was included with the mailing to
encourage response. If the patient did not return a mailed
packet by 4 weeks, a second packet was sent. If this second
packet was not returned by 2 weeks, the patient received a
telephone reminder call. The first mail-screen had a re-
sponse rate of approximately 38%, the second mailing in-
creased the response rate to 47%, and the combination of the
telephone reminder and a last mailing 6 months after the
telephone reminder increased the final response rate to
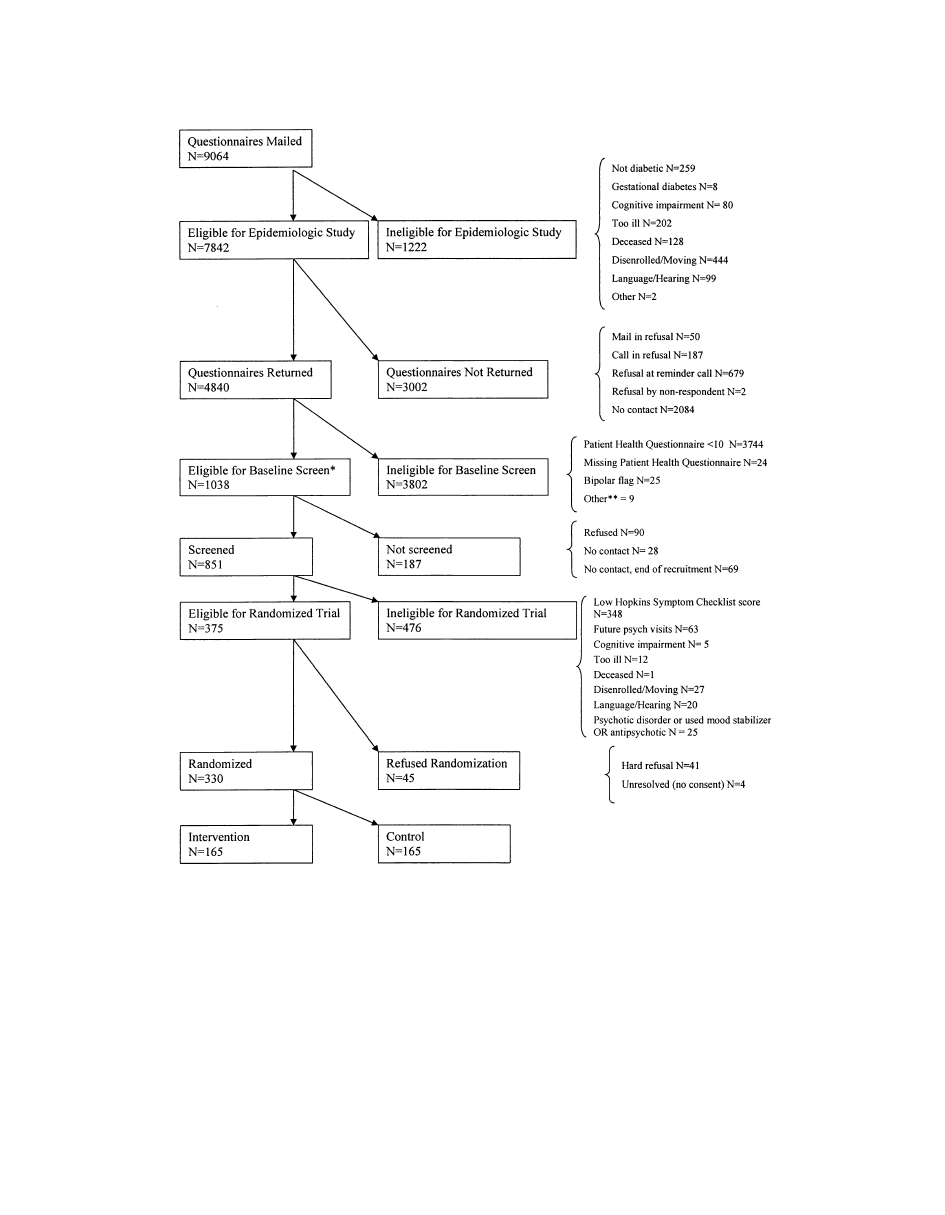
61.7%. Figure 1 describes the recruitment and reasons for
ineligibility or refusal at each phase of the study. The study
team has received permission from the Group Health Co-
operative Institutional Review Board to collect aggregate
data on nonrespondents to ascertain whether there are dif-
ferences in demographic (age, gender) or clinical variables
(health care costs, medical comorbidity, type of diabetes or
depression treatment, and HbA
1
C levels) between respon-
dents and nonrespondents.
A major methodological question was: “What is the best
depression screening tool to use?” Ideally this screen should be
brief, easy to score and provide both a DSM-IV diagnosis and
depression severity score. We elected to use the Patient Health
159
W.J. Katon et al. / General Hospital Psychiatry 25 (2003) 158 –168
Questionnaire (PHQ) based on this questionnaire’s ability to
provide both a dichotomous diagnosis of major depression as
well as a continuous severity score [17]. The PHQ diagnosis of
major depression has been found to have high agreement with
the diagnosis of major depression based on structure psychi-
atric interview [17]. Because we were also interested in the
DSM-IV diagnosis of dysthymia, which is not included in the
PHQ, we added questions from the NIMH Diagnostic Inter-
view Schedule [18] on dysthymia.
2.3. Methodology of the Pathways randomized controlled
trial
Patients were required to have a score of
ⱖ10 on the
initial PHQ in the mail screen, which has been found to be
the optimal cut-point in screening for major depression [17]
We required patients to have a second screen by telephone
about two weeks after scoring 10 or greater on the PHQ. On
this second screen, patients were required to have persistent
Fig. 1. Recruitment of epidemiologic study and randomized controlled trial.* Eligibility criteria: PHQ
⫽ 10 or greater.** Patients were categorized as
“Ineligible – Other” if: 1) they were enrolled in another study; 2) their spouse was enrolled in PATHWAYS; 3) they were high risk for self-harm or if they
refused a self-harm assessment; or 4) there were other special circumstances (i.e., – there was one case where the team deemed someone ineligible due to
a recent hospitalization for drug overdose).
