The new European Union (EU) law on chemicals and their safe use, known as
REACH (Registration, Evaluation, Authorisation and Restriction of Chemicals), came
into effect on the 1
st
June 2007. The aims of this new law are to improve the
protection of human health and the environment from the risks that can be posed
by chemical substances, to promote alternative safety testing methods and to
improve the safe handling and use of substances across all sectors of industry.
A switch in responsibility
Prior to REACH, regulatory bodies were largely responsible for evaluating the risks posed
by chemicals and providing safety information on substances. Under the new EU law, that
responsibility now lies within industry.
Manufacturers and importers of chemicals must now collate information on the properties
of their chemical substances and register this information as of 1
st
June 2008 into a
central database managed by the European Chemicals Agency (ECHA), based in Helsinki.
Safety information about a registered chemical on the database can then be accessed by experts as well as the general public,
improving the safe handling and use of the substance. Furthermore, under this new system, manufacturers will be able to
check for what uses a particular substance has been registered as being safe, enabling them to replace any substances
recognised as being unsafe with a safer alternative.
Increased safety
As well as improving the protection of human health and the environment from the risks that can be posed by chemical
substances, and improving the safe handling and use of substances across all sectors of industry, the REACH regulations also
aim to promote alternative safety testing methods, stating that the development of alternatives should be prioritised in future
EU research. Once alternative testing methods which do not involve the use of animals have been validated, the REACH
regulations will be adapted to phase out animal testing as soon as possible.
Implications of REACH
In the EU, health and safety tests on chemicals did not become mandatory until 1981. As a consequence, under the new
REACH regulations, over 100,000 substances placed on the market prior to 1981 will have to be registered onto the new
database. Consequently, over the next 10 years thousands of preexisting and new chemicals will be registered by the ECHA
as the new REACH regulation is slowly phased in.
Companies that manufacture or import 1 tonne or more of any chemical substance per year, or who expect to do so over the
REACH timings should preregister the substance with the European Chemicals Agency (ECHA) between 1
st
June and 1
st
December 2008. Failure to meet this deadline means that they cannot continue producing or importing the substance until they
have submitted a full registration dossier. With preregistration, companies can benefit from staggered registration deadlines
depending on the substance and the tonnage (2010, 2013 or 2018).
REACH does not require that all chemicals be registered. The use of substances in some sectors of industry, such as the food
industry, have been exempted as they are already covered by other EU laws. For instance, food ingredients, which are already
covered by the EU General Food Law Regulation 178/2002, do not have to be registered under the new REACH legislation.
However, the use of other substances in the food industry such as in packaging and in cleaning materials does.
Measurement of impact
In time, the impact of REACH on the food industry sector will be evaluated by the European Food Safety Authority (EFSA), the
forefront of EU food safety risk assessment. It is possible that the initiation of REACH may result in a change in how risks in the
food industry are assessed at the European level.
Implications for consumers
For the consumer, the implications of the REACH system will develop gradually as more and more chemicals are phased into
the new law. It is hoped that the registration of substances and their safe use will reassure those consumers who may be
concerned about product safety, and that the replacement of chemicals with safer alternatives will improve the safety of both
human health and the environment.
References
1.
Food Quality News, News articles section
2.
European Commission, Chemicals section:
3.
European Chemicals Agency, Publications section
New European Union law REACH regulating the use of chemical substances
Physical activity is related to health and lifestyle status and should be part of
everyone’s daily routine. With growing rates of obesity and its associated health
problems, physical activity is now more important than ever.
It is well known that the amount and type of exercise that an individual takes part in plays
a significant role in health and weight. Excess body fat is harmful to the body in that it puts
more strain on the joints and surrounding tissues, and it increases the risk of certain
cancers (including bowel, breast and kidney cancer), diabetes and heart disease.
Consequently, those individuals who exercise regularly can not only maintain a healthier
weight but also reduce their risk of developing chronic diseases and have healthier bones
and joints.
Healthy body weight
Body weight can be categorised into underweight, normal, overweight or obese based on
the Body Mass Index (BMI). The BMI is calculated by dividing body weight (kg) by the
square of body height (m
2
). For example, an individual who is 1.82 m tall and weighs 75
kg will have a BMI of 75/(1.82)
2
= 22.64 kg/m
2
. This figure is then used to assess where
the individual sits on a scale of body sizes.
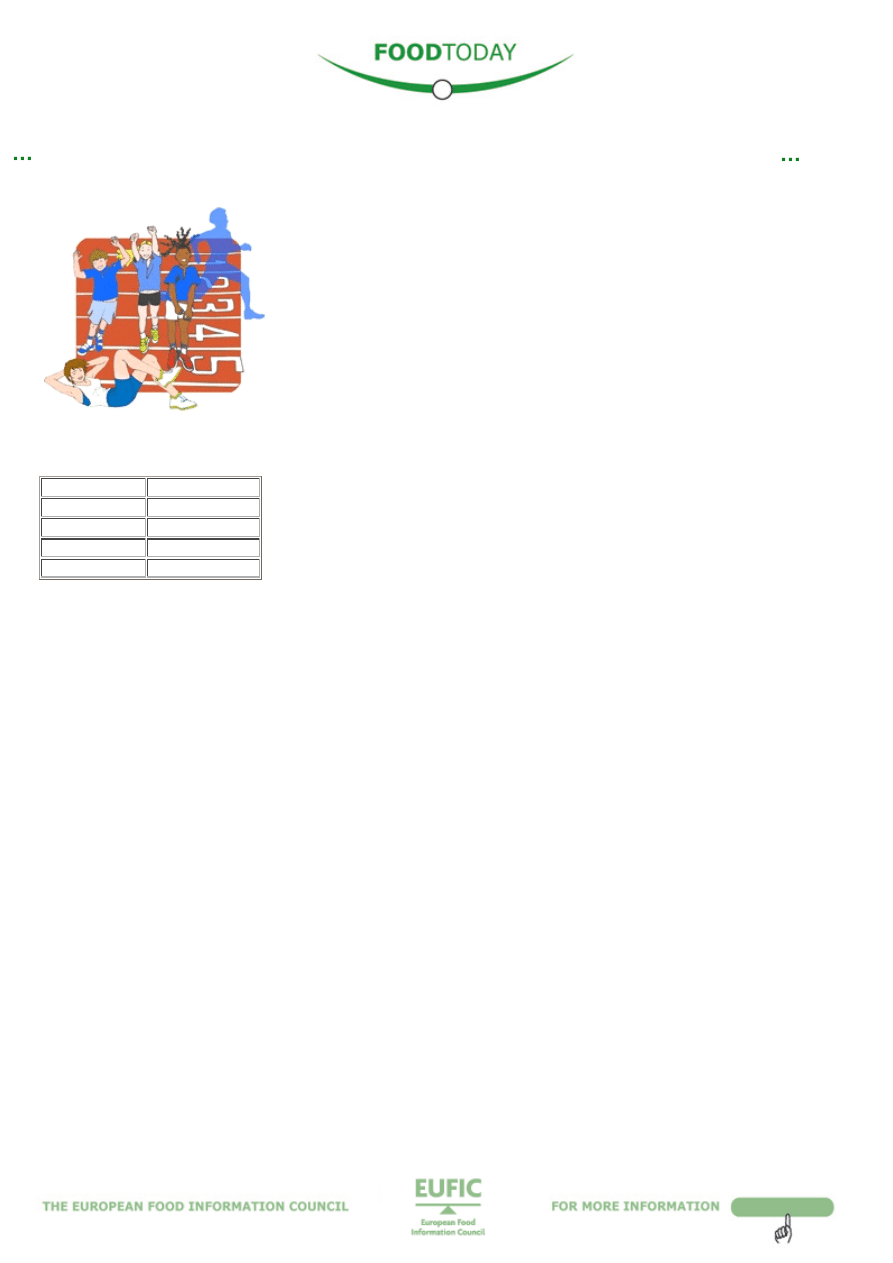
The categories of BMI for adults are as follows:
An important point to remember when using BMI is that it does not take into account how much of the individual is muscle or
fat. Those who are physically fit with a large amount of muscle mass could in fact be classified as obese while their higher
weight is actually due to having more muscle as opposed to high levels of body fat. Researchers tend to agree that body fat
rather than total weight is a better indicator of health status and disease risk. That is why the BMI can be complemented by
measuring waist circumference, which gives an indication of abdominal body fat. Abdominal fat is closely related to various
diseases. The higher the amount of abdominal fat, the higher the risk of getting type II diabetes, hypertension (increased
blood pressure) and coronary heart disease. A healthy male should have a waist circumference below 102 cm whilst a healthy
female should have a waist circumference below 80 cm.