160
W.J. Katon et al. / General Hospital Psychiatry 25 (2003) 158 –168

symptoms by having an SCL-20 depression [19] mean item
score of
ⱖ1.1. Double-screening eliminates those with tran-
sient or spontaneously resolving depression. A total of 348
patients were excluded based on an SCL
⬍1.1.
To recruit a representative sample, we had few medical
or psychiatric exclusions. We elected to include diabetics
who were already receiving antidepressant medication or
psychotherapy from nonpsychiatrist clinicians, but who still
had high depression scores. This decision was based on
prior findings that showed that many primary care patients
with depression are exposed to antidepressants at lower than
guideline-recommended dosage and duration [20]. Eligible
patients were ambulatory, English-speaking, with adequate
hearing to complete a telephone interview, and planned to
continue to be enrolled in GHC over the next year. Psychi-
atric exclusions were: 1) currently in care by, or scheduled
to see, a psychiatrist; 2) a diagnosis based on Group
Health’s automated diagnostic data of bipolar disorder or
schizophrenia; 3) use of antipsychotic or mood stabilizer
medication based on Group Health’s automated pharmacy
in the prior year; and 4) mental confusion on the interview
suggesting significant dementia (Fig. 1).
2.4. Randomization
After completion of the baseline telephone interview and
verbal informed consent, participants were informed that
they would be randomly assigned to the Intervention or
Usual Care group through a computer generated number.
Patients were told that if they were assigned to the Inter-
vention group a nurse would call them within one week to
set up an appointment. If they were assigned to the Usual
Care group they would receive a mailed written informed
consent for telephone follow-up calls and HbA
1
C blood
draws to sign and mail back, and the first telephone survey
call in three months.
After the baseline telephone call, the research assistant
handed a face sheet with a study identification number to the
project coordinator to put in an Access data base. The
Access data base then automatically generated a random
assignment number which indicated whether patients were
in the Intervention or Usual Care group. Randomization
allocation occurred in blocks of eight. For those patients in
the intervention group, the computer generated a face sheet
with a patient name and phone number that the project
coordinator delivered to the nurses. For both Intervention
and Usual Care patients the computer then added the patient
identification data to the telephone survey data base with the
specific dates for the series of follow-up interviews.
2.5. Intervention design
The intervention was an individualized, stepped care
depression treatment program provided by a Depression
Clinical Specialist (DCS) nurse in collaboration with the
primary care physician. This intervention design was based
on the intervention developed for the IMPACT Study,
which randomized 1801 elderly primary care depressed
patients to a nurse collaborative intervention or usual care
[21]. A key design question for the team was: “Would this
intervention be designed to enhance treatment of depression
only, or to improve quality of care for both depression and
diabetes?” We elected to design an intervention to improve
quality of care and outcomes of depression but to not di-
rectly intervene to improve diabetes education or care, ex-
cept to the extent that addressing diabetes care issues arose
in the context of treating depression. An example of a
diabetes issue that could have been addressed in problem
solving therapy would be if the patient chose lack of exer-
cise or having problems with diet as a problem she or he
wanted to work on. By improving depression care, we could
then test effects of improved depression outcomes on dia-
betes self-care (diet, exercise, medication adherence), and
glycemic control.
Efficacy studies often ask questions such as “Is this
antidepressant more effective than placebo?” The health
services question for this effectiveness study was: “Is an
innovative method to improve service delivery that provides
guideline level antidepressant treatment or brief psychother-
apy more effective than usual care?” In developing this
intervention, we tried to optimize patient recruitment and
retention by providing an initial choice based on patient
preference of either antidepressant medication or problem
solving therapy (PST). It is controversial whether providing
patient choice of treatment leads to better outcomes, [22]
but choice is more like “real world” treatment decisions that
physicians and patients negotiate. We expected choice to
enhance recruitment and retention of patients. Choice of
treatment is also consistent with the Institute of Medicine’s
emphasis on understanding patients’ beliefs and preferences
in negotiating a treatment plan [23]. Problem solving ther-
apy was chosen because it is patient-centered, brief and
well-accepted by primary care patients due to its psycho-
educational content. Problem solving therapy has been
found to be as effective in randomized trials in primary care
as antidepressants in improving depressive symptoms of
patients with major depression [24]. It was also easier to
train Depression Care Specialists in providing PST than
other forms of psychotherapy.
2.6. What type of professional should be trained as a
Depression Care Specialist (DCS)?
Given the need for the DCS to be proficient in medica-
tion management and PST, to have experience working with
patients with one or more chronic medical illnesses, and to
be comfortable working in a primary care setting, we chose
registered nurses to implement collaborative care treatment.
Registered nurses at GHC were already providing disease
management for diabetes and congestive heart failure.
Therefore, this model would have a greater chance to be
161
W.J. Katon et al. / General Hospital Psychiatry 25 (2003) 158 –168

integrated into the GHC plans for improving disease man-
agement of depression after the study.
We also required a registered nurse (R.N.) degree, not a
nurse practitioner (ARNP), since primary care physicians
would continue to prescribe and this level of training is
more generalizable and cost-effective.
We hired three half-time registered nurses. They each
covered two to four primary care clinics, that were geo-
graphically as far as 25 miles apart, with case loads of 40 to
65 patients each once the study was fully underway.
2.7. Training
Nurses received an initial one-week training course on
diagnosis and pharmacotherapy and an introduction to prob-
lem solving treatment methods. A psychiatrist, primary care
physician and psychologist participated in training. An in-
tervention manual from the IMPACT trial [25] was used to
train nurses on collaborative care, stepped care principles,
pharmacology and problem solving approaches.
Nurses were also trained using the manual for PST-PC
[26] during a training period following the protocol de-
scribed by Hegel and colleagues [27]. Formal training in-
cluded didactics, role play, observation of a videotaped
demonstration, and review of the treatment manual. Each
nurse was required to treat at least 4 depressed patients with
6 sessions of PST-PC over a 2-month period. Each session
was audiotaped, and sessions 1, 3 and 5 were rated using
Hegel’s PST Adherence and Competency Rating Scale [27].
Nurses were required to meet the criteria of at least 3 tapes
from each of two different patients’ audiotaped treatment
sessions being rated satisfactory by the team psychologist
(Dr. Ludman). During the training period, the nurses met
weekly with the psychologist for review of the audiotaped
sessions. During the course of the study, the nurses met
regularly with the psychologist to review audiotapes and
specific clinical problems arising in PST sessions. Group
supervision sessions were held weekly or twice a month for
the first months of the study, reducing in frequency over
time. During the second year, group supervision occurred
monthly. Individual PST-PC supervision sessions with
nurses occurred on an as-needed basis for review of difficult
sessions.
2.8. Collaborative care
A team of clinicians delivered the treatment for interven-
tion patients. Nurses carried out the majority of treatment
that included an initial one hour visit followed by twice a
month, half-hour appointments (telephone and in-person) in
the acute phase of treatment (0 to 12 weeks). The first
appointment included a semistructured biopsychosocial his-
tory, patient education, development of the therapeutic al-
liance, understanding the patient explanatory model of ill-
ness and negotiation whether to start treatment with an
antidepressant medication or problem solving therapy. Each
nurse had supervision twice a month with a team of a
psychiatrist, psychologist (on PST) and family physician to
review new cases and patient progress. Nurses interacted
regularly (via written notes and verbally) with the primary
care physician treating the patient. On alternative weeks,
nurses reviewed cases by telephone with the psychiatrist
supervisor. The psychiatrist supervisor regularly reviewed
choices and dosages of medication and clinical response,
and recommended changes, which the nurse discussed with
the primary care physician and patient.
A unique clinical monitoring system was developed us-
ing Pendragon software [28] for a hand-held organizer for
the nurses to enter tracking data after each patient contact
including initial PHQ score, initial date of intake, last date
seen and last PHQ score, whether the patient has had a 50%
decrease in PHQ score by 12 weeks, initial treatment (PST
or antidepressants), current treatment and number of outpa-
tient and telephone contacts. This monitoring system al-
lowed nurses and supervisors to easily check which patients
were due for telephone or in-person follow-up visits. Each
week these data were transferred to an Access file and an
updated printout of all cases was used in weekly supervi-
sion. This facilitated each supervisor’s review of the process
and outcomes of care for the large number of cases being
managed.
The printout included an asterisk for cases that had not
decreased 50% or more on the PHQ at 10 weeks. Supervi-
sion started on new cases, progressed to asterisked cases and
then to cases in initial phases of treatment.
2.9. Stepped care algorithm
A stepped care approach was used in which different
patients received different intensity of services based on
their observed outcome (Table 1). Stepped care recognizes
that patients have marked differences in psychiatric and
medical comorbidity as well as differences in response to
antidepressant medication and/or psychotherapy [29]. In the
Pathways trial if patients still had persistent depressive
symptoms (
⬍50% decrease in severity based on the PHQ)
10 to12 weeks after Step 1 level treatment with either PST
or antidepressant medication, they could either: a) switch to
a second antidepressant with a different mechanism or side-
effect profile; b) switch to the alternative treatment (from
PST to medication or vice versa); or c) receive augmenta-
tion of PST or antidepressant medication with the first
treatment they had received. This change in treatment at 10
to 12 weeks was labeled Step 2 care. Another option in Step
2 was a psychiatric consultation to evaluate treatment op-
tions. For patients who received one or more Step 2 inter-
ventions, persistent symptoms (
⬍50% improvement) and
lack of patient and clinician satisfaction with outcome after
a second treatment (8 to 12 weeks) could lead to referral to
the Group Health Cooperative (GHC) mental health system
for longer term follow-up including management by a psy-
chiatrist (Step 3).
162
W.J. Katon et al. / General Hospital Psychiatry 25 (2003) 158 –168

Step 1 included history taking and building the therapeu-
tic alliance, patient choice of initial treatment and behav-
ioral activation. In addition, the depression clinical special-
ist introduced the PHQ depression module as the key
monitoring tool for measuring response to treatment and set
up a schedule of telephone and in-person sessions. Regular
communication occurred with the primary care physician
(PCP). The goal of the intervention was clinical recovery
(
ⱖ50% decrease in PHQ score) and, if possible, remission
(a score of
⬍5 on PHQ) [17] and restoration of social and
vocational function. Once patients reached a significant
decrease in clinical symptoms, the nurse began continuation
phase treatment that involved monthly scheduled telephone
contacts. Nurses also set up optional continuation groups,
which involved a monthly group visit for patients with
persistent symptoms or social isolation instead of the
monthly telephone calls.
2.10. Usual care
Patients were informed prior to randomization that they
were eligible for a new program to help people with diabe-
tes better manage stress and depression. Patients were told
they would be called by the DCS within 10 days if they
were randomized to the intervention. It was also recom-
mended that whether or not they were chosen to receive the
additional services, they should work with their primary
care physician on these clinical issues.
In most cases, usual care for depression provided by
Group Health Cooperative family physicians involves a
prescription of an antidepressant medication, 2 visits over
the first 3 months of treatment and an option to refer to
Group Health Cooperative mental health services. Both
intervention and usual care patients could also self-refer to
a GHC mental health provider. We tracked and will report
these out-of-study mental health referrals and visits. Usual
care for diabetes in Group Health Cooperative is provided
by the primary care physician with occasional support from
diabetes nurses for patients with persistently high HbA
1
C
levels.