Adipose tissue and physical activity
Adipose tissue is made of fat cells. Due to hormonal influences, males are more likely to accumulate excess body fat around
their waist area, whereas females are more likely to store excess fat in a thin layer under the skin and in the hip and thigh
regions. The more excess body fat that is accumulated, particularly around the waistline, the higher an individual’s risk of
developing health problems.
The physical activity level (PAL) of an individual is calculated as the ratio of their total energy expenditure and their resting
energy expenditure over the course of a day (24 hours). In short, the more active an individual, the higher their PAL. A low
PAL is defined as <1.49, a medium PAL is ~1.5 and a high PAL is >1.9.
Being involved in vigorous physical activity is clearly linked to weight stability.
1,2
Vigorous exercise is any type of exercise
which elevates the heart rate and breathing rate (feeling out of breath) and requires a substantial effort. Examples of vigorous
activities are: running, fast cycling, aerobics and competitive sports such as football, hockey, and volleyball.
Children and adolescents who participate in relatively large amounts of physical activity have lower levels of body fat than
those who do not.
3,4
European children aged 910 years who engaged in vigorous physical activity for more than 40 minutes a
day had lower levels of body fat than those who only engaged in 1018 minutes of vigorous physical activity a day.
2
Studies suggest that a PAL of ~1.8 is needed for minimising any weight gain.
1
This PAL of 1.8 is consistent with moderate
activity, i.e., predominantly standing or walking work such as that seen with housewives, salespersons, waiters, mechanics,
and traders.
5,6
To equate this with the World Health Organisation (WHO) recommendation of 30 minutes of physical activity on
most days of the week, most individuals need to include some extra physical activity in their day. Those who vigorously
exercise will have a higher PAL as they are expending more energy.
In contrast, it has been shown that low and medium PALs are significantly related to an increase in body fat in both males and
females. Accordingly, an individual may need 6090 minutes of walking (briskly) or an equivalent amount of activity a day to
expend enough energy for weight stability.1 Although reducing calorie intake may also help maintain energy balance, it does
not provide the health benefits associated with physical activity.
In conclusion
To reduce levels of body fat and to get the health benefits seen in those who exercise regularly, we should try to make
physical activity a part of everyday living. The WHO recommends at least 30 minutes of regular, moderateintensity physical
The link between intense physical activity and a healthy body weight
BMI
Category
< 18.5
Underweight
18.5 – 24.9
Normal
25 – 29.9
Overweight
30+
Obese
3

activity on most days to reduce the risk of cardiovascular disease and diabetes, colon cancer and breast cancer.
7
More activity
may be required for weight control.
To provide a greater understanding of the important roles played by energy intake and expenditure, EUFIC has developed a
new Energy Balance section on its website where you can learn about your specific energy and physical activity needs.
www.eufic.org/block/en/show/energybalance/
References
1. Erlichman J, Kerbey AL, James WP. (2002). Physical activity and its impact on health outcomes. Paper 2: Prevention of
unhealthy weight gain and obesity by physical activity: an analysis of the evidence. Obesity Reviews 3:273287.
2. Ruiz JR, Rizzo NS, HurtigWennlöf A, Ortega FB, Wärnberg J, Sjöström M. (2006). Relations of total physical activity and
intensity to fitness and fatness in children: the European Heart Health Study. American Journal of Clinical Nutrition 84
(2):299303.
3. Ekelund U, Sardinha LB, Anderssen SA, Harro M, Franks PW, Brage S, Cooper AR, Andersen LB, Riddoch C, Froberg K.
(2004). Associations between objectively assessed physical activity and indicators of body fatness in 9 to 10yold
European children: a populationbased study from 4 distinct regions in Europe (the European Youth Heart Study).
American Journal of Clinical Nutrition 81(6):1449–50.
4. Gutin B, Humphries MC, Barbeau P. (2005). Relations of moderate and vigorous physical activity to fitness and fatness
in adolescents. American Journal of Clinical Nutrition 81(4):746 –50.
5. Black AE, Coward WA, Cole TJ, Prentice AM. (1996). Human energy expenditure in affluent societies: an analysis of 575
doublylabelled water measurements. European Journal of Clinical Nutrition 50:72–92.
6. German Nutrition Society, Austrian Nutrition Society, Swiss Society for Nutrition Research, Swiss Nutrition Association.