2.11. Evaluation
Given that patients entering the trial had evidence of at
least two medical illnesses, i.e., major depression and/or
dysthymia and diabetes mellitus, and that our intervention
was aimed primarily at improvement of depression, the
primary outcome variable was change in depressive symp-
toms. Changes in functioning were identified as important
secondary outcomes. Inherent in this discussion and the
focus of the intervention on depression was that if we
significantly improved depressive symptom and functional
outcomes, this would be considered a positive trial. We also
hypothesized that if the intervention significantly improved
depressive symptoms, we would find improvement on the
diabetes measures, including diabetes symptom burden, di-
Table 1
Stepped care intervention
Step 1: 0–12 weeks
History taking and building therapeutic alliance
Behavior activation based on increasing positive activities
Problem-solving therapy (PST) or antidepressant medication (patient choice)
Introduction of Patient Health Questionnaire (PHQ) as weekly measure of depressive symptoms
Schedule telephone and in-person follow-ups by Depression Clinical Specialist (DCS)
Regular communication with primary care physician
No Response
Recovery (
ⱖ50% decrease in PHQ OR
Step 2: 12 to 24 weeks
Remission (PHQ of
⬍5)
For patients who had not decreased by at least 50% on the initial PHQ
score and/or were dissatisfied with outcome, the DCS could:
Schedule monthly continuation telephone follow-up
a) switch to an alternative antidepressant medication if no or little
response to first medication
b) add an antidepressant if the patient had not responded to PST or add
PST if little or no response to antidepressant
c) augment with a second antidepressant if partial response to first
d) schedule a psychiatric consultation
Less than 50% Response Based on PHQ
Recovery or Remission
Step 3: 24–52 weeks
Schedule monthly continuation telephone follow-up
If patient has not had decrease by 50% in PHQ or remission:
a) consider referral to Group Health mental health service for longer-
term mental health care;
b) enter patient into DCS continuation/ maintenance phase group.
,
n
,
n
163
W.J. Katon et al. / General Hospital Psychiatry 25 (2003) 158 –168

abetes control and some measures of diabetes self-care
(particularly exercise and diet). The study was adequately
powered to detect a moderate-to-large effect on HbA
1
C. We
also planned a cost-effectiveness analysis (see below).
After randomization, telephone interviews were provided
at 3, 6, 12 and 24 months. Telephone interviews were
completed by interviewers blind to intervention status.
For measuring change in depression, the SCL-20 depres-
sion scale [19] was chosen to be the primary dependent
variable to measure change in affective symptoms based on
previous studies showing it to be sensitive to change
[30,31]. We used the PHQ at baseline, 6, 12 and 24 months
to measure changes in dichotomous diagnosis of major
depression as well as remission status (PHQ
⬍ 5) [17].
We utilized selected scales from the WHO-DAS-II
(Household and Work-Related Activities, Community and
Family Activities, Physical Health, Work Absenteeism and
Cut-Down days, Work Productivity) [32] and SF-36 (Gen-
eral Health, Social Role, Impairment, Emotional Role Im-
pairment) [33] to measure selected domains of function.
These scales were chosen because they are complementary
and responsive to change in depression status. The SF-36
does not capture all functional domains hypothesized to
improve with increased quality of depression care, while the
WHO-DAS-II has not been used in prior randomized trials.
We utilized well-validated, reliable scales to measure
diabetes symptom burden (9 items) [34], diabetes self-effi-
cacy (7 items) [35], and diabetes self-care activities (12
items) [36]. We selected these three scales because they
were shown to have a high correlation with severity of
depression in a prior epidemiologic study [7]. The Diabetes
Symptom Burden Scale inquires about 9 symptoms in the
last month, such as abnormal thirst, and codes the answer on
a Likert Scale of 1 (never) to 5 (qd) [34]. The Diabetes
Self-Efficacy Scale inquires about 7 items, such as how
much control over diabetes the patient believes she or he
has, on a 1 (none at all) to 5 (total control) Likert Scale [35].
The Diabetes Self-Care Activity Scale asks patients to eval-
uate how many of the last 7 days they have followed an
exercise or diet program, checked on their blood sugar level
and completed a foot check. Each answer is coded on a 0
(no days) to 7 (days) Likert Scale [36].
Enrolled patients were asked to agree to blood draws to
measure HbA
1
C at baseline, 6,12 and 24 months and were
reimbursed $25 for their time for each test. Virtually all
enrolled patients were willing to participate in the blood
draws. HbA
1
C measures exposure of red blood cells to
glucose over a 120-day period, and diabetes guidelines
recommend that primary care physicians order this test
twice a year [3]. Lowering HbA
1
C levels has been targeted
in patients with diabetes as a key mechanism to decrease
medical sequelae of poor diabetes control. The Diabetes
Complications and Control Trial demonstrated that inter-
ventions that significantly lowered HbA
1
C levels in patients
with diabetes decreased important medical complications
[37]. Operationally, we required a new HbA
1
C on patients
who had not had one within 14 days of each study scheduled
HbA
1
C.
Group Health’s computerized pharmacy and utilization
records were used to measure adherence to antidepressant
medication, oral hypoglycemic medications as well as am-
bulatory visits and tests and inpatient hospital days and
medical costs. The computerized pharmacy records allowed
examination of refills of antidepressant medications and
whether the patient received an adequate dosage based on
evidence-based guideline standards for 90 days or more
within each 6-month period of time. A recently developed
algorithm for oral hypoglycemic refills also allows measure-
ment of whether or not the patient was overdue in refilling
his or her prescription by 15 or more days and by more than
25% of the intended duration of use [7]. Prior research has
shown that depression is associated with significant gaps in
refills of oral hypoglycemics [7].
Computerized pharmacy records will also be used to
compute a revised chronic disease score (Rx Risk), a mea-
sure of chronic comorbidity based on prescription drug use
over the previous 6 months [38]. After review of the liter-
ature and consultation with diabetes consultants, a diabetes
severity score was developed based on the patient’s self-
rating of the number of complications of diabetes (neurop-
athy, nephropathy, retinopathy and myocardial infarction)
[39] the patient has had, whether the patient’s initial diabe-
tes medication was insulin or an oral hypoglycemic, and the
length of time he or she had diabetes. Both the chronic
disease score and diabetes severity score will be used as
covariates in assessing intervention versus usual care out-
comes. Patients were defined as having Type 1 diabetes
based on an age of onset less than age 30 and on insulin
being their first and current treatment.
Computerized health plan data will be used to identify all
health plan services provided or paid for by Group Health
Cooperative during the 12- and 24-month periods after
randomization (inpatient and outpatient services for mental
health or general medical care). All outpatient and inpatient
services provided by Group Health Cooperative are as-
signed costs based on health plan accounting records (in-
cluding actual personnel, supply and overhead costs). Ser-
vices purchased by GHC from external providers are
assigned costs equal to the amount reimbursed by Group
Health Cooperative for that type of care.