(2002). Reference values for nutrient intake. Frankfurt/Main: Umschau/Braus: German Nutrition Society.
7.
http://www.who.int/dietphysicalactivity/pa/en/index.html
4
Cholesterol often gets a bad press and, in a way, that is right because a high
level of bad cholesterol in your blood is a major risk factor for heart disease. A
healthy balanced lifestyle and diet can help reduce the risk of heart disease, but
cholesterol also plays a vital role in keeping the body healthy.
What is cholesterol?
Cholesterol is a waxlike substance, which together with fats and oils belongs to the family
of lipids. It is essential to all our body cells and has a special role in the formation of brain
cells, nerve cells and certain hormones. Although some foods contribute readymade
cholesterol, the majority of cholesterol in the body is manufactured by the liver.
The World Health Organisation (WHO) has estimated that amongst Europeans the average
total cholesterol levels in men vary from 4.5 mmol/l (millimoles per litre) in Turkey to 6.2
mmol/l in Serbia and Montenegro, and in women, average total cholesterol levels range
from 4.6 mmol/l in Turkey to 6.1 mmol/l in Norway.
1
For most people, the recommended
total cholesterol level is <5.0 mmol/l, but for people who already have some degree of cardiovascular disease, this
recommended level is <4.5 mmol/l.
2
Cholesterol and Health
Too much cholesterol in the blood (hypercholesterolaemia) is a major risk factor for coronary heart disease (CHD), which can
lead to a heart attack or stroke. Together, these are the main cause of death in Europe.
3
There are two main types of cholesterol: low density lipoprotein (LDL) cholesterol and high density lipoprotein (HDL)
cholesterol.
LDL cholesterol, often referred to as ‘bad’ cholesterol, carries fat around the body and is big, fluffy and sticky. If circumstances
are favourable, LDL cholesterol gets stuck in the walls of the arteries making them narrower (a process called atherosclerosis).
Such changes, in turn, lead to a higher tendency of the blood to clot. If a clot (thrombus) forms and blocks the narrowed artery
(thrombosis), this can result in a heart attack or stroke. Although LDL is made naturally by the body, some people make too
much. The diet can also affect the amount of LDL cholesterol.
HDL cholesterol, or ‘good’ cholesterol, scavenges for fat and returns it to the liver. Having plenty of HDL cholesterol means that
fatty deposits are less likely to build up in the arteries. A high HDL:LDL ratio, i.e. high levels of HDL cholesterol relative to LDL
cholesterol, protects against heart disease. Being physically active and eating healthier fats can help to raise HDL cholesterol
levels.
Diet, lifestyle and cholesterol
There are several factors that influence blood cholesterol levels. Eating a balanced diet, being of healthy weight and keeping
physically active, in particular, can help to keep cholesterol levels normal.
Dietary cholesterol
Some foods (eggs, liver, kidney and prawns) naturally contain cholesterol (dietary cholesterol). The cholesterol found in foods
in most cases does not influence blood cholesterol levels as much as the amount and type of fat eaten, but some people might
be sensitive to high cholesterol intakes.
Dietary fats
Dietary fat is often divided into saturated and unsaturated fat. In general, most types of saturated fat raise total and LDL
cholesterol levels. Saturated fats are found in butter, lard (and foods made from these including pastries, cakes and biscuits),
meat products (e.g., salami, pies and sausages), cream, cheese and foods containing coconut or palm oils. Some unsaturated
fats can help reduce LDL cholesterol levels, and generally it is a good idea to replace saturated fats with unsaturated fats.
Foods containing unsaturated fats include vegetable and seed oils and spreads (e.g., rapeseed oil, olive oil, soya spread), oily
fish (e.g., mackerel, salmon and herring), nuts and avocado.
Another type of fat, trans fat, is sometimes found in foods that contain partially hydrogenated fats (e.g., some pastry and
biscuits), although many companies in Europe have reduced levels of trans fats in their products to a minimum. Trans fats can
raise LDL (bad) cholesterol levels. Unlike saturated fats, trans fats also lead to a fall in HDL (or good) cholesterol and raise
blood triglyceride levels, both of which are associated with an increased risk of CHD. These negative effects may occur with
longterm intakes of trans fats of 510 g per day.
4,5
Apart from consuming the right fats, it is sensible to try to reduce the amount of fat overall as well, by baking, grilling, boiling,
poaching or steaming foods instead of frying them, and cutting down on foods that are high in fat. Look at the nutrition
information on food labels to compare the fat types and levels, especially saturated fats, in products.
A ‘portfolio’ of foods
In addition to the type of fat we eat, other foods can also help to keep cholesterol levels healthy. Eating plenty of fruits and
vegetables, foods containing soluble fibre (e.g., oats, lentils, beans and peas), tree nuts (e.g., almonds) and soya can be
useful. Note that products on the market containing added plant stanols or plant sterols are designed for people who have
excessive cholesterol levels and are not necessary for people with healthy cholesterol levels. Scientists have found that eating
a healthy lowfat diet, including a ‘portfolio’ of the foods mentioned above, can reduce cholesterol levels by up to 20%.
6
References
Cholesterol: the good, the bad and the average
5

1. WHO (2006). WHO global infobase online. Available at:
http://www.who.int/infobase/report.aspx?
2. Policy Analysis Centre (2007). European Cholesterol Guidelines Report.
Available at:
http://www.policycentre.com/downloads/EuropeanCholesterolGuidelines07.pdf
3. European cardiovascular disease statistics; 2008 edition. European Heart Network, Brussels, 2008.
Available at:
http://www.ehnheart.org/ files/EU%20stats%202008%20final155843A.pdf
4. Hunter JE. (2006). Dietary trans fatty acids: review of recent human studies and food industry responses. Lipids 41
(11):96792.
5. Stender S, Dyerberg J, Astrup A. (2006). High levels of trans fat in popular fast foods. New England Journal of Medicine
354:16501652.
6. Jenkins DJA, Kendall CWC, Marchie A, Faulkner DA, Wong JMW, de Souza R, Emam A, Parker TL, Vidgen E, Trautwein
EA, Lapsley KG, Josse RG, Leiter LA, Singer W, Connelli PW. (2005). Direct comparison of a dietary portfolio of
cholesterol lowering foods with a statin in hypercholesterolemic participants. American Journal of Clinical Nutrition
81:3807
6
Parents’ lack of money, time for cooking, and motivation are some of the
important barriers to achieving a healthy diet in children. Similarly, lack of sports
facilities, intolerant neighbours, and not having a garden can act as barriers to
being more physically active. These are the first results of the European IDEFICS
study (Identification and Prevention of Dietary and LifestyleInduced Health
Effects in Children and Infants).
Contributing to the prevention of childhood obesity in Europe
Childhood obesity and its related health problems are an increasing phenomenon in
Europe. Consequently, the IDEFICS study was set up to improve knowledge about dietary
factors, social environment, and lifestyle affecting children’s health in Europe. This
knowledge will be used to develop, implement, evaluate, and validate specific
interventions for reducing the prevalence of diet and lifestylerelated diseases.
As part of the IDEFICS study, focus groups were held at the child and parent level in eight
countries to gain insight into the factors that affect children’s nutrition and physical
activity. The focus groups’ participants comprised:
l
155 children aged 68 years (81 boys, 74 girls) split into 20 groups of 517 participants
l
106 parents of 24 year old and 83 parents of 68 year old children (28 men, 161 women) split into 36 groups of 512
participants
Barriers to a healthy diet
Not enough time for cooking, lack of money, limited motivation, little time available to spend with the children (to control what
they are eating), grandparents breaking food rules, and the wide availability of energydense, nutrientpoor foods were among
the factors mentioned that can hamper children eating healthily. Lowincome families are more likely to have diets that are
less healthy, where shopping is more influenced by price and taste preferences of the children and food choice rules are less
strict. There are large differences between countries in school rules on food consumption. Sweden has strict and clear rules,
nutritious meals are provided to children and vending machines are regulated. The absence of clear rules is, however,
common in other countries. Generally, there is a lack of nutrition education (except for Belgium and Spain), and eating fruit at
school is not facilitated.
Barriers to physical activity
Common environmental barriers include the lack of facilities, such as playgrounds, gyms, sporting grounds, swimming pools,
green spaces or cycle lanes, as well as safety issues that include too much traffic, the presence of teenage gangs, no or
unclear traffic signs and bad condition of cycle lanes and footpaths. Conditions at school, although variable from country to
country, are not optimal either, due to too short breaks and lack of space to play.