2.12. Data analysis
The study was powered using three different hypothe-
sized differences between Intervention and Usual Care pa-
tients including depressive symptoms, function and HbA
1
C
levels. Based on previous studies in which interventions and
controls had a 0.31 difference on the SCL-20 at 6 months
with a standard deviation for the SCL-20 of 0.7 (an effect
size of approximately 0.4), the study design had 80% power
to detect a 0.23 difference between groups, assuming ran-
domization of 300 patients and 85% patient retention in the
164
W.J. Katon et al. / General Hospital Psychiatry 25 (2003) 158 –168

study at 12 months. Based on previous primary care depres-
sion studies we expected both the SF-36 Social Role Func-
tioning and Emotional Role Functioning Scales to have a
standard deviation of 30. Based on the sample size of 300
and 85% retention, we calculated that we would have 80%
power to detect a 10-point difference in SF-Social or Emo-
tion Role Function scores, which is considered clinically
significant. Based on a recent study of depression and dia-
betes in primary care [7] we assumed a standard deviation
of HbA
1
C levels of 1.65 and a correlation between baseline
and follow-up levels of 0.6 (our actual estimates are
⬎0.7).
With a sample size of 145 in each group we will have 82.2%
power to detect a 0.5 difference between Intervention and
Controls. Given that we expect an 85% follow-up rate at 12
months, we projected needing 162 per group or a total
sample size of 324 to be able to detect a HbA
1
C difference
of 0.5.
The analyses of outcome differences between interven-
tion and control patients will follow an intent-to-treat ap-
proach. We will use random regression models to estimate
effects of the intervention relative to usual care, on the
primary dependent variables: depressive symptoms (contin-
uous SCL-20 outcomes as well as percent achieving recov-
ery based on
ⱖ50% decrease on SCL-20 and the patient
achieving remission based on a score of
⬍5 on PHQ or
⬍0.5 on SCL) and function (WHO-DAS and SF-36 sub-
scales). We will test two interaction terms in the model to
examine possible differences in intervention effects: out-
comes for insulin-dependent versus noninsulin-dependent
diabetics and outcomes for patients with HbA
1
C levels less
than and greater than guideline recommended levels. Pre-
vious studies suggest that depression may have a greater
impact on HbA
1
C levels in insulin-dependent diabetic pa-
tients [40] and change in depression should have the most
benefit in patients with high HbA
1
C levels. We will also use
random regression models to compare intervention versus
usual care effects on important secondary outcomes: diabe-
tes symptom burden, diabetes self-efficacy, diabetes self-
care, and HbA
1
C. In these models, we will adjust for dif-
ferences in patient demographics and clinical characteristics
across intervention and control patients.
2.13. Health care costs and cost effectiveness
We will follow patient costs over a 2-year period after
randomization (the initial patient was randomized on 4/27/
2001 and the last patient was randomized on 5/8/02), Pre-
vious data on health care costs in patients with depression
and diabetes for a 6-month period were estimated at $3,654
⫾ $4,258 in patients with depression and $2,094 ⫾ $3,052
in patients without depression [7]. Methodologic issues ad-
dressed by the skewed distribution of heath care costs in-
clude: using two-part models [41] which first uses logistic
regression to compare the percent of patients utilizing any
health care services. Linear regression techniques are then
used to compare health care costs among users of services.
Methods to correct for possible heteroscedasticity in cost
data such as “smearing” techniques [42] or gamma regres-
sion may be utilized [43]. The randomized trial will have
adequate power to detect a $1,000 reduction in ambulatory
costs per year from a projected base of $5,000 per year. This
reduction is greater than what we expect to observe in the
intervention group. However, descriptive trends in health
care costs in intervention and control groups may be im-
portant. If depression and/or diabetes outcomes were im-
proved without evidence of increased health care costs be-
tween intervention and usual care groups, this would be of
interest. We plan to attempt to obtain a better understanding
of the effect of the interventions on inpatient hospitalization
in two analyses. After controlling for age, gender, chronic
disease score and diabetes severity, we will examine the
effect of the intervention on the number of hospitalizations
using a negative binominal regression model. We will also
examine the effect of the intervention on time to first hos-
pitalization in the first year period using survival models.
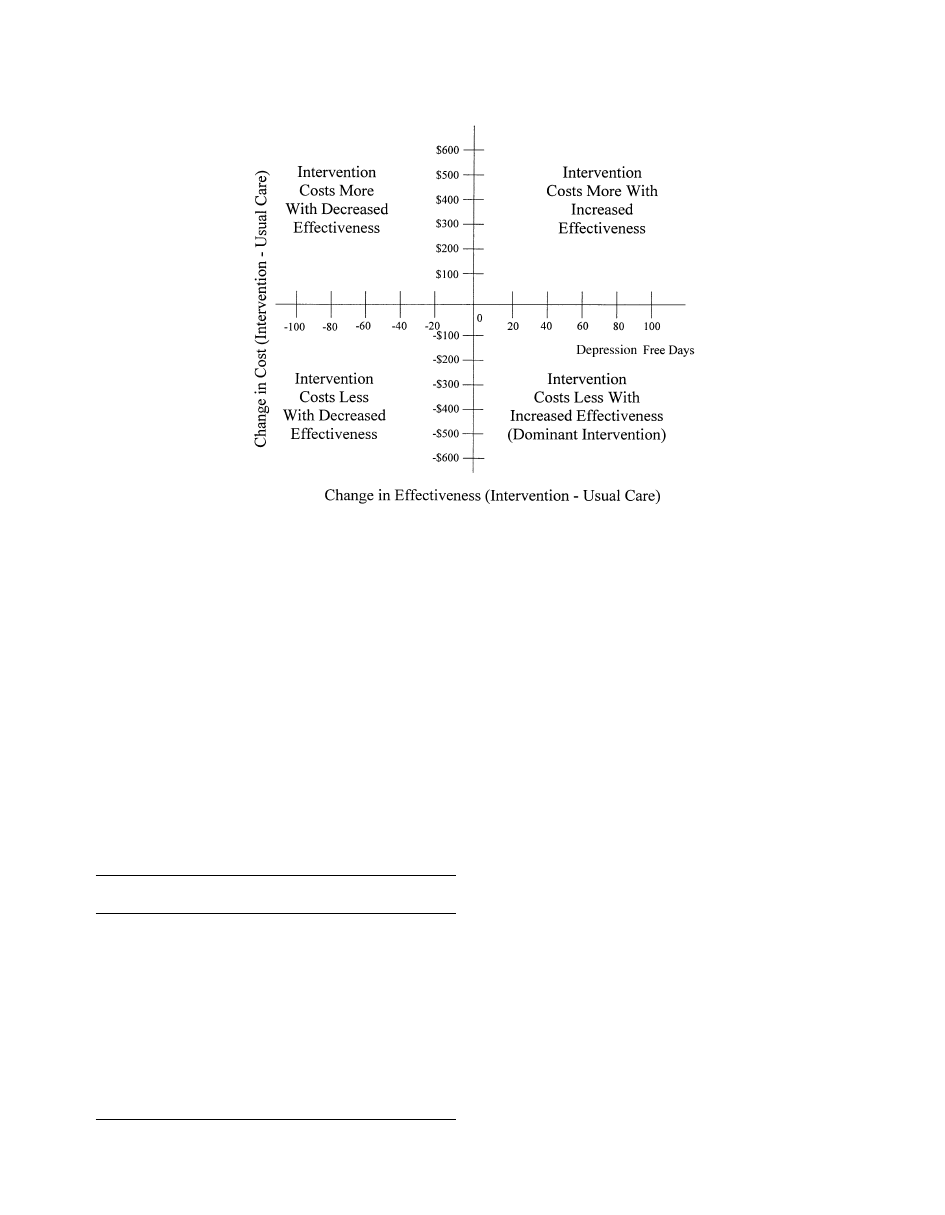
Costs and effectiveness of the intervention will be com-
pared with incremental cost-effectiveness ratios following
guidelines developed by Gold and colleagues [44]. We will
take a societal perspective and, in the numerator, will esti-
mate the one-year differences in total ambulatory costs and
time off work due to medical or mental health visits. In the
denominator we will use the method by Lave et al. [45] to
estimate differences in depression free days between inter-