Lack of organised activities for younger children and lack of sports organisations contribute to children doing little physical
activity. Lowincome families regarded the price of doing sports in a sports club as a major obstacle, although they would see
the participation of their children in organised activities as a way to keep them in a safe environment. Generally, the children
were more active during spring and summer.
Tearing down the barriers
Parents most often perceive school as an important facilitator for healthy diet and lifestyles. This is due to the fact that children
spend a significant amount of daytime at school. Nutrition education should thus be included since children from all socio
economic classes could be reached this way. It is also necessary to have a well elaborated and consistent school food policy
that is endorsed by the parents. This is important as parents need to become more aware of their responsibility for improving
their children’s diet and lifestyle.
Environmental changes like the creation of trafficfree zones, or safe streets with footpaths and cycle lanes will help increase
physical activity in children. Organising affordable activities for children will not only take them away from sedentary lifestyles,
but also keep them out of trouble, especially in lowincome families. Schools should make appropriate accommodation and
sports materials available, include active breaks, organise extracurricular activities, and motivate teachers to act as role
models. In Sweden, day care schools already offer such activities for younger children during and after school hours, and in
Hungary schools open their playgrounds for families to do sports activities together. Playing together is highly motivating for
children to go outdoors and be active.
The IDEFICS study continues
The results of the focus groups have been used to develop a communitybased lifestyle strategy that addresses nutrition and
physical activity interventions and is centred around primary and nursery schools. The nutrition intervention will include
education as well as training to develop cooking and shopping skills. For the intervention on physical activity, structured
activities and an environment that supports activity both at school and in the community will be necessary. Improving safety in
the neighbourhood, and largescale actions such as increasing the number of playgrounds or parks or family days, should be
part of a community programme and the focus of negotiations with community leaders. Finally, a healthy parental lifestyle
supporting physical activity and the availability of healthy foods will contribute to a healthier diet and higher activity levels in
their children.
Further information:
Breaking barriers to healthy food choice and physical activity in young
children
7

References
1. Ahrens W, Bammann K, de Henauw S, Halford J, Palou A, Pigeot I, Siani A, Sjostrom M. (2006) Understanding and
preventing childhood obesity and related disorders—IDEFICS: A European multilevel epidemiological approach.
Nutrition, Metabolism and Cardiovascular Diseases 16(4):302308.
2. Identification and prevention of Dietary and lifestyleinduced health EFfects In Children and infantS (IDEFICS).
European Commission Sixth Framework Programme. Contract n° 016181 (FOOD)
.
3. Haerens L, De Bourdeaudhuij I, Barba G, Eiben G, Fernandez J, Hebestreit A, Konstabel K, Kovács É, Lasn H, Regber S,
Shiakou M, De Henauw S, on behalf of the IDEFICS consortium (in press). Developing the IDEFICS community based
intervention program to enhance eating behaviors in 28 year old children: findings from focus groups with children and
parents. Health Education Research.
4. Haerens L, De Bourdeaudhuij I, Eiben G, Barba G, Bel S, Keimer K, Kovács E, Lasn H, Regber S, Shiakou M, Maes L on
behalf of the IDEFICS consortium (submitted). Formative research to develop the IDEFICS physical activity intervention
component: findings from focus groups with children and parents. IJBNPA.
5. EUFIC Food Today n°58 (May 2007) Learning Healthy Living – Development of a European Prevention Strategy.
Available at:
www.eufic.org/article/en/artid/Learnhealthylivingeuropeaninterventionstrategy/
8
Wyszukiwarka
Podobne podstrony:
FOOD TODAY #62 EUFIC
FOOD TODAY #77 EUFIC
FOOD TODAY #71 EUFIC
FOOD TODAY #90 EUFIC
FOOD TODAY #64 EUFIC
FOOD TODAY #66 EUFIC
FOOD TODAY #75 EUFIC
FOOD TODAY #80 EUFIC
FOOD TODAY #73 EUFIC
FOOD TODAY #91 EUFIC
FOOD TODAY #86 EUFIC
FOOD TODAY #83 EUFIC
FOOD TODAY #69 EUFIC
FOOD TODAY #70 EUFIC
FOOD TODAY #74 EUFIC
FOOD TODAY #56 EUFIC
FOOD TODAY #84 EUFIC
FOOD TODAY #67 EUFIC
FOOD TODAY #79 EUFIC
więcej podobnych podstron