vention and control patients over a 12-month period. Boot-
strap resampling with 1,000 draws using bias correction will
be used to estimate confidence intervals for both incremen-
tal cost measures and depression-free days and the ratio of
incremental costs to incremental depression-free days [46].
The bootstrap method will allow us to document the prob-
ability of this intervention being in each of the four quad-
rants in Fig. 2. Most new interventions are in the upper left
quadrant (costs more, but more effective), however, there is
also a possibility that, if improved depression care is asso-
ciated with improved diabetes care, there may be savings in
medical costs that partially or completely make-up for in-
creased depression costs inherent in the collaborative care
model. Because depression costs are mostly increased in the
first 6 months and medical cost savings may be delayed, we
will carry out follow-ups over a 2-year period.
3. Results
Upon completing enrollment, 330 primary care patients
with diabetes were randomized to the intervention or usual
care conditions. Table 2 presents demographic and clinical
characteristics of the randomized subjects. Approximately
23% of subjects are of minority ethnicity which is higher
that the rates in the Group Health system. This is because of
selecting clinics with high minority rates and the higher
percentage of non-Caucasians with diabetes. A substantial
number of patients have comorbid medical disorders in
165
W.J. Katon et al. / General Hospital Psychiatry 25 (2003) 158 –168
addition to diabetes and are from low socioeconomic status
both of which have been found to be risk factors for poor
depression outcomes [47,48].
The importance of choice in treatment was shown by the
exposure to prior treatment and the actual choices patients
initially made for treatment. Of the 165 patients randomized
to the collaborative care intervention, 48 (29.0%) initiated
treatment with PST only, 65 (39.4%) initiated treatment
with medication only, 48 (29.0%) initiated treatment with
PST and medication (because they were already on an
antidepressant, but still had significant depressive symp-
toms based on a screening PHQ score of
ⱖ10 and baseline
SCL of
ⱖ1.1), and only 4 (2.4%) never initiated treatment.
4. Discussion
The Pathways project has demonstrated the feasibility of
recruiting a population-based primary care sample of pa-
tients with diabetes and depression for an epidemiologic
study and a randomized controlled trial. The mail survey
coupled with telephone reminder calls successfully screened
61.7% of the population. We will be able to compare non-
respondents to respondents on multiple variables in the
GHC database (i.e., prior utilization and costs, medical
comorbidity, HbA
1
C levels) to ascertain respondent bias.
The Pathways intervention offers patients and providers
the necessary resources to increase the use of evidence-
based depression treatments. The nurse collaborative care
model exemplifies a system of care that both supports the
primary care delivery system and provides patient-centered
care. This intervention was modeled from the IMPACT
study where patients in the intervention arm were signifi-
cantly more satisfied with care over the first 3 months than
those treated in usual care [49]. The provision of choice of
treatments may have helped with speed of recruitment and
retention. Many patients had negative feelings about one of
the two treatments. For instance, some patient stated they
were already on multiple medications and wouldn’t take
another, whereas others were not interested in counseling
but agreed to try a medication. Choice mirrors how patients
and providers work together in “real world” systems and
should provide more realistic estimates of the feasibility and
effectiveness of such treatments in primary care.
The stepped care model is more complex than most
treatment protocols and targets scarce mental health re-
Fig. 2. Incremental cost effectiveness quandrant
Table 2
Demographics and clinical characteristics of patients with diabetes and
depression
Intervention
N
⫽ 165
Control
N
⫽ 165
Age (mean
⫾ SD)
58.6
⫾ 11.8
58.1
⫾ 12.0
% Female
64.7%
64.7%
% 1 year of college
80.0%
77.6%
% White
75.3%
81.1%
% Employed full- or part-time
53.9%
45.2%
SCL-depression (mean
⫾ SD)
34.15
⫾ 10.2
32.5
⫾ 9.1
% Lifetime dysthymia
67.7%
70.3%
% Major depression
62.8%
69.1%
% Current panic disorder
9.6%
11.9%
Years with diabetes (mean
⫾ SD)
9.6
⫾ 8.7
10.2
⫾ 10.1
Total diabetes symptoms (0–10)
(mean
⫾ SD)
4.6
⫾ 2.6
4.7
⫾ 2.3
HbA
1
C (mean
⫾ SD)
8.1
⫾ 1.6
8.0
⫾ 1.5
166
W.J. Katon et al. / General Hospital Psychiatry 25 (2003) 158 –168

sources to patients with the most persistent symptoms. This
is not a trial of PST versus medication versus usual care;
instead it is a trial of a health services intervention that
provides a choice of evidence-based depression treatments
versus usual care. We will not be able to analyze which
components of this multifaceted intervention are most im-
portant in improving outcomes; however, reviews of
chronic disease interventions that have successfully im-
proved patient-level outcomes have shown that interven-
tions aimed at multiple levels of care, including the patient,
physician and process of care are most effective [50].
Acknowledgments
Supported by grants #MH 4 –1739 and #MH 016473
from the National Institute of Mental Health Services Di-
vision, Bethesda, MD (Dr. Katon).
References
[1] Chipkin SR, Gottlieb P, Bogorad DD, Parker F. Diabetes mellitus. In:
Noble J, editor. Textbook of primary care medicine. 2
nd
ed. St. Louis,
Mosby-Yearbook, 1996, p. 476 – 498.
[2] Lustman P, Clouse R, Freedland K. Management of major depression
in adults with diabetes: implications of recent trials. Sem Clin Neu-
ropsych 1998;3:102–114.
[3] Centers for Disease Control and Prevention. National diabetes aware-
ness month, Nov 1997, MMWR, Morb Mortal Wkly Rep 46:1013,
1997.
[4] American Diabetes Association, Direct and indirect costs of diabetes
in the United States in 1992, Alexandria, VA, 1992.
[5] Gavard JA, Lustman PJ, Clouse PE. Prevalence of depression in
adults with diabetes. An epidemiologic evaluation. Diabetes Care
1992;16:1167–78.
[6] de Groot M, Anderson R, Freedland K, et al. Association of depres-
sion and diabetes complications: meta-analysis. Psychosom Med
2001;63:619 –30.
[7] Anderson R, Freedland K, Clouse R, Lustman P. Prevalence of
comorbid depression in adults with diabetes. A meta-analysis. Dia-
betes Care 2001;24:1069 –78.
[8] Lustman PJ, Anderson R, Freedland K, et al. Depression and poor
glycemic control: a meta-analytic review of the literature. Diabetes
Care 2000;23:934 – 42.
[9] Winokur A, Maislin G, Phillips J, Amsterdam J. Insulin resistance
after glucose tolerance testing in patients with major depression. Am J
Psychiatry 1988;145:325–30.
[10] DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor
for noncompliance with medical treatment: Meta-analysis of the ef-
fects of anxiety and depression on patient adherence. Arch Intern Med
2000;160:2101–7.
[11] Lustman PJ, Griffith LS, Clouse RE, et al. Effects of nortriptyline on
depression and glucose utilization in diabetes: results of a double-
blind placebo controlled trial. Psychosom Med 1997;59:241–50.
[12] Lustman PJ, Freedland KE, Griffith LS, Clouse RE. Fluoxetine for
depression in diabetes: a randomized double-blind placebo-controlled
trial. Diabetes Care 2000;23:618 –23.
[13] Lustman PJ, Griffith LS, Freedland KE, et al. Cognitive behavior
therapy for depression in type 2 diabetes mellitus: a randomized
controlled trial. Ann Intern Med 1998;129:613–21.
[14] Von Korff M, Gruman J, Schaefer J, et al. Collaborative management
of chronic illness. Ann Intern Med 1997;127:1097–1102.
[15] McCulloch D, Price M, Hindmarsh M, Wagner E. A population-
based approach to diabetes management in a primary care setting:
early results and lessons learned. Eff Clin Pract 1998;1:12–22.
[16] Walker E, Unutzer J, Rutter C, et al. Costs of health care use by
women HMO members with a history of childhood abuse and neglect.
Arch Gen Psychiatry 1999;56:609 –13.
[17] Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief
depression severity measure. J Gen Intern Med 2001;16:606 –13.
[18] Robins L, Helzer J. Diagnostic interview schedule (DIS): version
III-A. St Louis, MO, Washington University School of Medicine,
1985.
[19] Derogatis L, Rickels K, Uhlenhuth E, Coui C. The Hopkins Symptom
Checklist: a measure of primary symptom dimensions. In: Pichot
(editor), Psychological measurement in psychopharmacology: prob-
lems in psychopharmacology. Basel, Switzerland: Kargerman, 1974,
p. 79 –110.
[20] Simon G. Evidence review: efficacy and effectiveness of antidepres-
sant treatment in primary care. Gen Hosp Psychiatry 2002;24:213–24.
[21] Unu¨tzer J, Katon W, Williams J Jr, et al. Improving primary care for
depression in late life: the design of a multicenter randomized trial.
Med Care 2001;39:785–99.
[22] Ward E, King M, Lloyd M, et al. Randomized trial of nondirected
counseling, cognitive-behavioral therapy, and usual general practitio-
ner care for patients with depression. clinical effectiveness. BMJ
2000;321:1383– 88.
[23] Institute of Medicine. Crossing the quality chasm: a new health
system for the 21st century. Washington, D.C., National Academy
Press, 2001.
[24] Mynors-Wallis L, Gath D, Lloyd-Thomas A, Tomlinson D. Random-
ized controlled trial comparing problem solving treatment with ami-
triptyline and placebo for major depression in primary care. BMJ
1995;310:441–5.
[25] Unu¨tzer J. The IMPACT study investigators: IMPACT intervention
manual. Los Angeles, CA, Center for Health Services Research,
UCLA Neuropsychiatric Institute, 1999.
[26] Hegel MT, Barrett JE, Oxman TE Problem-solving treatment for
primary care (PST-PC): A treatment manual for depression, Hanover
NH: Dartmouth University, 1999.
[27] Hegel MT, Barrett JE, Oxman TE. Training United States therapists
in problem-solving treatment of depressive disorders in primary care
(PST-PC): lessons learned from the treatment effectiveness project.
Families Systems Health 2000;18(4):423–35.
[28] Pendragon Forms, Version 3.2. Pendragon Software Corporation,
Libertyville, IL 60048. www.Pendragonsoftware.com.
[29] Katon W, Von Korff M, Lin E, Simon G. Rethinking practitioner
roles in chronic illness: the specialist, primary care physician, and the
practice nurse. Gen Hosp Psychiatry 2001;23:138 – 44.
[30] Katon W, Von Koff M, Lin E, et al. Collaborative management to
achieve treatment guidelines: impact on depression in primary care.
JAMA 1995;273:1026 –31.
[31] Katon W, Robinson P, Von Korff M, et al. A multi-faceted interven-
tion to improve treatment of depression in primary care. Arch Gen
Psychiatry 1996;53:924 –32.
[32] Epping-Jordan J, Chatterji S, Ustun T. The World Health Organiza-
tion. Disability assessment schedule II (WHO-DAS II) a tool for
measuring clinical outcomes. Presented at NIMH Health Services
Research Meeting. Washington, D.C., July 2000.
[33] Ware J, Sherbourne C. The MOS 36-item Short Form Health Survey
(SF-36). Med Care 1992;30:473– 83.
[34] Whitty P, Steen N, Eccles M, et al. A new completion outcome
measure for diabetes: is it responsive to change? Qual Life Res
1997;6:407–13.
[35] Carey MP, Jorgenson RS, Weinstock, et al. Reliability and validity of
the appraisal of diabetes scale. J Behav Med 1991;14:43-51.
[36] Toobert D, Hampson S, Glascow R. The summary of the Diabetes
Self-Care Activities Measure: results from 7 studies and a revised
scale. Diabetes Care 2000;23:943–50.
167
W.J. Katon et al. / General Hospital Psychiatry 25 (2003) 158 –168

[37] The DCCT Research Group. Influence of intensive diabetes treatment
on quality-of-life outcomes in the Diabetes Control and Complica-
tions Trial. Diabetes Care 1996;19:195–203.
[38] Fishman P, Goodman M, Hornbrook M. Risk adjustment using auto-
mated pharmacy data: the Rx Risk Model. Med Care 2003;41:84 –99.
[39] Jacobson A, de Grout M, Samson J. The effects of psychiatric dis-
orders and symptoms on quality of life in patients with type 1 and
type 2 diabetes mellitus. Qual Life Res 1997;6:11–20.
[40] Ciechanowski P, Katon W, Russo J, Hirsch I. The relationship of
depressive symptoms to symptom reporting, self-care and glucose
control in diabetes. Gen Hosp Psychatry (In Press).
[41] Diehr R, Yanez D, Ash A, et al. Methods for analyzing health care
utilization and costs. Ann Rev Public Health 1999;20:125–144.
[42] Duan N. Smearing estimate: a nonparametric retransformation
method. J Am Statistical Assoc 1983;78:605–10.
[43] Manning WG. The logged dependent variable, heteroscedasticity, and
the retransformation problem. J Health Econ 1998;17:283–95.
[44] Gold M, Siegel J, Russel L, et al. Cost-Effectiveness in Health and
Medicine. New York, NY, Oxford University Press, 1996.
[45] Lave J, Frank R, Schulberg H, Kamlet M. Cost-effectiveness of
treatments for major depression in primary care practice. Arch Gen
Psychiatry 1998;55:645–51.
[46] O’Brien B, Drummond M, Labelle R, Williams A. In search of
power and significance: issues in the design and analysis of sto-
chastic cost-effectiveness studies in health care. Med Care 1994;
32:150 – 63.
[47] Weich S, Churchill R, Lewis G, et al. Do socioeconomic factors
predict the incidence and maintenance of psychiatric disorders in
primary care. Psychol Med 1997;27:73– 80.
[48] Cole M, Bellavance F, Mansour A. Prognosis of depression in elderly
community and primary care populations: a systematic review and
meta-analysis. Am J Psychiatry 1999;156:1182–9.
[49] Unu¨tzer J, Katon W, Williams J Jr, et al. The IMPACT trial: collab-
orative care management improves treatment and outcomes of late-
life depression. JAMA 2002;288:2836 – 45.
[50] Haynes R, McDonald H, Garg A, Montague P. Interventions for
helping patients to follow prescriptions for medications. Cochrane
Database Syst Rev 2002;(2):CD00011.
168
W.J. Katon et al. / General Hospital Psychiatry 25 (2003) 158 –168
Document Outline
- Improving primary care treatment of depression among patients with diabetes mellitus: the design of the Pathways Study
- Introduction
- Methods
- Study setting
- Sample recruitment
- Methodology of the Pathways randomized controlled trial
- Randomization
- Intervention design
- What type of professional should be trained as a Depression Care Specialist (DCS)
- Training
- Collaborative care
- Stepped care algorithm
- Usual care
- Evaluation
- Data analysis
- Health care costs and cost effectiveness
- Results
- Discussion
- Acknowledgments
- References
Wyszukiwarka
Podobne podstrony:
Leczenie depresji - farmakologia, LECZENIE DEPRESJI:
cukrzyca, LECZENIE NIEFARMAKOLOGICZNE PACJENTÓW Z CUKRZYCĄ, LECZENIE NIEFARMAKOLOGICZNE PACJENTÓW Z
depresja w ciazy z leczeniem
Depresja zimowa epidemiologia, etiopatogeneza, objawy i metody leczenia
LECZENIE CUKRZYCY II
Stopa cukrzycowa rozpoznanie i leczenie mp pl
Standardy leczenia cukrzycy
LECZENIE DEPRESJI
FARMAKOLOGIA wykład 07, FARMAKOLOGIA wykład 7 (26 XI 01) LECZENIE CUKRZYCY cz
LECZENIE DEPRESJI
Światło spolaryzowane w leczeniu stopy cukrzycowej opis przypadku
Leki wspomagajce leczenie cukrzycy
leczenie otyłości i cukrzycy monograf 2009
Problemy leczenia dzieci z cukrzycą
Leczenie cukrzycy
Cukrzyca typu 2 leczenie
więcej podobnych podstron